The Environmental Impacts of Disposable Nonwoven Fabrics during the COVID-19 Pandemic: Case Study on the Francesc de Borja Hospital
Abstract
:1. Introduction
2. Materials and Methods
2.1. Nonwoven Use in the Francesc de Borja Hospital
- Non-sterile gown: this gown is made with a single layer of spunbond nonwoven polypropylene. It is used in non-surgical applications.
- Sleeveless gown: this gown shares all the characteristics of the non-sterile gown, with the only difference being that it is sleeveless.
- Sterile surgical gown: This gown is made with Spunbond, Meltblown, Meltblown, Meltblown, and Spunbond (SMMMS). This means that the fabric is composed of five layers, one spunbond nonwoven polypropylene on each side and three layers of meltblown nonwoven polypropylene in the middle. The highest level of the commonly seen gowns in the market is typically made from this material, which provides the highest level of protection against fluids. These are ANSI/AAMI Level 2 surgical gowns.
- High-risk sterile surgical gown: Similar to the sterile surgical gown, this gown is made using SMMMS. In this case, the difference is that the layers’ density is higher and thus reaches ANSI/AAMI Level 4.
- Reinforced sterile surgical gown: This gown is made using polyester + PE, which means that it is made with a spunbond nonwoven polyester layer, a reinforcing, and a waterproofing layer of polyethylene. These are ANSI/AAMI Level 3 gowns.
- Type I. Conventional residues: While generated at the hospital, type I residues are not specific to the medical activity. This category includes cardboard, office supplies, food waste, or furniture. Those residues, which do not require any particular management practice, are classified in black bin bags.
- Type II. Non-specific sanitary residues: This type includes waste produced due to medical activity that has not been in contact with any infectious disease. Items such as casts, bandages, waste derived from small surgical interventions, or any other material not included in type III. Waste included in this group is classified in green bin bags.
- Type III. Special sanitary waste includes bio-contaminated materials, generally considered hazardous waste. This category includes materials in contact with infectious diseases, anatomic residues (not including corpses or corpse remains), blood and blood products in liquid form, needles, and other sharp materials and vaccines. This type of waste must be deposited inside red bags placed in rigid bins adequately identified with the official logo of bio-contaminated residues and the text “hazardous waste” written next to it.
- Type IV. Waste typified by specific regulations: This type includes cytostatic substances, traces of toxic or hazardous chemical substances, expired medical drugs, toxic metals, and radioactive residues. These residues must be placed in a single-use container with the external identification “Chemically contaminated material. Cytostatics”. Medical garments such as gowns have generally been considered type II residues. However, after the pandemic, every material was considered in contact with coronavirus and automatically classified as a type III residue.
2.2. Life Cycle Assessment Methodology
3. Results
3.1. Preliminary Analysis of the Potential Benefits Associated with the Implementation of a Circularity Model
4. Discussion
- Medical waste regulations: Regulations in some countries make it difficult to repurpose medical waste, as all the COVID-19-related waste in Valencian hospitals is currently classified as a type III residue. Type III residues must be burned through very strict procedures. This impedes the waste from being used in a circular economy model, as the disinfection of waste can be challenging [21].
- Hospital logistics: The hospital’s medical and logistics personnel must be committed to the circular economy model. Separating the different kinds of gowns is instrumental to developing a circular economy model in a medical context.
- Coordination between companies: To create a circular economy model, it would be necessary to coordinate a consortium of at least three companies. First, a company that collects the used gowns and transforms them into new raw materials, in the case of polypropylene, into PP granulate. Secondly, a company in charge of transforming the new raw material into nonwoven again. Finally, a company in charge of the cutting and sewing processes manufactures the new gown. Coordinating with several companies can be challenging.
- Technical difficulties: Gowns made from more than one kind of plastic cannot be directly introduced into the recycling machinery. Their materials must be separated for them to be recyclable. For example, in the case of the reinforced sterile surgical gown, the recycling process would need to start by separating the polyester, the fleece, and the PET. This is likely not realistic and would be labor-intensive. Even elastic rubber bands and hook-and-loop parts would need to be separated from the main nonwoven fabric. Not separating the materials would make it impossible for the spunbond extruder to function and could potentially damage the machine.
