Face Masks to Combat Coronavirus (COVID-19)—Processing, Roles, Requirements, Efficacy, Risk and Sustainability
Abstract
:1. Introduction
2. Role of Face Mask in Combating COVID-19
2.1. Observational Evidence
2.2. Randomized Control Trials
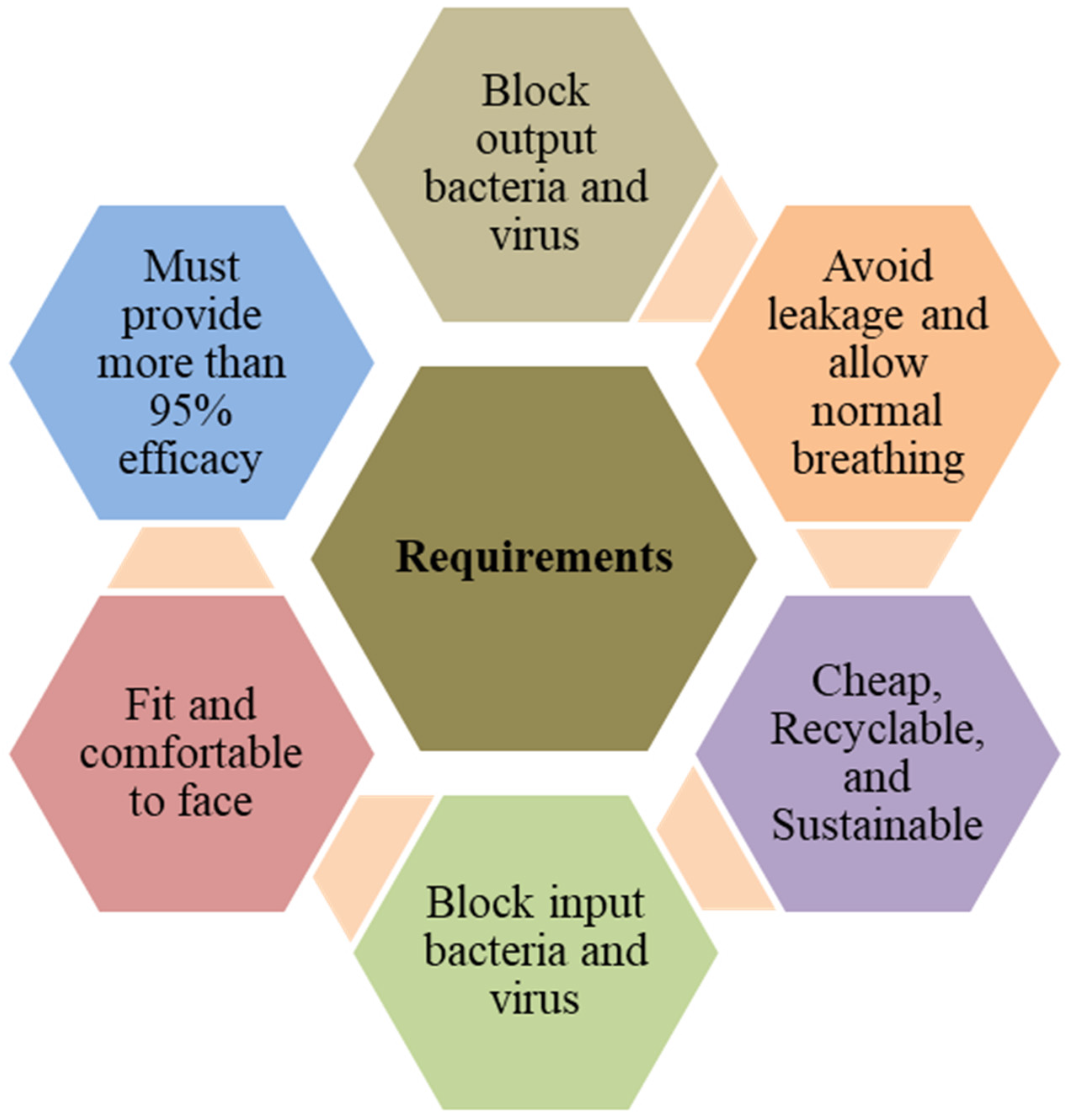
3. Requirements and Types of Face Masks
3.1. Medical Face Masks
3.2. Respirator Masks (N95 and FFP2 Variants)
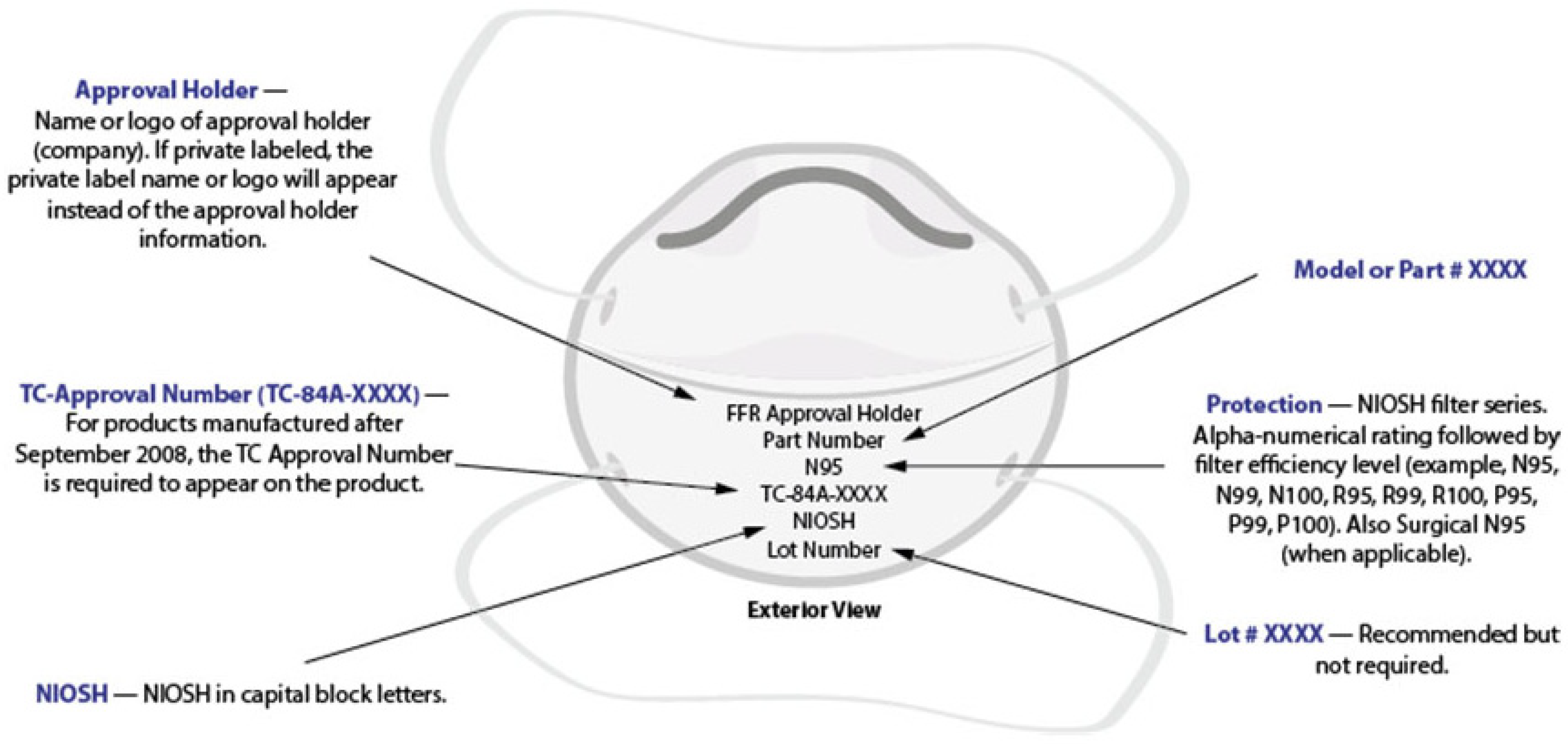
3.3. Single-Use Face Masks
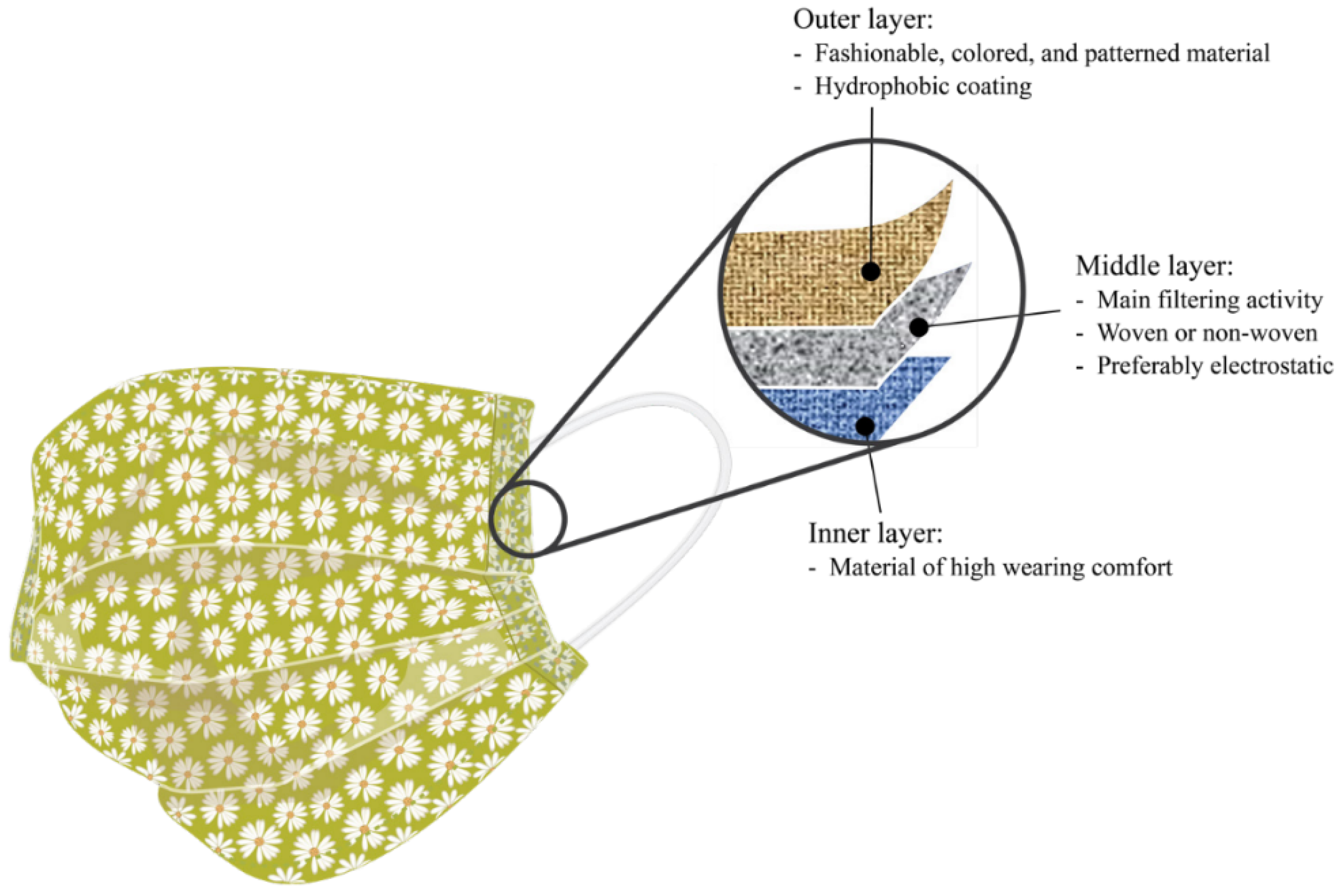
3.4. Cloth Face Mask
- (1)
- Masks for daily usage (temporary fabric masks, Figure 3b): These masks do not protect against infection to the wearer. However, there is a slight risk decrease for droplet transmission, particularly during exhale, which minimizes the possibility of viral spreading. Although these masks are widely suggested for the general public while strolling, shopping, or using public transport, these masks should not be worn in the medical setting.
- (2)
