Using Peek as a Framework Material for Maxillofacial Silicone Prosthesis: An In Vitro Study
Abstract
:1. Introduction
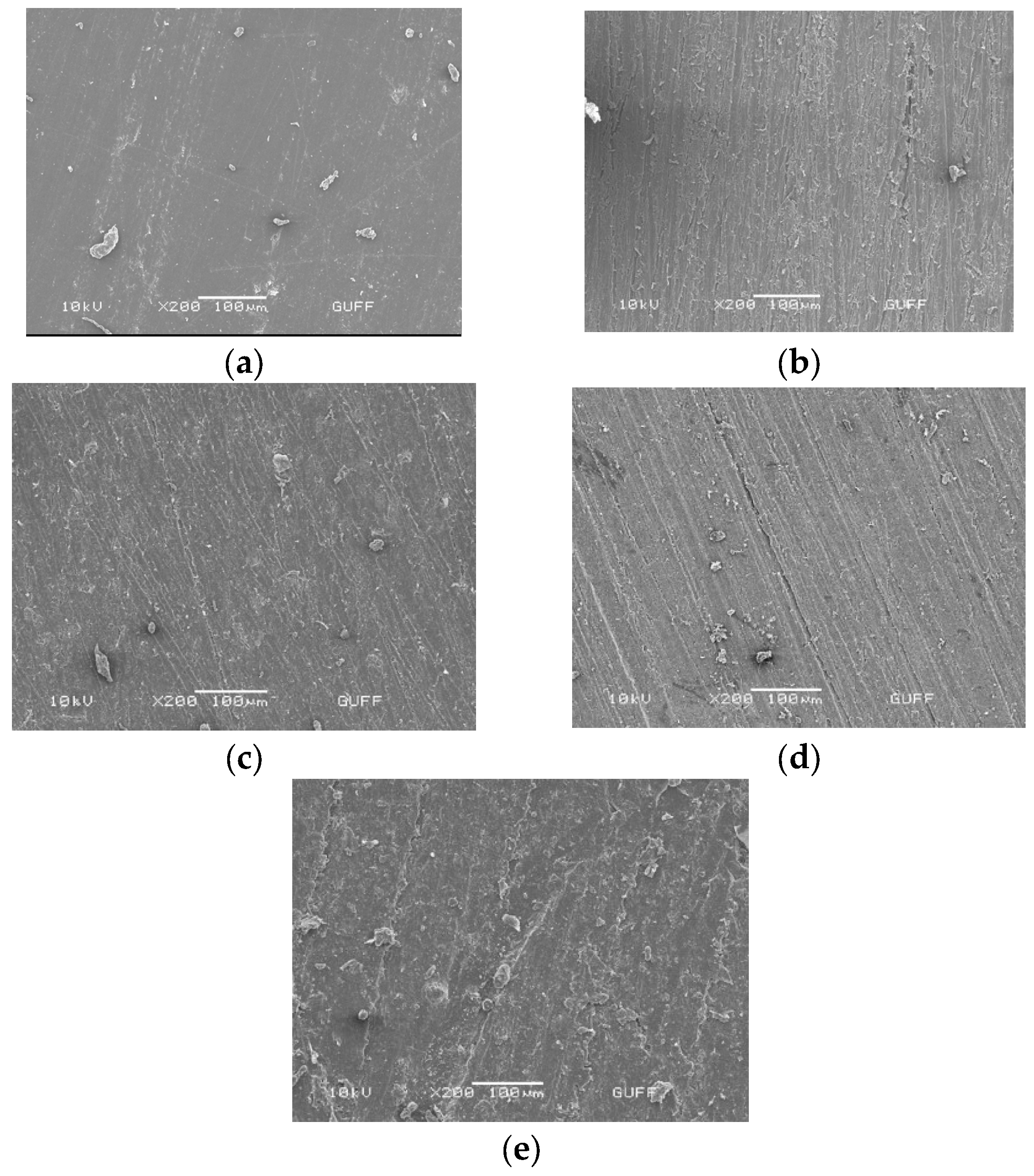
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- This study demonstrated that applying a platinum primer to PEEK structures resulted in a favorable bonding between platinum silicone elastomer and PEEK.
