Modeling Evaporation of Water Droplets as Applied to Survival of Airborne Viruses
Abstract
:1. Introduction
2. Evaporation of Airborne Microdroplets Carrying Viruses
2.1. Environmental Factors Affecting Airborne Viruses
2.2. Motion of Microdroplets in Ambient Air
2.3. Modeling of Evaporation of Microdroplets
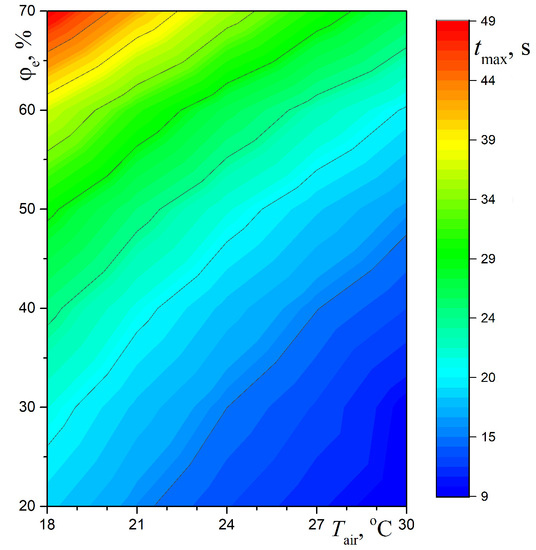
2.4. Numerical Results for Evaporation of Water Droplets
2.5. Effect of Solar Radiation
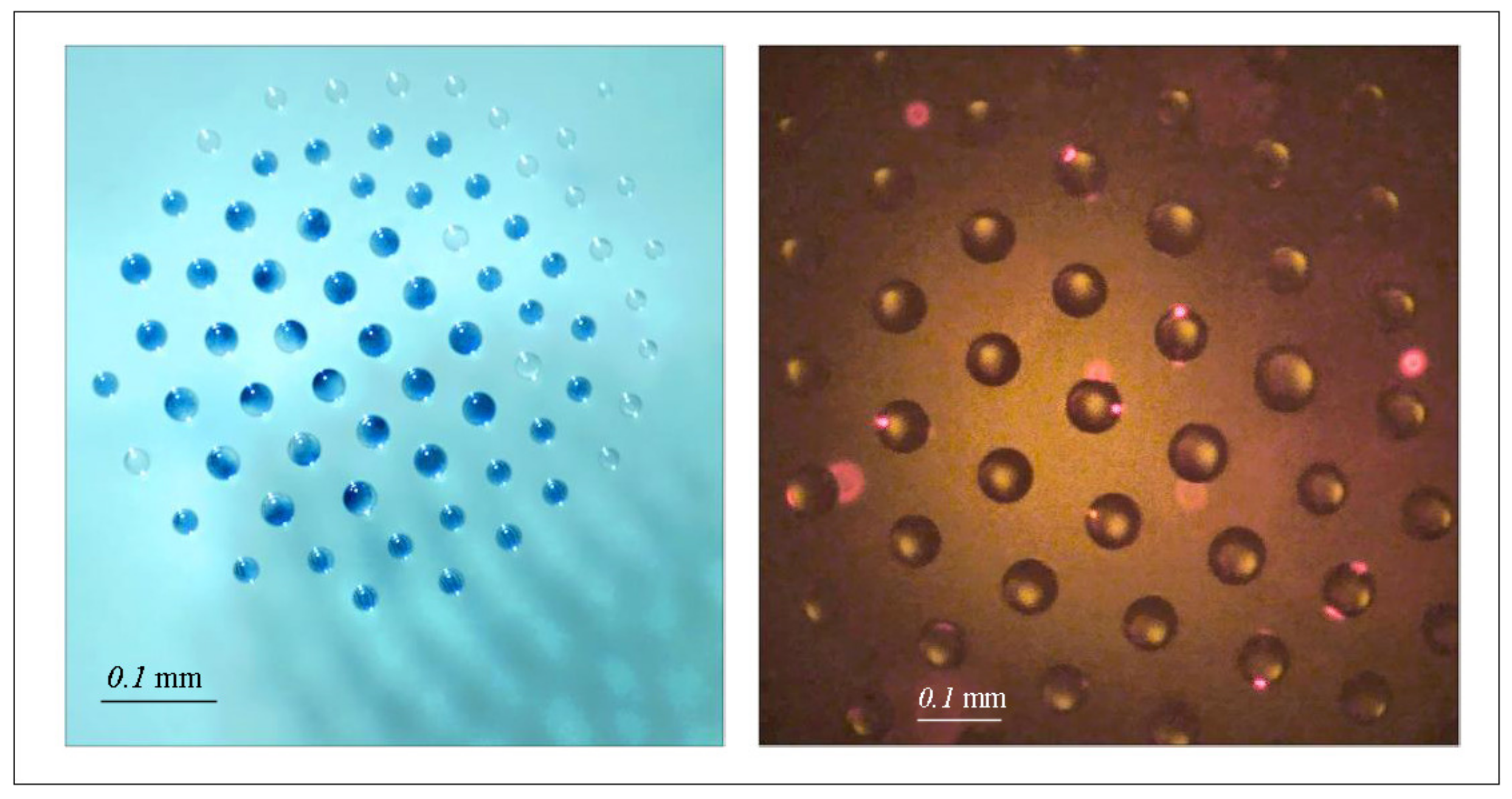
3. A Promising Technology for Tracing Submicron Scaled Particles in Bioaerosols
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Stilianakais, N.I.; Drossinos, Y. Dynamics of infectious disease transmission by inhalable respiratory droplets. J. R. Soc. Interface 2010, 7, 1355–1366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bourouiba, L. Turbulent gas clouds and respiratory pathogen emissions: Potential implications for reducing transmission of COVID-19. J. Am. Med. Assoc. 2020, 323, 1837–1838. [Google Scholar] [CrossRef] [PubMed]
- Lewis, D. Is the coronavirus airborne? Experts can’t agree. Nature 2020, 580, 175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 362, 1564–1567. [Google Scholar] [CrossRef]
- Shiu, E.Y.C.; Leung, N.H.L.; Cowling, B.J. Controversy around airborne versus droplet transmission of respiratory viruses: Implication for infection prevention. Curr. Opin. Infect. Dis. 2019, 32, 372–379. [Google Scholar] [CrossRef]
- Stadnytskyi, V.; Bax, C.E.; Bax, A.; Anfinrud, P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc. Nat. Acad. Sci. USA 2020, 117, 11875–11877. [Google Scholar] [CrossRef]
- Tellier, R.; Li, Y.; Cowling, B.J.; Tang, J.W. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect. Dis. 2019, 19, 101. [Google Scholar] [CrossRef]
- Lowen, A.C.; Steel, J. Roles of humidity and temperature in shaping influenza seasonality. J. Virol. 2014, 88, 7692–7695. [Google Scholar] [CrossRef] [Green Version]
- Mittal, R.; Ni, R.; Seo, J.H. The flow physics of COVID-19. J. Fluid Mech. 2020, 894, F2. [Google Scholar] [CrossRef]
- Després, V.R.; Huffman, J.A.; Burrows, S.M.; Hoose, C.; Safatov, A.S.; Buryak, G.; Fröhlich-Nowoisky, J.; Elbert, W.; Andreae, M.O.; Pöschl, U.; et al. Primary biological aerosol particles in the atmosphere: A review. Tellus B Chem. Phys. Meteorol. 2012, 64, 15598. [Google Scholar] [CrossRef] [Green Version]
