Modifier Genes in Microcephaly: A Report on WDR62, CEP63, RAD50 and PCNT Variants Exacerbating Disease Caused by Biallelic Mutations of ASPM and CENPJ
Abstract
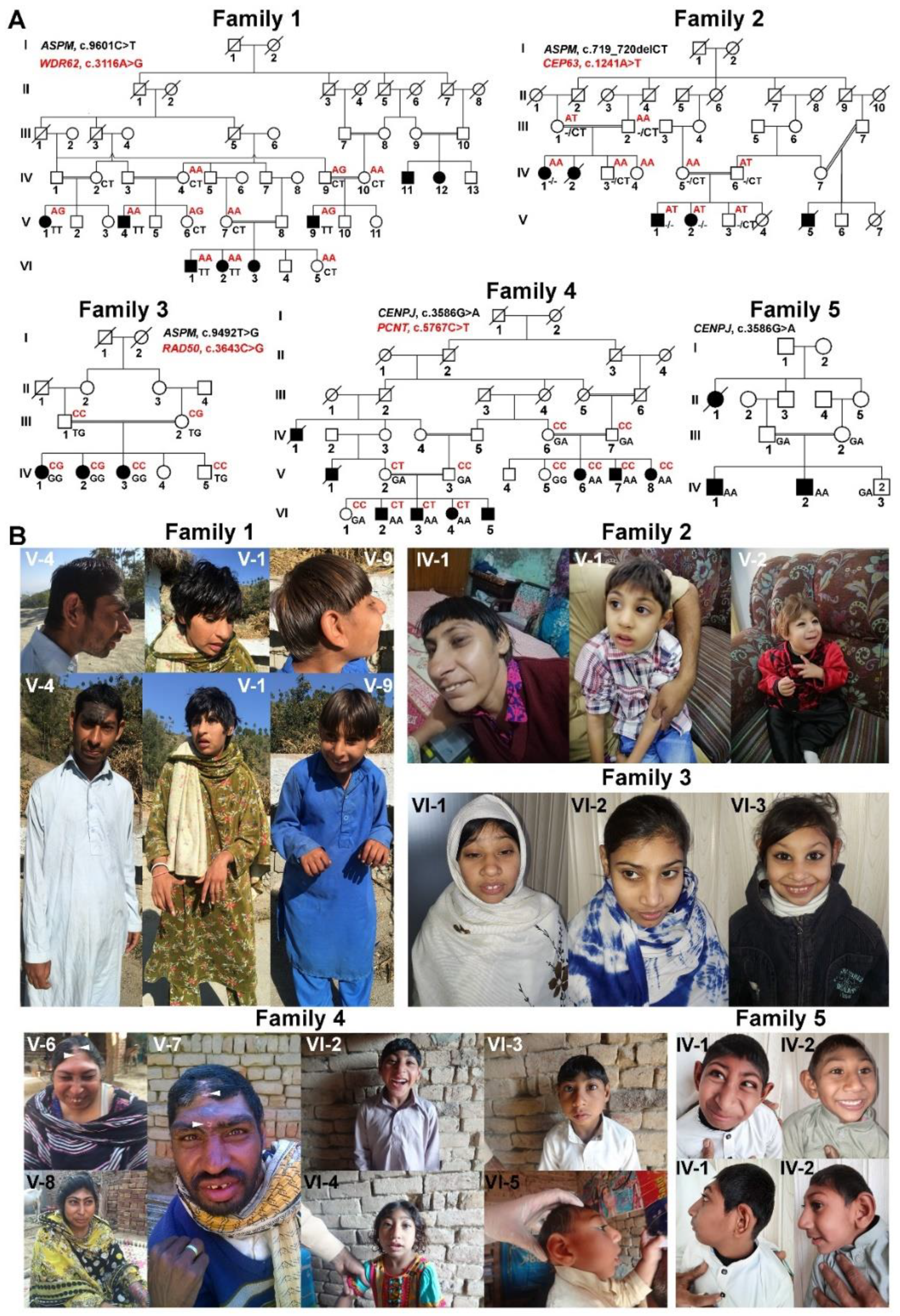
:1. Introduction
2. Materials and Methods
2.1. Clinical Manifestations
2.2. Next-Generation Sequencing
2.3. Linkage Analysis
2.4. Sanger Sequencing
2.5. In Silico Analyses of Identified Variants
2.6. Reverse Transcription PCR
2.7. Immunocytochemistry
2.8. Immunoblotting
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- von der Hagen, M. Diagnostic approach to primary microcephaly. Neuropediatrics 2017, 48, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Abuelo, D. Microcephaly syndromes. Semin. Pediatr. Neurol. 2007, 14, 118–127. [Google Scholar] [CrossRef]
- Jean, F.; Stuart, A.; Tarailo-Graovac, M. Dissecting the Genetic and Etiological Causes of Primary Microcephaly. Front. Neurol. 2020, 11, 570830. [Google Scholar] [CrossRef]
- Farooq, M.; Lindbaek, L.; Krogh, N.; Doganli, C.; Keller, C.; Monnich, M.; Goncalves, A.B.; Sakthivel, S.; Mang, Y.; Fatima, A.; et al. RRP7A links primary microcephaly to dysfunction of ribosome biogenesis, resorption of primary cilia, and neurogenesis. Nat. Commun. 2020, 11, 5816. [Google Scholar] [CrossRef]
- Parry, D.A.; Martin, C.A.; Greene, P.; Marsh, J.A.; Genomics England Research, C.; Blyth, M.; Cox, H.; Donnelly, D.; Greenhalgh, L.; Greville-Heygate, S.; et al. Heterozygous lamin B1 and lamin B2 variants cause primary microcephaly and define a novel laminopathy. Genet. Med. 2021, 23, 408–414. [Google Scholar] [CrossRef]
- Shaheen, R.; Maddirevula, S.; Ewida, N.; Alsahli, S.; Abdel-Salam, G.M.H.; Zaki, M.S.; Tala, S.A.; Alhashem, A.; Softah, A.; Al-Owain, M.; et al. Genomic and phenotypic delineation of congenital microcephaly. Genet. Med. 2019, 21, 545–552. [Google Scholar] [CrossRef]
- Jayaraman, D.; Bae, B.I.; Walsh, C.A. The Genetics of Primary Microcephaly. Annu. Rev. Genom. Hum. Genet. 2018, 19, 177–200. [Google Scholar] [CrossRef] [Green Version]
- Rauch, A.; Thiel, C.T.; Schindler, D.; Wick, U.; Crow, Y.J.; Ekici, A.B.; van Essen, A.J.; Goecke, T.O.; Al-Gazali, L.; Chrzanowska, K.H.; et al. Mutations in the pericentrin (PCNT) gene cause primordial dwarfism. Science 2008, 319, 816–819. [Google Scholar] [CrossRef]
- Sajid Hussain, M.; Marriam Bakhtiar, S.; Farooq, M.; Anjum, I.; Janzen, E.; Reza Toliat, M.; Eiberg, H.; Kjaer, K.W.; Tommerup, N.; Noegel, A.A.; et al. Genetic heterogeneity in Pakistani microcephaly families. Clin. Genet. 2013, 83, 446–451. [Google Scholar] [CrossRef] [PubMed]
