Mononuclear Phagocytes, Cellular Immunity, and Nobel Prizes: A Historic Perspective
Abstract
1. Introduction
- Emil von Behring, who received the first Nobel Prize for Physiology and Medicine in 1901 for introducing serum therapy as a passive vaccination against diphtheria and tetanus [15];
- Robert Koch, famed for his studies on tuberculosis and tuberculin-induced delayed hypersensitivity [16];
- Ramon Y. Cajal [17], who adapted Golgi’s silver staining method to map the intricate distribution of neurons in exquisite detail;

2. The Reticulo-Endothelial System (RES)
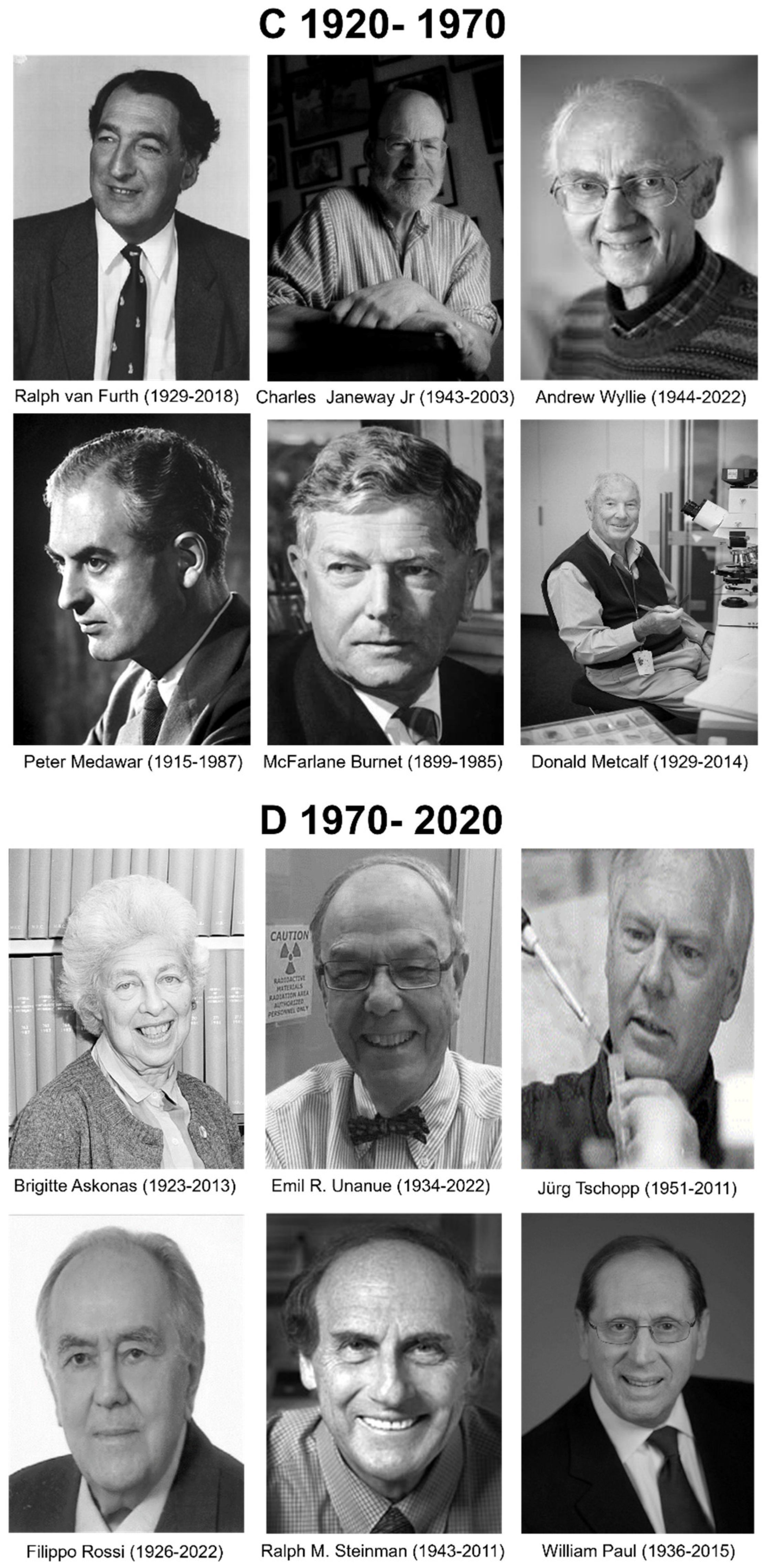
3. The Mononuclear Phagocyte System (MPS)
3.1. Enter the Lymphocytes
3.2. Enter Dendritic Cells (DCs)
3.3. Enter Monoclonal Antibodies
3.4. Resident Tissue Macrophages
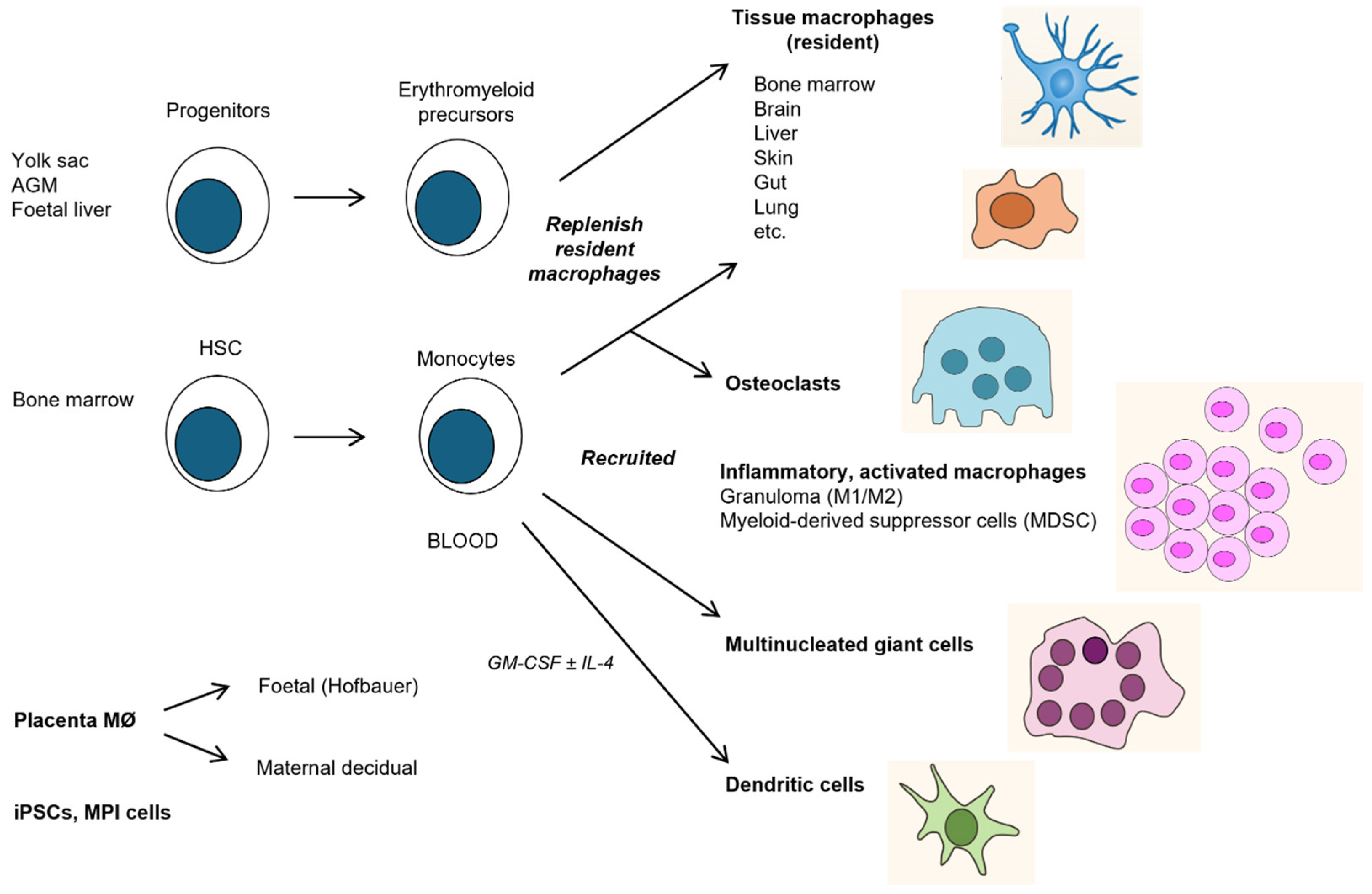
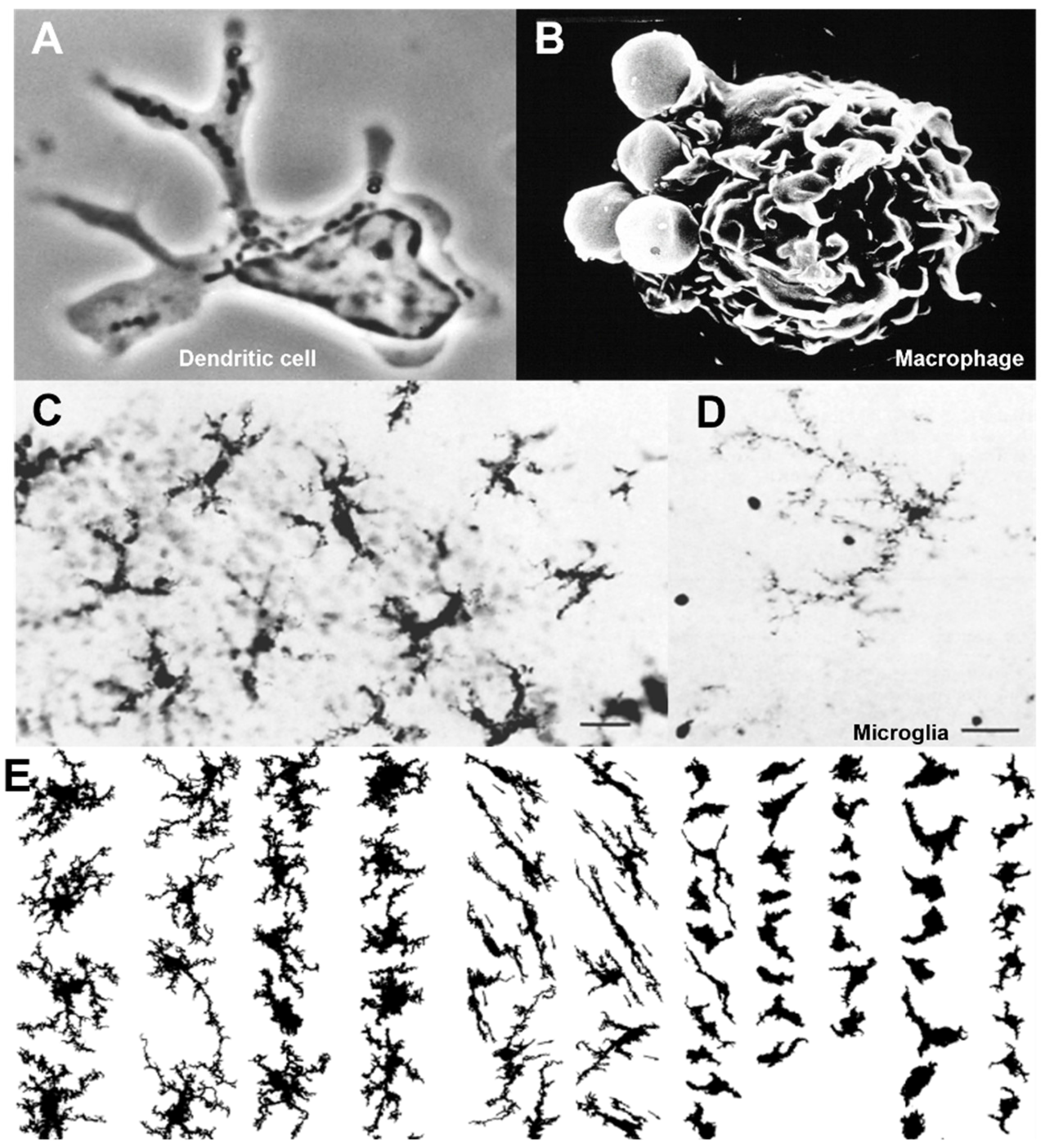
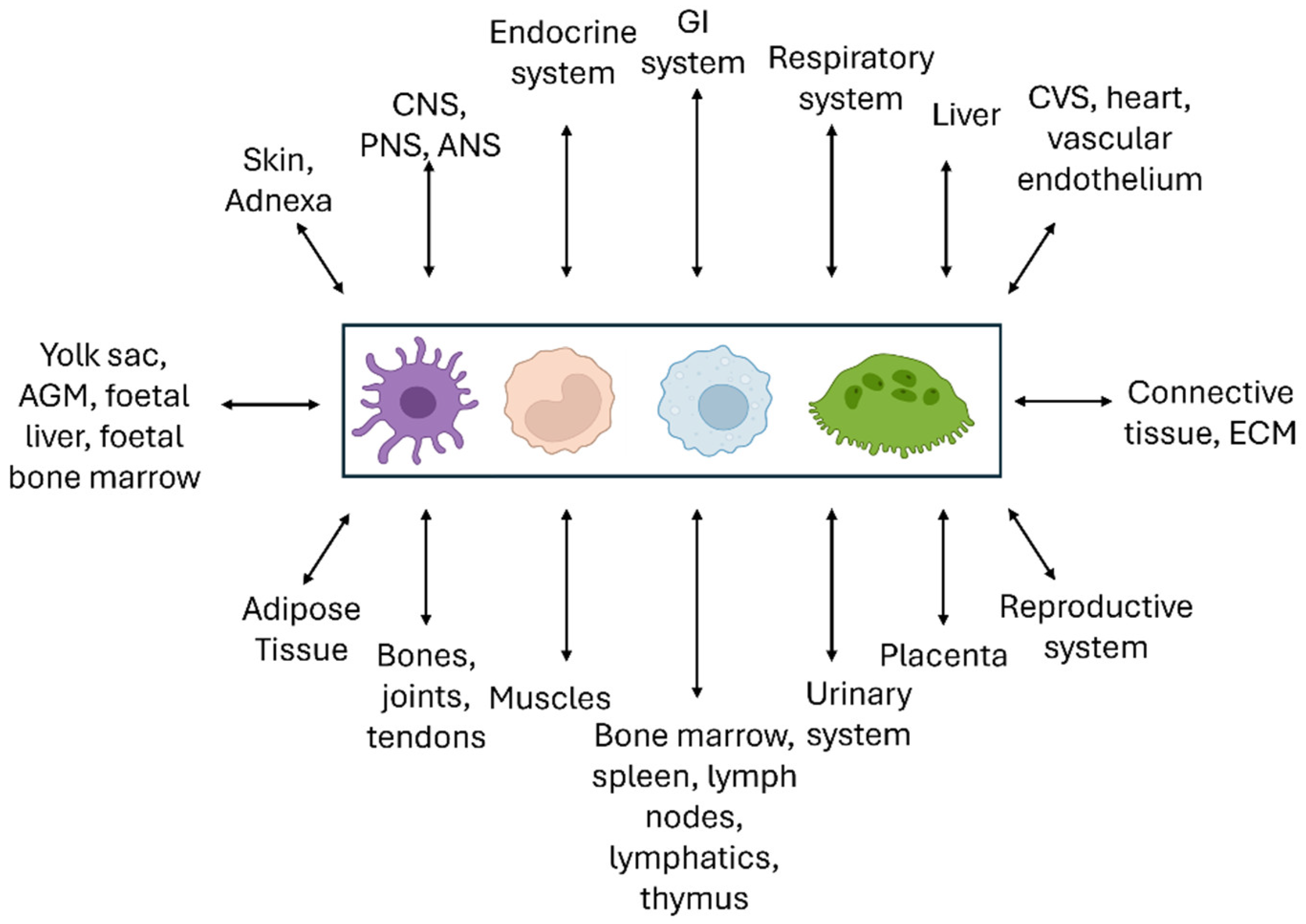
3.5. Development and Distribution
3.6. Distinct Properties of Elicited Monocyte-Derived Mononuclear Phagocytes
3.7. Re-Enter Complement
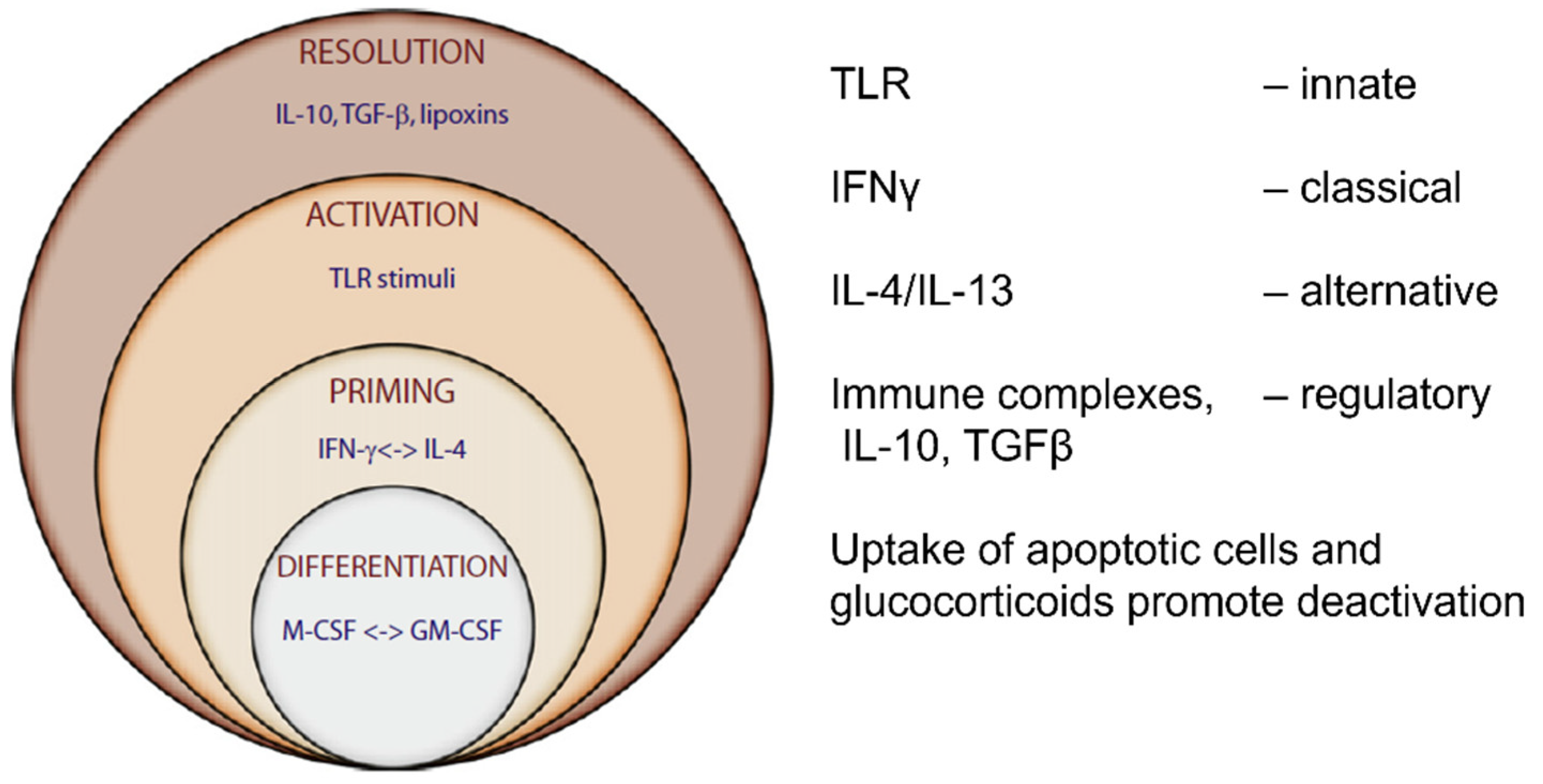
4. Cellular Functions of Mononuclear Phagocytes
4.1. Recognition, Uptake, and Degradation
4.2. Biosynthesis, Gene Expression, Metabolism, Cell Activation, and Secretion
4.3. Cellular Immunity and Granuloma Formation
