Associations between Exposure to Industrial Air Pollution and Prevalence of Asthma and Atopic Diseases in Haifa Bay Area
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Study Population
2.2. Outcome Assessment
2.3. Exposure Data
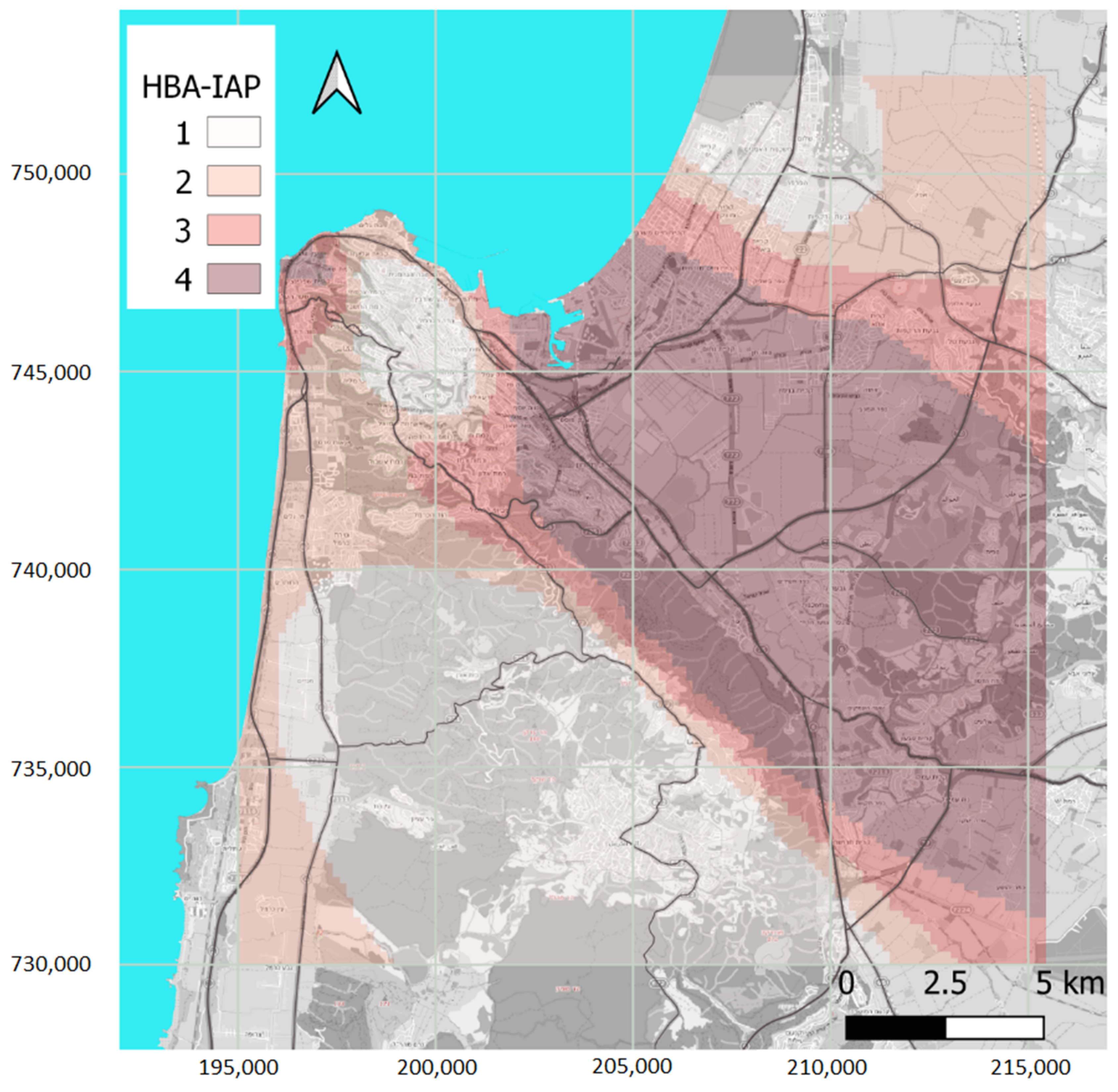
2.4. Exposure Assessment: Rationale and Method
- (1)
- Exposure to pollution from HBA industrial emissions occurs only where the emitted pollution can be transported by airflows previously passed by the industrial stacks. Thus, the industrial center location, the boundaries of residential areas, and the typical wind patterns that can bring air from the former to the latter are the most critical general considerations.