- Rasool, S.; Baig, J.M.; Moawia, A.; Ahmad, I.; Iqbal, M.; Waseem, S.S.; Asif, M.; Abdullah, U.; Makhdoom, E.U.H.; Kaygusuz, E.; et al. An update of pathogenic variants in ASPM, WDR62, CDK5RAP2, STIL, CENPJ, and CEP135 underlying autosomal recessive primary microcephaly in 32 consanguineous families from Pakistan. Mol. Genet. Genom. Med. 2020, 8, e1408. [Google Scholar] [CrossRef]
- Hou, J.; van Leeuwen, J.; Andrews, B.J.; Boone, C. Genetic Network Complexity Shapes Background-Dependent Phenotypic Expression. Trends Genet. 2018, 34, 578–586. [Google Scholar] [CrossRef]
- Rahit, K.; Tarailo-Graovac, M. Genetic Modifiers and Rare Mendelian Disease. Genes 2020, 11, 239. [Google Scholar] [CrossRef] [Green Version]
- Crawford, H.; Scerif, G.; Wilde, L.; Beggs, A.; Stockton, J.; Sandhu, P.; Shelley, L.; Oliver, C.; McCleery, J. Genetic modifiers in rare disorders: The case of fragile X syndrome. Eur. J. Hum. Genet. 2020, 29, 173–183. [Google Scholar] [CrossRef]
- Niemi, M.E.; Martin, H.C.; Rice, D.L.; Gallone, G.; Gordon, S.; Kelemen, M.; McAloney, K.; McRae, J.; Radford, E.J.; Yu, S. Common genetic variants contribute to risk of rare severe neurodevelopmental disorders. Nature 2018, 562, 268–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McTague, A.; Howell, K.B.; Cross, J.H.; Kurian, M.A.; Scheffer, I.E. The genetic landscape of the epileptic encephalopathies of infancy and childhood. Lancet Neurol. 2016, 15, 304–316. [Google Scholar] [CrossRef]
- Gaily, E.; Anttonen, A.K.; Valanne, L.; Liukkonen, E.; Träskelin, A.L.; Polvi, A.; Lommi, M.; Muona, M.; Eriksson, K.; Lehesjoki, A.E. Dravet syndrome: New potential genetic modifiers, imaging abnormalities, and ictal findings. Epilepsia 2013, 54, 1577–1585. [Google Scholar] [CrossRef] [PubMed]
- Poulton, C.J.; Schot, R.; Seufert, K.; Lequin, M.H.; Accogli, A.; Annunzio, G.D.; Villard, L.; Philip, N.; de Coo, R.; Catsman-Berrevoets, C.; et al. Severe presentation of WDR62 mutation: Is there a role for modifying genetic factors? Am. J. Med. Genet. Part A 2014, 164A, 2161–2171. [Google Scholar] [CrossRef] [PubMed]
- Snedeker, J.; Gibbons Jr, W.J.; Paulding, D.F.; Abdelhamed, Z.; Prows, D.R.; Stottmann, R.W. Gpr63 is a modifier of microcephaly in Ttc21b mouse mutants. PLoS Genet. 2019, 15, e1008467. [Google Scholar] [CrossRef]