- MNP (medical mouth–nose protection; see Figure 3c): It is also known as a "surgical mask." For preventing infection, strict restrictions govern the industrial manufacture of MNP. The filtering performance is comparable to that of daily use masks, and they are designed to protect patients. They have been authorized for use by medical personnel, and their main purpose is to protect patients from aerosols.
- (3)
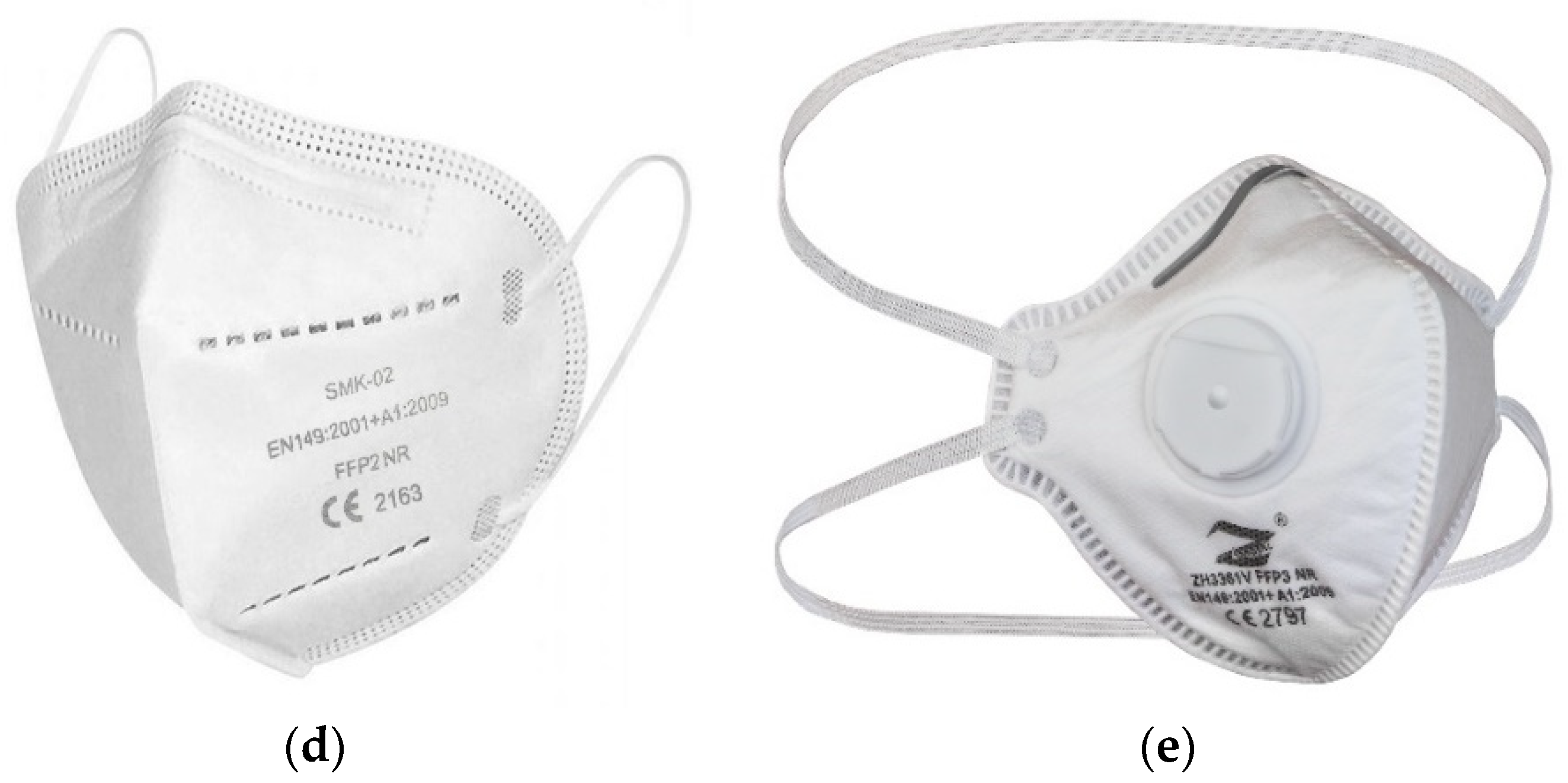
- FFP2 mask (face filtering component, Figure 3d)/N95-mask: FFP2 masks meet stricter safety standards. They shield the wearer’s lungs by preventing more than 95% of particles and droplets from entering the lungs during breathing. As long as there is no exhaling valve, FFP2 masks efficiently protect the environment. In contrast, masks with an exhaling valve enable exhaled air to escape unfiltered, contaminating the environment.
- (4)
- FFP3 mask: FFP3 masks (Figure 3e) protect the user even better than FFP2 because they filter out more than 99% of droplets and particles when inhaled. In the absence of an exhaling valve, FFP3-masks also protect the environment.
