Characterization of Radiation Shielding Capabilities of High Concentration PLA-W Composite for 3D Printing of Radiation Therapy Collimators
Abstract
1. Introduction
2. Materials and Methods
2.1. Material and Printing Properties
2.1.1. Material Composite
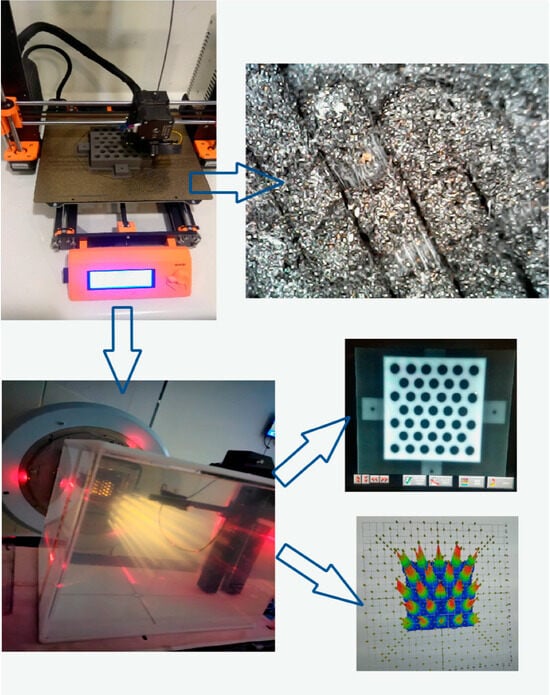
2.1.2. 3D Printer Device
2.1.3. Printing Settings Parameters
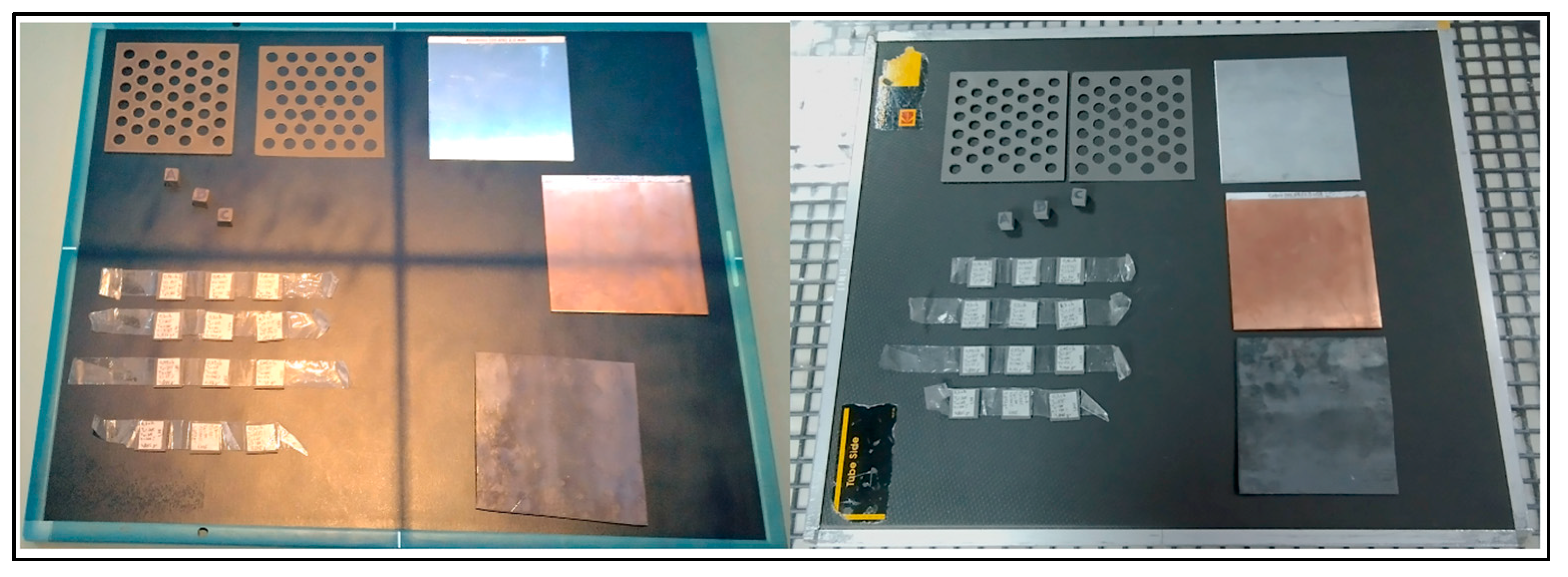
2.2. Physical and Mechanical Properties Analyzed
2.3. Radiation Properties
2.3.1. Radiation Shielding Homogeneity
2.3.2. Material Attenuation
2.4. Design and Characterization of the Radiotherapy Collimator Grid
2.4.1. Field Size and Beam Divergence
2.4.2. Radiation Shielding Capability
3. Results
3.1. Material and Printing Properties
3.1.1. Material Composite
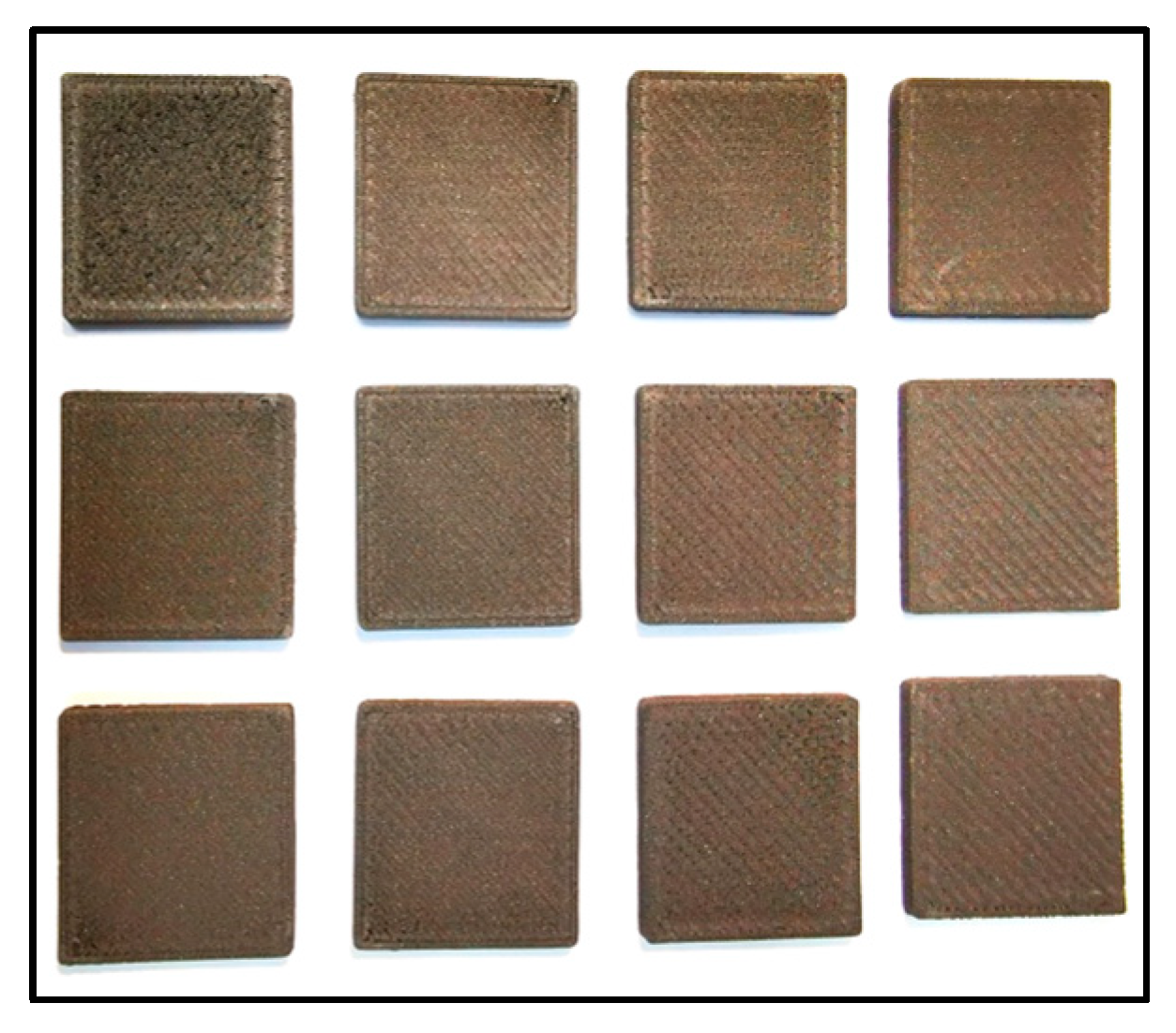
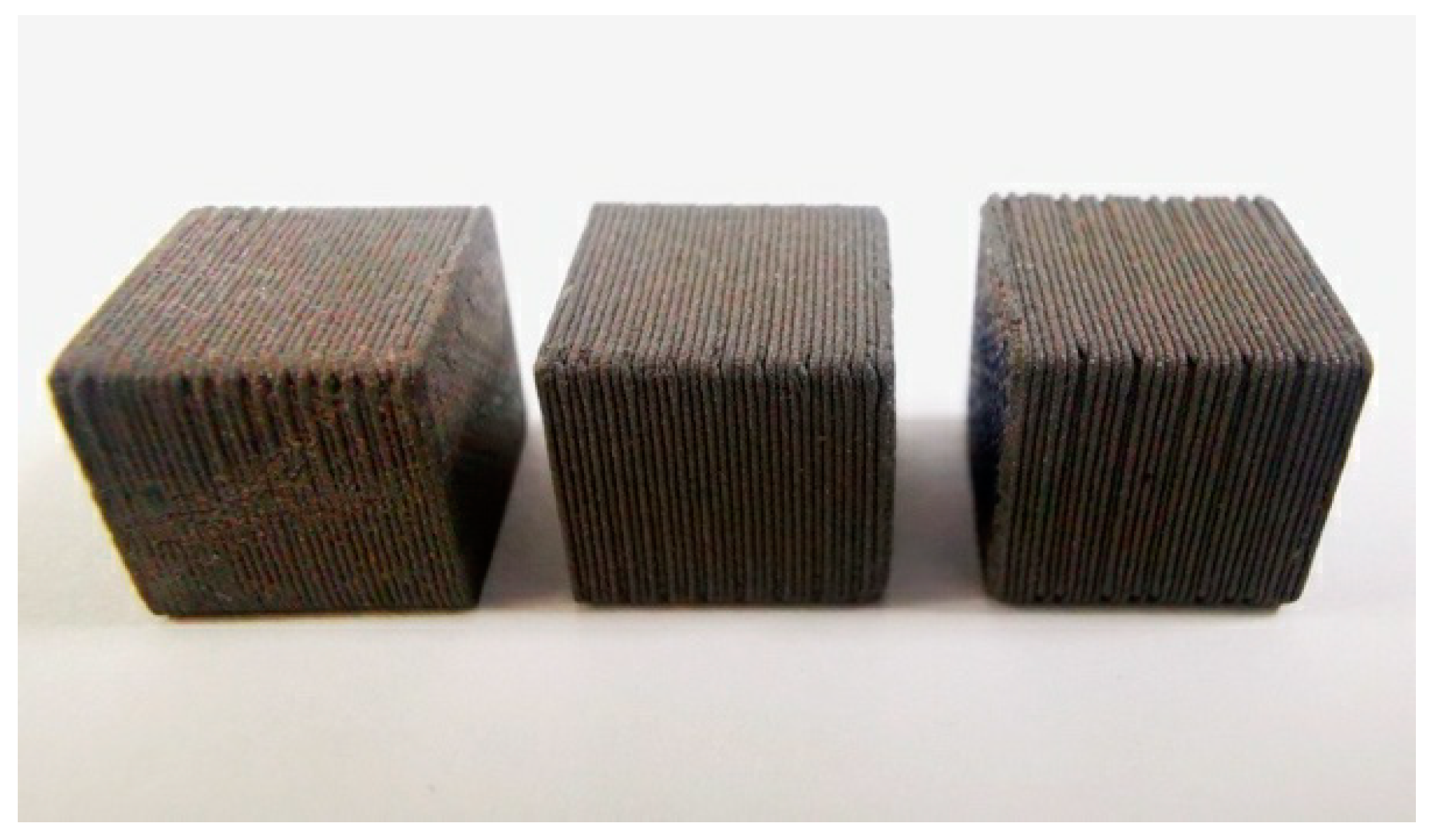
3.1.2. Physical Properties Analyzed as a Function of Printing Parameters
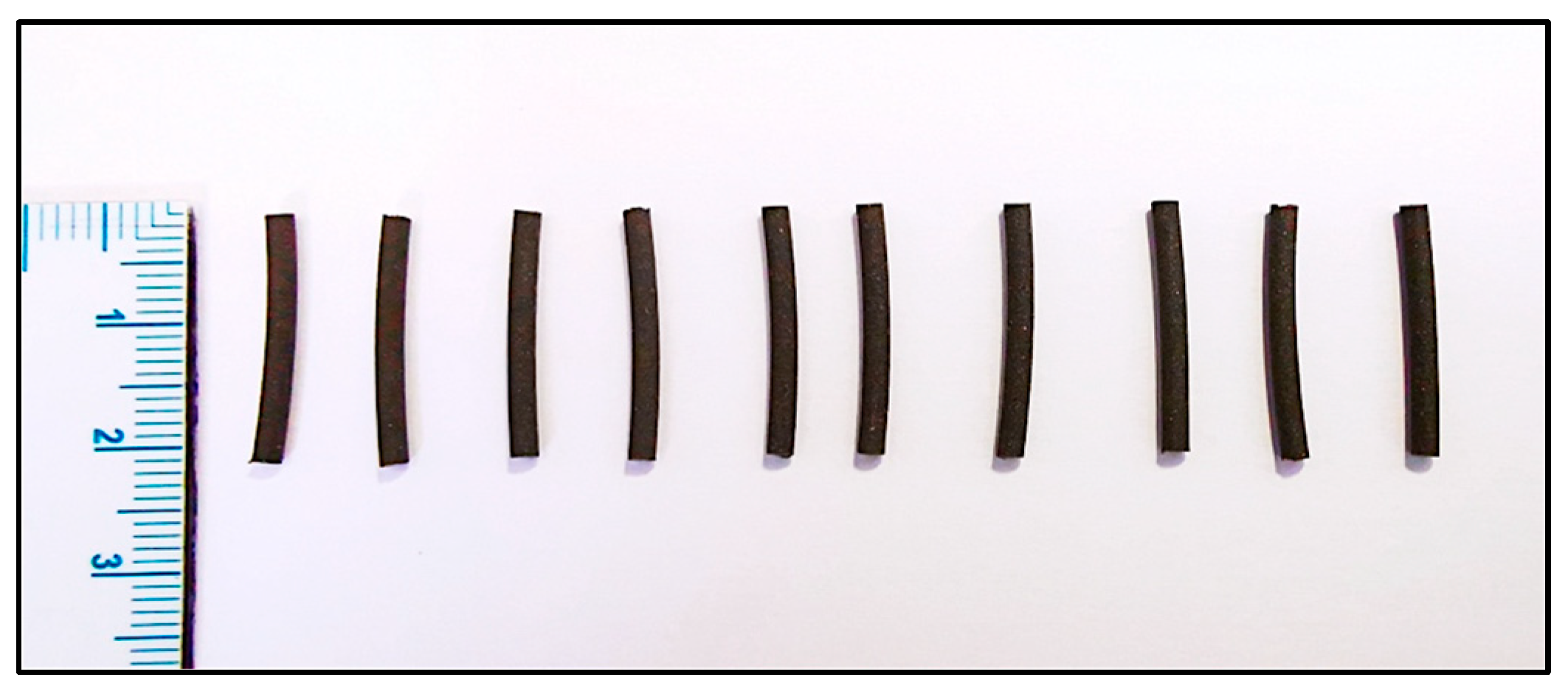
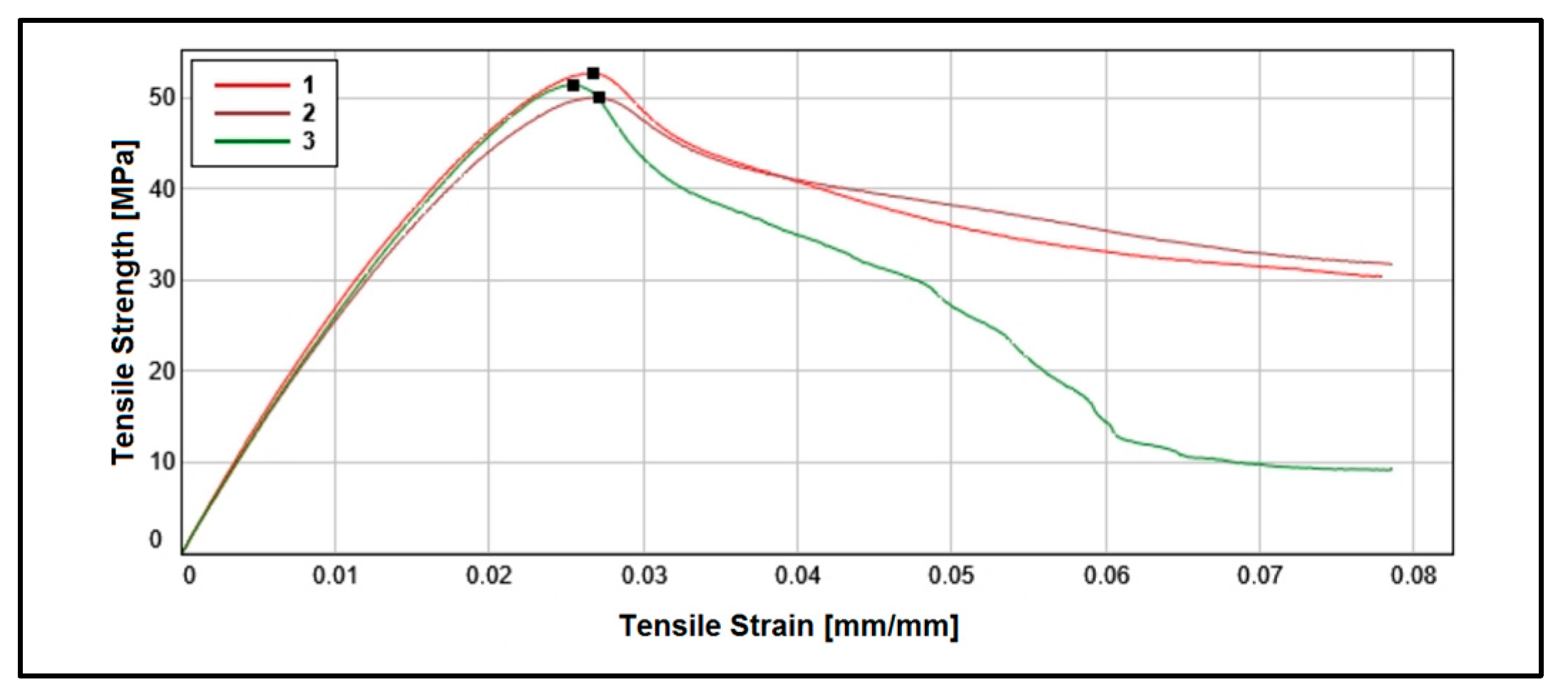
3.2. Mechanical Properties
3.3. Radiation Properties
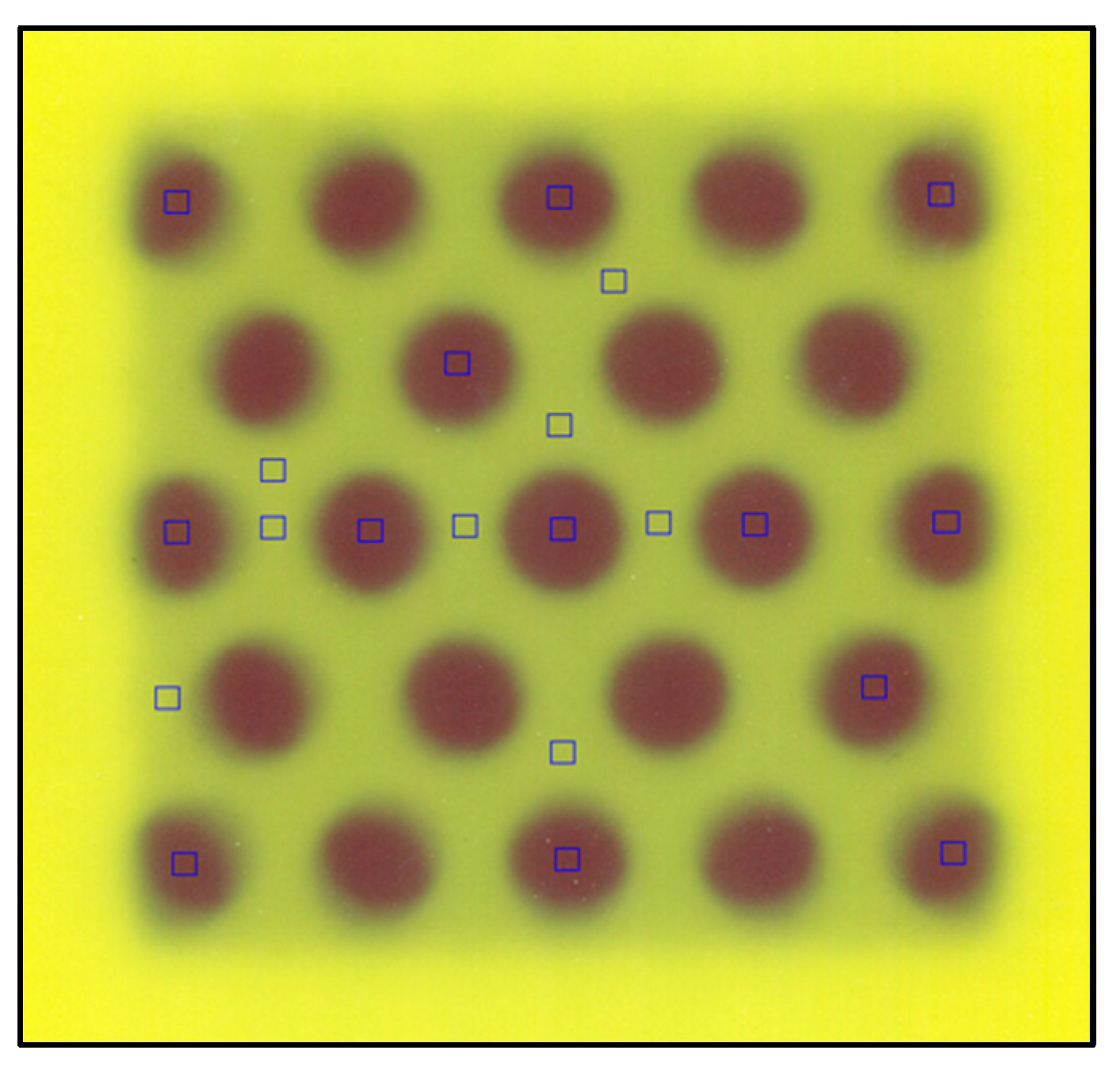
3.3.1. Radiation Shielding Homogeneity
3.3.2. Material Attenuation
3.4. Design and Characterization of the Radiotherapy Collimator Grid
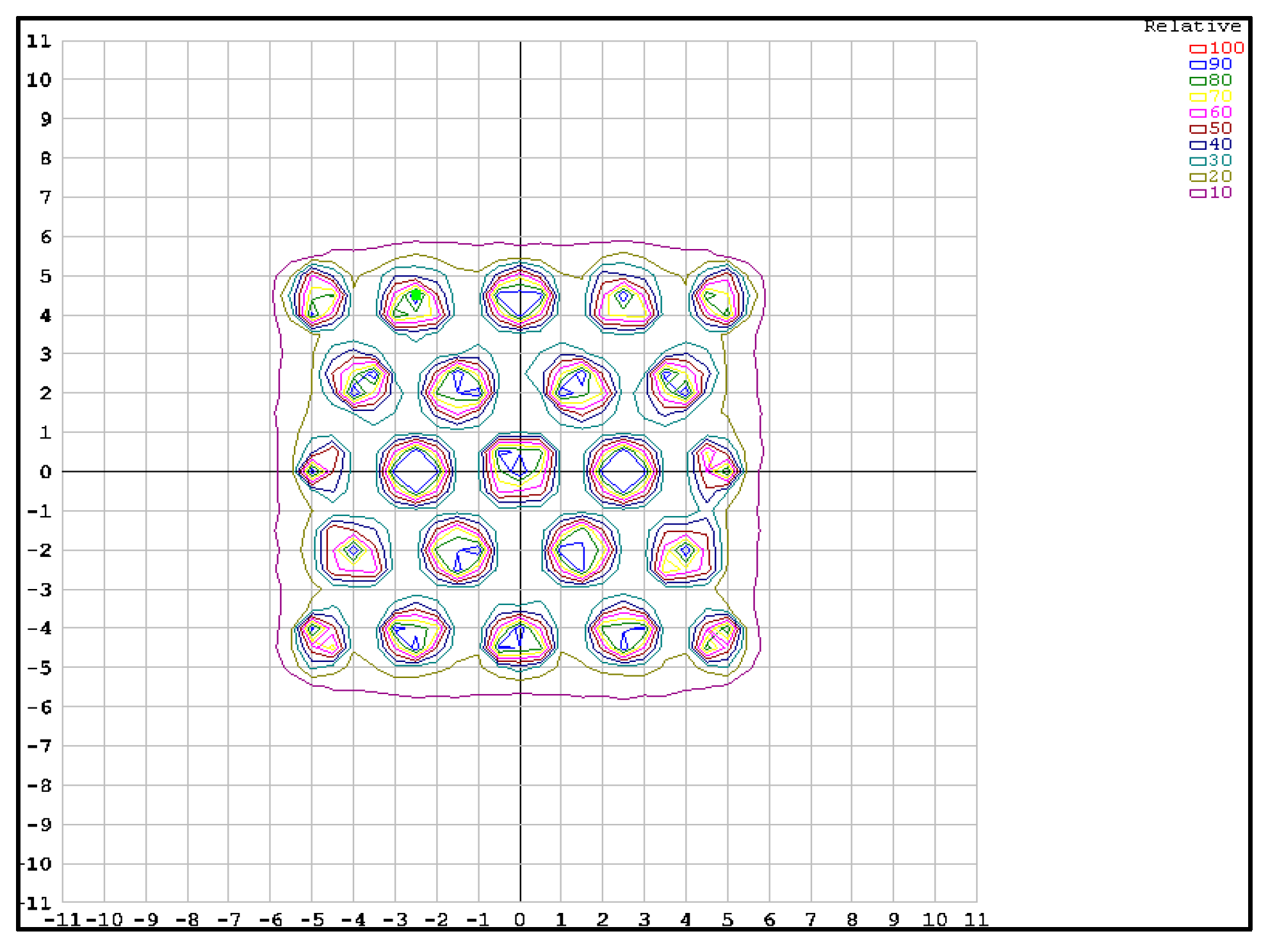
3.4.1. Field Size and Beam Divergence
3.4.2. Radiation Shielding Capacity
4. Discussion
5. Conclusions
- The achieved densities (7.15 ± 0.01) and the material’s high effective atomic number allow it to attain linear attenuation coefficients at MV photon energies, similar to commercially existing materials manufactured by traditional methods (0.3352 cm−1), with radiation shielding capability provided by HVL of 2.138 cm.
