How Is Indoor Air Quality during Sleep? A Review of Field Studies
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Data Extraction
3. Results
3.1. Studies’ Settings
3.2. Evaluation of Environmental Parameters
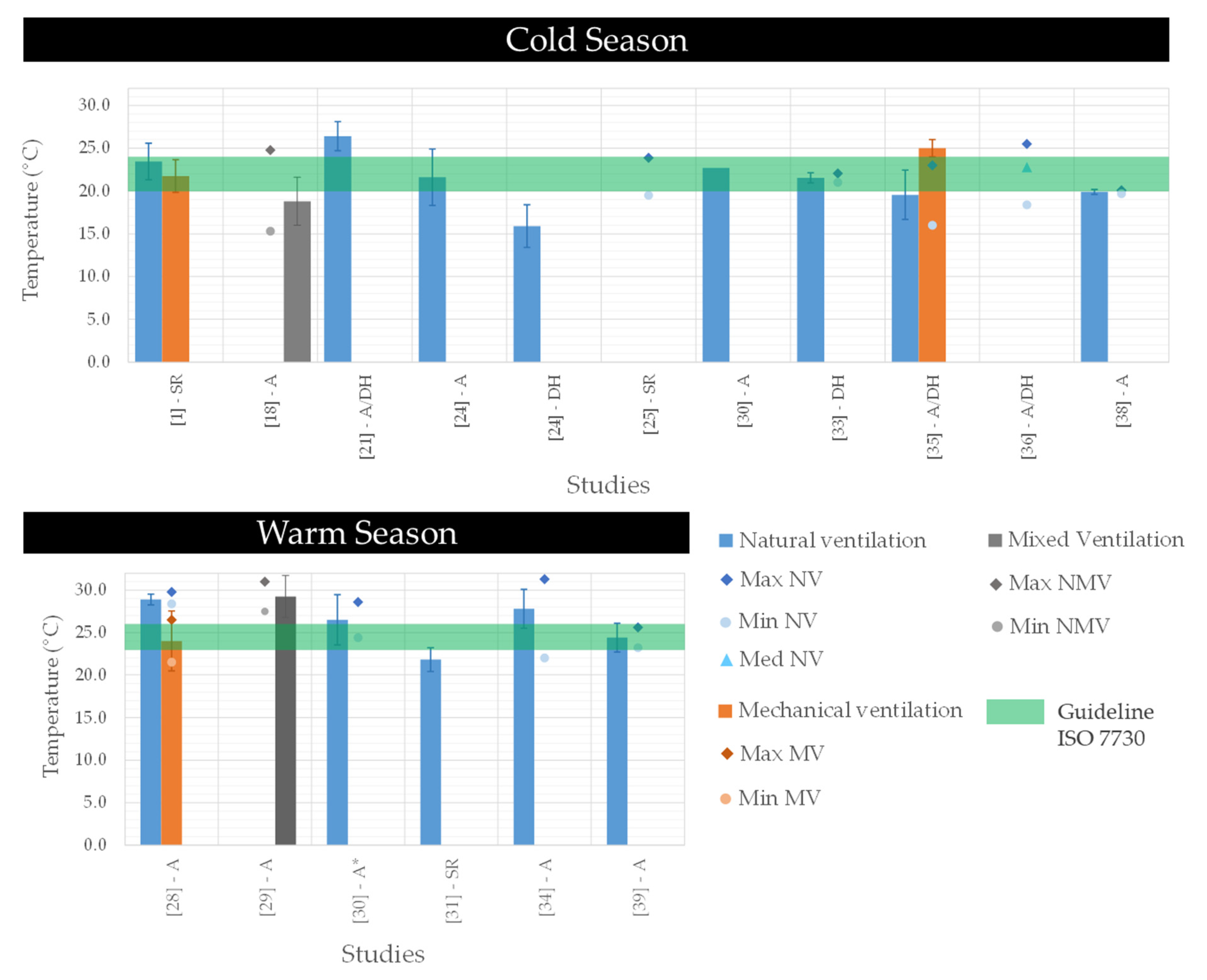
3.2.1. Temperature
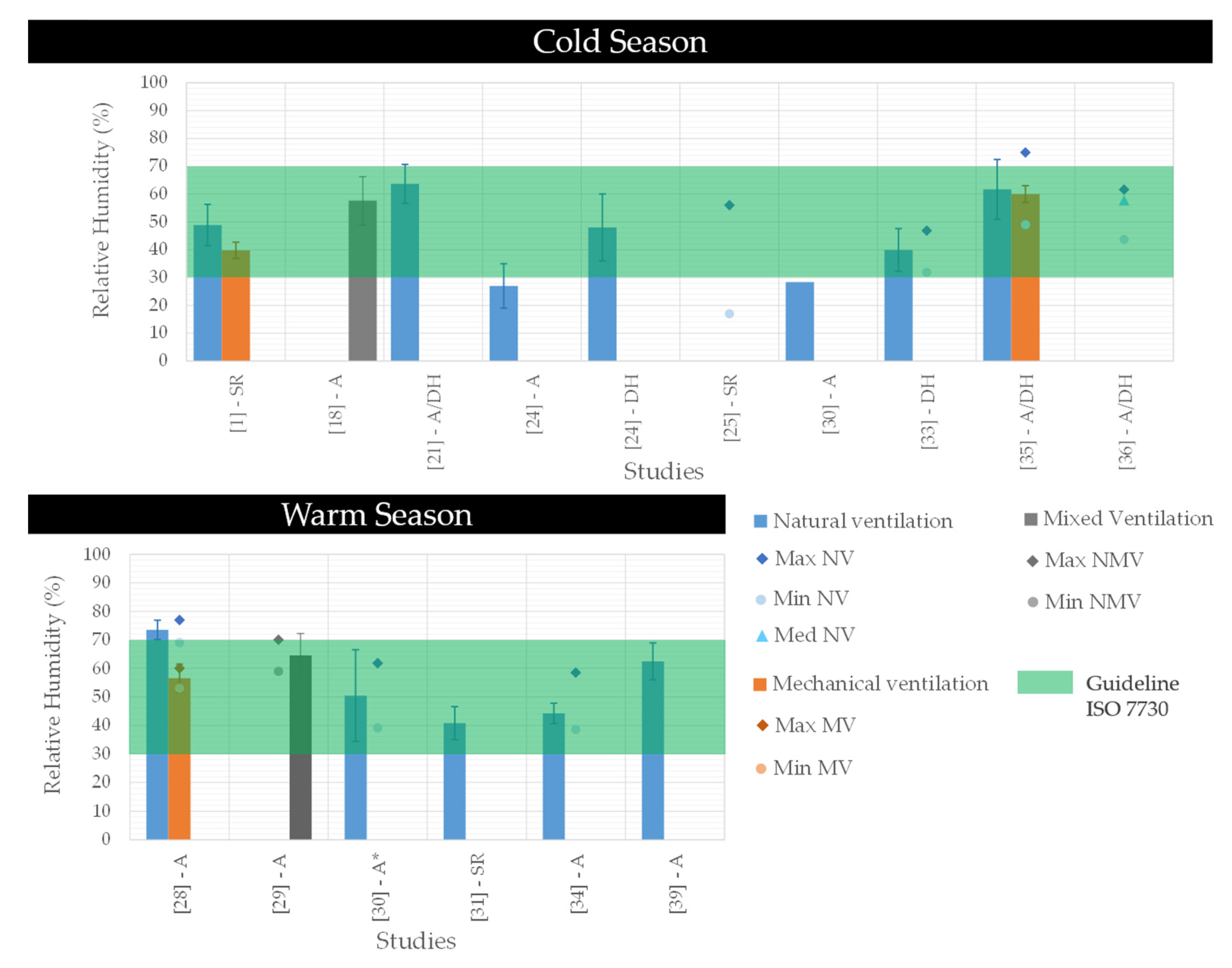
3.2.2. Relative Humidity
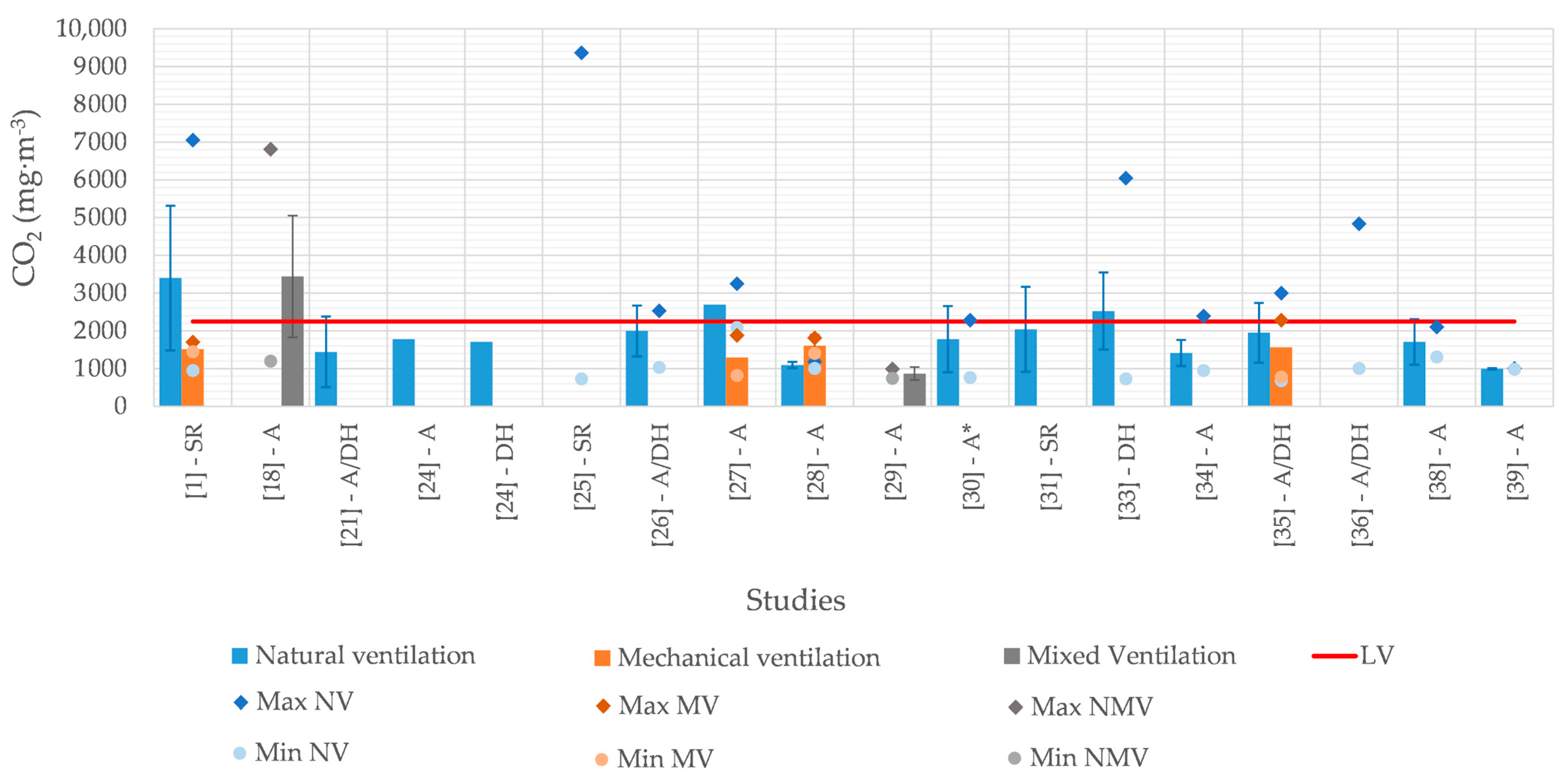
3.2.3. Carbon Dioxide
3.2.4. Carbon Monoxide
3.2.5. Volatile Organic Compounds
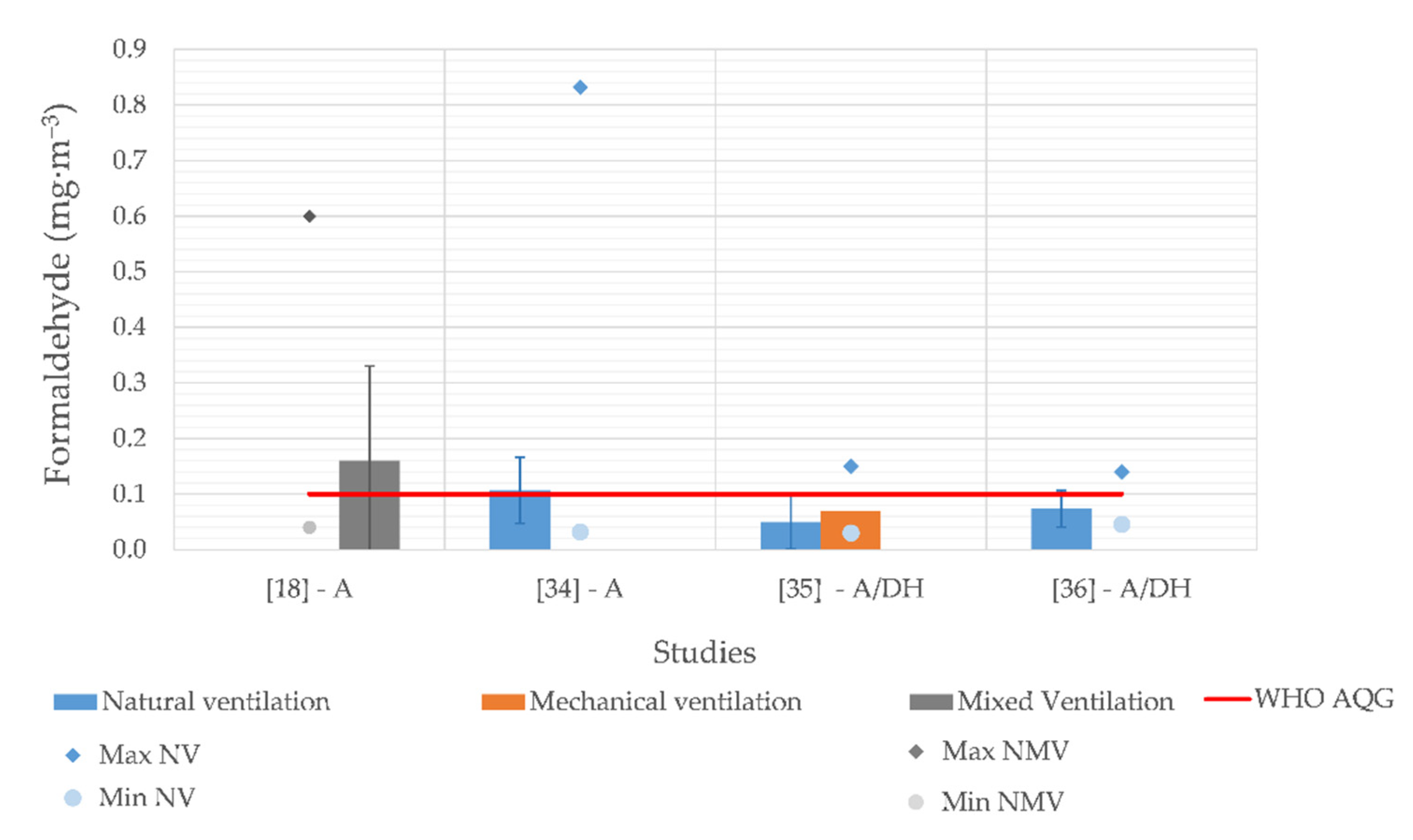
3.2.6. Formaldehyde
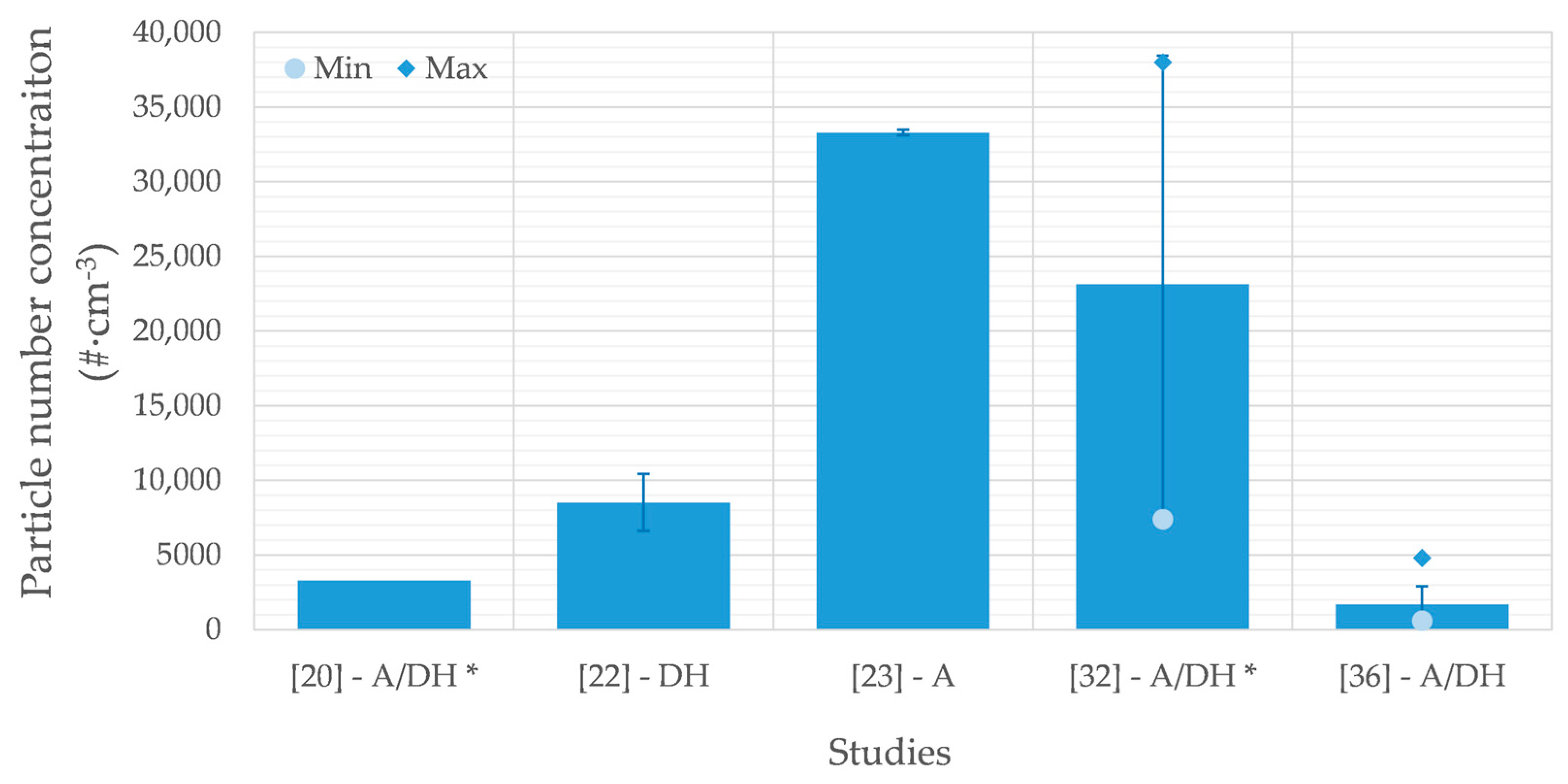
3.2.7. Particles
3.2.8. Air Changes per Hour
4. Discussion
4.1. Correlation between Air Pollutants during Sleep—Understanding Their Sources
