Molecular Mechanisms and Clinical Application of Multipotent Stem Cells for Spinal Cord Injury
Abstract
:1. Introduction
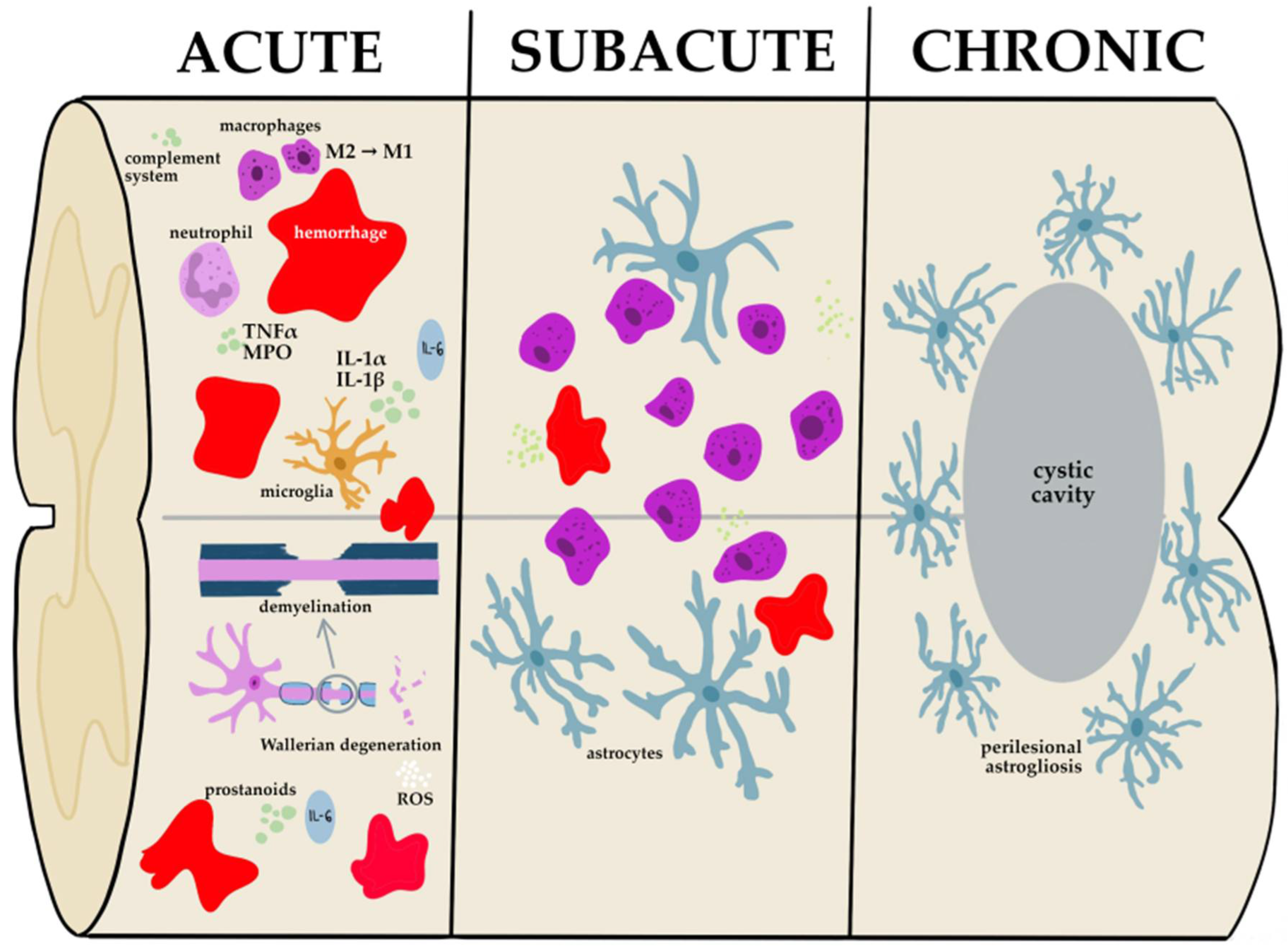
2. Pathophysiology of Spinal Cord Injury
3. Stem Cell Types for Stem Cell Therapy
3.1. Stem Cells’ Classification
3.2. Pluripotent Stem Cells
3.3. Multipotent Stem Cells
4. Molecular Mechanisms of Multipotent Stem Cells at SCI Microenvironment
4.1. Mesenchymal Stem Cells
4.2. Neural Stem Cells
4.3. Hematopoietic Stem Cells
5. Clinical Studies Regarding Multipotent Stem Cells for SCI Treatment
5.1. Mesenchymal Stem Cells
5.2. Neural Stem Cells
5.3. Hematopoietic Stem Cells
6. Optimal Protocol for Stem Cell Administration
6.1. Transplantation Route
6.2. Timing
6.3. Dosing
7. Novel Therapeutic Approaches Based on Stem Cell Therapy
7.1. Stem-Cell-Derived Exosomes
7.2. Gene-Modified Stem Cells
7.3. Biomaterials
8. Challenges, Barriers, and Future Directions
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Lo, J.; Chan, L.; Flynn, S. A Systematic Review of the Incidence, Prevalence, Costs, and Activity/Work Limitations of Amputation, Osteoarthritis, Rheumatoid Arthritis, Back Pain, Multiple Sclerosis, Spinal Cord Injury, Stroke, and Traumatic Brain Injury in the United States: A 2019 Update. Arch. Phys. Med. Rehabil. 2021, 102, 115. [Google Scholar] [CrossRef]
- Chay, W.; Kirshblum, S. Predicting Outcomes After Spinal Cord Injury. Phys. Med. Rehabil. Clin. N. Am. 2020, 31, 331–343. [Google Scholar] [CrossRef]
- Michel, M.; Goldman, M.; Peart, R.; Martinez, M.; Reddy, R.; Lucke-Wold, B. Spinal Cord Injury: A Review of Current Management Considerations and Emerging Treatments. J. Neurol. Sci. Res. 2021, 2, 14. [Google Scholar]
- Haddad, A.F.; Burke, J.F.; Dhall, S.S. The Natural History of Spinal Cord Injury. Neurosurg. Clin. N. Am. 2021, 32, 315–321. [Google Scholar] [CrossRef]
- Golestani, A.; Shobeiri, P.; Sadeghi-Naini, M.; Jazayeri, S.B.; Maroufi, S.F.; Ghodsi, Z.; Dabbagh Ohadi, M.A.; Mohammadi, E.; Rahimi-Movaghar, V.; Ghodsi, S.M. Epidemiology of Traumatic Spinal Cord Injury in Developing Countries from 2009 to 2020: A Systematic Review and Meta-Analysis. Neuroepidemiology 2022, 56, 219–239. [Google Scholar] [CrossRef]
- Kim, G.-U.; Sung, S.-E.; Kang, K.-K.; Choi, J.-H.; Lee, S.; Sung, M.; Yang, S.Y.; Kim, S.-K.; Kim, Y.I.; Lim, J.-H.; et al. Therapeutic Potential of Mesenchymal Stem Cells (MSCs) and MSC-Derived Extracellular Vesicles for the Treatment of Spinal Cord Injury. Int. J. Mol. Sci. 2021, 22, 3672. [Google Scholar] [CrossRef]
- Smith, É.; Fitzpatrick, P.; Lyons, F.; Morris, S.; Synnott, K. Epidemiology of Non-Traumatic Spinal Cord Injury in Ireland—A Prospective Population-Based Study. J. Spinal Cord Med. 2022, 45, 76–81. [Google Scholar] [CrossRef]
- Litak, J.; Czyżewski, W.; Szymoniuk, M.; Sakwa, L.; Pasierb, B.; Litak, J.; Hoffman, Z.; Kamieniak, P.; Roliński, J. Biological and Clinical Aspects of Metastatic Spinal Tumors. Cancers 2022, 14, 4599. [Google Scholar] [CrossRef]
- Gober, J.; Thomas, S.P.; Gater, D.R. Pediatric Spina Bifida and Spinal Cord Injury. J. Pers. Med. 2022, 12, 985. [Google Scholar] [CrossRef]
- Sahbani, K.; Cardozo, C.P.; Bauman, W.A.; Tawfeek, H.A. Inhibition of TGF-Beta Signaling Attenuates Disuse-Induced Trabecular Bone Loss After Spinal Cord Injury in Male Mice. Endocrinology 2022, 163, bqab230. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Tetreault, L.A.; Wilson, J.R.; Aarabi, B.; Anderson, P.; Arnold, P.M.; Brodke, D.S.; Burns, A.S.; Chiba, K.; Dettori, J.R.; et al. A Clinical Practice Guideline for the Management of Patients with Acute Spinal Cord Injury and Central Cord Syndrome: Recommendations on the Timing (≤24 Hours Versus >24 Hours) of Decompressive Surgery. Glob. Spine J. 2017, 7, 195S–202S. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Wilson, J.R.; Tetreault, L.A.; Aarabi, B.; Anderson, P.; Arnold, P.M.; Brodke, D.S.; Burns, A.S.; Chiba, K.; Dettori, J.R.; et al. A Clinical Practice Guideline for the Management of Patients with Acute Spinal Cord Injury: Recommendations on the Use of Methylprednisolone Sodium Succinate. Glob. Spine J. 2017, 7, 203S–211S. [Google Scholar] [CrossRef]
- Wang, T.Y.; Park, C.; Zhang, H.; Rahimpour, S.; Murphy, K.R.; Goodwin, C.R.; Karikari, I.O.; Than, K.D.; Shaffrey, C.I.; Foster, N.; et al. Management of Acute Traumatic Spinal Cord Injury: A Review of the Literature. Front. Surg. 2021, 8, 698736. [Google Scholar] [CrossRef]
- Albu, S.; Kumru, H.; Coll, R.; Vives, J.; Vallés, M.; Benito-Penalva, J.; Rodríguez, L.; Codinach, M.; Hernández, J.; Navarro, X.; et al. Clinical Effects of Intrathecal Administration of Expanded Wharton Jelly Mesenchymal Stromal Cells in Patients with Chronic Complete Spinal Cord Injury: A Randomized Controlled Study. Cytotherapy 2021, 23, 146–156. [Google Scholar] [CrossRef]
- Costăchescu, B.; Niculescu, A.G.; Dabija, M.G.; Teleanu, R.I.; Grumezescu, A.M.; Eva, L. Novel Strategies for Spinal Cord Regeneration. Int. J. Mol. Sci. 2022, 23, 4552. [Google Scholar] [CrossRef]
- Hoang, D.M.; Pham, P.T.; Bach, T.Q.; Ngo, A.T.L.; Nguyen, Q.T.; Phan, T.T.K.; Nguyen, G.H.; Le, P.T.T.; Hoang, V.T.; Forsyth, N.R.; et al. Stem Cell-Based Therapy for Human Diseases. Signal Transduct. Target. Ther. 2022, 7, 272. [Google Scholar] [CrossRef]
- Pucułek, M.; Baj, J.; Portincasa, P.; Sitarz, M.; Grochowski, C.; Radzikowska, E. The Morphology and Application of Stem Cells in Digestive System Surgery. Folia Morphol. 2021, 80, 13–19. [Google Scholar] [CrossRef] [Green Version]
- Li, T.-T.; Wang, Z.-R.; Yao, W.-Q.; Linghu, E.-Q.; Wang, F.-S.; Shi, L. Stem Cell Therapies for Chronic Liver Diseases: Progress and Challenges. Stem Cells Transl. Med. 2022, 11, 900–911. [Google Scholar] [CrossRef]
- Gruca, D.; Zając, M.; Wróblewski, W.; Borowiecka, M.; Buksak, D. The Relation between Adipose-Derived Stem Cells and Wound Healing Process—The Review. J. Educ. Health Sport 2022, 12, 87–93. [Google Scholar] [CrossRef]
- Sarsenova, M.; Issabekova, A.; Abisheva, S.; Rutskaya-Moroshan, K.; Ogay, V.; Saparov, A. Mesenchymal Stem Cell-Based Therapy for Rheumatoid Arthritis. Int. J. Mol. Sci. 2021, 22, 1592. [Google Scholar] [CrossRef]
- Hassanzadeh, A.; Shamlou, S.; Yousefi, N.; Nikoo, M.; Verdi, J. Genetically-Modified Stem Cell in Regenerative Medicine and Cancer Therapy; A New Era. Curr. Gene Ther. 2022, 22, 23–39. [Google Scholar] [CrossRef]
- Puranik, N.; Arukha, A.P.; Yadav, S.K.; Yadav, D.; Jin, J.O. Exploring the Role of Stem Cell Therapy in Treating Neurodegenerative Diseases: Challenges and Current Perspectives. Curr. Stem Cell Res. Ther. 2022, 17, 113–125. [Google Scholar] [CrossRef]
- Ejma, M.; Madetko, N.; Brzecka, A.; Alster, P.; Budrewicz, S.; Koszewicz, M.; Misiuk-Hojło, M.; Tomilova, I.K.; Somasundaram, S.G.; Kirkland, C.E. The Role of Stem Cells in the Therapy of Stroke. Curr. Neuropharmacol. 2022, 20, 630–647. [Google Scholar] [CrossRef]
- Peterson, S.; Jalil, A.; Beard, K.; Kakara, M.; Sriwastava, S. Updates on Efficacy and Safety Outcomes of New and Emerging Disease Modifying Therapies and Stem Cell Therapy for Multiple Sclerosis: A Review. Mult. Scler. Relat. Disord. 2022, 68, 104125. [Google Scholar] [CrossRef]
- Li, X.; Sundström, E. Stem Cell Therapies for Central Nervous System Trauma: The 4 Ws—What, When, Where, and Why. Stem Cells Transl. Med. 2022, 11, 14–25. [Google Scholar] [CrossRef]
- Zipser, C.M.; Cragg, J.J.; Guest, J.D.; Fehlings, M.G.; Jutzeler, C.R.; Anderson, A.J.; Curt, A. Cell-Based and Stem-Cell-Based Treatments for Spinal Cord Injury: Evidence from Clinical Trials. Lancet Neurol. 2022, 21, 659–670. [Google Scholar] [CrossRef]
- Saini, R.; Pahwa, B.; Agrawal, D.; Singh, P.K.; Gujjar, H.; Mishra, S.; Jagdevan, A.; Misra, M.C. Efficacy and Outcome of Bone Marrow Derived Stem Cells Transplanted via Intramedullary Route in Acute Complete Spinal Cord Injury—A Randomized Placebo Controlled Trial. J. Clin. Neurosci. 2022, 100, 7–14. [Google Scholar] [CrossRef]
- Yang, Y.; Pang, M.; Du, C.; Liu, Z.-Y.; Chen, Z.-H.; Wang, N.-X.; Zhang, L.-M.; Chen, Y.-Y.; Mo, J.; Dong, J.-W.; et al. Repeated Subarachnoid Administrations of Allogeneic Human Umbilical Cord Mesenchymal Stem Cells for Spinal Cord Injury: A Phase 1/2 Pilot Study. Cytotherapy 2021, 23, 57–64. [Google Scholar] [CrossRef]
- Hur, J.W.; Cho, T.H.; Park, D.H.; Lee, J.B.; Park, J.Y.; Chung, Y.G. Intrathecal Transplantation of Autologous Adipose-Derived Mesenchymal Stem Cells for Treating Spinal Cord Injury: A Human Trial. J. Spinal Cord Med. 2016, 39, 655–664. [Google Scholar] [CrossRef] [Green Version]
- Curt, A.; Hsieh, J.; Schubert, M.; Hupp, M.; Friedl, S.; Freund, P.; Huber, E.; Pfyffer, D.; Sutter, R.; Jutzeler, C.; et al. The Damaged Spinal Cord Is a Suitable Target for Stem Cell Transplantation. Neurorehabil. Neural Repair 2020, 34, 758–768. [Google Scholar] [CrossRef]
- Levi, A.D.; Anderson, K.D.; Okonkwo, D.O.; Park, P.; Bryce, T.N.; Kurpad, S.N.; Aarabi, B.; Hsieh, J.; Gant, K. Clinical Outcomes from a Multi-Center Study of Human Neural Stem Cell Transplantation in Chronic Cervical Spinal Cord Injury. J. Neurotrauma 2019, 36, 891–902. [Google Scholar] [CrossRef]
- Smirnov, V.A.; Radaev, S.M.; Morozova, Y.V.; Ryabov, S.I.; Yadgarov, M.Y.; Bazanovich, S.A.; Lvov, I.S.; Talypov, A.E.; Grin’, A.A. Systemic Administration of Allogeneic Cord Blood Mononuclear Cells in Adults with Severe Acute Contusion Spinal Cord Injury: Phase 1/2a Pilot Clinical Study-Safety and Primary Efficacy Evaluation. World Neurosurg. 2022, 161, e319–e338. [Google Scholar] [CrossRef]