- Joung, Y.S.; Ge, Z.; Buie, C.R. Bioaerosol generation by raindrops on soil. Nat. Commun. 2017, 8, 14668. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, M.; Weber, P.K.; Smith, J.B.; Hutcheon, J.D.; Klyce, B.; Wickramasinghe, N.C.; Narlikar, J.V.; Rajaratnam, P. Studies on bacteria-like particles sampled from the stratosphere. Aerobiologia 2004, 20, 237–240. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.; Yan, X.; Cao, W.; Wang, C.; Feng, J.; Duan, J.; Xie, S. Probing the structure of the SARS coronavirus using scanning electron microscopy. Antivir. Ther. 2004, 9, 287–289. [Google Scholar] [PubMed]
- Almeida, J.D.; Berry, D.M.; Cunningham, C.H.; Hamre, D.; Hofstad, M.S.; Mallucci, L.; McIntosh, K.; Tyrrell, D.A.J. Virology: Coronaviruses. Nature 1968, 220, 650. [Google Scholar]
- Fedorets, A.A.; Bormashenko, E.; Dombrovsky, L.A.; Nosonovsky, M. Droplet clusters: Nature-inspired biological reactors and aerosols. Philos. Trans. R. Soc. A 2019, 377, 20190121. [Google Scholar] [CrossRef] [Green Version]
- Perlmutter, J.D.; Hagan, M.F. Mechanisms of virus assembly. Annu. Rev. Phys. Chem. 2015, 66, 217–239. [Google Scholar] [CrossRef] [Green Version]
- Fedorets, A.A. Droplet cluster. JETP Lett. 2004, 79, 372–374. [Google Scholar] [CrossRef]
- Dombrovsky, L.A.; Fedorets, A.A.; Medvedev, D.N. The use of infrared irradiation to stabilize levitating clusters of water droplets. Infrared Phys. Technol. 2016, 75, 124–132. [Google Scholar] [CrossRef]
- Fedorets, A.A.; Dombrovsky, L.A. Generation of levitating droplet clusters above the locally heated water surface: A thermal analysis of modified installation. Int. J. Heat Mass Transf. 2017, 104, 1268–1274. [Google Scholar] [CrossRef]
- Fedorets, A.A.; Dombrovsky, L.A.; Ryumin, P.I. Expanding the temperature range for generation of droplet clusters over the locally heated water surface. Int. J. Heat Mass Transf. 2017, 113, 1054–1058. [Google Scholar] [CrossRef]
- Fedorets, A.A.; Frenkel, M.; Shulzinger, E.; Dombrovsky, L.A.; Bormashenko, E.; Nosonovsky, M. Self-assembled levitating clusters of water droplets: Pattern-formation and stability. Sci. Rep. 2017, 7, 1888. [Google Scholar] [CrossRef] [PubMed]
- Fedorets, A.A.; Frenkel, M.; Bormashenko, E.; Nosonovsky, M. Small levitating ordered droplet clusters: Stability, symmetry, and Voronoi entropy. J. Phys. Chem. Lett. 2017, 8, 5599–5602. [Google Scholar] [CrossRef] [PubMed]
- Dombrovsky, L.A.; Fedorets, A.A.; Levashov, V.Y.; Kryukov, A.P.; Bormashenko, E.; Nosonovsky, M. Stable cluster of identical water droplets formed under the infrared irradiation: Experimental study and theoretical modeling. Int. J. Heat Mass Transfer 2020, 161, 120255. [Google Scholar] [CrossRef]