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Darwin, C.; Beer, G. On the Origin of Species; OUP Oxford: Oxford, UK, 2008. [Google Scholar]
- Harris, H. The Birth of the Cell; Yale University Press: New Haven, CT, USA, 2000. [Google Scholar]
- Meyer, H.; Ackerknecht, E.H. Rudolf Virchow: Doctor, Statesman, Anthropologist. Books Abroad 1955, 29, 358. [Google Scholar] [CrossRef]
- Brock, T.D.; Geison, G.L.; Dubos, R.J. Pasteur and Modern Science; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Bernard, C. An Introduction to the Study of Experimental Medicine. 1865. Available online: https://www.britannica.com/topic/An-Introduction-to-the-Study-of-Experimental-Medicine (accessed on 11 August 2024).
- Cannon, W.B. The Wisdom of the Body; W.W. Norton, Incorporated: New York, NY, USA, 1939. [Google Scholar]
- Metchnikoff, E. Lectures on the Comparative Pathology of Inflammation: Delivered at the Pasteur Institute in 1891; Dover Publications: Mineola, NY, USA, 1968. [Google Scholar]
- Kaufmann, S.H. Immunology’s foundation: The 100-year anniversary of the Nobel Prize to Paul Ehrlich and Elie Metchnikoff. Nat. Immunol. 2008, 9, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, P. Paul Ehrlich-Nobel Lecture. Partial Cell Functions 1908. Available online: https://www.nobelprize.org/prizes/medicine/1908/ehrlich/lecture/ (accessed on 17 June 2024).
