Viability of Bacillus subtilis Cells in Airborne Bioaerosols on Face Masks
Abstract
:1. Introduction
2. Materials and Methods
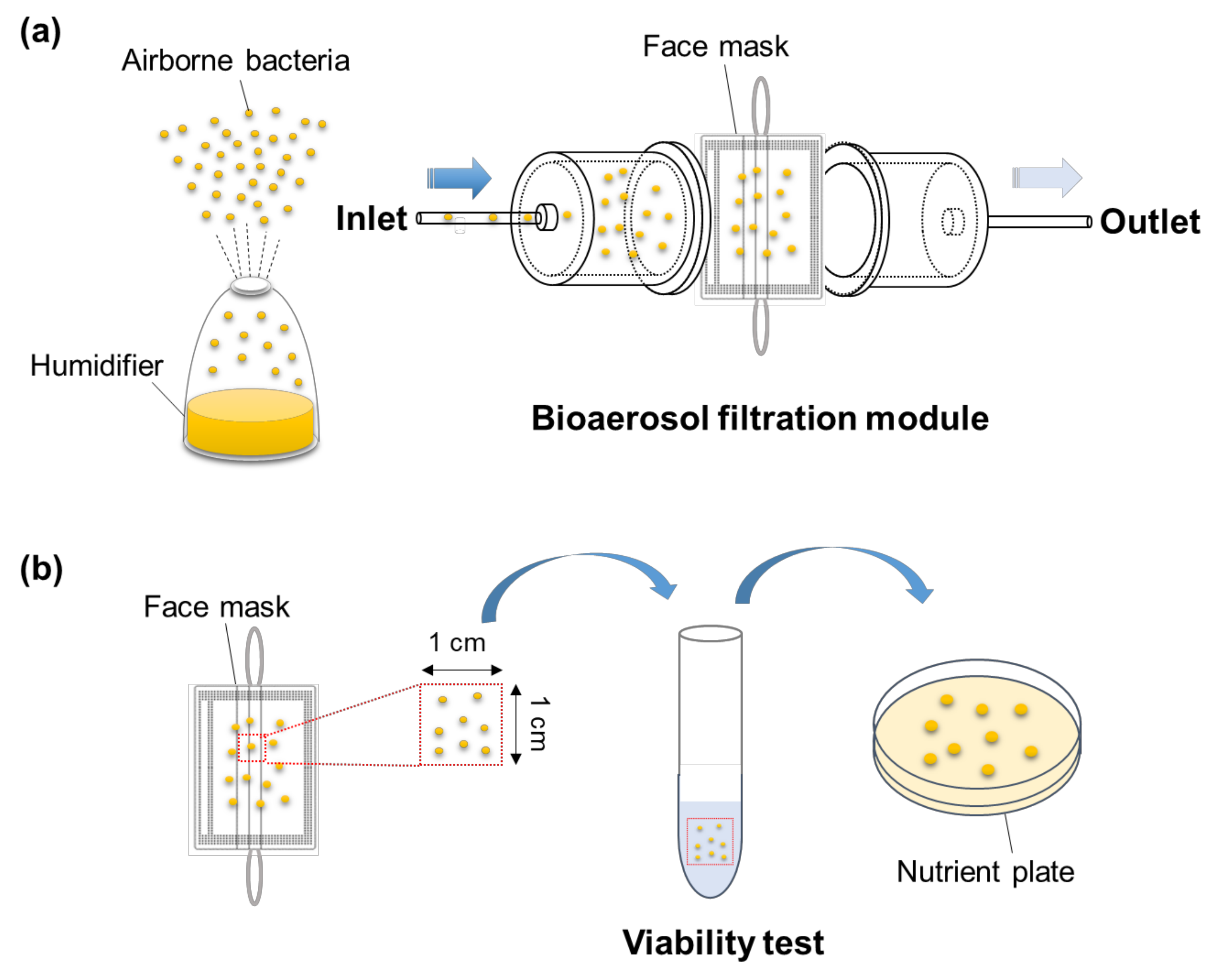
2.1. Filtration System Used to Evaluate the Viability of Bioaerosol Bacteria
2.2. Use of Face Masks to Filter Airborne Bacteria-Containing Droplets
2.3. Effects of Particulate Matters (PMs) on the Viability of Bioaerosol Bacteria on the Masks
