Association between Polymorphism rs61876744 in PNPLA2 Gene and Keratoconus in a Saudi Cohort
Abstract
:1. Introduction
2. Materials and Methods
2.1. Stduy Design and Cohort
2.2. DNA Preparation
2.3. Genotyping of rs138380 (G>A) and rs61876744 (T>C)
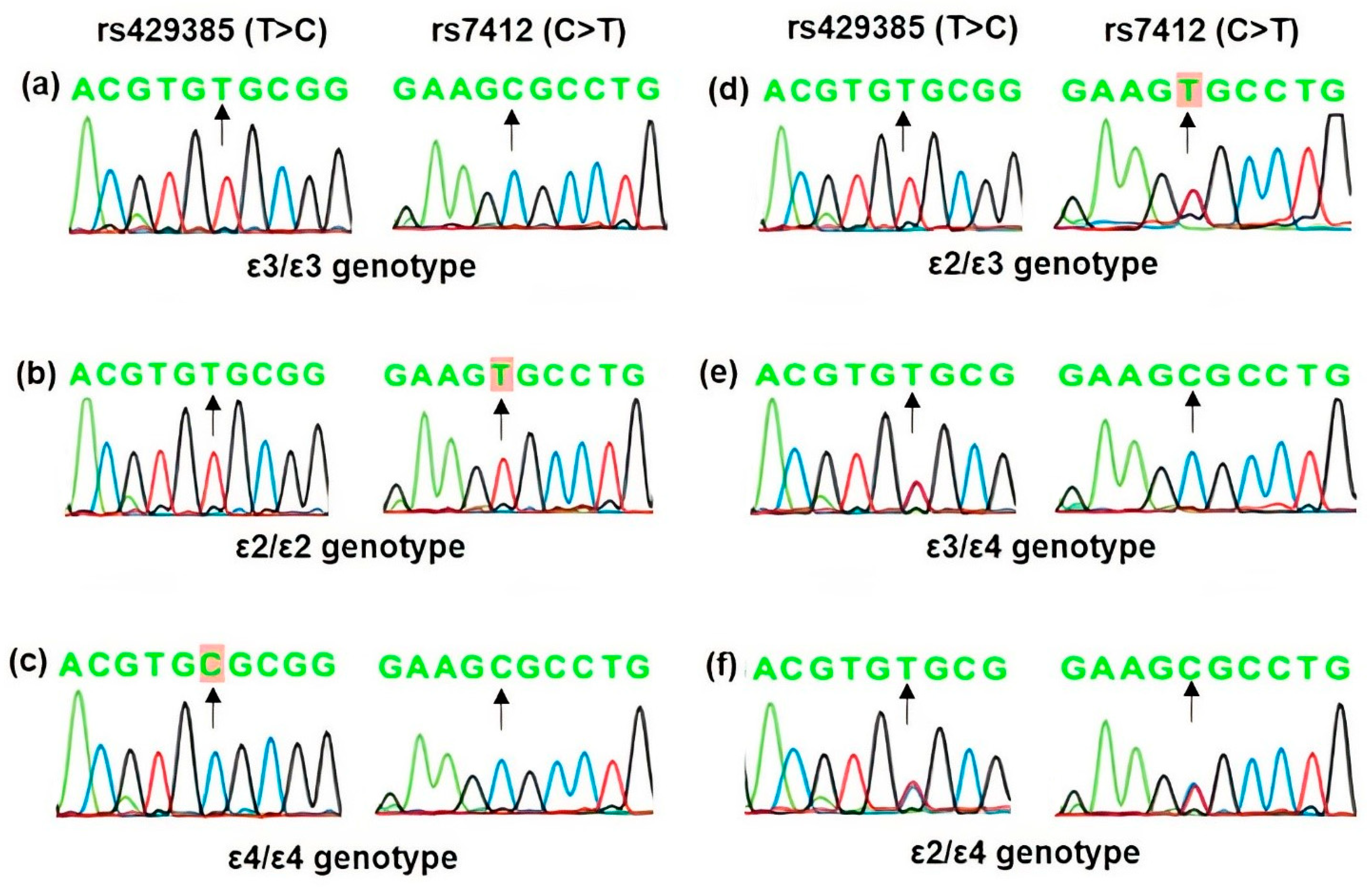
2.4. Genotyping of rs429358 (T>C) and rs7412 (C>T)
2.5. Statistics
3. Results
3.1. Demographic of Study Cohort
3.2. Allelic Association Analysis
3.3. Genotype Association Analysis
3.4. Regression Analysis
3.5. Power of This Study
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Davidson, A.E.; Hayes, S.; Hardcastle, A.J.; Tuft, S.J. The pathogenesis of keratoconus. Eye 2014, 28, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Shetty, R.; D’Souza, S.; Khamar, P.; Ghosh, A.; Nuijts, R.; Sethu, S. Biochemical markers and alterations in keratoconus. Asia Pac. J. Ophthalmol. 2020, 9, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Santodomingo-Rubido, J.; Carracedo, G.; Suzaki, A.; Villa-Collar, C.; Vincent, S.J.; Wolffsohn, J.S. Keratoconus: An updated review. Cont. Lens Anterior Eye 2022, 45, 101559. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, R.; Ong, Z.Z.; Rampat, R.; Alio Del Barrio, J.L.; Barua, A.; Ang, M.; Mehta, J.S.; Said, D.G.; Dua, H.S.; Ambrosio, R., Jr.; et al. Management of keratoconus: An updated review. Front. Med. 2023, 10, 1212314. [Google Scholar] [CrossRef]
- Almusawi, L.A.; Hamied, F.M. Risk factors for development of keratoconus: A matched pair case-control study. Clin. Ophthalmol. 2021, 15, 3473–3479. [Google Scholar] [CrossRef]
- Debourdeau, E.; Planells, G.; Chamard, C.; Touboul, D.; Villain, M.; Demoly, P.; Babeau, F.; Fournie, P.; Daien, V. New keratoconus risk factors: A cross-sectional case-control study. J. Ophthalmol. 2022, 2022, 6605771. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Heydarian, S.; Hooshmand, E.; Saatchi, M.; Yekta, A.; Aghamirsalim, M.; Valadkhan, M.; Mortazavi, M.; Hashemi, A.; Khabazkhoob, M. The prevalence and risk factors for keratoconus: A systematic review and meta-analysis. Cornea 2020, 39, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Soiberman, U.; Foster, J.W.; Jun, A.S.; Chakravarti, S. Pathophysiology of keratoconus: What do we know today. Open Ophthalmol. J. 2017, 11, 252–261. [Google Scholar] [CrossRef]