- The manufactured pieces exhibited excellent spatial congruence at sub-millimeter resolution and high homogeneity in material distribution and deposition, remaining stable over the course of 1 year.
- The decrease in mechanical properties due to the presence of a high concentration of W granules that break into PLA fiber mesh does not critically affect its stability for the intended application, far from values that could cause structural deformations, while maintaining radiation spatial modulation with great precision.
- The manufactured grid showed levels of dosimetric precision and spatial modulation of radiation through its radiation shielding/attenuation capacity in inter-collimator spaces, with values similar to commercially available grids (transmittance of 15% relative to the central axis) produced by traditional manufacturing methods.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Polonio-Alcalá, E.; Rabionet, M.; Guerra, A.J.; Yeste, M.; Ciurana, J.; Puig, T. Screening of Additive Manufactured Scaffolds Designs for Triple Negative Breast Cancer 3D Cell Culture and Stem-like Expansion. Int. J. Mol. Sci. 2018, 19, 3148. [Google Scholar] [CrossRef]
- Lu, Y.; Song, J.; Yao, X.; An, M.; Shi, Q.; Huang, X. 3D Printing Polymer-based Bolus Used for Radiotherapy. Int. J. Bioprint. 2021, 7, 414. [Google Scholar] [CrossRef]
- Singh, S.; Ramakrishna, S. Biomedical applications of additive manufacturing: Present and future. Curr. Opin. Biomed. Eng. 2017, 2, 105–115. [Google Scholar] [CrossRef]
- Ahangar, P.; Cooke, M.E.; Weber, M.H.; Rosenzweig, D.H. Current biomedical applications of 3D printing and additive manufacturing. Appl. Sci. 2019, 9, 1713. [Google Scholar] [CrossRef]
- Çevik, Ü.; Kam, M. A review study on mechanical properties of obtained products by FDM method and metal/polymer composite filament production. J. Nanomater. 2020, 2020, 6187149. [Google Scholar] [CrossRef]
- Ferry, M. Tungsten-Infused Filaments for Additive Manufacturing. Bachelor’s Thesis, College of William and Mary, Williamsburg, VA, USA, 2 May 2016. [Google Scholar]
- Vakharia, V.S.; Kuentz, L.; Salem, A.; Halbig, M.C.; Salem, J.A.; Singh, M. Additive manufacturing and characterization of metal particulate reinforced Polylactic Acid (PLA) polymer composites. Polymers 2021, 13, 3545. [Google Scholar] [CrossRef] [PubMed]
- Buj-Corral, I.; Sanz-Fraile, H.; Ulldemolins, A.; Tejo-Otero, A.; Domínguez-Fernández, A.; Almendros, I.; Otero, J. Characterization of 3D printed metal-PLA composite scaffolds for biomedical applications. Polymers 2022, 14, 2754. [Google Scholar] [CrossRef] [PubMed]
- Dey, A.; Roan Eagle, I.N.; Yodo, N. A review on filament materials for fused filament fabrication. J. Manuf. Mater. Process. 2021, 5, 69. [Google Scholar] [CrossRef]