2.4. Viability Tests for Airborne B. subtilis in Bioaerosols Filtered on the Masks
3. Results and Discussion
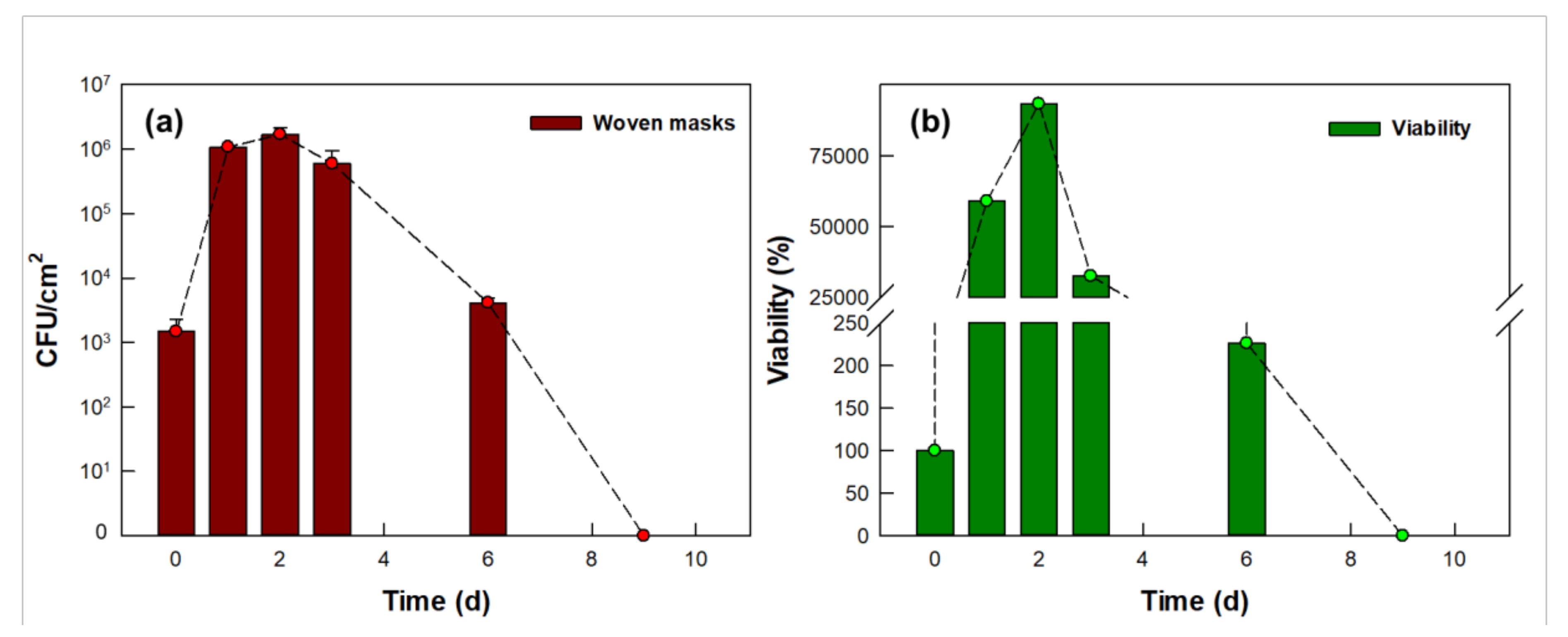
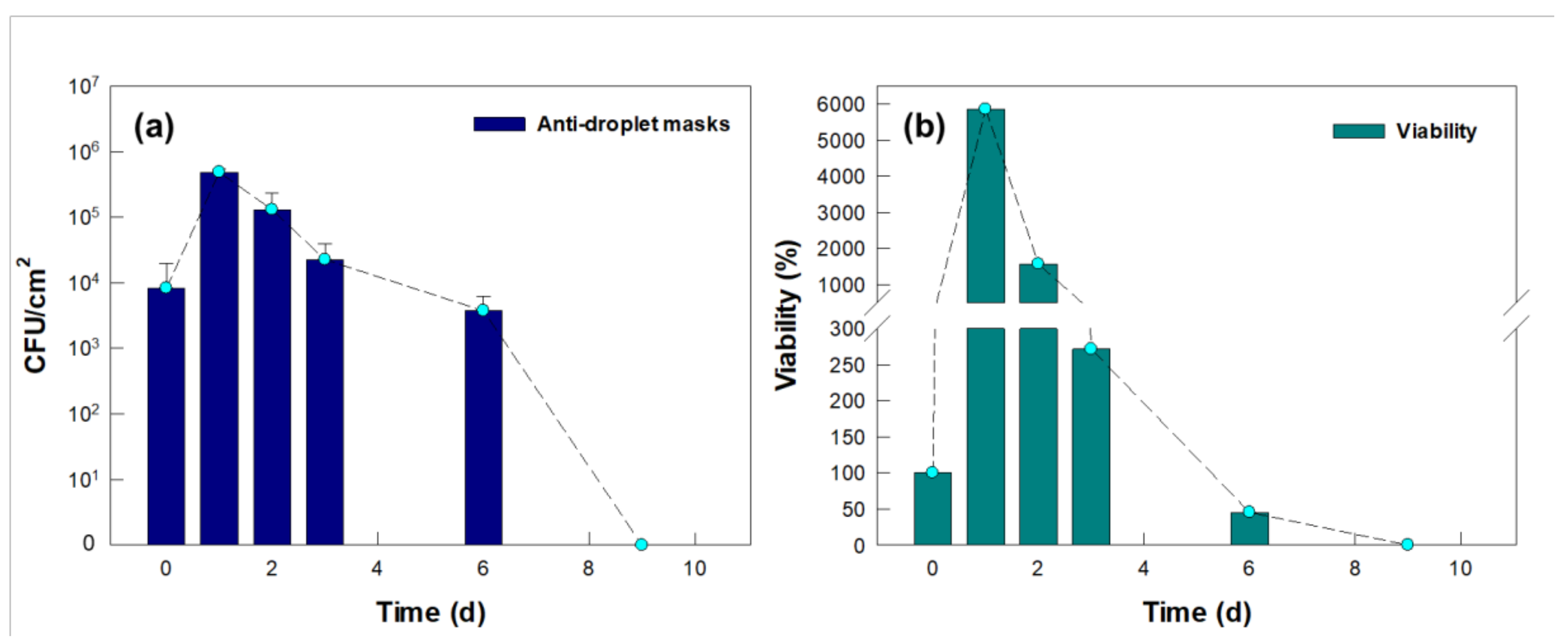
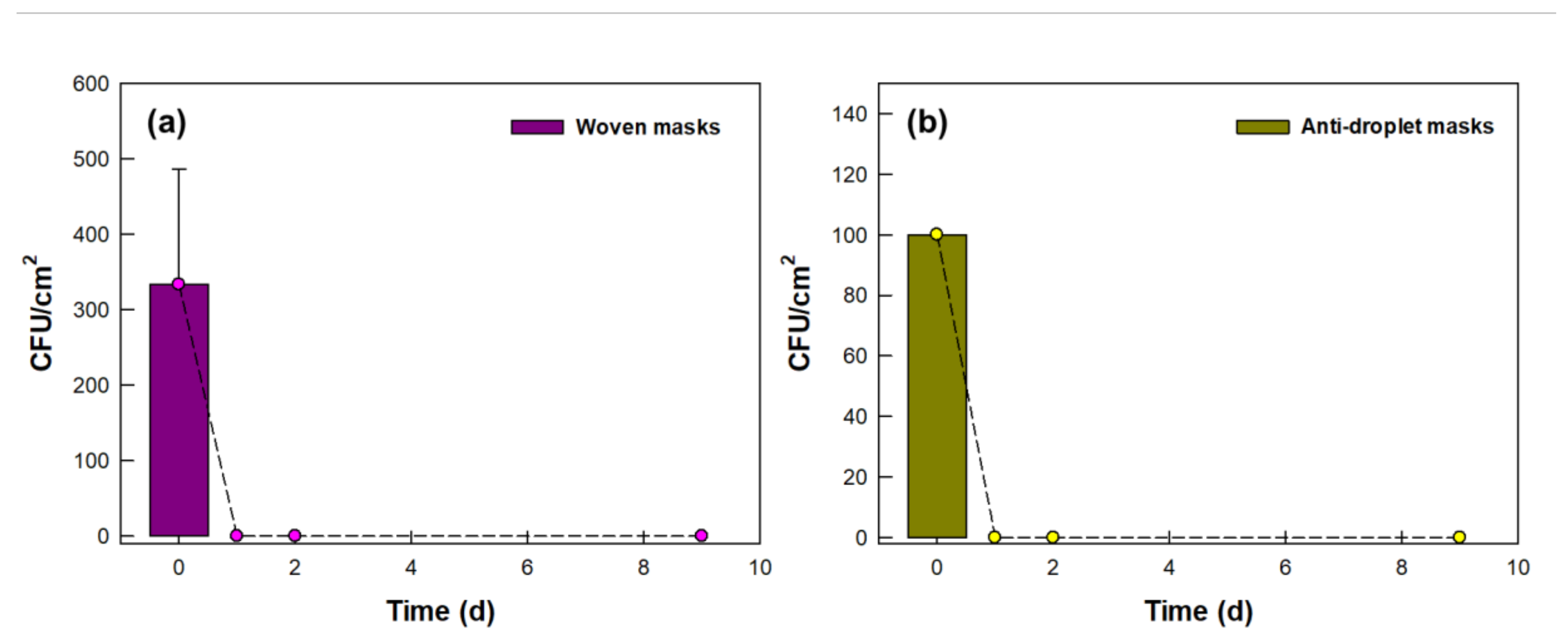
3.1. Viability of B. subtilis from Airborne Bioaerosols Filtered on Face Masks
3.2. Effects of Particulate Matters (PMs) on Viability of Bacteria in Airborne Bioaerosols Filtered on Masks
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, S.H. Personal Protective Equipment for Healthcare Workers during the COVID-19 Pandemic. Infect. Chemother. 2020, 52, 165–182. [Google Scholar] [CrossRef]
- W.H.O. WHO Coronavirus Disease (COVID-19) Dashboard (8 September 2021). Available online: https://covid19.who.int/ (accessed on 8 September 2021).