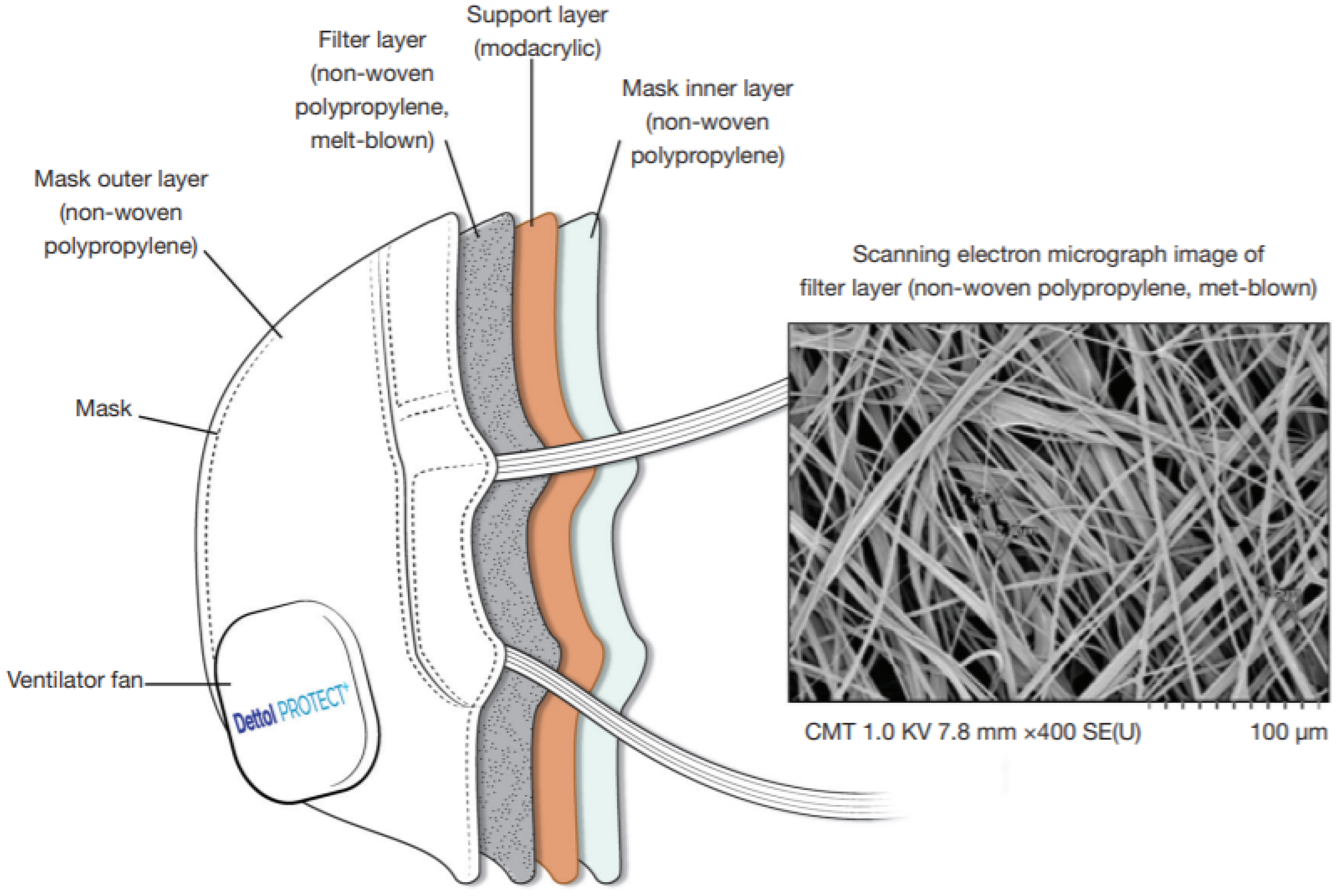
4. Materials and Methods Used in Manufacturing Face Masks
4.1. Mask Materials
4.2. Mask Manufacturing Techniques

5. Efficacy of Currently Available Face Masks
6. Challenges and Risks in Using Face Masks
7. Sustainability of Face Masks in Combatting COVID-19
7.1. Effects of Face Mask Waste Materials
7.1.1. Environmental Effects
7.1.2. Social and Behavioral Effects
7.1.3. Economic Effects
7.2. Sustainable Solutions
7.2.1. Waste Management
7.2.2. Using Sustainable Materials and Techniques
7.2.3. Education and Social Awareness
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wei, Z.-Y.; Qiao, R.; Chen, J.; Huang, J.; Wu, H.; Wang, W.-J.; Yu, H.; Xu, J.; Wang, C.; Gu, C.-H. The influence of pre-existing hypertension on coronavirus disease 2019 patients. Epidemiol. Infect. 2021, 149, e4. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Disease (COVID-19) Pandemic. 2019. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 5 February 2022).
- WHO. Coronavirus (COVID-19) Dashboard. 2020. Available online: https://covid19.who.int/ (accessed on 5 February 2022).
- Abera, A.; Belay, H.; Zewude, A.; Gidey, B.; Nega, D.; Dufera, B.; Abebe, A.; Endriyas, T.; Getachew, B.; Birhanu, H. Establishment of COVID-19 testing laboratory in resource-limited settings: Challenges and prospects reported from Ethiopia. Glob. Health Action 2020, 13, 1841963. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front. Psychol. 2020, 11, 1540. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.D.; Girish, M.; Yadav, G.; Shankar, A.; Yadav, R. Coronavirus disease 2019 and the cardiovascular system: Impacts and implications. Indian Heart J. 2020, 72, 1–6. [Google Scholar] [CrossRef]
- Giannis, D.; Geropoulos, G.; Matenoglou, E.; Moris, D. Impact of coronavirus disease 2019 on healthcare workers: Beyond the risk of exposure. Postgrad. Med. J. 2021, 97, 326–328. [Google Scholar] [CrossRef]
- Rahman, T.; Khandakar, A.; Hoque, M.E.; Ibtehaz, N.; Kashem, S.B.; Masud, R.; Shampa, L.; Hasan, M.M.; Islam, M.T.; Al-Madeed, S. Development and Validation of an Early Scoring System for Prediction of Disease Severity in COVID-19 using Complete Blood Count Parameters. IEEE Access 2021, 9, 120422–120441. [Google Scholar] [CrossRef]
- Gorain, B.; Choudhury, H.; Molugulu, N.; Athawale, R.B.; Kesharwani, P. Fighting strategies against the novel coronavirus pandemic: Impact on global economy. Front. Public Health 2020, 8, 606129. [Google Scholar] [CrossRef]
- Bhat, B.A.; Khan, S.; Manzoor, S.; Niyaz, A.; Tak, H.; Anees, S.; Gull, S.; Ahmad, I. A study on impact of COVID-19 lockdown on psychological health, economy and social life of people in Kashmir. Int. J. Sci. Healthc. Res. 2020, 5, 36–46. [Google Scholar]
- Sohrabi, C.; Alsafi, Z.; O’neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef]
- Shi, L.; Lu, Z.-A.; Que, J.-Y.; Huang, X.-L.; Liu, L.; Ran, M.-S.; Gong, Y.-M.; Yuan, K.; Yan, W.; Sun, Y.-K. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 2020, 3, e2014053. [Google Scholar] [CrossRef]
- Sabino-Silva, R.; Jardim, A.C.G.; Siqueira, W.L. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin. Oral Investig. 2020, 24, 1619–1621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hiscott, J.; Alexandridi, M.; Muscolini, M.; Tassone, E.; Palermo, E.; Soultsioti, M.; Zevini, A. The global impact of the coronavirus pandemic. Cytokine Growth Factor Rev. 2020, 53, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ares, G.; Bove, I.; Vidal, L.; Brunet, G.; Fuletti, D.; Arroyo, Á.; Blanc, M.V. The experience of social distancing for families with children and adolescents during the coronavirus (COVID-19) pandemic in Uruguay: Difficulties and opportunities. Child. Youth Serv. Rev. 2021, 121, 105906. [Google Scholar] [CrossRef]
- Ganesan, B.; Al-Jumaily, A.; Fong, K.N.; Prasad, P.; Meena, S.K.; Tong, R.K.-Y. Impact of Coronavirus Disease 2019 (COVID-19) outbreak quarantine, isolation, and lockdown policies on mental health and suicide. Front. Psychiatry 2021, 12, 565190. [Google Scholar] [CrossRef]
- Qiu, Y.; Chen, X.; Shi, W. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (COVID-19) in China. J. Popul. Econ. 2020, 33, 1127–1172. [Google Scholar] [CrossRef]
- Milman, E.; Lee, S.A.; Neimeyer, R.A. Social isolation and the mitigation of coronavirus anxiety: The mediating role of meaning. Death Stud. 2020, 46, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Helm, D. The environmental impacts of the coronavirus. Environ. Resour. Econ. 2020, 76, 21–38. [Google Scholar] [CrossRef]
- Sarkodie, S.A.; Owusu, P.A. Global assessment of environment, health and economic impact of the novel coronavirus (COVID-19). Environ. Dev. Sustain. 2021, 23, 5005–5015. [Google Scholar] [CrossRef] [PubMed]
- Isaifan, R. The dramatic impact of Coronavirus outbreak on air quality: Has it saved as much as it has killed so far? Glob. J. Environ. Sci. Manag. 2020, 6, 275–288. [Google Scholar]
- Rupani, P.F.; Nilashi, M.; Abumalloh, R.; Asadi, S.; Samad, S.; Wang, S. Coronavirus pandemic (COVID-19) and its natural environmental impacts. Int. J. Environ. Sci. Technol. 2020, 17, 4655–4666. [Google Scholar] [CrossRef]
- Sukharev, O.S. Economic crisis as a consequence COVID-19 virus attack: Risk and damage assessment. Quant. Financ. Econ. 2020, 4, 274–293. [Google Scholar] [CrossRef]
- Grignoli, N.; Petrocchi, S.; Bernardi, S.; Massari, I.; Traber, R.; Malacrida, R.; Gabutti, L. Influence of empathy disposition and risk perception on the psychological impact of lockdown during the coronavirus disease pandemic outbreak. Front. Public Health 2020, 8, 567337. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef] [PubMed]
- WHO. Coronavirus Disease (COVID-19) Advice for the Public: When and How to Use Masks. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks (accessed on 5 February 2022).