- Himmelweit, F. The Collected Papers of Paul Ehrlich: In Four Volumes Including a Complete Bibliography; Elsevier Science: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Ehrlich, P.; Himmelweit, T.; Marquardt, M.; Dale, H.H. The Collected Papers of Paul Ehrlich: Immunology and Cancer Research; Pergamon Press: Oxford, UK, 1957. [Google Scholar]
- Ehrlich, P.; Himmelweit, T.; Marquardt, M. The Collected Papers of Paul Ehrlich: Chemotherapy; Pergamon Press: Oxford, UK, 1960. [Google Scholar]
- Metchnikoff, E. Ilya Mechnikov-Nobel Lecture. On the Present State of the Question of Immunity in Infectious Diseases 1908. Available online: https://www.nobelprize.org/prizes/medicine/1908/mechnikov/lecture/ (accessed on 17 June 2024).
- Metchnikoff, O. Life of Elie Metchnikoff 1845–1916; Houghton Mifflin: New York, NY, USA, 1921. [Google Scholar]
- von Behring, E. Emil von Behring-Nobel Lecture. Serum Therapy in Therapeutics and Medical Science 1901. Available online: https://www.nobelprize.org/prizes/medicine/1901/behring/lecture/ (accessed on 17 June 2024).
- Brock, T.D. Robert Koch: A Life in Medicine and Bacteriology; ASM Press: Washington, DC, USA, 1999. [Google Scholar]
- Ehrlich, B. The Brain in Search of Itself: Santiago Ramón Y Cajal and the Story of the Neuron; Farrar, Straus and Giroux: New York, NY, USA, 2022. [Google Scholar]
- Dormandy, T. The White Death: A History of Tuberculosis; Hambledon Press: London, UK, 1999. [Google Scholar]
- Paolicelli, R.C.; Sierra, A.; Stevens, B.; Tremblay, M.-E.; Aguzzi, A.; Ajami, B.; Amit, I.; Audinat, E.; Bechmann, I.; Bennett, M.; et al. Microglia states and nomenclature: A field at its crossroads. Neuron 2022, 110, 3458–3483. [Google Scholar] [CrossRef] [PubMed]
- Vikhanski, L. Immunity: How Elie Metchnikoff Changed the Course of Modern Medicine; Chicago Review Press Incorporated: Chicago, IL, USA, 2016. [Google Scholar]
- Cavaillon, J.-M. The historical milestones in the understanding of leukocyte biology initiated by Elie Metchnikoff. J. Leukoc. Biol. 2011, 90, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Clarke, D.J.; Rebman, A.W.; Fan, J.; Soloski, M.J.; Aucott, J.N.; Ma’ayan, A. Gene set predictor for post-treatment Lyme disease. Cell Rep. Med. 2022, 3, 100816. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, N. René Dubos, the Autochthonous Flora, and the Discovery of the Microbiome. J. Hist. Biol. 2022, 55, 537–558. [Google Scholar] [CrossRef]
- Stambler, I.S. Elie Metchnikoff—The founder of longevity science and a founder of modern medicine: In honor of the 170th anniversary. Adv. Gerontol. 2015, 28, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Maisonneuve, P.; Metchnikoff, E.; Roux, P.P.E. The Experimental Prophylaxis of Syphilis; Creative Media Partners, LLC: Sacramento, CA, USA, 2015. [Google Scholar]
- Tolstoy, L. The Death of Ivan Ilyich; Open Road Media: New York, NY, USA, 2020. [Google Scholar]
- Rietschel, E.T.; Cavaillon, J.-M. Richard Pfeiffer and Alexandre Besredka: Creators of the concept of endotoxin and antiendotoxin. Microbes Infect. 2003, 5, 1407–1414. [Google Scholar] [CrossRef] [PubMed]
- Schama, S. Foreign Bodies: Pandemics, Vaccines and the Health of Nations; Simon & Schuster: London, UK, 2023. [Google Scholar]
- Bordet, J. The Nobel Prize in Physiology or Medicine. 1919. Available online: https://www.nobelprize.org/prizes/medicine/1919/summary/ (accessed on 18 June 2024).
- Hansson, N.; Angetter-Pfeiffer, D. Remembering innovative paediatrician Clemens von Pirquet on the 150th anniversary of his birth. Acta Paediatr. 2024, 113, 1778–1780. [Google Scholar] [CrossRef] [PubMed]
- NobelPrize.org. Charles Richet-Nobel Lecture. Available online: https://www.nobelprize.org/prizes/medicine/1913/richet/lecture/ (accessed on 25 June 2024).
- Nijweide, P.J.; Burger, E.H.; Feyen, J.H. Cells of bone: Proliferation, differentiation, and hormonal regulation. Physiol. Rev. 1986, 66, 855–886. [Google Scholar] [CrossRef] [PubMed]
- NobelPrize.org. The Nobel Prize in Physiology or Medicine 1945. Available online: https://www.nobelprize.org/prizes/medicine/1945/summary/ (accessed on 15 July 2024).
- NobelPrize.org. The Nobel Prize in Physiology or Medicine 1999. Available online: https://www.nobelprize.org/prizes/medicine/1999/summary/ (accessed on 15 July 2024).
- Hamann, J.; Petrenko, A.G. Introduction: History of the Adhesion GPCR Field. Handb. Exp. Pharmacol. 2016, 234, 1–11. [Google Scholar] [PubMed]
- Brown, G.D.; Gordon, S. Immune recognition. A new receptor for beta-glucans. Nature 2001, 413, 36–37. [Google Scholar] [CrossRef] [PubMed]
- NobelPrize.org. The Nobel Prize in Physiology or Medicine 2011. Available online: https://www.nobelprize.org/prizes/medicine/2011/summary/ (accessed on 15 July 2024).
- NobelPrize.org. The Nobel Prize in Physiology or Medicine 1980. Available online: https://www.nobelprize.org/prizes/medicine/1980/summary/ (accessed on 15 July 2024).
- Dzierzak, E.; de Pater, E. Regulation of Blood Stem Cell Development. Curr. Top. Dev. Biol. 2016, 118, 1–20. [Google Scholar] [PubMed]
- NobelPrize.org. The Nobel Prize in Physiology or Medicine 2019. Available online: https://www.nobelprize.org/prizes/medicine/2019/summary/ (accessed on 15 July 2024).
- Wake, K. Karl Wilhelm Kupffer and His Contributions To Modern Hepatology. Comp. Hepatol. 2004, 3, S2. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kodama, T.; Freeman, M.; Rohrer, L.; Zabrecky, J.; Matsudaira, P.; Krieger, M. Type I macrophage scavenger receptor contains α-helical and collagen-like coiled coils. Nature 1990, 343, 531–535. [Google Scholar] [CrossRef]
- Stanley, E.R.; Chitu, V. CSF-1 Receptor Signaling in Myeloid Cells. Cold Spring Harb. Perspect. Biol. 2014, 6, a021857. [Google Scholar] [CrossRef] [PubMed]
- Pappenheim, A.; Ferrata, A. Über die Verschiedenen Lymphoiden Zellformen des Normalen und Pathologischen Blutes. Folia Hematol. Frankfurt 1910, 10, 72–208. [Google Scholar]
- Beutler, B.; Cerami, A. The Biology of Cachectin/TNF—A Primary Mediator of the Host Response. Annu. Rev. Immunol. 1989, 7, 625–655. [Google Scholar] [CrossRef] [PubMed]
- Henson, P.M.; Bratton, D.L. Recognition and Removal of Apoptotic Cells, in Phagocyte-Pathogen Interactions: Macrophages and the Host Response to Infection; Russell, D.G., Gordon, S., Eds.; ASM Press: Washington, DC, USA, 2009; pp. 341–365. [Google Scholar]
- Crocker, P.R.; Gordon, S. Isolation and characterization of resident stromal macrophages and hematopoietic cell clusters from mouse bone marrow. J. Exp. Med. 1985, 162, 993–1014. [Google Scholar] [CrossRef] [PubMed]
- Nagata, S. Apoptosis and Clearance of Apoptotic Cells. Annu. Rev. Immunol. 2018, 36, 489–517. [Google Scholar] [CrossRef] [PubMed]
- Rossi, F. The O2−-forming NADPH oxidase of the phagocytes: Nature, mechanisms of activation and function. Biochim. Biophys. Acta 1986, 853, 65–89. [Google Scholar] [CrossRef] [PubMed]
- Waddington, C.H. Epigenetics and evolution. Symp. Soc. Exp. Biol. 1953, 7, 186–199. [Google Scholar]
- Blackburn, D.G.; Stewart, J.R. Morphological research on amniote eggs and embryos: An introduction and historical retrospective. J. Morphol. 2021, 282, 1024–1046. [Google Scholar] [CrossRef] [PubMed]
- Bessis, M. L’ilot erythroblastique. Unite functionelle de la moelle osseuse. Rev. Hematol. 1958, 13, 8–11. [Google Scholar]
- Kaufmann, S.H.E. Immunology’s Coming of Age. Front Immunol. 2019, 10, 684. [Google Scholar] [CrossRef] [PubMed]
- Silverstein, A.M. Paul Ehrlich’s Receptor Immunology: The Magnificent Obsession; Elsevier Science: Amsterdam, The Netherlands, 2001. [Google Scholar]
- Kay, A.B. Paul Ehrlich and the Early History of Granulocytes. Microbiol. Spectr. 2016, 4, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Aschoff, L. Das reticulo-endotheliale system. Ergeb. Inn. Med. Kinderheilk 1924, 26, 1–118. [Google Scholar]
- Cannon, W.B. The Way of an Investigator: A Scientist’s Experiences in Medical Research; W.W. Norton: New York, NY, USA, 1984. [Google Scholar]
- Tan, S.; Yip, A. Hans Selye (1907–1982): Founder of the stress theory. Singap. Med. J. 2018, 59, 170–171. [Google Scholar] [CrossRef]
- Dunnill, M.S. The Plato of Praed Street: The Life and Times of Almroth Wright; Royal Society of Medicine Press: London, UK, 2000. [Google Scholar]
- NobelPrize.org. The Nobel Prize in Physiology or Medicine 1972. 1972. Available online: https://www.nobelprize.org/prizes/medicine/1972/summary/ (accessed on 18 June 2024).