- Gant, K.L.; Guest, J.D.; Palermo, A.E.; Vedantam, A.; Jimsheleishvili, G.; Bunge, M.B.; Brooks, A.E.; Anderson, K.D.; Thomas, C.K.; Santamaria, A.J.; et al. Phase 1 Safety Trial of Autologous Human Schwann Cell Transplantation in Chronic Spinal Cord Injury. J. Neurotrauma 2022, 39, 285–299. [Google Scholar] [CrossRef]
- Tabakow, P.; Jarmundowicz, W.; Czapiga, B.; Fortuna, W.; Miedzybrodzki, R.; Czyz, M.; Huber, J.; Szarek, D.; Okurowski, S.; Szewczyk, P.; et al. Transplantation of Autologous Olfactory Ensheathing Cells in Complete Human Spinal Cord Injury. Cell Transplant. 2013, 22, 1591–1612. [Google Scholar] [CrossRef]
- Rövekamp, M.; von Glinski, A.; Volkenstein, S.; Dazert, S.; Sengstock, C.; Schildhauer, T.A.; Breisch, M. Olfactory Stem Cells for the Treatment of Spinal Cord Injury-A New Pathway to the Cure? World Neurosurg. 2022, 161, e408–e416. [Google Scholar] [CrossRef]
- Fessler, R.G.; Ehsanian, R.; Liu, C.Y.; Steinberg, G.K.; Jones, L.; Lebkowski, J.S.; Wirth, E.D.; McKenna, S.L. A Phase 1/2a Dose-Escalation Study of Oligodendrocyte Progenitor Cells in Individuals with Subacute Cervical Spinal Cord Injury. J. Neurosurg. Spine 2022, 37, 812–820. [Google Scholar] [CrossRef]
- Liu, J.; Gao, J.; Liang, Z.; Gao, C.; Niu, Q.; Wu, F.; Zhang, L. Mesenchymal Stem Cells and Their Microenvironment. Stem Cell Res. Ther. 2022, 13, 429. [Google Scholar] [CrossRef]
- Ahuja, C.S.; Nori, S.; Tetreault, L.; Wilson, J.; Kwon, B.; Harrop, J.; Choi, D.; Fehlings, M.G. Traumatic Spinal Cord Injury—Repair and Regeneration. Clin. Neurosurg. 2017, 80, S22–S90. [Google Scholar] [CrossRef]
- Garcia, E.; Aguilar-Cevallos, J.; Silva-Garcia, R.; Ibarra, A. Cytokine and Growth Factor Activation in Vivo and in Vitro after Spinal Cord Injury. Mediat. Inflamm. 2016, 2016, 9476020. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Q.; Liu, F.; Zhou, B.; Liu, H.; Wang, X.; Li, S. Ferroptosis: A Novel Therapeutic Direction of Spinal Cord Injury. Comput. Math. Methods Med. 2022, 2022, 790621. [Google Scholar] [CrossRef]
- Slater, P.G.; Domínguez-Romero, M.E.; Villarreal, M.; Eisner, V.; Larraín, J. Mitochondrial Function in Spinal Cord Injury and Regeneration. Cell. Mol. Life Sci. 2022, 79, 1–24. [Google Scholar] [CrossRef]
- Salman, M.M.; Kitchen, P.; Halsey, A.; Wang, M.X.; Törnroth-Horsefield, S.; Conner, A.C.; Badaut, J.; Iliff, J.J.; Bill, R.M. Emerging Roles for Dynamic Aquaporin-4 Subcellular Relocalization in CNS Water Homeostasis. Brain 2022, 145, 64–75. [Google Scholar] [CrossRef]
- Fan, B.; Wei, Z.; Yao, X.; Shi, G.; Cheng, X.; Zhou, X.; Zhou, H.; Ning, G.; Kong, X.; Feng, S. Microenvironment Imbalance of Spinal Cord Injury. Cell Transplant. 2018, 27, 853–866. [Google Scholar] [CrossRef] [Green Version]
- Beirowski, B.; Nógrádi, A.; Babetto, E.; Garcia-Alias, G.; Coleman, M.P. Mechanisms of Axonal Spheroid Formation in Central Nervous System Wallerian Degeneration. J. Neuropathol. Exp. Neurol. 2010, 69, 455–472. [Google Scholar] [CrossRef]
- Alizadeh, A.; Dyck, S.M.; Karimi-Abdolrezaee, S. Traumatic Spinal Cord Injury: An Overview of Pathophysiology, Models and Acute Injury Mechanisms. Front. Neurol. 2019, 10, 282. [Google Scholar] [CrossRef] [Green Version]
- Jia, M.; Njapo, S.A.N.; Rastogi, V.; Hedna, V.S. Taming Glutamate Excitotoxicity: Strategic Pathway Modulation for Neuroprotection. CNS Drugs 2015, 29, 153–162. [Google Scholar] [CrossRef]
- Brat, D.J. Normal Brain Histopathology. In Practical Surgical Neuropathology: A Diagnostic Approach; Elsevier: Amsterdam, The Netherlands, 2018; pp. 19–37. [Google Scholar] [CrossRef]
- Sharma, K.; Zhang, G.; Li, S. Astrogliosis and Axonal Regeneration. Neural Regen. 2015, 181–196. [Google Scholar] [CrossRef]
- Bacakova, L.; Zarubova, J.; Travnickova, M.; Musilkova, J.; Pajorova, J.; Slepicka, P.; Kasalkova, N.S.; Svorcik, V.; Kolska, Z.; Motarjemi, H.; et al. Stem Cells: Their Source, Potency and Use in Regenerative Therapies with Focus on Adipose-Derived Stem Cells—A Review. Biotechnol. Adv. 2018, 36, 1111–1126. [Google Scholar] [CrossRef]
- Sobhani, A.; Sobhani, A.; Khanlarkhani, N.; Baazm, M.; Mohammadzadeh, F.; Najafi, A.; Mehdinejadiani, S.; Aval, F.S. Multipotent Stem Cell and Current Application. Acta Med. Iran. 2017, 55, 6–23. [Google Scholar]
- Zakrzewski, W.; Dobrzyński, M.; Szymonowicz, M.; Rybak, Z. Stem Cells: Past, Present, and Future. Stem Cell Res. Ther. 2019, 10, 68. [Google Scholar] [CrossRef]
- Takahashi, K.; Tanabe, K.; Ohnuki, M.; Narita, M.; Ichisaka, T.; Tomoda, K.; Yamanaka, S. Induction of Pluripotent Stem Cells from Adult Human Fibroblasts by Defined Factors. Cell 2007, 131, 861–872. [Google Scholar] [CrossRef]
- Dulak, J.; Szade, K.; Szade, A.; Nowak, W.; Józkowicz, A. Adult Stem Cells: Hopes and Hypes of Regenerative Medicine* Definition of Stem and Progenitor Cell. Acta Biochim. Pol. 2015, 62, 329–337. [Google Scholar] [CrossRef] [Green Version]
- Mirzaei, H.; Sahebkar, A.; Sichani, L.S.; Moridikia, A.; Nazari, S.; Nahand, J.S.; Salehi, H.; Stenvang, J.; Masoudifar, A.; Mirzaei, H.R.; et al. Therapeutic Application of Multipotent Stem Cells. J. Cell. Physiol. 2018, 233, 2815–2823. [Google Scholar] [CrossRef]
- Paliwal, S.; Fiumera, H.L.; Mohanty, S. Stem Cell Plasticity and Regenerative Potential Regulation through Ca2+-Mediated Mitochondrial Nuclear Crosstalk. Mitochondrion 2021, 56, 1–14. [Google Scholar] [CrossRef]
- Grochowski, C.; Radzikowska, E.; Maciejewski, R. Neural Stem Cell Therapy—Brief Review. Clin. Neurol. Neurosurg. 2018, 173, 8–14. [Google Scholar] [CrossRef]
- Hawkins, K.E.; Corcelli, M.; Dowding, K.; Ranzoni, A.M.; Vlahova, F.; Hau, K.L.; Hunjan, A.; Peebles, D.; Gressens, P.; Hagberg, H.; et al. Embryonic Stem Cell-Derived Mesenchymal Stem Cells (MSCs) Have a Superior Neuroprotective Capacity Over Fetal MSCs in the Hypoxic-Ischemic Mouse Brain. Stem Cells Transl. Med. 2018, 7, 439–449. [Google Scholar] [CrossRef]
- Xia, Y.; Hu, G.; Chen, Y.; Yuan, J.; Zhang, J.; Wang, S.; Li, Q.; Wang, Y.; Deng, Z. Embryonic Stem Cell Derived Small Extracellular Vesicles Modulate Regulatory T Cells to Protect against Ischemic Stroke. ACS Nano 2021, 15, 7370–7385. [Google Scholar] [CrossRef]
- Wang, X.; Kimbrel, E.A.; Ijichi, K.; Paul, D.; Lazorchak, A.S.; Chu, J.; Kouris, N.A.; Yavanian, G.J.; Lu, S.J.; Pachter, J.S.; et al. Human ESC-Derived MSCs Outperform Bone Marrow MSCs in the Treatment of an EAE Model of Multiple Sclerosis. Stem Cell Rep. 2021, 16, 370–371. [Google Scholar] [CrossRef]
- Araki, R.; Mizutani, E.; Hoki, Y.; Sunayama, M.; Wakayama, S.; Nagatomo, H.; Kasama, Y.; Nakamura, M.; Wakayama, T.; Abe, M. The Number of Point Mutations in Induced Pluripotent Stem Cells and Nuclear Transfer Embryonic Stem Cells Depends on the Method and Somatic Cell Type Used for Their Generation. Stem Cells 2017, 35, 1189–1196. [Google Scholar] [CrossRef] [Green Version]
- Mousaei Ghasroldasht, M.; Seok, J.; Park, H.S.; Liakath Ali, F.B.; Al-Hendy, A. Stem Cell Therapy: From Idea to Clinical Practice. Int. J. Mol. Sci. 2022, 23, 2850. [Google Scholar] [CrossRef]
- Poetsch, M.S.; Strano, A.; Guan, K. Human Induced Pluripotent Stem Cells: From Cell Origin, Genomic Stability, and Epigenetic Memory to Translational Medicine. Stem Cells 2022, 40, 546–555. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Amponsah, A.E.; Kong, D.; He, J.; Ma, Z.; Ma, J.; Cui, H. HiPSC-Neural Stem/Progenitor Cell Transplantation Therapy for Spinal Cord Injury. Curr. Stem Cell Res. Ther. 2022, 17. [Google Scholar] [CrossRef] [PubMed]
- Ji, P.; Manupipatpong, S.; Xie, N.; Li, Y. Induced Pluripotent Stem Cells: Generation Strategy and Epigenetic Mystery behind Reprogramming. Stem Cells Int. 2016, 2016, 8415010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, X. The Immunogenicity of Cells Derived from Induced Pluripotent Stem Cells. Cell. Mol. Immunol. 2014, 11, 14. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.S.; Tang, C.; Rao, M.S.; Weissman, I.L.; Wu, J.C. Tumorigenicity as a Clinical Hurdle for Pluripotent Stem Cell Therapies. Nat. Med. 2013, 19, 998–1004. [Google Scholar] [CrossRef] [Green Version]
- Attia, N.; Mashal, M. Mesenchymal Stem Cells: The Past Present and Future. Adv. Exp. Med. Biol. 2021, 1312, 107–129. [Google Scholar] [CrossRef]
- Oh, S.K.; Choi, K.H.; Yoo, J.Y.; Kim, D.Y.; Kim, S.J.; Jeon, S.R. A Phase III Clinical Trial Showing Limited Efficacy of Autologous Mesenchymal Stem Cell Therapy for Spinal Cord Injury. Neurosurgery 2016, 78, 436–447. [Google Scholar] [CrossRef] [Green Version]
- Vaquero, J.; Zurita, M.; Rico, M.A.; Aguayo, C.; Fernandez, C.; Rodriguez-Boto, G.; Marin, E.; Tapiador, N.; Sevilla, M.; Carballido, J.; et al. Cell Therapy with Autologous Mesenchymal Stromal Cells in Post-Traumatic Syringomyelia. Cytotherapy 2018, 20, 796–805. [Google Scholar] [CrossRef]
- Peng, C.; Li, Y.; Lu, L.; Zhu, J.; Li, H.; Hu, J. Efficient One-Step Induction of Human Umbilical Cord-Derived Mesenchymal Stem Cells (UC-MSCs) Produces MSC-Derived Neurospheres (MSC-NS) with Unique Transcriptional Profile and Enhanced Neurogenic and Angiogenic Secretomes. Stem Cells Int. 2019, 2019, 9208173. [Google Scholar] [CrossRef]
- Qu, J.; Zhang, H. Roles of Mesenchymal Stem Cells in Spinal Cord Injury. Stem Cells Int. 2017, 2017, 5251313. [Google Scholar] [CrossRef] [Green Version]