5. Conclusions
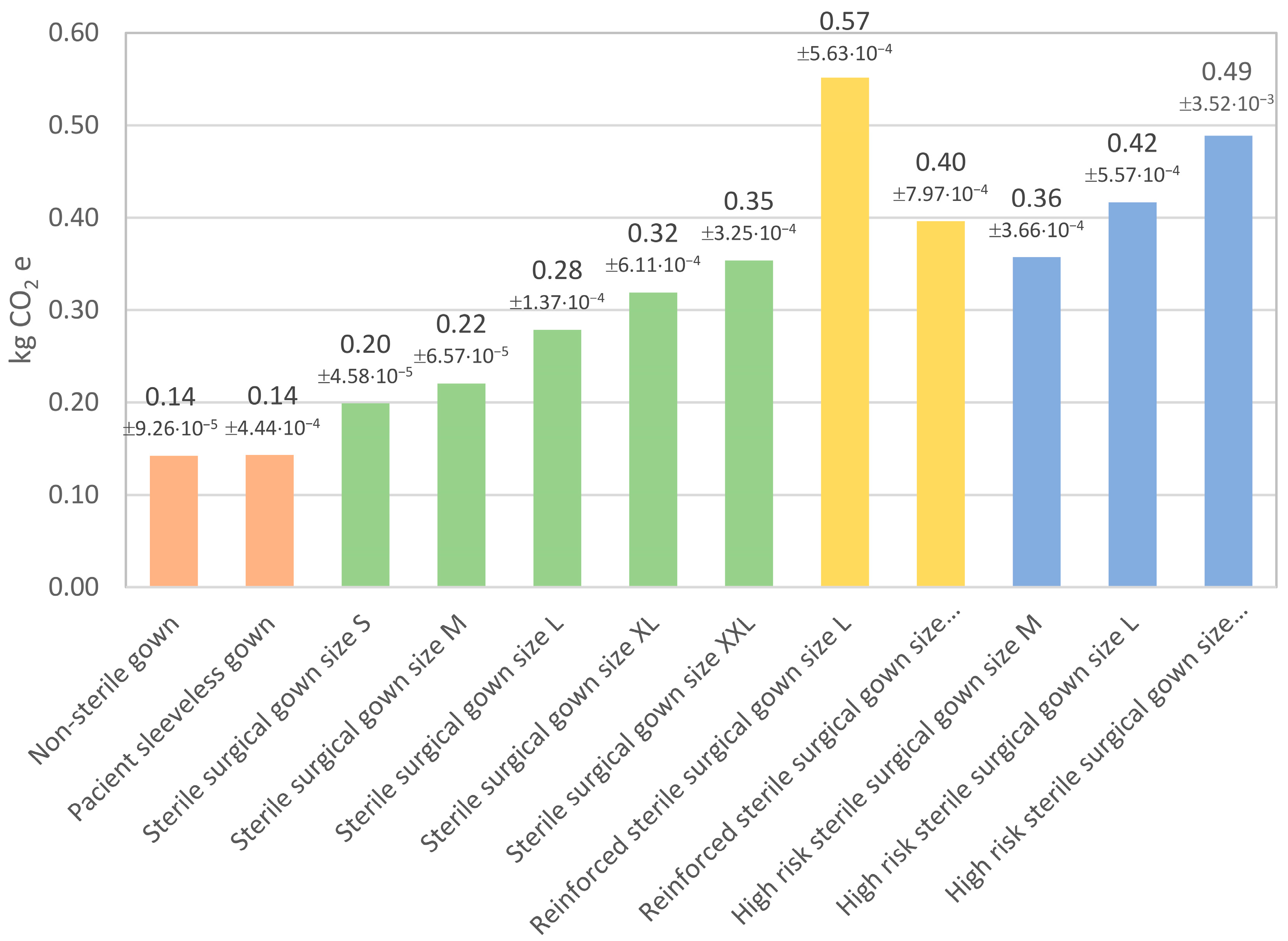
- As was expected, the more sophisticated gowns were those with a higher environmental impact overall, especially the high risk sterile surgical gown;
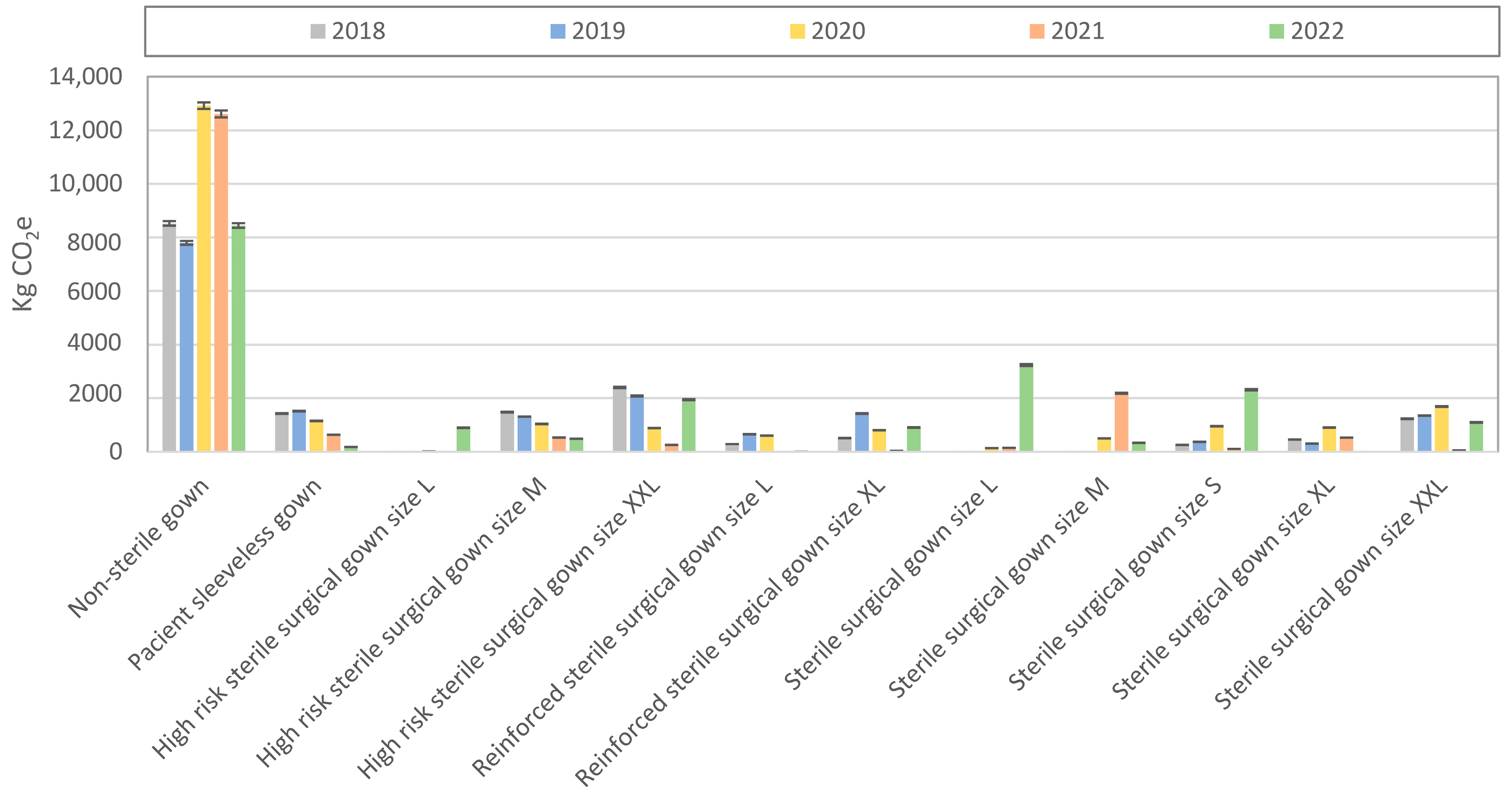
- Despite the lower environmental impacts per unit in every environmental footprint category, the non-sterile gowns were the ones that contributed more to the impacts generated by the Francesc de Borja Hospital due to their high annual consumption;
- Due to the high annual consumption, the non-sterile gown had more than a 600% higher annual carbon footprint than any other gown in the hospital;
- Gowns that incorporated nonwoven polyester tended to have higher environmental impacts than those made from nonwoven polypropylene;
- The consumption of disposable nonwoven fabrics in the hospital decreased slightly in 2022. However, it has not returned to the levels of the years prior to the pandemic;
- Considering that the non-sterile gown was mostly made of PP, designing a circular economy model for it would be easier than doing so for other gowns. Moreover, it would be more effective in reducing the carbon footprint of the hospital due to the higher consumption of these gowns;
- A circular economy model based on the non-sterile gown could reduce carbon emissions by 75% compared to the conventional manufacturing process of the gown.
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Uddin, F.; Chaudhary, N.A. Survey results of medical textiles in hospitals. Basic Clin. Pharmacol. Toxicol. 2019, 124, 3–4. [Google Scholar] [CrossRef]
- Rume, T.; Islam, S.M.D.U. Environmental effects of COVID-19 pandemic and potential strategies of sustainability. Heliyon 2020, 6, e04965. [Google Scholar] [CrossRef]
- Puig-Junoy, J.; Pérez-Sust, P. Integración vertical y contratación externa en los servicios generales de los hospitales españoles. Gac. Sanit. 2002, 16, 145–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gosavi, N.; Wadsworth, L.C.; Duckett, K.E. Nonwoven Laminates Containing Cotton for Medical Applications. J. Ind. Text. 2016, 24, 60–76. [Google Scholar] [CrossRef]