- Steuben, J.; Van Bossuyt, D.L.; Turner, C. Design for Fused Filament Fabrication Additive Manufacturing. In Proceedings of the Volume 4: 20th Design for Manufacturing and the Life Cycle Conference; 9th International Conference on Micro- and Nanosystems, Boston, MA, USA, 2–5 August 2015; American Society of Mechanical Engineers: New York, NY, USA, 2015. [Google Scholar]
- Solomon, I.J.; Sevvel, P.; Gunasekaran, J. A Review on the Various Processing Parameters in FDM. Mater. Today Proc. 2021, 37, 509–514. [Google Scholar] [CrossRef]
- Daminabo, S.C.; Goel, S.; Grammatikos, S.A.; Nezhad, H.Y.; Thakur, V.K. Fused Deposition Modeling-Based Additive Manufacturing (3D Printing): Techniques for Polymer Material Systems. Mater. Today Chem. 2020, 16, 100248. [Google Scholar] [CrossRef]
- Mohd Pu’ad, N.A.S.; Abdul Haq, R.H.; Mohd Noh, H.; Abdullah, H.Z.; Idris, M.I.; Lee, T.C. Review on the Fabrication of Fused Deposition Modelling (FDM) Composite Filament for Biomedical Applications. Mater. Today Proc. 2020, 29, 228–232. [Google Scholar] [CrossRef]
- Yoo, T.S.; Hamilton, T.; Hurt, D.E.; Caban, J.; Liao, D.; Chen, D.T. Toward Quantitative X-Ray CT Phantoms of Metastatic Tumors Using Rapid Prototyping Technology. In Proceedings of the 2011 IEEE International Symposium on Biomedical Imaging: From Nano to Macro, Chicago, IL, USA, 30 March–2 April 2011; IEEE: Piscataway, NJ, USA, 2011; pp. 1770–1773. [Google Scholar]
- Al-Buriahi, M.S.; Eke, C.; Alomairy, S.; Yildirim, A.; Alsaeedy, H.I.; Sriwunkum, C. Radiation attenuation properties of some commercial polymers for advanced shielding applications at low energies. Polym. Adv. Technol. 2021, 32, 2386–2396. [Google Scholar] [CrossRef]