- Cofano, F.; Boido, M.; Monticelli, M.; Zenga, F.; Ducati, A.; Vercelli, A.; Garbossa, D. Mesenchymal Stem Cells for Spinal Cord Injury: Current Options, Limitations, and Future of Cell Therapy. Int. J. Mol. Sci. 2019, 20, 2698. [Google Scholar] [CrossRef]
- Jiang, W.; Xu, J. Immune Modulation by Mesenchymal Stem Cells. Cell Prolif. 2020, 53, e12712. [Google Scholar] [CrossRef] [Green Version]
- Muthu, S.; Jeyaraman, M.; Gulati, A.; Arora, A. Current Evidence on Mesenchymal Stem Cell Therapy for Traumatic Spinal Cord Injury: Systematic Review and Meta-Analysis. Cytotherapy 2021, 23, 186–197. [Google Scholar] [CrossRef]
- Han, S.; Sun, H.M.; Hwang, K.C.; Kim, S.W. Adipose-Derived Stromal Vascular Fraction Cells: Update on Clinical Utility and Efficacy. Crit. Rev. Eukaryot. Gene Expr. 2015, 25, 145–152. [Google Scholar] [CrossRef]
- Berebichez-Fridman, R.; Montero-Olvera, P.R. Sources and Clinical Applications of Mesenchymal Stem Cells: State-of-the-Art Review. Sultan Qaboos Univ. Med. J. 2018, 18, e264. [Google Scholar] [CrossRef] [Green Version]
- Marino, L.; Castaldi, M.A.; Rosamilio, R.; Ragni, E.; Vitolo, R.; Fulgione, C.; Castaldi, S.G.; Serio, B.; Bianco, R.; Guida, M.; et al. Mesenchymal Stem Cells from the Wharton’s Jelly of the Human Umbilical Cord: Biological Properties and Therapeutic Potential. Int. J. Stem Cells 2019, 12, 218–226. [Google Scholar] [CrossRef]
- Liau, L.L.; Looi, Q.H.; Chia, W.C.; Subramaniam, T.; Ng, M.H.; Law, J.X. Treatment of Spinal Cord Injury with Mesenchymal Stem Cells. Cell Biosci. 2020, 10, 112. [Google Scholar] [CrossRef]
- Anderson, K.D.; Guest, J.D.; Dietrich, W.D.; Bartlett Bunge, M.; Curiel, R.; Dididze, M.; Green, B.A.; Khan, A.; Pearse, D.D.; Saraf-Lavi, E.; et al. Safety of Autologous Human Schwann Cell Transplantation in Subacute Thoracic Spinal Cord Injury. J. Neurotrauma 2017, 34, 2950–2963. [Google Scholar] [CrossRef]
- Andreopoulou, E.; Arampatzis, A.; Patsoni, M.; Kazanis, I. Being a Neural Stem Cell: A Matter of Character but Defined by the Microenvironment. Adv. Exp. Med. Biol. 2017, 1041, 81–118. [Google Scholar] [CrossRef]
- Shahbazi, E.; Moradi, S.; Nemati, S.; Satarian, L.; Basiri, M.; Gourabi, H.; Zare Mehrjardi, N.; Günther, P.; Lampert, A.; Händler, K.; et al. Conversion of Human Fibroblasts to Stably Self-Renewing Neural Stem Cells with a Single Zinc-Finger Transcription Factor. Stem Cell Rep. 2016, 6, 539–551. [Google Scholar] [CrossRef] [Green Version]
- García-González, D.; Murcia-Belmonte, V.; Esteban, P.F.; Ortega, F.; Díaz, D.; Sánchez-Vera, I.; Lebrón-Galán, R.; Escobar-Castañondo, L.; Martínez-Millán, L.; Weruaga, E.; et al. Anosmin-1 over-Expression Increases Adult Neurogenesis in the Subventricular Zone and Neuroblast Migration to the Olfactory Bulb. Brain Struct. Funct. 2016, 221, 239–260. [Google Scholar] [CrossRef]
- Danielson, N.; Byrne, M. Indications for Allogeneic Hematopoietic Cell Transplantation in Myelodysplastic Syndrome. Curr. Hematol. Malig. Rep. 2020, 15, 268–275. [Google Scholar] [CrossRef]
- Mohammadi, R.; Aryan, A.; Omrani, M.D.; Ghaderian, S.M.H.; Fazeli, Z. Autologous Hematopoietic Stem Cell Transplantation (AHSCT): An Evolving Treatment Avenue in Multiple Sclerosis. Biologics 2021, 15, 53–59. [Google Scholar] [CrossRef]
- Oliveira, M.C.; Elias, J.B.; de Moraes, D.A.; Simões, B.P.; Rodrigues, M.; Ribeiro, A.A.F.; Piron-Ruiz, L.; Ruiz, M.A.; Hamerschlak, N. A Review of Hematopoietic Stem Cell Transplantation for Autoimmune Diseases: Multiple Sclerosis, Systemic Sclerosis and Crohn’s Disease. Position Paper of the Brazilian Society of Bone Marrow Transplantation. Hematol. Transfus. Cell Ther. 2021, 43, 65–86. [Google Scholar] [CrossRef]
- Nikoonezhad, M.; Lasemi, M.V.; Alamdari, S.; Mohammadian, M.; Tabarraee, M.; Ghadyani, M.; Hamidpour, M.; Roshandel, E. Treatment of Insulin-Dependent Diabetes by Hematopoietic Stem Cell Transplantation. Transpl. Immunol. 2022, 75, 101682. [Google Scholar] [CrossRef]
- Koda, M.; Okada, S.; Nakayama, T.; Koshizuka, S.; Kamada, T.; Nishio, Y.; Someya, Y.; Yoshinaga, K.; Okawa, A.; Moriya, H.; et al. Hematopoietic Stem Cell and Marrow Stromal Cell for Spinal Cord Injury in Mice. Neuroreport 2005, 16, 1763–1767. [Google Scholar] [CrossRef]
- Ozdemir, Z.N.; Civriz Bozdağ, S. Graft Failure after Allogeneic Hematopoietic Stem Cell Transplantation. Transfus. Apher. Sci. 2018, 57, 163–167. [Google Scholar] [CrossRef]
- Deda, H.; Inci, M.C.; Kurekçi, A.; Kayihan, K.; Özgün, E.; Ustunsoy, G.; Kocabay, S. Treatment of Chronic Spinal Cord Injured Patients with Autologous Bone Marrow-Derived Hematopoietic Stem Cell Transplantation: 1-Year Follow-Up. Cytotherapy 2008, 10, 565–574. [Google Scholar] [CrossRef]
- Müller, A.M.; Huppertz, S.; Henschler, R. Hematopoietic Stem Cells in Regenerative Medicine: Astray or on the Path? Transfus. Med. Hemotherapy 2016, 43, 247–254. [Google Scholar] [CrossRef] [Green Version]
- Mosaad, Y.M. Hematopoietic Stem Cells: An Overview. Transfus. Apher. Sci. 2014, 51, 68–82. [Google Scholar] [CrossRef]
- Hou, Y.; Liu, X.; Guo, Y.; Liu, D.; Guo, P.; Liu, J. Strategies for Effective Neural Circuit Reconstruction After Spinal Cord Injury: Use of Stem Cells and Biomaterials. World Neurosurg. 2022, 161, 82–89. [Google Scholar] [CrossRef]
- Zhao, A.; Chung, M.; Yang, Y.; Pan, X.; Pan, Y.; Cai, S. The SDF-1/CXCR4 Signaling Pathway Directs the Migration of Systemically Transplanted Bone Marrow Mesenchymal Stem Cells towards the Lesion Site in a Rat Model of Spinal Cord Injury. Curr. Stem Cell Res. Ther. 2022, 18, 216–230. [Google Scholar] [CrossRef]
- Pelagalli, A.; Nardelli, A.; Lucarelli, E.; Zannetti, A.; Brunetti, A. Autocrine Signals Increase Ovine Mesenchymal Stem Cells Migration through Aquaporin-1 and CXCR4 Overexpression. J. Cell. Physiol. 2018, 233, 6241–6249. [Google Scholar] [CrossRef]
- Marquez-Curtis, L.A.; Gul-Uludag, H.; Xu, P.; Chen, J.; Janowska-Wieczorek, A. CXCR4 Transfection of Cord Blood Mesenchymal Stromal Cells with the Use of Cationic Liposome Enhances Their Migration toward Stromal Cell-Derived Factor-1. Cytotherapy 2013, 15, 840–849. [Google Scholar] [CrossRef]
- Xie, J.-L.; Wang, X.-R.; Li, M.-M.; Tao, Z.-H.; Teng, W.-W. Saijilafu Mesenchymal Stromal Cell Therapy in Spinal Cord Injury: Mechanisms and Prospects. Front. Cell. Neurosci. 2022, 16, 270. [Google Scholar] [CrossRef]
- Bang, O.Y.; Moon, G.J.; Kim, D.H.; Lee, J.H.; Kim, S.; Son, J.P.; Cho, Y.H.; Chang, W.H.; Kim, Y.H.; Sung, J.H.; et al. Stroke Induces Mesenchymal Stem Cell Migration to Infarcted Brain Areas Via CXCR4 and C-Met Signaling. Transl. Stroke Res. 2017, 8, 449–460. [Google Scholar] [CrossRef]
- He, W.; Shi, C.; Yin, J.; Huang, F.; Yan, W.; Deng, J.; Zhang, B.; Wang, B.; Wang, H. Spinal Cord Decellularized Matrix Scaffold Loaded with Engineered Basic Fibroblast Growth Factor-Overexpressed Human Umbilical Cord Mesenchymal Stromal Cells Promoted the Recovery of Spinal Cord Injury. J. Biomed. Mater. Res. Part B Appl. Biomater. 2022, 111, 51–61. [Google Scholar] [CrossRef]
- Song, P.; Han, T.; Xiang, X.; Wang, Y.; Fang, H.; Niu, Y.; Shen, C. The Role of Hepatocyte Growth Factor in Mesenchymal Stem Cell-Induced Recovery in Spinal Cord Injured Rats. Stem Cell Res. Ther. 2020, 11, 178. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, J.; Zhang, P.; Liu, T.; Xu, J.; Fan, Z.; Shen, Y.; Li, W.; Zhang, H. Calcitonin Gene-Related Peptide Is a Key Factor in the Homing of Transplanted Human MSCs to Sites of Spinal Cord Injury. Sci. Rep. 2016, 6, 27724. [Google Scholar] [CrossRef] [Green Version]
- Fu, X.; Liu, G.; Halim, A.; Ju, Y.; Luo, Q.; Song, G. Mesenchymal Stem Cell Migration and Tissue Repair. Cells 2019, 8, 784. [Google Scholar] [CrossRef] [Green Version]
- Nitzsche, F.; Müller, C.; Lukomska, B.; Jolkkonen, J.; Deten, A.; Boltze, J. Concise Review: MSC Adhesion Cascade-Insights into Homing and Transendothelial Migration. Stem Cells 2017, 35, 1446–1460. [Google Scholar] [CrossRef]
- Nam, D.; Park, A.; Dubon, M.J.; Yu, J.; Kim, W.; Son, Y.; Park, K.S. Coordinated Regulation of Mesenchymal Stem Cell Migration by Various Chemotactic Stimuli. Int. J. Mol. Sci. 2020, 21, 8561. [Google Scholar] [CrossRef]
- Rahimi-Sherbaf, F.; Nadri, S.; Nadri, S.; Rahmani, A.; Oskoei, A.D. Placenta Mesenchymal Stem Cells Differentiation toward Neuronal-like Cells on Nanofibrous Scaffold. BioImpacts 2020, 10, 117–122. [Google Scholar] [CrossRef] [Green Version]
- Zhang, K.; Liu, Z.; Li, G.; Lai, B.Q.; Qin, L.N.; Ding, Y.; Ruan, J.W.; Zhang, S.X.; Zeng, Y.S. Electro-Acupuncture Promotes the Survival and Differentiation of Transplanted Bone Marrow Mesenchymal Stem Cells Pre-Induced with Neurotrophin-3 and Retinoic Acid in Gelatin Sponge Scaffold after Rat Spinal Cord Transection. Stem Cell Rev. Rep. 2014, 10, 612–625. [Google Scholar] [CrossRef]
- Wang, C.; Shi, D.; Song, X.; Chen, Y.; Wang, L.; Zhang, X. Calpain Inhibitor Attenuates ER Stress-Induced Apoptosis in Injured Spinal Cord after Bone Mesenchymal Stem Cells Transplantation. Neurochem. Int. 2016, 97, 15–25. [Google Scholar] [CrossRef]
- Chung, H.J.; Chung, W.H.; Lee, J.H.; Chung, D.J.; Yang, W.J.; Lee, A.J.; Choi, C.B.; Chang, H.S.; Kim, D.H.; Suh, H.J.; et al. Expression of Neurotrophic Factors in Injured Spinal Cord after Transplantation of Human-Umbilical Cord Blood Stem Cells in Rats. J. Vet. Sci. 2016, 17, 97–102. [Google Scholar] [CrossRef]
- Kim, Y.; Jo, S.H.; Kim, W.H.; Kweon, O.K. Antioxidant and Anti-Inflammatory Effects of Intravenously Injected Adipose Derived Mesenchymal Stem Cells in Dogs with Acute Spinal Cord Injury. Stem Cell Res. Ther. 2015, 6, 229. [Google Scholar] [CrossRef] [Green Version]