- Russell, S.J. Handbook of Nonwovens; Woodhead Publishing: Sawston, UK, 2006. [Google Scholar]
- Midha, V.K.; Dakuri, A.; Midha, V. Studies on the properties of nonwoven surgical gowns. J. Ind. Text. 2012, 43, 174–190. [Google Scholar] [CrossRef]
- Association for the Advancement of Medical Instrumentation. ANSI/AAMI PB70:2012—Liquid Barrier Performance and Classification of Protective Apparel and Drapes in Health Care Facilities; Association for the Advancement of Medical Instrumentation: Washington, DC, USA, 2012. [Google Scholar]
- McQuerry, M.; Easter, E.; Cao, A. Disposable versus reusable medical gowns: A performance comparison. Am. J. Infect. Control. 2021, 49, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Hicks, A.; Temizel-Sekeryan, S.; Kontar, W.; Ghamkhar, R.; Rodríguez Morris, M. Personal respiratory protection and resiliency in a pandemic, the evolving disposable versus reusable debate and its effect on waste generation. Resour. Conserv. Recycl. 2021, 168, 105262. [Google Scholar] [CrossRef] [PubMed]
- Klemeš, J.J.; Van Fan, Y.; Tan, R.R.; Jiang, P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sustain. Energy Rev. 2020, 127, 109883. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Klemeš, J.J.; Saxon, M.; You, F. How sustainable are the biodegradable medical gowns via environmental and social life cycle assessment? J. Clean. Prod. 2022, 380, 135153. [Google Scholar] [CrossRef]
- Corbin, L.; Hoff, H.; Smith, A.; Owens, C.; Weisinger, K.; Philipsborn, R. A 24-hour waste audit of the neuro ICU during the COVID-19 pandemic and opportunities for diversion. J. Clim. Change Health 2022, 8, 100154. [Google Scholar] [CrossRef] [PubMed]
- Kheirabadi, S.; Sheikhi, A. Recent advances and challenges in recycling and reusing biomedical materials. Curr. Opin. Green Sustain. Chem. 2022, 38, 100695. [Google Scholar] [CrossRef] [PubMed]
- Generalitat Valenciana. Hospital Francesc de Borja—Departamento de Gandia. Available online: https://gandia.san.gva.es/hospital (accessed on 13 September 2022).
