Abstract
Gene editing (GE) is an efficient strategy for correcting genetic mutations in monogenic hereditary diseases, including β-thalassemia. We have elsewhere reported that CRISPR-Cas9-based gene editing can be employed for the efficient correction of the β039-thalassemia mutation. On the other hand, robust evidence demonstrates that the increased production of fetal hemoglobin (HbF) can be beneficial for patients with β-thalassemia. The aim of our study was to verify whether the de novo production of adult hemoglobin (HbA) using CRISPR-Cas9 gene editing can be combined with HbF induction protocols. The gene editing of the β039-globin mutation was obtained using a CRISPR-Cas9-based experimental strategy; the correction of the gene sequence and the transcription of the corrected gene were analyzed by allele-specific droplet digital PCR and RT-qPCR, respectively; the relative content of HbA and HbF was studied by high-performance liquid chromatography (HPLC) and Western blotting. For HbF induction, the repurposed drug rapamycin was used. The data obtained conclusively demonstrate that the maximal production of HbA and HbF is obtained in GE-corrected, rapamycin-induced erythroid progenitors isolated from β039-thalassemia patients. In conclusion, GE and HbF induction might be used in combination in order to achieve the de novo production of HbA together with an increase in induced HbF.
1. Introduction
The β-thalassemias are hereditary pathologies caused, at the molecular level, by more than 300 mutations of the adult β-globin gene, leading to low or absent production of adult hemoglobin (HbA) in erythroid cells [1,2,3,4]. Together with sickle cell disease (SCD), the economic and clinical impacts of β-thalassemias are devastating in developing countries, where the frequency of these diseases is very high, mainly due to the lack of genetic counseling and prenatal diagnosis [1,2]. The therapeutic protocols for patients affected by β-thalassemia are currently based on blood transfusion, chelation therapy and, alternatively, bone marrow transplantation [3,4].
Within the clinical community, it is known that high blood content of fetal hemoglobin (HbF) is highly beneficial for patients with β-thalassemia [5,6,7], leading to milder forms of the disease. The earliest clinical observations indicating a key role of HbF in ameliorating the β-thalassemia phenotype came from patients with rare forms of β-thalassemia, particularly those with large deletions responsible for δβ0-thalassemia or the hereditary persistence of fetal hemoglobin (HPFH), characterized by the absence of β-globin and HbA in the presence of elevated levels of γ-globin chain production, resulting in high levels of HbF accumulation with a relatively benign clinical course [8]. More recently, clinical studies have shown that naturally elevated production of HbF improves the clinical course in a variety of β-thalassemia patients [9,10,11,12,13]. Accordingly, these observations have prompted research studies on HbF inducers that can therapeutically mimic, at least in part, what occurs in patients characterized by the natural persistence of high levels of HbF [14,15,16,17]. Some of these HbF inducers are presently considered in clinical trials (examples are NCT01245179, NCT00790127 and NCT03877809).
In addition to the approaches based on the pharmacological induction of fetal hemoglobin, an exciting strategy recently proposed for β-thalassemia is genome editing using a variety of protocols widely validated for hematopoietic cells [18]. In this specific field of investigation, the clustered regularly interspaced short palindromic repeats (CRISPR)-Cas9 nuclease system, is among the most efficient [19,20,21,22].
The possibility of using highly efficient gene-editing protocols opens new opportunities in the field of precision medicine for personalized therapy for β-thalassemia [23]. In this context, we have recently reported a protocol for the CRISPR-Cas9-based gene correction of the β039-globin gene mutation (HGVS Name: HBB:c.118C > T), very frequent in the population of the Mediterranean area [24]. In addition to the precise correction of the β-thalassemia mutations, the CRISPR-Cas9-based gene editing approach has been extensively applied to the reactivation of HbF production in β-thalassemia erythroid cells, as demonstrated in the landmark work by Canver et al. [25]. In this case, the objective of the CRISPR-Cas9-based gene editing was (a) the silencing of transcriptional repressors of the γ-globin genes (such as BCL11A) [25,26,27,28,29,30] and (b) the disruption of their regulatory binding sites within the γ-globin genes, which in some cases mimics the natural HPFH mutations in the γ-globin gene [31,32,33,34,35,36,37]. For instance, Khosravi et al. demonstrated that the CRISPR-Cas9-based deletion of the BCL11A gene was associated with the reactivation of HbF production [26,27]. Of great interest is the fact that this strategy is currently under investigation in the NCT03655678 clinical trial, aimed at studying the safety and efficacy of CTX001 (hematopoietic cells gene-edited for elevated HbF production) on transfusion-dependent β-thalassemia (TDT) patients [29,38].
To maximize HbF production, these CRISPR-Cas9-based gene editing approaches can be combined, as recently proposed by Han et al. and by Samuelson et al. [39,40], who reported on a multiplex gene editing strategy based on the combination of two single gene editing approaches, one aimed at silencing the BCL11A repressor, the other aimed at disrupting the BCL11A binding sites present within the γ-globin gene promoter. Another example of multiplex gene editing approaches is that recently published by Psatha et al. [41], who studied the combination of CRISPR-Cas9-based cis and trans fetal globin reactivation mutations, demonstrating that this strategy leads to a significant increase in HbF production when comparison was performed with the single editing procedures. Accordingly, multiplex gene editing could be considered in clinical protocols finalized to the improvement of the clinical status of patients with a severe β-thalassemia phenotype. The results obtained in these studies concurrently demonstrated that these multiplex genomic editing protocols efficiently induced high levels of HbF production without increasing off-target effects [39] and without causing any defects in the proliferation rate or in the differentiation status of treated cells, either in vitro or in vivo [41].
The present study is aimed at determining whether HbF induction can be combined with the de novo production of HbA, obtained by the correction of a β039-globin gene mutation using the CRISPR-Cas9 technology, as recently reported by Cosenza et al. [24].
To obtain co-production of increased levels of HbF and de novo synthesis of HbA, we first considered the possibility to perform CRISPR-Cas9-based multiplex genomic editing for BCL11A silencing (as reported by Khosravi et al., Frangoul et al. and Bjurström et al.) [27,29,30] and β039 correction (as reported by Cosenza et al.) [24]. The advantage of this strategy is that both protocols use the same target cells (CD34+ erythroid progenitors) and no differences are expected in the clinical steps to be followed for collecting the CD34+ cells to be gene edited and for preparing the patients for the infusion of gene-edited cells (e.g., stem cells collected via mobilization and apheresis, myeloablative conditioning, infusion of corrected stem cells for the engraftment and immune reconstitution) [29]. On the other hand, a major drawback is expected, i.e., higher off-targeting effects and genotoxicity [40]. Supporting a caution in using multiplexed CRISPR-Cas9-based approaches, Samuelson et al. recently reported that multiplex CRISPR-Cas9 genome editing in hematopoietic stem cells for fetal hemoglobin reinduction generates chromosomal translocations [40]. For these reasons, we therefore decided to use for HbF induction a repositioned drug, rapamycin [42,43,44,45,46,47,48], among those already validated and used in clinical trials [49,50,51,52]. To the best of our knowledge, this strategy is novel, as no study is available on the combination of pharmacological induction of HbF with gene editing procedures aimed at the de novo production of HbA following the CRISPR-Cas9-based correction of genetic mutations.
Rapamycin, also known as sirolimus, is a potent inducer of HbF in in vitro systems [42,43,44,45,46,47,52], in in vivo animal models [46,47,53,54], and in few but highly informative patients affected by sickle-cell disease (SCD) [55,56]. In conclusion, all the available in vitro data concurrently indicate that rapamycin can be repurposed for the treatment of β-thalassemia for the following reasons: (a) rapamycin increases HbF in cultures from β-thalassemia patients with different basal HbF levels; (b) rapamycin increases the overall Hb content per cell; (c) rapamycin selectively induces γ-globin mRNA accumulation, with only minor effects on β-globin protein and β-globin mRNAs; (d) there is a strong correlation between the HbF increase induced by rapamycin and the increase in γ-globin mRNA content.
Accordingly, rapamycin is at present employed in two clinical trials recruiting β-thalassemia patients, NCT03877809 and NCT04247750 [57,58].
2. Materials and Methods
2.1. Isolation of Erythroid Precursor Cells (ErPCs) and ErPCs Cultures
ErPCs cultures were prepared from 25 mL of peripheral blood, following the Fibach protocol [59], as described by Zuccato et al. [58] and fully reported in the Supplementary Materials (SM1). Immunological flow cytometry (FCM) characterization using antibodies for CD71 and CD235a demonstrated that the yield (% of ErPCs) was always higher than 85%, in agreement with previously reported data [58]. Representative FCM data and morphological analysis are shown in Figures S3 and S4. Elsewhere, published data demonstrate that the large majority of ErPCs undergo erythroid differentiation, as demonstrated with flow cytometry analysis using antibodies against transferrin receptor and glycophorin [60]. We carefully considered the fact that FBS might heavily affect ex vivo erythroid differentiation and hemoglobin production, thereby creating variability. For this reason, we screened all the FBS batches, selecting only those lacking effects on the differentiation of ErPCs and on HBF production after exposure to HbF inducers. Moreover, the same batch of FBS was used throughout all the experiments reported in the present study.
2.2. Treatment of Cells with β039 CRISPR-Cas9 System and Rapamycin
On the third day of phase II, the ErPCs were considered ready to be treated with rapamycin, with β039 CRISPR-Cas9 system or with the combined β039 CRISPR-Cas9 system and rapamycin. Rapamycin (sirolimus, SIR, cat. R0395, Sigma Aldrich, St. Louis, MO, USA) was administered at the starting point of the ErPCs cultures at a concentration of 200 nM, and the stock solution was prepared by diluting the powder in EtOH 96% to reach a 50 μM concentration.
2.3. Cell Electroporation with CRISPR-Cas9 System for Correction of the β039-Globin Gene Mutation
We followed the protocol described by Cosenza et al. [24], further detailed in Supplementary Materials (SM4). Briefly, the genomic sgRNA target sequence was 5′-TGGTCTACCCTTGGACCTAGAGG-3′ (sgRNA target sequence underlined, PAM in bold); the gRNA complex begins by joining a tracrRNA (ATTO 550 labeled Alt-R® CRISPR-Cas9 tracrRNA, IDT, USA), and the Alt-R® CRISPR-Cas9 crRNA (IDT) oligonucleotide in thermoblock at 95 °C for 5 min.
2.4. Genomic DNA Extraction
The DNA was extracted from 200–300 µL of whole blood as described by Cosenza et al. [24] and detailed in the Supplementary Materials (SM5). The quality of the genomic DNA was verified by gel electrophoresis using 0.8% agarose gels and quantified by spectrophotometry using the SmartSpec™ Plus instrument (Biorad Smartspec Plus, Bio-Rad).