- Mastellos, D.C.; Hajishengallis, G.; Lambris, J.D. A guide to complement biology, pathology and therapeutic opportunity. Nat. Rev. Immunol. 2023, 24, 118–141. [Google Scholar] [CrossRef] [PubMed]
- Janeway, C.; Travers, P.; Walport, M.; Shlomchik, M. Immunobiology: The Immune System in Health and Disease; Garland Science: London, UK, 2005. [Google Scholar]
- MacPhail, T. Allergic: How Our Immune System Reacts to a Changing World; Penguin Books Limited: London, UK, 2023. [Google Scholar]
- Shaw, B.; Laurence, D. The Doctor’s Dilemma; Penguin Books Ltd.: London, UK, 1946. [Google Scholar]
- Berry, A.; Browne, J. Mendel and Darwin. Proc. Natl. Acad. Sci. USA 2022, 119, e2122144119. [Google Scholar] [CrossRef] [PubMed]
- Bearn, A.G. Archibald Garrod and the Individuality of Man; Clarendon Press: Oxford, UK, 1993. [Google Scholar]
- Roos, D.; Boer, M. Molecular diagnosis of chronic granulomatous disease. Clin. Exp. Immunol. 2014, 175, 139–149. [Google Scholar] [CrossRef] [PubMed]
- Bastard, P.; Rosen, L.B.; Zhang, Q.; Michailidis, E.; Hoffmann, H.-H.; Zhang, Y.; Dorgham, K.; Philippot, Q.; Rosain, J.; Béziat, V.; et al. Auto-antibodies against type I IFNs in patients with life-threatening COVID-19. Science 2020, 370, eabd4585. [Google Scholar] [CrossRef] [PubMed]
- Savic, S.; Coe, J.; Laws, P. Autoinflammation: Interferonopathies and Other Autoinflammatory Diseases. J. Investig. Dermatol. 2021, 142, 781–792. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, G.A.; Hughes, D. Emerging Therapies, in Lysosomal Storage Disorders; Lysosomal Storage Disorders; Wiley Online Library: Minneapolis, MN, USA, 2022; pp. 287–294. [Google Scholar]
- Rous, P.; Beard, J.W. Selection with the magnet and cultivation of reticulo-endothelial cells (kupffer cells). J. Exp. Med. 1934, 59, 577–591. [Google Scholar] [CrossRef] [PubMed]
- Sabin, F.R.; Cunningham, R.S.; Doan, C.A. Studies of the Blood in Experimental Tuberculosis: The Mono-cyte-Lymphocyte Ratio; The Anemia-Leucopenia Phase; National Tuberculosis Association: Seoul, Republic of Korea, 1926. [Google Scholar]
- Dannenberg, A.M. Cellular hypersensitivity and cellular immunity in the pathogensis of tuberculosis: Specificity, systemic and local nature, and associated macrophage enzymes. Bacteriol. Rev. 1968, 32, 85–102. [Google Scholar] [CrossRef] [PubMed]
- NobelPrize.org. Karl Landsteiner-Nobel Lecture. On Individual Differences in Human Blood. Available online: https://www.nobelprize.org/prizes/medicine/1930/landsteiner/lecture/ (accessed on 25 June 2024).
- Landsteiner, K.; Chase, M.W. Experiments on Transfer of Cutaneous Sensitivity to Simple Compounds. Exp. Biol. Med. 1942, 49, 688–690. [Google Scholar] [CrossRef]
- Fleming, A.; Wright, A.E. On a remarkable bacteriolytic element found in tissues and secretions. Proc. R. Soc. Lond. Ser. B Contain. Pap. A Biol. Character 1922, 93, 306–317. [Google Scholar]
- Leonard, C. Alexander Fleming, 1881–1955. Biogr. Mems Fell. R. Soc. 1956, 2, 117–127. [Google Scholar]
- Fleming, A. On the antibacterial action of cultures of a penicillium, with special reference to their use in the isolation of B. influenzae. Bull. World Health Organ. 1929, 79, 780–790. [Google Scholar] [CrossRef]
- MacFarlane, R.G. Howard Florey: The Making of a Great Scientist. Oxford University Press: Oxford, UK, 1979. [Google Scholar]
- Florey, H. General Pathology; W. B. Saunders Company: St. Louis, MO, USA, 1970. [Google Scholar]
- Mackaness, G.B. The action of drugs on intracellular tubercle bacilli. J. Pathol. Bacteriol. 1952, 64, 429–446. [Google Scholar] [CrossRef] [PubMed]
- Gowans, J.L.; Knight, E.J. The route of re-circulation of lymphocytes in the rat. Proc. R. Soc. London. Ser. B Boil. Sci. 1964, 159, 257–282. [Google Scholar] [CrossRef]
- Harris, H. Role of Chemotaxis in Inflammation. Physiol. Rev. 1954, 34, 529–562. [Google Scholar] [CrossRef] [PubMed]
- Billingham, R.E.; Brent, L.; Medawar, P.B. ‘Actively Acquired Tolerance’ of Foreign Cells. Nature 1953, 172, 603–606. [Google Scholar] [CrossRef] [PubMed]
- Medawar, P.B. Immunological tolerance. Science 1961, 133, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Porterfield, J.S. The National Institute for Medical Research, Mill Hill. Arch. Virol. 1995, 140, 1329–1336. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, A.; Lindenmann, J.; Andrewes, C.H. Virus interference. I. The interferon. Proc. R. Soc. Lond. Ser. B Biol. Sci. 1957, 147, 258–267. [Google Scholar]
- Armstrong, J.A.; Hart, P.D. Response of cultured macrophages to Mycobacterium tuberculosis, with observations on fusion of lysosomes with phagosomes. J. Exp. Med. 1971, 134, 713–740. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, J.H.; Grennan, D. Different macrophage populations distinguished by means of fluorescent polysaccharides. Recognition and properties of marginal-zone macrophages. Eur. J. Immunol. 1981, 11, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Mitchison, T.J.; Beverley, P.C. Nicholas Avrion Mitchison. 5 May 1928–28 December 2022. Biogr. Mems Fell. R. Soc. 2024. [Google Scholar] [CrossRef]
- Moberg, C.L.; Steinman, R.M. James Gerald Hirsch. Biogr. Mem. Natl. Acad. Sci. 2004, 84, 182–203. [Google Scholar] [PubMed]
- Steinman, R.M.; Moberg, C.L. Zanvil Alexander Cohn 1926–1993. J. Exp. Med. 1994, 179, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Moberg, C.L. An appreciation of Ralph Marvin Steinman (1943–2011). J. Exp. Med. 2011, 208, 2337–2342. [Google Scholar] [CrossRef]
- Moberg, C.L. René Dubos, Friend of the Good Earth: Microbiologist, Medical Scientist. Environmentalist; ASM Press: Washington, DC, USA, 2005. [Google Scholar]
- Woodruff, H.B.; Selman, A. Waksman, winner of the 1952 Nobel Prize for physiology or medicine. Appl. Environ. Microbiol. 2014, 80, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Pringle, P. Experiment Eleven: Dark Secrets Behind the Discovery of a Wonder Drug; Bloomsbury Publishing: London, UK, 2012. [Google Scholar]
- Hirsch, J.G. Bactericidal action of histone. J. Exp. Med. 1958, 108, 925–944. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, M.A. The Legionnaires’ disease bacterium (Legionella pneumophila) inhibits phagosome-lysosome fusion in human monocytes. J. Exp. Med. 1983, 158, 2108–2126. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.C.; Hirsch, J.G. The interaction between Toxoplasma gondii and mammalian cells. II. The absence of lysosomal fusion with phagocytic vacuoles containing living parasites. J. Exp. Med. 1972, 136, 1173–1194. [Google Scholar] [CrossRef] [PubMed]
- Johnson, W.D.; Mei, B.; Cohn, Z.A. The separation, long-term cultivation, and maturation of the human monocyte. J. Exp. Med. 1977, 146, 1613–1626. [Google Scholar] [CrossRef]
- NobelPrize.org. George E. Palade-Facts. Available online: https://www.nobelprize.org/prizes/medicine/1974/palade/facts/ (accessed on 20 June 2024).
- De Duve, C. Vital Dust: The Origin and Evolution of Life on Earth; Basic Books: New York, NY, USA, 1995. [Google Scholar]
- Rabinovitch, M. Professional and non-professional phagocytes: An introduction. Trends Cell Biol. 1995, 5, 85–87. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, G.; Cohn, Z.A. The immunobiology of leprosy. Int. Rev. Exp. Pathol. 1986, 28, 45–78. [Google Scholar] [PubMed]
- Kaplan, G.; Cohn, Z.A. Leprosy and cell-mediated immunity. Curr. Opin. Immunol. 1991, 3, 91–96. [Google Scholar] [CrossRef]
- McElrath, M.J.; Steinman, R.M.; Cohn, Z.A. Latent HIV-1 infection in enriched populations of blood monocytes and T cells from seropositive patients. J. Clin. Investig. 1991, 87, 27–30. [Google Scholar] [CrossRef]
- Van Furth, R. Mononuclear Phagocytes, Mononuclear Phagocytes; Blackwell Scientific Publications (C1970): Oxford, UK, 1970. [Google Scholar]
- Van Furth, R. Mononuclear Phagocytes in Immunity, Infection and Pathology; Mosby, Incorporated: St. Louis, MO, USA, 1975. [Google Scholar]
- Van Furth, R. Mononuclear Phagocytes: Functional Aspects; Springer: Dordrecht, The Netherlands, 1980. [Google Scholar]
- Van Furth, R. Mononuclear Phagocytes: Characteristics, Physiology and Function; Springer: Dordrecht, The Netherlands, 1985. [Google Scholar]
- Van Furth, R.; Cohn, Z.A.; Hirsch, J.G.; Humphrey, J.H.; Spector, W.G.; Langevoort, H.L. The mononuclear phagocyte system: A new classification of macrophages, monocytes, and their precursor cells. Bull. World Health Organ. 1972, 46, 845–852. [Google Scholar] [PubMed]
- Tauber, A.I. The birth of immunology: III. The fate of the phagocytosis theory. Cell. Immunol. 1992, 139, 505–530. [Google Scholar] [CrossRef] [PubMed]
- Gowans, J.L. First Medawar prize lecture. The recirculating small lymphocyte. Transplant Proc. 1991, 23, 7–8. [Google Scholar] [PubMed]
- Volkman, A.; Gowans, J. Origin of macrophages from bone marrow in rat. Br. J. Exp. Pathol. 1965, 46, 62–70. [Google Scholar] [PubMed]
- Marchesi, V.T.; Gowans, J.L. The migration of lymphocytes through the endothelium of venules in lymph nodes: An electron microscope study. Proc. R. Soc. London. Ser. B Biol. Sci. 1964, 159, 283–290. [Google Scholar] [CrossRef]
- Miller, J.F.A.P. Immunological function of the thymus. Lancet 1961, 278, 748–749. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.F.A.P. The discovery of thymus function and of thymus-derived lymphocytes. Immunol. Rev. 2002, 185, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.F.; Sprent, J. Cell-to-cell interaction in the immune response. VI. Contribution of thymus-derived cells and anti-body-forming cell precursors to immunological memory. J. Exp. Med. 1971, 134, 66–82. [Google Scholar] [CrossRef] [PubMed]
- Nature Milestones: T Cells. 2022. Available online: https://www.nature.com/immersive/d42859-022-00032-7/index.html (accessed on 20 June 2024).
- Gitlin, A.D.; Nussenzweig, M.C. Immunology: Fifty years of B lymphocytes. Nature 2015, 517, 139–141. [Google Scholar] [CrossRef] [PubMed]
- Zoltan Fehervari, Z.; Bordon, Y.; Dellisanti, C.; Bernard, N.; Wilson, J.D.K. Nature Milestones in Antibodies. 2016. Available online: https://www.nature.com/articles/d42859-021-00068-1 (accessed on 20 June 2024).
- Burnet, M. Self and Not-Self: Cellular Immunology Book One; Cambridge University Press: Cambridge, UK, 1969. [Google Scholar]
- Burnet, F.M. Immunological Recognition of Self. Science 1961, 133, 307–311. [Google Scholar] [CrossRef] [PubMed]
- NobelPrize.org. The Nobel Prize in Physiology or Medicine 1996. Available online: https://www.nobelprize.org/prizes/medicine/1996/summary/ (accessed on 20 June 2024).
