Proton-Transfer-Reaction Mass Spectrometry for Rapid Dynamic Measurement of Ethylene Oxide Volatilization from Medical Masks
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
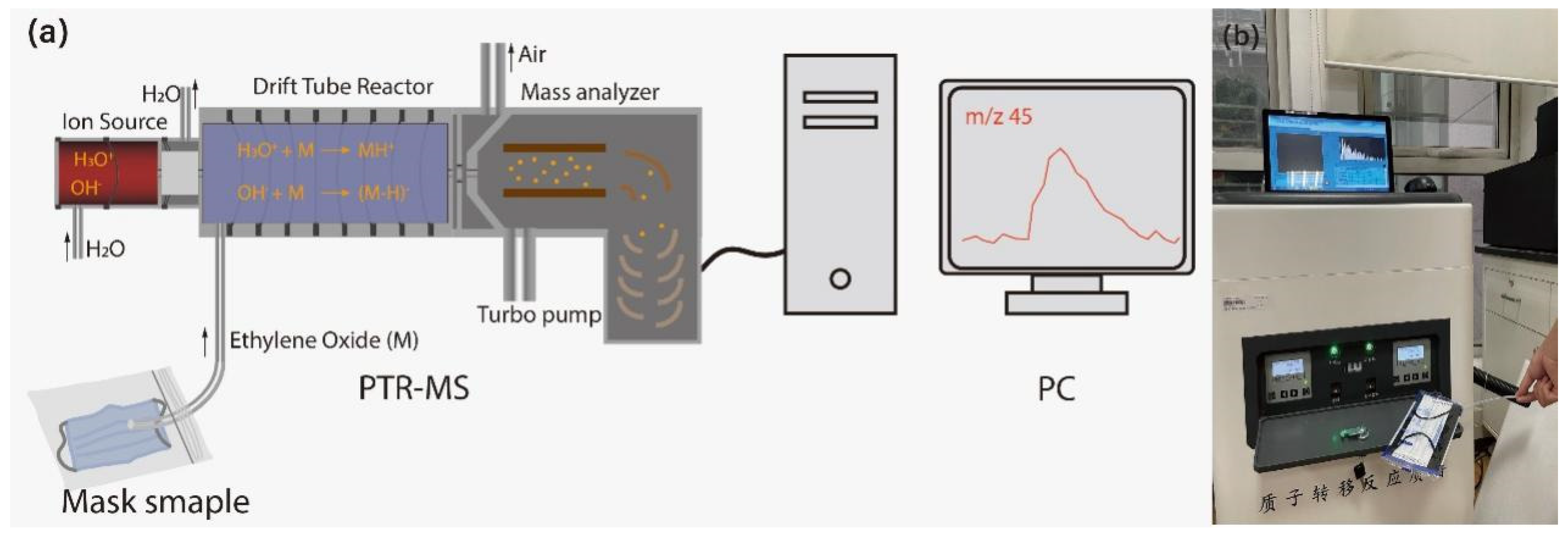
2.2. Methods
2.3. Volume of Ethylene Oxide Inhaled
3. Results and Discussion
3.1. Identification of Ethylene Oxide
3.2. Changes in the Ethylene Oxide Concentration in the Mask during Use
3.3. Mass of Ethylene Oxide Inhaled by Humans
3.4. Methods for Reducing the Ethylene Oxide Concentration in Masks
3.4.1. Natural Airing
3.4.2. Shaking the Mask
3.4.3. Blowing Air on the Mask
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gautam, S.; Hens, L.J.E. COVID-19: Impact by and on the environment, health and economy. Dev. Sustain. 2020, 22, 4953–4954. [Google Scholar]
- Liao, M.; Liu, H.; Wang, X.; Hu, X.; Huang, Y.; Liu, X.; Brenan, K.; Mecha, J.; Nirmalan, M.; Lu, J.R. A technical review of face mask wearing in preventing respiratory COVID-19 transmission. Curr. Opin. Colloid Interface Sci. 2021, 52, 101417. [Google Scholar]
- Mendes, G.C.; Brandao, T.R.; Silva, C.L. Ethylene oxide sterilization of medical devices: A review. Am. J. Infect. Control. 2007, 35, 574–581. [Google Scholar] [CrossRef] [PubMed]
- Mendes, G.; Brandão, T.R.; Silva, C.L. Ethylene oxide (EO) sterilization of healthcare products. In Sterilisation of Biomaterials and Medical Devices; Elsevier: Amsterdam, The Netherlands, 2012; pp. 71–96. [Google Scholar]
- Gollapudi, B.B.; Su, S.; Li, A.A.; Johnson, G.E.; Reiss, R.; Albertini, R.J.J.E.; Mutagenesis, M. Genotoxicity as a toxicologically relevant endpoint to inform risk assessment: A case study with ethylene oxide. Environ. Mol. Mutagen. 2020, 61, 852–871. [Google Scholar] [CrossRef]
- Jinot, J.; Fritz, J.M.; Vulimiri, S.V.; Keshava, N. Carcinogenicity of ethylene oxide: Key findings and scientific issues. Toxicol. Mech. Methods 2018, 28, 386–396. [Google Scholar] [PubMed]
- Kirman, C.R.; Li, A.A.; Sheehan, P.J.; Bus, J.S.; Lewis, R.C.; Hays, S.M. Ethylene oxide review: Characterization of total exposure via endogenous and exogenous pathways and their implications to risk assessment and risk management. J. Toxicol. Environ. Health Part B 2021, 24, 1–29. [Google Scholar] [CrossRef] [PubMed]
- IARC. 1,3-Butadiene, Ethylene Oxide and Vinyl Halides (Vinyl Fluoride, Vinyl Chloride and Vinyl Bromide); IARC: Lyon, France, 2008; Volume 97, p. 3.
- World Health Organization. IARC Monographs on the Identification of Carcinogenic Hazards to Humans; IARC: Lyon, France, 2020; Volume 97, pp. 1–125.