- Generalitat Valenciana Decreto 240/1994, de 22 de Noviembre, del Gobierno Valenciano, por el que se Aprueba el Reglamento Regulador de la Gestión de los Residuos Sanitarios. (DOGV núm. 2401 de 05.12.1994). 2021. Available online: https://dogv.gva.es/datos/1994/12/05/pdf/1994_833224.pdf (accessed on 2 November 1994).
- ISO 14040; Environmental Management. Life Cycle Assessment. Principles and Framework. ISO: Geneva, Switzerland, 2006.
- ISO 14025; Environmental Labels and Declarations. Type III Environmental Declarations. Principles and Procedures. ISO: Geneva, Switzerland, 2006.
- Zampori, L.; Pant, R. Suggestions for updating the Product Environmental Footprint (PEF) Method; Publications Office of the European Union: Luxembourg, 2019.
- European Commission. Recommendation 2013/179/EU on the Use of Common Methods to Measure and Communicate the Life Cycle Environmental Performance of Products and Organisations; Publications Office of the European Union: Luxembourg, 2013.
- Sepetis, A.; Zaza, P.N.; Rizos, F.; Bagos, P.G. Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector. Int. J. Environ. Res. Public Health 2022, 19, 9821. [Google Scholar] [CrossRef] [PubMed]
- Harussani, M.M.; Rashid, U.; Sapuan, S.M.; Abdan, K. Low-Temperature Thermal Degradation of Disinfected COVID-19 Non-Woven Polypropylene—Based Isolation Gown Wastes into Carbonaceous Char. Polymer 2021, 13, 3980. [Google Scholar] [CrossRef] [PubMed]
- Stahel, W.R. The circular economy. Nature 2016, 531, 435–438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toronto University Health Network. Development of a Novel Hood Shield to Enhance PPE Security and Minimize COVID-19 Transmission to Front-line Health Care Workers Performing High-risk Procedures; Toronto University Health Network: Toronto, ON, Canada, 2021. [Google Scholar]
- European Commission. First Circular Economy Action Plan. Available online: https://environment.ec.europa.eu/topics/circular-economy/first-circular-economy-action-plan_en (accessed on 11 December 2022).
- Lee, B.K.; Ellenbecker, M.J.; Moure-Eraso, R. Analyses of the recycling potential of medical plastic wastes. Waste Manag. 2002, 22, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Kane, G.M.; Bakker, C.A.; Balkenende, A.R. Towards design strategies for circular medical products. Resour. Conserv. Recycl. 2018, 135, 38–47. [Google Scholar] [CrossRef]
- Voudrias, E.A. Healthcare waste management from the point of view of circular economy. Waste Manag. 2018, 75, 1–2. [Google Scholar] [CrossRef]
- World Health Organization. Circular Economy and Health: Opportunities and Risks; World Health Organization: Geneva, Switzerland, 2018; ISBN 9789289053341. [Google Scholar]
- Scavarda, A.; Daú, G.L.; Scavarda, L.F.; Korzenowski, A.L. A proposed healthcare supply chain management framework in the emerging economies with the sustainable lenses: The theory, the practice, and the policy. Resour. Conserv. Recycl. 2019, 141, 418–430. [Google Scholar] [CrossRef]