- (2)
- Since the late 1970s, heavy industry and, to a lesser degree, the seaport were the only substantial emitters of SO2 in HBA [29]. In recent years, with the port remaining by far its largest source, SO2 levels have been shallow and close to the monitoring analyzer’s detection and quantification limits. Thus, we assume that SO2 observations at the beginning of the 21st century, which were higher by a factor of 4–10 compared with current levels (Figure S3), were dominated by HBA heavy industry emissions. Background SO2 concentrations are not negligible [30]. Still, they can be considered in the limited aerial extent of HBA to be homogeneous without impacting the shape of the SO2 spatial patterns.
- (3)
- We expect SO2 dispersion and the shape of its spatial concentrations pattern to be similar to those of other industrial pollutants with comparable or a longer atmospheric lifetime.
- (4)
- Dispersion of industry-emitted pollutants with atmospheric lifetime shorter than that of SO2 (e.g., most VOCs) may result in different spatial patterns. Still, we expect that their dispersion lobes’ central axes will be along those of the SO2 spatial distribution (i.e., they will be contained within those of the SO2).
- (5)
- Use of the observed SO2 concentrations in the early years of the 21st century for assessing exposures to industrial pollution emitted in the last decades of the 20th century is warranted, only if the relevant meteorological factors (mainly the wind field) have not changed substantially. This is indeed the case in HBA (see below).
- (6)
- Due to the possible large decline in industry-born ambient concentrations during the study period, driven by a parallel reduction in the industrial emissions, an analysis using the spatial SO2 pattern must account for its temporal concentration variability.
- (7)
- SO2 spatial patterns based on relatively sparse observed concentrations (at the AQM stations) might be affected by the locations of the observations [31]. To minimize this effect, it is desirable to use as many observation sites as possible (see Figure S2). Still, reliance on small-scale details of the spatial patterns should be avoided, and only their general outline should be used.
2.5. Statistical Analyses
3. Results
3.1. Study Population
3.2. Prevalence of Asthma and Other Atopic Conditions by HBA-IAP Exposure Categories
3.3. Adjusted Associations of HBA-IAP Exposure with Prevalent Health Conditions at Age 17
3.4. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. The Sensitivity of the SO2 Spatial Pattern



Appendix A.2. Temporal Variability of the Wind Pattern


References
- Goren, A.I.; Hellman, S.; Brenner, S.; Egoz, N.; Rishpon, S. Prevalence of respiratory conditions among schoolchildren exposed to different levels of air pollutants in the Haifa Bay Area, Israel. Environ. Health Perspect. 1990, 89, 225–231. [Google Scholar] [CrossRef]
- Tritscher, T.; Raz, R.; Levi, Y.; Levy, I.; Broday, D.M. Emissions vs. turbulence and atmospheric stability: A study of their relative importance in determining air pollutant concentrations. Sci. Total Environ. 2020, 733, 139300. [Google Scholar] [CrossRef]
- Israel Ministry of Environmental Protection. Air Quality Data. Available online: https://www.svivaaqm.net/Default.rtl.aspx (accessed on 31 August 2020).
- Wolf, K.; Cyrys, J.; Harciníková, T.; Gu, J.; Kusch, T.; Hampel, R.; Schneider, A.; Peters, A. Land use regression modeling of ultrafine particles, ozone, nitrogen oxides and markers of particulate matter pollution in Augsburg, Germany. Sci. Total Environ. 2017, 579, 1531–1540. [Google Scholar] [CrossRef] [Green Version]
- Irigaray, P.; Newby, J.A.; Clapp, R.; Hardell, L.; Howard, V.; Montagnier, L.; Epstein, S.; Belpomme, D. Lifestyle-related factors and environmental agents causing cancer: An overview. Biomed. Pharmacother. 2007, 61, 640–658. [Google Scholar] [CrossRef] [PubMed]
- Rumchev, K.; Brown, H.; Spickett, J. Volatile organic compounds: Do they present a risk to our health? Rev. Environ. Health 2007, 22, 39–55. [Google Scholar] [CrossRef] [PubMed]
- Maio, S.; Simoni, M.; Baldacci, S.; Sherrill, D.; Viegi, G. Indoor air pollution and airway disease. Int. J. Tuberc. Lung Dis. 2004, 8, 1401–1415. [Google Scholar]
- Miller, R.L.; Peden, D.B. Environmental effects on immune responses in patients with atopy and asthma. J. Allergy Clin. Immunol. 2014, 134, 1001–1008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weisel, C.P. Assessing exposure to air toxics relative to asthma. Environ. Health Perspect. 2002, 110 (Suppl. 4), 527–537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delfino, R.J. Epidemiologic evidence for asthma and exposure to air toxics: Linkages between occupational, indoor, and community air pollution research. Environ. Health Perspect. 2002, 110 (Suppl. 4), 573–589. [Google Scholar] [CrossRef] [PubMed]
- Health Status in Israel 2010. Israeli Center for Disease Control (ICDC). 2011. Available online: https://www.health.gov.il/PublicationsFiles/Health_Status_in_Israel2010.pdf (accessed on 5 March 2021).