- Sayyed, M. Investigation of shielding parameters for smart polymers. Chin. J. Phys. 2016, 54, 408–415. [Google Scholar] [CrossRef]
- Akhdar, H.; Alshehri, M. Geant4 Simulation of Photon- and Neutron-Shielding Capabilities of Biopolymer Blends of Poly(Lactic Acid) and Poly(Hydroxybutyrate). Polymers 2023, 15, 4257. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, M.; Pekdemir, M.E.; Öner, E. Evaluation of Pb doped Poly(lactic acid) (PLA)/Poly(ethylene glycol) (PEG) blend composites regarding physicochemical and radiation shielding properties. Radiat. Phys. Chem. 2023, 202, 110509. [Google Scholar] [CrossRef]
- Akhdar, H.; Alotaibi, R. Geant4 Simulation of the Effect of Different Composites on Polyimide Photon and Neutron Shielding Properties. Polymers 2023, 15, 1973. [Google Scholar] [CrossRef]
- Abdali, K. Crystal Structural, Morphological and Gamma Ray Shielding (γ-S) Efficiency of PVA/PAAM/PAA Polymer Blend Loaded with Silver Nanoparticles via Casting Method. Res. Sq. 2021. [Google Scholar] [CrossRef]
- Eom, D.-G.; Kim, S.-H. 3D Printing of Tungsten-Polymer Composites for Radiation Shielding. J. Korean Soc. Radiol. 2020, 14, 643–650. [Google Scholar]
- Cho, Y.-I.; Kim, J.-H.; Bae, S.-I. Evaluation of Shielding Performance of Tungsten Containing 3D Printing Materials for High-Energy Electron Radiation Therapy. J. Korean Soc. Radiol. 2023, 17, 641–649. [Google Scholar]