- Metcalf, D. Growth and Differentiation Factors. Microbiol. Spectr. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Pixley, F.J.; Stanley, E.R. CSF-1 regulation of the wandering macrophage: Complexity in action. Trends Cell Biol. 2004, 14, 628–638. [Google Scholar] [CrossRef] [PubMed]
- Mackaness, G.B. The Immunological Basis of Acquired Cellular Resistance. J. Exp. Med. 1964, 120, 105–120. [Google Scholar] [CrossRef]
- Sorg, C.; Bloom, B.R. Products of activated lymphocytes: I. The use of radiolabeling techniques in the characterization and partial purification of the migration inhibitory factor of the guinea pig. J. Exp. Med. 1973, 137, 148–170. [Google Scholar] [CrossRef] [PubMed]
- Dinarello, C.A. Historical insights into cytokines. Eur. J. Immunol. 2007, 37 (Suppl. S1), S34–S45. [Google Scholar] [CrossRef] [PubMed]
- Mosmann, T.R.; Coffman, R.L. TH1 and TH2 Cells: Different Patterns of Lymphokine Secretion Lead to Different Functional Properties. Annu. Rev. Immunol. 1989, 7, 145–173. [Google Scholar] [CrossRef] [PubMed]
- Nathan, C.F.; Murray, H.W.; Wiebe, M.E.; Rubin, B.Y. Identification of interferon-gamma as the lymphokine that activates human macrophage oxidative metabolism and antimicrobial activity. J. Exp. Med. 1983, 158, 670–689. [Google Scholar] [CrossRef] [PubMed]
- Gray, P.W.; Goeddel, D.V. Structure of the human immune interferon gene. Nature 1982, 298, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Moberg, C.L. The discovery of dendritic cells. J. Exp. Med. 2021, 218, e20210830. [Google Scholar] [CrossRef] [PubMed]
- Steinman, R. Dendritic Cells: Linking Innate to Different Forms of Adaptive Immunity in The Biomedical & Biomedical Life Sciences Collection; Henry Stewart Talks: London, UK, 2009. [Google Scholar]
- Unanue, E.R.; Askonas, B.A. Persistence of immunogenicity of antigen after uptake by macrophages. J. Exp. Med. 1968, 127, 915–926. [Google Scholar] [CrossRef] [PubMed]
- Silverstein, S.C.; Steinman, R.M.; Cohn, Z.A. Endocytosis. Annu. Rev. Biochem. 1977, 46, 669–722. [Google Scholar] [CrossRef] [PubMed]
- Elliott, T.; Elvin, J.; Cerundolo, V.; Allen, H.; Townsend, A. Structural requirements for the peptide-induced conformational change of free major histocompatibility com-plex class I heavy chains. Eur. J. Immunol. 1992, 22, 2085–2091. [Google Scholar] [CrossRef] [PubMed]
- Bjorkman, P.J.; Saper, M.A.; Samraoui, B.; Bennett, W.S.; Strominger, J.L.; Wiley, D.C. Structure of the human class I histocompatibility antigen, HLA-A2. Nature 1987, 329, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Steinman, R.M.; Cohn, Z.A. Identification of a novel cell type in peripheral lymphoid organs of mice: I. morphology, quantitation, tissue distribution. J. Exp. Med. 1973, 137, 1142–1162. [Google Scholar] [CrossRef]
- Nussenzweig, M.C.; Steinman, R.M. Contribution of dendritic cells to stimulation of the murine syngeneic mixed leukocyte reaction. J. Exp. Med. 1980, 151, 1196–1212. [Google Scholar] [CrossRef] [PubMed]
- Paul, W.E. Dendritic Cells Bask in the Limelight. Cell 2007, 130, 967–970. [Google Scholar] [CrossRef] [PubMed]
- Inaba, K.; Inaba, M.; Romani, N.; Aya, H.; Deguchi, M.; Ikehara, S.; Muramatsu, S.; Steinman, R.M. Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granu-locyte/macrophage colony-stimulating factor. J. Exp. Med. 1992, 176, 1693–1702. [Google Scholar] [CrossRef] [PubMed]
- Merad, M.; Sathe, P.; Helft, J.; Miller, J.; Mortha, A. The Dendritic Cell Lineage: Ontogeny and Function of Dendritic Cells and Their Subsets in the Steady State and the Inflamed Setting. Annu. Rev. Immunol. 2013, 31, 563–604. [Google Scholar] [CrossRef] [PubMed]
- Bálint, Š.; Müller, S.; Fischer, R.; Kessler, B.M.; Harkiolaki, M.; Valitutti, S.; Dustin, M.L. Supramolecular attack particles are autonomous killing entities released from cytotoxic T cells. Science 2020, 368, 897–901. [Google Scholar] [CrossRef] [PubMed]
- Horton, C.; Shanmugarajah, K.; Fairchild, P.J. Harnessing the properties of dendritic cells in the pursuit of immunological tolerance. Biomed. J. 2017, 40, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Qin, S.; Cobbold, S.P.; Pope, H.; Elliott, J.; Kioussis, D.; Davies, J.; Waldmann, H. “Infectious” Transplantation Tolerance. Science 1993, 259, 974–977. [Google Scholar] [CrossRef] [PubMed]
- Mellman, I.; Chen, D.S.; Powles, T.; Turley, S.J. The cancer-immunity cycle: Indication, genotype, and immunotype. Immunity 2023, 56, 2188–2205. [Google Scholar] [CrossRef] [PubMed]
- Bearn, A.G.; Dixon, F.J.; Benacerraf, B.; Henry, G. Kunkel 1916–1983. An appreciation of the man and his scientific contri-butions & a bibliography of his research papers. J. Exp. Med. 1985, 161, 869–895. [Google Scholar]
- Harris, H.; Watkins, J.F.; Ford, C.E.; Schoefl, G.I. Artificial heterokaryons of animal cells from different species. J. Cell Sci. 1966, 1, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Klein, G.; Friberg, S., Jr.; Harris, H. Two kinds of antigen suppression in tumor cells revealed by cell fusion. J. Exp. Med. 1972, 135, 839–849. [Google Scholar] [CrossRef]
- Köhler, G.; Milstein, C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 1975, 256, 495–497. [Google Scholar] [CrossRef] [PubMed]
- Crumpton, M.J. Alan Frederick Williams 25 May 1945–9 April 1992. Biogr. Mem. Fellows R. Soc. 2004, 50, 351–366. [Google Scholar] [CrossRef] [PubMed]
- Springer, T.; Galfré, G.; Secher, D.S.; Milstein, C. Mac-1: A macrophage differentiation antigen identified by monoclonal antibody. Eur. J. Immunol. 1979, 9, 301–306. [Google Scholar] [CrossRef]
- Diamond, M.S.; Staunton, D.E.; Marlin, S.D.; Springer, T.A. Binding of the integrin Mac-1 (CD11b/CD18) to the third immunoglobulin-like domain of ICAM-1 (CD54) and its regulation by glycosylation. Cell 1991, 65, 961–971. [Google Scholar] [CrossRef]
- Feldman, M.; Feldman, M.; Taylor, P.; Paleolog, E.; Brennan, F.M.; Maini, R.N. Anti-TNF alpha therapy is useful in rheumatoid arthritis and Crohn’s disease: Analysis of the mechanism of action predicts utility in other diseases. Transplant Proc. 1998, 30, 4126–4127. [Google Scholar] [CrossRef] [PubMed]
- Austyn, J.M.; Gordon, S. F4/80, a monoclonal antibody directed specifically against the mouse macrophage. Eur. J. Immunol. 1981, 11, 805–815. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.; Plüddemann, A. Tissue macrophages: Heterogeneity and functions. BMC Biol. 2017, 15, 1–18. [Google Scholar] [CrossRef]
- Taylor, P.; Martinez-Pomares, L.; Stacey, M.; Lin, H.-H.; Brown, G.; Gordon, S. Macrophage receptors and immune recognition. Annu. Rev. Immunol. 2005, 23, 901–944. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.-H.; Ng, K.-F.; Chen, T.-C.; Tseng, W.-Y. Ligands and Beyond: Mechanosensitive Adhesion GPCRs. Pharmaceuticals 2022, 15, 219. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.S.; Hu, C.H.; Tseng, W.Y.; Cheng, C.H.; Stacey, M.; Gordon, S.; Chang, G.W.; Lin, H.H. Activation of Adhesion GPCR EMR2/ADGRE2 Induces Macrophage Differentiation and Inflammatory Responses via Gα(16)/Akt/MAPK/NF-κB Signaling Pathways. Front Immunol. 2017, 8, 373. [Google Scholar]
- Lin, H.H.; Faunce, D.E.; Stacey, M.; Terajewicz, A.; Nakamura, T.; Zhang-Hoover, J.; Kerley, M.; Mucenski, M.L.; Gordon, S.; Stein-Streilein, J. The macrophage F4/80 receptor is required for the induction of antigen-specific efferent regulatory T cells in peripheral tolerance. J. Exp. Med. 2005, 201, 1615–1625. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.; Plüddemann, A.; Mukhopadhyay, S. Plasma membrane receptors of tissue macrophages: Functions and role in pathology. J. Pathol. 2020, 250, 656–666. [Google Scholar] [CrossRef] [PubMed]
- Zulu, M.Z.; Martinez, F.O.; Gordon, S.; Gray, C.M. The Elusive Role of Placental Macrophages: The Hofbauer Cell. J. Innate Immun. 2019, 11, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 2006, 126, 663–676. [Google Scholar] [CrossRef] [PubMed]
- Fejer, G.; Wegner, M.D.; Gyory, I.; Cohen, I.; Engelhard, P.; Voronov, E.; Manke, T.; Ruzsics, Z.; Dolken, L.; Prazeres Da Costa, O.; et al. Nontransformed, GM-CSF-dependent macrophage lines are a unique model to study tissue macrophage func-tions. Proc. Natl. Acad. Sci. USA 2013, 110, E2191–E2198. [Google Scholar] [CrossRef] [PubMed]
- Mass, E.; Ballesteros, I.; Farlik, M.; Halbritter, F.; Günther, P.; Crozet, L.; Jacome-Galarza, C.E.; Händler, K.; Klughammer, J.; Kobayashi, Y.; et al. Specification of tissue-resident macrophages during organogenesis. Science 2016, 353. [Google Scholar] [CrossRef] [PubMed]
- Guilliams, M.; Scott, C.L. Liver macrophages in health and disease. Immunity 2022, 55, 1515–1529. [Google Scholar] [CrossRef]
- Amit, I.; Winter, D.R.; Jung, S. The role of the local environment and epigenetics in shaping macrophage identity and their effect on tissue homeostasis. Nat. Immunol. 2016, 17, 18–25. [Google Scholar] [CrossRef]
- Ginhoux, F.; Greter, M.; Leboeuf, M.; Nandi, S.; See, P.; Gokhan, S.; Mehler, M.F.; Conway, S.J.; Ng, L.G.; Stanley, E.R.; et al. Fate mapping analysis reveals that adult microglia derive from primitive macrophages. Science 2010, 330, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Hume, D.A.; Perry, V.H.; Gordon, S. The mononuclear phagocyte system of the mouse defined by immunohistochemical localisation of antigen F4/80: Macrophages associated with epithelia. Anat. Rec. 1984, 210, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Lawson, L.J.; Perry, V.H.; Dri, P.; Gordon, S. Heterogeneity in the distribution and morphology of microglia in the normal adult mouse brain. Neuroscience 1990, 39, 151–170. [Google Scholar] [CrossRef]
- Silverstein, S.C.; Michl, J.; Loike, J.D. Studies of the Mechanism of Phagocytosis, in International Cell Biology 1980–1981: Papers Presented at the Second International Congress on Cell Biology Berlin (West), 31 August–5 September 1980; Schweiger, H.G., Ed.; Springer: Berlin/Heidelberg, Germany, 1981; pp. 604–612. [Google Scholar]
- Yona, S.; Kim, K.-W.; Wolf, Y.; Mildner, A.; Varol, D.; Breker, M.; Strauss-Ayali, D.; Viukov, S.; Guilliams, M.; Misharin, A.; et al. Fate Mapping Reveals Origins and Dynamics of Monocytes and Tissue Macrophages under Homeostasis. Immunity 2013, 38, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Mariani, S.A.; Li, Z.; Rice, S.; Krieg, C.; Fragkogianni, S.; Robinson, N.; Vink, C.S.; Pollard, J.W.; Dzierzak, E. Pro-inflammatory Aorta-Associated Macrophages Are Involved in Embryonic Development of Hemato-poietic Stem Cells. Immunity 2019, 50, 1439–1452.e5. [Google Scholar] [CrossRef] [PubMed]