- Abu-Amero, K.K.; Al-Muammar, A.M.; Kondkar, A.A. Genetics of keratoconus: Where do we stand? J. Ophthalmol. 2014, 2014, 641708. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Li, X.Y.; Jin, J.J.; Shen, R.J.; Mao, J.Y.; Cheng, F.F.; Chen, Z.J.; Linardaki, E.; Voulgaraki, S.; Aslanides, I.M.; et al. Genetic screening revealed latent keratoconus in asymptomatic individuals. Front. Cell Dev. Biol. 2021, 9, 650344. [Google Scholar] [CrossRef]
- Loukovitis, E.; Sfakianakis, K.; Syrmakesi, P.; Tsotridou, E.; Orfanidou, M.; Bakaloudi, D.R.; Stoila, M.; Kozei, A.; Koronis, S.; Zachariadis, Z.; et al. Genetic aspects of keratoconus: A literature review exploring potential genetic contributions and possible genetic relationships with comorbidities. Ophthalmol. Ther. 2018, 7, 263–292. [Google Scholar] [CrossRef] [PubMed]
- Netto, E.A.T.; Al-Otaibi, W.M.; Hafezi, N.L.; Kling, S.; Al-Farhan, H.M.; Randleman, J.B.; Hafezi, F. Prevalence of keratoconus in paediatric patients in riyadh, saudi arabia. Br. J. Ophthalmol. 2018, 102, 1436–1441. [Google Scholar] [CrossRef] [PubMed]
- Froukh, T.; Hawwari, A.; Al Zubi, K. Whole exome sequencing highlights variants in association with keratoconus in jordanian families. BMC Med. Genet. 2020, 21, 177. [Google Scholar] [CrossRef]
- Lu, Y.; Vitart, V.; Burdon, K.P.; Khor, C.C.; Bykhovskaya, Y.; Mirshahi, A.; Hewitt, A.W.; Koehn, D.; Hysi, P.G.; Ramdas, W.D.; et al. Genome-wide association analyses identify multiple loci associated with central corneal thickness and keratoconus. Nat. Genet. 2013, 45, 155–163. [Google Scholar] [CrossRef] [PubMed]
- McComish, B.J.; Sahebjada, S.; Bykhovskaya, Y.; Willoughby, C.E.; Richardson, A.J.; Tenen, A.; Charlesworth, J.C.; MacGregor, S.; Mitchell, P.; Lucas, S.E.M.; et al. Association of genetic variation with keratoconus. JAMA Ophthalmol. 2020, 138, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Fish, K.J.; Cegielska, A.; Getman, M.E.; Landes, G.M.; Virshup, D.M. Isolation and characterization of human casein kinase i epsilon (cki), a novel member of the cki gene family. J. Biol. Chem. 1995, 270, 14875–14883. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Jin, J.; Wang, Q.; Xue, H.; Zhang, N.; Du, Y.; Zhang, T.; Zhang, B.; Wu, J.; Liu, Z. A de novo pathogenic csnk1e mutation identified by exome sequencing in family trios with epileptic encephalopathy. Hum. Mutat. 2019, 40, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Alagarsamy, J.; Jaeschke, A.; Hui, D.Y. Apolipoprotein e in cardiometabolic and neurological health and diseases. Int. J. Mol. Sci. 2022, 23, 9892. [Google Scholar] [CrossRef] [PubMed]