- Wu, L.-T. A treatise on pneumonic plague. In A Treatise on Pneumonic Plague; League of Nations Health Organization: Geneva, Switzerland, 1926. [Google Scholar]
- Goh, L.; Ho, T.; Phua, K. Wisdom and western science: The work of Dr Wu Lien-Teh. Asia Pac. J. Public Health 1987, 1, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Tian, H.; Zhang, L.; Zhang, M.; Guo, D.; Wu, W.; Zhang, X.; Kan, G.L.; Jia, L.; Huo, D. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: A cohort study in Beijing, China. BMJ Glob. Health 2020, 5, e002794. [Google Scholar] [CrossRef]
- Usher Institute, The University of Edinburgh. Does the Use of Face Masks in the General Population Make a Difference to Spread of Infection? 2020. Available online: https://www.ed.ac.uk/files/atoms/files/uncover_003-03_summary_-_facemasks_community_anon.pdf (accessed on 5 February 2022).
- Gupta, M.; Gupta, K.; Gupta, S. The use of face masks by the general population to prevent transmission of COVID-19 infection: A systematic review. medRxiv 2020. [Google Scholar] [CrossRef]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J.; El-harakeh, A.; Bognanni, A.; Lotfi, T.; Loeb, M. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Wu, J.; Xu, F.; Zhou, W.; Feikin, D.R.; Lin, C.-Y.; He, X.; Zhu, Z.; Liang, W.; Chin, D.P.; Schuchat, A. Risk factors for SARS among persons without known contact with SARS patients, Beijing, China. Emerg. Infect. Dis. 2004, 10, 210. [Google Scholar] [CrossRef]
- Jefferson, T.; Del Mar, C.B.; Dooley, L.; Ferroni, E.; Al-Ansary, L.A.; Bawazeer, G.A.; Van Driel, M.L.; Jones, M.A.; Thorning, S.; Beller, E.M.; et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst. Rev. 2020, 11, CD006207. [Google Scholar]
- MacIntyre, C.R.; Chughtai, A.A. A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. Int. J. Nurs. Stud. 2020, 108, 103629. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Dwyer, D.; Seale, H.; Fasher, M.; Booy, R.; Cheung, P.; Ovdin, N.; Browne, G. The first randomized, controlled clinical trial of mask use in households to prevent respiratory virus transmission. Int. J. Infect. Dis. 2008, 12, e328. [Google Scholar] [CrossRef]
- Suess, T.; Remschmidt, C.; Schink, S.B.; Schweiger, B.; Nitsche, A.; Schroeder, K.; Doellinger, J.; Milde, J.; Haas, W.; Koehler, I. The role of facemasks and hand hygiene in the prevention of influenza transmission in households: Results from a cluster randomised trial; Berlin, Germany, 2009–2011. BMC Infect. Dis. 2012, 12, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Cowling, B.J.; Chan, K.-H.; Fang, V.J.; Cheng, C.K.; Fung, R.O.; Wai, W.; Sin, J.; Seto, W.H.; Yung, R.; Chu, D.W. Face masks and hand hygiene to prevent influenza transmission in households: A cluster randomized trial. Ann. Intern. Med. 2009, 151, 437–446. [Google Scholar] [CrossRef] [Green Version]
- Aiello, A.E.; Murray, G.F.; Perez, V.; Coulborn, R.M.; Davis, B.M.; Uddin, M.; Shay, D.K.; Waterman, S.H.; Monto, A.S. Mask use, hand hygiene, and seasonal influenza-like illness among young adults: A randomized intervention trial. J. Infect. Dis. 2010, 201, 491–498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aiello, A.E.; Perez, V.; Coulborn, R.M.; Davis, B.M.; Uddin, M.; Monto, A.S. Face masks, hand hygiene, and influenza among young adults: A randomized intervention trial. PLoS ONE 2012, 7, e29744. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Robertson, P. Comparison of Mask Standards, Ratings, and Filtration Effectiveness. 2021. Available online: https://smartairfilters.com/en/blog/comparison-mask-standards-rating-effectiveness/ (accessed on 1 January 2022).
- Ghosh, S. Composite nonwovens in medical applications. Compos. Non-Woven Mater. 2014, 211–224. [Google Scholar] [CrossRef]
- Garcia, R.A.; Stevanovic, T.; Berthier, J.; Njamen, G.; Tolnai, B.; Achim, A. Cellulose, Nanocellulose, and Antimicrobial Materials for the Manufacture of Disposable Face Masks: A Review. BioResources 2021, 16, 4321–4353. [Google Scholar] [CrossRef]
- Ogbuoji, E.A.; Zaky, A.M.; Escobar, I.C. Advanced Research and Development of Face Masks and Respirators Pre and Post the Coronavirus Disease 2019 (COVID-19) Pandemic: A Critical Review. Polymers 2021, 13, 1998. [Google Scholar] [CrossRef]
- Konda, A.; Prakash, A.; Moss, G.A.; Schmoldt, M.; Grant, G.D.; Guha, S. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS Nano 2020, 14, 6339–6347. [Google Scholar] [CrossRef]
- Occupational Exposure to COVID-19; Emergency Temporary Standard. 2021. Available online: https://www.federalregister.gov/documents/2021/06/21/2021-12428/occupational-exposure-to-covid-19-emergency-temporary-standard (accessed on 1 May 2021).
- 3M Company. Comparison of P2, FFP2, KN95, and N95 and Other Filtering Facepiece Respirator Classes; 3M Company: St. Paul, MN, USA, 2021. [Google Scholar]
- NIOSH-Approved Particulate Filtering Facepiece Respirators. 2021. Available online: https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/default.html (accessed on 3 October 2021).
- Ottawa Public Health. Ways to Have Better Fit and Extra Protection with Cloth and Disposable Masks; Ottawa Public Health: Nepean, ON, Canada, 2022; Available online: https://www.ottawapublichealth.ca/en/public-health-topics/masks.aspx (accessed on 8 January 2022).