- Schulz, C.; Gomez Perdiguero, E.; Chorro, L.; Szabo-Rogers, H.; Cagnard, N.; Kierdorf, K.; Prinz, M.; Wu, B.; Jacobsen, S.E.W.; Pollard, J.W.; et al. A Lineage of Myeloid Cells Independent of Myb and Hematopoietic Stem Cells. Science 2012, 336, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Ginhoux, F.; Guilliams, M. Tissue-Resident Macrophage Ontogeny and Homeostasis. Immunity 2016, 44, 439–449. [Google Scholar] [CrossRef] [PubMed]
- Orsenigo, F.; Stewart, A.; Hammer, C.P.; Clarke, E.; Simpkin, D.; Attia, H.; Rockall, T.; Gordon, S.; Martinez, F.O. Unifying considerations and evidence of macrophage activation mosaicism through human CSF1R and M1/M2 genes. Cell Rep. 2024, 43, 114352. [Google Scholar] [CrossRef]
- Ziegler-Heitbrock, L.; Ancuta, P.; Crowe, S.; Dalod, M.; Grau, V.; Hart, D.N.; Leenen, P.J.M.; Liu, Y.-J.; MacPherson, G.; Randolph, G.J.; et al. Nomenclature of monocytes and dendritic cells in blood. Blood 2010, 116, e74–e80. [Google Scholar] [CrossRef] [PubMed]
- Carlin, L.M.; Auffray, C.; Satoh, T.; Woollard, K.; Geissmann, F. Functions and molecular mechanisms of patrolling monocytes. Vasc. Pharmacol. 2012, 56, 328. [Google Scholar] [CrossRef]
- Janssen, H.; Kahles, F.; Liu, D.; Downey, J.; Koekkoek, L.L.; Roudko, V.; D’souza, D.; McAlpine, C.S.; Halle, L.; Poller, W.C.; et al. Monocytes re-enter the bone marrow during fasting and alter the host response to infection. Immunity 2023, 56, 783–796.e7. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.; Kubes, P. Innate immune cells orchestrate the repair of sterile injury in the liver and beyond. Eur. J. Immunol. 2019, 49, 831–841. [Google Scholar] [CrossRef] [PubMed]
- Bellingan, G.J.; Caldwell, H.; Howie, S.E.; Dransfield, I.; Haslett, C. In vivo fate of the inflammatory macrophage during the resolution of inflammation: Inflammatory macrophages do not die locally, but emigrate to the draining lymph nodes. J. Immunol. 1996, 157, 2577–2585. [Google Scholar] [CrossRef] [PubMed]
- Bonnardel, J.; T’jonck, W.; Gaublomme, D.; Browaeys, R.; Scott, C.L.; Martens, L.; Vanneste, B.; De Prijck, S.; Nedospasov, S.A.; Kremer, A.; et al. Stellate Cells, Hepatocytes, and Endothelial Cells Imprint the Kupffer Cell Identity on Monocytes Colonizing the Liver Macrophage Niche. Immunity 2019, 51, 638–654.e9. [Google Scholar] [CrossRef]
- Cugurra, A.; Mamuladze, T.; Rustenhoven, J.; Dykstra, T.; Beroshvili, G.; Greenberg, Z.J.; Baker, W.; Papadopoulos, Z.; Drieu, A.; Blackburn, S.; et al. Skull and vertebral bone marrow are myeloid cell reservoirs for the meninges and CNS parenchyma. Science 2021, 373, eabf7844. [Google Scholar] [CrossRef] [PubMed]
- Jacome-Galarza, C.E.; Percin, G.I.; Muller, J.T.; Mass, E.; Lazarov, T.; Eitler, J.; Rauner, M.; Yadav, V.K.; Crozet, L.; Bohm, M.; et al. Developmental origin, functional maintenance and genetic rescue of osteoclasts. Nature 2019, 568, 541–545. [Google Scholar] [CrossRef]
- Alvarez, D.; Vollmann, E.H.; von Andrian, U.H. Mechanisms and Consequences of Dendritic Cell Migration. Immunity 2008, 29, 325–342. [Google Scholar] [CrossRef] [PubMed]
- Towiwat, P.; Chhana, A.; Dalbeth, N. The anatomical pathology of gout: A systematic literature review. BMC Musculoskelet. Disord. 2019, 20, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Pillemer, L.; Blum, L.; Lepow, I.H.; Ross, O.A.; Todd, E.W.; Wardlaw, A.C. The Properdin System and Immunity: I. Demonstration and Isolation of a New Serum Protein, Properdin, and Its Role in Immune Phenomena. Science 1954, 120, 279–285. [Google Scholar] [CrossRef]
- Götze, O.; Müller-eberhard, H.J. The Alternative Pathway of Complement Activation. In Advances in Immunology; Dixon, F.J., Kunkel, H.G., Eds.; Academic Press: Cambridge, MA, USA, 1976; pp. 1–35. [Google Scholar]
- Turner, M. The role of mannose-binding lectin in health and disease. Mol. Immunol. 2003, 40, 423–429. [Google Scholar] [CrossRef]
- Sawaya, A.P.; Vecin, N.M.; Burgess, J.L.; Ojeh, N.; DiBartolomeo, G.; Stone, R.C.; Pastar, I.; Tomic-Canic, M. Calreticulin: A multifunctional protein with potential therapeutic applications for chronic wounds. Front. Med. 2023, 10, 1207538. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Valentino, S.; Gentile, S.; Inforzato, A.; Bottazzi, B.; Garlanda, C. The long pentraxin PTX3: A paradigm for humoral pattern recognition molecules. Ann. N. Y. Acad. Sci. 2013, 1285, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Colten, H.R. Ontogeny of the Human Complement System: In Vitro Biosynthesis of Individual Complement Components by Fetal Tissues. J. Clin. Investig. 1972, 51, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Gao, Y.; Shi, C.; Tong, J.; Ma, D.; Shen, J.; Yang, J.; Ji, M. Complement C1q drives microglia-dependent synaptic loss and cognitive impairments in a mouse model of lipopolysaccharide-induced neuroinflammation. Neuropharmacology 2023, 237, 109646. [Google Scholar] [CrossRef] [PubMed]
- West, E.E.; Kemper, C. Complosome—The intracellular complement system. Nat. Rev. Nephrol. 2023, 19, 426–439. [Google Scholar] [CrossRef] [PubMed]
- Matzinger, P. Tolerance, Danger, and the Extended Family. Annu. Rev. Immunol. 1994, 12, 991–1045. [Google Scholar] [CrossRef]
- Medzhitov, R.; Janeway, C., Jr. Innate immune recognition: Mechanisms and pathways. Immunol. Rev. 2000, 173, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Kerr, J.F.; Wyllie, A.H.; Currie, A.R. Apoptosis: A basic biological phenomenon with wide-ranging implications in tissue kinetics. Br. J. Cancer 1972, 26, 239–257. [Google Scholar] [CrossRef] [PubMed]
- Willingham, S.B.; Volkmer, J.-P.; Gentles, A.J.; Sahoo, D.; Dalerba, P.; Mitra, S.S.; Wang, J.; Contreras-Trujillo, H.; Martin, R.; Cohen, J.D.; et al. The CD47-signal regulatory protein alpha (SIRPa) interaction is a therapeutic target for human solid tumors. Proc. Natl. Acad. Sci. USA 2012, 109, 6662–6667. [Google Scholar] [CrossRef] [PubMed]
- Griffin, F.M., Jr.; Bianco, C.; Silverstein, S.C. Characterization of the macrophage receptro for complement and demon-stration of its functional independence from the receptor for the Fc portion of immunoglobulin G. J. Exp. Med. 1975, 141, 1269–1277. [Google Scholar] [CrossRef]
- Botelho, R.J.; Teruel, M.; Dierckman, R.; Anderson, R.; Wells, A.; York, J.D.; Meyer, T.; Grinstein, S. Localized Biphasic Changes in Phosphatidylinositol-4,5-Bisphosphate at Sites of Phagocytosis. J. Cell Biol. 2000, 151, 1353–1368. [Google Scholar] [CrossRef] [PubMed]
- Goodridge, H.S.; Reyes, C.N.; Becker, C.A.; Katsumoto, T.R.; Ma, J.; Wolf, A.J.; Bose, N.; Chan, A.S.H.; Magee, A.S.; Danielson, M.E.; et al. Activation of the innate immune receptor Dectin-1 upon formation of a ‘phagocytic synapse’. Nature 2011, 472, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.J.; van der Merwe, P.A. The kinetic-segregation model: TCR triggering and beyond. Nat. Immunol. 2006, 7, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Halstead, S.B. Antibodies Determine Virulence in Dengue. Ann. N. Y. Acad. Sci. 2009, 1171, E48–E56. [Google Scholar] [CrossRef] [PubMed]
- Peiris, J.S.M.; Gordon, S.; Unkeless, J.C.; Porterfield, J.S. Monoclonal anti-Fc receptor IgG blocks antibody enhancement of viral replication in macrophages. Nature 1981, 289, 189–191. [Google Scholar] [CrossRef] [PubMed]
- Cardosa, B.M.J.; Porterfield, J.S.; Gordon, S. Complement receptor mediates enhanced flavivirus replication in macro-phages. J. Exp. Med. 1983, 158, 258–263. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Zhong, L.; Yan, H.; Virata, M.L.; Deng, L.; Mishra, A.K.; Struble, E.; Scott, D.; Zhang, P. In vitro enhancement of Zika virus infection by preexisting West Nile virus antibodies in human plasma-derived immunoglobulins revealed after P2 binding site-specific enrichment. Microbiol. Spectr. 2024, 12, e0075824. [Google Scholar] [CrossRef]
- Schafer, D.P.; Lehrman, E.K.; Kautzman, A.G.; Koyama, R.; Mardinly, A.R.; Yamasaki, R.; Ransohoff, R.M.; Greenberg, M.E.; Barres, B.A.; Stevens, B. Microglia sculpt postnatal neural circuits in an activity and complement-dependent manner. Neuron 2012, 74, 691–705. [Google Scholar] [CrossRef] [PubMed]
- Menon, V.; Ghaffari, S. Erythroid enucleation: A gateway into a “bloody” world. Exp. Hematol. 2021, 95, 13–22. [Google Scholar] [CrossRef]
- Nicolás-Ávila, J.A.; Lechuga-Vieco, A.V.; Esteban-Martínez, L.; Sánchez-Díaz, M.; Díaz-García, E.; Santiago, D.J.; Rubio-Ponce, A.; Li, J.L.; Balachander, A.; Quintana, J.A.; et al. A Network of Macrophages Supports Mitochondrial Homeostasis in the Heart. Cell 2020, 183, 94–109.e23. [Google Scholar] [CrossRef]
- Brestoff, J.R.; Wilen, C.B.; Moley, J.R.; Li, Y.; Zou, W.; Malvin, N.P.; Rowen, M.N.; Saunders, B.T.; Ma, H.; Mack, M.R.; et al. Intercellular Mitochondria Transfer to Macrophages Regulates White Adipose Tissue Homeostasis and Is Impaired in Obesity. Cell Metab. 2020, 33, 270–282.e8. [Google Scholar] [CrossRef] [PubMed]
- Steinman, R.M.; Mellman, I.S.; A Muller, W.; Cohn, Z.A. Endocytosis and the recycling of plasma membrane. J. Cell Biol. 1983, 96, 1–27. [Google Scholar] [CrossRef]
- Hilligan, K.L.; Ronchese, F. Antigen presentation by dendritic cells and their instruction of CD4+ T helper cell responses. Cell. Mol. Immunol. 2020, 17, 587–599. [Google Scholar] [CrossRef] [PubMed]
- Randolph, G.J.; Jakubzick, C.; Qu, C. Antigen presentation by monocytes and monocyte-derived cells. Curr. Opin. Immunol. 2007, 20, 52–60. [Google Scholar] [CrossRef]
- Puleston, D.J.; Simon, A.K. Autophagy in the immune system. Immunology 2013, 141, 1–8. [Google Scholar] [CrossRef]
- Russell, D.G. Mycobacterium tuberculosis and the intimate discourse of a chronic infection. Immunol. Rev. 2011, 240, 252–268. [Google Scholar] [CrossRef]
- Gordon, S. Phagocytosis: An Immunobiologic Process. Immunity 2016, 44, 463–475. [Google Scholar] [CrossRef] [PubMed]
- NobelPrize.org. The Nobel Prize in Chemistry 2004. Available online: https://www.nobelprize.org/prizes/chemistry/2004/summary/ (accessed on 27 June 2024).