- Kenny, C.; Priyadarshini, A. Review of Current Healthcare Waste Management Methods and Their Effect on Global Health. Healthcare 2021, 9, 284. [Google Scholar] [CrossRef] [PubMed]
- van Straten, B.; Ligtelijn, S.; Droog, L.; Putman, E.; Dankelman, J.; Weiland, N.H.S.; Horeman, T. A life cycle assessment of reprocessing face masks during the Covid-19 pandemic. Sci. Rep. 2021, 11, 17680. [Google Scholar] [CrossRef] [PubMed]



| Level 1 | Test | Liquid Challenge | Result | Expected Barrier Effectiveness |
|---|---|---|---|---|
| 1 | AATCC 42 Impact Penetration 2 | Water | 4.5 g | Minimal water resistance (some resistance to water spray) |
| 2 | AATCC 42 Impact Penetration | Water | 1.0 g | Low water resistance (resistant to water spray and some resistance to water penetration under constant contact with increasing pressure) |
| AATCC 127 Hydrostatic Pressure 3 | Water | 20 cm | ||
| 3 | AATCC 42 Impact Penetration | Water | 1.0 g | Moderate water resistance (resistant to water spray and some resistance to water penetration under constant contact with increasing pressure) |
| AATCC 127 Hydrostatic Pressure | Water | 50 cm | ||
| 4 | ASTM F1670 Synthetic Blood Penetration Test (for surgical drapes) | Surrogate Blood | no penetration at 2 psi (13.8 kPa) | Blood and viral penetration resistance (2 psi) |
| ASTM F1671 Viral Penetration Test (for surgical and isolation gowns) | BacteriophagePhi-X174 | no penetration at 2 psi (13.8 kPa) |
| Item | 2018 | 2019 | 2020 | 2021 | 2022 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Units | kg | Units | kg | Units | kg | Units | kg | Units | kg | |
| Non-sterile gown | 59,860 | 3155.82 ± 14.37 | 54,793 | 2888.69 ± 13.15 | 90,777 | 4785.76 ± 21.79 | 98,741 | 5205.63 ± 23.7 | 59,335 | 3128.14 ± 14.24 |
| Sleeveless gown | 10,048 | 532.79 ± 11.50 | 10,621 | 563.18 ± 12.16 | 8015 | 424.99 ± 9.18 | 13,081 | 693.62 ± 14.98 | 1296 | 68.72 ± 1.48 |
| High risk sterile surgical gown L | 1098 | 157.79 ± 0.49 | 739 | 106.2 ± 0.33 | 2167 | 311.41 ± 0.96 | 1690 | 205.75 ± 0.75 | 2142 | 307.82 ± 0.95 |
| High risk sterile surgical gown M | 723 | 88.02 ± 0.24 | 1045 | 127.22 ± 0.35 | 2651 | 322.75 ± 0.89 | 1683 | 241.86 ± 0.56 | 1369 | 166.67 ± 0.46 |
| High risk sterile surgical gown XXL | 2506 | 427.67 ± 6.11 | 2760 | 471.02 ± 6.73 | 3460 | 590.48 ± 8.44 | 2825 | 482.11 ± 6.89 | 3984 | 679.91 ± 9.72 |
| Reinforced sterile surgical gown L | 0 | 0 | 0 | 0 | 256 | 34.17 ± 0.08 | 3654 | 487.74 ± 0.21 | 19 | 2.54 ± 0.01 |
| Reinforced sterile surgical gown XL | 0 | 0 | 0 | 0 | 1264 | 179.44 ± 0.9 | 722 | 102.5 ± 2.59 | 2286 | 324.52 ± 1.62 |
| Sterile surgical gown L | 8598 | 863.36 ± 1.50 | 7458 | 748.89 ± 1.31 | 3160 | 317.31 ± 0.55 | 0 | 0 | 11,608 | 1165.62 ± 2.03 |
| Sterile surgical gown M | 6736 | 531.03 ± 0.71 | 5940 | 468.28 ± 0.62 | 4680 | 368.95 ± 0.49 | 2727 | 214.98 ± 0.29 | 1528 | 120.46 ± 0.16 |
| Sterile surgical gown S | 0 | 0 | 0 | 0 | 74 | 5.18 ± 0.01 | 5472 | 549.47 ± 0.44 | 11,608 | 812.79 ± 0.93 |