- Phinney, D.G.; Pittenger, M.F. Concise Review: MSC-Derived Exosomes for Cell-Free Therapy. Stem Cells 2017, 35, 851–858. [Google Scholar] [CrossRef] [Green Version]
- Pittenger, M.F.; Discher, D.E.; Péault, B.M.; Phinney, D.G.; Hare, J.M.; Caplan, A.I. Mesenchymal Stem Cell Perspective: Cell Biology to Clinical Progress. NPJ Regen. Med. 2019, 4, 22. [Google Scholar] [CrossRef] [Green Version]
- Tahmasebi, F.; Barati, S. Effects of Mesenchymal Stem Cell Transplantation on Spinal Cord Injury Patients. Cell Tissue Res. 2022, 389, 373–384. [Google Scholar] [CrossRef]
- Martins, L.F.; Costa, R.O.; Pedro, J.R.; Aguiar, P.; Serra, S.C.; Teixeira, F.G.; Sousa, N.; Salgado, A.J.; Almeida, R.D. Mesenchymal Stem Cells Secretome-Induced Axonal Outgrowth Is Mediated by BDNF. Sci. Rep. 2017, 7, 4153. [Google Scholar] [CrossRef]
- Chang, D.J.; Cho, H.Y.; Hwang, S.; Lee, N.; Choi, C.; Lee, H.; Hong, K.S.; Oh, S.H.; Kim, H.S.; Shin, D.A.; et al. Therapeutic Effect of BDNF-Overexpressing Human Neural Stem Cells (F3.BDNF) in a Contusion Model of Spinal Cord Injury in Rats. Int. J. Mol. Sci. 2021, 22, 6970. [Google Scholar] [CrossRef]
- Sieck, G.C.; Gransee, H.M.; Zhan, W.Z.; Mantilla, C.B. Neural Circuits: Acute Intrathecal BDNF Enhances Functional Recovery after Cervical Spinal Cord Injury in Rats. J. Neurophysiol. 2021, 125, 2158. [Google Scholar] [CrossRef]
- Walker, M.J.; Xu, X.M. History of Glial Cell Line-Derived Neurotrophic Factor (GDNF) and Its Use for Spinal Cord Injury Repair. Brain Sci. 2018, 8, 109. [Google Scholar] [CrossRef] [Green Version]
- Pajer, K.; Bellák, T.; Nógrádi, A. Stem Cell Secretome for Spinal Cord Repair: Is It More than Just a Random Baseline Set of Factors? Cells 2021, 10, 3214. [Google Scholar] [CrossRef]
- Sivak, W.N.; White, J.D.; Bliley, J.M.; Tien, L.W.; Liao, H.T.; Kaplan, D.L.; Marra, K.G. Delivery of Chondroitinase ABC and Glial Cell Line-Derived Neurotrophic Factor from Silk Fibroin Conduits Enhances Peripheral Nerve Regeneration. J. Tissue Eng. Regen. Med. 2017, 11, 733–742. [Google Scholar] [CrossRef]
- Kitamura, K.; Nagoshi, N.; Tsuji, O.; Matsumoto, M.; Okano, H.; Nakamura, M. Application of Hepatocyte Growth Factor for Acute Spinal Cord Injury: The Road from Basic Studies to Human Treatment. Int. J. Mol. Sci. 2019, 20, 1054. [Google Scholar] [CrossRef] [Green Version]
- Agrelo, I.S.; Schira-Heinen, J.; Beyer, F.; Groh, J.; Bütermann, C.; Estrada, V.; Poschmann, G.; Bribian, A.; Jadasz, J.J.; Lopez-Mascaraque, L.; et al. Secretome Analysis of Mesenchymal Stem Cell Factors Fostering Oligodendroglial Differentiation of Neural Stem Cells In Vivo. Int. J. Mol. Sci. 2020, 21, 4350. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, S.; Liu, C.; Han, X.; Gu, X.; Zhou, S. Deciphering Glial Scar after Spinal Cord Injury. Burn. Trauma 2021, 9, tkab035. [Google Scholar] [CrossRef]
- Kim, M.; Kim, K.H.; Song, S.U.; Yi, T.G.; Yoon, S.H.; Park, S.R.; Choi, B.H. Transplantation of Human Bone Marrow-Derived Clonal Mesenchymal Stem Cells Reduces Fibrotic Scar Formation in a Rat Spinal Cord Injury Model. J. Tissue Eng. Regen. Med. 2018, 12, e1034–e1045. [Google Scholar] [CrossRef]
- Huang, F.; Gao, T.; Wang, W.; Wang, L.; Xie, Y.; Tai, C.; Liu, S.; Cui, Y.; Wang, B. Engineered Basic Fibroblast Growth Factor-Overexpressing Human Umbilical Cord-Derived Mesenchymal Stem Cells Improve the Proliferation and Neuronal Differentiation of Endogenous Neural Stem Cells and Functional Recovery of Spinal Cord Injury by Activating the PI3K-Akt-GSK-3β Signaling Pathway. Stem Cell Res. Ther. 2021, 12, 468. [Google Scholar] [CrossRef]
- Pang, Q.M.; Chen, S.Y.; Xu, Q.J.; Fu, S.P.; Yang, Y.C.; Zou, W.H.; Zhang, M.; Liu, J.; Wan, W.H.; Peng, J.C.; et al. Neuroinflammation and Scarring After Spinal Cord Injury: Therapeutic Roles of MSCs on Inflammation and Glial Scar. Front. Immunol. 2021, 12, 751021. [Google Scholar] [CrossRef]
- Lv, C.; Zhang, T.; Li, K.; Gao, K. Bone Marrow Mesenchymal Stem Cells Improve Spinal Function of Spinal Cord Injury in Rats via TGF-Beta/Smads Signaling Pathway. Exp. Ther. Med. 2020, 19, 3657–3663. [Google Scholar] [CrossRef] [Green Version]
- Kim, C.; Kim, H.J.; Lee, H.; Lee, H.; Lee, S.J.; Lee, S.T.; Yang, S.-R.; Chung, C.K. Mesenchymal Stem Cell Transplantation Promotes Functional Recovery through MMP2/STAT3 Related Astrogliosis after Spinal Cord Injury. Int. J. Stem Cells 2019, 12, 331–339. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Cao, T.T.; Tian, Z.M.; Gao, H.; Wen, H.Q.; Pang, M.; He, W.J.; Wang, N.X.; Chen, Y.Y.; Wang, Y.; et al. Subarachnoid Transplantation of Human Umbilical Cord Mesenchymal Stem Cell in Rodent Model with Subacute Incomplete Spinal Cord Injury: Preclinical Safety and Efficacy Study. Exp. Cell Res. 2020, 395, 112184. [Google Scholar] [CrossRef]
- Fu, Q.; Liu, Y.; Liu, X.; Zhang, Q.; Chen, L.; Peng, J.; Ao, J.; Li, Y.; Wang, S.; Song, G.; et al. Engrafted Peripheral Blood-Derived Mesenchymal Stem Cells Promote Locomotive Recovery in Adult Rats after Spinal Cord Injury. Am. J. Transl. Res. 2017, 9, 3950. [Google Scholar]
- Cao, Y.; Xu, Y.; Chen, C.; Xie, H.; Lu, H.; Hu, J. Local Delivery of USC-Derived Exosomes Harboring ANGPTL3 Enhances Spinal Cord Functional Recovery after Injury by Promoting Angiogenesis. Stem Cell Res. Ther. 2021, 12, 20. [Google Scholar] [CrossRef]
- Zhong, D.; Cao, Y.; Li, C.J.; Li, M.; Rong, Z.J.; Jiang, L.; Guo, Z.; Lu, H.B.; Hu, J.Z. Highlight Article: Neural Stem Cell-Derived Exosomes Facilitate Cord Functional Recovery after Injury by Promoting. Exp. Biol. Med. 2020, 245, 54. [Google Scholar] [CrossRef]
- Al Mamun, A.; Monalisa, I.; Tul Kubra, K.; Akter, A.; Akter, J.; Sarker, T.; Munir, F.; Wu, Y.; Jia, C.; Afrin Taniya, M.; et al. Advances in Immunotherapy for the Treatment of Spinal Cord Injury. Immunobiology 2021, 226, 152033. [Google Scholar] [CrossRef]
- Urdzíková, L.M.; Růžička, J.; LaBagnara, M.; Kárová, K.; Kubinová, Š.; Jiráková, K.; Murali, R.; Syková, E.; Jhanwar-Uniyal, M.; Jendelová, P. Human Mesenchymal Stem Cells Modulate Inflammatory Cytokines after Spinal Cord Injury in Rat. Int. J. Mol. Sci. 2014, 15, 11275–11293. [Google Scholar] [CrossRef] [Green Version]
- Hakim, R.; Covacu, R.; Zachariadis, V.; Frostell, A.; Sankavaram, S.R.; Brundin, L.; Svensson, M. Mesenchymal Stem Cells Transplanted into Spinal Cord Injury Adopt Immune Cell-like Characteristics. Stem Cell Res. Ther. 2019, 10, 115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glennie, S.; Soeiro, I.; Dyson, P.J.; Lam, E.W.F.; Dazzi, F. Bone Marrow Mesenchymal Stem Cells Induce Division Arrest Anergy of Activated T Cells. Blood 2005, 105, 2821–2827. [Google Scholar] [CrossRef] [PubMed]
- Volarevic, V.; Gazdic, M.; Simovic Markovic, B.; Jovicic, N.; Djonov, V.; Arsenijevic, N. Mesenchymal Stem Cell-Derived Factors: Immuno-Modulatory Effects and Therapeutic Potential. Biofactors 2017, 43, 633–644. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, Q.; Wang, Z.; Tong, H.; Ma, L.; Zhang, Y.; Shan, F.; Meng, Y.; Yuan, Z. Comparative Analysis of Human Mesenchymal Stem Cells from Fetal-Bone Marrow, Adipose Tissue, and Warton’s Jelly as Sources of Cell Immunomodulatory Therapy. Hum. Vaccin. Immunother. 2016, 12, 85. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Pei, S.; Han, L.; Guo, B.; Li, Y.; Duan, R.; Yao, Y.; Xue, B.; Chen, X.; Jia, Y. Mesenchymal Stem Cell-Derived Exosomes Reduce A1 Astrocytes via Downregulation of Phosphorylated NFκB P65 Subunit in Spinal Cord Injury. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2018, 50, 1535–1559. [Google Scholar] [CrossRef] [PubMed]
- An, N.; Yang, J.; Wang, H.; Sun, S.; Wu, H.; Li, L.; Li, M. Mechanism of Mesenchymal Stem Cells in Spinal Cord Injury Repair through Macrophage Polarization. Cell Biosci. 2021, 11, 41. [Google Scholar] [CrossRef]
- Wu, L.-L.; Pan, X.-M.; Chen, H.-H.; Fu, X.-Y.; Jiang, J.; Ding, M.-X. Repairing and Analgesic Effects of Umbilical Cord Mesenchymal Stem Cell Transplantation in Mice with Spinal Cord Injury. Biomed Res. Int. 2020, 2020, 7650354. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Chang, M.; Zhang, R.; Wo, J.; Wu, B.; Zhang, H.; Zhou, Z.; Li, Z.; Zhang, F.; Zhong, C.; et al. Spinal Cord Injury Target-Immunotherapy with TNF-α Autoregulated and Feedback-Controlled Human Umbilical Cord Mesenchymal Stem Cell Derived Exosomes Remodelled by CRISPR/Cas9 Plasmid. Biomater. Adv. 2022, 133, 112624. [Google Scholar] [CrossRef]
- Litak, J.; Szymoniuk, M.; Czyżewski, W.; Hoffman, Z.; Litak, J.; Sakwa, L.; Kamieniak, P. Metallic Implants Used in Lumbar Interbody Fusion. Materials 2022, 15, 3650. [Google Scholar] [CrossRef]
- Litak, J.; Czyzewski, W.; Szymoniuk, M.; Pastuszak, B.; Litak, J.; Litak, G.; Grochowski, C.; Rahnama-Hezavah, M.; Kamieniak, P. Hydroxyapatite Use in Spine Surgery—Molecular and Clinical Aspect. Materials 2022, 15, 2906. [Google Scholar] [CrossRef]