4.2. Impact of Air Pollutants on Sleep Quality
4.3. Considerations and Future Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Strøm-Tejsen, P.; Zukowska, D.; Wargocki, P.; Wyon, D.P. The effects of bedroom air quality on sleep and next-day performance. Indoor Air 2016, 26, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Boor, B.E.; Spilak, M.P.; Laverge, J.; Novoselac, A.; Xu, Y. Human exposure to indoor air pollutants in sleep microenvironments: A literature review. Build. Environ. 2017, 125, 528–555. [Google Scholar] [CrossRef]
- Liu, J.; Wu, T.; Liu, Q.; Wu, S.; Chen, J.-C. Air pollution exposure and adverse sleep health across the life course: A systematic review. Environ. Pollut. 2020, 262, 114263. [Google Scholar] [CrossRef] [PubMed]
- Bekö, G.; Lund, T.; Nors, F.; Toftum, J.; Clausen, G. Ventilation rates in the bedrooms of 500 Danish children. Build. Environ. 2010, 45, 2289–2295. [Google Scholar] [CrossRef]
- Van Tran, V.; Park, D.; Lee, Y.-C. Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality. Int. J. Environ. Res. Public Health 2020, 17, 2927. [Google Scholar] [CrossRef]
- Sundell, J. On the history of indoor air quality and health. Indoor Air 2004, 14 (Suppl. 7), 51–58. [Google Scholar] [CrossRef]
- World Health Organization Household Air Pollution and Health. Available online: https://www.who.int/en/news-room/fact-sheets/detail/household-air-pollution-and-health (accessed on 20 December 2020).