| Sterile surgical gown XL | 916 | 105.67 ± 0.63 | 2056 | 237.19 ± 1.41 | 1897 | 218.85 ± 1.3 | 143 | 16.5 ± 0.1 | 0 | 0 |
| Sterile surgical gown XXL | 1445 | 185.08 ± 0.48 | 4064 | 520.52 ± 1.34 | 2268 | 290.49 ± 0.75 | 1463 | 187.38 ± 0.48 | 3085 | 395.13 ± 1.02 |
| High risk boot cover | 225 | 7.23 ± 0.01 | 775 | 24.9 ± 0.02 | 2300 | 73.91 ± 0.06 | 2000 | 64.27 ± 1.56 | 1000 | 32.14 ± 0.78 |
| Boot cover | 183,430 | 648.43 ± 26.60 | 155,236 | 548.76 ± 22.51 | 163,109 | 576.59 ± 23.65 | 39,689 | 140 ± 5.75 | 47,627 | 168 ± 6.91 |
| Protective hat | 0 | 0 | 0 | 0 | 90,655 | 349.48 ± 0.27 | 153,310 | 591.01 ± 0.19 | 75,572 | 291 ± 0.23 |
| Total | 277,127 | 6702.9 ± 62.64 | 246,751 | 6704.86 ± 59.93 | 402,627 | 9578.47 ± 69.31 | 454,429 | 9632.86 ± 57.9 | 222,459 | 7663.45 ± 39.76 |
| Impact Category | Unit | Non-Sterile Gown | Patient Sleeveless Gown | Sterile Surgical Gown S | Sterile Surgical Gown M | Sterile Surgical Gown L | Sterile Surgical Gown XL |
|---|---|---|---|---|---|---|---|
| Climate change | kg CO2 eq | 0.1426 | 0.1434 | 0.2003 | 0.2221 | 0.2804 | 0.3208 |
| ±9.26 × 10−5 | ±4.44 × 10−4 | ±4.58 × 10−5 | ±6.57 × 10−5 | ±1.37 × 10−4 | ±6.11 × 10−4 | ||
| Ozone depletion | kg CFC11 eq | 5.96 × 10−9 | 5.99 ×10−9 | 1.16 × 10−8 | 1.25 × 10−8 | 1.49 × 10−8 | 1.66 × 10−8 |
| ±1.62 × 10−19 | ±7.75 × 10−19 | ±1.54 × 10−19 | ±2.08 × 10−19 | ±3.87 × 10−19 | ±1.64 × 10−18 | ||
| Ionizing radiation | kBq U-235 eq | 2.42 × 10−3 | 2.44 × 10−3 | 4.14 × 10−3 | 4.51 × 10−3 | 5.50 × 10−3 | 6.18 × 10−3 |
| ±2.67× 10−8 | ±1.29 × 10−7 | ±1.96 × 10−8 | ±2.71 × 10−8 | ±5.27 × 10−8 | ±2.27 × 10−7 | ||
| Photochemical ozone formation | kg NMVOC eq | 5.73× 10−4 | 5.77 × 10−4 | 8.47 × 10−4 | 9.36 × 10−4 | 1.17 × 10−3 | 1.33 × 10−3 |
| ±1.49 × 10−9 | ±7.19 × 10−9 | ±8.20 × 10−10 | ±1.17 × 10−9 | ±2.39 × 10−9 | ±1.05 × 10−8 | ||
| Particulate matter | disease inc. | 5.89 × 10−9 | 5.93 × 10−9 | 8.62 × 10−9 | 9.52 × 10−9 | 1.19 × 10−8 | 1.36 × 10−8 |
| ±1.58 × 10−19 | ±7.59 × 10−19 | ±8.49 × 10−20 | ±1.21 × 10−19 | ±2.47 × 10−19 | ±1.10 × 10−18 | ||
| Human toxicity, non-cancer | CTUh | 1.33 × 10−9 | 1.34 × 10−9 | 1.87 × 10−9 | 2.07 × 10−9 | 2.62 × 10−9 | 2.99 × 10−9 |
| ±8.05 × 10−21 | ±3.88 × 10−20 | ±4.00 × 10−21 | ±5.71 × 10−21 | ±1.20 × 10−20 | ±5.31 × 10−20 | ||
| Human toxicity, cancer | CTUh | 5.30 × 10−11 | 5.33 × 10−11 | 7.66 × 10−11 | 8.47 × 10−11 | 1.06 × 10−10 | 1.21 × 10−10 |
| ±1.28 × 10−23 | ±6.13 × 10−23 | ±6.70 × 10−24 | ±9.56 × 10−24 | ±1.96 × 10−23 | ±8.69 × 10−23 | ||
| Acidification | mol H+ eq | 6.82 × 10−4 | 6.86 × 10−4 | 1.02 × 10−3 | 1.12 × 10−3 | 1.40 × 10−3 | 1.59 × 10−3 |
| ±2.12 × 10−9 | ±1.02 × 10−8 | ±1.19 × 10−9 | ±1.67 × 10−9 | ±3.42 × 10−9 | ±1.50 × 10−8 | ||
| Eutrophication, freshwater | kg P eq | 2.69 × 10−6 | 2.71 × 10−6 | 3.84 × 10−6 | 4.24 × 10−6 | 5.35 × 10−6 | 6.11 × 10−6 |
| ±3.29 × 10−14 | ±1.59 × 10−13 | ±1.68 × 10−14 | ±2.39 × 10−14 | ±4.99 × 10−14 | ±2.22 × 10−13 | ||
