The Pathogenesis and Virulence of the Major Enterovirus Pathogens Associated with Severe Clinical Manifestations: A Comprehensive Review
Abstract
Highlights
- The review provides a systematic analysis of the distinct pathogenesis and tissue tropisms of major enteroviruses, linking these characteristics to severe clinical outcomes.
- The review summarizes the comprehensive landscape of key host receptors that mediate viral entry, which underlies their distinct pathogenesis.
- The review highlights successful vaccines against EV-A71 and polio. Furthermore, it summarizes promising preclinical advances for other prevalent and transmissible serotypes, such as EV-D68, while underscoring the critical gap in approved vaccines for them.
Abstract
1. Introduction
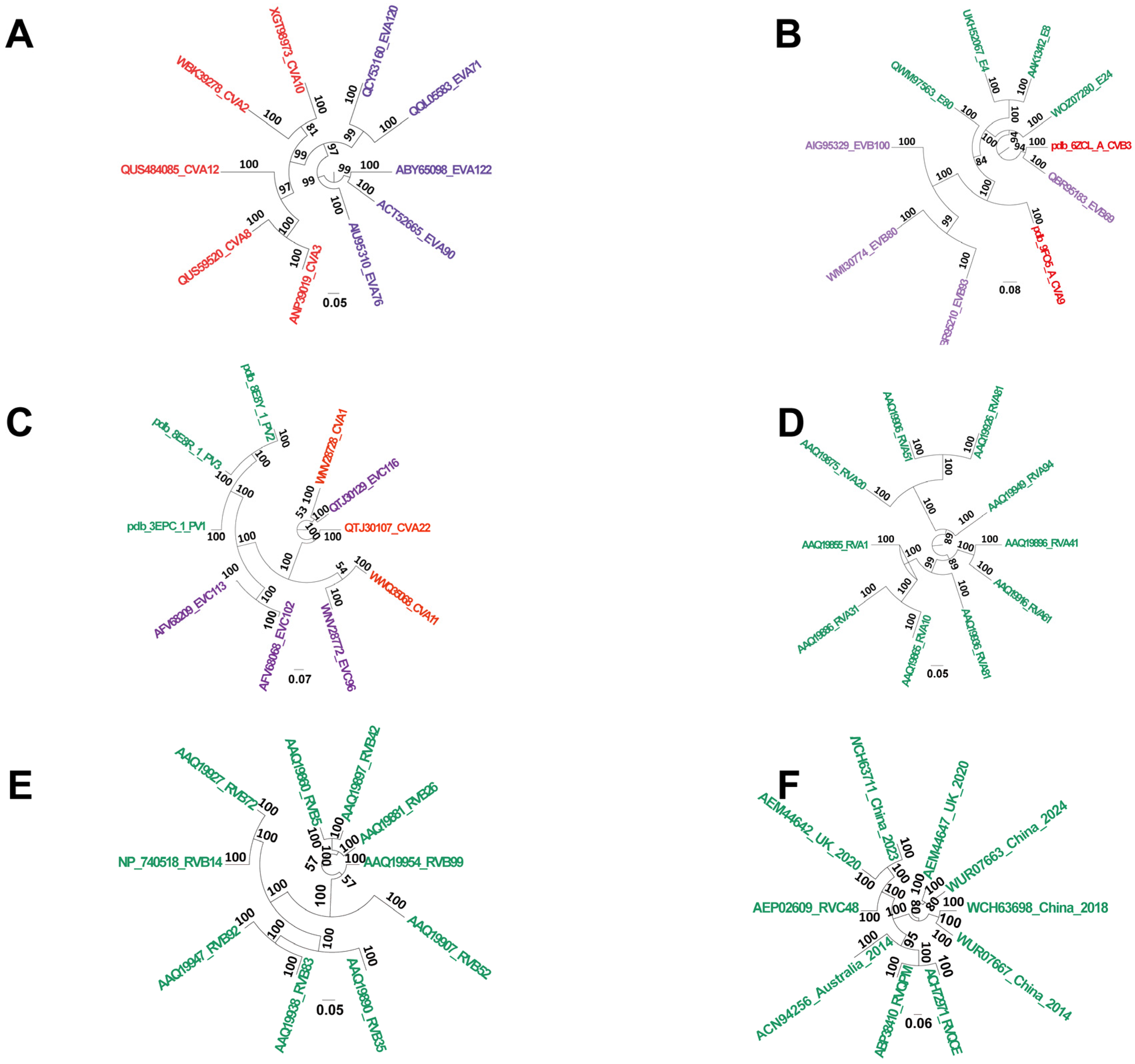
2. The Taxonomy of Enterovirus
2.1. The Pattern of Organism Invasion by Typical Serotypes of Common Enteroviruses Associated with Human Diseases
2.2. Representative Serotypes of Common Enterovirus Subtypes Implicated in Clinical Diseases
2.3. Receptors for Typical Serotypes of Common Enterovirus Subtypes
| Receptor | Distribution | Function | Type | Ref. |
|---|---|---|---|---|
| SCARB2 | SCARB2 demonstrates ubiquitous expression but shows enriched levels in specific cell populations: neurons, pulmonary cells, hepatocytes, splenic germinal center B cells, and the epithelial linings of the renal tubules and intestines. | Facilitates virus binding, internalization, and uncoating; involved in the early stages of viral infection | Capsid receptor | [54,55] |
| PSGL-1 | Expression of PSGL-1 is largely restricted to the hematopoietic system, particularly within myeloid and lymphoid cell populations. | Not directly involved in infection | Adsorption receptor | [56,57] |
| Sialylated glycans | Widely distributed across nearly all tissues | Concentrates virions on the host cell surface and enhances infectivity | Adsorption receptor | [58] |
| Heparan sulfate (HS) | HS is widely distributed and is particularly enriched on the surface of vascular endothelial cells, hepatic sinusoidal endothelial cells, and in the basement membranes of renal glomeruli. | Facilitates viral adsorption but does not support replication or propagation | Adsorption receptor | [59,60] |
| Annexin A2 (Anx2) | Expressed in a wide range of cells and tissues | Promotes viral attachment to the cell surface, enhancing infectivity | Adsorption receptor | [55,61] |
| Prohibitin | Localized to multiple cellular compartments, including the nucleus and mitochondria | Supports viral adsorption and plays a role in intracellular replication | Adsorption receptor | [62,63] |
| Fibronectin | Present in the extracellular matrix of various tissues | Mediates viral adsorption | Adsorption receptor | [64] |
| Vimentin | Vimentin serves as a critical accomplice in viral infection, being exploited by viruses to facilitate their own replication, dissemination, and evasion of immune clearance. | Facilitates viral adhesion | Adsorption receptor | [65] |
3. Coxsackievirus Receptors
Poliovirus Receptor
4. Vaccines Against Enteroviruses: Current Status and Developments
4.1. EV-A71 Vaccines
4.2. EV-D68 Vaccines
4.3. CV-A16 Vaccines
4.4. CV-B3 Vaccine Development
4.5. Poliovirus Vaccines
5. Discussion
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, Y.; Li, H.; Huang, X.; Huang, Y.; Lv, M.; Tang, H.; Han, X.; Liu, J.; Liang, Y.; Zang, G.; et al. NAD+ Suppresses EV-D68 Infection by Enhancing Anti-Viral Effect of SIRT1. Viruses 2025, 17, 175. [Google Scholar] [CrossRef]
- Kinobe, R.; Wiyatno, A.; Artika, I.M.; Safari, D. Insight into the Enterovirus A71: A review. Rev. Med. Virol. 2022, 32, e2361. [Google Scholar] [CrossRef]
- Wang, H.; Wang, W.; Chen, G.; Hu, C.; Chen, S.; Mao, L.; Shen, H. Molecular characteristics of the structure protein VP1 in Coxsackievirus A10 Isolates from China. J. Infect. Dev. Ctries. 2024, 18, 1118–1123. [Google Scholar] [CrossRef]