- Assefa, S.Z.; Diaz-Abad, M.; Wickwire, E.M.; Scharf, S. The Functions of Sleep. AIMS Neurosci. 2015, 2, 155–171. [Google Scholar] [CrossRef]
- Zielinski, M.R.; McKenna, J.T.; McCarley, R.W. Functions and Mechanisms of Sleep. AIMS Neurosci. 2016, 3, 67–104. [Google Scholar] [CrossRef]
- Scott, A.J.; Webb, T.L.; Rowse, G. Does improving sleep lead to better mental health? A protocol for a meta-analytic review of randomised controlled trials. BMJ Open 2017, 7, e016873. [Google Scholar] [CrossRef]
- Magnavita, N.; Garbarino, S. Sleep, Health and Wellness at Work: A Scoping Review. Int. J. Environ. Res. Public Health 2017, 14, 1347. [Google Scholar] [CrossRef]
- Okamoto-Mizuno, K.; Mizuno, K. Effects of thermal environment on sleep and circadian rhythm. J. Physiol. Anthr. 2012, 31, 14. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Lian, Z.; Lan, L. Investigation of sleep quality under different temperatures based on subjective and physiological measurements. HVAC R Res. 2012, 18, 1030–1043. [Google Scholar] [CrossRef]
- Blume, C.; Garbazza, C.; Spitschan, M. Effects of light on human circadian rhythms, sleep and mood. Somnologie 2019, 23, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Halperin, D. Environmental noise and sleep disturbances: A threat to health? Sleep Sci. 2014, 7, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Katsoyiannis, A.; Cincinelli, A. ‘Cocktails and dreams’: The indoor air quality that people are exposed to while sleeping. Curr. Opin. Environ. Sci. Health 2019, 8, 6–9. [Google Scholar] [CrossRef]
- Lan, L.; Lian, Z. Ten questions concerning thermal environment and sleep quality. Build. Environ. 2016, 99, 252–259. [Google Scholar] [CrossRef]
- Canha, N.; Alves, A.C.A.C.O.; Marta, C.S.C.S.; Lage, J.; Belo, J.; Faria, T.; Cabo Verde, S.; Viegas, C.; Alves, C.; Almeida, S.M.S.M. Compliance of indoor air quality during sleep with legislation and guidelines—A case study of Lisbon dwellings. Environ. Pollut. 2020, 264, 114619. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Mazaheri, M.; Clifford, S.; Jayaratne, R.; Mokhtar, M.A.M.; Fuoco, F.; Buonanno, G.; Morawska, L. School Children’s Personal Exposure to Ultrafine Particles in the Urban Environment. Environ. Sci. Technol. 2014, 48, 113–120. [Google Scholar] [CrossRef]
- Xiong, J.; Lan, L.; Lian, Z.; De Dear, R. Associations of bedroom temperature and ventilation with sleep quality. Sci. Technol. Built Environ. 2020, 26, 1274–1284. [Google Scholar] [CrossRef]
- Wangchuk, T.; Mazaheri, M.; Clifford, S.; Dudzinska, M.R.; He, C.; Buonanno, G.; Morawska, L. Children’s personal exposure to air pollution in rural villages in Bhutan. Environ. Res. 2015, 140, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Mazaheri, M.; Lin, W.; Clifford, S.; Yue, D.; Zhai, Y.; Xu, M.; Rizza, V.; Morawska, L. Characteristics of school children’s personal exposure to ultrafine particles in Heshan, Pearl River Delta, China—A pilot study. Environ. Int. 2019, 132, 105134. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.; Xie, J.; Yoshino, H.; Yanagi, U.; Hasegawa, K.; Kagi, N.; Goto, T.; Zhang, Q.; Wang, C.; Liu, J. Indoor environmental conditions in urban and rural homes with older people during heating season: A case in cold region, China. Energy Build. 2018, 167, 334–346. [Google Scholar] [CrossRef]
- Lei, Z.; Liu, C.; Wang, L.; Li, N. Effect of natural ventilation on indoor air quality and thermal comfort in dormitory during winter. Build. Environ. 2017, 125, 240–247. [Google Scholar] [CrossRef]
- Hou, J.; Zhang, Y.; Sun, Y.; Wang, P.; Zhang, Q.; Kong, X.; Sundell, J. Air change rates at night in northeast Chinese homes. Build. Environ. 2018, 132, 273–281. [Google Scholar] [CrossRef]
- Lin, Z.; Deng, S. The outdoor air ventilation rate in high-rise residences employing room air conditioners. Build. Environ. 2003, 38, 1389–1399. [Google Scholar] [CrossRef]
- Wong, N.H.; Huang, B. Comparative study of the indoor air quality of naturally ventilated and air-conditioned bedrooms of residential buildings in Singapore. Build. Environ. 2004, 39, 1115–1123. [Google Scholar] [CrossRef]
- Sekhar, S.C.; Goh, S.E. Thermal comfort and IAQ characteristics of naturally/mechanically ventilated and air-conditioned bedrooms in a hot and humid climate. Build. Environ. 2011, 46, 1905–1916. [Google Scholar] [CrossRef]
- Kim, M.; Chun, C.; Han, J. A Study on Bedroom Environment and Sleep Quality in Korea. Indoor Built Environ. 2010, 19, 123–128. [Google Scholar] [CrossRef]
- Liao, C.; Marc Delghust, J.L. Association between indoor air quality and sleep quality. In Proceedings of the 40th AIVC—8th TightVent—6th Venticool Conference, Ghent, Belgium, 15–16 October 2019; p. 10. [Google Scholar]
- Buonanno, G.; Marini, S.; Morawska, L.; Fuoco, F.C. Individual dose and exposure of Italian children to ultrafine particles. Sci. Total Environ. 2012, 438, 271–277. [Google Scholar] [CrossRef]
- Mainka, A.; Zajusz-Zubek, E. Keeping Doors Closed as One Reason for Fatigue in Teenagers—A Case Study. Appl. Sci. 2019, 9, 3533. [Google Scholar] [CrossRef]
- Canha, N.; Lage, J.; Candeias, S.; Alves, C.; Almeida, S.M. Indoor air quality during sleep under different ventilation patterns. Atmos. Pollut. Res. 2017, 8, 1132–1142. [Google Scholar] [CrossRef]
- Almeida-Silva, M.; Wolterbeek, H.T.; Almeida, S.M. Elderly exposure to indoor air pollutants. Atmos. Environ. 2014, 85, 54–63. [Google Scholar] [CrossRef]