- Jayaraman, D.; Kodani, A.; Gonzalez, D.M.; Mancias, J.D.; Mochida, G.H.; Vagnoni, C.; Johnson, J.; Krogan, N.; Harper, J.W.; Reiter, J.F.; et al. Microcephaly Proteins Wdr62 and Aspm Define a Mother Centriole Complex Regulating Centriole Biogenesis, Apical Complex, and Cell Fate. Neuron 2016, 92, 813–828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hussain, M.S.; Baig, S.M.; Neumann, S.; Peche, V.S.; Szczepanski, S.; Nurnberg, G.; Tariq, M.; Jameel, M.; Khan, T.N.; Fatima, A.; et al. CDK6 associates with the centrosome during mitosis and is mutated in a large Pakistani family with primary microcephaly. Hum. Mol. Genet. 2013, 22, 5199–5214. [Google Scholar] [CrossRef] [PubMed]
- Thiele, H.; Nurnberg, P. HaploPainter: A tool for drawing pedigrees with complex haplotypes. Bioinformatics 2005, 21, 1730–1732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmad, I.; Baig, S.M.; Abdulkareem, A.R.; Hussain, M.S.; Sur, I.; Toliat, M.R.; Nurnberg, G.; Dalibor, N.; Moawia, A.; Waseem, S.S.; et al. Genetic heterogeneity in Pakistani microcephaly families revisited. Clin. Genet. 2017, 92, 62–68. [Google Scholar] [CrossRef]
- Hussain, M.S.; Baig, S.M.; Neumann, S.; Nurnberg, G.; Farooq, M.; Ahmad, I.; Alef, T.; Hennies, H.C.; Technau, M.; Altmuller, J.; et al. A truncating mutation of CEP135 causes primary microcephaly and disturbed centrosomal function. Am. J. Hum. Genet. 2012, 90, 871–878. [Google Scholar] [CrossRef] [Green Version]
- Gabriel, E.; Wason, A.; Ramani, A.; Gooi, L.M.; Keller, P.; Pozniakovsky, A.; Poser, I.; Noack, F.; Telugu, N.S.; Calegari, F.; et al. CPAP promotes timely cilium disassembly to maintain neural progenitor pool. EMBO J. 2016, 35, 803–819. [Google Scholar] [CrossRef]
- Kilmartin, J.V.; Wright, B.; Milstein, C. Rat monoclonal antitubulin antibodies derived by using a new nonsecreting rat cell line. J. Cell Biol. 1982, 93, 576–582. [Google Scholar] [CrossRef]
- Olsen, J.V.; Vermeulen, M.; Santamaria, A.; Kumar, C.; Miller, M.L.; Jensen, L.J.; Gnad, F.; Cox, J.; Jensen, T.S.; Nigg, E.A.; et al. Quantitative Phosphoproteomics Reveals Widespread Full Phosphorylation Site Occupancy During Mitosis. Sci. Signal. 2010, 3, ra3. [Google Scholar] [CrossRef]
- Nicholas, A.K.; Khurshid, M.; Desir, J.; Carvalho, O.P.; Cox, J.J.; Thornton, G.; Kausar, R.; Ansar, M.; Ahmad, W.; Verloes, A.; et al. WDR62 is associated with the spindle pole and is mutated in human microcephaly. Nat. Genet. 2010, 42, 1010–1014. [Google Scholar] [CrossRef]
- Yu, T.W.; Mochida, G.H.; Tischfield, D.J.; Sgaier, S.K.; Flores-Sarnat, L.; Sergi, C.M.; Topcu, M.; McDonald, M.T.; Barry, B.J.; Felie, J.M.; et al. Mutations in WDR62, encoding a centrosome-associated protein, cause microcephaly with simplified gyri and abnormal cortical architecture. Nat. Genet. 2010, 42, 1015–1020. [Google Scholar] [CrossRef] [Green Version]