- Clarke, A.J.; Dickson, A.; Dowling, D.P. Fabrication and Performance of Continuous 316 Stainless Steel Fibre-Reinforced 3D-Printed PLA Composites. Polymers 2023, 16, 63. [Google Scholar] [CrossRef]
- Seltzer, S. Tables of X-ray Mass Attenuation Coefficients and Mass Energy-Absorption Coefficients; NIST Standard Reference Database 126; NIST: Gaithersburg, MD, USA, 1995. [Google Scholar]
- Podgorsak, E.B.; Internationale Atom Energie Agency (Eds.) Radiation Oncology Physics: A Handbook for Teachers and Students; STI/PUB; International Atomic Energy Agency: Vienna, Austria, 2005; ISBN 978-92-0-107304-4. [Google Scholar]
- International Atomic Energy Agency. Absorbed Dose Determination in External Beam Radiotherapy; Technical Reports Series No. 398; IAEA: Vienna, Austria, 2000. [Google Scholar]
- Almond, P.R.; Biggs, P.J.; Coursey, B.M.; Hanson, W.F.; Huq, M.S.; Nath, R.; Rogers, D.W. AAPM’s TG-51 protocol for clinical reference dosimetry of high-energy photon and electron beams. Med. Phys. 1999, 26, 1847–1870. [Google Scholar] [CrossRef]
- Chang, S.X.; Cullip, T.J.; Deschesne, K.M.; Miller, E.P.; Rosenman, J.G. Compensators: An alternative IMRT delivery technique. J. Appl. Clin. Med. Phys. 2004, 5, 15–36. [Google Scholar] [CrossRef]
- Meigooni, A.S.; Malik, U.; Zhang, H.; Dini, S.A.; Meigooni, N.J.; Komanduri, K.; Mohiuddin, M. Grid: A location dependent intensity modulated radiotherapy for bulky tumors. Iran. J. Radiat. Res. 2005, 2, 167–174. [Google Scholar]
- The Virtual Foundry: Rapid 3D Shield Radiation. Available online: https://rapid3dshield.com/3d-shield/ (accessed on 24 February 2024).