- Surface treatments on PEEK did not affect the bonding between PEEK and silicone. The obtained bond strength values revealed that PEEK may be a preferred supporting material over PMMA frameworks for fabricating implant-supported maxillofacial silicone elastomers. Notably, the control PMMA specimens exhibited significantly lower bond strength compared to the control PEEK specimens.
- The strong bonding observed between silicone and PEEK has practical implications in the development of maxillofacial silicone prostheses, benefiting both patients and clinicians.
- Future studies with larger specimen sizes should focus on investigating the bonding of PEEK frameworks with implant-supporting parts in such prostheses, further advancing our understanding in this area.
- Additionally, future studies could explore a wider range of surface treatment parameters and use larger specimen sizes to provide a more comprehensive understanding of the bonding characteristics between PEEK and silicone in maxillofacial silicone prostheses.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jindal, S.K.; Sherriff, M.; Waters, M.G.; Smay, J.E.; Coward, T.J. Development of a 3D printable maxillofacial silicone: Part II. Optimization of moderator and thixotropic agent. J. Prosthet. Dent. 2018, 119, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Lemon, J.C.; Chambers, M.S. Locking retentive attachment for an implant-retained auricular prosthesis. J. Prosthet. Dent. 2002, 87, 336–338. [Google Scholar] [CrossRef] [PubMed]
- Hatamleh, M.M.; Watts, D.C. Bonding of maxillofacial silicone elastomers to an acrylic substrate. Dent. Mater. 2010, 26, 387–395. [Google Scholar] [CrossRef] [PubMed]
- McMordie, R.; King, G.E. Evaluation of primers used for bonding silicone to denture base material. J. Prosthet. Dent. 1989, 61, 636–639. [Google Scholar] [CrossRef] [PubMed]
- Goiato, M.C.; Garcia-Júnior, I.R.; Magro-Filho, O.; Dos Santos, D.M.; Pellizzer, E.P. Implant-retained thumb prosthesis with anti-rotational attachment for a geriatric patient: Short report. Gerodontology 2010, 27, 243–247. [Google Scholar] [CrossRef]
- Hooper, S.M.; Westcott, T.; Evans, P.L.L.; Bocca, A.P.; Jagger, D.C. Implant-supported facial prostheses provided by a maxillofacial unit in a U.K. regional hospital: Longevity and patient opinions. J. Prosthodont. 2005, 14, 32–38. [Google Scholar] [CrossRef]
- Qudah, S.; Harrison, A.; Huggett, R. Soft lining materials in prosthetic dentistry: A review. Int. J. Prosthodont. 1990, 3, 477–483. [Google Scholar]
- Haddad, M.F.; Goiato, M.C.; dos Santos, D.M.; Crepaldi, N.d.M.; Pesqueira, A.A.; Bannwart, L.C. Bond strength between acrylic resin and maxillofacial silicone. J. Appl. Oral Sci. 2012, 20, 649–654. [Google Scholar] [CrossRef]