- Sir, J.H.; Barr, A.R.; Nicholas, A.K.; Carvalho, O.P.; Khurshid, M.; Sossick, A.; Reichelt, S.; D’Santos, C.; Woods, C.G.; Gergely, F. A primary microcephaly protein complex forms a ring around parental centrioles. Nat. Genet. 2011, 43, 1147–1153. [Google Scholar] [CrossRef] [Green Version]
- Waltes, R.; Kalb, R.; Gatei, M.; Kijas, A.W.; Stumm, M.; Sobeck, A.; Wieland, B.; Varon, R.; Lerenthal, Y.; Lavin, M.F.; et al. Human RAD50 Deficiency in a Nijmegen Breakage Syndrome-like Disorder. Am. J. Hum. Genet. 2009, 84, 605–616. [Google Scholar] [CrossRef] [Green Version]
- Willems, M.; Genevieve, D.; Borck, G.; Baumann, C.; Baujat, G.; Bieth, E.; Edery, P.; Farra, C.; Gerard, M.; Heron, D.; et al. Molecular analysis of pericentrin gene (PCNT) in a series of 24 Seckel/microcephalic osteodysplastic primordial dwarfism type II (MOPD II) families. J. Med. Genet. 2010, 47, 797–802. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Paull, T.T. Direct activation of the ATM protein kinase by the Mre11/Rad50/Nbs1 complex. Science 2004, 304, 93–96. [Google Scholar] [CrossRef]
- Tang, C.J.; Lin, S.Y.; Hsu, W.B.; Lin, Y.N.; Wu, C.T.; Lin, Y.C.; Chang, C.W.; Wu, K.S.; Tang, T.K. The human microcephaly protein STIL interacts with CPAP and is required for procentriole formation. EMBO J. 2011, 30, 4790–4804. [Google Scholar] [CrossRef] [Green Version]
- Zheng, X.; Gooi, L.M.; Wason, A.; Gabriel, E.; Mehrjardi, N.Z.; Yang, Q.; Zhang, X.; Debec, A.; Basiri, M.L.; Avidor-Reiss, T.; et al. Conserved TCP domain of Sas-4/CPAP is essential for pericentriolar material tethering during centrosome biogenesis. Proc. Natl. Acad. Sci. USA 2014, 111, E354–E363. [Google Scholar] [CrossRef] [Green Version]
- Bond, J.; Roberts, E.; Springell, K.; Lizarraga, S.B.; Scott, S.; Higgins, J.; Hampshire, D.J.; Morrison, E.E.; Leal, G.F.; Silva, E.O.; et al. A centrosomal mechanism involving CDK5RAP2 and CENPJ controls brain size. Nat. Genet. 2005, 37, 353–355. [Google Scholar] [CrossRef]
- Yigit, G.; Brown, K.E.; Kayserili, H.; Pohl, E.; Caliebe, A.; Zahnleiter, D.; Rosser, E.; Bogershausen, N.; Uyguner, Z.O.; Altunoglu, U.; et al. Mutations in CDK5RAP2 cause Seckel syndrome. Mol. Genet. Genom. Med. 2015, 3, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Duerinckx, S.; Jacquemin, V.; Drunat, S.; Vial, Y.; Passemard, S.; Perazzolo, C.; Massart, A.; Soblet, J.; Racape, J.; Desmyter, L.; et al. Digenic inheritance of human primary microcephaly delineates centrosomal and non-centrosomal pathways. Hum. Mutat. 2020, 41, 512–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| (a) | ||||||||||||
| Family 1 | Family 2 | Family 3 | ||||||||||