- Tsai, S.-W.; Tsai, S.-T.; Wang, V.-S.; Lai, J.-S. Laboratory and field validations of a solid-phase microextraction device for the determination of ethylene oxide. J. Chromatogr. A 2004, 1026, 25–30. [Google Scholar] [CrossRef]
- Ge, Y.; Jun, F.; Taohong, H. Determination of ethylene oxide and 2-chloroethanol in medical masks and protective clothing by headspace-gas chromatography. Environ. Chem. 2020, 39, 1448–1450. [Google Scholar]
- Salter, W.B.; Kinney, K.; Wallace, W.H.; Lumley, A.E.; Heimbuch, B.K.; Wander, J.D. Analysis of residual chemicals on filtering facepiece respirators after decontamination. J. Occup. Environ. Hyg. 2010, 7, 437–445. [Google Scholar] [CrossRef]
- Lee, D.; Cojocariu, C. A Fast, Cost-Effective HS-GC-FID Method for the Analysis of Ethylene Oxide in Surgical-Style face Masks; Thermo Fisher Scientific: Runcorn, UK, 2020. [Google Scholar]
- Hansel, A.; Jordan, A.; Holzinger, R.; Prazeller, P.; Vogel, W.; Lindinger, W. Proton transfer reaction mass spectrometry: On-line trace gas analysis at the ppb level. Int. J. Mass Spectrom. Ion Process. 1995, 149, 609–619. [Google Scholar]
- Lindinger, W.; Jordan, A. Proton-transfer-reaction mass spectrometry (PTR–MS): On-line monitoring of volatile organic compounds at pptv levels. Chem. Soc. Rev. 1998, 27, 347–375. [Google Scholar] [CrossRef]
- Ellis, A.M.; Mayhew, C.A. Proton Transfer Reaction Mass Spectrometry: Principles and Applications; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Hartungen, E.; Jürschik, S.; Jordan, A.; Edtbauer, A.; Feil, S.; Hanel, G.; Seehauser, H.; Haidacher, S.; Schottkowsky, R.; Märk, L.; et al. Proton transfer reaction-mass spectrometry: Fundamentals, recent advances and applications. Eur. Phys. J. Appl. Phys. 2013, 61, 24303. [Google Scholar] [CrossRef]
- Pedrotti, M.; Spaccasassi, A.; Biasioli, F.; Fogliano, V. Ethnicity, gender and physiological parameters: Their effect on in vivo flavour release and perception during chewing gum consumption. Food Res. Int. 2019, 116, 57–70. [Google Scholar] [CrossRef]
- Amann, A.; Poupart, G.; Telser, S.; Ledochowski, M.; Schmid, A.; Mechtcheriakov, S. Applications of breath gas analysis in medicine. Int. J. Mass Spectrom. 2004, 239, 227–233. [Google Scholar]
- Han, K.H.; Zhang, J.S.; Wargocki, P.; Knudsen, H.N.; Guo, B. Determination of material emission signatures by PTR-MS and their correlations with odor assessments by human subjects. Indoor Air 2010, 20, 341–354. [Google Scholar] [PubMed]