- Polyzois, G.L.; Frangou, M.I.; Andrcopouioi, A.C. The effect of bonding agents on the bond strengths of facial silicone elastomers to a visible light-activated resin. Int. J. Prosthodont. 1991, 4, 440–444. [Google Scholar]
- Sanohkan, S.; Kukiattrakoon, B.; Peampring, C. Tensile bond strength of facial silicone and acrylic resin using different primers. J. Orofac. Sci. 2017, 9, 48–51. [Google Scholar] [CrossRef]
- Minami, H.; Suzuki, S.; Ohashi, H.; Kurashige, H.; Tanaka, T. Effect of surface treatment on the bonding of an autopolymerizing soft denture liner to a denture base resin. Int. J. Prosthodont. 2004, 17, 297–301. [Google Scholar]
- Polyzois, G.L.; Frangou, M.J. Bonding of Silicone Prosthetic Elastomers to Three Different Denture Resins. Int. J. Prosthodont. 2002, 15, 535–538. [Google Scholar]
- Hatamleh, M.M.; Watts, D.C. Effects of bond primers on bending strength and bonding of glass fibers in fiber-embedded maxillofacial silicone prostheses. J. Prosthodont. 2011, 20, 113–119. [Google Scholar] [CrossRef]
- Mutluay, M.M.; Ruyter, I.E. Evaluation of bond strength of soft relining materials to denture base polymers. Dent. Mater. 2007, 23, 1373–1381. [Google Scholar] [CrossRef]
- Bonatto, L.d.R.; Goiato, M.C.; da Silva, E.V.F.; Oliveira, S.H.P.; Haddad, M.F.; Chaves Neto, A.H.; Brito, V.G.B.; dos Santos, D.M. Biocompatibility of primers and an adhesive used for implant-retained maxillofacial prostheses: An in vitro analysis. J. Prosthet. Dent. 2017, 117, 799–805. [Google Scholar] [CrossRef] [Green Version]
- Haleem, A.; Javaid, M. Polyether ether ketone (PEEK) and its manufacturing of customised 3D printed dentistry parts using additive manufacturing. Clin. Epidemiol. Glob. Health 2019, 7, 654–660. [Google Scholar] [CrossRef] [Green Version]
- Silthampitag, P.; Chaijareenont, P.; Tattakorn, K.; Banjongprasert, C.; Takahashi, H.; Arksornnukit, M. Effect of surface pretreatments on resin composite bonding to PEEK. Dent. Mater. J. 2016, 35, 668–674. [Google Scholar] [CrossRef] [Green Version]
- Najeeb, S.; Khurshid, Z.; Zohaib, S.; Zafar, M.S. Bioactivity and osseointegration of PEEK are inferior to those of titanium: A systematic review. J. Oral Implantol. 2016, 42, 512–516. [Google Scholar] [CrossRef]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J. Prosthodont. Res. 2016, 60, 12–19. [Google Scholar] [CrossRef]
- Skirbutis, G.; Dzingutė, A.; Masiliūnaitė, V.; Šulcaitė, G.; Žilinskas, J. PEEK polymer’s properties and its use in prosthodontics. A review. Stomatologija 2018, 20, 54–58. [Google Scholar]