- Jan, A.T.; Azam, M.; Siddiqui, K.; Ali, A.; Choi, I.; Haq, Q.M.R. Heavy metals and human health: Mechanistic insight into toxicity and counter defense system of antioxidants. Int. J. Mol. Sci. 2015, 16, 29592–29630. [Google Scholar] [CrossRef] [Green Version]
- Rosa, M.J.; Benedetti, C.; Peli, M.; Donna, F.; Nazzaro, M.; Fedrighi, C.; Zoni, S.; Marcon, A.; Zimmerman, N.; Wright, R.; et al. Association between personal exposure to ambient metals and respiratory disease in Italian adolescents: A cross-sectional study. BMC Pulm. Med. 2016, 16, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunea, D.; Iordache, S.; Liu, H.-Y.; Bøhler, T.; Pohoata, A.; Radulescu, C. Quantifying the impact of PM2.5 and associated heavy metals on respiratory health of children near metallurgical facilities. Environ. Sci. Pollut. Res. 2016, 23, 15395–15406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paz, S.; Linn, S.; Portnov, B.A.; Lazimi, A.; Futerman, B.; Barchana, M. Non-Hodgkin Lymphoma (NHL) linkage with residence near heavy roads—A case study from Haifa Bay, Israel. Health Place 2009, 15, 636–641. [Google Scholar] [CrossRef] [PubMed]
- Zusman, M.; Dubnov, J.; Barchana, M.; Portnov, B.A. Residential proximity to petroleum storage tanks and associated cancer risks: Double Kernel Density approach vs. zonal estimates. Sci. Total Environ. 2012, 441, 265–276. [Google Scholar] [CrossRef]
- Eitan, O.; Barchana, M.; Dubnov, J.; Linn, S.; Carmel, Y.; Broday, D.M. Spatial analysis of air pollution and cancer incidence rates in Haifa Bay, Israel. Sci. Total Environ. 2010, 408, 4429–4439. [Google Scholar] [CrossRef]
- Portnov, B.A.; Dubnov, J.; Barchana, M. Studying the association between air pollution and lung cancer incidence in a large metropolitan area using a kernel density function. Socioecon. Plann. Sci. 2009, 43, 141–150. [Google Scholar] [CrossRef]
- Svechkina, A.; Portnov, B.A. A new approach to spatial identification of potential health hazards associated with childhood asthma. Sci. Total Environ. 2017, 595, 413–424. [Google Scholar] [CrossRef]
- Rottenberg, Y.; Zick, A.; Barchana, M.; Peretz, T. Organ specific cancer incidence in an industrial sub-district: A population-based study with 12 years follow up. Am. J. Cancer Epidemiol. Prev. 2013, 1, 13–22. [Google Scholar]
- Freedman, D. The Ecological Fallacy. Available online: http://www.stat.berkeley.edu/~census/ecofall.txt (accessed on 5 March 2021).