- Canha, N.; Lage, J.; Coutinho, J.T.; Alves, C.; Almeida, S.M. Comparison of indoor air quality during sleep in smokers and non-smokers’ bedrooms: A preliminary study. Environ. Pollut. 2019, 249, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Almeida-Silva, M.; Almeida, S.M.; Gomes, J.F.; Albuquerque, P.C.; Wolterbeek, H.T. Determination of Airborne Nanoparticles in Elderly Care Centers. J. Toxicol. Environ. Health Part A Curr. Issues 2014, 77, 867–878. [Google Scholar] [CrossRef]
- Mishra, A.K.; Van Ruitenbeek, A.M.; Loomans, M.G.L.C.; Kort, H.S.M. Window/door opening-mediated bedroom ventilation and its impact on sleep quality of healthy, young adults. Indoor Air 2018, 28, 339–351. [Google Scholar] [CrossRef]
- Williams, A.A.; Spengler, J.D.; Catalano, P.; Allen, J.G.; Cedeno-Laurent, J.G. Building Vulnerability in a Changing Climate: Indoor Temperature Exposures and Health Outcomes in Older Adults Living in Public Housing during an Extreme Heat Event in Cambridge, MA. Int. J. Environ. Res. Public Health 2019, 16, 2373. [Google Scholar] [CrossRef]
- Mølhave, L.; Krzyzanowski, M. The right to healthy indoor air: Status by 2002. Indoor Air 2003, 13, 50–53. [Google Scholar] [CrossRef]
- WHO. WHO Guidelines for Indoor Air Quality: Selected Pollutants; WHO European Centre for Environment and Health: Bonn, Germany, 2010. [Google Scholar]
- Abdul-Wahab, S.A.; Chin Fah En, S.; Elkamel, A.; Ahmadi, L.; Yetilmezsoy, K. A review of standards and guidelines set by international bodies for the parameters of indoor air quality. Atmos. Pollut. Res. 2015, 6, 751–767. [Google Scholar] [CrossRef]
- Settimo, G.; Manigrasso, M.; Avino, P. Indoor Air Quality: A Focus on the European Legislation and State-of-the-Art Research in Italy. Atmosphere 2020, 11, 370. [Google Scholar] [CrossRef]
- Ministérios do Ambiente, Ordenamento do Território e Energia, da Saúde e da Solidariedade, Emprego e Segurança Social. Portaria No. 353-A/2013; 1.ª série — N.º 235 — 4 de dezembro de 2013; Diário da República: Lisbon, Portugal, 2013; p. 6644(8). [Google Scholar]
- Farraia, M.; Paciência, I.; Ribeiro, A.I.; Moreira, A.; Rufo, J.C. Indoor Air Quality in Hospitals: How Is the Situation in Portugal? In Occupational and Environmental Safety and Health; Springer International Publishing: Berlin, Germany, 2019; pp. 303–311. [Google Scholar]
- ISO. ISO 7730:2005 ISO 7730—Ergonomics of the Thermal Environment—Analytical Determination and Interpretation of Thermal Comfort Using Calculation of the PMV and PPD Indices and Local Thermal Comfort Criteria; International Organization for Standardization: Geneva, Switzerland, 2005. [Google Scholar]
- European Committee for Standardization (CEN). EN 16798-1:2019|Energy Performance of Buildings—Ventilation for Buildings—Part 1: Indoor Environmental Input Parameters for Design and Assessment of Energy Performance of Buildings Addressing Indoor Air Quality, Thermal Environment, Lighting and Aco; European Committee for Standardization: Brussels, Belgium, 2019. [Google Scholar]
- EEA. Air Quality in Europe—2019 Report—EEA Report No 10/2019; Publications Office of the European Union: Luxembourg, 2019. [Google Scholar]
- Loomis, D.; Grosse, Y.; Lauby-Secretan, B.; El Ghissassi, F.; Bouvard, V.; Benbrahim-Tallaa, L.; Guha, N.; Baan, R.; Mattock, H.; Straif, K. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013, 14, 1262–1263. [Google Scholar] [CrossRef]
- Persily, A.; De Jonge, L. Carbon dioxide generation rates for building occupants. Indoor Air 2017, 27, 868–879. [Google Scholar] [CrossRef]
- Canha, N.; Mandin, C.; Ramalho, O.; Wyart, G.; Ribéron, J.; Dassonville, C.; Hänninen, O.; Almeida, S.M.; Derbez, M. Assessment of ventilation and indoor air pollutants in nursery and elementary schools in France. Indoor Air 2016, 26, 350–365. [Google Scholar] [CrossRef] [PubMed]
- Mullen, N.A.; Li, J.; Russell, M.L.; Spears, M.; Less, B.D.; Singer, B.C. Results of the California Healthy Homes Indoor Air Quality Study of 2011–2013: Impact of natural gas appliances on air pollutant concentrations. Indoor Air 2016, 26, 231–245. [Google Scholar] [CrossRef] [PubMed]
- Canha, N.; Lage, J.; Galinha, C.; Coentro, S.; Alves, C.; Almeida, S. Impact of Biomass Home Heating, Cooking Styles, and Bread Toasting on the Indoor Air Quality at Portuguese Dwellings: A Case Study. Atmosphere 2018, 9, 214. [Google Scholar] [CrossRef]
- Ramos, C.A.; Wolterbeek, H.T.; Almeida, S.M. Air pollutant exposure and inhaled dose during urban commuting: A comparison between cycling and motorized modes. Air Qual. Atmos. Health 2016, 9, 867–879. [Google Scholar] [CrossRef]
- Zhou, M.; Liu, Y.; Duan, Y. Breath biomarkers in diagnosis of pulmonary diseases. Clin. Chim. Acta 2012, 413, 1770–1780. [Google Scholar] [CrossRef]
- Wu, L.; Wang, R. Carbon Monoxide: Endogenous Production, Physiological Functions, and Pharmacological Applications. Pharmacol. Rev. 2005, 57, 585–630. [Google Scholar] [CrossRef]
- Canha, N.; Almeida, S.M.; Freitas, M.C.; Täubel, M.; Hänninen, O. Winter Ventilation Rates at Primary Schools: Comparison Between Portugal and Finland. J. Toxicol. Environ. Health Part A Curr. Issues 2013, 76, 400–408. [Google Scholar] [CrossRef]
- Becher, R.; Øvrevik, J.; Schwarze, P.E.; Nilsen, S.; Hongslo, J.K.; Bakke, J.V. Do Carpets Impair Indoor Air Quality and Cause Adverse Health Outcomes: A Review. Int. J. Environ. Res. Public Health 2018, 15, 184. [Google Scholar] [CrossRef]