- Siegel, J.D.; Rhinehart, E.; Jackson, M.; Chiarello, L.; Healthcare infection control practices advisory committee. 2007 Guideline for isolation precautions: Preventing transmission of infectious agents in healthcare settings. Am. J. Infect. Control. 2007, 35, S65–S164. [Google Scholar] [CrossRef] [PubMed]
- Otter, J.A.; Donskey, C.; Yezli, S.; Douthwaite, S.; Goldenberg, S.; Weber, D.J. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: The possible role of dry surface contamination. J. Hosp. Infect. 2016, 92, 235–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- W.H.O. Coronavirus Disease (COVID-19) Advice for the Public. 2021. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 2 September 2021).
- W.H.O. The WHO Guidelines Infection Prevention and Control of Epidemic and Pandemic-Prone Acute Respiratory Infections in Health Care; WHO Press: Geneva, Switzerland, 2014. [Google Scholar]
- Roberge, R.J. Face shields for infection control: A review. J. Occup. Environ. Hyg. 2016, 13, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.-H.; Lee, S.-W.; Moon, S.; Son, J. Performance Evaluation of Commercially Available Masks in Korea for Filtering Airborne Droplets Containing Bacteria. Int. J. Environ. Res. Public Health 2021, 18, 7909. [Google Scholar] [CrossRef]
- Jeong, S.B.; Ko, H.S.; Seo, S.C.; Jung, J.H. Evaluation of filtration characteristics and microbial recovery rates of commercial filtering facepiece respirators against airborne bacterial particles. Sci. Total. Environ. 2019, 682, 729–736. [Google Scholar] [CrossRef]
- Milton, D.K.; Fabian, M.P.; Cowling, B.; Grantham, M.L.; McDevitt, J.J. Influenza Virus Aerosols in Human Exhaled Breath: Particle Size, Culturability, and Effect of Surgical Masks. PLoS Pathog. 2013, 9, e1003205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, D.F.; Druce, J.; Birch, C.; Grayson, M.L. A Quantitative Assessment of the Efficacy of Surgical and N95 Masks to Filter Influenza Virus in Patients with Acute Influenza Infection. Clin. Infect. Dis. 2009, 49, 275–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.C.; Bae, S.; Kim, J.Y.; Park, S.Y.; Lim, J.S.; Sung, M.; Kim, S.H. Effectiveness of surgical, KF94, and N95 respirator masks in blocking SARS-CoV-2: A controlled comparison in 7 patients. Infect. Dis. 2020, 52, 908–912. [Google Scholar] [CrossRef]
- W.H.O. Coronavirus Disease (COVID-19) Advice for the Public: When and How to Use Masks. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks?gclid=Cj0KCQjwm9yJBhDTARIsABKIcGYyT3maOXWZ8aYahBAZ2izflp8I5pvXkY03eNiLeRaa8YClW4Q2b30aApMyEALw_wcB (accessed on 8 September 2021).