- Mahley, R.W.; Rall, S.C., Jr. Apolipoprotein e: Far more than a lipid transport protein. Annu. Rev. Genom. Hum. Genet. 2000, 1, 507–537. [Google Scholar] [CrossRef] [PubMed]
- Civeira-Marin, M.; Cenarro, A.; Marco-Benedi, V.; Bea, A.M.; Mateo-Gallego, R.; Moreno-Franco, B.; Ordovas, J.M.; Laclaustra, M.; Civeira, F.; Lamiquiz-Moneo, I. Apoe genotypes modulate inflammation independently of their effect on lipid metabolism. Int. J. Mol. Sci. 2022, 23, 12947. [Google Scholar] [CrossRef]
- Wu, Y.; Pang, J.; Peng, J.; Cao, F.; Guo, Z.; Jiang, L.; Teng, Z.; Huang, Z.; Cheng, C.; Jiang, Y.; et al. Apolipoprotein e deficiency aggravates neuronal injury by enhancing neuroinflammation via the jnk/c-jun pathway in the early phase of experimental subarachnoid hemorrhage in mice. Oxidative Med. Cell. Longev. 2019, 2019, 3832648. [Google Scholar] [CrossRef] [PubMed]
- Butterfield, D.A.; Mattson, M.P. Apolipoprotein e and oxidative stress in brain with relevance to alzheimer’s disease. Neurobiol. Dis. 2020, 138, 104795. [Google Scholar] [CrossRef] [PubMed]
- Hiebert, P.R.; Wu, D.; Granville, D.J. Granzyme b degrades extracellular matrix and contributes to delayed wound closure in apolipoprotein e knockout mice. Cell Death Differ. 2013, 20, 1404–1414. [Google Scholar] [CrossRef] [PubMed]
- Shinde, V.; Hu, N.; Renuse, S.; Mahale, A.; Pandey, A.; Eberhart, C.; Stone, D.; Al-Swailem, S.A.; Maktabi, A.; Chakravarti, S. Mapping keratoconus molecular substrates by multiplexed high-resolution proteomics of unpooled corneas. OMICS 2019, 23, 583–597. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, P.M.; Han, B.; Liu, F.; Mace, B.E.; Ervin, J.F.; Wu, S.; Koger, D.; Paul, S.; Bales, K.R. Reduced levels of human apoe4 protein in an animal model of cognitive impairment. Neurobiol. Aging 2011, 32, 791–801. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, J.W.; Bula, M.; Davila-Velderrain, J.; Akay, L.A.; Zhu, L.; Frank, A.; Victor, M.B.; Bonner, J.M.; Mathys, H.; Lin, Y.T.; et al. Reconstruction of the human blood-brain barrier in vitro reveals a pathogenic mechanism of apoe4 in pericytes. Nat. Med. 2020, 26, 952–963. [Google Scholar] [CrossRef] [PubMed]
- Abu-Amero, K.K.; Kondkar, A.A.; Azad, T.A.; Sultan, T.; Kalantan, H.; Al-Muammar, A.M. Keratoconus is associated with increased copy number of mitochondrial DNA. Mol. Vis. 2014, 20, 1203–1208. [Google Scholar] [PubMed]
- Zimmermann, R.; Strauss, J.G.; Haemmerle, G.; Schoiswohl, G.; Birner-Gruenberger, R.; Riederer, M.; Lass, A.; Neuberger, G.; Eisenhaber, F.; Hermetter, A.; et al. Fat mobilization in adipose tissue is promoted by adipose triglyceride lipase. Science 2004, 306, 1383–1386. [Google Scholar] [CrossRef]