- Matuschek, C.; Moll, F.; Fangerau, H.; Fischer, J.C.; Zänker, K.; van Griensven, M.; Schneider, M.; Kindgen-Milles, D.; Knoefel, W.T.; Lichtenberg, A. Face masks: Benefits and risks during the COVID-19 crisis. Eur. J. Med. Res. 2020, 25, 1–8. [Google Scholar] [CrossRef]
- Armentano, I.; Barbanera, M.; Carota, E.; Crognale, S.; Marconi, M.; Rossi, S.; Rubino, G.; Scungio, M.; Taborri, J.; Calabro, G. Polymer materials for respiratory protection: Processing, end use, and testing methods. ACS Appl. Polym. Mater. 2021, 3, 531–548. [Google Scholar] [CrossRef]
- Wibisono, Y.; Fadila, C.R.; Saiful, S.; Bilad, M.R. Facile approaches of polymeric face masks reuse and reinforcements for micro-aerosol droplets and viruses filtration: A review. Polymers 2020, 12, 2516. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, W.; Jiang, R.; Guo, C. Antiviral Electrospun Polymer Composites: Recent Advances and Opportunities for Tackling COVID-19. Front. Mater. 2021, 8, 470. [Google Scholar] [CrossRef]
- Rahman, M.Z. Influence of Fiber Treatment on the Damping Performance of Plant Fiber Composites. In Vibration and Damping Behavior of Biocomposites; CRC Press: Boca Raton, FL, USA, 2022; pp. 113–135. [Google Scholar]
- Rahman, M.Z.; Mace, B.R.; Jayaraman, K. Vibration damping of natural fibre-reinforced composite materials. In Proceedings of the 17th European Conference on Composite Material, Munich, Germany, 26–30 June 2016. [Google Scholar]
- Selvaranjan, K.; Navaratnam, S.; Rajeev, P.; Ravintherakumaran, N. Environmental challenges induced by extensive use of face masks during COVID-19: A review and potential solutions. Environ. Chall. 2021, 3, 100039. [Google Scholar] [CrossRef]
- Rahman, M.Z. Mechanical and damping performances of flax fibre composites–A review. Compos. Part C Open Access 2021, 4, 100081. [Google Scholar] [CrossRef]
- Rahman, M.Z.; Jayaraman, K.; Mace, B.R. Vibration damping of flax fibre-reinforced polypropylene composites. Fibers Polym. 2017, 18, 2187–2195. [Google Scholar] [CrossRef]
- Seidi, F.; Deng, C.; Zhong, Y.; Liu, Y.; Huang, Y.; Li, C.; Xiao, H. Functionalized Masks: Powerful Materials against COVID-19 and Future Pandemics. Small 2021, 17, 2102453. [Google Scholar] [CrossRef]
- Rahman, M.Z.; Jayaraman, K.; Mace, B.R. Impact energy absorption of flax fiber-reinforced polypropylene composites. Polym. Compos. 2018, 39, 4165–4175. [Google Scholar] [CrossRef]
- Rahman, M.Z.; Jayaraman, K.; Mace, B.R. Influence of damping on the bending and twisting modes of flax fibre-reinforced polypropylene composite. Fibers Polym. 2018, 19, 375–382. [Google Scholar] [CrossRef]
- Jung, S.; Lee, S.; Dou, X.; Kwon, E.E. Valorization of disposable COVID-19 mask through the thermo-chemical process. Chem. Eng. J. 2021, 405, 126658. [Google Scholar] [CrossRef]
- Rahman, M.Z. Fabrication, Morphologies and Properties of Single Polymer Composites Based on LLDPE, PP, and CNT Loaded PBT; University of Auckland: Auckland, New Zealand, 2013. [Google Scholar]
- Rahman, M.Z. Static and Dynamic Characterisation of Flax Fibre-Reinforced Polypropylene Composites. Ph.D. Thesis, University of Auckland, Auckland, New Zealand, 2017. [Google Scholar]
- Amini, G.; Karimi, M.; Zokaee Ashtiani, F. Hybrid electrospun membrane based on poly (vinylidene fluoride)/poly (acrylic acid)–poly (vinyl alcohol) hydrogel for waterproof and breathable applications. J. Ind. Text. 2020, 1528083720904675. [Google Scholar] [CrossRef]
- O’Dowd, K.; Nair, K.M.; Forouzandeh, P.; Mathew, S.; Grant, J.; Moran, R.; Bartlett, J.; Bird, J.; Pillai, S.C. Face masks and respirators in the fight against the COVID-19 pandemic: A review of current materials, advances and future perspectives. Materials 2020, 13, 3363. [Google Scholar] [CrossRef] [PubMed]
- Adanur, S.; Jayswal, A. Filtration mechanisms and manufacturing methods of face masks: An overview. J. Ind. Text. 2020, 22, 1528083720980169. [Google Scholar] [CrossRef]
- Kulmala, I.; Heinonen, K.; Salo, S. Improving Filtration Efficacy of Medical Face Masks. Aerosol Air Qual. Res. 2021, 21, 210043. [Google Scholar] [CrossRef]
- Shimasaki, N.; Okaue, A.; Morimoto, M.; Uchida, Y.; Koshiba, T.; Tsunoda, K.; Arakawa, S.; Shinohara, K. A multifaceted evaluation on the penetration resistance of protective clothing fabrics against viral liquid drops without pressure. Biocontrol Sci. 2020, 25, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Chua, M.H.; Cheng, W.; Goh, S.S.; Kong, J.; Li, B.; Lim, J.Y.; Mao, L.; Wang, S.; Xue, K.; Yang, L. Face masks in the new COVID-19 normal: Materials, testing, and perspectives. Research 2020, 2020, 7286735. [Google Scholar] [CrossRef] [PubMed]
- Babaahmadi, V.; Amid, H.; Naeimirad, M.; Ramakrishna, S. Biodegradable and multifunctional surgical face masks: A brief review on demands during COVID-19 pandemic, recent developments, and future perspectives. Sci. Total Environ. 2021, 798, 149233. [Google Scholar] [CrossRef]
- Mukhopadhyay, A. Composite nonwovens in filters: Applications. In Composite Non-Woven Materials; Elsevier: Amsterdam, The Netherlands, 2014; pp. 164–210. [Google Scholar]
- Davison, A.M. Pathogen inactivation and filtration efficacy of a new anti-microbial and anti-viral surgical facemask and N95 against dentistry-associated microorganisms. Int. Dent. Australas. Ed. 2012, 7, 36–42. [Google Scholar]
- Chellamani, K.; Veerasubramanian, D.; Balaji, R.V. Surgical face masks: Manufacturing methods and classification. J. Acad. Ind. Res. 2013, 2, 320–324. [Google Scholar]
- Zhao, M.; Liao, L.; Xiao, W.; Yu, X.; Wang, H.; Wang, Q.; Lin, Y.L.; Kilinc-Balci, F.S.; Price, A.; Chu, L. Household materials selection for homemade cloth face coverings and their filtration efficiency enhancement with triboelectric charging. Nano Lett. 2020, 20, 5544–5552. [Google Scholar] [CrossRef]
- Essa, W.K.; Yasin, S.A.; Saeed, I.A.; Ali, G.A. Nanofiber-Based Face Masks and Respirators as COVID-19 Protection: A Review. Membranes 2021, 11, 250. [Google Scholar] [CrossRef] [PubMed]
- Epps, H.H.; Leonas, K.K. Pore size and air permeability of four nonwoven fabrics. Int. Nonwovens J. 2000, 9, 18–22. [Google Scholar] [CrossRef]
- Verma, D. Effectiveness of Masks: Fast Answers with Automated SEM Analysis; Nanoscience Instruments: Phoenix, AZ, USA, 2021; Available online: https://www.nanoscience.com/applications/materials-science/effectiveness-of-masks-fast-answers-with-automated-sem-analysis/ (accessed on 15 January 2022).
- Nuge, T.; Tshai, K.Y.; Lim, S.S.; Nordin, N.; Hoque, M.E. Characterization and optimization of the mechanical properties of electrospun gelatin nanofibrous scaffolds. World J. Eng. 2020, 17, 12–20. [Google Scholar] [CrossRef]
- Majumder, S.; Sharif, A.; Hoque, M.E. Electrospun cellulose acetate nanofiber: Characterization and applications. In Advanced Processing, Properties, and Applications of Starch and Other Bio-Based Polymers; Faris, M.A., Sapuan, S.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 139–155. [Google Scholar]
- Pradeep, S.A.; Kumar, G.P.; Phani, A.R.; Prasad, R.G.S.V.; Hoque, M.E.; Raghavendra, H.L. Fabrication, characterization and in vitro osteogenic potential of polyvinyl pyrrolidone-titania (PVP-TiO) nanofibers. Anal. Chem. Lett. 2015, 5, 61–72. [Google Scholar] [CrossRef]
- Hoque, M.E.; Peiris, A.M.; Rahman, S.M.A.; Wahab, M.A. New Generation Antibacterial Nanofibrous Membrane For Potential Water Filtration. Curr. Anal. Chem. 2018, 14, 278–284. [Google Scholar] [CrossRef]
- Alayande, A.B.; Kang, Y.; Jang, J.; Jee, H.; Lee, Y.-G.; Kim, I.S.; Yang, E. Antiviral Nanomaterials for Designing Mixed Matrix Membranes. Membranes 2021, 11, 458. [Google Scholar] [CrossRef]
- Palmieri, L.; Vanacore, N.; Donfrancesco, C.; Lo Noce, C.; Canevelli, M.; Punzo, O.; Raparelli, V.; Pezzotti, P.; Riccardo, F.; Bella, A.; et al. Clinical characteristics of hospitalized individuals dying with COVID-19 by age group in Italy. J. Gerontol. Ser. A. 2020, 75, 1796–1800. [Google Scholar] [CrossRef] [PubMed]
- Stan, A.; Steiner, S.; Majeed, S.; Weber, S.S.; Gosh, S.; Semren, T.Ž.; Guy, P.A.; Lebrun, S.; Steinhauser, J.; Tardy, Y.; et al. Aerosol filtration testing of fabrics for development of reusable face masks. Aerosol Air Qual. Research 2021, 21, 210052. [Google Scholar] [CrossRef]