| Eutrophication, marine | kg N eq | 1.45 × 10−4 | 1.46 × 10−4 | 2.16 × 10−4 | 2.39 × 10−4 | 2.98 × 10−4 | 3.39 × 10−4 |
| ±9.57 × 10−11 | ±4.60 × 10−10 | ±5.33 × 10−11 | ±7.61 × 10−11 | ±1.55 × 10−10 | ±6.82 × 10−10 | ||
| Eutrophication, terrestrial | mol N eq | 1.65 × 10−3 | 1.66 × 10−3 | 2.45 × 10−3 | 2.71 × 10−3 | 3.38 × 10−3 | 3.85 × 10−3 |
| ±1.24 × 10−8 | ±5.95 × 10−8 | ±6.86 × 10−9 | ±9.78 × 10−9 | ±1.99 × 10−8 | ±8.80 × 10−8 | ||
| Ecotoxicity, freshwater | CTUe | 1.51 | 1.52 | 2.18 | 2.42 | 3.03 | 3.46 |
| ±1.04 × 10−2 | ±4.99 × 10−2 | ±5.43 × 10−3 | ±7.80 × 10−3 | ±1.60 × 10−2 | ±7.11 × 10−2 | ||
| Land use | Pt | 0.51 | 0.52 | 0.76 | 0.84 | 1.05 | 1.19 |
| ±1.18 × 10−3 | ±5.84 × 10−3 | ±6.60 × 10−4 | ±9.40 × 10−4 | ±1.92 × 10−3 | ±8.41 × 10−3 | ||
| Water use | m3 depriv. | 0.0543 | 0.0546 | 0.0781 | 0.0863 | 0.1085 | 0.1239 |
| ±1.34 × 10−5 | ±6.44 × 10−5 | ±6.97 × 10−5 | ±9.92 × 10−6 | ±2.05 × 10−5 | ±9.12 × 10−5 | ||
| Resource use, fossils | MJ | 4.26 | 4.28 | 5.77 | 6.42 | 8.16 | 9.37 |
| ±8.26 × 10−2 | ±3.96 × 10−1 | ±3.80 × 10−2 | ±5.49 × 10−2 | ±1.16 × 10−1 | ±5.21 × 10−1 |
| Impact Category | Unit | Sterile Surgical Gown XXL | Reinforced Sterile Surgical Gown L | Reinforced Sterile Surgical Gown XL | High Risk Sterile Surgical Gown M | High Risk Sterile Surgical Gown L | High Risk Sterile Surgical Gown XXL |
|---|---|---|---|---|---|---|---|
| Climate change | kg CO2 eq | 0.3553 | 0.5686 | 0.3993 | 0.3645 | 0.4243 | 0.4962 |
| ±3.25 × 10−4 | ±5.63 × 10−4 | ±7.97 × 10−4 | ±3.66 × 10−4 | ±5.57 × 10−4 | ±3.52 × 10−3 | ||
| Ozone depletion | kg CFC11 eq | 1.81 × 10−8 | 1.43 × 10−6 | 2.12× 10−8 | 6.65 × 10−7 | 6.73 × 10−7 | 6.65 × 10−7 |
| ±8.44 × 10−19 | ±3.56 × 10−15 | ±2.25 × 10−18 | ±1.22 × 10−15 | ±1.40 × 10−15 | ±6.32 × 10−15 | ||
| Ionizing radiation | kBq U-235 eq | 6.77 × 10−3 | 1.17 × 10−2 | 7.18 × 10−3 | 7.53 × 10−3 | 8.56 × 10−3 | 9.75 × 10−3 |
| ±1.18 × 10−7 | ±2.39 × 10−7 | ±2.58 × 10−7 | ±1.56 × 10−7 | ±2.27 × 10−7 | ±1.36 × 10−6 | ||
| Photochemical ozone formation | kg NMVOC eq | 1.47 × 10−3 | 2.35 × 10−3 | 1.63 × 10−3 | 1.41 × 10−3 | 1.65 × 10−3 | 1.93 × 10−3 |
| ±5.57 × 10−9 | ±9.62 × 10−9 | ±1.33 × 10−8 | ±5.47 × 10−9 | ±8.43 × 10−9 | ±5.33 × 10−8 | ||
| Particulate matter | disease inc. | 1.50 × 10−8 | 2.54 × 10−8 | 1.65× 10−8 | 1.45 × 10−8 | 1.69 × 10−8 | 1.99 × 10−8 |
| ±5.80 × 10−19 | ±1.12 × 10−18 | ±1.36 × 10−18 | ±5.79 × 10−19 | ±8.84 × 10−19 | ±5.66 × 10−18 | ||
| Human toxicity, non-cancer | CTUh | 3.32 × 10−9 | 5.54 × 10−9 | 3.68× 10−9 | 3.25 × 10−9 | 3.80 × 10−9 | 4.48 × 10−9 |
| ±2.84 × 10−20 | ±5.35 × 10−20 | ±6.77 × 10−20 | ±2.91 × 10−20 | ±4.47 × 10−20 | ±2.87× 10−19 | ||
| Human toxicity, cancer | CTUh | 1.34 × 10−10 | 5.03 × 10−10 | 1.50 × 10−10 | 2.21 × 10−10 | 2.44 × 10−10 | 2.70 × 10−10 |
| ±4.63 × 10−23 | ±4.41 × 10−22 | ±1.13 × 10−22 | ±1.34 × 10−22 | ±1.84 × 10−22 | ±1.04 × 10−21 | ||
| Acidification | mol H+ eq | 1.76 × 10−3 | 2.55 × 10−3 | 1.93 × 10−3 | 1.69 × 10−3 | 1.97 × 10−3 | 2.31 × 10−3 |