- Hara, M.; Wu, W.; Malechka, V.V.; Takahashi, Y.; Ma, J.X.; Moiseyev, G. Pnpla2 mobilizes retinyl esters from retinosomes and promotes the generation of 11-cis-retinal in the visual cycle. Cell Rep. 2023, 42, 112091. [Google Scholar] [CrossRef]
- Subramanian, P.; Becerra, S.P. Role of the pnpla2 gene in the regulation of oxidative stress damage of rpe. Adv. Exp. Med. Biol. 2019, 1185, 377–382. [Google Scholar]
- You, J.; Corley, S.M.; Wen, L.; Hodge, C.; Hollhumer, R.; Madigan, M.C.; Wilkins, M.R.; Sutton, G. Rna-seq analysis and comparison of corneal epithelium in keratoconus and myopia patients. Sci. Rep. 2018, 8, 389. [Google Scholar] [CrossRef]
- Singh, P.P.; Singh, M.; Mastana, S.S. Apoe distribution in world populations with new data from india and the uk. Ann. Hum. Biol. 2006, 33, 279–308. [Google Scholar] [CrossRef] [PubMed]
- Di Battista, A.M.; Heinsinger, N.M.; Rebeck, G.W. Alzheimer’s disease genetic risk factor apoe-epsilon4 also affects normal brain function. Curr. Alzheimer Res. 2016, 13, 1200–1207. [Google Scholar] [CrossRef] [PubMed]
- Lumsden, A.L.; Mulugeta, A.; Zhou, A.; Hypponen, E. Apolipoprotein e (apoe) genotype-associated disease risks: A phenome-wide, registry-based, case-control study utilising the uk biobank. EBioMedicine 2020, 59, 102954. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, M.; Tashiro, Y.; Suzuki, K.; Fukumori, A.; Bu, G.; Sato, N. Interaction between apoe genotype and diabetes in cognitive decline. Alzheimers Dement. 2020, 12, e12006. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, K.L.; Tybjaerg-Hansen, A.; Nordestgaard, B.G.; Frikke-Schmidt, R. Associations of alzheimer disease-protective apoe variants with age-related macular degeneration. JAMA Ophthalmol. 2023, 141, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Levy, O.; Lavalette, S.; Hu, S.J.; Housset, M.; Raoul, W.; Eandi, C.; Sahel, J.A.; Sullivan, P.M.; Guillonneau, X.; Sennlaub, F. Apoe isoforms control pathogenic subretinal inflammation in age-related macular degeneration. J. Neurosci. 2015, 35, 13568–13576. [Google Scholar] [CrossRef]
- Davignon, J.; Gregg, R.E.; Sing, C.F. Apolipoprotein e polymorphism and atherosclerosis. Arteriosclerosis 1988, 8, 1–21. [Google Scholar] [CrossRef]