- Tsai, P.P.; Schreuder-Gibson, H.; Gibson, P. Different electrostatic methods for making electret filters. J. Electrost. 2002, 54, 333–341. [Google Scholar] [CrossRef]
- Chowdhury, M.A.; Shuvho, M.B.; Shahid, M.A.; Haque, A.M.; Kashem, M.A.; Lam, S.S.; Ong, H.C.; Uddin, M.A.; Mofijur, M. Prospect of biobased antiviral face mask to limit the coronavirus outbreak. Environ. Res. 2021, 192, 110294. [Google Scholar] [CrossRef]
- Jain, M.; Kim, S.T.; Xu, C.; Li, H.; Rose, G. Efficacy and use of cloth masks: A scoping review. Cureus 2020, 12, 10423. [Google Scholar] [CrossRef]
- Darby, S.; Chulliyallipalil, K.; Przyjalgowski, M.; McGowan, P.; Jeffers, S.; Giltinan, A.; Lewis, L.; Smith, N.; Sleator, R.D. COVID-19: Mask efficacy is dependent on both fabric and fit. Future Microbiol. 2021, 16, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Gierthmuehlen, M.; Kuhlenkoetter, B.; Parpaley, Y.; Gierthmuehlen, S.; Köhler, D.; Dellweg, D. Evaluation and discussion of handmade face-masks and commercial diving-equipment as personal protection in pandemic scenarios. PLoS ONE 2020, 15, e0237899. [Google Scholar] [CrossRef]
- Formentini, G.; Rodríguez, N.B.; Favi, C.; Marconi, M. Challenging the engineering design process for the development of facial masks in the constraint of the COVID-19 pandemic. Procedia Cirp. 2021, 100, 660–665. [Google Scholar] [CrossRef]
- Lindsley, W.G.; Blachere, F.M.; Law, B.F.; Beezhold, D.H.; Noti, J.D. Efficacy of face masks, neck gaiters and face shields for reducing the expulsion of simulated cough-generated aerosols. Aerosol Sci. Technol. 2021, 55, 449–457. [Google Scholar] [CrossRef]
- Mboowa, G.; Semugenze, D.; Nakabuye, H.; Bulafu, D.; Aruhomukama, D. Efficacy of Face Masks Used in Uganda: A Laboratory-Based Inquiry during the COVID-19 Pandemic. Am. J. Trop. Med. Hyg. 2021, 104, 1703. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Pinto, R.; Saha, A.; Chaudhuri, S.; Basu, S. On secondary atomization and blockage of surrogate cough droplets in single-and multilayer face masks. Sci. Adv. 2021, 7, eabf0452. [Google Scholar] [CrossRef] [PubMed]
- Teesing, G.R.; van Straten, B.; de Man, P.; Horeman-Franse, T. Is there an adequate alternative to commercially manufactured face masks? A comparison of various materials and forms. J. Hosp. Infect. 2020, 106, 246–253. [Google Scholar] [CrossRef]
- Wilson, A.M.; Abney, S.E.; King, M.F.; Weir, M.H.; López-García, M.; Sexton, J.D.; Dancer, S.J.; Proctor, J.; Noakes, C.J.; Reynolds, K.A. COVID-19 and use of non-traditional masks: How do various materials compare in reducing the risk of infection for mask wearers? J. Hosp. Infect. 2020, 105, 640–642. [Google Scholar] [CrossRef]
- Fischer, E.P.; Fischer, M.C.; Grass, D.; Henrion, I.; Warren, W.S.; Westman, E. Low-cost measurement of face mask efficacy for filtering expelled droplets during speech. Sci. Adv. 2020, 6, 1–5. [Google Scholar] [CrossRef]
- Aydin, O.; Emon, B.; Cheng, S.; Hong, L.; Chamorro, L.P.; Saif, M.T.A. Performance of fabrics for home-made masks against the spread of COVID-19 through droplets: A quantitative mechanistic study. Extrem. Mech. Lett. 2020, 40, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Serfozo, N.; Ondrácek, J.; Zíková, N.; Lazaridis, M.; Ždímal, V. Size-resolved penetration of filtering materials from CE-marked filtering facepiece respirators. Aerosol Air Qual. Res. 2017, 17, 1305–1315. [Google Scholar] [CrossRef]
- Ippolito, M.; Vitale, F.; Accurso, G.; Iozzo, P.; Gregoretti, C.; Giarratano, A.; Cortegiani, A. Medical masks and Respirators for the Protection of Healthcare Workers from SARS-CoV-2 and other viruses. Pulmonology 2020, 26, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Scully, J.R.; Hutchison, M.; Santucci, R.J., Jr. The COVID-19 Pandemic, Part 2: Understanding the efficacy of oxidized copper compounds in suppressing infectious aerosol-based virus transmission. Corrosion 2021, 77, 370–375. [Google Scholar] [CrossRef]
- Bhimaraju, H.; Jain, R.; Nag, N. Low-Cost Enhancement of Facial Mask Filtration to Prevent Transmission of COVID-19. Biom. Biostat. Int. J. 2020, 9, 169–177. [Google Scholar] [CrossRef]
- Lima, M.M.D.S.; Cavalcante, F.M.L.; Macêdo, T.S.; Galindo-Neto, N.M.; Caetano, J.Á.; Barros, L.M. Cloth face masks to prevent COVID-19 and other respiratory infections. Rev. Lat. Am. De Enferm. 2020, 28. [Google Scholar] [CrossRef]
- Grover, C. Efficacy of face masks depends on spatial relation between host and recipient and who is being protected. BMJ 2020, 369, m2016. [Google Scholar] [CrossRef]
- Ronen, A.; Rotter, H.; Elisha, S.; Sevilia, S.; Parizer, B.; Hafif, N.; Manor, A. Investigation of the protection efficacy of face shields against aerosol cough droplets. J. Occup. Environ. Hyg. 2021, 18, 72–83. [Google Scholar] [CrossRef]
- Jefferson, T.; Foxlee, R.; Del Mar, C.; Dooley, L.; Ferroni, E.; Hewak, B.; Prabhala, A.; Nair, S.; Rivetti, A. Physical interventions to interrupt or reduce the spread of respiratory viruses: Systematic review. BMJ 2008, 336, 77–80. [Google Scholar] [CrossRef] [Green Version]
- Zhou, S.S.; Lukula, S.; Chiossone, C.; Nims, R.W.; Suchmann, D.B.; Ijaz, M.K. Assessment of a respiratory face mask for capturing air pollutants and pathogens including human influenza and rhinoviruses. J. Thorac. Dis. 2018, 10, 2059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verbeek, J.H.; Rajamaki, B.; Ijaz, S.; Sauni, R.; Toomey, E.; Blackwood, B.; Tikka, C.; Ruotsalainen, J.H.; Balci, F.S.K. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst. Rev. 2020, 4, CD011621. [Google Scholar] [PubMed]
- Tirupathi, R.; Bharathidasan, K.; Palabindala, V.; Salim, S.A.; Al-Tawfiq, J.A. Comprehensive review of mask utility and challenges during the COVID-19 pandemic. Infez Med. 2020, 28, 57–63. [Google Scholar]
- Tucho, G.T.; Kumsa, D.M. Universal Use of Face Masks and Related Challenges During COVID-19 in Developing Countries. Risk Manag. Healthc. Policy 2021, 14, 511–517. [Google Scholar] [CrossRef] [PubMed]
- De Man, P.; van Straten, B.; van den Dobbelsteen, J.; Van Der Eijk, A.; Horeman, T.; Koeleman, H. Sterilization of disposable face masks by means of standardized dry and steam sterilization processes; an alternative in the fight against mask shortages due to COVID-19. J. Hosp. Infect. 2020, 105, 356–357. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Cloth Masks and Mask Sterilisation as Options in Case of Shortage of Surgical Masks and Respirators; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2020.
- Lowe, J.J.; Paladino, K.D.; Farke, J.D.; Boulter, K.; Cawcutt, K.; Emodi, M.; Gibbs, S.; Hankins, R.; Hinkle, L.; Micheels, T.; et al. N95 Filtering Facepiece Respirator Ultraviolet Germicidal Irradiation (Uvgi) Process for Decontamination and Reuse; University of Nebraska Medical Center: Omaha, NE, USA, 2020; pp. 1–19. [Google Scholar]
- Ma, Q.X.; Shan, H.; Zhang, C.M.; Zhang, H.L.; Li, G.M.; Yang, R.M.; Chen, J.M. Decontamination of face masks with steam for mask reuse in fighting the pandemic COVID-19: Experimental supports. J. Med. Virol. 2020, 92, 1971–1974. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, A.; Stiegel, M.; Greeson, N.; Vogel, A.; Thomann, W.; Brown, M.; Sempowski, G.D.; Alderman, T.S.; Condreay, J.P.; Burch, J.; et al. Decontamination and reuse of N95 respirators with hydrogen peroxide vapor to address worldwide personal protective equipment shortages during the SARS-CoV-2 (COVID-19) pandemic. Appl. Biosaf. 2020, 25, 67–70. [Google Scholar] [CrossRef]
- Wehlage, D.; Blattner, H.; Sabantina, L.; Böttjer, R.; Grothe, T.; Rattenholl, A.; Gudermann, F.; Lütkemeyer, D.; Ehrmann, A. Sterilization of PAN/gelatin nanofibrous mats for cell growth. Tekstilec 2019, 62, 77–88. [Google Scholar] [CrossRef]
- Mackenzie, D. Reuse of N95 Masks. Engineering 2020, 6, 593–596. [Google Scholar] [CrossRef]
- Coffey, C.; D’Alessandro, M.M.; Cichowicz, J.K. Respiratory Protection During Outbreaks: Respirators versus Surgical Mask. Available online: https://blogs.cdc.gov/niosh-science-blog/2020/04/09/masks-v-respirators/ (accessed on 10 January 2022).