- Chung, H.; Park, S. Ghrelin Regulates Cell Cycle-Related Gene Expression in Cultured Hippocampal Neural Stem Cells. J. Endocrinol. 2016, 230, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Glass, J.D.; Hertzberg, V.S.; Boulis, N.M.; Riley, J.; Federici, T.; Polak, M.; Bordeau, J.; Fournier, C.; Johe, K.; Hazel, T.; et al. Transplantation of Spinal Cord–Derived Neural Stem Cells for ALS. Neurology 2016, 87, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Todd, K.L.; Baker, K.L.; Eastman, M.B.; Kolling, F.W.; Trausch, A.G.; Nelson, C.E.; Conover, J.C. EphA4 Regulates Neuroblast and Astrocyte Organization in a Neurogenic Niche. J. Neurosci. 2017, 37, 3331–3341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mardones, M.D.; Andaur, G.A.; Varas-Godoy, M.; Henriquez, J.F.; Salech, F.; Behrens, M.I.; Couve, A.; Inestrosa, N.C.; Varela-Nallar, L. Frizzled-1 Receptor Regulates Adult Hippocampal Neurogenesis. Mol. Brain 2016, 9, 29. [Google Scholar] [CrossRef] [Green Version]
- Meneghini, V.; Frati, G.; Sala, D.; De Cicco, S.; Luciani, M.; Cavazzin, C.; Paulis, M.; Mentzen, W.; Morena, F.; Giannelli, S.; et al. Generation of Human Induced Pluripotent Stem Cell-Derived Bona Fide Neural Stem Cells for Ex Vivo Gene Therapy of Metachromatic Leukodystrophy. Stem Cells Transl. Med. 2017, 6, 352–368. [Google Scholar] [CrossRef]
- Morell, M.; Tsan, Y.; O’Shea, K.S. Inducible Expression of Noggin Selectively Expands Neural Progenitors in the Adult SVZ. Stem Cell Res. 2015, 14, 79–94. [Google Scholar] [CrossRef]
- Wang, J.; Fu, X.; Zhang, D.; Yu, L.; Li, N.; Lu, Z.; Gao, Y.; Wang, M.; Liu, X.; Zhou, C.; et al. ChAT-Positive Neurons Participate in Subventricular Zone Neurogenesis after Middle Cerebral Artery Occlusion in Mice. Behav. Brain Res. 2017, 316, 145–151. [Google Scholar] [CrossRef] [Green Version]
- Yu, X.; Li, Z.; Zheng, H.; Ho, J.; Chan, M.T.V.; Wu, W.K.K. Protective Roles of Melatonin in Central Nervous System Diseases by Regulation of Neural Stem Cells. Cell Prolif. 2017, 50, e12323. [Google Scholar] [CrossRef] [Green Version]
- Zhang, M.; Lin, Y.H.; Sun, Y.J.; Zhu, S.; Zheng, J.; Liu, K.; Cao, N.; Li, K.; Huang, Y.; Ding, S. Pharmacological Reprogramming of Fibroblasts into Neural Stem Cells by Signaling-Directed Transcriptional Activation. Cell Stem Cell 2016, 18, 653–667. [Google Scholar] [CrossRef] [Green Version]
- Aggarwal, R.; Lu, J.; Pompili, V.J.; Das, H. Hematopoietic Stem Cells: Transcriptional Regulation, Ex Vivo Expansion and Clinical Application. Curr. Mol. Med. 2012, 12, 34–49. [Google Scholar] [CrossRef] [Green Version]
- Frolov, A.A.; Bryukhovetskiy, A.S. Effects of Hematopoietic Autologous Stem Cell Transplantation to the Chronically Injured Human Spinal Cord Evaluated by Motor and Somatosensory Evoked Potentials Methods. Cell Transplant. 2012, 21, 49–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moghaddam, S.A.; Yousefi, B.; Sanooghi, D.; Faghihi, F.; Hayati Roodbari, N.; Bana, N.; Joghataei, M.T.; Pooyan, P.; Arjmand, B. Differentiation Potential of Human CD133 Positive Hematopoietic Stem Cells into Motor Neuron- like Cells, in Vitro. J. Chem. Neuroanat. 2017, 86, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Xiong, L.L.; Liu, F.; Deng, S.K.; Liu, J.; Dan, Q.Q.; Zhang, P.; Zou, Y.; Xia, Q.J.; Wang, T.H. Transplantation of Hematopoietic Stem Cells Promotes Functional Improvement Associated with NT-3-MEK-1 Activation in Spinal Cord-Transected Rats. Front. Cell. Neurosci. 2017, 11, 213. [Google Scholar] [CrossRef] [Green Version]
- Takakura, N.; Watanabe, T.; Suenobu, S.; Yamada, Y.; Noda, T.; Ito, Y.; Satake, M.; Suda, T. A Role for Hematopoietic Stem Cells in Promoting Angiogenesis. Cell 2000, 102, 199–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Kelamangalath, L.; Kim, H.; Han, S.B.; Tang, X.; Zhai, J.; Hong, J.W.; Lin, S.; Son, Y.J.; Smith, G.M. NT-3 Promotes Proprioceptive Axon Regeneration When Combined with Activation of the MTor Intrinsic Growth Pathway but Not with Reduction of Myelin Extrinsic Inhibitors. Exp. Neurol. 2016, 283, 73. [Google Scholar] [CrossRef] [Green Version]
- Keefe, K.M.; Sheikh, I.S.; Smith, G.M. Targeting Neurotrophins to Specific Populations of Neurons: NGF, BDNF, and NT-3 and Their Relevance for Treatment of Spinal Cord Injury. Int. J. Mol. Sci. 2017, 18, 548. [Google Scholar] [CrossRef] [Green Version]
- Ataei, M.L.; Karimipour, M.; Shahabi, P.; Pashaei-Asl, R.; Ebrahimie, E.; Pashaiasl, M. The Restorative Effect of Human Amniotic Fluid Stem Cells on Spinal Cord Injury. Cells 2021, 10, 2565. [Google Scholar] [CrossRef]
- Satti, H.S.; Waheed, A.; Ahmed, P.; Ahmed, K.; Akram, Z.; Aziz, T.; Satti, T.M.; Shahbaz, N.; Khan, M.A.; Malik, S.A. Autologous Mesenchymal Stromal Cell Transplantation for Spinal Cord Injury: A Phase I Pilot Study. Cytotherapy 2016, 18, 518–522. [Google Scholar] [CrossRef]
- Vaquero, J.; Zurita, M.; Rico, M.A.; Aguayo, C.; Fernández, C.; Gutiérrez, R.; Rodríguez-Boto, G.; Saab, A.; Hassan, R.; Ortega, C. Intrathecal Administration of Autologous Bone Marrow Stromal Cells Improves Neuropathic Pain in Patients with Spinal Cord Injury. Neurosci. Lett. 2018, 670, 14–18. [Google Scholar] [CrossRef]
- Chen, X.; Xue, B.; Li, Y.; Song, C.; Jia, P.; Ren, X.; Zang, W.; Wang, J. Meta-Analysis of Stem Cell Transplantation for Reflex Hypersensitivity after Spinal Cord Injury. Neuroscience 2017, 363, 66–75. [Google Scholar] [CrossRef] [Green Version]
- Kazim, S.F.; Bowers, C.A.; Cole, C.D.; Varela, S.; Karimov, Z.; Martinez, E.; Ogulnick, J.V.; Schmidt, M.H. Corticospinal Motor Circuit Plasticity After Spinal Cord Injury: Harnessing Neuroplasticity to Improve Functional Outcomes. Mol. Neurobiol. 2021, 58, 5494–5516. [Google Scholar] [CrossRef] [PubMed]
- Zamani, H.; Soufizomorrod, M.; Oraee-Yazdani, S.; Naviafar, D.; Akhlaghpasand, M.; Seddighi, A.; Soleimani, M. Safety and Feasibility of Autologous Olfactory Ensheathing Cell and Bone Marrow Mesenchymal Stem Cell Co-Transplantation in Chronic Human Spinal Cord Injury: A Clinical Trial. Spinal Cord 2022, 60, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Oraee-Yazdani, S.; Akhlaghpasand, M.; Golmohammadi, M.; Hafizi, M.; Zomorrod, M.S.; Kabir, N.M.; Oraee-Yazdani, M.; Ashrafi, F.; Zali, A.; Soleimani, M. Combining Cell Therapy with Human Autologous Schwann Cell and Bone Marrow-Derived Mesenchymal Stem Cell in Patients with Subacute Complete Spinal Cord Injury: Safety Considerations and Possible Outcomes. Stem Cell Res. Ther. 2021, 12, 445. [Google Scholar] [CrossRef] [PubMed]
- Deng, W.S.; Ma, K.; Liang, B.; Liu, X.Y.; Xu, H.Y.; Zhang, J.; Shi, H.Y.; Sun, H.T.; Chen, X.Y.; Zhang, S. Collagen Scaffold Combined with Human Umbilical Cord-Mesenchymal Stem Cells Transplantation for Acute Complete Spinal Cord Injury. Neural Regen. Res. 2020, 15, 1686–1700. [Google Scholar] [CrossRef]
- Sharma, A.; Sane, H.; Gokulchandran, N.; Kulkarni, P.; Jose, A.; Nair, V.; Das, R.; Lakhanpal, V.; Badhe, P. Intrathecal Transplantation of Autologous Bone Marrow Mononuclear Cells in Patients with Sub-Acute and Chronic Spinal Cord Injury: An Open-Label Study. Int. J. Health Sci. 2020, 14, 24–32. [Google Scholar]
- Levi, A.D.; Okonkwo, D.O.; Park, P.; Jenkins, A.L.; Kurpad, S.N.; Parr, A.M.; Ganju, A.; Aarabi, B.; Kim, D.; Casha, S.; et al. Emerging Safety of Intramedullary Transplantation of Human Neural Stem Cells in Chronic Cervical and Thoracic Spinal Cord Injury. Neurosurgery 2018, 82, 562–575. [Google Scholar] [CrossRef]
- Curtis, E.; Martin, J.R.; Gabel, B.; Sidhu, N.; Rzesiewicz, T.K.; Mandeville, R.; Van Gorp, S.; Leerink, M.; Tadokoro, T.; Marsala, S.; et al. A First-in-Human, Phase I Study of Neural Stem Cell Transplantation for Chronic Spinal Cord Injury. Cell Stem Cell 2018, 22, 941–950.e6. [Google Scholar] [CrossRef] [Green Version]
- Xiao, Z.; Tang, F.; Zhao, Y.; Han, G.; Yin, N.; Li, X.; Chen, B.; Han, S.; Jiang, X.; Yun, C.; et al. Significant Improvement of Acute Complete Spinal Cord Injury Patients Diagnosed by a Combined Criteria Implanted with NeuroRegen Scaffolds and Mesenchymal Stem Cells. Cell Transplant. 2018, 27, 907–915. [Google Scholar] [CrossRef] [Green Version]
- Vaquero, J.; Zurita, M.; Rico, M.A.; Bonilla, C.; Aguayo, C.; Fernández, C.; Tapiador, N.; Sevilla, M.; Morejón, C.; Montilla, J.; et al. Repeated Subarachnoid Administrations of Autologous Mesenchymal Stromal Cells Supported in Autologous Plasma Improve Quality of Life in Patients Suffering Incomplete Spinal Cord Injury. Cytotherapy 2017, 19, 349–359. [Google Scholar] [CrossRef] [Green Version]
- Ammar, A.S.; Osman, Y.; Hendam, A.T.; Hasen, M.A.; Al Rubaish, F.A.; Al Nujaidi, D.Y.; Al Abbas, F.M. A Method for Reconstruction of Severely Damaged Spinal Cord Using Autologous Hematopoietic Stem Cells and Platelet-Rich Protein as a Biological Scaffold. Asian J. Neurosurg. 2017, 12, 681. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, H.; Wang, H.; Huang, J.; Yang, Y.; Li, G.; Yu, K.; Yang, L. A Comparative Study of Different Stem Cell Transplantation for Spinal Cord Injury: A Systematic Review and Network Meta-Analysis. World Neurosurg. 2022, 159, e232–e243. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Liu, W.; Bai, Y.; Zhou, Y.; Zhang, Y.; Wang, C.; Lin, S.; He, H. Transplantation of Mesenchymal Stem Cells for Spinal Cord Injury: A Systematic Review and Network Meta-Analysis. J. Transl. Med. 2021, 19, 178. [Google Scholar] [CrossRef] [PubMed]
- Tang, Q.R.; Xue, H.; Zhang, Q.; Guo, Y.; Xu, H.; Liu, Y.; Liu, J.M. Evaluation of the Clinical Efficacy of Stem Cell Transplantation in the Treatment of Spinal Cord Injury: A Systematic Review and Meta-Analysis. Cell Transplant. 2021, 30. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.; Yang, X. The Efficacy and Safety of Mesenchymal Stem Cell Transplantation for Spinal Cord Injury Patients: A Meta-Analysis and Systematic Review. Cell Transplant. 2019, 28, 36–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fan, X.; Wang, J.Z.; Lin, X.M.; Zhang, L. Stem Cell Transplantation for Spinal Cord Injury: A Meta-Analysis of Treatment Effectiveness and Safety. Neural Regen. Res. 2017, 12, 815–825. [Google Scholar] [CrossRef]