- Guillaume, D.; Bertrand, P.; Dea, D.; Davignon, J.; Poirier, J. Apolipoprotein e and low-density lipoprotein binding and internalization in primary cultures of rat astrocytes: Isoform-specific alterations. J. Neurochem. 1996, 66, 2410–2418. [Google Scholar] [CrossRef]
- Shea, T.B.; Rogers, E.; Ashline, D.; Ortiz, D.; Sheu, M.S. Apolipoprotein e deficiency promotes increased oxidative stress and compensatory increases in antioxidants in brain tissue. Free Radic. Biol. Med. 2002, 33, 1115–1120. [Google Scholar] [CrossRef]
- Piccarducci, R.; Daniele, S.; Polini, B.; Carpi, S.; Chico, L.; Fusi, J.; Baldacci, F.; Siciliano, G.; Bonuccelli, U.; Nieri, P.; et al. Apolipoprotein e polymorphism and oxidative stress in human peripheral blood cells: Can physical activity reactivate the proteasome system through epigenetic mechanisms? Oxidative Med. Cell. Longev. 2021, 2021, 8869849. [Google Scholar] [CrossRef]
- Dose, J.; Huebbe, P.; Nebel, A.; Rimbach, G. Apoe genotype and stress response—A mini review. Lipids Health Dis. 2016, 15, 121. [Google Scholar] [CrossRef]
- Wojcik, K.A.; Kaminska, A.; Blasiak, J.; Szaflik, J.; Szaflik, J.P. Oxidative stress in the pathogenesis of keratoconus and fuchs endothelial corneal dystrophy. Int. J. Mol. Sci. 2013, 14, 19294–19308. [Google Scholar] [CrossRef] [PubMed]
| rs138380 | Primers and Probe Sequences (5′–3′) |
|---|---|
| Forward Primer | GGGAAACAATCAAATATTTTGACAAATAATCGT |
| Reverse Primer | CTCAGAAAATAATTCAGTAGCAACAAGGT |
| Probe Reporter dye [VIC/FAM] | CCAGGAATC[T/C]CCTTGTT |
| rs61876744 | |
| Forward Primer | TGAACTTTGTCCTGGGAGGGA |
| Reverse Primer | GGCTGTTCCCAATAATAGCTCTAGT |
| Probe Reporter dye [VIC/FAM] | CAGAAGTGAACC[T/C]CTCAGG |
| PCR Primers | Primer Sequences (5′–3′) |
|---|---|
| APOE-Forward | TGTAAAACGACGGCCAGTGACCATGAAGGAGTTGAAGGCCTAC |
| APOE-Reverse | CAGGAAACAGCTATGACCGATGGCGCTGAGGCCGCGCT |
| Sequencing Primers | |
| M13-Forward | TGTAAAACGACGGCCAGT |
| M13-Reverse | CAGGAAACAGCTATGACC |
| Type | n | Mean Age, Years (SD) | % Male |
|---|---|---|---|
| Keratoconus | 98 | 25.8 (7.3) | 56 |
| Controls | 167 | 60.1 (8.1) | 52 |
| SNP ID | Gene/ Locus | Chromosome | Position * | Minor Allele | Minor Allele Frequency | Odds Ratio (95% Confidence Interval) | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Controls | Cases | |||||||
| rs138380 | CSNK1E | 22q13.1 | 38400624 | G | 0.50 | 0.52 | 1.06 (0.74–1.51) | 0.729 |
| rs61876744 | PNPLA2 | 11p15.5 | 820754 | T | 0.43 | 0.33 | 0.64 (0.44–0.93) | 0.020 |
| rs429358 | APOE | 19q13.32 | 44908683 | C | 0.09 | 0.10 | 1.05 (0.57–1.91) | 0.887 |