- Gaume, L.; Chabrolles, H.; Bisseux, M.; Lopez-Coqueiro, I.; Dehouck, L.; Mirand, A.; Henquell, C.; Gosselet, F.; Archimbaud, C.; Bailly, J.L. Enterovirus A71 crosses a human blood-brain barrier model through infected immune cells. Microbiol. Spectr. 2024, 12, e0069024. [Google Scholar] [CrossRef]
- Waghchaure, R.; Kunjumon, J.; Ashraf, A.F.; Raju, R.M.; Shete, A.; Cherian, S.; Lavania, M. Complete-Genome Analysis of Echovirus-30 Isolated from an Encephalitis Case in India Revealed Distinct Mutations. Microorganisms 2025, 13, 1580. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, X.; Zhang, Y.; Li, H.; Zheng, H.; Wang, J.; Liao, Y.; Yu, L.; Li, D.; Zhao, H.; et al. The Expression Pattern of the Splice Variants of Coxsackievirus and Adenovirus Receptor Impacts CV-B3-Induced Encephalitis and Myocarditis in Neonatal Mice. Int. J. Mol. Sci. 2025, 26, 7163. [Google Scholar] [CrossRef] [PubMed]
- Sepúlveda, R.T.; Jiang, S.; Beischel, J.; Bellamy, W.T.; Watson, R.R. Cocaine injection and coxsackievirus B3 infection increase heart disease during murine AIDS. J. Acquir. Immune Defic. Syndr. 2000, 25 (Suppl. S1), S19–S26. [Google Scholar] [CrossRef]
- Huisman, J.S.; Torii, S.; Wynn, H.K.; Gan, C.; Voellmy, I.K.; Huber, M.; Julian, T.R.; Kohn, T. Transmission dynamics of Norovirus GII and Enterovirus in Switzerland during the COVID-19 pandemic (2021–2022) as evidenced in wastewater. Epidemics 2025, 52, 100851. [Google Scholar] [CrossRef]
- Zhang, X.; Sun, R.; Hou, J.; Jia, W.; Li, P.; Shi, S.; Song, C.; Cheng, Y. Clinical characteristics of fatal cases of hand, foot and mouth disease in children. Front. Pediatr. 2025, 13, 1522164. [Google Scholar] [CrossRef] [PubMed]
- George, G.M.; Darius, J.D.H.; Mathew, L.; Peter, D.; George, L.; Pulimood, S.; Abraham, A.M.; Mammen, S. Changing epidemiology of human enteroviruses (HEV) in a hand, foot and mouth disease outbreak in Vellore, south India. Indian J. Med. Microbiol. 2022, 40, 394–398. [Google Scholar] [CrossRef]
- Peternell, A.; Schödl, C.; Odri Komazec, I.; Baumann, M.; Lechner, C. Clinical Presentation and Outcome of Five Neonates With Enterovirus Central Nervous System Infection: Contrasting One Kawasaki-Like Case With Cardiac Involvement and Seizures With Four Benign Cases. Case Rep. Pediatr. 2025, 2025, 5569829. [Google Scholar] [CrossRef]
- Lizasoain, A.; Martínez, N.; de Mora, C.; Rodríguez, E.; Ledezma, N.; Colina, R. Identification of the Emerging C1-like Lineage of Enterovirus A71 in Two Uruguayan Children with Hand-Foot-and-Mouth Disease and Neurological Complications. Viruses 2024, 16, 1752. [Google Scholar] [CrossRef]
- Lin, M.T.; Wang, J.K.; Lu, F.L.; Wu, E.T.; Yeh, S.J.; Lee, W.L.; Wu, J.M.; Wu, M.H. Heart rate variability monitoring in the detection of central nervous system complications in children with enterovirus infection. J. Crit. Care 2006, 21, 280–286. [Google Scholar] [CrossRef]
- Hu, Y.L.; Cheng, A.L.; Chen, S.H.; Fang, C.T.; Chang, L.Y. Febrile young infants and the association with enterovirus infection. J. Formos. Med. Assoc. = Taiwan Yi Zhi, 2024; Online ahead of print. [Google Scholar] [CrossRef]
- Nafisa, S.; Paul, P.; Sovani, M. A Case Report of Acute Flaccid Paralysis Caused by Enterovirus D68 Infection: The Beginning of a Polio-Like Epidemic? Cureus 2021, 13, e15625. [Google Scholar] [CrossRef]
- Baba, M.M.; Oderinde, B.S.; Patrick, P.Z.; Jarmai, M.M. Sabin and wild polioviruses from apparently healthy primary school children in northeastern Nigeria. J. Med. Virol. 2012, 84, 358–364. [Google Scholar] [CrossRef]
- Phyu, W.K.; Ong, K.C.; Wong, K.T. A Consistent Orally-Infected Hamster Model for Enterovirus A71 Encephalomyelitis Demonstrates Squamous Lesions in the Paws, Skin and Oral Cavity Reminiscent of Hand-Foot-and-Mouth Disease. PLoS ONE 2016, 11, e0147463. [Google Scholar] [CrossRef]