- Fuhrmann, G.; Steiner, M.; Freitag-Wolf, S.; Kern, M. Resin bonding to three types of polyaryletherketones (PAEKs)—Durability and influence of surface conditioning. Dent. Mater. 2014, 30, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Taft, R.M.; Cameron, S.M.; Knudson, R.C.; Runyan, D.A. The effect of primers and surface characteristics on the adhesion-in-peel force of silicone elastomers bonded to resin materials. J. Prosthet. Dent. 1996, 76, 515–518. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Devine, J.N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 2007, 28, 4845–4869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feerick, E.M.; Kennedy, J.; Mullett, H.; FitzPatrick, D.; McGarry, P. Investigation of metallic and carbon fibre PEEK fracture fixation devices for three-part proximal humeral fractures. Med. Eng. Phys. 2013, 35, 712–722. [Google Scholar] [CrossRef] [PubMed]
- Yildirim Bicer, A.Z.; Dogan, A.; Keskin, S.; Dogan, O.M. Effect of argon plasma pretreatment on tensile bond strength of a silicone soft liner to denture base polymers. J. Adhes. 2013, 89, 594–610. [Google Scholar] [CrossRef]
- Schmidlin, P.R.; Stawarczyk, B.; Wieland, M.; Attin, T.; Hämmerle, C.H.F.; Fischer, J. Effect of different surface pre-treatments and luting materials on shear bond strength to PEEK. Dent. Mater. 2010, 26, 553–559. [Google Scholar] [CrossRef] [Green Version]
- Kern, M.; Lehmann, F. Influence of surface conditioning on bonding to polyetheretherketon (PEEK). Dent. Mater. 2012, 28, 1280–1283. [Google Scholar] [CrossRef]
- Caglar, I.; Ates, S.M.; Yesil Duymus, Z. An In Vitro Evaluation of the Effect of Various Adhesives and Surface Treatments on Bond Strength of Resin Cement to Polyetheretherketone. J. Prosthodont. 2019, 28, e342–e349. [Google Scholar] [CrossRef] [Green Version]
- Stawarczyk, B.; Bähr, N.; Beuer, F.; Wimmer, T.; Eichberger, M.; Gernet, W.; Jahn, D.; Schmidlin, P.R. Influence of plasma pretreatment on shear bond strength of self-adhesive resin cements to polyetheretherketone. Clin. Oral Investig. 2014, 18, 163–170. [Google Scholar] [CrossRef] [Green Version]
- Tsuka, H.; Morita, K.; Kato, K.; Kimura, H.; Abekura, H.; Hirata, I.; Kato, K.; Tsuga, K. Effect of laser groove treatment on shear bond strength of resin-based luting agent to polyetheretherketone (PEEK). J. Prosthodont. Res. 2019, 63, 52–57. [Google Scholar] [CrossRef]
- Ebnesajjad, S. Surface preparation of thermoplastics, thermosets, and elastomers. In Handbook of Adhesives and Surface Preparation; William Andrew Publishing: Norwich, NY, USA, 2011; pp. 107–134. ISBN 9781437744613. [Google Scholar]
- Chaijareenont, P.; Prakhamsai, S.; Silthampitag, P.; Takahashi, H.; Arksornnukit, M. Effects of different sulfuric acid etching concentrations on PEEK surface bonding to resin composite. Dent. Mater. J. 2018, 37, 385–392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barani, H.; Calvimontes, A. Effects of oxygen plasma treatment on the physical and chemical properties of wool fiber surface. Plasma Chem. Plasma Process. 2014, 34, 1291–1302. [Google Scholar] [CrossRef]