- Fedorets, A.A.; Dombrovsky, L.A.; Gabyshev, D.N.; Bormashenko, E.; Nosonovsky, M. An effect of external electric field on dynamics of levitating water droplets. Int. J. Therm. Sci. 2020, 153, 106375. [Google Scholar] [CrossRef]
- Chaudhuri, S.; Basu, S.; Kabi, P.; Unni, V.R.; Saha, A. Modelling the role of respiratory droplets in COVID-19 type pandemics. Phys. Fluids 2020, 32, 063309. [Google Scholar] [CrossRef]
- Dombrovsky, L.A.; Levashov, V.Y.; Kryukov, A.P.; Dembele, S.; Wen, J.X. A comparative analysis of shielding of thermal radiation of fires using mist curtains containing droplets of pure water or sea water. Int. J. Therm. Sci. 2020, 152, 106299. [Google Scholar] [CrossRef]
- Agranovski, I.E.; Safatov, A.S.; Pyankov, O.V.; Sergeev, A.N.; Agafonov, A.P.; Ignatiev, G.M.; Ryabchikova, E.I.; Borodulin, A.I.; Sergeev, A.A.; Doerr, H.W.; et al. Monitoring of viable airborne SARS virus in ambient air. Atmos. Environ. 2004, 38, 3879–3884. [Google Scholar] [CrossRef]
- Bhardway, R.; Agrawal, A. Likelihood of survival of coronavirus in a respiratory droplet deposited on a solid surface. Phys. Fluids 2020, 32, 061704. [Google Scholar] [CrossRef]
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmann, E. Persistence of coronavituses on inanimate surfaces and their inactivation with biological agents. J. Hosp. Infect. 2020, 104, 246–251. [Google Scholar] [CrossRef] [Green Version]
- Bormashenko, E.Y. Wetting of Real Surfaces, 2nd ed.; De Gruyter: Berlin, Germany, 2019. [Google Scholar]
- Mukherjee, D.V.; Cohen, B.; Bovino, M.E.; Desai, S.; Whittier, S.; Larson, E.L. Survival of influenza virus on hands and fomites in community and laboratory settings. Am. J. Infect. Control 2012, 40, 590–594. [Google Scholar] [CrossRef]
- Oxford, J.; Berezin, E.N.; Courvalin, P.; Dwyer, D.E.; Exner, M.; Jana, L.A.; Kaku, M.; Lee, C.; Letlape, K.; Low, D.E.; et al. The survival of influenza A(H1N1)pdm09 virus on 4 household surfaces. Am. J. Infect. Control 2014, 42, 423–425. [Google Scholar] [CrossRef] [PubMed]
- Otter, J.A.; Donskey, C.; Yezli, S.; Douthwaite, S.; Goldenberg, S.D.; Weber, D.J. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: The possible role of dry surface contamination. J. Hosp. Infect. 2016, 92, 235–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ijaz, M.K.; Karim, Y.G.; Sattar, S.A.; Johnson-Lussenburg, C.M. Development of methods to study the survival of airborne viruses. J. Virol. Meth. 1987, 18, 87–106. [Google Scholar] [CrossRef]