| ±7.98 × 10−9 | ±1.13 × 10−8 | ±1.86 × 10−8 | ±7.86 × 10−9 | ±1.20 × 10−8 | ±7.63 × 10−8 | ||
| Eutrophication, freshwater | kg P eq | 6.76 × 10−6 | 1.88 × 10−5 | 7.26 × 10−6 | 8.54 × 10−6 | 9.68 × 10−6 | 1.10 × 10−5 |
| ±1.18 × 10−13 | ±6.16 × 10−13 | ±2.64 × 10−13 | ±2.01 × 10−13 | ±2.90 × 10−13 | ±1.73 × 10−12 | ||
| Eutrophication, marine | kg N eq | 3.75 × 10−4 | 5.49 × 10−4 | 4.11 × 10−4 | 3.64 × 10−4 | 4.26 × 10−4 | 4.97 × 10−4 |
| ±3.62 × 10−10 | ±5.25 × 10−10 | ±8.45 × 10−10 | ±3.65 × 10−10 | ±5.62 × 10−10 | ±3.53× 10−9 | ||
| Eutrophication, terrestrial | mol N eq | 4.26 × 10−3 | 6.62 × 10−3 | 4.65 × 10−3 | 4.07 × 10−3 | 4.76 × 10−3 | 5.58 × 10−3 |
| ±4.68 × 10−8 | ±7.64 × 10−8 | ±1.08 × 10−7 | ±4.56 × 10−8 | ±7.02 × 10−8 | ±4.45 × 10−7 | ||
| Ecotoxicity, freshwater | CTUe | 3.83 | 6.7 | 4.18 | 3.59 | 4.22 | 4.99 |
| ±3.78 × 10−2 | ±7.82 × 10−2 | ±8.74 × 10−2 | ±3.55 × 10−2 | ±5.51 × 10−2 | ±3.56 × 10−1 | ||
| Land use | Pt | 1.32 | 2.26 | 1.33 | 1.37 | 1.58 | 1.84 |
| ±4.49 × 10−3 | ±8.90 × 10−3 | ±8.85 × 10−3 | ±5.16 × 10−3 | ±7.73 × 10−3 | ±4.84 × 10−2 | ||
| Water use | m3 depriv. | 0.137 | 0.3085 | 0.1595 | 0.1768 | 0.1999 | 0.2268 |
| ±4.84 × 10−5 | ±1.66 × 10−4 | ±1.27 × 10−4 | ±8.60 × 10−5 | ±1.24 × 10−4 | ±7.35 × 10−4 | ||
| Resource use, fossils | MJ | 10.39 | 12.09 | 11.61 | 9.59 | 11.36 | 13.54 |
| ±2.78 × 10−1 | ±2.55 × 10−1 | ±6.74 × 10−1 | ±2.53 × 10−1 | ±4.00 × 10−1 | ±2.62 | ||
| Resource use, minerals, and metals | kg Sb eq | 7.32 × 10−6 | −4.50 × 10−6 | 8.33 × 10−6 | 6.73 × 10−7 | 1.85 × 10−6 | 3.47 × 10−6 |
| ±1.38 × 10−13 | ±3.53 × 10−14 | ±3.47 × 10−13 | ±1.25 × 10−15 | ±1.06 × 10−14 | ±1.72 × 10−13 |
| Item | Nonwoven PP | Nonwoven Polyester | PET | Fleece | Rubber Bands | Hook-and-Loop | Transportation |
|---|---|---|---|---|---|---|---|
| Non-sterile gown | 93.9 | - | - | - | - | - | 6.1 |
| Sterile surgical gown size L | 85.70 | - | - | - | 4.79 | 2.50 | 6.20 |
| Reinforced sterile surgical gown size L | - | 53.80 | 18.10 | 20.40 | - | - | 3.00 |
| High risk sterile surgical gown size L | 56.50 | - | 32.50 | - | 3.16 | - | 4.34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quintana-Gallardo, A.; del Rey, R.; González-Conca, S.; Guillén-Guillamón, I. The Environmental Impacts of Disposable Nonwoven Fabrics during the COVID-19 Pandemic: Case Study on the Francesc de Borja Hospital. Polymers 2023, 15, 1130. https://doi.org/10.3390/polym15051130
Quintana-Gallardo A, del Rey R, González-Conca S, Guillén-Guillamón I. The Environmental Impacts of Disposable Nonwoven Fabrics during the COVID-19 Pandemic: Case Study on the Francesc de Borja Hospital. Polymers. 2023; 15(5):1130. https://doi.org/10.3390/polym15051130
Chicago/Turabian StyleQuintana-Gallardo, Alberto, Romina del Rey, Salvador González-Conca, and Ignacio Guillén-Guillamón. 2023. "The Environmental Impacts of Disposable Nonwoven Fabrics during the COVID-19 Pandemic: Case Study on the Francesc de Borja Hospital" Polymers 15, no. 5: 1130. https://doi.org/10.3390/polym15051130