| Patient ID | VI-1 | VI-2 | VI-3 | V-4 | V-1 | V-9 | IV-1 | V-1 | V-2 | IV-1 | IV-2 | IV-3 |
| Gene 1 | ||||||||||||
| Gene name | ASPM | ASPM | ASPM | ASPM | ASPM | ASPM | ASPM | ASPM | ASPM | ASPM | ASPM | ASPM |
| Zygosity | Homo | Homo | Homo | Homo | Homo | Homo | Homo | Homo | Homo | Homo | Homo | Homo |
| cDNA mutation | c.9601C>T | c.9601C>T | c.9601C>T | c.9601C>T | c.9601C>T | c.9601C>T | c.719_720delCT | c.719_720delCT | c.719_720delCT | c.9492T>G | c.9492T>G | c.9492T>G |
| Protein mutation | p.(Gln3201*) | p.(Gln3201*) | p.(Gln3201*) | p.(Gln3201*) | p.(Gln3201*) | p.(Gln3201*) | p.(Ser240Cysfs*16) | p.(Ser240Cysfs*16) | p.(Ser240Cysfs*16) | p.(Tyr3164*) | p.(Tyr3164*) | p.(Tyr3164*) |
| Gene 2 | ||||||||||||
| Gene name | - | - | - | - | WDR62 | WDR62 | - | CEP63 | CEP63 | RAD50 | RAD50 | - |
| Zygosity | - | - | - | - | Hetero | Hetero | - | Hetero | Hetero | Hetero | Hetero | - |
| cDNA mutation | - | - | - | - | c.3116A>G | c.3116A>G | - | c.1241A>T | c.1241A>T | c.3643C>G | c.3643C>G | - |
| Protein mutation | - | - | - | - | p.(Ser1106Gly) | p.(Ser1106Gly) | - | p.(Thr421Ser) | p.(Thr421Ser) | p.(Leu1215Val) | p.(Leu1215Val) | - |
| Measurement | ||||||||||||
| Age (years) | 12 | 9 | 6 | 23 | 32 | 10 | 34 | 6 | 3 | 18 | 14 | 10 |
| Gender | Male | Female | Female | Male | Female | Male | Female | Male | Female | Female | Female | Female |
| HC (cm) | 41 | 35 | 34 | 42 | 41.5 | 37 | 35 | 37.5 | 32 | 41 | 43 | 38 |
| HC (SD) | −10 | −14.55 | −15 | −10 | −10 | −12 | −14.55 | −11 | −15 | −10.5 | −9 | −13 |
| Height (cm) | 133 | 115 | 105 | 162 | 124 | 99 | 145 | 93 | 76 | 137 | 145 | 112 |
| Height (SD) | −2 | −3 | −2.5 | −2 | −7 | −6 | −3 | −5 | −5 | −5 | −3 | −4 |
| Neurological features | ||||||||||||
| ID | Moderate | Mild | Severe | Moderate | Severe | Mild | Moderate | Moderate | Moderate | Severe | Severe | Mild |
| Behavior | Aggressive | Aggressive | Aggressive | Aggressive | Aggressive | Aggressive | Aggressive | Aggressive | Aggressive | Aggressive | Aggressive | Normal |
| Speech impairment | Severe | Severe | Severe | Severe | Severe | Severe | Severe | Moderate | Severe | Mild | Mild | Mild |
| Musculoskeletal abnormalities | ||||||||||||
| Contractures | - | - | - | - | Joints (elbow and hands) | Joints (elbow and hands) | - | - | - | - | - | - |
| Clinodactyly of toes | - | - | - | - | - | - | - | - | - | - | - | - |
| Clinodactyly of fingers | - | - | - | - | - | - | - | - | - | - | - | - |
| Brachydactyly of fingers | - | - | - | - | - | - | - | - | - | - | - | - |
| Brachydactyly of toes | - | - | - | - | - | - | - | - | - | - | - | - |