- Hernández-Morán, B.A.; Taylor, G.; Lorente-Macías, Á.; Wood, A.J. Degron tagging for rapid protein degradation in mice. Dis. Model. Mech. 2024, 17, dmm050613. [Google Scholar] [CrossRef]
- NobelPrize.org. The Nobel Prize in Physiology or Medicine 1985. Available online: https://www.nobelprize.org/prizes/medicine/1985/summary/ (accessed on 27 June 2024).
- Nairz, M.; Theurl, I.; Swirski, F.K.; Weiss, G. “Pumping iron”-how macrophages handle iron at the systemic, microenvironmental, and cellular levels. Pflugers. Arch. 2017, 469, 397–418. [Google Scholar] [CrossRef] [PubMed]
- Nathan, C. Secretory products of macrophages: Twenty-five years on. J. Clin. Investig. 2012, 122, 1189–1190. [Google Scholar] [CrossRef] [PubMed]
- Liebold, I.; Al Jawazneh, A.; Casar, C.; Lanzloth, C.; Leyk, S.; Hamley, M.; Wong, M.N.; Kylies, D.; Gräfe, S.K.; Edenhofer, I.; et al. Apoptotic cell identity induces distinct functional responses to IL-4 in efferocytic macrophages. Science 2024, 384, eabo7027. [Google Scholar] [CrossRef] [PubMed]
- Martinez, F.O.; Gordon, S. The M1 and M2 paradigm of macrophage activation: Time for reassessment. F1000Prime Rep. 2014, 6, 13. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.; Martinez, F.O. Alternative Activation of Macrophages: Mechanism and Functions. Immunity 2010, 32, 593–604. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.; Todd, J.; Cohn, Z.A. In vitro synthesis and secretion of lysozyme by mononuclear phagocytes. J. Ex-Perimental Med. 1974, 139, 1228–1248. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.; Werb, Z. Secretion of macrophage neutral proteinase is enhanced by colchicine. Proc. Natl. Acad. Sci. USA 1976, 73, 872–876. [Google Scholar] [CrossRef] [PubMed]
- Amersfoort, J.; Eelen, G.; Carmeliet, P. Immunomodulation by endothelial cells—Partnering up with the immune system? Nat. Rev. Immunol. 2022, 22, 576–588. [Google Scholar] [CrossRef]
- Winkler, J.; Abisoye-Ogunniyan, A.; Metcalf, K.J.; Werb, Z. Concepts of extracellular matrix remodelling in tumour progression and metastasis. Nat. Commun. 2020, 11, 5120. [Google Scholar] [CrossRef] [PubMed]
- NobelPrize.org. The Nobel Prize in Physiology or Medicine 1931. Available online: https://www.nobelprize.org/prizes/medicine/1931/summary/ (accessed on 27 June 2024).
- NobelPrize.org. Available online: https://www.nobelprize.org/prizes/medicine/1953/summary/ (accessed on 27 June 2024).
- Murphy, M.P.; O’neill, L.A.J. A break in mitochondrial endosymbiosis as a basis for inflammatory diseases. Nature 2024, 626, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Sica, A.; Locati, M. Macrophage Polarization Comes of Age. Immunity 2005, 23, 344–346. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.; Chung, M.; Harris, S.; Martinez-Estrada, F.; Mukhopadhyay, S. Macrophage Class A Scavenger Receptors—A Functional Perspective. In Encyclopedia of Cell Biology; Elsevier: Amsterdam, The Netherlands, 2022. [Google Scholar]
- Pick, E. In Memoriam: Filippo Rossi (1926–2022). J. Leukoc. Biol. 2023, 113, 231–235. [Google Scholar] [CrossRef]
- Nathan, C.; Liu, P.; Adams, J.S.; Modlin, R.L. Role of iNOS in Human Host Defense. Science 2006, 312, 1874–1875. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.; Keshav, S.; Harris, N.; Gordon, S. Interleukin 4 potently enhances murine macrophage mannose receptor activity: A marker of alternative im-munologic macrophage activation. J. Exp. Med. 1992, 176, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Sica, A.; Sozzani, S.; Allavena, P.; Vecchi, A.; Locati, M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004, 25, 677–686. [Google Scholar] [CrossRef]
- Park, M.D.; Belabed, M.; Chen, S.T.; Hamon, P.; Hegde, S.; Mattiuz, R.; Marron, T.U.; Merad, M. On the Biology and Therapeutic Modulation of Macrophages and Dendritic Cells in Cancer. Annu. Rev. Cancer Biol. 2023, 7, 291–311. [Google Scholar] [CrossRef]
- Cassetta, L.; Pollard, J.W. Tumor-associated macrophages. Curr. Biol. 2020, 30, R246–R248. [Google Scholar] [CrossRef] [PubMed]
- Balkwill, F.R.; Mantovani, A. Cancer-related inflammation: Common themes and therapeutic opportunities. Semin. Cancer Biol. 2011, 22, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Blériot, C.; Dunsmore, G.; Alonso-Curbelo, D.; Ginhoux, F. A temporal perspective for tumor-associated macrophage identities and functions. Cancer Cell 2024, 42, 747–758. [Google Scholar] [CrossRef]
- Mantovani, A.; Dinarello, C.A.; Molgora, M.; Garlanda, C. Interleukin-1 and Related Cytokines in the Regulation of Inflammation and Immunity. Immunity 2019, 50, 778–795. [Google Scholar] [CrossRef] [PubMed]
- Martinon, F.; Burns, K.; Tschopp, J. The inflammasome: A molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Mol Cell 2002, 10, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Barnett, K.C.; Li, S.; Liang, K.; Ting, J.P.Y. A 360° view of the inflammasome: Mechanisms of activation, cell death, and diseases. Cell 2023, 186, 2288–2312. [Google Scholar] [CrossRef] [PubMed]
- Hertzog, J.; Rehwinkel, J. Regulation and inhibition of the DNA sensor cGAS. Embo Rep. 2020, 21, e51345. [Google Scholar] [CrossRef] [PubMed]
- Lawn, S.D.; Meintjes, G. Pathogenesis and prevention of immune reconstitution disease during antiretroviral therapy. Expert Rev. Anti-Infect. Ther. 2011, 9, 415–430. [Google Scholar] [CrossRef]
- Webb, B.J. Defining COVID-19-associated hyperinflammatory syndrome in specific populations. Lancet Rheumatol. 2021, 3, e609–e611. [Google Scholar] [CrossRef] [PubMed]
- Dexamethasone in Hospitalized Patients with Covid-19. New Engl. J. Med. 2021, 384, 693–704. [CrossRef] [PubMed]
- Roberti, A.; Chaffey, L.E.; Greaves, D.R. NF-κB Signaling and Inflammation-Drug Repurposing to Treat Inflammatory Disorders? Biology 2022, 11, 372. [Google Scholar] [CrossRef] [PubMed]
- Altmann, D.M.; Whettlock, E.M.; Liu, S.; Arachchillage, D.J.; Boyton, R.J. The immunology of long COVID. Nat. Rev. Immunol. 2023, 23, 618–634. [Google Scholar] [CrossRef] [PubMed]
- Mariano, M.; Spector, W.G. The formation and properties of macrophage polykaryons (inflammatory giant cells). J. Pathol. 1974, 113, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Hughes, E.J.; Tobin, D.M. Decoding the tuberculous granuloma. Immunity 2022, 55, 819–821. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.R.; Horsley, H.; Frankel, P.; Khosravi, M.; Goble, T.; Carter, S.; Antonelou, M.; Evans, R.D.R.; Zhang, X.; Chu, T.-Y.; et al. Proteinase 3 promotes formation of multinucleated giant cells and granuloma-like structures in patients with granulomatosis with polyangiitis. Ann. Rheum. Dis. 2023, 82, 848–856. [Google Scholar] [CrossRef] [PubMed]
- Spector, W.G. Immunologic components of granuloma formation. Epithelioid cells, giant cells, and sarcoidosis. Ann. N. Y. Acad. Sci. 1976, 278, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, C.; Fallon, P.G. Schistosoma “Eggs-Iting” the Host: Granuloma Formation and Egg Excretion. Front. Immunol. 2018, 9, 2492. [Google Scholar] [CrossRef] [PubMed]
- Ahmadzadeh, K.; Pereira, M.; Vanoppen, M.; Bernaerts, E.; Ko, J.H.; Mitera, T.; Maksoudian, C.; Manshian, B.B.; Soenen, S.; Rose, C.D.; et al. Multinucleation resets human macrophages for specialized functions at the expense of their identity. EMBO Rep. 2023, 24, e56310. [Google Scholar] [CrossRef] [PubMed]
- Brooks, P.J.; Glogauer, M.; McCulloch, C.A. An Overview of the Derivation and Function of Multinucleated Giant Cells and Their Role in Pathologic Processes. Am. J. Pathol. 2019, 189, 1145–1158. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.; Petretto, E.; Gordon, S.; Bassett, J.H.D.; Williams, G.R.; Behmoaras, J. Common signalling pathways in macrophage and osteoclast multinucleation. J. Cell Sci. 2018, 131, jcs216267. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.F.; Togbe, D.; Ryffel, B. Editorial: Ozone as a Driver of Lung Inflammation and Innate Immunity and as a Model for Lung Disease. Front. Immunol. 2021, 12, 714161. [Google Scholar] [CrossRef]
- Dobzhansky, T. Nothing in Biology Makes Sense except in the Light of Evolution. Am. Biol. Teach. 1973, 35, 125–129. [Google Scholar] [CrossRef]