- Meigooni, A.S.; Gnaster, M.; Dou, K.; Johnson, E.L.; Meigooni, N.J.; Kudrimoti, M. Dosimetric evaluation of parallel opposed spatially fractionated radiation therapy of deep-seated bulky tumors. Med. Phys. 2007, 34, 2. [Google Scholar] [CrossRef]
- Grams, M.P.; Deufel, C.L.; Kavanaugh, J.A.; Corbin, K.S.; Ahmed, S.K.; Haddock, M.G.; Lester, S.C.; Ma, D.J.; Petersen, I.A.; Finley, R.R.; et al. Clinical Aspects of Spatially Fractionated Radiation Therapy Treatments. Phys. Medica 2023, 111, 102616. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.I.; Daniels, J.; Cohen, D.; Li, Y.; Ha, C.S.; Eng, T.Y. Clinical Outcomes of Spatially Fractionated GRID Radiotherapy in the Treatment of Bulky Tumors of the Head and Neck. Cureus 2019, 11, e4637. [Google Scholar] [CrossRef] [PubMed]
- DotDecimal: Spatially Fractionated GRID Radiotherapy. Available online: https://dotdecimal.com/wp-content/uploads/2019/06/Photon-Grid-Blocks-Overview-Datasheet-MKT-438-Rev.-06042019.pdf (accessed on 24 February 2024).
- Avelino, S.R.; Silva, L.F.O.; Miosso, C.J. Use of 3D-Printers to Create Intensity-Modulated Radiotherapy Compensator Blocks. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; IEEE: Piscataway, NJ, USA, 2012; pp. 5718–5721. [Google Scholar]
- Schulz, J.B.; Gibson, C.; Dubrowski, P.; Marquez, C.M.; Million, L.; Qian, Y.; Skinner, L.; Yu, A.S. Shaping success: Clinical implementation of a 3D-printed electron cutout program in external beam radiation therapy. Front. Oncol. 2023, 9, 1237037. [Google Scholar] [CrossRef] [PubMed]
- Van Schelt, J.; Smith, D.L.; Fong, N.; Toomeh, D.; Sponseller, P.A.; Brown, D.W.; Macomber, M.W.; Mayr, N.A.; Patel, S.; Shulman, A.; et al. A Ring-Based Compensator IMRT System Optimized for Low- and Middle-Income Countries: Design and Treatment Planning Study. Med. Phys. 2018, 45, 3275–3286. [Google Scholar] [CrossRef] [PubMed]
- Dickson, A.N.; Abourayana, H.M.; Dowling, D.P. 3D printing of fibre-reinforced thermoplastic composites using fused filament fabrication—A review. Polymers 2020, 12, 2188. [Google Scholar] [CrossRef] [PubMed]
- Tymrak, B.M.; Kreiger, M.; Pearce, J.M. Mechanical Properties of Components Fabricated with Open-Source 3-D Printers under Realistic Environmental Conditions. Mater. Des. 2014, 58, 242–246. [Google Scholar] [CrossRef]
- Mohammadizadeh, M.; Lu, H.; Fidan, I.; Tantawi, K.; Gupta, A.; Hasanov, S.; Zhang, Z.; Alifui-Segbaya, F.; Rennie, A. Mechanical and Thermal Analyses of Metal-PLA. Inventions 2020, 5, 44. [Google Scholar] [CrossRef]
- International Atomic Energy Agency (IAEA). Physical Aspects of Quality Assurance in Radiotherapy: Quality Control Protocol; Technical Document No. 1151 (TECDOC 1151); IAEA: Viena, Austria, 2000. [Google Scholar]
- International Atomic Energy Agency. Dosimetry in Diagnostic Radiology: An International Code of Practice; Technical Reports Series No. 457; IAEA: Vienna, Austria, 2007. [Google Scholar]
- Fisher Scientific. Available online: https://www.fishersci.ca/shop/products/tungsten-powder-50-100-mesh-99-metals-basis-thermo-scientific/p-7059837 (accessed on 24 January 2024).
- ASTM D792; Standard Test Methods for Density and Specific Gravity (Relative Density) of Plastics by Displacement. ASTM: West Conshohocken, PA, USA, 2020.
- Aruanno, B.; Paoli, A.; Razionale, A.V.; Tamburrino, F. Effect of printing parameters on extrusion-based additive manufacturing using highly filled CuSn12 filament. Int. J. Adv. Manuf. Technol. 2023, 128, 1101–1114. [Google Scholar] [CrossRef]
- Patel, A.; Taufik, M. Extrusion-Based Technology in Additive Manufacturing: A Comprehensive Review. Arab. J. Sci. Eng. 2022, 49, 1309–1342. [Google Scholar] [CrossRef]
- Ehrmann, G.; Ehrmann, A. Investigation of the shape-memory properties of 3D printed PLA structures with different infills. Polymers 2021, 13, 164. [Google Scholar] [CrossRef]
- Porter, J.H.; Cain, T.M.; Fox, S.L.; Harvey, P.S. Influence of infill properties on flexural rigidity of 3D-printed structural members. Virtual Phys. Prototyp. 2019, 14, 148–159. [Google Scholar] [CrossRef]
- ASTM D638; Standard Test Method for Tensile Properties of Plastics. ASTM: West Conshohocken, PA, USA, 2022.
- Nobah, A.; Mohiuddin, M.; Devic, S.; Moftah, B. Effective spatially fractionated GRID radiation treatment planning for a passive grid block. Br. J. Radiol. 2015, 88, 20140363. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health (NIH) 8-Bit Grayscale Standard for 8 Bits Images in ImageJ. Available online: https://imagej.net/nih-image/index.html (accessed on 24 January 2024).