2.5. RNA Isolation, cDNA Reverse Transcription and RT-qPCR
The total cellular RNA was extracted using the TRI Reagent® (Sigma-Aldrich). After washing once with cold 75% ethanol, the RNA was dried and dissolved in diethylpyrocarbonate-treated water (WMBR: Water Molecular Biology Reagent nuclease-free, Sigma-Aldrich). For analysis of gene expression, 0.5 μg of total RNA was reverse transcribed by using the TaqMan® Reverse Transcription Reagents and Random Hexamer (Applied Biosystems, Life Technologies, Thermo-Fisher, Waltham, MA, USA). The relative content of α-, β-, and γ-globin mRNAs were quantified by multiplex qPCR using primers and FAM, HEX and Cy5/ZEN/IBFQ-labeled hydrolysis probes purchased as custom-designed PrimeTime qPCR Assays from IDT and listed in Table 1.

Table 1.
List of oligonucleotides (primers and probes) used to evaluate the correction degree obtained on the β-globin gene and study the accumulation of α-, β- and γ-globin mRNAs.
Data of RT-qPCR experiments were analyzed using CFX Manager™ software (Bio-Rad). The relative expression of globins’ mRNAs was calculated using the comparative cycle threshold method (ΔΔCt method) using as reference genes human GAPDH sequences [24,58,61].
2.6. Droplet Digital PCR (ddPCR) to Evaluate Genomic and Transcriptomic β039 Globin Correction
The evaluation of the β-globin gene correction levels in the position of codon 39 was carried out with droplet digital PCR [24,62]. In these experiments, Taq-Man probes marked with FAM and HEX fluorophores were used, designed specifically for the identification of the sequence containing the β039 mutation (HEX) in the β-globin gene and the corresponding corrected sequence (FAM) (Table 1). The protocols have been reported by Cosenza et al. [24] and detailed in Supplementary Materials (SM6).
2.7. HPLC Analysis of Hemoglobins
Analysis of HbA, HbF and free α-globin chains was performed with HPLC as elsewhere reported [24,58,61,63]. Lysates have been loaded into a PolyCAT-A cation exchange column and then eluted in a sodium-chloride-BisTris-KCN aqueous mobile phase using HPLC Beckman Coulter instrument System Gold 126 Solvent Module-166 detector, which allows to obtain for the quantification of the hemoglobins present in the sample. Further details can be found in Supplementary Materials (SM7 and SM9).
2.8. Western Blotting Analysis
The accumulation of β-globin (16 kDa) and γ-globin (15 kDa) proteins was assessed with Western blotting as described by Cosenza et al. [24] and detailed in Supplementary Materials (SM8).
2.9. Amplicon Sequencing and Whole Genome Sequencing
All the experiments for the construction of the amplicon libraries, the sequencing of the fragments, and all the bioinformatics analysis (including the estimation of CRISPR-Cas9 OFF-target sites and analysis of OFF-target insertion) were performed at Genartis—Innovative Genomic Technologies laboratories (Genartis Srl, Verona, Italy, https://genartis.it/, accessed on 1 June 2022), following the same protocols reported in the previous work by Cosenza et al. [24].
2.10. Statistical Analysis
All the data are presented as mean ± S.D. Statistical differences have been determined using ANOVA (analyses of variance between groups) followed by Dunnett’s post hoc tests. Statistical differences were considered significant when p < 0.05, highly significant when p < 0.01 [58].
3. Results
3.1. Experimental Strategy for CRISPR-Cas9 Correction of the Thalassemia β039 Mutation and for Co-Treatment with Rapamycin
Figures S1 and S2 show the experimental strategy for the CRISPR-Cas9-based correction of the β039-globin gene mutation in erythroid precursor cells (ErPCs) isolated from β-thalassemia patients and for the combination of this CRISPR-Cas9 treatment with rapamycin-based HbF induction. Rapamycin was used at 200 nM final concentration. ErPCs were first cultured for 7 days without erythropoietin (EPO) (Phase I). Then, the cells were transferred to a medium containing EPO (Phase II), for stimulating the erythroid differentiation and the production of hemoglobin. After three days of Phase II culture, the cells were electroporated in the presence of a reaction mix containing all the elements of the CRISPR-Cas9 system and/or treated with 200 nM rapamycin. After electroporation and genomic editing and/or rapamycin treatment, the cells were maintained in Phase II medium and, after 5 days, analyzed to evaluate the biological effects of the treatments. The immunophenotype of ErPCs and further details concerning morphology and key features of in vitro ErPCs differentiation are reported in Figures S3 and S4. In addition, key features of in vitro ErPCs differentiation have been reported elsewhere and discussed in the study published by Bianchi et al. [60]. In brief, the flow cytometry analysis of transferrin receptor (TR) and glycophorin A (GYPA) surface marker expression in ErPCs phase II cultures from β-thalassemia patients revealed GYPA as a late erythroid marker, with an increase from day 4 to day 8 along with Hb production, and TR as an early marker with unchanged expression from day 4, at >80% cells positive for either marker at both time points [60].
Concerning the analysis of gene editing, the used techniques allowed us to evaluate gene correction at the following levels: genomic (using sequencing and ddPCR protocols), transcriptomic (using RT-qPCR and RT-ddPCR approaches) and proteomic (using Western blotting and HPLC). Concerning the analysis of HbF induction, RT-qPCR and HPLC allowed us to compare the effects of the treatments on the accumulation of γ-globin mRNA and increased production of HbF, respectively.
The CRISPR-Cas9 model used for the correction of the β039-globin gene mutation has been described by Cosenza et al. [24] and presented in Figure S2.
3.2. End-Point of the Gene Editing of the β039-Globin Gene: Genomic Analyses and RT-ddPCR to Detect Corrected Normal β039-Globin Gene and mRNA
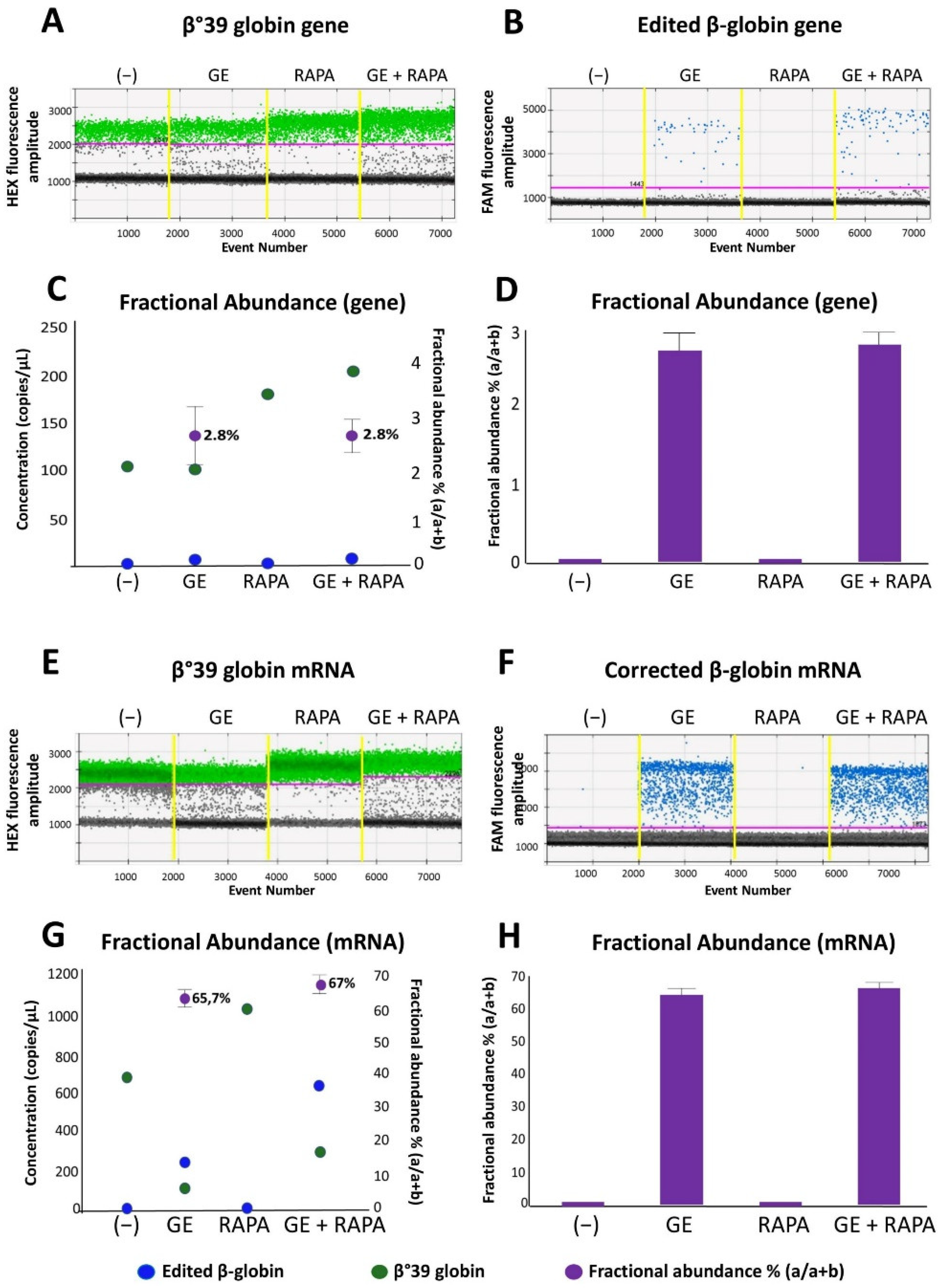
In order to verify the presence of the normal β-globin gene after CRISPR-Cas9 correction of the β039-thalassemia mutation, two complementary approaches were employed: (a) allele-specific PCR, performed using droplet-digital PCR and (b) amplicon sequencing. Figure 1A,B, shows a representative analysis of gene correction with the CRISPR-Cas9 system performed on ErPCs genomic DNA isolated from a homozygous β039-thalassemia patient and cultured without treatments (−) or using the following experimental conditions: (a) CRISPR-Cas9 gene editing (GE); (b) 200 nM rapamycin (RAPA); (c) GE and rapamycin treatment (200 nM) (GE + RAPA). The correction data plotted are represented in the 1d dot plot, obtained from the ddPCR analysis software.
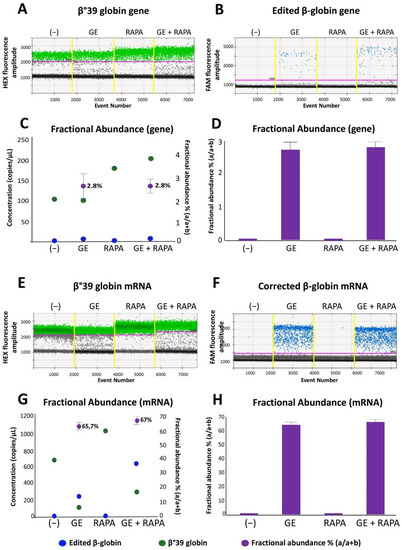
Figure 1.
Evaluation of the effects of CRISPR-Cas9 system on β-globin gene and mRNA in ErPCs cultures. The panels show the data relating to a representative result obtained after gene correction treatments performed with the CRISPR-Cas9 system on a culture of β039 ErPCs and analyzed with ddPCR assay. (A,B) and (E,F) refer to 1d dot plots obtained after analysis of mock treated (A,E—green dots) and edited (B,F—blue dots) β-globin gene and mRNA, respectively. (C,G) Correlation between the concentration of the samples (expressed in copies/µL) and the fractional abundance (purple dot) related to the representative example reported in panels (A,B) and (E,F). (D,H) Histograms extrapolated from the analysis of the fractional abundance of the representative sample used in the experiment. (−) control untreated cells; GE (cells treated with the CRISPR-Cas9 system), RAPA (rapamycin 200 nM) and GE + RAPA (cells treated with the CRISPR-Cas9 system and then cultured in the presence of rapamycin).