| Others | ||||||||||||
| Drooling | - | - | - | - | Yes | Yes | - | - | - | - | - | - |
| Locomotion | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Hyperactive | Hyperactive | Normal | Normal | Normal |
| Seizures | - | - | - | - | - | - | - | Yes | Yes | Yes | Yes | - |
| Hypopigmentation | - | - | - | - | - | - | - | - | - | - | - | - |
| Teeth | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Normal |
| (b) | ||||||||||||
| Family 4 | Family 5 | |||||||||||
| Patient ID | V-6 | V-7 | V-8 | VI-2 | VI-3 | VI-4 | IV-1 | IV-2 | ||||
| Gene 1 | ||||||||||||
| Gene name | CENPJ | CENPJ | CENPJ | CENPJ | CENPJ | CENPJ | CENPJ | CENPJ | ||||
| Zygosity | Homo | Homo | Homo | Homo | Homo | Homo | Homo | Homo | ||||
| cDNA mutation | c.3586G>A | c.3586G>A | c.3586G>A | c.3586G>A | c.3586G>A | c.3586G>A | c.3586G>A | c.3586G>A | ||||
| Protein mutation | p.(Asp1196Asn) and p.(Val1181_Val1206del) | p.(Asp1196Asn) and p.(Val1181_Val1206del) | p.(Asp1196Asn) and p.(Val1181_Val1206del) | p.(Asp1196Asn) and p.(Val1181_Val1206del) | p.(Asp1196Asn) and p.(Val1181_Val1206del) | p.(Asp1196Asn) and p.(Val1181_Val1206del) | p.(Asp1196Asn) and p.(Val1181_Val1206del) | p.(Asp1196Asn) and p.(Val1181_Val1206del) | ||||
| Gene 2 | ||||||||||||
| Gene name | - | - | - | PCNT | PCNT | PCNT | - | - | ||||
| Zygosity | - | - | - | Hetero | Hetero | Hetero | - | - | ||||
| cDNA mutation | - | - | - | c.5767C>T | c.5767C>T | c.5767C>T | - | - | ||||
| Protein mutation | - | - | - | p.(Arg1923*) | p.(Arg1923*) | p.(Arg1923*) | - | - | ||||
| Measurement | ||||||||||||
| Age (years) | 32 | 22 | 20 | 8 | 6 | 4 | 10 | 4 | ||||
| Gender | Female | Male | Female | Male | Male | Female | Male | Male | ||||
| HC (cm) | 44 | 47 | 45 | 39 | 35 | 35 | 35 | 35 | ||||
| HC (SD) | −8.5 | −7 | −7.5 | −10 | −13 | −11.5 | −12 | −11 | ||||
| Height (cm) | 139 | 156 | 145 | 107 | 91 | 86 | 114 | 81 | ||||
| Height (SD) | −4.5 | −4 | −4 | −4 | −5 | −4 | −4 | −5 | ||||
| Neurological features | ||||||||||||
| ID | Moderate | Moderate | Moderate | Mild | Mild | Mild | Moderate | Moderate | ||||
| Behavior | - | - | - | - | - | - | Normal | Aggressive | ||||
| Speech impairment | Severe | Moderate | Mild | Moderate | Severe | Moderate | Moderate | Moderate | ||||
| Musculoskeletal abnormalities | ||||||||||||
| Contractures | - | - | - | - | - | - | - | - | ||||
| Clinodactyly of toes | - | - | - | Yes (bilateral) | Yes (bilateral) | Yes (bilateral) | - | - | ||||
| Clinodactyly of fingers | - | - | - | - | - | - | - | - | ||||
| Brachydactyly of fingers | - | - | - | Yes (bilateral) | Yes (bilateral) | Yes (bilateral) | - | - | ||||