- Harper, G.J. Airborne micro-organisms: Survival tests with four viruses. J. Hyg. 1961, 59, 479–486. [Google Scholar] [CrossRef] [Green Version]
- Schaffer, F.L.; Soergel, M.E.; Straube, D.C. Survival of airborne influenza virus: Effects of propagating host, relative humidity, and composition of spray fluids. Arch. Virol. 1976, 51, 263–273. [Google Scholar] [CrossRef]
- Zhao, Y.; Aarnink, A.J.A.; Dijkman, R.; Fabri, T.; De Jong, M.C.M.; Koerkamp, P.W.G.G. Effects of temperature, relative humidity, absolute humidity, and evaporation potential on survival of airborne gumboro vaccine virus. Appl. Environ. Microbiol. 2012, 78, 1048–1054. [Google Scholar] [CrossRef] [Green Version]
- Ijaz, M.K.; Brunner, A.H.; Sattar, S.A.; Nair, R.C.; Johnson-Lussenburg, C.M. Survival characteristics of airborne human coronavirus 229E. J. Gen. Virol. 1985, 66, 2743–2748. [Google Scholar] [CrossRef]
- Pyankov, O.V.; Bodnev, S.A.; Pyankova, O.G.; Agranovski, I.E. Survival of aerosolized coronavirus in the ambient air. J. Aerosol Sci. 2018, 115, 158–163. [Google Scholar] [CrossRef]
- Kormuth, K.A.; Lin, K.; Qian, Z.; Myerburg, M.M.; Marr, L.C.; Lakdawala, S.S. Environmental persistence of influenza viruses is dependent upon virus type and host origin. mSphere 2019, 4, e00552-19. [Google Scholar] [CrossRef] [Green Version]
- Tamerius, J.; Nelson, M.I.; Zhou, S.Z.; Viboud, C.; Miller, M.A.; Alonso, W.J. Global influenza seasonality: Reconciling pattern across temperate and tropical regions. Environ. Health Perspect. 2011, 119, 439–445. [Google Scholar] [CrossRef] [Green Version]
- Reche, I.; D’Orta, G.; Mladenov, N.; Winget, D.M.; Suttle, C.A. Deposition rates of viruses and bacteria above the atmospheric boundary layer. ISME J. 2018, 12, 1154–1162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, W.; Marr, L.C. Mechanisms by which ambient humidity may affect viruses in aerosols. Appl. Environ. Microbiol. 2012, 78, 6781–6788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linn, K.; Marr, L.C. Humidity-dependent decay of viruses, but not bacteria, in aerosols and droplets follows disinfection kinetics. Environ. Sci. Technol. 2020, 54, 1024–1032. [Google Scholar] [CrossRef] [PubMed]
- Marr, L.C.; Tang, J.W.; Van Mullekom, J.; Lakdawala, S.S. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J. R. Soc. Interface 2019, 16, 20180298. [Google Scholar] [CrossRef]
- Duan, S.M.; Zhao, X.S.; Wen, R.F.; Huang, J.J.; Pi, G.H.; Zhang, S.X.; Han, J.; Bi, S.L.; Ruan, L.; Dong, X.P. Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed. Environ. Sci. 2003, 16, 246–255. [Google Scholar]