| rs7412 | APOE | 19q13.32 | 44908821 | T | 0.03 | 0.03 | 1.14 (0.40–3.25) | 0.806 |
| SNP ID | Genetic Model | Genotype | Control n (%) | Cases n (%) | Odds Ratio (95% Confidence Interval) | p-Value |
|---|---|---|---|---|---|---|
| rs138380 | Additive | A/A | 43 (25.8) | 27 (27.6) | 1.00 | - |
| G/A | 81 (48.5) | 41 (41.8) | 0.80 (0.437–0.148) | 0.488 | ||
| G/G | 43 (25.8) | 30 (30.6) | 1.11 (0.56–2.17) | 0.764 | ||
| Dominant | A/A | 43 (25.8) | 27 (27.6) | 1.00 | ||
| G/G-G/A | 124 (74.2) | 71 (72.5) | 0.91 (0.52–1.60) | 0.751 | ||
| Recessive | G/A-A/A | 124 (74.2 | 68 (69.4) | 1.00 | ||
| G/G | 43 (25.8) | 30 (30.6) | 1.27 (0.73–2.20) | 0.392 | ||
| CA trend * | 167/167 | 101/95 | 1.06 (0.74–1.51) | 0.729 | ||
| rs61876744 | Additive | C/C | 56 (33.5) | 48 (49) | 1.00 | - |
| T/C | 79 (47.3) | 36 (36.7) | 0.53 (0.31–0.92) | 0.024 | ||
| T/T | 32 (19.2) | 14 (14.3) | 0.51 (0.24–1.07) | 0.071 | ||
| Dominant | C/C | 56 (33.5) | 48 (49) | 1.00 | ||
| T/C-T/T | 111 (66.5) | 50 (51) | 0.53 (0.32–0.88) | 0.013 | ||
| Recessive | C/C-T/C | 135 (80.8) | 84 (85.7) | 1.00 | ||
| T/T | 32 (19.2) | 14 (14.3) | 0.70 (0.35–1.39) | 0.310 | ||
| CA trend * | 143/191 | 64/132 | 0.64 (0.44–0.93) | 0.020 |
| SNP ID | Genetic Model | Genotype | Control n (%) | Cases n (%) | Odds Ratio (95% Confidence Interval) | p-Value |
|---|---|---|---|---|---|---|
| rs429358 | Additive | T/T | 136 (81.4) | 82 (83.7) | 1.00 | - |
| T/C | 31 (18.6) | 13 (13.3) | 0.70 (0.34–1.41) | 0.310 | ||
| C/C | 0 (0) | 3 (3.1) | NA (0.00–NA) | 0.055 † | ||
| Dominant | T/T | 136 (81.4) | 82 (83.7) | 1.00 | ||
| T/C-C/C | 31 (18.6) | 16 (16.3) | 0.86 (0.44–1.66) | 0.640 | ||
| Recessive | T/T-T/C | 167 (100) | 95 (96.9) | 1.00 | ||
| C/C | 0 (0) | 3 (3.1) | NA (0.00–NA) | 0.014 | ||
| CA trend * | 31/303 | 19/177 | 1.05 (0.57–1.91) | 0.887 | ||
| rs7412 | Additive | C/C | 159 (95.2) | 92 (93.8) | 1.00 | - |
| C/T | 7 (4.2) | 6 (6.1) | 1.48 (0.48–4.52) | 0.560 | ||
| T/T | 1 (0.6) | 0 (0) | NA (0.00–NA) | 1.00 † | ||
| Dominant | C/C | 159 (95.2) | 92 (89.8) | 1.00 | ||
| C/T-T/T | 8 (4.8) | 6 (10.2) | 1.29 (0.43–3.85) | 0.639 | ||
| Recessive | C/C-C/T | 166 (99.4) | 98 (100) | 1.00 | ||
| T/T | 1 (0.6) | 0 (0) | NA (0.00–NA) | 0.340 | ||
| CA trend * | 9/325 | 6/190 | 1.14 (0.39–3.25) | 0.806 |
| APOE | Controls n (%) | Cases n (%) | Odds Ratio (95% Confidence Interval) | p-Value |
|---|---|---|---|---|
| Alleles | ||||
| ε3 | 294 (88.0) | 171 (87.2) | 1.00 | - |
| ε2 | 9 (2.7) | 6 (3.1) | 1.14 (0.40–3.27) | 0.806 |