As is clearly evident, the presence of amplified edited β-globin gene sequences is absent in control untreated (−) and in rapamycin-treated (RAPA) ErPCs but present in both genome edited (GE) and edited + rapamycin-treated (GE + RAPA) cultures. The correction level obtained is reported as concentration (copies/µL of reaction) and in the form of fractional abundance %, calculated as an edited/edited + mutated concentration.
In Figure 1C,D the fractional abundance of corrected gene sequences is shown, obtained from four ErPCs populations. Results from amplicon sequencing (Figure S5) confirmed the editing of ErPCs.
Figure 1E,F shows a representative example of accumulation of β-globin mRNA using ErPCs from a β039/β039 homozygous β-thalassemia patient treated as described in Figure S1 and analyzed by RT-ddPCR assay.
In Figure 1G,H, the data obtained from the same representative experiment are reported as concentration (copies/µL of reaction) and in the form of fractional abundance %, calculated as an edited/(edited + mutated) concentration. The fractional abundance data shown in Figure 1G,H demonstrate a high content of the edited β-globin mRNA in CRISPR-Cas9 treated ErPCs either in the absence or in the presence of the HbF inducer rapamycin.
Despite the fact that a direct translation from “fractional abundance” to “% of corrected cells” cannot be proposed, the data shown in Figure 1 clearly indicate that corrected β-globin gene (Figure 1A–D) and corrected β-globin mRNA (Figure 1E–H) are detectable only in gene-edited (GE) ErPCs populations. The high content of corrected β-globin mRNA is expected since it is well established that the β039-globin mRNA (as most of mRNAs carrying stop-codon mutations) are highly unstable [24].
In order to evaluate the correction level of β039-globin gene mutation obtained from ErPCs treated with our CRISPR-Cas9 system, we analyzed both mutated β039 and edited β-globin mRNAs, using also an RT-ddPCR approach. γ-globin and α-globin transcripts were also analyzed.
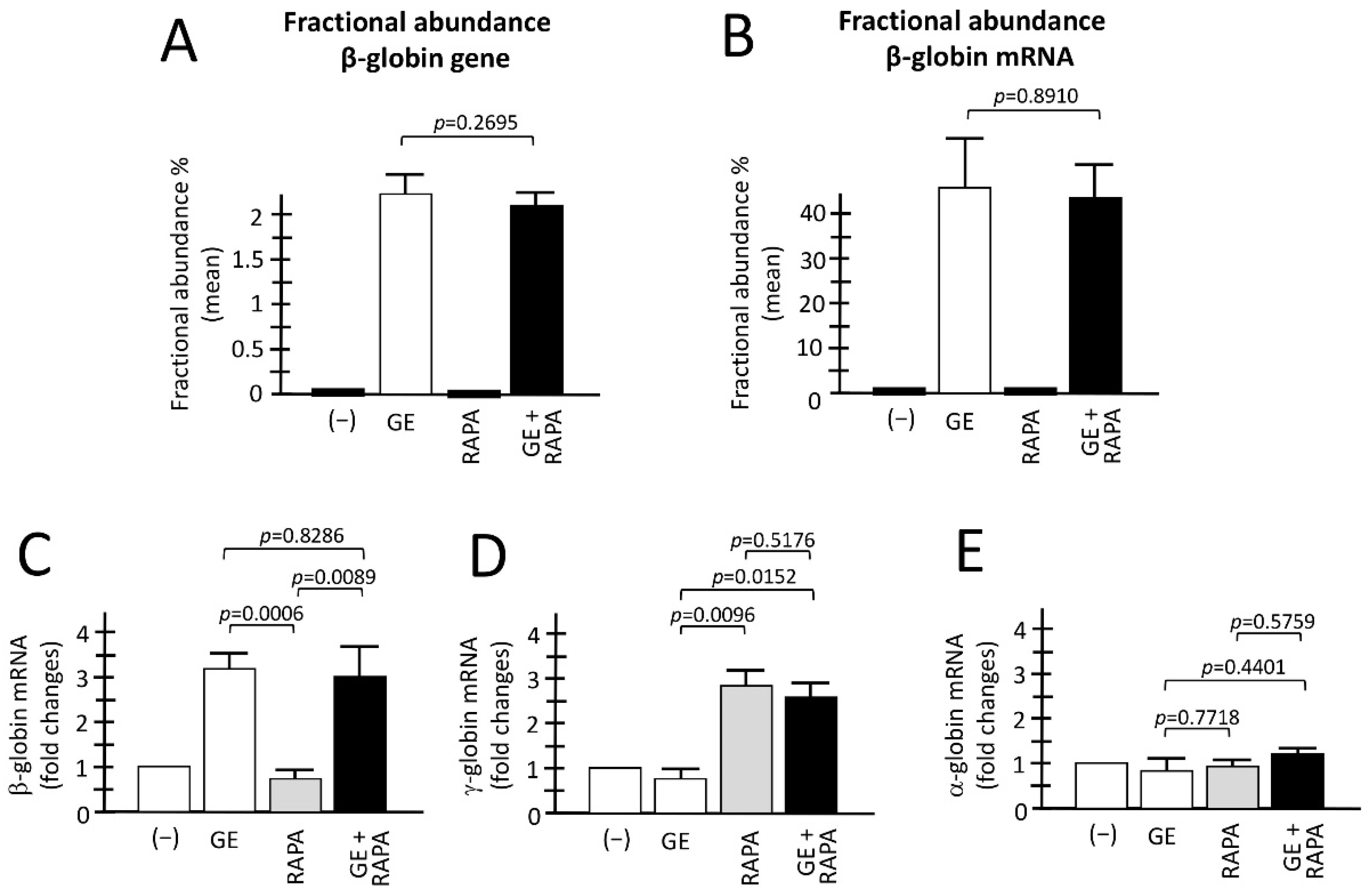
3.3. De Novo Production of Edited β-Globin mRNA and Induction of γ-Globin Gene Transcription in the Same ErPCs Populations
Figure 2A,B reports a summary of the genomic and RT-ddPCR analyses to detect corrected normal β-globin mRNA, as well as the accumulation of α-globin, β-globin and γ-globin mRNA in the ErPCs analyzed obtained from different patients, comparing control untreated (−), with cells GE-corrected, cells treated with the HbF inducer rapamycin, and cells GE-treated and HbF induced. As expected, and in agreement with a previously published report from our laboratory [24] corrected β-globin gene sequences are present only in GE-treated cell populations, irrespectively to co-treatment with rapamycin (Figure 2A). In all the samples containing GE corrected β-globin gene sequences, the production of normal β-globin mRNA was readily detectable. The two ErPCs populations (GE and GE plus rapamycin) did not differ significantly with respect to the presence of the corrected β-globin gene (Figure 2A) and production of corrected β-globin mRNA (Figure 2B) (p = 0.2695 and p = 0.8910, respectively).
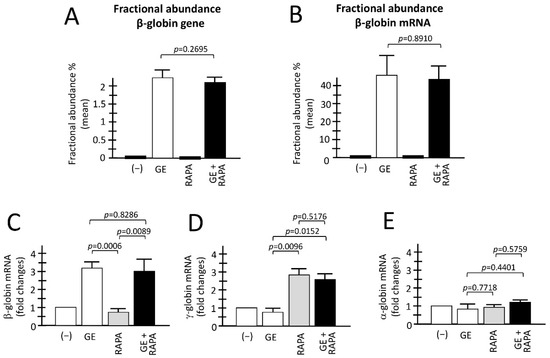
Figure 2.
Evaluation of the combination between CRISPR-Cas9 gene editing and rapamycin-mediated HbF induction. (A,B) Fractional abundance obtained after treatment performed by CRISPR-Cas9 system on ErPCs isolated from β039-thalassemia patients and analyzed by ddPCR assay. The histograms show the data related to β-globin gene (A) and β-globin mRNA (B). (C–E) The histograms show the relative content of the β-, γ- and α-globin mRNAs analyzed by multiplex RT-qPCR. (−): untreated cells; GE: cells treated with the CRISPR-Cas9 system; RAPA: rapamycin 200 nM treated cells; GE + RAPA: cells treated with the CRISPR-Cas9 system and cultured in the presence of rapamycin. All the data of RT-qPCR were normalized using GAPDH as housekeeping internal control gene, as described in Material and Methods. Results are expressed as fold changes with respect to control untreated cells (−). Results are from independent experiments using ErPCs cultures from three (A) and five (B–E) homozygous β039-thalassemia patients. The level of statistical significance is reported as p-value (p).
When the analysis was conducted for the content of α-, β-, and γ-globin mRNAs using RT-qPCR, the following results were obtained (Figure 2C–E). First of all, in agreement with Figure 2B, a significant increase in β-globin mRNA was detectable only in GE and GE plus rapamycin cultures (p = 0.0006 and p = 0.0089, respectively, with respect to rapamycin-only treated cultures) (Figure 2C,D). Importantly, when GE and GE plus rapamycin cultures were compared, no significant change in β-globin mRNA content was observed (p = 0.8286), demonstrating that rapamycin treatment has no major effects on β-globin mRNA content.
As a second and most relevant result, a significant increase in γ-globin mRNA was detectable only in rapamycin and GE plus rapamycin cultures (p = 0.0096 and p = 0.0152, respectively), with respect to GE-only treated cultures.
Moreover, when rapamycin and GE plus rapamycin cultures were compared, no significant change in the accumulation of γ-globin mRNA was observed (p = 0.5176), demonstrating that gene editing has no major effects on the rapamycin-mediated induction of the expression of γ-globin genes. Interestingly, no change in α-globin mRNA content was found in the ErPCs populations, indicating that the expression of α-globin genes in ErPCs treated with GE, rapamycin and GE plus rapamycin is similar to control untreated ErPCs (−). The data shown in Figure 2C–E were obtained using GAPDH sequences as internal reference. However, the same conclusion can be reached using RPL13A or β-actin internal controls (unpublished results).