- Yildirim, A.Z.; Unver, S.; Mese, A.; Bayram, C.; Denkbas, E.B.; Cevik, P. Effect of argon plasma and Er:YAG laser on tensile bond strength between denture liner and acrylic resin. J. Prosthet. Dent. 2020, 124, 799.e1–799.e5. [Google Scholar] [CrossRef] [PubMed]
- Shetty, U.S.; Guttal, S.S. Evaluation of bonding efficiency between facial silicone and acrylic resin using different bonding agents and surface alterations. J. Adv. Prosthodont. 2012, 4, 121–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Georgiev, J.; Vlahova, A.; Kissov, H.; Aleksandrov, S.; Kazakova, R. Possible Application of Biohpp in Prosthetic Dentistry: A Literature Review. J. IMAB—Annu. Proc. (Sci. Pap.) 2018, 24, 1896–1898. [Google Scholar] [CrossRef]
- Gama, L.T.; Duque, T.M.; Özcan, M.; Philippi, A.G.; Mezzomo, L.A.M.; Gonçalves, T.M.S.V. Adhesion to high-performance polymers applied in dentistry: A systematic review. Dent. Mater. 2020, 36, e93–e108. [Google Scholar] [CrossRef]
- Jin, H.Y.; Teng, M.H.; Wang, Z.J.; Li, X.; Liang, J.Y.; Wang, W.X.; Jiang, S.; Zhao, B.D. Comparative evaluation of BioHPP and titanium as a framework veneered with composite resin for implant-supported fixed dental prostheses. J. Prosthet. Dent. 2019, 122, 383–388. [Google Scholar] [CrossRef]
- Zhou, L.; Qian, Y.; Zhu, Y.; Liu, H.; Gan, K.; Guo, J. The effect of different surface treatments on the bond strength of PEEK composite materials (DEMA-D-13-00481). Dent. Mater. 2014, 30, e209–e215. [Google Scholar] [CrossRef]
- Uhrenbacher, J.; Schmidlin, P.R.; Keul, C.; Eichberger, M.; Roos, M.; Gernet, W.; Stawarczyk, B. The effect of surface modification on the retention strength of polyetheretherketone crowns adhesively bonded to dentin abutments. J. Prosthet. Dent. 2014, 112, 1489–1497. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Taufall, S.; Roos, M.; Schmidlin, P.R.; Lümkemann, N. Bonding of composite resins to PEEK: The influence of adhesive systems and air-abrasion parameters. Clin. Oral Investig. 2018, 22, 763–771. [Google Scholar] [CrossRef]
- Hoy, C.L.; Ferhanoǧlu, O.; Yildirim, M.; Kim, K.H.; Karajanagi, S.S.; Chan, K.M.C.; Kobler, J.B.; Zeitels, S.M.; Ben-Yakar, A. Clinical ultrafast laser surgery: Recent advances and future directions. IEEE J. Sel. Top. Quantum Electron. 2014, 20, 242–255. [Google Scholar] [CrossRef]
- Kerse, C.; Kalaycloĝ Lu, H.; Elahi, P.; Çetin, B.; Kesim, D.K.; Akçaalan, Ö.; Yavaş, S.; Aşlk, M.D.; Öktem, B.; Hoogland, H.; et al. Ablation-cooled material removal with ultrafast bursts of pulses. Nature 2016, 537, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Keul, C.; Beuer, F.; Roos, M.; Schmidlin, P.R. Tensile bond strength of veneering resins to PEEK: Impact of different adhesives. Dent. Mater. J. 2013, 32, 441–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stawarczyk, B.; Jordan, P.; Schmidlin, P.R.; Roos, M.; Eichberger, M.; Gernet, W.; Keul, C. PEEK surface treatment effects on tensile bond strength to veneering resins. J. Prosthet. Dent. 2014, 112, 1278–1288. [Google Scholar] [CrossRef] [Green Version]