| ε4 | 31 (9.2) | 19 (9.7) | 1.08 (0.59–1.96) | 0.862 |
| Genotypes | ||||
| ε2/ε2 | 01 (0.6) | 00 (0) | 0.00 (0.00–NA) | 0.770 |
| ε2/ε3 | 01 (0.6) | 06 (6.1) | 10.5 (1.25–89.52) | 0.012 |
| ε2/ε4 | 06 (3.6) | 00 (0) | 0.00 (0.00–NA) | 0.092 |
| ε3/ε3 | 134 (80.2) | 76 (77.5) | 1.00 | - |
| ε3/ε4 | 25 (15.0) | 13 (13.3) | 0.91 (0.44–1.89) | 0.823 |
| ε4/ε4 | 00 (0) | 03 (3.1) | 0.00 (0.00–NA) | 0.095 |
| Carrier a | ||||
| ε3/ε3 | 134 (83.2) | 76 (80.8) | 1.00 | - |
| ε*2 b | 02 (1.2) | 06 (6.4) | 5.28 (1.04–26.8) | 0.055 |
| ε*4 c | 25 (15.5) | 16 (12.8) | 1.12 (0.56–2.24) | 0.730 |
| Group Variables | B | SE | Wald | p-Value |
|---|---|---|---|---|
| Age | −1.102 | 0.627 | 3.090 | 0.079 |
| Sex | 3.859 | 2.182 | 3.127 | 0.077 |
| rs138380 | 2.462 | 0.292 | ||
| G/A | 9.775 | 6.553 | 2.225 | 0.136 |
| G/G | 5.520 | 4.783 | 1.332 | 0.248 |
| rs61876744 | 1.111 | 0.574 | ||
| C/T | −0.298 | 2.305 | 0.017 | 0.897 |
| T/T | 3.214 | 3.051 | 1.110 | 0.292 |
| rs429358 | 2.262 | 0.323 | ||
| T/C | −0.603 | 0.401 | 2.262 | 0.133 |
| C/C | 21.578 | 23,051.628 | 0.000 | 0.999 |
| rs7412 | 0.036 | 0.982 | ||
| C/T | 1.473 | 7.727 | 0.036 | 0.849 |
| T/T | 10.171 | 27,454.935 | 0.000 | 1.000 |
| Constant | 35.883 | 20.081 | 3.193 | 0.074 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kondkar, A.A.; Azad, T.A.; Sultan, T.; Khatlani, T.; Alshehri, A.A.; Lobo, G.P.; Kalantan, H.; Al-Obeidan, S.A.; Al-Muammar, A.M. Association between Polymorphism rs61876744 in PNPLA2 Gene and Keratoconus in a Saudi Cohort. Genes 2023, 14, 2108. https://doi.org/10.3390/genes14122108
Kondkar AA, Azad TA, Sultan T, Khatlani T, Alshehri AA, Lobo GP, Kalantan H, Al-Obeidan SA, Al-Muammar AM. Association between Polymorphism rs61876744 in PNPLA2 Gene and Keratoconus in a Saudi Cohort. Genes. 2023; 14(12):2108. https://doi.org/10.3390/genes14122108
Chicago/Turabian StyleKondkar, Altaf A., Taif A. Azad, Tahira Sultan, Tanvir Khatlani, Abdulaziz A. Alshehri, Glenn P. Lobo, Hatem Kalantan, Saleh A. Al-Obeidan, and Abdulrahman M. Al-Muammar. 2023. "Association between Polymorphism rs61876744 in PNPLA2 Gene and Keratoconus in a Saudi Cohort" Genes 14, no. 12: 2108. https://doi.org/10.3390/genes14122108
APA StyleKondkar, A. A., Azad, T. A., Sultan, T., Khatlani, T., Alshehri, A. A., Lobo, G. P., Kalantan, H., Al-Obeidan, S. A., & Al-Muammar, A. M. (2023). Association between Polymorphism rs61876744 in PNPLA2 Gene and Keratoconus in a Saudi Cohort. Genes, 14(12), 2108. https://doi.org/10.3390/genes14122108