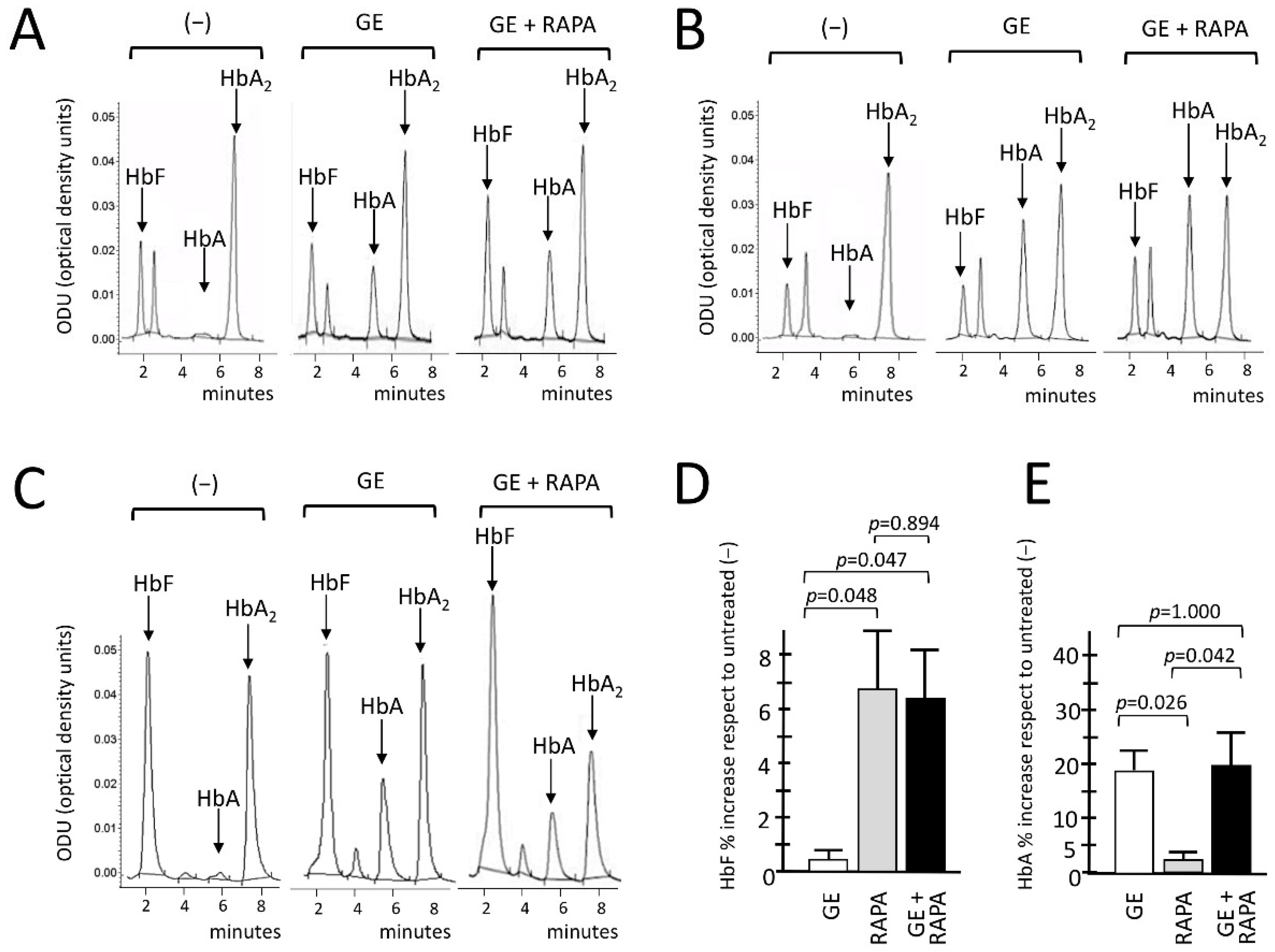
3.4. Co-Production of HbA (De Novo) and HbF (Induced) in Gene-Edited ErPCs Treated with Rapamycin
We conclusively demonstrated the de novo production of HbA and the increased production of HbF in gene-edited, HbF-induced, ErPCs using HPLC. Representative HPLC analysis performed on CRISPR-Cas9 edited, rapamycin-induced ErPCs from three β039/β039-thalassemia patients are reported in Figure 3A–C.
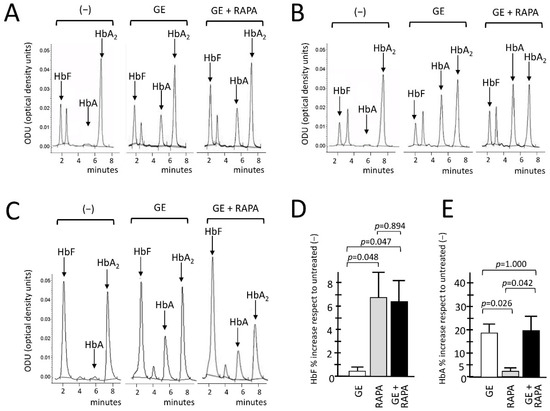
Figure 3.
Effects of β039 CRISPR-Cas9 treatment on HbA and HbF hemoglobins, evaluated with HPLC. (A–C) Chromatograms related to the HPLC analysis conducted of the protein lysates of the ErPCs cultures derived from three β039-thalassemic patients. For each of them, the expression pattern of hemoglobins in ErPCs untreated (−), treated with β039 CRISPR-Cas9 system alone (GE) and with the editing system in combination with rapamycin (GE + RAPA) were analyzed. The average of all patients analyzed for the relative increase in fetal hemoglobin HbF and adult hemoglobin HbA, expressed as a percentage, are shown in panels (D,E), respectively. The level of statistical significance is reported as p-value (p), significant when p< 0.05.
The HPLC data, as clearly shown in the representative chromatograms, indicate a de novo production of adult hemoglobin (HbA) in all GE-samples analyzed, in agreement with the data indicating efficient gene editing (Figure 1 and Figure 2A,B). An increased production of HbF was in addition observed when the GE plus rapamycin cultures were compared with the GE-only samples. Figure 3D,E show the summary of the treatments performed in which the GE, rapamycin and GE plus rapamycin samples were compared with control untreated cells. The results obtained confirm that GE treatment does not interfere with HbF induction (Figure 3D). In addition, despite the fact that with the presence of the reactivation of γ-globin genes the β-globin gene expression might be analogically reduced, the data obtained demonstrate that the rapamycin induction of γ-globin genes does not interfere with the de novo HbA production using the GE approach (Figure 3E).
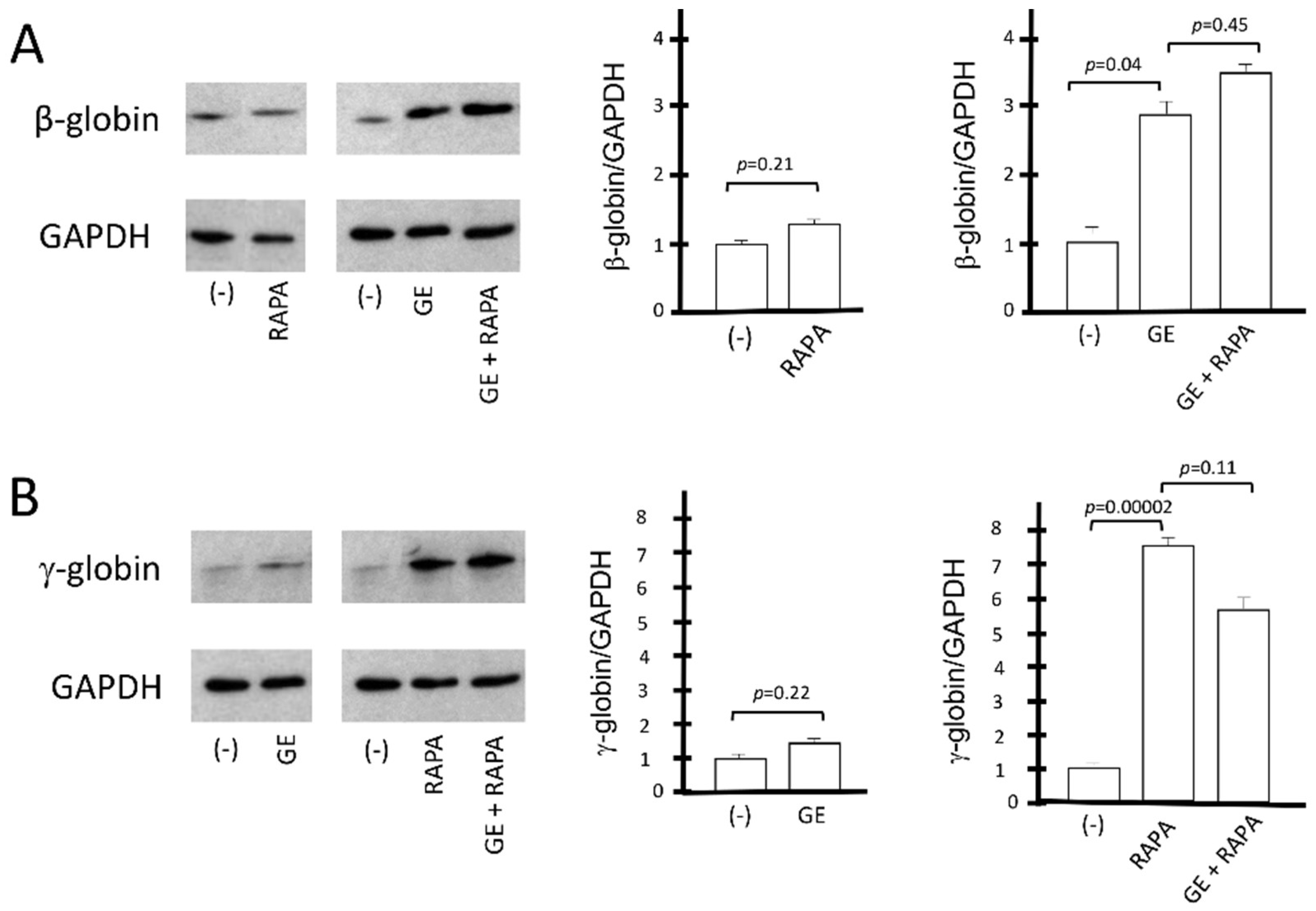
The conclusions of the HPLC studies were further confirmed by the Western blotting analyses shown in Figure 4, which aimed at evaluating the β-globin and γ-globin proteins produced under the different experimental conditions depicted in Figure 3. The amounts of CRISPR-Cas9-corrected β-globin protein (16 kDa) and γ-globin protein (15 kDa) were normalized with the quantity of housekeeping GAPDH (37 kDa) protein. The data obtained show that rapamycin, as expected, does not induce an increase in the β-globin protein in control cells; in addition, rapamycin treatment does not affect the accumulation of β-globin in CRISPR-Cas9 corrected ErPCs (Figure 4A).
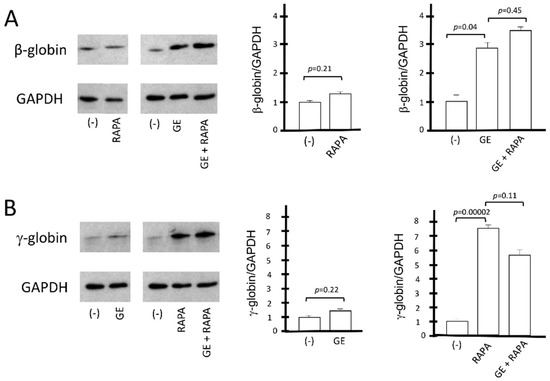
Figure 4.