- Rajal, V.B.; McSwain, B.S.; Thompson, D.E.; Leutenegger, C.M.; Wuertz, S. Molecular quantitative analysis of human viruses in California stormwater. Water Res. 2007, 41, 4287–4298. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Zhang, X.Y.; Jin, W.P.; Wang, C.; Qian, S.S.; Wang, M.J.; Wang, W.H.; Meng, S.L.; Guo, J.; Wang, Z.J.; et al. Identification of a Conserved, Linear Epitope on VP3 of Enterovirus A Species Recognized by a Broad-Spectrum Monoclonal Antibody. Viruses 2023, 15, 1028. [Google Scholar] [CrossRef] [PubMed]
- Helgers, L.C.; Bhoekhan, M.S.; Pajkrt, D.; Wolthers, K.C.; Geijtenbeek, T.B.H.; Sridhar, A. Human Dendritic Cells Transmit Enterovirus A71 via Heparan Sulfates to Target Cells Independent of Viral Replication. Microbiol. Spectr. 2022, 10, e0282222. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Liu, B.; Yue, L.; Xie, T.; Li, H.; Shao, M.; Yang, R.; Luo, F.; Long, R.; Xie, Z. Preclinical safety assessment of a combined vaccine against Hepatitis a virus and enterovirus 71. Vaccine 2021, 39, 3952–3963. [Google Scholar] [CrossRef]
- Gu, J.; Wu, J.; Cao, Y.; Zou, X.; Jia, X.; Yin, Y.; Shen, L.; Fang, D.; Mao, L. A Mouse Model for Infection with Enterovirus A71 in Small Extracellular Vesicles. mSphere 2020, 5, e00377-20. [Google Scholar] [CrossRef] [PubMed]
- Phyu, W.K.; Ong, K.C.; Kong, C.K.; Alizan, A.K.; Ramanujam, T.M.; Wong, K.T. Squamous epitheliotropism of Enterovirus A71 in human epidermis and oral mucosa. Sci. Rep. 2017, 7, 45069. [Google Scholar] [CrossRef]
- Xing, J.; Liu, D.; Shen, S.; Su, Z.; Zhang, L.; Duan, Y.; Tong, F.; Liang, Y.; Wang, H.; Deng, F.; et al. Pathologic Studies of Fatal Encephalomyelitis in Children Caused by Enterovirus 71. Am. J. Clin. Pathol. 2016, 146, 95–106. [Google Scholar] [CrossRef]
- Qin, X.X.; Deng, M.; Wu, J.; Yang, J.; You, L.; Meng, S.L.; Guo, J.; Qian, S.S.; Shen, S. Cellular response, persistent humoral response and efficacy elicited by a CV-A16 vaccine candidate in mice. Vaccine 2025, 61, 127276. [Google Scholar] [CrossRef]
- Yogarajah, T.; Ong, K.C.; Perera, D.; Wong, K.T. Enterovirus A71 and coxsackievirus A16 show different replication kinetics in human neuronal and non-neuronal cell lines. Arch. Virol. 2017, 162, 727–737. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.P.; Chong, Y.M.; Tay, C.G.; Koh, M.T.; Chem, Y.K.; Noordin, N.; Jahis, R.; Sam, I.C.; Chan, Y.F. Detection of enteroviruses during a 2018 hand, foot and mouth disease outbreak in Malaysia. Trop. Biomed. 2021, 38, 150–153. [Google Scholar] [CrossRef]
- Zhao, T.S.; Du, J.; Sun, D.P.; Zhu, Q.R.; Chen, L.Y.; Ye, C.; Wang, S.; Liu, Y.Q.; Cui, F.; Lu, Q.B. A review and meta-analysis of the epidemiology and clinical presentation of coxsackievirus A6 causing hand-foot-mouth disease in China and global implications. Rev. Med. Virol. 2020, 30, e2087. [Google Scholar] [CrossRef]
- Blomqvist, S.; Klemola, P.; Kaijalainen, S.; Paananen, A.; Simonen, M.L.; Vuorinen, T.; Roivainen, M. Co-circulation of coxsackieviruses A6 and A10 in hand, foot and mouth disease outbreak in Finland. J. Clin. Virol. 2010, 48, 49–54. [Google Scholar] [CrossRef]
- Hubiche, T.; Schuffenecker, I.; Boralevi, F.; Léauté-Labrèze, C.; Bornebusch, L.; Chiaverini, C.; Phan, A.; Maruani, A.; Miquel, J.; Lafon, M.E.; et al. Dermatological spectrum of hand, foot and mouth disease from classical to generalized exanthema. Pediatr. Infect. Dis. J. 2014, 33, e92–e98. [Google Scholar] [CrossRef] [PubMed]
- Broccolo, F.; Drago, F.; Ciccarese, G.; Genoni, A.; Puggioni, A.; Rosa, G.M.; Parodi, A.; Manukyan, H.; Laassri, M.; Chumakov, K.; et al. Severe atypical hand-foot-and-mouth disease in adults due to coxsackievirus A6: Clinical presentation and phylogenesis of CV-A6 strains. J. Clin. Virol. 2019, 110, 1–6. [Google Scholar] [CrossRef]
- Lau, S.K.P.; Zhao, P.S.H.; Sridhar, S.; Yip, C.C.Y.; Aw-Yong, K.L.; Chow, E.Y.Y.; Cheung, K.C.M.; Hui, R.W.H.; Leung, R.Y.H.; Lai, Y.S.K.; et al. Molecular epidemiology of coxsackievirus A6 circulating in Hong Kong reveals common neurological manifestations and emergence of novel recombinant groups. J. Clin. Virol. 2018, 108, 43–49. [Google Scholar] [CrossRef]