- Maqueda, A.; Rodriguez, F.J. Efficacy of Human HC016 Cell Transplants on Neuroprotection and Functional Recovery in a Rat Model of Acute Spinal Cord Injury. J. Tissue Eng. Regen. Med. 2020, 14, 319–333. [Google Scholar] [CrossRef] [PubMed]
- Dasari, V.R.; Spomar, D.G.; Li, L.; Gujrati, M.; Rao, J.S.; Dinh, D.H. Umbilical Cord Blood Stem Cell Mediated Downregulation of Fas Improves Functional Recovery of Rats after Spinal Cord Injury. Neurochem. Res. 2008, 33, 134–149. [Google Scholar] [CrossRef] [Green Version]
- Cabanes, C.; Bonilla, S.; Tabares, L.; Martínez, S. Neuroprotective Effect of Adult Hematopoietic Stem Cells in a Mouse Model of Motoneuron Degeneration. Neurobiol. Dis. 2007, 26, 408–418. [Google Scholar] [CrossRef]
- Bryukhovetskiy, A.S. Effectiveness of Repeated Transplantations of Hematopoietic Stem Cells in Spinal Cord Injury. World J. Transplant. 2015, 5, 110. [Google Scholar] [CrossRef]
- Thakkar, U.; Vanikar, A.; Trivedi, H.; Shah, V.; Dave, S.; Dixit, S.; Tiwari, B.; Shah, H. Infusion of Autologous Adipose Tissue Derived Neuronal Differentiated Mesenchymal Stem Cells and Hematopoietic Stem Cells in Post-Traumatic Paraplegia Offers a Viable Therapeutic Approach. Adv. Biomed. Res. 2016, 5, 51. [Google Scholar] [CrossRef]
- Zakerinia, M.; Kamgarpour, A.; Nemati, H.; Zare, H.R.; Ghasemfar, M.; Rezvani, A.R.; Karimi, M.; Nourani Khojasteh, H.; Dehghani, M.; Vojdani, R.; et al. Intrathecal Autologous Bone Marrow-Derived Hematopoietic Stem Cell Therapy in Neurological Diseases. Int. J. Organ Transplant. Med. 2018, 9, 157–167. [Google Scholar] [PubMed]
- Dryla, A.; Szymoniuk, M.; Rogatko, K.; Piecewicz-Szczęsna, H. Alveolar Osteitis: The Current State of Knowledge. J. Educ. Health Sport 2022, 12, 204–216. [Google Scholar] [CrossRef]
- Sharara, F.I.; Lelea, L.L.; Rahman, S.; Klebanoff, J.S.; Moawad, G.N. A Narrative Review of Platelet-Rich Plasma (PRP) in Reproductive Medicine. J. Assist. Reprod. Genet. 2021, 38, 1003. [Google Scholar] [CrossRef]
- Hajipour, H.; Farzadi, L.; Latifi, Z.; Keyhanvar, N.; Navali, N.; Fattahi, A.; Nouri, M.; Dittrich, R. An Update on Platelet-Rich Plasma (PRP) Therapy in Endometrium and Ovary Related Infertilities: Clinical and Molecular Aspects. Syst. Biol. Reprod. Med. 2021, 67, 177–188. [Google Scholar] [CrossRef]
- Garcia-Ayuso, D.; Di Pierdomenico, J.; García-Bernal, D.; Vidal-Sanz, M.; Villegas-Pérez, M.P. Bone Marrow-Derived Mononuclear Stem Cells in the Treatment of Retinal Degenerations. Neural Regen. Res. 2022, 17, 1937. [Google Scholar] [CrossRef]
- dos Ramalho, B.S.; de Almeida, F.M.; Martinez, A.M.B. Cell Therapy and Delivery Strategies for Spinal Cord Injury. Histol. Histopathol. 2021, 36, 907–920. [Google Scholar] [CrossRef]
- Veneruso, V.; Rossi, F.; Villella, A.; Bena, A.; Forloni, G.; Veglianese, P. Stem Cell Paracrine Effect and Delivery Strategies for Spinal Cord Injury Regeneration. J. Control. Release 2019, 300, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Mukhamedshina, Y.O.; Gracheva, O.A.; Mukhutdinova, D.M.; Chelyshev, Y.A.; Rizvanov, A.A. Mesenchymal Stem Cells and the Neuronal Microenvironment in the Area of Spinal Cord Injury. Neural Regen. Res. 2019, 14, 227–237. [Google Scholar] [CrossRef]
- Zhu, H.; Poon, W.; Liu, Y.; Leung, G.K.-K.; Wong, Y.; Feng, Y.; Ng, S.C.P.; Tsang, K.S.; Sun, D.T.F.; Yeung, D.K.; et al. Phase I-II Clinical Trial Assessing Safety and Efficacy of Umbilical Cord Blood Mononuclear Cell Transplant Therapy of Chronic Complete Spinal Cord Injury. CELL Transplant. 2016, 25, 1925–1943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krupa, P.; Vackova, I.; Ruzicka, J.; Zaviskova, K.; Dubisova, J.; Koci, Z.; Turnovcova, K.; Urdzikova, L.M.; Kubinova, S.; Rehak, S.; et al. The Effect of Human Mesenchymal Stem Cells Derived from Wharton’s Jelly in Spinal Cord Injury Treatment Is Dose-Dependent and Can Be Facilitated by Repeated Application. Int. J. Mol. Sci. 2018, 19, 1503. [Google Scholar] [CrossRef] [Green Version]
- Bansal, H.; Verma, P.; Agrawal, A.; Leon, J.; Sundell, I.B.; Koka, P.S. Autologous Bone Marrow-Derived Stem Cells in Spinal Cord Injury. J. Stem Cells 2016, 11, 51–61. [Google Scholar] [PubMed]
- Li, J.; Chen, L.; Chen, Q.; Hu, D.; Lin, J. Effect of Granulocyte Colony-Stimulating Factor Mobilizing Bone Marrow Mesenchymal Stell Cells Homing to Injury Sites in Spinal Cord Injury of Rats. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2019, 33, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Kabat, M.; Bobkov, I.; Kumar, S.; Grumet, M. Trends in Mesenchymal Stem Cell Clinical Trials 2004-2018: Is Efficacy Optimal in a Narrow Dose Range? Stem Cells Transl. Med. 2020, 9, 17–27. [Google Scholar] [CrossRef]
- Ferrini, E.; Stellari, F.F.; Franceschi, V.; Macchi, F.; Russo, L.; Murgia, A.; Grisendi, G.; Villetti, G.; Dominici, M.; Donofrio, G. Persistency of Mesenchymal Stromal/Stem Cells in Lungs. Front. Cell Dev. Biol. 2021, 9, 1825. [Google Scholar] [CrossRef] [PubMed]
- Moll, G.; Ankrum, J.A.; Kamhieh-Milz, J.; Bieback, K.; Ringdén, O.; Volk, H.D.; Geissler, S.; Reinke, P. Intravascular Mesenchymal Stromal/Stem Cell Therapy Product Diversification: Time for New Clinical Guidelines. Trends Mol. Med. 2019, 25, 149–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramalho, B.D.S.; De Almeida, F.M.; Sales, C.M.; De Lima, S.; Martinez, A.M.B. Injection of Bone Marrow Mesenchymal Stem Cells by Intravenous or Intraperitoneal Routes Is a Viable Alternative to Spinal Cord Injury Treatment in Mice. Neural Regen. Res. 2018, 13, 1046–1053. [Google Scholar] [CrossRef]
- Oh, S.K.; Jeon, S.R. Current Concept of Stem Cell Therapy for Spinal Cord Injury: A Review. Korean J. Neurotrauma 2016, 12, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boido, M.; Ghibaudi, M.; Gentile, P.; Favaro, E.; Fusaro, R.; Tonda-Turo, C. Chitosan-Based Hydrogel to Support the Paracrine Activity of Mesenchymal Stem Cells in Spinal Cord Injury Treatment. Sci. Rep. 2019, 9, 6402. [Google Scholar] [CrossRef] [Green Version]
- Liu, W.; Wang, Y.; Gong, F.; Rong, Y.; Luo, Y.; Tang, P.; Zhou, Z.; Zhou, Z.; Xu, T.; Jiang, T.; et al. Exosomes Derived from Bone Mesenchymal Stem Cells Repair Traumatic Spinal Cord Injury by Suppressing the Activation of A1 Neurotoxic Reactive Astrocytes. J. Neurotrauma 2019, 36, 469–484. [Google Scholar] [CrossRef]
- Okuda, A.; Horii-Hayashi, N.; Sasagawa, T.; Shimizu, T.; Shigematsu, H.; Iwata, E.; Morimoto, Y.; Masuda, K.; Koizumi, M.; Akahane, M.; et al. Bone Marrow Stromal Cell Sheets May Promote Axonal Regeneration and Functional Recovery with Suppression of Glial Scar Formation after Spinal Cord Transection Injury in Rats. J. Neurosurg. Spine 2017, 26, 388–395. [Google Scholar] [CrossRef]
- Cheng, I.; Park, D.Y.; Mayle, R.E.; Githens, M.; Smith, R.L.; Park, H.Y.; Hu, S.S.; Alamin, T.F.; Wood, K.B.; Kharazi, A.I. Does Timing of Transplantation of Neural Stem Cells Following Spinal Cord Injury Affect Outcomes in an Animal Model? J. Spine Surg. 2017, 3, 567. [Google Scholar] [CrossRef] [PubMed]
- Shang, Z.; Li, D.; Chen, J.; Wang, R.R.; Wang, M.; Zhang, B.; Wang, X.; Wanyan, P. What Is the Optimal Timing of Transplantation of Neural Stem Cells in Spinal Cord Injury? A Systematic Review and Network Meta-Analysis Based on Animal Studies. Front. Immunol. 2022, 13, 855309. [Google Scholar] [CrossRef] [PubMed]
- de Araújo, L.T.; Macêdo, C.T.; Damasceno, P.K.F.; Das Neves, Í.G.C.; de Lima, C.S.; Santos, G.C.; de Santana, T.A.; Sampaio, G.L.d.A.; Silva, D.N.; Villarreal, C.F.; et al. Clinical Trials Using Mesenchymal Stem Cells for Spinal Cord Injury: Challenges in Generating Evidence. Cells 2022, 11, 1019. [Google Scholar] [CrossRef] [PubMed]
- Vaquero, J.; Zurita, M.; Rico, M.A.; Bonilla, C.; Aguayo, C.; Montilla, J.; Bustamante, S.; Carballido, J.; Marin, E.; Martinez, F.; et al. An Approach to Personalized Cell Therapy in Chronic Complete Paraplegia: The Puerta de Hierro Phase I/II Clinical Trial. Cytotherapy 2016, 18, 1025–1036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, W.; Ma, Z.; Li, J.; Kang, X. Mesenchymal Stem Cell-Derived Exosomes: Therapeutic Opportunities and Challenges for Spinal Cord Injury. Stem Cell Res. Ther. 2021, 12, 102. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Wu, J.-H.; Zhu, J.-H.; Yang, H. Exosomes Secreted by Hypoxia-Pre-Conditioned Adipose-Derived Mesenchymal Stem Cells Reduce Neuronal Apoptosis in Rats with Spinal Cord Injury. J. Neurotrauma 2022, 39, 701–714. [Google Scholar] [CrossRef]
- Koprivec, S.; Novak, M.; Bernik, S.; Voga, M.; Mohorič, L.; Majdič, G. Treatment of Cranial Cruciate Ligament Injuries in Dogs Using a Combination of Tibial Tuberosity Advancement Procedure and Autologous Mesenchymal Stem Cells/Multipotent Mesenchymal Stromal Cells—A Pilot Study. Acta Vet. Hung. 2021, 68, 405–412. [Google Scholar] [CrossRef]
- Chen, Y.; Tian, Z.; He, L.; Liu, C.; Wang, N.; Rong, L.; Liu, B. Exosomes Derived from MiR-26a-Modified MSCs Promote Axonal Regeneration via the PTEN/AKT/MTOR Pathway Following Spinal Cord Injury. Stem Cell Res. Ther. 2021, 12, 224. [Google Scholar] [CrossRef]
- Herbert, F.J.; Bharathi, D.; Suresh, S.; David, E.; Kumar, S. Regenerative Potential of Stem Cell-Derived Extracellular Vesicles in Spinal Cord Injury (SCI). Curr. Stem Cell Res. Ther. 2022, 17, 280–293. [Google Scholar] [CrossRef]