| Brachydactyly of toes | - | - | - | Yes (bilateral) | Yes (bilateral) | Yes (bilateral) | - | - | ||||
| Others | ||||||||||||
| Drooling | - | - | - | Yes | Yes | Yes | Very rare | - | ||||
| Locomotion | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Normal | ||||
| Seizures | - | - | - | - | - | - | Very rare | Normal | ||||
| Hypopigmentation | Yes (forehead) | Yes (forehead) | - | - | - | - | - | - | ||||
| Teeth | Normal | Normal | Normal | Normal | Normal | Normal | Malocclusion | Normal | ||||
| (a) | ||||||||||
| ID | Gene | Transcript ID | Exon | cDNA Change | Protein Change | ACMG Interpretation | gnomAD Frequency | CADD- Score | Mutation Taster | Polyphen-2 |
| Fam. 1 | ASPM | NM_018136.4 | 23 | c.9601C>T | p.(Gln3201*) | Pathogenic (PVS1, PM2, PP3) | - | 41 | Disease causing (6.0) | NA |
| WDR62 | NM_001083961.1 | 27 | c.3316A>G | p.(Ser1106Gly) | Uncertain significance (PM2) | 0.0000325 | 19.21 | Polymorphism (56) | Benign (0.09) | |
| Fam. 2 | ASPM | NM_018136.4 | 3 | c.719_720delCT | p.(Ser240Cysfs*16) | NA | 0.0000325 | - | Disease causing | NA |
| CEP63 | NM_025180.3 | 12 | c.1261A>T | p.(Thr421Ser) | Uncertain significance (PM2, BP1) | - | 25.1 | Disease causing (58) | Probably damaging (1.000) | |
| Fam. 3 | ASPM | NM_018136.4 | 23 | c.9492T>G | p.(Tyr3164*) | Pathogenic (PVS1, PM2, PP5) | - | 35 | Disease causing (6.0) | NA |
| RAD50 | NM_005732.3 | 24 | c.3643C>G | p.(Leu1215Val) | Likely benign (PM1, PM2, BP1, BP4) | - | 23.5 | Disease causing (32) | Probably damaging (1.000) | |
| Fam. 4 | CENPJ | NM_018451.4 | 14 | c.3586G>A (c.3541_3618del) † | p.(Asp1196Asn) p.(Val1181_Val1206del) †† | Likely pathogenic (PM1, PM2, PP3, PP5) | - | 28.1 | Disease Causing (23) | Probably Damaging (1.000) |
| PCNT | NM_006031.5 | 28 | c.5767C>T | p.(Arg1923*) | Pathogenic (PVS1, PM2, PP3, PP5) | 0.0000122 | 42 | Disease Causing (6.0) | NA | |
| Fam. 5 | CENPJ | NM_018451.4 | 14 | c.3586G>A (c.3541_3618del) † | p.(Asp1196Asn) p.(Val1181_Val1206del) †† | Likely pathogenic (PM1, PM2, PP3, PP5) | - | 28.1 | Disease Causing (23) | Probably Damaging (1.000) |
| (b) | ||||||||||
| ID | Gene | Provean | PANTHER | PhD-SNP | SIFT | SNAP | Meta SNP | MuPro | SNPs&GO | MetaDome |
| Fam. 1 | ASPM | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| WDR62 | Neutral (−1.216) | NA | Disease causing (0.589) | Disease causing (0.010) | Disease causing (0.505) | Disease causing (0.514) | DDG = −1.6848846 (DECREASE stability) | Neutral | Slightly tolerant (0.93) | |