- Cooper, S.J. From Claude Bernard to Walter Cannon. Emergence of the concept of homeostasis. Appetite 2008, 51, 419–427. [Google Scholar] [CrossRef]
- Pirzgalska, R.M.; Seixas, E.; Seidman, J.S.; Link, V.M.; Sanchez, N.M.; Mahú, I.; Mendes, R.; Gres, V.; Kubasova, N.; Morris, I.; et al. Sympathetic neuron–associated macrophages contribute to obesity by importing and metabolizing norepinephrine. Nat. Med. 2017, 23, 1309–1318. [Google Scholar] [CrossRef] [PubMed]
- Hulsmans, M.; Clauss, S.; Xiao, L.; Aguirre, A.D.; King, K.R.; Hanley, A.; Hucker, W.J.; Wülfers, E.M.; Seemann, G.; Courties, G.; et al. Macrophages Facilitate Electrical Conduction in the Heart. Cell 2017, 169, 510–522.e20. [Google Scholar] [CrossRef] [PubMed]
- Schulthess, J.; Pandey, S.; Capitani, M.; Rue-Albrecht, K.C.; Arnold, I.; Franchini, F.; Chomka, A.; Ilott, N.E.; Johnston, D.G.W.; Pires, E.; et al. The Short Chain Fatty Acid Butyrate Imprints an Antimicrobial Program in Macrophages. Immunity 2019, 50, 432–445.e437. [Google Scholar] [CrossRef]
- Tabas, I. 2016 Russell Ross Memorial Lecture in Vascular Biology. Arter. Thromb. Vasc. Biol. 2017, 37, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Huby, T.; Gautier, E.L. Immune cell-mediated features of non-alcoholic steatohepatitis. Nat. Rev. Immunol. 2021, 22, 429–443. [Google Scholar] [CrossRef] [PubMed]
- Mildner, A.; Schlevogt, B.; Kierdorf, K.; Böttcher, C.; Erny, D.; Kummer, M.P.; Quinn, M.; Brück, W.; Bechmann, I.; Heneka, M.T.; et al. Distinct and non-redundant roles of microglia and myeloid subsets in mouse models of Alzheimer’s disease. J. Neurosci. 2011, 31, 11159–11171. [Google Scholar] [CrossRef] [PubMed]
- Cooper, M. Which came first, T cells or B cells? Nat. Rev. Immunol. 2021, 21, 616–617. [Google Scholar] [CrossRef] [PubMed]
- NobelPrize.org. Svante Pääbo-Nobel Lecture. Available online: https://www.nobelprize.org/prizes/medicine/2022/paabo/lecture/ (accessed on 1 July 2024).
- Quintana-Murci, L.; Clark, A.G. Population genetic tools for dissecting innate immunity in humans. Nat. Rev. Immunol. 2013, 13, 280–293. [Google Scholar] [CrossRef] [PubMed]
- Barreiro, L.B.; Quintana-Murci, L. From evolutionary genetics to human immunology: How selection shapes host defence genes. Nat. Rev. Genet. 2009, 11, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Margulis, L.; Margulis, U.M.A.M.L. Symbiosis in Cell Evolution: Life and Its Environment on the Early Earth; W. H. Freeman: New York, NY, USA, 1981. [Google Scholar]
- Margulis, L.; Sagan, D. Lynn Margulis: The Life and Legacy of a Scientific Rebel; Chelsea Green Publishing: Junction, UT, USA, 2012. [Google Scholar]
- Dopkins, N.; Nixon, D.F. Activation of human endogenous retroviruses and its physiological consequences. Nat. Rev. Mol. Cell Biol. 2023, 25, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Martin, N.; Li, M.; Mann, S. Living material assembly of bacteriogenic protocells. Nature 2022, 609, 1029–1037. [Google Scholar] [CrossRef] [PubMed]



| Year | Names | Topic | Comment |
|---|---|---|---|
| 1901 | Von Behring | Diphtheria | Antibodies |
| 1905 | Koch | TB | Cell-mediated |
| 1908 | Metchnikoff, Ehrlich | Phagocytosis, Receptors | Cell-mediated and antibodies |
| 1912 | Carrel | Work on vascular suture and the transplantation of blood vessels and organs | Cell culture |
| 1913 | Richet | Anaphylaxis | Cell-mediated and antibodies |
| 1919 | Bordet | Complement | Humoral |
| 1930 | Landsteiner | Blood groups | Antibodies |
| 1931 | Warburg | Respiration | Metabolism |
| 1945 | Fleming, Chain, Florey | Penicillin | Antibiotics |
| 1950 | Kendall, Reichstein, Hench | Corticosteroids | Anti-inflammatory |
| 1951 | Theiler | Yellow fever vaccine | Adaptive |
| 1952 | Waksman | Streptomycin | Antibiotic TB |
| 1953 | Krebs, Lipmann | Citric acid cycle, coenzyme A | Metabolism |
| 1954 | Enders, Weller, Robbins | Polio virus | Isolation |
| 1960 | Burnet, Medawar | Self and non-self, tolerance | Cell-mediated, transplantation |
| 1966 | Rous, Huggins | Viral malignancy | Magnetic beads macrophage isolation |
| 1972 | Edelman, Porter | Antibodies | Structure |
| 1974 | Claude, de Duve, Palade | Cell structure | Cell biology, transmission EM |
| 1975 | Baltimore, Dulbecco, Temin | Viral replication | NF-κB pathway |
| 1976 | Blumberg, Gajdusek | Hepatitis, Prions | Infection |
| 1980 | Benacerraf, Dausset, Snell | Histocompatibility antigens | Genetics |
| 1982 | Bergstrom, Samuelsson, Vane | Prostaglandins | Regulatory |
| 1984 | Jerne, Kohler, Milstein | Monoclonal antibodies | Specific targeting |
| 1985 | Brown, Goldstein | Cholesterol | Scavenger receptor |
| 1987 | Tonegawa | Genetic control of antibodies | Lymphocytes |
| 1990 | Murray, Thomas | Transplantation | Cell-mediated |
| 1994 | Gilman, Rodbell | G-proteins | Signalling |
| 1996 | Doherty, Zinkernagel | MHC peptide recognition | Cell-mediated and lymphocytes |
| 1998 | Furchgott, Ignarro, Murad | NO | Effector metabolite |
| 1999 | Blobel | Protein signal peptide | Membrane transport |
| 2001 | Hartwell, Hunt, Nurse | Regulators of cell cycle | Cell cycle |
| 2002 | Brenner, Horvitz, Sulston | Genetics of organ development, programmed cell death | Evolution, C. elegans |
| 2005 | Marshall, Warren | Helicobacter pylori infection | Peptic ulcers |
| 2008 | Zur Hausen, Barre-Sinoussi, Montagnier | HPV and HIV | CD4 depletion, opportunistic infection |
| 2011 | Hoffmann, Beutler, Steinman | Insect, TNF, TLR, DCs | Innate immunity and antigen presentation |
| 2012 | Gurdon, Yamanaka | Reprogramming differentiation | iPSC |
| 2013 | Rothman, Schekman, Sudhof | Vesicular trafficking | Cell biology |
| 2016 | Ohsumi | Autophagy | Macrophages |
| 2018 | Allison, Honjo | Cancer immunotherapy | Checkpoint inhibitors |
| 2019 | Ratcliffe, Kaelin, Semenza | Oxygen sensing | Respiratory burst |
| 2020 | Houghton, Alter, Rice | Hepatitis C virus | Virus |
| 2021 | Patapoutian, Julius | Receptors for temperature and touch | Receptor biology |
| 2022 | Paabo | Genomes of extinct hominins and human evolution | Evolution and genetics |
| Chemistry and Physics | |||
| 1902 | Fischer | Sugar and purine synthesis | Biochemistry |
| 1946 | Stanley, Northrop | Tobacco mosaic virus crystallization | Viral structure |
| 1948 | Tiselius | Electrophoresis | Method |
| Pauling | Protein bonds | Structural Biology/Chemistry | |
| 1958 | Sanger | Proteins | Sequence |
| 1962 | Perutz, Kendrew | Protein Structure | Analytic |
| 1972 | Anfinsen | Ribonuclease | Protein strucure |
| 1980 | Berg, Gilbert, Sanger | DNA | Sequencing |
| 1982 | Klug | Crystallography | Protein structure |
| 1993 | Mullis, Smith | PCR and mutagenesis | Nucleic acid |
| 2004 | Ciechanover, Hershko, Rose | Protein ubiquitination | Degradation |
| 2009 | Ramakrishnan, Steitz, Yonath | Ribosome | Structural biology |
| 2008 | Shimomura, Chalfie, Tsien | Green fluorescent protein | Detection, microscopy |
| 2012 | Lefkowitz, Kobilka | GPCRs | Signalling |
| 2018 | Arnold, Smith, Winter | Enzymes, phage display of peptides and antibodies | Directed evolution |
| 2020 | Charpentier, Doudna | Genome editing | CRISPR |
| 2022 | Bertozzi, Meldal, Sharpless | Click chemistry and biorthogonal chemistry | Protein and therapeutics |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gordon, S.; Roberti, A.; Kaufmann, S.H.E. Mononuclear Phagocytes, Cellular Immunity, and Nobel Prizes: A Historic Perspective. Cells 2024, 13, 1378. https://doi.org/10.3390/cells13161378
Gordon S, Roberti A, Kaufmann SHE. Mononuclear Phagocytes, Cellular Immunity, and Nobel Prizes: A Historic Perspective. Cells. 2024; 13(16):1378. https://doi.org/10.3390/cells13161378
Chicago/Turabian StyleGordon, Siamon, Annabell Roberti, and Stefan H. E. Kaufmann. 2024. "Mononuclear Phagocytes, Cellular Immunity, and Nobel Prizes: A Historic Perspective" Cells 13, no. 16: 1378. https://doi.org/10.3390/cells13161378
APA StyleGordon, S., Roberti, A., & Kaufmann, S. H. E. (2024). Mononuclear Phagocytes, Cellular Immunity, and Nobel Prizes: A Historic Perspective. Cells, 13(16), 1378. https://doi.org/10.3390/cells13161378