- Yousefifard, M.; Sarveazad, A.; Babahajian, A.; Rafiei Alavi, S.N.; Madani Neishaboori, A.; Vaccaro, A.R.; Hosseini, M.; Rahimi-Movaghar, V. Growth Factor Gene-Modified Cells in Spinal Cord Injury Recovery: A Systematic Review. World Neurosurg. 2022, 162, 150–162.e1. [Google Scholar] [CrossRef]
- Lu, D.; Yang, Y.; Zhang, P.; Ma, Z.; Li, W.; Song, Y.; Feng, H.; Yu, W.; Ren, F.; Li, T.; et al. Development and Application of Three-Dimensional Bioprinting Scaffold in the Repair of Spinal Cord Injury. Tissue Eng. Regen. Med. 2022, 19, 1113–1127. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Wen, L.L.; Li, Y.F.; Wu, K.M.; Duan, R.R.; Yao, Y.B.; Jing, L.J.; Gong, Z.; Teng, J.F.; Jia, Y.J. Exosomes Derived from Bone Marrow Mesenchymal Stem Cells Protect the Injured Spinal Cord by Inhibiting Pericyte Pyroptosis. Neural Regen. Res. 2022, 17, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Tian, F.; Yang, J.; Xia, R. Exosomes Secreted from CircZFHX3-Modified Mesenchymal Stem Cells Repaired Spinal Cord Injury Through Mir-16-5p/IGF-1 in Mice. Neurochem. Res. 2022, 47, 2076–2089. [Google Scholar] [CrossRef] [PubMed]
- Shao, C.; Chen, Y.; Yang, T.; Zhao, H.; Li, D. Mesenchymal Stem Cell Derived Exosomes Suppress Neuronal Cell Ferroptosis Via IncGm36569/MiR-5627-5p/FSP1 Axis in Acute Spinal Cord Injury. Stem Cell Rev. Rep. 2022, 18, 1127–1142. [Google Scholar] [CrossRef]
- Kang, J.; Guo, Y. Human Umbilical Cord Mesenchymal Stem Cells Derived Exosomes Promote Neurological Function Recovery in a Rat Spinal Cord Injury Model. Neurochem. Res. 2022, 47, 1532–1540. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Chen, Y.; Wang, Z.; Xu, C.; Qiao, S.; Liu, T.; Qi, K.; Tong, D.; Li, C. Bone Marrow Mesenchymal Stem Cell Exosome Attenuates Inflammasome-Related Pyroptosis via Delivering Circ_003564 to Improve the Recovery of Spinal Cord Injury. Mol. Neurobiol. 2022, 59, 6771–6789. [Google Scholar] [CrossRef]
- Zhang, C.; Deng, R.; Zhang, G.; He, X.; Chen, H.; Chen, B.; Wan, L.; Kang, X. Therapeutic Effect of Exosomes Derived from Stem Cells in Spinal Cord Injury: A Systematic Review Based on Animal Studies. Front. Neurol. 2022, 13, 847444. [Google Scholar] [CrossRef]
- Feng, Y.; Li, Y.; Shen, P.P.; Wang, B. Gene-Modified Stem Cells for Spinal Cord Injury: A Promising Better Alternative Therapy. Stem Cell Rev. Rep. 2022, 18, 2662–2682. [Google Scholar] [CrossRef]
- Zhang, B.; Wang, D.; Li, X.; Yang, S.; Yuan, H. NEP1-40-Overexpressing Neural Stem Cells Enhance Axon Regeneration by Inhibiting Nogo-A/NgR1 Signaling Pathway. Curr. Neurovasc. Res. 2021, 18, 271–278. [Google Scholar] [CrossRef]
- Zhang, D.; Sun, Y.; Liu, W. Motor Functional Recovery Efficacy of Scaffolds with Bone Marrow Stem Cells in Rat Spinal Cord Injury: A Bayesian Network Meta-Analysis. Spinal Cord 2022, 1–6. [Google Scholar] [CrossRef]
- Haggerty, A.E.; Maldonado-Lasuncion, I.; Nitobe, Y.; Yamane, K.; Marlow, M.M.; You, H.; Zhang, C.; Cho, B.; Li, X.; Reddy, S.; et al. The Effects of the Combination of Mesenchymal Stromal Cells and Nanofiber-Hydrogel Composite on Repair of the Contused Spinal Cord. Cells 2022, 11, 1137. [Google Scholar] [CrossRef] [PubMed]
- Czyżewski, W.; Jachimczyk, J.; Hoffman, Z.; Szymoniuk, M.; Litak, J.; Maciejewski, M.; Kura, K.; Rola, R.; Torres, K. Low-Cost Cranioplasty-A Systematic Review of 3D Printing in Medicine. Materials 2022, 15, 4731. [Google Scholar] [CrossRef] [PubMed]
- Rezmer, J.; Wasilewska, I.; Świątek, Ł. Use of 3d Printing Technology in the Treatment of Microtia and Other Outer Ear Deformities. J. Educ. Health Sport 2022, 12, 381–387. [Google Scholar] [CrossRef]
- Rezmer, J.; Wasilewska, I.; Świątek, Ł. The Use of 3d Printing Technology in the Development of a Prosthetic Thumb. J. Educ. Health Sport 2022, 12, 405–409. [Google Scholar] [CrossRef]
- Zarepour, A.; Hooshmand, S.; Gökmen, A.; Zarrabi, A.; Mostafavi, E. Spinal Cord Injury Management through the Combination of Stem Cells and Implantable 3D Bioprinted Platforms. Cells 2021, 10, 3189. [Google Scholar] [CrossRef]
- Chen, C.; Zhao, M.L.; Zhang, R.K.; Lu, G.; Zhao, C.Y.; Fu, F.; Sun, H.T.; Zhang, S.; Tu, Y.; Li, X.H. Collagen/Heparin Sulfate Scaffolds Fabricated by a 3D Bioprinter Improved Mechanical Properties and Neurological Function after Spinal Cord Injury in Rats. J. Biomed. Mater. Res. A 2017, 105, 1324–1332. [Google Scholar] [CrossRef]
- Sun, Y.; Yang, C.; Zhu, X.; Wang, J.J.; Liu, X.Y.; Yang, X.P.; An, X.W.; Liang, J.; Dong, H.J.; Jiang, W.; et al. 3D Printing Collagen/Chitosan Scaffold Ameliorated Axon Regeneration and Neurological Recovery after Spinal Cord Injury. J. Biomed. Mater. Res. Part A 2019, 107, 1898–1908. [Google Scholar] [CrossRef]
- Li, X.H.; Zhu, X.; Liu, X.Y.; Xu, H.H.; Jiang, W.; Wang, J.J.; Chen, F.; Zhang, S.; Li, R.X.; Chen, X.Y.; et al. The Corticospinal Tract Structure of Collagen/Silk Fibroin Scaffold Implants Using 3D Printing Promotes Functional Recovery after Complete Spinal Cord Transection in Rats. J. Mater. Sci. Mater. Med. 2021, 32, 31. [Google Scholar] [CrossRef]
- Koffler, J.; Zhu, W.; Qu, X.; Platoshyn, O.; Dulin, J.N.; Brock, J.; Graham, L.; Lu, P.; Sakamoto, J.; Marsala, M.; et al. Biomimetic 3D-Printed Scaffolds for Spinal Cord Injury Repair. Nat. Med. 2019, 25, 263–269. [Google Scholar] [CrossRef]
- Zarepour, A.; Bal Öztürk, A.; Koyuncu Irmak, D.; Yaşayan, G.; Gökmen, A.; Karaöz, E.; Zarepour, A.; Zarrabi, A.; Mostafavi, E. Combination Therapy Using Nanomaterials and Stem Cells to Treat Spinal Cord Injuries. Eur. J. Pharm. Biopharm. 2022, 177, 224–240. [Google Scholar] [CrossRef]
- Somuncu, D.; Gartenberg, A.; Cho, W. Investigational Therapies for Gunshot Wounds to the Spine: A Narrative Review. Clin. Spine Surg. 2022, 35, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Hachmann, J.T.; Yousak, A.; Wallner, J.J.; Gad, P.N.; Edgerton, V.R.; Gorgey, A.S. Epidural Spinal Cord Stimulation as an Intervention for Motor Recovery after Motor Complete Spinal Cord Injury. J. Neurophysiol. 2021, 126, 1843–1859. [Google Scholar] [CrossRef] [PubMed]
- Duan, R.; Qu, M.; Yuan, Y.; Lin, M.; Liu, T.; Huang, W.; Gao, J.; Zhang, M.; Yu, X. Clinical Benefit of Rehabilitation Training in Spinal Cord Injury: A Systematic Review and Meta-Analysis. Spine 2021, 46, E398–E410. [Google Scholar] [CrossRef] [PubMed]
- Hicks, A.L. Locomotor Training in People with Spinal Cord Injury: Is This Exercise? Spinal Cord 2021, 59, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Gaojian, T.; Dingfei, Q.; Linwei, L.; Xiaowei, W.; Zheng, Z.; Wei, L.; Tong, Z.; Benxiang, N.; Yanning, Q.; Wei, Z.; et al. Parthenolide Promotes the Repair of Spinal Cord Injury by Modulating M1/M2 Polarization via the NF-ΚB and STAT 1/3 Signaling Pathway. Cell Death Discov. 2020, 6, 97. [Google Scholar] [CrossRef]
- Fang, H.; Yang, M.; Pan, Q.; Jin, H.L.; Li, H.F.; Wang, R.R.; Wang, Q.Y.; Zhang, J.P. MicroRNA-22-3p Alleviates Spinal Cord Ischemia/Reperfusion Injury by Modulating M2 Macrophage Polarization via IRF5. J. Neurochem. 2021, 156, 106–120. [Google Scholar] [CrossRef]

| Type of Stem Cells | Differentiation Potential | Sourcing | Main Advantages | Limitations | Application in Spinal Cord Injury | Refs |
|---|---|---|---|---|---|---|
| Embryonal Stem Cells | totipotent, pluripotent | morula, blastocyst, umbilical cord, amniotic fluid, amnion, chorion, generated from adult somatic cells | possibility to generate any cell lines, e.g., neurons or oligodendrocytes | the risk of immune rejection, the ethical concern regarding the use of human embryos, the risk of tumorigenicity | Preclinical studies | [16,49,50,52,56,61] |
| Induced Pluripotent Stem Cells | pluripotent | generated from adult somatic cells using so-called OSKM transcription factors | lack of ethical issues and immune suppression (in autologous method) | the risk of immune rejections, instability of iPSCs’ genome, potential tumorigenicity | Preclinical studies | [52,64,65,66,92] |
| Mesenchymal Stem Cells | multipotent | bone marrow, umbilical cord blood, adipose tissue | capability to generate adipocytes, bone, and chondrocytes, easy extraction, rapid proliferation, low immunogenicity; ADMSCs and BMSCs can be generated without ethical issues | ADMSCs and BMSCs require liposuction or bone marrow aspirate followed by cultivation, which makes them time-consuming, and expensive sources; Umbilical cord or Wharton’s Jelly MSCs require conducting complex procedures namely lyophilization to avoid immunological responses and are controversial from the ethical point of view | Clinical studies | [14,27,53,68,69,70,73,74,76] |
| Hematopoietic Stem Cells | multipotent | placenta, cord blood, adult bone marrow | capability to differentiate into all cell types of the hematopoietic system, treatment for many diseases such as hematopoietic diseases, multiple sclerosis, Cron’s disease, and diabetes | the risk of immune rejection | Clinical studies | [53,61,84,85,86] |
| Neural Stem Cells | multipotent | ventricular system of the brain, central canal of the spinal cord, dentate gyrus of the hippocampus, differentiation from somatic cells, iPSCs | capability to differentiate into neurons, oligodentrocytes and astrocytes | the risk of immune rejection, low progress of the research due to ethical and financial problems | Clinical studies | [92] |