- Beale, R.; Liss, P.S.; Dixon, J.L.; Nightingale, P.D. Quantification of oxygenated volatile organic compounds in seawater by membrane inlet-proton transfer reaction/mass spectrometry. Anal. Chim. Acta 2011, 706, 128–134. [Google Scholar]
- De Gouw, J.; Warneke, C. Measurements of volatile organic compounds in the earth’s atmosphere using proton-transfer-reaction mass spectrometry. Mass Spectrom. Rev. 2007, 26, 223–257. [Google Scholar] [CrossRef]
- Karl, T.; Harren, F.; Warneke, C.; De Gouw, J.; Grayless, C.; Fall, R. Senescing grass crops as regional sources of reactive volatile organic compounds. J. Geophys. Res. Atmos. 2005, 110. [Google Scholar] [CrossRef]
- Mozaffar, A.; Schoon, N.; Bachy, A.; Digrado, A.; Heinesch, B.; Aubinet, M.; Fauconnier, M.L.; Delaplace, P.; du Jardin, P.; Amelynck, C. Biogenic volatile organic compound emissions from senescent maize leaves and a comparison with other leaf developmental stages. Atmos. Environ. 2018, 176, 71–81. [Google Scholar]
- Bianchi, T.; Weesepoel, Y.; Koot, A.; Iglesias, I.; Eduardo, I.; Gratacós-Cubarsí, M.; Guerrero, L.; Hortós, M.; van Ruth, S. Investigation of the aroma of commercial peach (Prunus persica L. Batsch) types by Proton Transfer Reaction–Mass Spectrometry (PTR-MS) and sensory analysis. Food Res. Int. 2017, 99, 133–146. [Google Scholar]
- Majchrzak, T.; Wojnowski, W.; Wasik, A. Revealing dynamic changes of the volatile profile of food samples using PTR–MS. Food Chem. 2021, 364, 130404. [Google Scholar] [PubMed]
- Del Río, R.F.; O’Hara, M.E.; Pemberton, P.; Whitehouse, T.; Mayhew, C.A. Elimination characteristics of post-operative isoflurane levels in alveolar exhaled breath via PTR-MS analysis. J. Breath Res. 2016, 10, 046006. [Google Scholar] [CrossRef] [PubMed]
- Moser, B.; Bodrogi, F.; Eibl, G.; Lechner, M.; Rieder, J.; Lirk, P. Mass spectrometric profile of exhaled breath—Field study by PTR-MS. Respir. Physiol. Neurobiol. 2005, 145, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Nyord, T.; Rong, L.; Feilberg, A. Real-time quantification of emissions of volatile organic compounds from land spreading of pig slurry measured by PTR-MS and wind tunnels. Sci. Total Environ. 2018, 639, 1079–1087. [Google Scholar] [CrossRef]
- Ramirez, K.S.; Lauber, C.L.; Fierer, N. Microbial consumption and production of volatile organic compounds at the soil-litter interface. Biogeochemistry 2010, 99, 97–107. [Google Scholar] [CrossRef]
- Hallett, S.; Toro, F.; Ashurst, J.V. Physiology, Tidal Volume. 2018. Available online: http://europepmc.org/abstract/MED/29494108 (accessed on 12 January 2024).