Western blotting analysis of β-globin protein and γ-globin protein. The relative content of β-globin (16 kDa) and γ-globin (15 kDa) proteins was determined by Western blotting analysis, after comparison with the housekeeping GAPDH (37 kDa) protein. (A) The effect on β-globin production of the β039 CRISPR-Cas9 system is shown as representative data and graphically reported in the form of gel bands (panel (A), left). These results are reported in the right part of panel (A) as values of the densitometric analysis with respect to the reference protein GAPDH. (B) Representative data graphically show the impact of the β039 CRISPR-Cas9 system on γ-globin expression. For the same samples, the data obtained from densitometric analysis of the Western blotting bands normalized on the housekeeping protein GAPDH (panel (B), left) are reported, and statistical significance is indicated as p-value (p). (−): untreated cells; GE (cells treated with the CRISPR-Cas9 system), RAPA (rapamycin 200 nM) and GE + RAPA (cells treated with the CRISPR-Cas9 system and then cultured in the presence of rapamycin). The original uncut versions of the gels are shown in Figure S6.
On the other hand, the gene editing treatment has no effect on γ-globin accumulation, and, importantly, gene editing has no effect on rapamycin-mediated increase in γ-globin (Figure 4B). These data are consistent with the conclusion that the co-induction of β-globin and γ-globin proteins occurs in CRISPR-Cas9-edited, rapamycin-treated ErPCs.
3.5. Amplicon-Based and WGS Sequencing Results
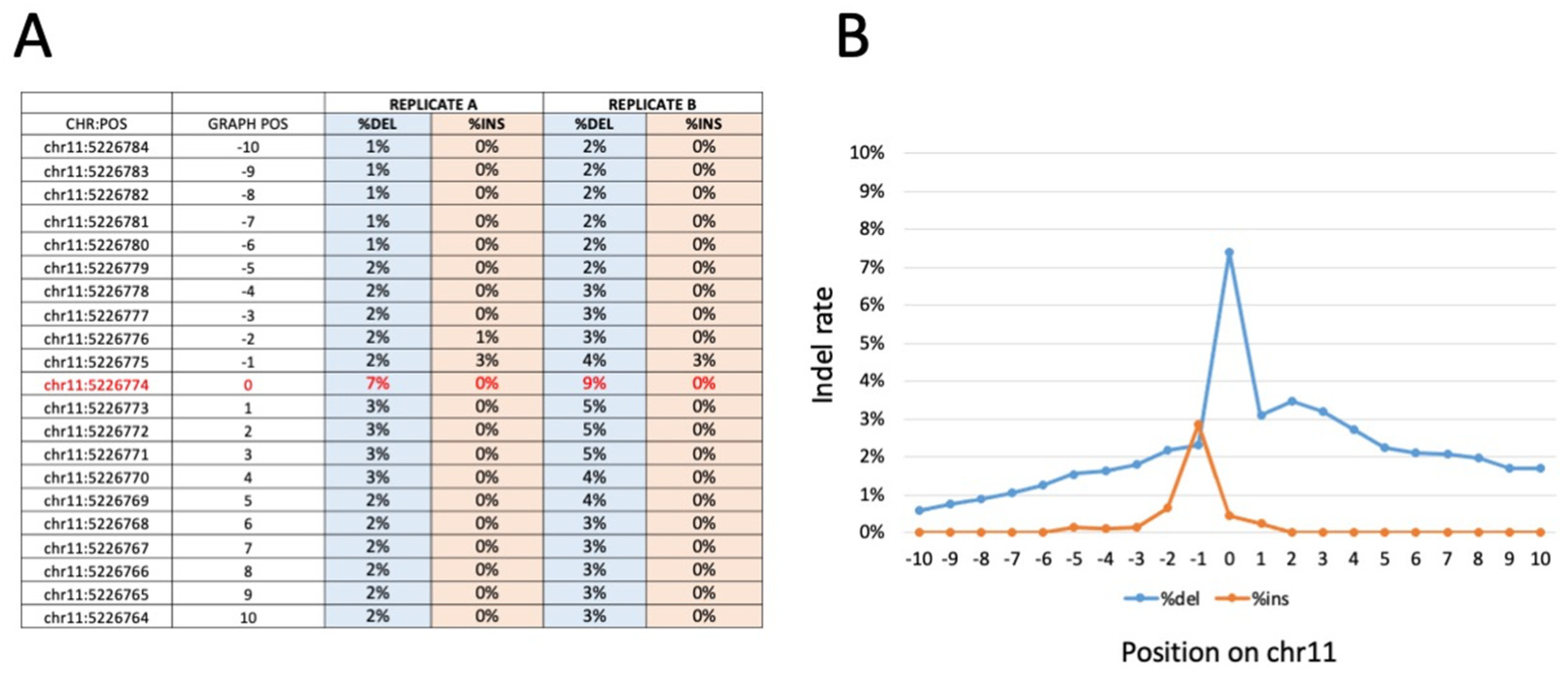
Bar-coded amplicons were sequenced on a NovaSeq 6000 platform 150 phycoerythrin (PE) mode. The obtained number of fragments was ∼400,000 for the 18 (9 in duplicate) samples sequenced. The calculation of the frequency of the edited base and the indels at the sites of interest showed an editing rate between 7.1% and 8.8% for the edited base (chr11:5,226,774), with a deletion rate between 9.4% and 7.4%. A very low occurrence of insertions (lower than 0.1%) was detectable (Figure 5, Figures S4 and S6). All samples showed an editing rate above the control samples, generated as expected background values, indicating that the gene editing was efficient in all samples analyzed. The data show that, as expected and in agreement with the results published by Cosenza et al. [24] and with the data presented in Figure 5, Figures S5 and S7 of the present paper, a consistent proportion of corrected sequences is present in all of the edited samples.
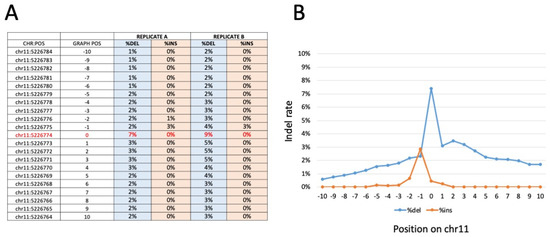
Figure 5.
Representative indel frequency and positioning around the β039 CRISPR-Cas9 editing target site, obtained with amplicon sequencing of β039 ErPCs treated with the CRISPR-Cas9 system. Panel (A) shows the indel frequency values for the amplicon replicates analyzed. In particular, the ten positions upstream and downstream from position chr11: 5226.774 (β039 target site indicated in red) were analyzed. The data obtained are reported in panel (B) in which the percentage of deletion (blue line) and insertion (orange line) is graphically reported as a function of each nucleotide position investigated. Similar results were obtained with WGS sequencing (Figure S7).
Interestingly, and fully in agreement with Figure 3A–C and Figure 4A, no corrected sequences are present in rapamycin-treated cells, and no further increase in corrected sequences is present in samples isolated from GE-ErPCs treated with rapamycin. Concerning indel effects, no insertions were found. On the contrary, deletions were detected in a proportion similar to the insertion of corrected sequences. Similar results were obtained in a WGS study (Figure S7, representative data), in which we calculated the frequency of the edited base and of the indels on the sites of interest. In particular, on the target site, no insertions were found, whereas there was a low number of deletions, in agreement with data obtained with the previously described amplicon sequencing approach.
4. Discussion
Gene editing with CRISPR-Cas9 technology is one of the most promising strategies to be exploited for the precise correction of hereditary mutations in a variety of monogenetic diseases. For instance, CRISPR-Cas9 has been employed in cystic fibrosis [64,65], sickle-cell disease [66,67], Huntington’s chorea [68], Duchenne muscular dystrophy [69,70], hemophilia [71,72], and chronic granulomatous disease [73].
Concerning thalassemia, CRISPR-Cas9 gene editing can be proposed for the efficient correction of the β039-globin gene mutation (one of the most frequent in the Mediterranean area) recently reported by Cosenza et al. [24]. This approach was demonstrated to be able to force gene-edited cells to de novo produce HbA, with possible clinical advantages in case the protocol is used in clinical trials focusing on homozygous β039-thalassemia patients.
On the other hand, robust evidence demonstrates that fetal hemoglobin (HbF) can be highly beneficial to β-thalassemia patients, leading to a milder phenotype and lower requirement of blood transfusions [27,31]. In this respect, several clinical trials with β-thalassemia and/or sickle-cell anemia patients are ongoing using HbF inducers, such as NCT01245179 (based on the HDAC inhibitor Panobinostat) [74], NCT00790127 (based on 2,2-dimethylbutyrate, HQK-1001) [50] and NCT03877809 (based on the mTOR inhibitor rapamycin) [58].
The aim of our study was to verify whether the de novo production of HbA using CRISPR-Cas9-based gene editing can be combined with HbF induction protocols. This idea is not new, as it was validated by Zuccato et al. using a combination of gene therapy using lentiviral vectors and HbF induction [75,76]. This strategy was deemed useful in consideration of the fact that while an increase in β-globin gene expression in β-thalassemia cells can be achieved with gene therapy, the de novo production of clinically relevant levels of adult Hb may be difficult to obtain. On the other hand, the fact that the increased production of HbF is beneficial in β-thalassemia, the combination of gene therapy and HbF induction appears to be a pertinent strategy for achieving clinically relevant results.
Combined treatment using gene editing and HbF induction approaches together have not been described so far. Our results conclusively demonstrate that gene editing and HbF induction might be used in combination in order to achieve the de novo production of HbA together with the increased production of induced HbF. In these combined treatments, mild conditions of gene editing can be used, thereby limiting off-targeting and genotoxic effects. These issues are important considering that GE in thalassemia and rapamycin treatment of β-thalassemia patients are both in clinical trials (see NCT03728322, NCT03655678, NCT05444894, NCT03877809 and NCT04247750). In this respect, it should be underlined that the approach here described based on combined treatments might be considered within the therapeutic field of personalized treatments in precision medicine. In this context, the CRISPR-Cas9-based correction of the β039-thalassemia mutation can be applied to any patient with at least one β-globin allele carrying the β039 mutation, such as β039/β039 homozygotes and compound heterozygotes for the β039-globin gene. On the other hand, HbF induction can also be considered a personalized approach, as several gene polymorphisms (such as the XmnI) have been reported to be associated with high HbF induction levels [77,78,79].
In conclusion, the protocol here described is expected to be of interest to all clinicians working on hematological diseases, such as β-thalassemia, in particular for those working on β0-thalassemias. It should be underlined that also researchers working with sickle-cell disease (SCD) patients might be interested since, apart from the gene editing of the SCD locus, HbF is expected to be useful for SCD [49].
A limitation of this study is that no attempt has been made to fully characterize the biochemical/molecular targets of rapamycin. This should be done in future experimental efforts, as it will help in understanding some therapeutically relevant findings of our study. For instance, the absence of reciprocal regulation of the expression of γ- and β-globin genes is still remarkable, although the lack of inhibitory effects on β-globin gene expression in rapamycin-treated erythroid cells has already been reported [43,45,58]. In this respect, while a reciprocal decrease in β-globin was expected in HbF-producing cells [35], from the HPLC (Figure 3) and Western blotting (Figure 4) analysis, we do not see any reduction of HbA in RAPA- and GE-treated cells when comparison was conducted with GE-only treated cells. Analysis of the transcription machinery might be proposed for better understanding this finding. In addition, post-transcriptional effects cannot be excluded, considering the well-known effects of mTOR inhibitors on protein synthesis [80].