- Wang, J.; Liu, T.; Gu, S.; Yang, H.H.; Xie, W.; Gao, C.; Gu, D. Cytoplasm Hydrogelation-Mediated Cardiomyocyte Sponge Alleviated Coxsackievirus B3 Infection. Nano Lett. 2023, 23, 8881–8890. [Google Scholar] [CrossRef]
- Yuan, C.; Zhou, J.; Yuan, L.; Dong, R.; Yang, X.; Li, S.; Liu, J.; Wu, J.; Wang, Y.; Chen, Y.; et al. A 2B Protein-Derived Peptide Effectively Inhibits Coxsackievirus B3 Infection. FASEB J. 2025, 39, e70915. [Google Scholar] [CrossRef]
- Peischard, S.; Ho, H.T.; Theiss, C.; Strutz-Seebohm, N.; Seebohm, G. A Kidnapping Story: How Coxsackievirus B3 and Its Host Cell Interact. Cell. Physiol. Biochem. 2019, 53, 121–140. [Google Scholar] [CrossRef]
- Wessels, E.; Duijsings, D.; Lanke, K.H.; Melchers, W.J.; Jackson, C.L.; van Kuppeveld, F.J. Molecular determinants of the interaction between coxsackievirus protein 3A and guanine nucleotide exchange factor GBF1. J. Virol. 2007, 81, 5238–5245. [Google Scholar] [CrossRef] [PubMed]
- Vuorinen, T.; Vainionp, R.; Heino, J.; Hyypi, T. Enterovirus receptors and virus replication in human leukocytes. J. Gen. Virol. 1999, 80 Pt 4, 921–927. [Google Scholar] [CrossRef]
- Wang, Y.J.; Sun, T.; Xue, S.T.; Cai, Z.D.; Yi, H.; Lv, M.; Kou, S.B.; Liu, R.; Peng, X.Z.; Li, Z.R. A Novel Class of Multi-substituted Diaryl Scaffold Derivatives Inhibit Glioblastoma Progression by Targeting CD155. Adv. Sci. 2025, 12, e06688. [Google Scholar] [CrossRef] [PubMed]
- Dawson, K.L.D.; Seuberlich, T.; Pesavento, P.A. Neurotropic enteric viruses in animals: Comparative research, knowledge gaps, and the role of pathology. Vet. Pathol. 2025; Online ahead of print. [Google Scholar] [CrossRef]
- Kramarov, S.; Palatna, L.; Shpak, I.; Seriakova, I.; Zakordonets, L.; Verbova, L.; Molodetskyi, O.; Myroniak, L.; Isayenko, T. Acute Transverse Myelitis in a Child Following Oral Live Polio Vaccine Administration. Int. Med. Case Rep. J. 2025, 18, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Grizer, C.S.; Messacar, K.; Mattapallil, J.J. Enterovirus-D68—A Reemerging Non-Polio Enterovirus that Causes Severe Respira-tory and Neurological Disease in Children. Front. Virol. 2024, 4, 1328457. [Google Scholar]
- Laksono, B.M.; Sooksawasdi Na Ayudhya, S.; Aguilar-Bretones, M.; Embregts, C.W.E.; van Nierop, G.P.; van Riel, D. Human B cells and dendritic cells are susceptible and permissive to enterovirus D68 infection. mSphere 2024, 9, e0052623. [Google Scholar] [CrossRef]
- Aguglia, G.; Coyne, C.B.; Dermody, T.S.; Williams, J.V.; Freeman, M.C. Contemporary enterovirus-D68 isolates infect human spinal cord organoids. mBio 2023, 14, e0105823. [Google Scholar] [CrossRef]
- Pereirinha da Silva, A.K.; van Trijp, J.P.; Montenarie, A.; Fok, J.A.; Sooksawasdi Na Ayudhya, S.; Pieters, R.J.; Boons, G.J.; van Riel, D.; de Vries, R.P.; Bauer, L. Sialic Acid-Containing Glycolipids Extend the Receptor Repertoire of Enterovirus-D68. ACS Infect. Dis. 2025, 11, 2090–2103. [Google Scholar] [CrossRef]
- Lizasoain, A.; Mir, D.; Salvo, M.; Bortagaray, V.; Masachessi, G.; Farías, A.; Rodríguez-Osorio, N.; Nates, S.; Victoria, M.; Colina, R. First evidence of enterovirus A71 and echovirus 30 in Uruguay and genetic relationship with strains circulating in the South American region. PLoS ONE 2021, 16, e0255846. [Google Scholar] [CrossRef]
- de Schrijver, S.; Vanhulle, E.; Ingenbleek, A.; Alexakis, L.; Johannesen, C.K.; Broberg, E.K.; Harvala, H.; Fischer, T.K.; Benschop, K.S.M. Epidemiological and Clinical Insights into Enterovirus Circulation in Europe, 2018-2023: A Multicenter Retrospective Surveillance Study. J. Infect. Dis. 2025, 232, e104–e115. [Google Scholar] [CrossRef]
- Vlok, M.; Majer, A. Global Prevalence of Non-Polio Enteroviruses Pre- and Post COVID-19 Pandemic. Microorganisms 2025, 13, 1801. [Google Scholar] [CrossRef]
- Yang, T.; Sun, Q.; Liu, H.; Yang, M.; Chen, S.; Sun, W.; Xu, J.; Yan, D.; Zhu, S.; Han, Z.; et al. Characteristics of CVA16 B1c strains isolated for the first time in the Heilongjiang Province of China. Front. Microbiol. 2025, 16, 1634547. [Google Scholar] [CrossRef]