- Korkmaz, F.M.; Bagis, B.; Özcan, M.; Durkan, R.; Turgut, S.; Ates, S.M. Peel strength of denture liner to PMMA and polyamide: Laser versus air-abrasion. J. Adv. Prosthodont. 2013, 5, 287–295. [Google Scholar] [CrossRef] [Green Version]
- Ates, S.M.; Korkmaz, F.M.; Caglar, I.S.; Duymus, Z.Y.; Turgut, S.; Bagis, E.A. The effect of ultrafast fiber laser application on the bond strength of resin cement to titanium. Lasers Med. Sci. 2017, 32, 1121–1129. [Google Scholar] [CrossRef]
- Korkmaz, F.M.; Aycan, S. Effect of fiber laser irradiation on the shear bond strength between acrylic resin and titanium. Scanning 2019, 2019, 5452919. [Google Scholar] [CrossRef]
- Mutel, B.; Grimblot, J.; Dessaux, O.; Goudmand, P. XPS investigations of nitrogen-plasma-treated polypropylene in a reactor coupled to the spectrometer. Surf. Interface Anal. 2000, 30, 401–406. [Google Scholar] [CrossRef]
- Lee, J.-H.; Jo, J.-K.; Kim, D.-A.; Patel, K.D.; Kim, H.-W.; Lee, H.-H. Nano-graphene oxide incorporated into PMMA resin to prevent microbial adhesion. Dent. Mater. 2018, 34, e63–e72. [Google Scholar] [CrossRef]
- Vesel, A.; Mozetic, M.; Drenik, A.; Milosevic, S.; Krstulovic, N.; Balat-Pichelin, M.; Poberaj, I.; Babic, D. Cleaning of Porous Aluminium Titanate by Oxygen Plasma. Plasma Chem. Plasma Process. 2006, 26, 577–584. [Google Scholar] [CrossRef]
- Tsuka, H.; Morita, K.; Kato, K.; Kawano, H.; Abekura, H.; Tsuga, K. Evaluation of shear bond strength between PEEK and resin-based luting material. J. Oral Biosci. 2017, 59, 231–236. [Google Scholar] [CrossRef]
- Chen, J.H.; Ruckenstein, E. Solvent-stimulated surface rearrangement of polyurethanes. J. Colloid Interface Sci. 1990, 135, 496–507. [Google Scholar] [CrossRef]
- Picard, L.; Phalip, P.; Fleury, E.; Ganachaud, F. Chemical adhesion of silicone elastomers on primed metal surfaces: A comprehensive survey of open and patent literatures. Prog. Org. Coatings 2015, 80, 120–141. [Google Scholar] [CrossRef]
- Plueddemann, E.P. Silane Coupling Agents; Plenum Press: New York, NY, USA, 1982. [Google Scholar]
- Chang, P.P.; Hansen, N.A.; Phoenix, R.D.; Schneid, T.R. The effects of primers and surface bonding characteristics on the adhesion of polyurethane to two commonly used silicone elastomers. J. Prosthodont. 2009, 18, 23–31. [Google Scholar] [CrossRef]
- Cevik, P.; Schimmel, M.; Yilmaz, B. New generation CAD-CAM materials for implant-supported definitive frameworks fabricated by using subtractive technologies. Biomed Res. Int. 2022, 2022, 3074182. [Google Scholar] [CrossRef]