- Rabenau, H.F.; Cinatl, J.; Morgenstern, B.; Bauer, G.; Preiser, W.; Doerr, H.W. Stability and inactivation of SARS coronavirus. Med. Microbiol. Immunol. 2005, 194, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Chaudhuri, S.; Basu, S.; Saha, A. Analysing the dominant SARS-CoV-2 transmission routes towards an ab-initio SEIR model. arXiv 2020, arXiv:2007.13596. [Google Scholar]
- Kryukov, A.P.; Levashov, V.Y.; Sazhin, S.S. Evaporation of diesel fuel droplets: Kinetic versus hydrodynamic models. Int. J. Heat Mass Transf. 2004, 47, 2541–2549. [Google Scholar] [CrossRef]
- Kryukov, A.P.; Levashov, V.Y.; Shishkova, I.N. Evaporation in mixture of vapour and gas mixture. Int. J. Heat Mass Transf. 2009, 52, 5585–5590. [Google Scholar] [CrossRef]
- Levashov, V.Y.; Kryukov, A.P. Numerical simulation of water droplet evaporation into vapor–gas medium. Colloid J. 2017, 79, 647–653. [Google Scholar] [CrossRef]
- Levashov, V.Y.; Kryukov, A.P.; Shishkova, I.N. Influence of the noncondensable component on the characteristics of temperature change and the intensity of water droplet evaporation. Int. J. Heat Mass Transf. 2018, 127, 115–122. [Google Scholar] [CrossRef]
- Borodulin, V.Y.; Letushko, V.N.; Nizovtsev, M.I.; Sterlyagov, A.N. Determination of parameters of heat and mass transfer in evaporating drops. Int. J. Heat Mass Transf. 2017, 109, 609–618. [Google Scholar] [CrossRef]
- Sirignano, W.A. Fluid Dynamics and Transport of Droplets and Sprays; Cambridge University Press: Cambridge, UK, 1999. [Google Scholar]
- Dombrovsky, L.A.; Sazhin, S.S. A simplified non-isothermal model for droplet heating and evaporation. Int. Commun. Heat Mass Transf. 2003, 30, 787–796. [Google Scholar] [CrossRef]
- Erbil, Y. Evaporation of pure liquid sessile and spherical suspended drops: A review. Adv. Colloid Interface Sci. 2012, 170, 67–86. [Google Scholar] [CrossRef] [PubMed]
- Sazhin, S. Droplets and Sprays; Springer: London, UK, 2014. [Google Scholar]
- Lefebvre, H.; McDonell, V.G. Atomizastion and Strays, 2nd ed.; CRC Press: New York, NY, USA, 2017. [Google Scholar]
- Stull, D.R. Vapor pressure of pure substances. Organic and inorganic compounds. Ind. Eng. Chem. 1947, 39, 517–550. [Google Scholar] [CrossRef]
- Dombrovsky, L.A.; Frenkel, M.; Legchenkova, I.; Bormashenko, E. Effect of thermal properties of a substrate on formation of self-arranged surface structures on evaporated polymer films. Int. J. Heat Mass Transf. 2020, 158, 120053. [Google Scholar] [CrossRef]