- Abzug, M.J. The enteroviruses: Problems in need of treatments. J. Infect. 2014, 68 (Suppl. S1), S108–S114. [Google Scholar] [CrossRef]
- Cevallos, C.; Jarmoluk, P.; Sviercz, F.; Freiberger, R.N.; López, C.A.M.; Delpino, M.V.; Quarleri, J. Ferroptosis and mitochondrial ROS are central to SARS-CoV-2-induced hepatocyte death. Front. Cell. Infect. Microbiol. 2025, 15, 1625928. [Google Scholar] [CrossRef]
- Chen, Q.; Zhang, F.; Bai, J.; Che, Q.; Xiang, L.; Zhang, Z.; Wang, Y.; Sjöling, Å.; Martín-Rodríguez, A.J.; Zhu, B.; et al. Bacteriophage-resistant carbapenem-resistant Klebsiella pneumoniae shows reduced antibiotic resistance and virulence. Int. J. Antimicrob. Agents 2024, 64, 107221. [Google Scholar] [CrossRef]
- Yuan, Y.; Zu, S.; Zhang, Y.; Zhao, F.; Jin, X.; Hu, H. Porcine Deltacoronavirus Utilizes Sialic Acid as an Attachment Receptor and Trypsin Can Influence the Binding Activity. Viruses 2021, 13, 2442. [Google Scholar] [CrossRef]
- Xu, Z.S.; Du, W.T.; Wang, S.Y.; Wang, M.Y.; Yang, Y.N.; Li, Y.H.; Li, Z.Q.; Zhao, L.X.; Yang, Y.; Luo, W.W.; et al. LDLR is an entry receptor for Crimean-Congo hemorrhagic fever virus. Cell Res. 2024, 34, 140–150. [Google Scholar] [CrossRef]
- Hamidi, M.; Ong, K.C.; Tan, S.H.; Wong, K.T. An Intracerebrally-Infected Mouse Model of Enterovirus A71 Demonstrates Restricted Inter-Neuronal Spread Within the Brain Parenchyma Despite Strong SCARB2 Expression. Neuropathol. Appl. Neurobiol. 2025, 51, e70031. [Google Scholar] [CrossRef]
- Wang, W.G.; Wang, X.; Li, N.; Kuang, D.X.; Tong, P.F.; Lu, C.X.; Han, Y.Y.; Sun, X.M.; Dai, J.J.; Liu, L.D. EV-A71 invades the central nervous system and affects the blood-brain barrier in a tree shrew model. Front. Immunol. 2025, 16, 1583768. [Google Scholar] [CrossRef]
- Wang, X.; Qian, J.; Mi, Y.; Li, Y.; Cao, Y.; Qiao, K. Correlations of PSGL-1 VNTR polymorphism with the susceptibility to severe HFMD associated with EV-71 and the immune status after infection. Virol. J. 2024, 21, 187. [Google Scholar] [CrossRef]
- Li, M.; Kong, X.P.; Liu, H.; Cheng, L.X.; Huang, J.L.; Quan, L.; Wu, F.Y.; Hao, B.; Liu, C.; Luo, B. Expression of EV71-VP1, PSGL-1 and SCARB2 in Tissues of Infants with Brain Stem Encephalitis. Fa Yi Xue Za Zhi 2015, 31, 97–101, 104. [Google Scholar]
- Yang, B.; Chuang, H.; Yang, K.D. Sialylated glycans as receptor and inhibitor of enterovirus 71 infection to DLD-1 intestinal cells. Virol. J. 2009, 6, 141. [Google Scholar] [CrossRef]
- Ke, X.; Zhang, Y.; Liu, Y.; Miao, Y.; Zheng, C.; Luo, D.; Sun, J.; Hu, Q.; Xu, Y.; Wang, H.; et al. A Single Mutation in the VP1 Gene of Enterovirus 71 Enhances Viral Binding to Heparan Sulfate and Impairs Viral Pathogenicity in Mice. Viruses 2020, 12, 883. [Google Scholar] [CrossRef]
- Kobayashi, K.; Sudaka, Y.; Takashino, A.; Imura, A.; Fujii, K.; Koike, S. Amino Acid Variation at VP1-145 of Enterovirus 71 Determines Attachment Receptor Usage and Neurovirulence in Human Scavenger Receptor B2 Transgenic Mice. J. Virol. 2018, 92, 10–1128. [Google Scholar] [CrossRef]
- Lui, Y.L.; Lin, Z.; Lee, J.J.; Chow, V.T.; Poh, C.L.; Tan, E.L. Beta-actin variant is necessary for Enterovirus 71 replication. Biochem. Biophys. Res. Commun. 2013, 433, 607–610. [Google Scholar] [CrossRef]
- Too, I.H.K.; Bonne, I.; Tan, E.L.; Chu, J.J.H.; Alonso, S. Prohibitin plays a critical role in Enterovirus 71 neuropathogenesis. PLoS Pathog. 2018, 14, e1006778. [Google Scholar] [CrossRef]
- Su, W.; Huang, S.; Zhu, H.; Zhang, B.; Wu, X. Interaction between PHB2 and Enterovirus A71 VP1 Induces Autophagy and Affects EV-A71 Infection. Viruses 2020, 12, 414. [Google Scholar] [CrossRef]
- He, Q.Q.; Ren, S.; Xia, Z.C.; Cheng, Z.K.; Peng, N.F.; Zhu, Y. Fibronectin Facilitates Enterovirus 71 Infection by Mediating Viral Entry. J. Virol. 2018, 92, 10–1128. [Google Scholar] [CrossRef]