- Das, O.; Neisiany, R.E.; Capezza, A.J.; Hedenqvist, M.S.; Försth, M.; Xu, Q.; Jiang, L.; Ji, D.; Ramakrishna, S. The need for fully bio-based facemasks to counter coronavirus outbreaks: A perspective. Sci. Total Environ. 2020, 736, 139611. [Google Scholar] [CrossRef]
- Zhang, D.; Liu, X.; Huang, W.; Li, J.; Wang, C.; Zhang, D.; Zhang, C. Microplastic pollution in deep-sea sediments and organisms of the Western Pacific Ocean. Environ. Pollut. 2020, 259, 113948. [Google Scholar] [CrossRef]
- Sangkham, S. Face mask and medical waste disposal during the novel COVID-19 pandemic in Asia. Case Stud. Chem. Environ. Eng. 2020, 2, 100052. [Google Scholar] [CrossRef]
- Allison, A.L.; Ambrose-Dempster, E.; Aparsi, T.D.; Bawn, M.; Casas Arredondo, M.; Chau, C.; Chandler, K.; Dobrijevic, D.; Hailes, H.; Lettieri, P. The Environmental Dangers of Employing Single-Use Face Masks as Part of a COVID-19 Exit Strategy; UCL Press: London, UK, 2020; Volume 3, pp. 1–43. [Google Scholar]
- Abbasi, S.A.; Khalil, A.B.; Arslan, M. Extensive use of face masks during COVID-19 pandemic:(micro-) plastic pollution and potential health concerns in the Arabian Peninsula. Saudi J. Biol. Sci. 2020, 27, 3181–3186. [Google Scholar] [CrossRef] [PubMed]
- Webb, H.K.; Arnott, J.; Crawford, R.J.; Ivanova, E.P. Plastic degradation and its environmental implications with special reference to poly (ethylene terephthalate). Polymers 2013, 5, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Kumar, H.; Azad, A.; Gupta, A.; Sharma, J.; Bherwani, H.; Labhsetwar, N.K.; Kumar, R. COVID-19 Creating another problem? Sustainable solution for PPE disposal through LCA approach. Environ. Dev. Sustain. 2021, 23, 9418–9432. [Google Scholar] [CrossRef]
- Roy, P.; Mohanty, A.K.; Wagner, A.; Sharif, S.; Khalil, H.; Misra, M. Impacts of COVID-19 Outbreak on the Municipal Solid Waste Management: Now and beyond the Pandemic. ACS Environ. Au. 2021, 1, 32–45. [Google Scholar] [CrossRef]
- Betsch, C.; Korn, L.; Sprengholz, P.; Felgendreff, L.; Eitze, S.; Schmid, P.; Böhm, R. Social and behavioral consequences of mask policies during the COVID-19 pandemic. Proc. Natl. Acad. Sci. USA 2020, 117, 21851–21853. [Google Scholar] [CrossRef]
- Carbon, C.-C. Wearing face masks strongly confuses counterparts in reading emotions. Front. Psychol. 2020, 11, 2526. [Google Scholar] [CrossRef]
- Marini, M.; Ansani, A.; Paglieri, F.; Caruana, F.; Viola, M. The impact of facemasks on emotion recognition, trust attribution and re-identification. Sci. Rep. 2021, 11, 1–14. [Google Scholar] [CrossRef]
- NIST. NIST Launches Studies into Masks’ Effect on Face Recognition Software; NIST: Gaithersburg, MD, USA, 2020. Available online: https://www.nist.gov/news-events/news/2020/07/nist-launches-studies-masks-effect-face-recognition-software (accessed on 10 September 2021).
- Prata, J.C.; Silva, A.L.; Walker, T.R.; Duarte, A.C.; Rocha-Santos, T. COVID-19 pandemic repercussions on the use and management of plastics. Environ. Sci. Technol. 2020, 54, 7760–7765. [Google Scholar] [CrossRef]
- Conzachi, K. What You Can Do to Reduce the Environmental Impacts of COVID-19. 2020. Available online: https://www.colorado.edu/ecenter/2020/11/13/what-you-can-do-reduce-environmental-impacts-COVID-1 (accessed on 12 December 2021).
- Tsukiji, M.; Gamaralalage, P.J.D.; Pratomo, I.S.Y.; Onogawa, K.; Alverson, K.; Honda, S.; Ternald, D.; Dilley, M.; Fujioka, J.; Condrorini, D. Waste Management during the COVID-19 Pandemic from Response to Recovery; United Nations Environment Programme, International Environmental Technology Centre (IETC) IGES Center Collaborating with UNDP on Environmental Technologies (CCET): Osaka, Japan, 2020. [Google Scholar]
- Leja, K.; Lewandowicz, G. Polymer biodegradation and biodegradable polymers-a review. Pol. J. Environ. Stud. 2010, 19, 255–266. [Google Scholar]
- Tebyetekerwa, M.; Xu, Z.; Yang, S.; Ramakrishna, S. Electrospun nanofibers-based face masks. Adv. Fiber Mater. 2020, 2, 161–166. [Google Scholar] [CrossRef]
- Nicosia, A.; Gieparda, W.; Foksowicz-Flaczyk, J.; Walentowska, J.; Wesołek, D.; Vazquez, B.; Prodi, F.; Belosi, F. Air filtration and antimicrobial capabilities of electrospun PLA/PHB containing ionic liquid. Sep. Purif. Technol. 2015, 154, 154–160. [Google Scholar] [CrossRef]
- Purwar, R.; Goutham, K.S.; Srivastava, C.M. Electrospun Sericin/PVA/Clay nanofibrous mats for antimicrobial air filtration mask. Fibers Polym. 2016, 17, 1206–1216. [Google Scholar] [CrossRef]
- Tiliket, G.; Le Sage, D.; Moules, V.; Rosa-Calatrava, M.; Lina, B.; Valleton, J.; Nguyen, Q.; Lebrun, L. A new material for airborne virus filtration. Chem. Eng. J. 2011, 173, 341–351. [Google Scholar] [CrossRef]
- De Sio, L.; Ding, B.; Focsan, M.; Kogermann, K.; Pascoal-Faria, P.; Petronela, F.; Mitchell, G.; Zussman, E.; Pierini, F. Personalized Reusable Face Masks with Smart Nano-Assisted Destruction of Pathogens for COVID-19: A Visionary Road. Chem. Eur. J. 2021, 27, 6112–6130. [Google Scholar] [CrossRef] [PubMed]




| Mask Type | Standards | Filtration Effectiveness | |
|---|---|---|---|
Single-UseFace Mask | China: YY/T0969 | ||
| 3.0 Microns: ≥95% 0.1 Microns: X | |||
SurgicalMask | China: YY 0469 | 3.0 Microns: 95% | |
| 0.1 Microns: 30% | |||
| USA: ASTM F2100 | Level 1 | Level 2 | |
| 3.0 Microns: ≥95% | 3.0 Microns: ≥98% | ||
| 0.1 Microns: ≥95% | 0.1 Microns: ≥98% | ||
| Europe: EN 14683 | Type I | Type II | |
| 3.0 Microns: ≥95% | 3.0 Microns: ≥98% | ||
| 0.1 Microns: X | 0.1 Microns: X | ||
RespiratorMask | USA: NIOSH (42 | N95/KN95 | N99/KN99 |
| CFR 84) China: GB2626 | |||
| 0.3 Microns: ≥95% | 0.3 Microns: ≥99% | ||
| FFP1 | FFP2 | ||
| Europe: EN 149:2001 | 0.3 Microns: ≥80% | 0.3 Microns: ≥94% | |
| ASTM F2100-19 | EN 14683:2019 Barrier levels | ||||||
|---|---|---|---|---|---|---|---|
| Level 1 | Level 2 | Level 3 | Type I | Type II | Type IIR | ||
| Barrier testing | BFE (%) ASTM F2101, EN 14683 | ≥95 | ≥98 | ≥95 | ≥98 | ||
| PFE (%) ASTM F2299 | ≥95 | ≥98 | Not required | ||||
| Splash resistance, Synthetic blood ASTM F1862, ISO22609 | Pass at 80 mmHg | Pass at 120 mmHg | Pass at 160 mmHg | Not required | Pass at ≥ 16.0 kPa (120 mmHg) | ||
| Physical testing | Differential pressure EN 14683 | 5 mmH2O/cm2 | 6 mmH2O/cm2 | 40 Pa/cm2 | 60 Pa/cm2 | ||
| Safety testing | Flammability 16 CFR Part 1610 | Class 1 (≥3.5 seconds) | See European Medical Directive (2007/47/EC, MDD 93/42/EEC) | ||||
| Microbial cleanliness ISO 11737-1 | Not required | ≤30 cfu/g | |||||
| Biocompatibility ISO 10993 | 510 k Guidance recommends testing to ISO 10993 | Complete an evaluation according to ISO 10993 | |||||
| Sampling ANSI/ASQC Z1.4 ISO 2859-1 | ▪ AQL 4% for BFE, PFE, delta P ▪ 32 masks for synthetic blood (Pass ≥29 passing, Fail ≤28 passing) ▪ 14 masks for flammability | ▪ Minimum of 5 masks up to an AQL of 4% for BFE, delta P and microbial cleanliness ▪ 32 masks for synthetic blood splash resistance (Pass ≥ 29 passing, Fail ≤ 28 passing) | |||||
| Polymers | Products | Properties | |
|---|---|---|---|