A second major limitation of our study is that we have not addressed in depth the effects of the treatment of gene-edited ErPCs populations with rapamycin apart from the changes in hemoglobin pattern found in the experiments reported in Figure 3 and Figure 4. This is an important point for identifying the required end-points of a possible future clinical trial based on the present study. In this respect, one of the issues to be considered is the effects of rapamycin treatment on the excess of free α-globin chains. In fact, rapamycin exhibits a very interesting effect, i.e., the decrease in this excess in vitro and in vivo [58], with the consequent reduction of the unbalanced α-globin/ β-like globin chain ratios [1]. This is a clinically relevant end point, since low α-globin protein expression is beneficial in β-thalassemia patients [81,82]. Interestingly, Lachauve at al. have demonstrated that the effect of rapamycin on the excess of free α-globin chains is caused by the ULK-1-dependent activation of autophagy [54]. It will be of interest to determine whether autophagy and decrease in the excess of free α-globin chains is activated in gene-edited rapamycin-treated ErPCs. To this end, ULK-1 mRNA and the autophagy-related p62, LC3-I/II proteins should be quantified in gene-edited rapamycin-treated ErPCs. Preliminary data obtained by HPLC analyses support the hypothesis that rapamycin treatment further reduces the free α-globin peak in gene-edited ErPCs (Figure S8).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/genes13101727/s1, Supplementary Methods SM1: Erythroid precursor cells (ErPCs) isolation and ErPCs culture; Supplementary Methods SM2: Flow cytometry-based characterization of in vitro cultured ErPCs; Supplementary Methods SM3: Cytospin and morphological analysis of ErPCs; Supplementary Methods SM4: Cell electroporation with CRISPR-Cas9 system for correction of the β039-globin gene mutation; Supplementary Methods SM5: Genomic DNA extraction; Supplementary Methods SM6: Droplet digital PCR (ddPCR) to evaluate genomic and transcriptomic β039 globin correction; Supplementary Methods SM7: HPLC Analysis of Hemoglobins; Supplementary Methods SM8: Western blotting analysis; Supplementary Methods SM9: HPLC-based analysis of the excess of “free α-globin chains”. Figure S1: Scheme of the experimental strategy; Figure S2: Model of the β039 CRISPR-Cas9 system used for gene editing experiments; Figure S3: FCS analysis of ErPCs; Figure S4: Cytospin analysis from cultured ErPCs from a β039-thalassemia patient; Figure S5: Editing results obtained by amplicon sequencing from ErPCs isolated from a β039 thalassemia patient; Figure S6: Uncut version of the Western blots; Figure S7: Alignment of the fragments generated by the WGS sequencing obtained from an ErPCs sample edited with the β039 CRISPR-Cas9 system; Figure S8: Reduction of the free α-globin peak after rapamycin treatment of gene-edited ErPCs.
Author Contributions
Conceptualization, L.C.C., R.G. and A.F.; methodology, validation, L.C.C., C.Z. and M.Z.; formal analysis, L.C.C., R.G. and A.F.; investigation, L.C.C. and A.F.; lab resources, R.G. and A.F.; data curation, L.C.C. and A.F.; statistical analysis, L.C.C. and C.Z.; writing—original draft preparation, L.C.C., R.G. and A.F.; writing—review and editing, L.C.C., R.G. and A.F.; supervision, R.G. and A.F.; project administration, A.F.; funding acquisition, R.G. and A.F. All authors have read and agreed to the published version of the manuscript.
Funding
This study was sponsored by the Wellcome Trust (innovator award 208872/Z/17/Z) and AIFA (AIFA-2016-02364887). The research leading to these results has received funding also from the UE THALAMOSS Project (Thalassemia Modular Stratification System for Personalized Therapy of Βeta-Thalassemia; no. 306201-FP7-HEALTH-2012-INNOVATION-1), FIR and FAR funds to AF from the University of Ferrara. This research was also supported by A.L.T. (Associazione per la lotta alla Talassemia) “Rino Vullo”—Ferrara, A.V.L.T. (Associazione Veneta per la Lotta alla Talassemia) “Elio Zago”-APS-Rovigo, and by the Interuniversity Consortium for the Biotechnology (C.I.B., Italy).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and the use of human material was approved by the Ethics Committee of Ferrara’s District, protocol name: THAL-THER, document number 533/2018/Sper/AOUFe, approved on 14 November 2018. All samples of peripheral blood were obtained after receiving written informed consent from donor patients or their legal representatives.
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper. No details have been included in the manuscript that allows patient identification.
Data Availability Statement
Most of the data are included in the text and in the Supplementary Materials File. Additional information will be made freely available upon request to the corresponding authors.
Acknowledgments
We thank Associazione Tutti per Chiara Onlus for supporting L.C.C., C.Z. and M.Z. with post-doc fellowships. This study is dedicated to the memory of Chiara Gemmo and Elio Zago.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Weatherall, D.J. Phenotype-genotype relationships in monogenic disease: Lessons from the thalassaemias. Nat. Rev. Genet. 2001, 2, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Origa, R. β-Thalassemia. Genet. Med. 2017, 19, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Fucharoen, S.; Weatherall, D.J. Progress toward the Control and Management of the Thalassemias. Hematol. Oncol. Clin. N. Am. 2016, 30, 359–371. [Google Scholar] [CrossRef] [PubMed]
- Galanello, R.; Origa, R. Β-thalassemia. Orphanet J. Rare Dis. 2010, 5, 11. [Google Scholar] [CrossRef] [PubMed]
- Sripichai, O.; Fucharoen, S. Fetal hemoglobin regulation in β-thalassemia: Heterogeneity, modifiers and therapeutic approaches. Expert Rev. Hematol. 2016, 9, 1129–1137. [Google Scholar] [CrossRef]
- Liu, D.; Zhang, X.; Yu, L.; Cai, R.; Ma, X.; Zheng, C.; Zhou, Y.; Liu, Q.; Wei, X.; Lin, L.; et al. KLF1 mutations are relatively more common in a thalassemia endemic region and ameliorate the severity of β-thalassemia. Blood 2014, 124, 803–811. [Google Scholar] [CrossRef]
- Musallam, K.M.; Sankaran, V.G.; Cappellini, M.D.; Duca, L.; Nathan, D.G.; Taher, A.T. Fetal hemoglobin levels and morbidity in untransfused patients with β-thalassemia intermedia. Blood 2012, 119, 364–367. [Google Scholar] [CrossRef]
- Forget, B.G. Molecular basis of hereditary persistence of fetal hemoglobin. Ann. N. Y. Acad. Sci. 1998, 850, 38–44. [Google Scholar] [CrossRef]
- Nuinoon, M.; Makarasara, W.; Mushiroda, T.; Setianingsih, I.; Wahidiyat, P.A.; Sripichai, O.; Kumasaka, N.; Takahashi, A.; Svasti, S.; Munkongdee, T.; et al. A genome-wide association identified the common genetic variants influence disease severity in β0-thalassemia/hemoglobin E. Hum. Genet. 2010, 127, 303–314. [Google Scholar] [CrossRef]
- Galanello, R.; Sanna, S.; Perseu, L.; Sollaino, M.C.; Satta, S.; Lai, M.E.; Barella, S.; Uda, M.; Usala, G.; Abecasis, G.R.; et al. Amelioration of Sardinian β0 thalassemia by genetic modifiers. Blood 2009, 114, 3935–3937. [Google Scholar] [CrossRef]
- Danjou, F.; Anni, F.; Perseu, L.; Satta, S.; Dessì, C.; Lai, M.E.; Devoto, M.; Galanello, R. Genetic modifiers of b-thalassemia and clinical severity as assessed by age at first transfusion. Haematologica 2012, 97, 989–993. [Google Scholar] [CrossRef] [PubMed]
- Badens, C.; Joly, P.; Agouti, I.; Thuret, I.; Gonnet, K.; Fattoum, S.; Loundou, A.; Pissard, S. Variants in genetic modifiers of β-thalassemia can help to predict the major or intermedia type of the disease. Haematologica 2011, 96, 1712–1714. [Google Scholar] [CrossRef] [PubMed]
- Uda, M.; Galanello, R.; Sanna, S.; Lettre, G.; Sankaran, V.G.; Chen, W.; Usala, G.; Busonero, F.; Maschio, A.; Albai, G.; et al. Genome wide association study shows BCL11A associated with persistent fetal hemoglobin and amelioration of the phenotype of β-thalassemia. Proc. Natl. Acad. Sci. USA 2008, 105, 1620–1625. [Google Scholar] [CrossRef] [PubMed]
- Gambari, R.; Fibach, E. Medicinal chemistry of fetal hemoglobin inducers for treatment of β-thalassemia. Curr. Med. Chem. 2007, 14, 199–212. [Google Scholar] [CrossRef] [PubMed]
- Lavelle, D.; Engel, J.D.; Saunthararajah, Y. Fetal Hemoglobin Induction by Epigenetic Drugs. Semin. Hematol. 2018, 55, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Finotti, A.; Gambari, R. Recent trends for novel options in experimental biological therapy of β-thalassemia. Expert Opin. Biol. Ther. 2014, 14, 1443–1454. [Google Scholar] [CrossRef] [PubMed]
- Nuamsee, K.; Chuprajob, T.; Pabuprapap, W.; Jintaridth, P.; Munkongdee, T.; Phannasil, P.; Vadolas, J.; Chaichompoo, P.; Suksamrarn, A.; Svasti, S. Trienone analogs of curcuminoids induce fetal hemoglobin synthesis via demethylation at (G)γ-globin gene promoter. Sci. Rep. 2021, 11, 8552. [Google Scholar] [CrossRef]
- Boulad, F.; Mansilla-Soto, J.; Cabriolu, A.; Rivière, I.; Sadelain, M. Gene Therapy and Genome Editing. Hematol. Oncol. Clin. N. Am. 2018, 32, 329–342. [Google Scholar] [CrossRef]