- Wang, W.; Sun, J.; Wang, N.; Sun, Z.; Ma, Q.; Li, J.; Zhang, M.; Xu, J. Enterovirus A71 capsid protein VP1 increases blood-brain barrier permeability and virus receptor vimentin on the brain endothelial cells. J. Neurovirol. 2020, 26, 84–94. [Google Scholar] [CrossRef]
- Sridhar, A.; Depla, J.A.; Mulder, L.A.; Karelehto, E.; Brouwer, L.; Kruiswijk, L.; Vieira de Sá, R.; Meijer, A.; Evers, M.M.; van Kuppeveld, F.J.M.; et al. Enterovirus D68 Infection in Human Primary Airway and Brain Organoids: No Additional Role for Heparan Sulfate Binding for Neurotropism. Microbiol. Spectr. 2022, 10, e0169422. [Google Scholar] [CrossRef]
- Hixon, A.M.; Clarke, P.; Tyler, K.L. Contemporary Circulating Enterovirus D68 Strains Infect and Undergo Retrograde Axonal Transport in Spinal Motor Neurons Independent of Sialic Acid. J. Virol. 2019, 93, 10–1128. [Google Scholar] [CrossRef]
- Wei, W.; Guo, H.; Chang, J.; Yu, Y.; Liu, G.; Zhang, N.; Willard, S.H.; Zheng, S.; Yu, X.F. ICAM-5/Telencephalin Is a Functional Entry Receptor for Enterovirus D68. Cell Host Microbe 2016, 20, 631–641. [Google Scholar] [CrossRef]
- Baggen, J.; Liu, Y.; Lyoo, H.; van Vliet, A.L.W.; Wahedi, M.; de Bruin, J.W.; Roberts, R.W.; Overduin, P.; Meijer, A.; Rossmann, M.G.; et al. Bypassing pan-enterovirus host factor PLA2G16. Nat. Commun. 2019, 10, 3171. [Google Scholar] [CrossRef]
- Nakamura, M.; Uehara, Y.; Asada, M.; Honda, E.; Nagai, N.; Kimata, K.; Suzuki, M.; Imamura, T. Sulfated glycosaminoglycans are required for specific and sensitive fibroblast growth factor (FGF) 19 signaling via FGF receptor 4 and betaKlotho. J. Biol. Chem. 2011, 286, 26418–26423. [Google Scholar] [CrossRef]
- Varanese, L.; Xu, L.; Peters, C.E.; Pintilie, G.; Roberts, D.S.; Raj, S.; Liu, M.; Ooi, Y.S.; Diep, J.; Qiao, W.; et al. MFSD6 is an entry receptor for enterovirus D68. Nature 2025, 641, 1268–1275. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Li, H.; Liu, X.; Zhou, J.; Gao, D.; Yang, W.; Xia, H.; Dou, C.; Yu, Z.; Guo, H.; et al. Characterisation of a secreted MFSD6-Fc microbody as a decoy receptor for respiratory enterovirus D68. eBioMedicine 2025, 120, 105915. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Li, H.; Li, Z.; Gao, D.; Zhou, J.; Ni, F.; Yu, Q.; Huang, Y.; Tang, Y.; Xue, L.; et al. MFSD6 is an entry receptor for respiratory enterovirus D68. Cell Host Microbe 2025, 33, 267–278.e4. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Zeng, S.; Ji, X.; Meng, X.; Lei, N.; Yang, H.; Mu, X. Type I Interferon-Induced TMEM106A Blocks Attachment of EV-A71 Virus by Interacting With the Membrane Protein SCARB2. Front. Immunol. 2022, 13, 817835. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, Q.; Liu, C.; Wang, G.; Song, H.; Shang, G.; Peng, R.; Qu, X.; Liu, S.; Cui, Y.; et al. Molecular basis of differential receptor usage for naturally occurring CD55-binding and -nonbinding coxsackievirus B3 strains. Proc. Natl. Acad. Sci. USA 2022, 119, e2118590119. [Google Scholar] [CrossRef]
- Bastea, L.I.; Liu, X.; Fleming, A.K.; Pandey, V.; Döppler, H.; Edenfield, B.H.; Krishna, M.; Zhang, L.; Thompson, E.A.; Grandgenett, P.M.; et al. Coxsackievirus and adenovirus receptor expression facilitates enteroviral infections to drive the development of pancreatic cancer. Nat. Commun. 2024, 15, 10547. [Google Scholar] [CrossRef]
- Feng, M.; Ma, Q.; Zhang, B.; Chen, Y.; Yang, Y.; He, X.; Zeng, Y.; Jing, M.; Ou, X.; Liu, Y.; et al. Targeting the poliovirus receptor to activate T cells and induce myeloid-derived suppressor cells to differentiate to pro-inflammatory macrophages via the IFN-γ-p-STAT1-IRF8 axis in cancer therapy. Cell Death Differ. 2025, 2, 1791–1805. [Google Scholar] [CrossRef]
- Wei, M.; Meng, F.; Wang, S.; Li, J.; Zhang, Y.; Mao, Q.; Hu, Y.; Liu, P.; Shi, N.; Tao, H.; et al. 2-Year Efficacy, Immunogenicity, and Safety of Vigoo Enterovirus 71 Vaccine in Healthy Chinese Children: A Randomized Open-Label Study. J. Infect. Dis. 2017, 215, 56–63. [Google Scholar] [CrossRef]