- Twig, G.; Yaniv, G.; Levine, H.; Leiba, A.; Goldberger, N.; Derazne, E.; Shor, D.B.A.; Tzur, D.; Afek, A.; Shamiss, A.; et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N. Engl. J. Med. 2016, 374, 2430–2440. [Google Scholar] [CrossRef]
- Twig, G.; Reichman, B.; Afek, A.; Derazne, E.; Hamiel, U.; Furer, A.; Gershovitz, L.; Bader, T.; Cukierman-Yaffe, T.; Kark, J.D.; et al. Severe obesity and cardio-metabolic comorbidities: A nationwide study of 2.8 million adolescents. Int. J. Obes. 2019, 43, 1391–1399. [Google Scholar] [CrossRef]
- Furer, A.; Afek, A.; Sommer, A.; Keinan-Boker, L.; Derazne, E.; Levi, Z.; Tzur, D.; Tiosano, S.; Shina, A.; Glick, Y.; et al. Adolescent obesity and midlife cancer risk: A population-based cohort study of 2·3 million adolescents in Israel. Lancet Diabetes Endocrinol. 2020, 8, 216–225. [Google Scholar] [CrossRef]
- Twig, G.; Zucker, I.; Afek, A.; Cukierman-Yaffe, T.; Bendor, C.D.; Derazne, E.; Lutski, M.; Shohat, T.; Mosenzon, O.; Tzur, D.; et al. Adolescent Obesity and Early-Onset Type 2 Diabetes. Diabetes Care 2020, 43, 1487–1495. [Google Scholar] [CrossRef] [PubMed]
- Leiba, A.; Fishman, B.; Twig, G.; Gilad, D.; Derazne, E.; Shamiss, A.; Shohat, T.; Ron, O.; Grossman, E. Association of Adolescent Hypertension with Future End-stage Renal Disease. JAMA Intern. Med. 2019, 179, 517–523. [Google Scholar] [CrossRef]
- Leiba, A.; Twig, G.; Vivante, A.; Skorecki, K.; Golan, E.; Derazne, E.; Tzur, D.; Grossman, E.; Dichtiar, R.; Kark, J.D.; et al. Prehypertension among 2.19 million adolescents and future risk for end-stage renal disease. J. Hypertens. 2017, 35, 1290–1296. [Google Scholar] [CrossRef]
- Galili, E.; Barzilai, A.; Twig, G.; Caspi, T.; Daniely, D.; Shreberk-Hassidim, R.; Astman, N. Allergic rhinitis and asthma among adolescents with psoriasis: A population-based cross-sectional study. Acta Derm. Venereol. 2020, 100, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Operating Cars (Engine and Fuel) (Diesel for Transportation) Statute; Israel. 2003. Available online: https://www.nevo.co.il/law_html/law01/999_952.htm (accessed on 5 March 2021).
- Asaf, D.; Pedersen, D.; Peleg, M.; Matveev, V.; Luria, M. Evaluation of background levels of air pollutants over Israel. Atmos. Environ. 2008, 42, 8453–8463. [Google Scholar] [CrossRef]
- Broday, D.M. High-resolution spatial patterns of long-term mean concentrations of air pollutants in Haifa Bay area. Atmos. Environ. 2006, 40, 3653–3664. [Google Scholar] [CrossRef]
- Levy, I.; Levin, N.; Yuval, Y.; Schwartz, J.D.; Kark, J.D. Back-extrapolating a land use regression model for estimating past exposures to traffic-related air pollution. Environ. Sci. Technol. 2015, 49, 3603–3610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levy, I.; Broday, D.M. Improving modeled air pollution concentration maps by residual interpolation. Sci. Total Environ. 2017, 598, 780–788. [Google Scholar] [CrossRef]
- Real Time Maps & Map Data|HERE. Available online: https://www.here.com/ (accessed on 21 October 2020).
- Kloog, I.; Sorek-Hamer, M.; Lyapustin, A.; Coull, B.; Wang, Y.; Just, A.C.; Schwartz, J.; Broday, D.M. Estimating daily PM2.5 and PM10 across the complex geo-climate region of Israel using MAIAC satellite-based AOD data. Atmos. Environ. 2015, 122, 409–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shtein, A.; Karnieli, A.; Katra, I.; Raz, R.; Levy, I.; Lyapustin, A.; Dorman, M.; Broday, D.M.; Kloog, I. Estimating daily and intra-daily PM10 and PM2.5 in Israel using a spatio-temporal hybrid modeling approach. Atmos. Environ. 2018, 191, 142–152. [Google Scholar] [CrossRef]
- Kark, J.D.; Laor, A. Cigarette smoking and educational level among young Israelis upon release from military service in 1988—A public health challenge. Isr. J. Med. Sci. 1992, 28, 33–37. [Google Scholar] [PubMed]