- Papasavva, P.; Kleanthous, M.; Lederer, C.W. Rare Opportunities: CRISPR/Cas-Based Therapy Development for Rare Genetic Diseases. Mol. Diagn. Ther. 2019, 23, 201–222. [Google Scholar] [CrossRef]
- Lau, C.H. Applications of CRISPR-Cas in Bioengineering, Biotechnology, and Translational Research. CRISPR J. 2018, 1, 379–404. [Google Scholar] [CrossRef]
- Hu, X. CRISPR/Cas9 system and its applications in human hematopoietic cells. Blood Cells Mol. Dis. 2016, 62, 6–12. [Google Scholar] [CrossRef]
- Dever, D.P.; Bak, R.O.; Reinisch, A.; Camarena, J.; Washington, G.; Nicolas, C.E.; Pavel-Dinu, M.; Saxena, N.; Wilkens, A.B.; Mantri, S. CRISPR/Cas9 β-globin gene targeting in human haematopoietic stem cells. Nature 2016, 539, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zeng, J.; Roscoe, B.P.; Liu, P.; Yao, Q.; Lazzarotto, C.R.; Clement, K.; Cole, M.A.; Luk, K.; Baricordi, C.; et al. Highly efficient therapeutic gene editing of human hematopoietic stem cells. Nat. Med. 2019, 25, 776–783. [Google Scholar] [CrossRef] [PubMed]
- Cosenza, L.C.; Gasparello, J.; Romanini, N.; Zurlo, M.; Zuccato, C.; Gambari, R.; Finotti, A. Efficient CRISPR-Cas9-based genome editing of β-globin gene on erythroid cells from homozygous β039-thalassemia patients. Mol. Ther. Methods Clin. Dev. 2021, 21, 507–523. [Google Scholar] [CrossRef] [PubMed]
- Canver, M.C.; Smith, E.C.; Sher, F.; Pinello, L.; Sanjana, N.E.; Shalem, O.; Chen, D.D.; Schupp, P.G.; Vinjamur, D.S.; Garcia, S.P.; et al. BCL11A enhancer dissection by Cas9-mediated in situ saturating mutagenesis. Nature 2015, 527, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Fu, B.; Liao, J.; Chen, S.; Li, W.; Wang, Q.; Hu, J.; Yang, F.; Hsiao, S.; Jiang, Y.; Wang, L.; et al. CRISPR-Cas9-mediated gene editing of the BCL11A enhancer for pediatric β0/β0 transfusion-dependent β-thalassemia. Nat. Med. 2022, 28, 1573–1580. [Google Scholar] [CrossRef] [PubMed]
- Khosravi, M.A.; Abbasalipour, M.; Concordet, J.P.; Berg, J.V.; Zeinali, S.; Arashkia, A.; Azadmanesh, K.; Buch, T.; Karimipoor, M. Targeted deletion of BCL11A gene by CRISPR-Cas9 system for fetal hemoglobin reactivation: A promising approach for gene therapy of β thalassemia disease. Eur. J. Pharmacol. 2019, 854, 398–405. [Google Scholar] [CrossRef]
- Khosravi, M.A.; Abbasalipour, M.; Concordet, J.P.; Berg, J.V.; Zeinali, S.; Arashkia, A.; Buch, T.; Karimipoor, M. Expression analysis data of BCL11A and γ-globin genes in KU812 and KG-1 cell lines after CRISPR/Cas9-mediated BCL11A enhancer deletion. Data Brief 2019, 28, 104974. [Google Scholar] [CrossRef]
- Frangoul, H.; Altshuler, D.; Cappellini, M.D.; Chen, Y.S.; Domm, J.; Eustace, B.K.; Foell, J.; de la Fuente, J.; Grupp, S.; Handgretinger, R.; et al. CRISPR-Cas9 Gene Editing for Sickle Cell Disease and β-Thalassemia. N. Engl. J. Med. 2021, 384, 252–260. [Google Scholar] [CrossRef]
- Bjurström, C.F.; Mojadidi, M.; Phillips, J.; Kuo, C.; Lai, D.S.; Lill, G.R.; Cooper, A.; Kaufman, M.; Urbinati, F.; Wang, X.; et al. Reactivating Fetal Hemoglobin Expression in Human Adult Erythroblasts Through BCL11A Knockdown Using Targeted Endonucleases. Mol. Ther. Nucleic Acids 2016, 5, e351. [Google Scholar] [CrossRef]
- Weber, L.; Frati, G.; Felix, T.; Hardouin, G.; Casini, A.; Wollenschlaeger, C.; Meneghini, V.; Masson, C.; de Cian, A.; Chalumeau, A.; et al. Editing a γ-globin repressor binding site restores fetal hemoglobin synthesis and corrects the sickle cell disease phenotype. Sci. Adv. 2020, 6, eaay9392. [Google Scholar] [CrossRef] [PubMed]
- Métais, J.Y.; Doerfler, P.A.; Mayuranathan, T.; Bauer, D.E.; Fowler, S.C.; Hsieh, M.M.; Katta, V.; Keriwala, S.; Lazzarotto, C.R.; Luk, K.; et al. Genome editing of HBG1 and HBG2 to induce fetal hemoglobin. Blood Adv. 2019, 3, 3379–3392. [Google Scholar] [CrossRef] [PubMed]
- Antoniani, C.; Meneghini, V.; Lattanzi, A.; Felix, T.; Romano, O.; Magrin, E.; Weber, L.; Pavani, G.; El Hoss, S.; Kurita, R.; et al. Induction of fetal hemoglobin synthesis by CRISPR/Cas9-mediated editing of the human β-globin locus. Blood 2018, 131, 1960–1973. [Google Scholar] [CrossRef] [PubMed]
- Lamsfus-Calle, A.; Daniel-Moreno, A.; Antony, J.S.; Epting, T.; Heumos, L.; Baskaran, P.; Admard, J.; Casadei, N.; Latifi, N.; Siegmund, D.M. Comparative targeting analysis of KLF1, BCL11A, and HBG1/2 in CD34+ HSPCs by CRISPR/Cas9 for the induction of fetal hemoglobin. Sci. Rep. 2020, 10, 10133. [Google Scholar] [CrossRef] [PubMed]
- Topfer, S.K.; Feng, R.; Huang, P.; Ly, L.C.; Martyn, G.E.; Blobel, G.A.; Weiss, M.J.; Quinlan, K.G.R.; Crossley, M. Disrupting the adult globin promoter alleviates promoter competition and reactivates fetal globin gene expression. Blood J. Am. Soc. Hematol. 2022, 139, 2107–2118. [Google Scholar] [CrossRef]
- Lu, D.; Xu, Z.; Peng, Z.; Yang, Y.; Song, B.; Xiong, Z.; Ma, Z.; Guan, H.; Chen, B.; Nakamura, Y.; et al. Induction of Fetal Hemoglobin by Introducing Natural Hereditary Persistence of Fetal Hemoglobin Mutations in the γ-Globin Gene Promoters for Genome Editing Therapies for β-Thalassemia. Front. Genet. 2022, 13, 881937. [Google Scholar] [CrossRef]
- Ye, L.; Wang, J.; Tan, Y.; Beyer, A.I.; Xie, F.; Muench, M.O.; Kan, Y.W. Genome editing using CRISPR-Cas9 to create the HPFH genotype in HSPCs: An approach for treating sickle cell disease and β-thalassemia. Proc. Natl. Acad. Sci. USA 2016, 113, 10661–10665. [Google Scholar] [CrossRef]
- Hirakawa, M.P.; Krishnakumar, R.; Timlin, J.A.; Carney, J.P.; Butler, K.S. Gene editing and CRISPR in the clinic: Current and future perspectives. Biosci. Rep. 2020, 40, BSR20200127. [Google Scholar] [CrossRef]
- Han, Y.; Tan, X.; Jin, T.; Zhao, S.; Hu, L.; Zhang, W.; Kurita, R.; Nakamura, Y.; Liu, J.; Li, D.; et al. CRISPR/Cas9-based multiplex genome editing of BCL11A and HBG efficiently induces fetal hemoglobin expression. Eur. J. Pharmacol. 2022, 918, 174788. [Google Scholar] [CrossRef]
- Samuelson, C.; Radtke, S.; Zhu, H.; Llewellyn, M.; Fields, E.; Cook, S.; Huang, M.W.; Jerome, K.R.; Kiem, H.; Humbert, O. Multiplex CRISPR/Cas9 genome editing in hematopoietic stem cells for fetal hemoglobin reinduction generates chromosomal translocations. Mol. Ther. Methods Clin. Dev. 2021, 23, 507–523. [Google Scholar] [CrossRef]
- Psatha, N.; Georgakopoulou, A.; Li, C.; Nandakumar, V.; Georgolopoulos, G.; Acosta, R.; Paschoudi, K.; Nelson, J.; Chee, D.; Athanasiadou, A.; et al. Enhanced HbF reactivation by multiplex mutagenesis of thalassemic CD34+ cells in vitro and in vivo. Blood 2021, 138, 1540–1553. [Google Scholar] [CrossRef]
- Mischiati, C.; Sereni, A.; Lampronti, I.; Bianchi, N.; Borgatti, M.; Prus, E.; Fibach, E.; Gambari, R. Rapamycin-mediated induction of γ-globin mRNA accumulation in human erythroid cells. Br. J. Haematol. 2004, 126, 612–621. [Google Scholar] [CrossRef] [PubMed]
- Fibach, E.; Bianchi, N.; Borgatti, M.; Zuccato, C.; Finotti, A.; Lampronti, I.; Prus, E.; Mischiati, C.; Gambari, R. Effects of rapamycin on accumulation of α-, β- and γ-globin mRNAs in erythroid precursor cells from β-thalassaemia patients. Eur. J. Haematol. 2006, 77, 437–441. [Google Scholar] [CrossRef]
- Zuccato, C.; Bianchi, N.; Borgatti, M.; Lampronti, I.; Massei, F.; Favre, C.; Gambari, R. Everolimus is a potent inducer of erythroid differentiation and γ-globin gene expression in human erythroid cells. Acta Haematol. 2007, 117, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Pecoraro, A.; Troia, A.; Calzolari, R.; Scazzone, C.; Rigano, P.; Martorana, A.; Sacco, M.; Maggio, A.; di Marzo, R. Efficacy of Rapamycin as Inducer of Hb F in Primary Erythroid Cultures from Sickle Cell Disease and β-Thalassemia Patients. Hemoglobin 2015, 39, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Khaibullina, A.; Almeida, L.E.; Wang, L.; Kamimura, S.; Wong, E.C.; Nouraie, M.; Maric, I.; Albani, S.; Finkel, J.; Quezado, Z.M. Rapamycin increases fetal hemoglobin and ameliorates the nociception phenotype in sickle cell mice. Blood Cells Mol. Dis. 2015, 55, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Tran, J.; Wang, H.; Guo, C.; Harro, D.; Campbell, A.D.; Eitzman, D.T. mTOR Inhibition improves anaemia and reduces organ damage in a murine model of sickle cell disease. Br. J. Haematol. 2016, 174, 461–469. [Google Scholar] [CrossRef]
- Prosdocimi, M.; Zuccato, C.; Cosenza, L.C.; Borgatti, M.; Lampronti, I.; Finotti, A.; Gambari, R. A Rational Approach to Drug Repositioning in β-thalassemia: Induction of Fetal Hemoglobin by Established Drugs. Wellcome Open Res. 2022, 23, 150. [Google Scholar] [CrossRef]
- Paikari, A.; Sheehan, V.A. Fetal haemoglobin induction in sickle cell disease. Br. J. Haematol. 2018, 180, 189–200. [Google Scholar] [CrossRef]
- Reid, M.E.; El Beshlawy, A.; Inati, A.; Kutlar, A.; Abboud, M.R.; Haynes, J., Jr.; Ward, R.; Sharon, B.; Taher, A.T.; Smith, W.; et al. A double-blind, placebo-controlled phase II study of the efficacy and safety of 2,2-dimethylbutyrate (HQK-1001), an oral fetal globin inducer, in sickle cell disease. Am. J. Hematol. 2014, 89, 709–713. [Google Scholar] [CrossRef]