- Gutiérrez, T.J. 3D Printing of Biopolymers: Trends and Opportunities for Medical Applications. In Handbook of Biopolymers; Ahmed, S., Kanchi, S., Kumar, G., Eds.; Stanford Publishing: Singapore, 2020; pp. 45–74. ISBN 978-981-4800-17-4. [Google Scholar]
- Rekow, E.D. Digital dentistry: The new state of the art—Is it disruptive or destructive? Dent. Mater. 2020, 36, 9–24. [Google Scholar] [CrossRef]
- Costa-Palau, S.; Torrents-Nicolas, J.; Brufau-De Barberà, M.; Cabratosa-Termes, J. Use of polyetheretherketone in the fabrication of a maxillary obturator prosthesis: A clinical report. J. Prosthet. Dent. 2014, 112, 680–682. [Google Scholar] [CrossRef]
- Tasopoulos, T.; Chatziemmanouil, D.; Kouveliotis, G.; Karaiskou, G.; Wang, J.; Zoidis, P. PEEK Maxillary Obturator Prosthesis Fabrication Using Intraoral Scanning, 3D Printing, and CAD/CAM. Int. J. Prosthodont. 2020, 33, 333–340. [Google Scholar] [CrossRef]
- Heimer, S.; Schmidlin, P.R.; Roos, M.; Stawarczyk, B. Surface properties of polyetheretherketone after different laboratory and chairside polishing protocols. J. Prosthet. Dent. 2017, 117, 419–425. [Google Scholar] [CrossRef] [Green Version]


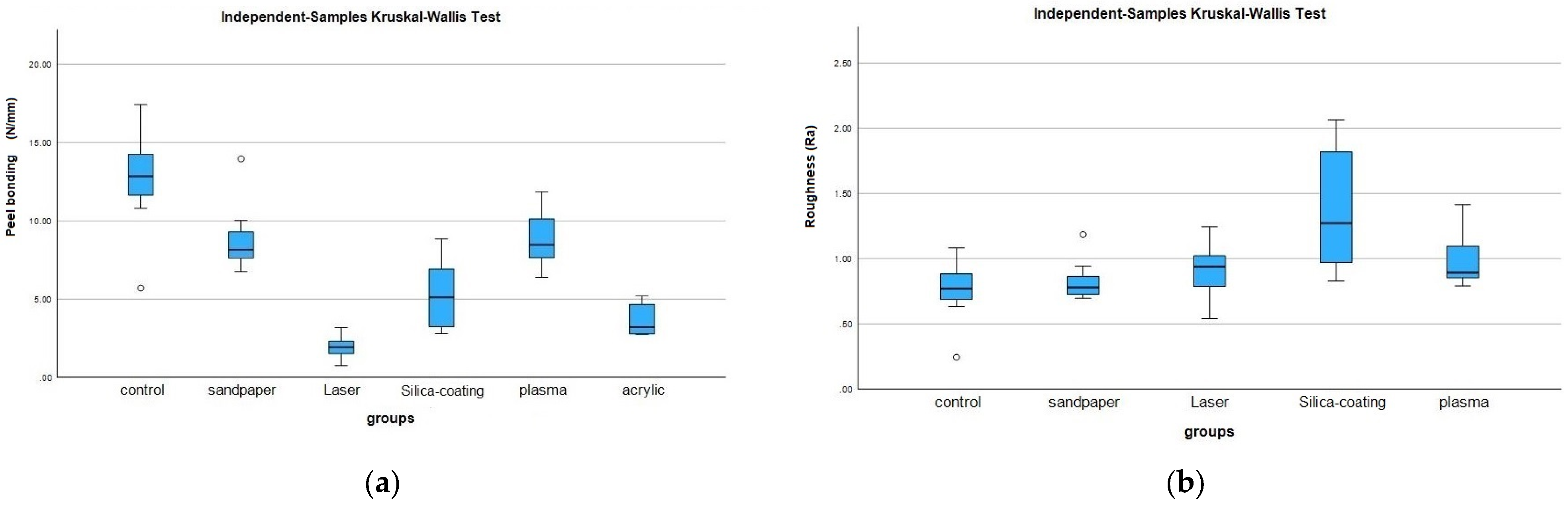
| Groups | Median | IQR |
|---|---|---|
| Control PEEK | 0.77 a | 0.63–0.88 |
| Sandpaper | 0.78 ab | 7.10–10.03 |
| Laser | 0.94 ab | 0.64–1.04 |
| Silica coating | 1.27 b | 0.87–2.01 |
| Plasma | 0.89 ab | 0.81–1.17 |
| p | <0.001 |
| Groups | Median | IQR |
|---|---|---|
| Control PEEK | 12.85 a | 10.80–14.84 |
| Sandpaper | 8.15 a | 7.10–10.03 |
| Laser | 1.93 b | 1.12–2.67 |
| Silica coating | 5.11 b | 3.08–7.93 |
| Plasma | 8.47 a | 7.53–10.34 |
| PMMA | 3.21 b | 2.76–4.79 |
| p | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cevik, P.; Yildirim, A.Z.; Demir Sevinc, E.H.; Gonder, A.; Kiat-Amnuay, S. Using Peek as a Framework Material for Maxillofacial Silicone Prosthesis: An In Vitro Study. Polymers 2023, 15, 2694. https://doi.org/10.3390/polym15122694
Cevik P, Yildirim AZ, Demir Sevinc EH, Gonder A, Kiat-Amnuay S. Using Peek as a Framework Material for Maxillofacial Silicone Prosthesis: An In Vitro Study. Polymers. 2023; 15(12):2694. https://doi.org/10.3390/polym15122694
Chicago/Turabian StyleCevik, Pinar, Arzu Zeynep Yildirim, Emine Hulya Demir Sevinc, Aykut Gonder, and Sudarat Kiat-Amnuay. 2023. "Using Peek as a Framework Material for Maxillofacial Silicone Prosthesis: An In Vitro Study" Polymers 15, no. 12: 2694. https://doi.org/10.3390/polym15122694
APA StyleCevik, P., Yildirim, A. Z., Demir Sevinc, E. H., Gonder, A., & Kiat-Amnuay, S. (2023). Using Peek as a Framework Material for Maxillofacial Silicone Prosthesis: An In Vitro Study. Polymers, 15(12), 2694. https://doi.org/10.3390/polym15122694