- Wieslander, G.; Norbäck, D.; Björnsson, E.; Janson, C.; Boman, G. Asthma and the indoor environment: The significance of emission of formaldehyde and volatile organic compounds from newly painted indoor surfaces. Int. Arch. Occup. Environ. Health 1996, 69, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Chin, J.-Y.; Godwin, C.; Parker, E.; Robins, T.; Lewis, T.; Harbin, P.; Batterman, S. Levels and sources of volatile organic compounds in homes of children with asthma. Indoor Air 2014, 24, 403–415. [Google Scholar] [CrossRef] [PubMed]
- Vicente, E.D.; Ribeiro, J.P.; Custódio, D.; Alves, C.A. Assessment of the indoor air quality in copy centres at Aveiro, Portugal. Air Qual. Atmos. Health 2017, 10, 117–127. [Google Scholar] [CrossRef]
- Shrubsole, C.; Dimitroulopoulou, S.; Foxall, K.; Gadeberg, B.; Doutsi, A. IAQ guidelines for selected volatile organic compounds (VOCs) in the UK. Build. Environ. 2019, 165, 106382. [Google Scholar] [CrossRef]
- Savdie, J.; Canha, N.; Buitrago, N.; Almeida, S.M. Passive Exposure to Pollutants from a New Generation of Cigarettes in Real Life Scenarios. Int. J. Environ. Res. Public Health 2020, 17, 3455. [Google Scholar] [CrossRef]
- Mueller, D.; Uibel, S.; Braun, M.; Klingelhoefer, D.; Takemura, M.; Groneberg, D.A. Tobacco smoke particles and indoor air quality (ToPIQ)—The protocol of a new study. J. Occup. Med. Toxicol. 2011, 6, 35. [Google Scholar] [CrossRef]
- Bahl, V.; Jacob, P.; Havel, C.; Schick, S.F.; Talbot, P. Thirdhand Cigarette Smoke: Factors Affecting Exposure and Remediation. PLoS ONE 2014, 9, e108258. [Google Scholar] [CrossRef]
- Sun, X.; He, J.; Yang, X. Human breath as a source of VOCs in the built environment, Part I: A method for sampling and detection species. Build. Environ. 2017, 125, 565–573. [Google Scholar] [CrossRef]
- He, J.; Sun, X.; Yang, X. Human respiratory system as sink for volatile organic compounds: Evidence from field measurements. Indoor Air 2019, 29, 968–978. [Google Scholar] [CrossRef]
- Tsushima, S.; Wargocki, P.; Tanabe, S. Sensory evaluation and chemical analysis of exhaled and dermally emitted bioeffluents. Indoor Air 2018, 28, 146–163. [Google Scholar] [CrossRef]
- Rovira, J.; Roig, N.; Nadal, M.; Schuhmacher, M.; Domingo, J.L. Human health risks of formaldehyde indoor levels: An issue of concern. J. Environ. Sci. Health Part A Toxic/Hazard. Subst. Environ. Eng. 2016, 51, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, G.D.; Larsen, S.T.; Wolkoff, P. Re-evaluation of the WHO (2010) formaldehyde indoor air quality guideline for cancer risk assessment. Arch. Toxicol. 2017, 91, 35–61. [Google Scholar] [CrossRef] [PubMed]
- Salthammer, T. Formaldehyde sources, formaldehyde concentrations and air exchange rates in European housings. Build. Environ. 2019, 150, 219–232. [Google Scholar] [CrossRef]
- Uchiyama, S.; Tomizawa, T.; Tokoro, A.; Aoki, M.; Hishiki, M.; Yamada, T.; Tanaka, R.; Sakamoto, H.; Yoshida, T.; Bekki, K.; et al. Gaseous chemical compounds in indoor and outdoor air of 602 houses throughout Japan in winter and summer. Environ. Res. 2015, 137, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Haghighat, F.; De Bellis, L. Material emission rates: Literature review, and the impact of indoor air temperature and relative humidity. Build. Environ. 1998, 33, 261–277. [Google Scholar] [CrossRef]
- Caddick, Z.A.; Gregory, K.; Arsintescu, L.; Flynn-Evans, E.E. A review of the environmental parameters necessary for an optimal sleep environment. Build. Environ. 2018, 132, 11–20. [Google Scholar] [CrossRef]
- Wallace, L.A.; Wheeler, A.J.; Kearney, J.; Van Ryswyk, K.; You, H.; Kulka, R.H.; Rasmussen, P.E.; Brook, J.R.; Xu, X. Validation of continuous particle monitors for personal, indoor, and outdoor exposures. J. Expo. Sci. Environ. Epidemiol. 2011, 21, 49–64. [Google Scholar] [CrossRef]
- McNamara, M.L.; Noonan, C.W.; Ward, T.J. Correction Factor for Continuous Monitoring of Wood Smoke Fine Particulate Matter. Aerosol Air Qual. Res. 2011, 11, 316–323. [Google Scholar] [CrossRef]
- Cavaliere, A.; Carotenuto, F.; Di Gennaro, F.; Gioli, B.; Gualtieri, G.; Martelli, F.; Matese, A.; Toscano, P.; Vagnoli, C.; Zaldei, A. Development of Low-Cost Air Quality Stations for Next Generation Monitoring Networks: Calibration and Validation of PM2.5 and PM10 Sensors. Sensors 2018, 18, 2843. [Google Scholar] [CrossRef]
- Liu, H.-Y.; Schneider, P.; Haugen, R.; Vogt, M. Performance Assessment of a Low-Cost PM2.5 Sensor for a near Four-Month Period in Oslo, Norway. Atmosphere 2019, 10, 41. [Google Scholar] [CrossRef]
- Ohlwein, S.; Kappeler, R.; Kutlar Joss, M.; Künzli, N.; Hoffmann, B. Health effects of ultrafine particles: A systematic literature review update of epidemiological evidence. Int. J. Public Health 2019, 64, 547–559. [Google Scholar] [CrossRef] [PubMed]
- Schraufnagel, D.E. The health effects of ultrafine particles. Exp. Mol. Med. 2020, 52, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhao, B. Review of relationship between indoor and outdoor particles: I/O ratio, infiltration factor and penetration factor. Atmos. Environ. 2011, 45, 275–288. [Google Scholar] [CrossRef]
- Stephens, B.; Siegel, J.A. Penetration of ambient submicron particles into single-family residences and associations with building characteristics. Indoor Air 2012, 22, 501–513. [Google Scholar] [CrossRef] [PubMed]
- Hussein, T.; Alameer, A.; Jaghbeir, O.; Albeitshaweesh, K.; Malkawi, M.; Boor, B.E.; Koivisto, A.J.; Löndahl, J.; Alrifai, O.; Al-Hunaiti, A. Indoor Particle Concentrations, Size Distributions, and Exposures in Middle Eastern Microenvironments. Atmosphere 2019, 11, 41. [Google Scholar] [CrossRef]