- Taherkhani, A.; Mohammadi, M.; Saboori, M.; Changizi, V. Evauation of the physical characteristic of Cerrobend blocks used for radiation therapy. Iran. J. Radiat. Res. 2010, 8, 93–101. [Google Scholar]
- Heidari-Rarani, M.; Rafiee-Afarani, M.; Zahedi, A.M. Mechanical characterization of FDM 3D printing of continuous carbon fiber reinforced PLA composites. Compos. Part B Eng. 2019, 175, 107147. [Google Scholar] [CrossRef]
- Yao, Y.; Li, M.; Lackner, M.; Herfried, L. A continuous fiber-reinforced additive manufacturing processing based on PET fiber and PLA. Materials 2020, 13, 3044. [Google Scholar] [CrossRef]
- West, C.; McTaggart, R.; Letcher, T.; Raynie, D.; Roy, R. Effects of gamma irradiation upon the mechanical and chemical properties of 3D-printed samples of polylactic acid. J. Manuf. Sci. Eng 2019, 141, 041002. [Google Scholar] [CrossRef]







| Sample | Layer Height (mm) | Deposition Speed (mm/s) | Nozzle Temperature (°C) |
|---|---|---|---|
| 1 | 0.15 | 52.5 | 215 |
| 2 | 0.15 | 70 | 215 |
| 3 | 0.15 | 105 | 215 |
| 4 | 0.30 | 52.5 | 215 |
| 5 | 0.30 | 70 | 215 |
| 6 | 0.30 | 105 | 215 |
| 7 | 0.45 | 52.5 | 215 |
| 8 | 0.45 | 70 | 215 |
| 9 | 0.45 | 105 | 215 |
| 10 | 0.30 | 70 | 205 |
| 11 | 0.30 | 70 | 225 |
| 12 | 0.30 | 70 | 235 |
| Adjustment Parameters and Printing Characteristics | |
|---|---|
| Extruder nozzle diameter (mm) | 0.6 |
| Deposition speed (mm/s) | 70 |
| Extruder temperature (°C) | 215 |
| Layer height (mm) | 0.15, 0.30, 0.45 |
| Infill percentage (%) | 100 |
| Diameter of both strands (mm) | 1.75 |
| Material | %w/w |
|---|---|
| H | 0.00386 |
| C | 0.03450 |
| O | 0.03064 |
| W | 0.93100 |
| Samples | Length (cm) | Width (cm) | Thickness (cm) | Mass (g) | Density (g/cm3) |
|---|---|---|---|---|---|
| 1 | 1.940 | 1.950 | 0.175 | 4.8229 | 7.30 |
| 2 | 1.830 | 1.830 | 0.166 | 4.0136 | 7.22 |
| 3 | 1.940 | 1.950 | 0.173 | 4.5862 | 7.03 |
| 4 | 2.000 | 1.950 | 0.176 | 4.8169 | 7.02 |
| 5 | 1.977 | 1.978 | 0.177 | 4.7807 | 6.91 |
| 6 | 2.005 | 2.005 | 0.174 | 4.6583 | 6.66 |
| 7 | 1.993 | 1.992 | 0.180 | 4.8488 | 6.79 |
| 8 | 1.993 | 1.991 | 0.182 | 4.8345 | 6.71 |
| 9 | 1.991 | 1.994 | 0.176 | 4.7261 | 6.78 |
| 10 | 1.880 | 1.880 | 0.179 | 3.8089 | 6.02 |
| 11 | 2.010 | 2.005 | 0.180 | 4.8486 | 6.71 |
| 12 | 2.018 | 2.018 | 0.168 | 4.8942 | 7.18 |
| Infill | Year 2023 | Year 2024 | ||||
|---|---|---|---|---|---|---|
| Length (cm) | Width (cm) | Thickness (cm) | Length (cm) | Width (cm) | Thickness (cm) | |
| 15% | 0.964±0.002 | 0.964 ± 0.002 | 1.006 ± 0.002 | 0.962 ± 0.002 | 0.963 ± 0.002 | 1.006 ± 0.002 |
| 50% | 0.976 ± 0.002 | 0.972 ± 0.002 | 1.006 ± 0.002 | 0.971 ± 0.002 | 0.970 ± 0.002 | 1.004 ± 0.002 |
| 100% | 1.009 ± 0.002 | 1.008 ± 0.002 | 1.008 ± 0.002 | 1.010 ± 0.002 | 1.008 ± 0.002 | 1.009 ± 0.002 |
| Material | Layer Height (mm) | Young Module (MPa) | Energy at Maximum Tensile Stress (J) | Tensile Strength (MPa) |
|---|---|---|---|---|
| PLA | 0.15 | 2932.04 | 0.19 | 52.69 |
| 0.30 | 2741.82 | 0.18 | 50.03 | |
| 0.45 | 2784.30 | 0.17 | 51.42 | |
| PLA-W | 0.15 | 2316.58 | 0.02 | 10.06 |
| 0.30 | 2293.17 | 0.02 | 12.24 | |
| 0.45 | 2347.98 | 0.02 | 12.91 |
| Sample | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Value | 0.109 | 0.131 | 0.181 | 0.147 | 0.032 | 0.100 | 0.145 | 0.166 | 0.024 | 0.076 | 0.131 | 0.181 |
| STD | 0.053 | 0.054 | 0.051 | 0.061 | 0.045 | 0.050 | 0.054 | 0.056 | 0.041 | 0.045 | 0.053 | 0.056 |
| Energy | 1 MeV | 1.5 MeV | 2 MeV | 3 MeV | 4 MeV | 5 MeV | 6 MeV |
|---|---|---|---|---|---|---|---|
| μm | 6.628 × 10−2 | 5.550 × 10−2 | 4.461 × 10−2 | 4.042 × 10−2 | 3.950 × 10−2 | 3.970 × 10−2 | 4.039 × 10−2 |
| Energy [MV] | First HVL [cm] | μm [cm2/g] | Effective Energy Beam [MeV] | Density [g/cm3] | μ [cm−1] |
|---|---|---|---|---|---|
| 6 | 2.138 | 0.04692 | 1.747 | 6.91 | 0.3242 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Velásquez, J.; Fuentealba, M.; Santibáñez, M. Characterization of Radiation Shielding Capabilities of High Concentration PLA-W Composite for 3D Printing of Radiation Therapy Collimators. Polymers 2024, 16, 769. https://doi.org/10.3390/polym16060769
Velásquez J, Fuentealba M, Santibáñez M. Characterization of Radiation Shielding Capabilities of High Concentration PLA-W Composite for 3D Printing of Radiation Therapy Collimators. Polymers. 2024; 16(6):769. https://doi.org/10.3390/polym16060769
Chicago/Turabian StyleVelásquez, José, Melani Fuentealba, and Mauricio Santibáñez. 2024. "Characterization of Radiation Shielding Capabilities of High Concentration PLA-W Composite for 3D Printing of Radiation Therapy Collimators" Polymers 16, no. 6: 769. https://doi.org/10.3390/polym16060769
APA StyleVelásquez, J., Fuentealba, M., & Santibáñez, M. (2024). Characterization of Radiation Shielding Capabilities of High Concentration PLA-W Composite for 3D Printing of Radiation Therapy Collimators. Polymers, 16(6), 769. https://doi.org/10.3390/polym16060769