| Fam. 2 | ASPM | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| CEP63 | Deleterious (−2.830) | NA | Neutral (0.380) | NA | NA | Neutral (0.203) | DDG = −0.54948253 (DECREASE stability) | Neutral | Tolerant (1.33) | |
| Fam. 3 | ASPM | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| RAD50 | Neutral (−2.238) | Disease causing (0.603) | Disease causing (0.591) | Disease causing (0.010) | Disease causing (0.645) | Disease causing (0.654) | DDG = −0.79919509 (DECREASE stability) | Neutral | Intolerant (0.42) | |
| Fam. 4 | CENPJ | Deleterious (−4.841) | NA | Disease causing (0.833) | Disease causing (0.000) | Disease causing (0.685) | Disease causing (0.706) | DDG = −0.82129284 (DECREASE stability) | Neutral | Intolerant (0.33) |
| PCNT | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| Fam. 5 | CENPJ | Deleterious (−4.841) | NA | Disease causing (0.833) | Disease causing (0.000) | Disease causing (0.685) | Disease causing (0.706) | DDG = −0.82129284 (DECREASE stability) | Neutral | Intolerant (0.33) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makhdoom, E.U.H.; Waseem, S.S.; Iqbal, M.; Abdullah, U.; Hussain, G.; Asif, M.; Budde, B.; Höhne, W.; Tinschert, S.; Saadi, S.M.; et al. Modifier Genes in Microcephaly: A Report on WDR62, CEP63, RAD50 and PCNT Variants Exacerbating Disease Caused by Biallelic Mutations of ASPM and CENPJ. Genes 2021, 12, 731. https://doi.org/10.3390/genes12050731
Makhdoom EUH, Waseem SS, Iqbal M, Abdullah U, Hussain G, Asif M, Budde B, Höhne W, Tinschert S, Saadi SM, et al. Modifier Genes in Microcephaly: A Report on WDR62, CEP63, RAD50 and PCNT Variants Exacerbating Disease Caused by Biallelic Mutations of ASPM and CENPJ. Genes. 2021; 12(5):731. https://doi.org/10.3390/genes12050731
Chicago/Turabian StyleMakhdoom, Ehtisham Ul Haq, Syeda Seema Waseem, Maria Iqbal, Uzma Abdullah, Ghulam Hussain, Maria Asif, Birgit Budde, Wolfgang Höhne, Sigrid Tinschert, Saadia Maryam Saadi, and et al. 2021. "Modifier Genes in Microcephaly: A Report on WDR62, CEP63, RAD50 and PCNT Variants Exacerbating Disease Caused by Biallelic Mutations of ASPM and CENPJ" Genes 12, no. 5: 731. https://doi.org/10.3390/genes12050731
APA StyleMakhdoom, E. U. H., Waseem, S. S., Iqbal, M., Abdullah, U., Hussain, G., Asif, M., Budde, B., Höhne, W., Tinschert, S., Saadi, S. M., Yousaf, H., Ali, Z., Fatima, A., Kaygusuz, E., Khan, A., Jameel, M., Khan, S., Tariq, M., Anjum, I., ... Hussain, M. S. (2021). Modifier Genes in Microcephaly: A Report on WDR62, CEP63, RAD50 and PCNT Variants Exacerbating Disease Caused by Biallelic Mutations of ASPM and CENPJ. Genes, 12(5), 731. https://doi.org/10.3390/genes12050731