- Afshari, A.; Matson, U.; Ekberg, L.E. Characterization of indoor sources of fine and ultrafine particles: A study conducted in a full-scale chamber. Indoor Air 2005, 15, 141–150. [Google Scholar] [CrossRef]
- Manigrasso, M.; Guerriero, E.; Avino, P. Ultrafine Particles in Residential Indoors and Doses Deposited in the Human Respiratory System. Atmosphere 2015, 6, 1444–1461. [Google Scholar] [CrossRef]
- Sekhar, C.; Akimoto, M.; Fan, X.; Bivolarova, M.; Liao, C.; Lan, L.; Wargocki, P. Bedroom ventilation: Review of existing evidence and current standards. Build. Environ. 2020, 184, 107229. [Google Scholar] [CrossRef]
- González-Martín, J.; Kraakman, N.J.R.; Pérez, C.; Lebrero, R.; Muñoz, R. A state–of–the-art review on indoor air pollution and strategies for indoor air pollution control. Chemosphere 2021, 262, 128376. [Google Scholar] [CrossRef]
- Franco, A.; Leccese, F. Measurement of CO2 concentration for occupancy estimation in educational buildings with energy efficiency purposes. J. Build. Eng. 2020, 32, 101714. [Google Scholar] [CrossRef]
- Hospodsky, D.; Qian, J.; Nazaroff, W.W.; Yamamoto, N.; Bibby, K.; Rismani-Yazdi, H.; Peccia, J. Human Occupancy as a Source of Indoor Airborne Bacteria. PLoS ONE 2012, 7, e34867. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez, V.; Silva, J.; Cauli, O. A survey on sleep assessment methods. PeerJ 2018, 6, e4849. [Google Scholar] [CrossRef] [PubMed]
- Marino, M.; Li, Y.; Rueschman, M.N.; Winkelman, J.W.; Ellenbogen, J.M.; Solet, J.M.; Dulin, H.; Berkman, L.F.; Buxton, O.M. Measuring Sleep: Accuracy, Sensitivity, and Specificity of Wrist Actigraphy Compared to Polysomnography. Sleep 2013, 36, 1747–1755. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez, V.; Silva, J.; Navarro, E.; Cauli, O. Sleep assessment devices: Types, market analysis, and a critical view on accuracy and validation. Expert Rev. Med. Devices 2019, 16, 1041–1052. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Lian, Z.; Shen, J.; Cao, T.; Zhu, J.; Lin, X.; Qing, K.; Zhang, W.; Zhang, T. Experimental study on sleep quality affected by carbon dioxide concentration. Indoor Air 2020, ina12748. [Google Scholar] [CrossRef]
- Accinelli, R.A.; Llanos, O.; López, L.M.; Pino, M.I.; Bravo, Y.A.; Salinas, V.; Lazo, M.; Noda, J.R.; Sánchez-Sierra, M.; Zárate, L.; et al. Adherence to reduced-polluting biomass fuel stoves improves respiratory and sleep symptoms in children. BMC Pediatr. 2014, 14, 12. [Google Scholar] [CrossRef]
- Wei, F.; Nie, G.; Zhou, B.; Wang, L.; Ma, Y.; Peng, S.; Ou, S.; Qin, J.; Zhang, L.; Li, S.; et al. Association between Chinese cooking oil fumes and sleep quality among a middle-aged Chinese population. Environ. Pollut. 2017, 227, 543–551. [Google Scholar] [CrossRef]
- Chuang, H.C.; Su, T.Y.; Chuang, K.J.; Hsiao, T.C.; Lin, H.L.; Hsu, Y.T.; Pan, C.H.; Lee, K.Y.; Ho, S.C.; Lai, C.H. Pulmonary exposure to metal fume particulate matter cause sleep disturbances in shipyard welders. Environ. Pollut. 2018, 232, 523–532. [Google Scholar] [CrossRef]
- Lappharat, S.; Taneepanichskul, N.; Reutrakul, S.; Chirakalwasan, N. Effects of Bedroom Environmental Conditions on the Severity of Obstructive Sleep Apnea. J. Clin. Sleep Med. 2018, 14, 565–573. [Google Scholar] [CrossRef]
- Castañeda, J.L.; Kheirandish-Gozal, L.; Gozal, D.; Accinelli, R.A. Effect of reductions in biomass fuel exposure on symptoms of sleep apnea in children living in the peruvian andes: A preliminary field study. Pediatr. Pulmonol. 2013, 48, 996–999. [Google Scholar] [CrossRef]
- Sánchez, T.; Gozal, D.; Smith, D.L.; Foncea, C.; Betancur, C.; Brockmann, P.E. Association between air pollution and sleep disordered breathing in children. Pediatr. Pulmonol. 2019, 54, 544–550. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A. Sleep duration across the lifespan: Implications for health. Sleep Med. Rev. 2012, 16, 199–201. [Google Scholar] [CrossRef] [PubMed]
- Canha, N.; Almeida, S.M.; Freitas, M.D.C.; Trancoso, M.; Sousa, A.; Mouro, F.; Wolterbeek, H.T. Particulate matter analysis in indoor environments of urban and rural primary schools using passive sampling methodology. Atmos. Environ. 2014, 83, 21–34. [Google Scholar] [CrossRef]
- Simoni, M.; Baldacci, S.; Maio, S.; Cerrai, S.; Sarno, G.; Viegi, G. Adverse effects of outdoor pollution in the elderly. J. Thorac. Dis. 2015, 7, 34–45. [Google Scholar] [PubMed]
- Almeida, S.M.; Ramos, C.A.; Almeida-Silva, M. Exposure and inhaled dose of susceptible population to chemical elements in atmospheric particles. J. Radioanal. Nucl. Chem. 2016, 309, 309–315. [Google Scholar] [CrossRef]
- Tang, J.; Liao, Y.; Kelly, B.C.; Xie, L.; Xiang, Y.-T.; Qi, C.; Pan, C.; Hao, W.; Liu, T.; Zhang, F.; et al. Gender and Regional Differences in Sleep Quality and Insomnia: A General Population-based Study in Hunan Province of China. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fatima, Y.; Doi, S.A.R.; Najman, J.M.; Al Mamun, A. Exploring Gender Difference in Sleep Quality of Young Adults: Findings from a Large Population Study. Clin. Med. Res. 2016, 14, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Hall, M.L.; Strollo, P.J.; Kamarck, T.W.; Owens, J.; Lee, L.; Reis, S.E.; Matthews, K.A. Relationships Between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and Clinical/Polysomnographic Measures in a Community Sample. J. Clin. Sleep Med. 2008, 4, 563–571. [Google Scholar] [CrossRef]
- Mong, J.A.; Cusmano, D.M. Sex differences in sleep: Impact of biological sex and sex steroids. Philos. Trans. R. Soc. B Biol. Sci. 2016, 371, 20150110. [Google Scholar] [CrossRef]