- Liang, Z.L.; Mao, Q.Y.; Wang, Y.P.; Zhu, F.C.; Li, J.X.; Yao, X.; Gao, F.; Wu, X.; Xu, M.; Wang, J.Z. Progress on the research and development of inactivated EV71 whole-virus vaccines. Hum. Vaccines Immunother. 2013, 9, 1701–1705. [Google Scholar] [CrossRef]
- Warner, N.L.; Archer, J.; Park, S.; Singh, G.; McFadden, K.M.; Kimura, T.; Nicholes, K.; Simpson, A.; Hawman, D.W.; Feldmann, H.; et al. A self-amplifying RNA vaccine prevents enterovirus D68 infection and disease in preclin-ical models. Sci. Transl. Med. 2024, 16, eadi1625. [Google Scholar] [CrossRef]
- Cheng, J.; Krug, P.W.; Lei, H.; Moss, D.L.; Lang, Z.C.; Morton, A.J.; Shen, C.-H.; Pletnev, S.; Huang, R.K.; Pierson, T.C.; et al. Structural insights from vaccine candidates for EV-D68. Commun. Biol. 2025, 8, 860. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.H.; Chong, W.L.; Lee, V.S.; Abdullah, S.; Jasni, K.; Suarni, S.Q.; Perera, D.; Sam, I.C.; Chan, Y.F. Substitution of Coxsackievirus A16 VP1 BC and EF Loop Altered the Protective Immune Responses in Chimera Enterovirus A71. Vaccines 2023, 11, 1363. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Xie, T.; Li, H.; Song, X.; Yue, L.; Wang, X.; Shen, D.; Ma, K.; Jiang, Q.; Long, R.; et al. Immune responses of a CV-A16 live attenuated candidate strain and its protective effects in rhesus monkeys. Emerg. Microbes Infect. 2020, 9, 2136–2146. [Google Scholar] [CrossRef] [PubMed]
- Yew, J.S.; Ong, S.K.; Lim, H.X.; Tan, S.H.; Ong, K.C.; Wong, K.T.; Poh, C.L. Immunogenicity of trivalent DNA vaccine candidate encapsulated in Chitosan-TPP nanoparticles against EV-A71 and CV-A16. Nanomedicine 2024, 19, 1779–1799. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, Y.; Mao, N.; Zhu, S.; Ji, T.; Xu, W. Intranasal immunization with coxsackievirus A16 virus-like particles confers protection against lethal infection in neonatal mice. Arch. Virol. 2019, 164, 2975–2984. [Google Scholar] [CrossRef]
- Mao, Q.; Wang, Y.; Bian, L.; Xu, M.; Liang, Z. EV-A71 vaccine licensure: A first step for multivalent enterovirus vaccine to control HFMD and other severe diseases. Emerg. Microbes Infect. 2016, 5, e75. [Google Scholar] [CrossRef]
- Godin, A.; Brickley, E.B.; Connor, R.I.; Wieland-Alter, W.F.; Weiner, J.A.; Ackerman, M.E.; Modlin, J.F.; Sajjad, O.M.; Arita, M.; Gast, C.; et al. Intestinal mucosal immune responses to novel oral poliovirus vaccine type 2 in healthy newborns. Clin. Infect. Dis. 2025, ciaf484. [Google Scholar] [CrossRef]
- MacLeod, D.A.; Tobin, J.K.; Bushnell, R.V.; Wiggins, T.J.; Ts, S.; Nadipelly, R.; Lawson, S.; Pillai, V.V.; Tobin, G.J.; Dollery, S.J. Immune and Safety Analysis of ultraIPV(TM), a Novel UVC-Inactivated Polio Vaccine. Viruses 2025, 17, 915. [Google Scholar] [CrossRef]
- Liang, J.; Zhang, Q.; Li, Y.; Wang, L. Advances and challenges in poliomyelitis vaccines: A comprehensive review of development, production, and global deployment. Front. Public Health 2025, 13, 1611028. [Google Scholar] [CrossRef]
- Ogieuhi, I.J.; Ajekiigbe, V.O.; Aremu, S.O.; Okpujie, V.; Bassey, P.U.; Babalola, A.E.; Gbolagade-Jonathan, P.; Anthony, C.S.; Bakare, I.S. Global partnerships in combating tropical diseases: Assessing the impact of a U.S. withdrawal from the WHO. Trop. Med. Health 2025, 53, 36. [Google Scholar] [CrossRef]
- Zuckerman, N.S.; Lustig, Y.; Sofer, D.; Shulman, L.M.; Weiss, L.; Vasserman, R.; Gabai, R.; Friedman, K.; Eliyahu, H.; Bar-Liss, N.; et al. Early detection of a circulating pre-vaccine-derived poliovirus type 1 (pre-VDPV1) variant linked to an acute flaccid polio case prior to VDPV1 emergence, Israel, 2024 to 2025. Euro Surveill. 2025, 30, 2500605. [Google Scholar] [CrossRef] [PubMed]