- Wang, Y.; Shen, C.; Li, J.; Wang, H.; Wang, H.; Jiang, H.; Chu, Y. Thermal desorption extraction proton transfer reaction mass spectrometer (TDE-PTR-MS) for rapid determination of residual solvent and sterilant in disposable medical devices. J. Pharm. Biomed. Anal. 2011, 55, 1213–1217. [Google Scholar]
- Liu, Y.; Wang, Z.; Wang, W.; Xing, J.; Zhang, Q.; Ma, Q.; Lv, Q. Non-targeted analysis of unknown volatile chemicals in medical masks. Environ. Int. 2022, 161, 107122. [Google Scholar]
- Yáñez-Serrano, A.M.; Filella, I.; Llusià, J.; Gargallo-Garriga, A.; Granda, V.; Bourtsoukidis, E.; Williams, J.; Seco, R.; Cappellin, L.; Werner, C.; et al. GLOVOCS—Master compound assignment guide for proton transfer reaction mass spectrometry users. Atmos. Environ. 2021, 244, 117929. [Google Scholar] [CrossRef]
- Lepelletier, D.; Grandbastien, B.; Romano-Bertrand, S.; Aho, S.; Chidiac, C.; Géhanno, J.F.; Chauvin, F. What face mask for what use in the context of the COVID-19 pandemic? The French guidelines. J. Hosp. Infect. 2020, 105, 414–418. [Google Scholar] [CrossRef]





| Number | Group | Brand and Source of Masks |
|---|---|---|
| 1 | A | AISHIYIJIA, Zhejiang, China |
| 2 | B | YOUHEKANG, Guangzhou, China |
| 3 | C | MILKON, Xiantao, China |
| 4 | D | ZHENDE, Shaoxing, China |
| 5 | E | YALANSHI, Wuhan, China |
| No. | Gender | Age/Year | Height/cm | Weight/kg | Smoking or Not |
|---|---|---|---|---|---|
| 1 | Female | 25 | 165 | 50 | No |
| 2 | Female | 10 | 142 | 31 | No |
| 3 | Male | 28 | 176 | 73 | No |
| 4 | Male | 32 | 175 | 76 | No |
| 5 | Male | 8 | 132 | 26 | No |
| 6 | Male | 10 | 137 | 33 | No |
| Group | A | B | C | D |
|---|---|---|---|---|
| Concentration of ethylene oxide (ppbv) | 37.2 | 104.8 | 41.5 | 30.5 |
| Group | A | B | C | D |
|---|---|---|---|---|
| Ratio of ethylene oxide decrease (ppbv/min) | 33.86 | 74.5 | 23.61 | 34.08 |
| Inhalation of ethylene oxide (μg) | 0.40 | 1.02 | 0.27 | 0.40 |
| Safety Standards | GBZ2.1-2019(China) | ACGIH, OSHA | NIOSH |
|---|---|---|---|
| Upper limit of ethylene oxide inhalation (μg) | 72 | 64.79 | 6.48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, R.; Zhang, Y.; Jiao, L.; Zhao, X.; Gao, Z.; Dong, D. Proton-Transfer-Reaction Mass Spectrometry for Rapid Dynamic Measurement of Ethylene Oxide Volatilization from Medical Masks. Atmosphere 2024, 15, 114. https://doi.org/10.3390/atmos15010114
Wang R, Zhang Y, Jiao L, Zhao X, Gao Z, Dong D. Proton-Transfer-Reaction Mass Spectrometry for Rapid Dynamic Measurement of Ethylene Oxide Volatilization from Medical Masks. Atmosphere. 2024; 15(1):114. https://doi.org/10.3390/atmos15010114
Chicago/Turabian StyleWang, Runyu, Yunhe Zhang, Leizi Jiao, Xiande Zhao, Zhen Gao, and Daming Dong. 2024. "Proton-Transfer-Reaction Mass Spectrometry for Rapid Dynamic Measurement of Ethylene Oxide Volatilization from Medical Masks" Atmosphere 15, no. 1: 114. https://doi.org/10.3390/atmos15010114
APA StyleWang, R., Zhang, Y., Jiao, L., Zhao, X., Gao, Z., & Dong, D. (2024). Proton-Transfer-Reaction Mass Spectrometry for Rapid Dynamic Measurement of Ethylene Oxide Volatilization from Medical Masks. Atmosphere, 15(1), 114. https://doi.org/10.3390/atmos15010114