- Serrano-Jiménez, A.; Lizana, J.; Molina-Huelva, M.; Barrios-Padura, Á. Indoor environmental quality in social housing with elderly occupants in Spain: Measurement results and retrofit opportunities. J. Build. Eng. 2020, 30, 101264. [Google Scholar] [CrossRef]
- Bo, M.; Salizzoni, P.; Clerico, M.; Buccolieri, R. Assessment of Indoor-Outdoor Particulate Matter Air Pollution: A Review. Atmosphere 2017, 8, 136. [Google Scholar] [CrossRef]
- Galvão, E.S.; Santos, J.M.; Lima, A.T.; Reis, N.C.; Orlando, M.T.D.A.; Stuetz, R.M. Trends in analytical techniques applied to particulate matter characterization: A critical review of fundaments and applications. Chemosphere 2018, 199, 546–568. [Google Scholar] [CrossRef] [PubMed]
- Hopke, P.K.; Dai, Q.; Li, L.; Feng, Y. Global review of recent source apportionments for airborne particulate matter. Sci. Total Environ. 2020, 740, 140091. [Google Scholar] [CrossRef] [PubMed]
- Vicente, E.D.; Vicente, A.M.; Evtyugina, M.; Calvo, A.I.; Oduber, F.; Alegre, C.B.; Castro, A.; Fraile, R.; Nunes, T.; Lucarelli, F.; et al. Impact of vacuum cleaning on indoor air quality. Build. Environ. 2020, 180, 107059. [Google Scholar] [CrossRef]
- Isaxon, C.; Gudmundsson, A.; Nordin, E.Z.; Lönnblad, L.; Dahl, A.; Wieslander, G.; Bohgard, M.; Wierzbicka, A. Contribution of indoor-generated particles to residential exposure. Atmos. Environ. 2015, 106, 458–466. [Google Scholar] [CrossRef]
- Manoukian, A.; Quivet, E.; Temime-Roussel, B.; Nicolas, M.; Maupetit, F.; Wortham, H. Emission characteristics of air pollutants from incense and candle burning in indoor atmospheres. Environ. Sci. Pollut. Res. 2013, 20, 4659–4670. [Google Scholar] [CrossRef]
- Serfozo, N.; Chatoutsidou, S.E.; Lazaridis, M. The effect of particle resuspension during walking activity to PM 10 mass and number concentrations in an indoor microenvironment. Build. Environ. 2014, 82, 180–189. [Google Scholar] [CrossRef]
- Alves, C.A. A short review on atmospheric cellulose. Air Qual. Atmos. Health 2017, 10, 669–678. [Google Scholar] [CrossRef]
- Faria, T.; Martins, V.; Correia, C.; Canha, N.; Diapouli, E.; Manousakas, M.; Eleftheriadis, K.; Almeida, S.M. Children’s exposure and dose assessment to particulate matter in Lisbon. Build. Environ. 2020, 171, 106666. [Google Scholar] [CrossRef]
- Gall, E.T.; Carter, E.M.; Earnest, C.M.; Stephens, B. Indoor Air Pollution in Developing Countries: Research and Implementation Needs for Improvements in Global Public Health. Am. J. Public Health 2013, 103, e67–e72. [Google Scholar] [CrossRef]
- Zhang, J.; Smith, K.R. Indoor air pollution: A global health concern. Br. Med. Bull. 2003, 68, 209–225. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A.; Smith, T.E.; Jackson, N.; Jackson, T.; Burgard, S.; Branas, C. Geographic distribution of insufficient sleep across the United States: A county-level hotspot analysis. Sleep Health 2015, 1, 158–165. [Google Scholar] [CrossRef] [PubMed]





| Number of Studies | ||||||
|---|---|---|---|---|---|---|
| Parameter | Setting | Australia | Asia | Europe | North America | Total |
| Type of environment | Urban | 2 | 6 | 5 | 1 | 14 |
| Suburban | 1 | 1 | ||||
| Mixed (urban and suburban) | 2 | 2 | ||||
| Rural | 1 | 1 | ||||
| Mixed (urban and rural) | 2 | 2 | 4 | |||
| Total | 2 | 9 | 10 | 1 | 22 | |
| Type of housing | Apartment | 5 | 3 | 1 | 9 | |
| Detached house | 1 | 1 | 2 | |||
| Mixed (apartment and detached house) | 2 | 2 | 2 | 6 | ||
| Scholar residence | 1 | 2 | 3 | |||
| Elderly care centre | 2 | 2 | ||||
| Total | 2 | 9 | 10 | 1 | 22 | |
| Type of ventilation | Natural | 1 | 5 | 5 | 1 | 12 |
| Mixed (natural and mechanical) | 3 | 4 | 7 | |||
| No info available | 1 | 1 | 1 | 3 | ||
| Total | 2 | 9 | 10 | 1 | 22 | |
| Number of occupants per bedroom | 1 | 3 | 7 | 10 | ||
| 2 | 2 | 3 | 5 | |||
| 1 or 2 | 1 | 1 | ||||
| 4 or 6 | 1 | 1 | ||||
| No info available | 1 | 3 | 1 | 5 | ||
| Total | 2 | 9 | 10 | 1 | 22 | |
| Type of Season | Warm season | 3 | 2 | 1 | 6 | |
| Cold season | 1 | 2 | 8 | 10 | ||
| Both seasons | 1 | 3 | 5 | |||
| No info available | 1 | 1 | ||||
| Total | 2 | 9 | 10 | 1 | 22 | |
| Parameter | WHO Air Quality Guideline | Reference Value | Reference |
|---|---|---|---|
| CO2 | - | 2250 mg·m−3 (8 h) | [44] |
| CO | 10 mg·m−3 (8 h) | - | [41] |
| VOC | - | 600 µg·m−3 (8 h) | [44] |
| CH2O | 0.1 mg·m−3 (30 min) | - | [41] |
| PM2.5 | 25 µg·m−3 (24 h), 10 µg·m−3 (1 year) | - | [41] |
| PM10 | 50 µg·m−3 (24 h), 20 µg·m−3 (1 year) | - | [41] |
| T | - | 20–24 °C (cold season) | [46] |
| - | 23–26 °C (warm season) | ||
| RH | - | 30–70% | |
| Air changes per hour | - | 0.7 h−1 | [47] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Canha, N.; Teixeira, C.; Figueira, M.; Correia, C. How Is Indoor Air Quality during Sleep? A Review of Field Studies. Atmosphere 2021, 12, 110. https://doi.org/10.3390/atmos12010110
Canha N, Teixeira C, Figueira M, Correia C. How Is Indoor Air Quality during Sleep? A Review of Field Studies. Atmosphere. 2021; 12(1):110. https://doi.org/10.3390/atmos12010110
Chicago/Turabian StyleCanha, Nuno, Catarina Teixeira, Mónica Figueira, and Carolina Correia. 2021. "How Is Indoor Air Quality during Sleep? A Review of Field Studies" Atmosphere 12, no. 1: 110. https://doi.org/10.3390/atmos12010110
APA StyleCanha, N., Teixeira, C., Figueira, M., & Correia, C. (2021). How Is Indoor Air Quality during Sleep? A Review of Field Studies. Atmosphere, 12(1), 110. https://doi.org/10.3390/atmos12010110