| Polyolefin | Polypropylene (PP) | Nonwoven melt blown and spunbond fibers | Low cost, lightest weight among all synthetic fabrics due to its low density and specific gravity, ability to filter dry particulates, high chemical (alkali and acid) resistance, ease of processing, recyclability, modifiable inherent hydrophobicity, good mechanical strength, abrasion resistance, and micropore distribution uniformity make PP a promising option for manufacturing face masks. PP has higher mechanical strength and is less expensive than PE. |
| Polyethylene (PE) | Meltblown nonwoven fibers | PE with different densities, including high-density PE, low-density PE, and linear low-density PE, can be made. Good chemical resistance, lightweight, and hydrophobic. PE is easier to extrude than PP due to the high shear sensitivity and higher melting temperature of PP. | |
| Polyesters | Polyethylene terephthalate (PET) | Spunbond nonwoven fibers | Higher tensile modulus, strength, and heat stability, but less cost-effective than PP and more difficult to recycle. |
| Polyamide | Nylon 6 and 6–6 | Spunbond nonwoven fabrics | Fiber lightness and high melting temperature (260 °C), but unsuitable for face masks due to water absorption. |
| Cellulose Acetate (CA) | Electrospun nanofibrous membranes | High filtration efficacy, low thickness, hydrophobic, low production cost, biodegradable, high water stability, but soluble in organic solvents. | |
| Poly- (vinyl alcohol) (PVA) | Nanofibrous membranes | Lightweight, biodegradable, cost-effective, washable, and reusable. | |
| Polylactic Acid (PLA) | Nanofibrous membranes | Biodegradable, cost-effective, favorable mechanical properties, and filtration efficiency of 99.99%. | |
| Polytetrafluoroethylene (PTFE) | Air filter membranes | Lightweight, hydrophobic, great chemical stability, high surface fracture toughness, and high heat resistance. Because of its strong C-C and C-F bonds, PTEF membrane is extensively utilized as an air filter membrane with high filtration and fine particle rejection rate of greater than 99.99%. | |
| Polyacrylonitrile (PAN) | Waterproof membranes | High cost, significant variations in fiber diameters and mat morphologies, chemical and thermal stabilizations. | |
| Material | Source | Structure | Basis Weight (gm−2) | Bulk Density (Basis Weight/Thickness) (gm−2µm−1) | Initial Filtration Efficiency (%) | Initial Pressure Drop (Pa) | Filter Quality Factor, Q (kPa−1) |
|---|---|---|---|---|---|---|---|
| Personal Protection Materials | |||||||
| PP 1 | Particulate FFR | Meltblown (nonwoven) | 25 | 0.17 | 95.94 ± 2 | 9.0 ± 2.0 | 162.7 ± 21.3 |
| PP 2 | Medical face mask | Meltblown (nonwoven) | 26 | 0.21 | 33.06 ± 0.95 | 34.3 ± 0.5 | 5 ± 0.1 |
| PP 3 | Medical face mask | Meltblown (nonwoven) | 20 | 0.20 | 18.81 ± 0.5 | 16.3 ± 0.5 | 5.5 ± 0.1 |
| Household Materials | |||||||
| PP 4 | Interfacing material, purchased as-is | Spunbond (Nonwoven) | 30 | 0.26 | 6.15 ± 2.18 | 1.6 ± 0.5 | 16.9 ± 3.4 |
| Cotton 1 | Clothing (T-shirt) | Woven | 116 | 0.57 | 5.04 ± 0.64 | 4.5 ± 2.1 | 5.4 ± 1.9 |
| Cotton 2 | Clothing (T-shirt) | Knit | 157 | 0.37 | 21.62 ± 1.84 | 14.5 ± 2.1 | 7.4 ± 1.7 |
| Cotton 3 | Clothing (Sweater) | Knit | 360 | 0.45 | 25.88 ± 1.41 | 17 ± 0.0 | 7.6 ± 0.4 |
| Polyester | Clothing (Toddler wrap) | Knit | 200 | 0.38 | 17.50 ± 5.10 | 12.3 ± 0.5 | 6.8 ± 2.4 |
| Silk | Napkin | Woven | 84 | 0.54 | 4.77 ± 1.47 | 7.3 ± 1.5 | 2.8 ± 0.4 |
| Nylon | Clothing (Exercise pants) | Woven | 164 | 0.70 | 23.33 ± 1.18 | 244 ± 5.5 | 0.4 ± 0.0 |
| Cellulose | Paper towel | Bonded | 42.9 | 0.33 | 10.41 ± 0.28 | 11 ± 0.0 | 4.3 ± 2.8 |
| Cellulose | Tissue paper | Bonded | 32.8 | 0.39 | 20.2 ± 0.32 | 19 ± 1 | 5.1 ± 3.2 |
| Cellulose | Copy paper | Bonded | 72.8 | 0.76 | 99.85 ± 0.02 | 1883.6 ± 39.3 | 1.5 ± 0.2 |
| Mask Type | Surgical | N-95 | Cloth/Fabric |
|---|---|---|---|
 |  |  | |
| Fibers | Polypropylene Rayon Polyethylene Polyacrylonitrile Polyester Polyolefin Thermoplastic polymer | Cellulosic natural fiber Polypropylene Polytetrafluoroethylene Polyvinylidene fluoride Cellulose acetate | Densely woven fabric and knitted jersey fabric of natural cotton Silk fibers Pillowcase Kitchen towels Tea cloths |
| Characteristics | SMS non-woven, loose fitting, health worker wears readily, 3-layer, total 60–70 GSM | Facile tight-fitting, smart valve, efficient filtration of airborne particles (more than 95%), very high GSM | Used by the general population, any layer and fabric of different GSM can be assembled quickly, 3–4 layers, moderate GSM (250–450) |
| Benefits | Good filtration ability (more than 80%), cheap, single time use | For health personnel, efficient protection (MERS, SARS, Avian Flu, Ebola Virus, and PM2.5), good protection against COVID-19 | Easily made, homemade cloth reuse, washable, good fit |
| Shortcomings | Air leakage, a lot of copy products in the market | Uncomfortable to use, high cost | Not very efficient against COVID-19, insufficient protection to aerosols |
| Suggestions |
| ||
| Bio-Based Media | Structure and Materials | Applications |
|---|---|---|
| Protein | Keratin/polyamide 6 nanofiber | Water and air filtration |
| Electrospun sericin nanofibrous mats | Air filtration mask | |
| Silk nanofibers | Air filtration mask | |
| Gluten nanofiber | Face mask | |
| Soy protein isolate/PVA hybrid nanofiber | Air filtration mask | |
| Cellulose | Nanomembrane lyocell fibers | Surgical face mask |
| Cellulose non-woven layers | Surgical face mask | |
| Cellulose acetate nanofibers | Air filtration | |
| 3-ply cotton-PLA-cotton layered | Face mask | |
| Fungal hyphae and cellulose fibers (wood and hemp) | Alternative to synthetic melt and spun-blown materials for PPE | |
| Banana stem fiber | Face mask | |
| Non-woven cellulosic fiber | Face mask | |
| Chitosan | Nanofibrous chitosan non-woven | Water and air filtration |
| Poly lactic acid | Poly lactic acid fibrous membranes | Air filtration |
| 3D printed and electrospun polylactic acid | Face mask filter | |
| Gelatin | Gelatin/β–cyclodextrin composite nanofiber | Respiratory filter |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahman, M.Z.; Hoque, M.E.; Alam, M.R.; Rouf, M.A.; Khan, S.I.; Xu, H.; Ramakrishna, S. Face Masks to Combat Coronavirus (COVID-19)—Processing, Roles, Requirements, Efficacy, Risk and Sustainability. Polymers 2022, 14, 1296. https://doi.org/10.3390/polym14071296
Rahman MZ, Hoque ME, Alam MR, Rouf MA, Khan SI, Xu H, Ramakrishna S. Face Masks to Combat Coronavirus (COVID-19)—Processing, Roles, Requirements, Efficacy, Risk and Sustainability. Polymers. 2022; 14(7):1296. https://doi.org/10.3390/polym14071296
Chicago/Turabian StyleRahman, Md Zillur, Md Enamul Hoque, Md Rubel Alam, Md Abdur Rouf, Saiful Islam Khan, Huaizhong Xu, and Seeram Ramakrishna. 2022. "Face Masks to Combat Coronavirus (COVID-19)—Processing, Roles, Requirements, Efficacy, Risk and Sustainability" Polymers 14, no. 7: 1296. https://doi.org/10.3390/polym14071296
APA StyleRahman, M. Z., Hoque, M. E., Alam, M. R., Rouf, M. A., Khan, S. I., Xu, H., & Ramakrishna, S. (2022). Face Masks to Combat Coronavirus (COVID-19)—Processing, Roles, Requirements, Efficacy, Risk and Sustainability. Polymers, 14(7), 1296. https://doi.org/10.3390/polym14071296