| Clinical Study | Type of Stem Cells | Study Design | Phase of Study | Country | Number of Patients | The Initial ASIA Grade | The Initial Phase of SCI | Route of Administration | Dose of Cells | Combined with | Follow-Up Duration | Clinical Outcomes | Adverse Effects |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Saini et al. 2022 [27] | BMSCs | randomized placebo controlled trial | II | India | 27 | A | acute | intramedullary | 2 × 108 | n/a | 3 years | improvement in 6 patients of stem cells group and 1 in placebo group in ASIA score | n/a |
| Zamani et al. 2022 [163] | BMSCs | non-randomized open-labeled controlled trial | I | Iran | 3 | A | chronic | subarachnoid | 3 × 107 | OECs | 2 years | 1 patient improved from A to B in AISA score | no significant adverse effects, mostly headache and neurophatic pain |
| Smirnov et al. 2022 [32] | UCBCs | non-randomized open-labeled controlled trial | I/II | Russian Federation | 10 | A (n = 6), B (n = 4) | acute | intravenous | 4 doses, 1.2 × 109 | n/a | 12 months | the mean increase in level of ASIA was 2.2 points; the 1-year LEMS parameter was >25 points in 6 patients | no significant adverse effects |
| Albu et al. 2021 [14] | WJ-MSCs | randomized placebo controlled trial | I/II | Spain | 10 | A | chronic | subarachnoid | 1 × 107 | n/a | 6 months | improvement sensation in the dermatomes below the level of injury in stem cells group; decrease neurogenic hyperactivity in bladder, decrease external sphincter dyssynergy, increase maximum capacity and compliance in bladder | no significant adverse effects |
| Yang et al. 2021 [28] | UCMSCs | prospective single-arm study | I/II | China | 41 | A, B, C, D | chronic | subarachnoid | 4 doses, 1 × 106 cells/kg | n/a | 12 months | ASIA and IANR-SCIFRS total scores revealed statistical increases, mainly reflected in the improvement of pinprick, light touch, motor and sphincter scores, decrease in muscle spasticity | no significant side effects, mostly fever and headache |
| Oraee-Yazdani et al. 2021 [164] | BMSCs | single-arm study | I/II | Iran | 11 | A | subacute | subarachnoid | 3 × 108 | Schwann cells | 12 months | positive sensory changes in AIS score, motor recovery; improvement in the trunk movement, equilibrium in standing/sitting positions, a reduction in the severity of constipation, improvement in sensation of the filling bladder and rectum, empowerment of voiding | increase in spasticity, numbness, or tingling sensation, neuropathic pain, headache and facial flushing |
| Deng et al 2020 [165] | UC-MSCs | non-randomized open-labeled controlled trial | I | China | 40 | A | acute | intramedullary | 4 × 107 | collagen scaffolds | 12 months | improvement in urinary functions and ASIA score in treatment group | no significant adverse effects |
| Curt et al. 2020 [30] | CNS- NSCs | non-randomized open-labeled controlled trial | I/II | Switzerland, Canada | 12 | A (n = 7), B (n = 5) | chronic | intramedullary | 2 × 107 | n/a | 6 years | improvement with reliable sensory improvements | headache, spasticity, pressure ulcer, erythema |
| Sharma et al. 2020 [166] | BMMNCs | non-randomized open-labeled controlled trial | II | India | 180 | A (n = 138), B (n = 28), C (n = 10), D (n = 3) | subacute and acute | subarachnoid | 1.06 × 108 | n/a | 9 ± 7 months | statistically significant improvement on FIM and WISCI scores | no significant adverse effects, mostly fever, headache |
| Levi et al. 2019 [31] | CNS- NSCs | randomized single-blinded controlled trial | II | United States | 16 | A (n = 3), B (n = 9) | chronic | intramedullary | 1.5 × 107–4 × 107 | n/a | 12 months | no significant improvement | musculoskeletal pain and infections |
| Levi et al. 2018 [167] | CNS- NSCs | non-randomized open-labeled controlled trial | I/II | United States | 12 | A (n = 8), B (n = 4) | chronic | intramedullary | 2 × 107 | n/a | 28–57 months | n/a | cerebrospinal fluid leakage, constipation and UTI, staph epidermidis wound infection, autonomic dysreflexia, postprocedural sepsis, posterior reversible encephalopathy syndrome, constipation, seizure, wound hematoma, aphasia |
| Levi et al. 2018 [167] | CNS- NSCs | randomized single-blinded controlled trial | II | United States | 17 | A (n = 3), B (n = 14) | chronic | intramedullary | 1.5 × 107–4 × 107 | n/a | 1–12 months | ||
| Curtis et al. 2018 [168] | SC- NSCs | single-arm study | I | United States | 4 | A | chronic | intramedullary | 1.2 × 106 | n/a | 60 months | no significant improvement | no adverse effects |
| Xiao et al. 2018 [169] | UCMSCs | single-arm study | I | China | 2 | A | acute | intramedullary | 4 × 107 | collagen scaffolds | 1 year | recovery of the sensory and motor functions; the sensory level expanded below the injury level, and the patients regained the sense function in bowel and bladder; 2 patients were improved from ASIA A to ASIA C; the recovery of the interrupted neural conduction | no adverse effects |
| Vaquero et al. 2018 [160] | BMSCs | non-randomized open-labeled uncontrolled trial | II | Spain | 11 | A (n = 3), B (n = 4), C (n = 3), D (n = 1) | chronic | subarachnoid | 1 × 108 | n/a | 10 months | improvement in sensitivity, motor power, spasms, spasticity, neuropathic pain, sexual function or sphincter dysfunction; 3 patients, initially classified as ASIA A, B and C, changed to ASIA B, C and D; decrease in postmicturition residue and improvement in bladder compliance; improvement in somatosensory or motor-evoked potentials, improvement in voluntary muscle contraction together with infralesional active muscle reinnervation | no significant adverse effects, mostly transitory sciatic pain, headaches, pain in the area of lumbar puncture |
| Vaquero et al. 2017 [170] | BMSCs | non-randomized open-labeled uncontrolled trial | I | Spain | 10 | B (n = 4), C (n = 5), D (n = 1) | chronic | subarachnoid | 4 doses, 3 × 107 | n/a | 12 months | improvement in sensitivity and motor function; improvement of sexual function; neuropathic pain disappeared or decreased; improvement in bladder and bowel control; improvement in spasms; decrease in spasticity | no significant adverse effects, mostly headaches and pain in the area of lumbar puncture |
| Ammar et al. 2017 [171] | HSCs | single-arm study | I | Saudi Arabia | 4 | A | chronic | intramedullary | 2.8 × 106 | PRP | 2–3 years | One patient demonstrated motor and objective sensory improvement (P = 0.05); two other patients reported subjective sensory improvement, and the fourth one remained without any improvement | no adverse effects |
| Technology | Phase of Studies | Advantages | Limitations | Refs | |
|---|---|---|---|---|---|
| Stem cell-derived exosomes | preclinical | comparable effectiveness with SCT avoids immune rejection and risk of carcinogenicity, avoids problems with low survival rate, dedifferentiation, and difficult obtainment of stem cells | not entirely studied the content of exosomes, lack of unified obtainment procedure, unstandardized number of injections, its frequency, and dosage | [206,207,208,209,210] | |
| Gene-modified stem cells | preclinical | better outcomes compared with non-modified stem cells, enables manipulation of the specific molecular pathways of spinal cord injury microenvironment to enhance treatment efficacy | safety concerns regarding the use of viral vectors for genetic engineering | [211] | |
| Biomaterials | Cell-free 3D-printed scaffolds | preclinical | creates a suitable microenvironment for stem cells, provides a bridging role, improves neural regeneration, resistance to toxic, temperature, and UV radiation during the fabrication process | immune rejection, cumbersome bioprinting procedure, limited availability of printable bioinks | [92,212] |
| 3D-printed scaffold loaded with stem cells | preclinical | possibility to create a "spinal cord-like" scaffold | restricted conditions of the manufacturing process, immune rejection, cumbersome bioprinting procedure, limited availability of printable bioinks | [92,212] | |
| Hydrogels | clinical | high biocompatibility may be used as a cell or cell factors’ carrier for its transport into the lesion site | fast degradation rate, low mechanical strength, and durability | [92] | |
| Nanomaterials | preclinical | improves stem cell transport and viability | not established release time and dose of drugs loaded on nanoparticles | [92] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szymoniuk, M.; Litak, J.; Sakwa, L.; Dryla, A.; Zezuliński, W.; Czyżewski, W.; Kamieniak, P.; Blicharski, T. Molecular Mechanisms and Clinical Application of Multipotent Stem Cells for Spinal Cord Injury. Cells 2023, 12, 120. https://doi.org/10.3390/cells12010120
Szymoniuk M, Litak J, Sakwa L, Dryla A, Zezuliński W, Czyżewski W, Kamieniak P, Blicharski T. Molecular Mechanisms and Clinical Application of Multipotent Stem Cells for Spinal Cord Injury. Cells. 2023; 12(1):120. https://doi.org/10.3390/cells12010120
Chicago/Turabian StyleSzymoniuk, Michał, Jakub Litak, Leon Sakwa, Aleksandra Dryla, Wojciech Zezuliński, Wojciech Czyżewski, Piotr Kamieniak, and Tomasz Blicharski. 2023. "Molecular Mechanisms and Clinical Application of Multipotent Stem Cells for Spinal Cord Injury" Cells 12, no. 1: 120. https://doi.org/10.3390/cells12010120
APA StyleSzymoniuk, M., Litak, J., Sakwa, L., Dryla, A., Zezuliński, W., Czyżewski, W., Kamieniak, P., & Blicharski, T. (2023). Molecular Mechanisms and Clinical Application of Multipotent Stem Cells for Spinal Cord Injury. Cells, 12(1), 120. https://doi.org/10.3390/cells12010120