- Mercer, L.D.; Seña, A.C.; Colgate, E.R.; Crothers, J.W.; Wright, P.F.; Al-Ibrahim, M.; Tritama, E.; Vincent, A.; Mainou, B.A.; Zhang, Y.; et al. Safety and immunogenicity of novel live attenuated type 1 and type 3 oral poliomyelitis vaccines in healthy adults in the USA: A first-in-human, observer-masked, multicentre, phase 1 randomised controlled trial. Lancet Infect. Dis. 2025; Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Cheng, Z.; Chen, J.; Qian, L.; Wang, H.; Liu, Y. Advances in human norovirus research: Vaccines, genotype distribution and antiviral strategies. Virus Res. 2024, 350, 199486. [Google Scholar] [CrossRef] [PubMed]
- Seo, S.H.; Choi, J.A.; Yang, E.; Park, H.; Jung, D.I.; Kim, J.O.; Yang, J.S.; Song, M. Mouse strain-dependent neutralizing antibody responses to Zika virus vaccines. J. Microbiol. 2025, 63, e2504005. [Google Scholar] [CrossRef]
- Thornhill-Wadolowski, E.; Ruter, D.L.; Yan, F.; Gajera, M.; Kurt, E.; Samanta, L.; Leigh, K.; Zhu, J.; Guo, Z.; Wang, Z.; et al. Development of an Influenza/COVID-19 Combination mRNA Vaccine Containing a Novel Multivalent Antigen Design That Enhances Immunogenicity of Influenza Virus B Hemagglutinins. Vaccines 2025, 13, 628. [Google Scholar] [CrossRef]
- Calvin, B.Z.; Géorcelin, A.G.; Phillipe, B.E.K.; Pascal, O.A.; Laure, M.F.A.; Joyce, K.W.J.; Laure, N.E.; Blaise, A.A.G.; Bertrand, D.A.; Sylvie, H.-A.M. The Anti-parasitic Effect of Extract of Ceiba pentandra (L.) Gaertn Is Related to Its Anti-inflammatory, Analgesic and Anthelmintic Activities on Haemonchus contortus. Clin. Complement. Med. Pharmacol. 2023, 3, 100088. [Google Scholar] [CrossRef]
- Bin-Asal, F.S.N.; Saeed, A.A.M.; Yahia, A.-R.A.B. Ceropegia variegata: Phytochemical profiling, antioxidant prowess, and antimicrobial potential. Clin. Tradit. Med. Pharmacol. 2025, 6, 200194. [Google Scholar] [CrossRef]
| Receptor | Distribution | Function | Type | Ref. |
|---|---|---|---|---|
| Sialic acid (SIA) | SIA is widely present on the termini of glycoproteins and glycolipids across numerous cell types and serves as the primary receptor for most EV-D68 strains. | Binds to viral capsid proteins, mediating viral attachment and entry; facilitates viral uncoating and genome release into the cytoplasm. | Primary entry receptor | [42,66] |
| Intercellular adhesion molecule-5 (ICAM-5) | Predominantly expressed in neurons. | Expression level correlates strongly with viral infectivity and tropism; mediates efficient entry and infection in neuronal cells. | Functional receptor | [67,68] |
| Sulfated glycosaminoglycans (sGAGs) | Expressed on the surface of various cell types, including neural and epithelial cells. | Enhances viral concentration on the cell surface, promoting attachment and increasing infection efficiency; acts as a co-receptor. | Attachment factor/Co-receptor | [69,70] |
| Major facilitator superfamily-domain-containing protein 6 (MFSD6) | Membrene protein expressed on the human respiratory cell lines (Calu-3, BEAS-2B, A549), primary human bronchial epithelial cells (HBECs), etc. | Acts as a key cellular receptor for EV-D68, mediating viral entry into host cells | Entry receptor | [71,72,73] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Maisimu, M.; Ge, Z.; Xiao, S.; Wang, H. The Pathogenesis and Virulence of the Major Enterovirus Pathogens Associated with Severe Clinical Manifestations: A Comprehensive Review. Cells 2025, 14, 1617. https://doi.org/10.3390/cells14201617
Liu Y, Maisimu M, Ge Z, Xiao S, Wang H. The Pathogenesis and Virulence of the Major Enterovirus Pathogens Associated with Severe Clinical Manifestations: A Comprehensive Review. Cells. 2025; 14(20):1617. https://doi.org/10.3390/cells14201617
Chicago/Turabian StyleLiu, Yuwei, Maiheliya Maisimu, Zhihang Ge, Suling Xiao, and Haoran Wang. 2025. "The Pathogenesis and Virulence of the Major Enterovirus Pathogens Associated with Severe Clinical Manifestations: A Comprehensive Review" Cells 14, no. 20: 1617. https://doi.org/10.3390/cells14201617
APA StyleLiu, Y., Maisimu, M., Ge, Z., Xiao, S., & Wang, H. (2025). The Pathogenesis and Virulence of the Major Enterovirus Pathogens Associated with Severe Clinical Manifestations: A Comprehensive Review. Cells, 14(20), 1617. https://doi.org/10.3390/cells14201617