- Guellich, A.; Tella, E.; Ariane, M.; Grodner, C.; Nguyen-Chi, H.-N.; Mahé, E. The face mask-touching behavior during the COVID-19 pandemic: Observational study of public transportation users in the greater Paris region: The French-mask-touch study. J. Transp. Health 2021, 21, 101078. [Google Scholar] [CrossRef]
- Chughtai, A.A.; Stelzer-Braid, S.; Rawlinson, W.; Pontivivo, G.; Wang, Q.; Pan, Y.; Zhang, D.; Zhang, Y.; Li, L.; MacIntyre, C.R. Contamination by respiratory viruses on outer surface of medical masks used by hospital healthcare workers. BMC Infect. Dis. 2019, 19, 491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulrich, N.; Nagler, K.; Laue, M.; Cockell, C.S.; Setlow, P.; Moeller, R. Experimental studies addressing the longevity of Bacillus subtilis spores—The first data from a 500-year experiment. PLoS ONE 2018, 13, e0208425. [Google Scholar] [CrossRef] [PubMed]
- Chada, V.G.R.; Sanstad, E.A.; Wang, R.; Driks, A. Morphogenesis of Bacillus Spore Surfaces. J. Bacteriol. 2003, 185, 6255–6261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, W.-I.; Chung, M.-S. Bacillus spores: A review of their properties and inactivation processing technologies. Food Sci. Biotechnol. 2020, 29, 1447–1461. [Google Scholar] [CrossRef]
- Bressuire-Isoard, C.; Broussolle, V.; Carlin, F. Sporulation environment influences spore properties in Bacillus: Evidence and insights on underlying molecular and physiological mechanisms. FEMS Microbiol. Rev. 2018, 42, 614–626. [Google Scholar] [CrossRef] [Green Version]
- Bin Jeong, S.; Heo, K.J.; Ko, H.S.; Ahn, J.P.; Lee, S.; Jung, J.H. Evaluation of survival rates of airborne microorganisms on the filter layers of commercial face masks. Indoor Air 2021, 31, 1134–1143. [Google Scholar] [CrossRef]
- Lin, T.-H.; Tang, T.-H.; Chiang, C.-H.; Chang, C.-P.; Lai, C.-Y. Recovery of bacteria in filtering facepiece respirators and effects of artificial saliva/perspiration on bacterial survival and performance of respirators. Aerosol. Air Qual. Res. 2017, 17, 187–197. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z. Survival of Bacteria on Respirator Filters. Aerosol Sci. Technol. 1999, 30, 300–308. [Google Scholar] [CrossRef]
- Noda, J.; Tomizawa, S.; Hoshino, B.; Munkhjargal, E.; Kawai, K.; Kai, K. Atmospheric dust as a possible survival factor for bioaerosols. E3S Web Conf. 2019, 99, 04007. [Google Scholar] [CrossRef]
- Hara, K.; Zhang, D. Bacterial abundance and viability in long-range transported dust. Atmospheric Environ. 2012, 47, 20–25. [Google Scholar] [CrossRef]
- Gong, J.; Qi, J.; Yin, B.E.; Gao, D. Concentration, viability and size distribution of bacteria in atmospheric bioaerosols under different types of pollution. Environ. Pollut. 2020, 257, 113485. [Google Scholar] [CrossRef] [PubMed]
- Madhwal, S.; Prabhu, V.; Sundriyal, S.; Shridhar, V. Ambient bioaerosol distribution and associated health risks at a high traffic density junction at Dehradun city, India. Environ. Monit. Assess. 2020, 192, 196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shammi, M.; Rahman, M.; Tareq, S.M. Distribution of Bioaerosols in Association With Particulate Matter: A Review on Emerging Public Health Threat in Asian Megacities. Front. Environ. Sci. 2021, 9, 9. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, X.; Zhang, H.; Yao, X.; Zhou, M.; Wang, J.; He, Z.; Zhang, H.; Lou, L.; Mao, W.; et al. Effect of air pollution on the total bacteria and pathogenic bacteria in different sizes of particulate matter. Environ. Pollut. 2018, 233, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Amarloei, A.; Fazlzadeh, M.; Jafari, A.J.; Zarei, A.; Mazloomi, S. Particulate matters and bioaerosols during Middle East dust storms events in Ilam, Iran. Microchem. J. 2020, 152, 104280. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, E.-H.; Chang, Y.; Lee, S.-W. Viability of Bacillus subtilis Cells in Airborne Bioaerosols on Face Masks. Atmosphere 2021, 12, 1496. https://doi.org/10.3390/atmos12111496
Lee E-H, Chang Y, Lee S-W. Viability of Bacillus subtilis Cells in Airborne Bioaerosols on Face Masks. Atmosphere. 2021; 12(11):1496. https://doi.org/10.3390/atmos12111496
Chicago/Turabian StyleLee, Eun-Hee, Yunsoo Chang, and Seung-Woo Lee. 2021. "Viability of Bacillus subtilis Cells in Airborne Bioaerosols on Face Masks" Atmosphere 12, no. 11: 1496. https://doi.org/10.3390/atmos12111496