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 2020, 582, 557–560. [Google Scholar] [CrossRef]
- Hu, J.; Lei, C.; Chen, Z.; Liu, W.; Hu, X.; Pei, R.; Su, Z.; Deng, F.; Huang, Y.; Sun, X.; et al. Airborne SARS-CoV-2 and the use of masks for protection against its spread in Wuhan, China. Preprints 2020, 2020050464. [Google Scholar]
- Contini, D.; Costabile, F. Does air pollution influence COVID-19 outbreaks? Atmosphere 2020, 11, 377. [Google Scholar] [CrossRef] [Green Version]
- Dombrovsky, L.A.; Baillis, D. Thermal Radiation in Disperse Systems: An Engineering Approach; Begell House: New York, NY, USA, 2010. [Google Scholar]
- Dombrovsky, L.A.; Solovjov, V.P.; Webb, B.W. Attenuation of solar radiation by water mist and sprays from the ultraviolet to the infrared range. J. Quant. Spectr. Radiat. Transf. 2011, 112, 1182–1190. [Google Scholar] [CrossRef]
- Bohren, C.F.; Huffman, D.R. Absorption and Scattering of Light by Small Particles; Wiley: New York, NY, USA, 1983. [Google Scholar]
- Mishchenko, M.I.; Travis, L.D.; Lacis, A.A. Scattering, Absorption, and Emission of Light by Small Particles; Cambridge University Press: Cambridge, MA, USA, 2002. [Google Scholar]
- Hale, G.M.; Querry, M.P. Optical constants of water in the 200 nm to 200 μm wavelength region. Appl. Opt. 1973, 12, 555–563. [Google Scholar] [CrossRef]






© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dombrovsky, L.A.; Fedorets, A.A.; Levashov, V.Y.; Kryukov, A.P.; Bormashenko, E.; Nosonovsky, M. Modeling Evaporation of Water Droplets as Applied to Survival of Airborne Viruses. Atmosphere 2020, 11, 965. https://doi.org/10.3390/atmos11090965
Dombrovsky LA, Fedorets AA, Levashov VY, Kryukov AP, Bormashenko E, Nosonovsky M. Modeling Evaporation of Water Droplets as Applied to Survival of Airborne Viruses. Atmosphere. 2020; 11(9):965. https://doi.org/10.3390/atmos11090965
Chicago/Turabian StyleDombrovsky, Leonid A., Alexander A. Fedorets, Vladimir Yu. Levashov, Alexei P. Kryukov, Edward Bormashenko, and Michael Nosonovsky. 2020. "Modeling Evaporation of Water Droplets as Applied to Survival of Airborne Viruses" Atmosphere 11, no. 9: 965. https://doi.org/10.3390/atmos11090965
APA StyleDombrovsky, L. A., Fedorets, A. A., Levashov, V. Y., Kryukov, A. P., Bormashenko, E., & Nosonovsky, M. (2020). Modeling Evaporation of Water Droplets as Applied to Survival of Airborne Viruses. Atmosphere, 11(9), 965. https://doi.org/10.3390/atmos11090965