- Shafran-Nathan, R.; Yuval; Broday, D.M. Impacts of Personal Mobility and Diurnal Concentration Variability on Exposure Misclassification to Ambient Pollutants. Environ. Sci. Technol. 2018, 52, 3520–3526. [Google Scholar] [CrossRef] [PubMed]
- Shafran-Nathan, R.; Yuval Broday, D.M. Mapping spatio-temporal variables: The impact of the time-averaging window width on the spatial accuracy. Atmos. Environ. 2005, 39, 3611–3619. [Google Scholar] [CrossRef]
- Walmsley, J.L.; Bagg, D.L. A method of correlating wind data between two stations with application to the alberta oil sands. Atmos. Ocean 1978, 16, 333–347. [Google Scholar] [CrossRef]



| Characteristic | Non-HBA n (%) | HBA-IAP Category “1” n (%) | HBA-IAP Category “2” n (%) | HBA-IAP Category “3” n (%) | HBA-IAP Category “4” n (%) |
|---|---|---|---|---|---|
| Total n | 2,216,927 | 56,480 | 56,637 | 56,587 | 56,612 |
| Male Sex | 1,321,299 (59.6) | 32,506 (57.5) | 32,368 (57.15) | 31,308 (55.3) | 32,030 (56.58) |
| Year of Birth | |||||
| 1947–1959 | 262,747 (11.9) | 8683 (15.4) | 8562 (15.1) | 7345 (13.0) | 6860 (12.1) |
| 1960–1969 | 344,439 (15.5) | 10,797 (19.1) | 10,704 (18.9) | 10,389 (18.4) | 8954 (15.8) |
| 1970–1979 | 504,159 (22.7) | 13,208 (23.4) | 15,338 (27.1) | 14,854 (26.3) | 13,609 (24.0) |
| 1980–1989 | 523,074 (23.6) | 11,933 (21.1) | 12,038 (21.2) | 13,088 (23.1) | 13,887 (24.5) |
| 1990–2001 | 582,509 (26.3) | 11,859 (21.0) | 9995 (17.7) | 10,911 (19.3) | 13,302 (23.5) |
| School Orientation | |||||
| Secular | 1,680,070 (75.8) | 45,895 (81.3) | 45,857 (81.0) | 46,567 (82.3) | 46,031 (81.3) |
| Religious | 194,218 (8.8) | 1522 (2.7) | 2519 (4.5) | 2448 (4.3) | 2980 (5.3) |
| Ultra-orthodox | 42,047 (1.9) | 502 (0.9) | 227 (0.4) | 258 (0.5) | 503 (0.9) |
| Missing | 300,593 (13.6) | 8561 (15.2) | 8034 (14.2) | 7314 (12.92) | 7098 (12.5) |
| BMI (kg/m2) | |||||
| (<18.5) | 292,938 (13.2) | 6856 (12.1) | 6783 (12.0) | 6945 (12.3) | 7147 (12.6) |
| (18.5–24.9) | 1,543,243 (69.6) | 39,786 (70.4) | 40,604 (71.7) | 40,499 (71.6) | 39,746 (70.2) |
| (25–29.9) | 244,320 (11.0) | 6647 (11.8) | 6432 (11.4) | 6358 (11.2) | 6575 (11.6) |
| (≥30) | 74,017 (3.3) | 2016 (3.6) | 1841 (3.3) | 1821 (3.2) | 2106 (3.7) |
| Missing | 62,410 (2.8) | 1173 (2.1) | 977 (1.7) | 964 (1.7) | 1038 (1.8) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raz, R.; Yuval; Lev Bar-Or, R.; Kark, J.D.; Sinnreich, R.; Broday, D.M.; Harari-Kremer, R.; Bentur, L.; Gileles-Hillel, A.; Keinan-Boker, L.; et al. Associations between Exposure to Industrial Air Pollution and Prevalence of Asthma and Atopic Diseases in Haifa Bay Area. Atmosphere 2021, 12, 516. https://doi.org/10.3390/atmos12040516
Raz R, Yuval, Lev Bar-Or R, Kark JD, Sinnreich R, Broday DM, Harari-Kremer R, Bentur L, Gileles-Hillel A, Keinan-Boker L, et al. Associations between Exposure to Industrial Air Pollution and Prevalence of Asthma and Atopic Diseases in Haifa Bay Area. Atmosphere. 2021; 12(4):516. https://doi.org/10.3390/atmos12040516
Chicago/Turabian StyleRaz, Raanan, Yuval, Ruth Lev Bar-Or, Jeremy D. Kark, Ronit Sinnreich, David M. Broday, Ruthie Harari-Kremer, Lea Bentur, Alex Gileles-Hillel, Lital Keinan-Boker, and et al. 2021. "Associations between Exposure to Industrial Air Pollution and Prevalence of Asthma and Atopic Diseases in Haifa Bay Area" Atmosphere 12, no. 4: 516. https://doi.org/10.3390/atmos12040516
APA StyleRaz, R., Yuval, Lev Bar-Or, R., Kark, J. D., Sinnreich, R., Broday, D. M., Harari-Kremer, R., Bentur, L., Gileles-Hillel, A., Keinan-Boker, L., Lyubarsky, A., Tsur, D., Afek, A., Levin, N., Derazne, E., & Twig, G. (2021). Associations between Exposure to Industrial Air Pollution and Prevalence of Asthma and Atopic Diseases in Haifa Bay Area. Atmosphere, 12(4), 516. https://doi.org/10.3390/atmos12040516