- Ross, J.M.; Forté, S.; Soulières, D. Emerging drugs for the treatment of sickle cell disease: A review of phase II/III trials. Expert Opin. Emerg. Drugs 2022, 27, 211–224. [Google Scholar] [CrossRef] [PubMed]
- Yasara, N.; Wickramarathne, N.; Mettananda, C.; Silva, I.; Hameed, N.; Attanayaka, K.; Rodrigo, R.; Wickramasinghe, N.; Perera, L.; Manamperi, A.; et al. A randomised double-blind placebo-controlled clinical trial of oral hydroxyurea for transfusion-dependent β-thalassaemia. Sci. Rep. 2022, 12, 2752. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Campreciós, G.; Rimmelé, P.; Liang, R.; Yalcin, S.; Mungamuri, S.K.; Barminko, J.; D’Escamard, V.; Baron, M.H.; Brugnara, C.; et al. FOXO3-mTOR metabolic cooperation in the regulation of erythroid cell maturation and homeostasis. Am. J. Hematol. 2014, 89, 954–963. [Google Scholar] [CrossRef] [PubMed]
- Lechauve, C.; Keith, J.; Khandros, E.; Fowler, S.; Mayberry, K.; Freiwan, A.; Thom, C.S.; Delbini, P.; Romero, E.B.; Zhang, J.; et al. The autophagy-activating kinase ULK1 mediates clearance of free α-globin in β-thalassemia. Sci. Transl. Med. 2019, 11, eaav4881. [Google Scholar] [CrossRef]
- Gaudre, N.; Cougoul, P.; Bartolucci, P.; Dörr, G.; Kamar, N.; del Bello, A.; Bura-Riviere, A. Improved Fetal Hemoglobin with mTOR Inhibitor-Based Immunosuppression in a Kidney Transplant Recipient with Sickle Cell Disease. Am. J. Transplant. 2017, 17, 2212–2214. [Google Scholar] [CrossRef]
- Al-Khatti, A.A.; Alkhunaizi, A.M. Additive effect of sirolimus and hydroxycarbamide on fetal haemoglobin level in kidney transplant patients with sickle cell disease. Br. J. Haematol. 2019, 185, 959–961. [Google Scholar] [CrossRef]
- Gamberini, M.R.; Prosdocimi, M.; Gambari, R. Sirolimus for Treatment of β-Thalassemia: From Pre-Clinical Studies to the Design of Clinical Trials. Health Educ. Public Health 2021, 4, 425–435. [Google Scholar]
- Zuccato, C.; Cosenza, L.C.; Zurlo, M.; Gasparello, J.; Papi, C.; D’Aversa, E.; Breveglieri, G.; Lampronti, I.; Finotti, A.; Borgatti, M.; et al. Expression of γ-globin genes in β-thalassemia patients treated with sirolimus: Results from a pilot clinical trial (Sirthalaclin). Ther. Adv. Hematol. 2022, 13, 20406207221100648. [Google Scholar] [CrossRef]
- Fibach, E.; Bianchi, N.; Borgatti, M.; Prus, E.; Gambari, R. Mithramycin induces fetal hemoglobin production in normal and thalassemic human erythroid precursor cells. Blood 2003, 102, 1276–1281. [Google Scholar] [CrossRef]
- Bianchi, N.; Finotti, A.; Ferracin, M.; Lampronti, I.; Zuccato, C.; Breveglieri, G.; Brognara, E.; Fabbri, E.; Borgatti, M.; Negrini, M.; et al. Increase of microRNA-210, decrease of raptor gene expression and alteration of mammalian target of rapamycin regulated proteins following mithramycin treatment of human erythroid cells. PLoS ONE 2015, 10, e0121567. [Google Scholar] [CrossRef]
- Zuccato, C.; Cosenza, L.C.; Zurlo, M.; Lampronti, I.; Borgatti, M.; Scapoli, C.; Gambari, R.; Finotti, A. Treatment of Erythroid Precursor Cells from β-Thalassemia Patients with Cinchona Alkaloids: Induction of Fetal Hemoglobin Production. Int. J. Mol. Sci. 2021, 22, 13433. [Google Scholar] [CrossRef] [PubMed]
- D’Aversa, E.; Breveglieri, G.; Boutou, E.; Balassopoulou, A.; Voskaridou, E.; Pellegatti, P.; Guerra, G.; Scapoli, C.; Gambari, R.; Borgatti, M. Droplet Digital PCR for Non-Invasive Prenatal Detection of Fetal Single-Gene Point Mutations in Maternal Plasma. Int. J. Mol. Sci. 2022, 23, 2819. [Google Scholar] [CrossRef] [PubMed]
- Lampronti, I.; Bianchi, N.; Borgatti, M.; Fibach, E.; Prus, E.; Gambari, R. Accumulation of γ-globin mRNA in human erythroid cells treated with angelicin. Eur. J. Haematol. 2003, 71, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Schwank, G.; Koo, B.K.; Sasselli, V.; Dekkers, J.F.; Heo, I.; Demircan, T.; Sasaki, N.; Boymans, S.; Cuppen, E.; van der Ent, C.K.; et al. Functional repair of CFTR by CRISPR/Cas9 in intestinal stem cell organoids of cystic fibrosis patients. Cell Stem. Cell 2013, 13, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Firth, A.L.; Menon, T.; Parker, G.S.; Qualls, S.J.; Lewis, B.M.; Ke, E.; Dargitz, C.T.; Wright, R.; Khanna, A.; Gage, F.H.; et al. Functional gene correction for cystic fibrosis in lung epithelial cells generated from patient iPSCs. Cell Rep. 2015, 12, 1385–1390. [Google Scholar] [CrossRef] [PubMed]
- Hoban, M.D.; Lumaquin, D.; Kuo, C.Y.; Romero, Z.; Long, J.; Ho, M.; Young, C.S.; Mojadidi, M.; Fitz-Gibbon, S.; Cooper, A.R.; et al. CRISPR/Cas9-mediated correction of the sickle mutation in human CD34+ cells. Mol. Ther. 2016, 24, 1561–1569. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Lee, C.M.; Deshmukh, H.; Bao, G. Therapeutic CRISPR/Cas9 genome editing for treating sickle cell disease. Blood 2016, 128, 4703. [Google Scholar] [CrossRef]
- Shin, J.W.; Kim, K.H.; Chao, M.J.; Atwal, R.S.; Gillis, T.; MacDonald, M.E.; Gusella, J.F.; Lee, J.M. Permanent inactivation of Huntington’s disease mutation by personalized allele-specific CRISPR/Cas. Hum. Mol. Genet. 2016, 25, 4566–4576. [Google Scholar]
- Ousterout, D.G.; Kabadi, A.M.; Thakore, P.I.; Majoros, W.H.; Reddy, T.E.; Gersbach, C.A. Multiplex CRISPR/Cas9-based genome editing for correction of dystrophin mutations that cause Duchenne muscular dystrophy. Nat. Commun. 2015, 6, 6244. [Google Scholar] [CrossRef]
- Li, H.L.; Fujimoto, N.; Sasakawa, N.; Shirai, S.; Ohkame, T.; Sakuma, T.; Tanaka, M.; Amano, N.; Watanabe, A.; Sakurai, H.; et al. Precise correction of the dystrophin gene in duchenne muscular dystrophy patient induced pluripotent stem cells by TALEN and CRISPR-Cas9. Stem. Cell. Reports 2015, 4, 143–154. [Google Scholar] [CrossRef]
- Park, C.Y.; Kim, D.H.; Son, J.S.; Sung, J.J.; Lee, J.; Bae, S.; Kim, J.H.; Kim, D.W.; Kim, J.S. Functional correction of large factor VIII gene chromosomal inversions in Hemophilia A patient-derived iPSCs using CRISPR-Cas9. Cell. Stem. Cell 2015, 17, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Guan, Y.; Ma, Y.; Li, Q.; Sun, Z.; Ma, L.; Wu, L.; Wang, L.; Zeng, L.; Shao, Y.; Chen, Y.; et al. CRISPR/Cas9-mediated somatic correction of a novel coagulator factor IX gene mutation ameliorates hemophilia in mouse. EMBO Mol. Med. 2016, 8, 477–488. [Google Scholar] [CrossRef]
- Flynn, R.; Grundmann, A.; Renz, P.; Hänseler, W.; James, W.S.; Cowley, S.A.; Moore, M.D. CRISPR-mediated genotypic and phenotypic correction of a chronic granulomatous disease mutation in human iPS cells. Exp. Hematol. 2015, 43, 838–848.e3. [Google Scholar] [CrossRef] [PubMed]
- Bou-Fakhredin, R.; de Franceschi, L.; Motta, I.; Cappellini, M.D.; Taher, A.T. Pharmacological Induction of Fetal Hemoglobin in β-Thalassemia and Sickle Cell Disease: An Updated Perspective. Pharmaceuticals 2022, 15, 753. [Google Scholar] [CrossRef] [PubMed]
- Zuccato, C.; Breda, L.; Salvatori, F.; Breveglieri, G.; Gardenghi, S.; Bianchi, N.; Brognara, E.; Lampronti, I.; Borgatti, M.; Rivella, S.; et al. A combined approach for β-thalassemia based on gene therapy-mediated adult hemoglobin (HbA) production and fetal hemoglobin (HbF) induction. Ann. Hematol. 2012, 91, 1201–1213. [Google Scholar] [CrossRef][Green Version]
- Breda, L.; Rivella, S.; Zuccato, C.; Gambari, R. Combining gene therapy and fetal hemoglobin induction for treatment of β-thalassemia. Expert Rev. Hematol. 2013, 6, 255–264. [Google Scholar] [CrossRef]
- Biswas, S.; Nag, A.; Ghosh, K.; Ray, R.; Roy, K.; Bandyopadhyay, A.; Bhattacharyya, M. Genetic determinants related to pharmacological induction of foetal haemoglobin in transfusion-dependent HbE-β thalassaemia. Ann. Hematol. 2019, 98, 289–299. [Google Scholar] [CrossRef]
- Ghosh, D.; Panja, A.; Saha, D.; Banerjee, U.; Datta, A.K.; Basu, A. Drug Repurposing: Hydroxyurea Therapy Improves the Transfusion-Free Interval in HbE/β-Thalassemia-Major Patients with the XmnI Polymorphism. Genet. Test. Mol. Biomarkers 2021, 25, 563–570. [Google Scholar] [CrossRef]
- Breveglieri, G.; Bianchi, N.; Cosenza, L.C.; Gamberini, M.R.; Chiavilli, F.; Zuccato, C.; Montagner, G.; Borgatti, M.; Lampronti, I.; Finotti, A.; et al. An Aγ-globin G->A gene polymorphism associated with β039 thalassemia globin gene and high fetal hemoglobin production. BMC Med. Genet. 2017, 18, 93. [Google Scholar] [CrossRef]
- Wang, X.; Proud, C.G. The mTOR pathway in the control of protein synthesis. Physiology (Bethesda) 2006, 21, 362–369. [Google Scholar] [CrossRef]
- Mettananda, S.; Gibbons, R.J.; Higgs, D.R. α-Globin as a molecular target in the treatment of β-thalassemia. Blood 2015, 125, 3694–3701. [Google Scholar] [CrossRef] [PubMed]
- Cromer, M.K.; Camarena, J.; Martin, R.M.; Lesch, B.J.; Vakulskas, C.A.; Bode, N.M.; Kurgan, G.; Collingwood, M.A.; Rettig, G.R.; Behlke, M.A.; et al. Gene replacement of α-globin with β-globin restores hemoglobin balance in β-thalassemia-derived hematopoietic stem and progenitor cells. Nat. Med. 2021, 27, 677–687. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).