Differential Impacts on Human Physiological Responses on Heatwave and Non-Heatwave Days: A Comparative Study Using Wearable Devices in Beijing
Abstract
1. Introduction
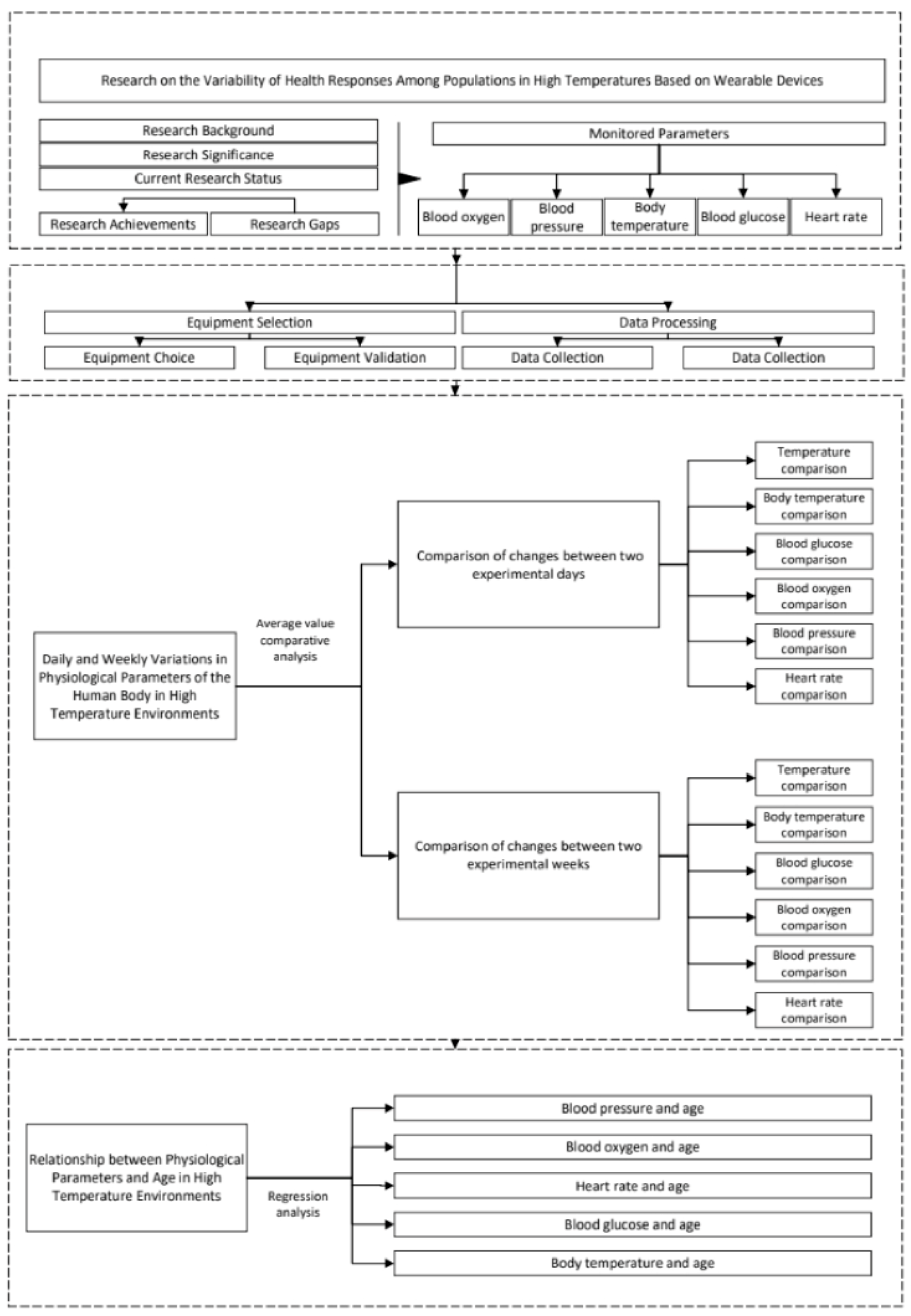
2. Materials and Methods
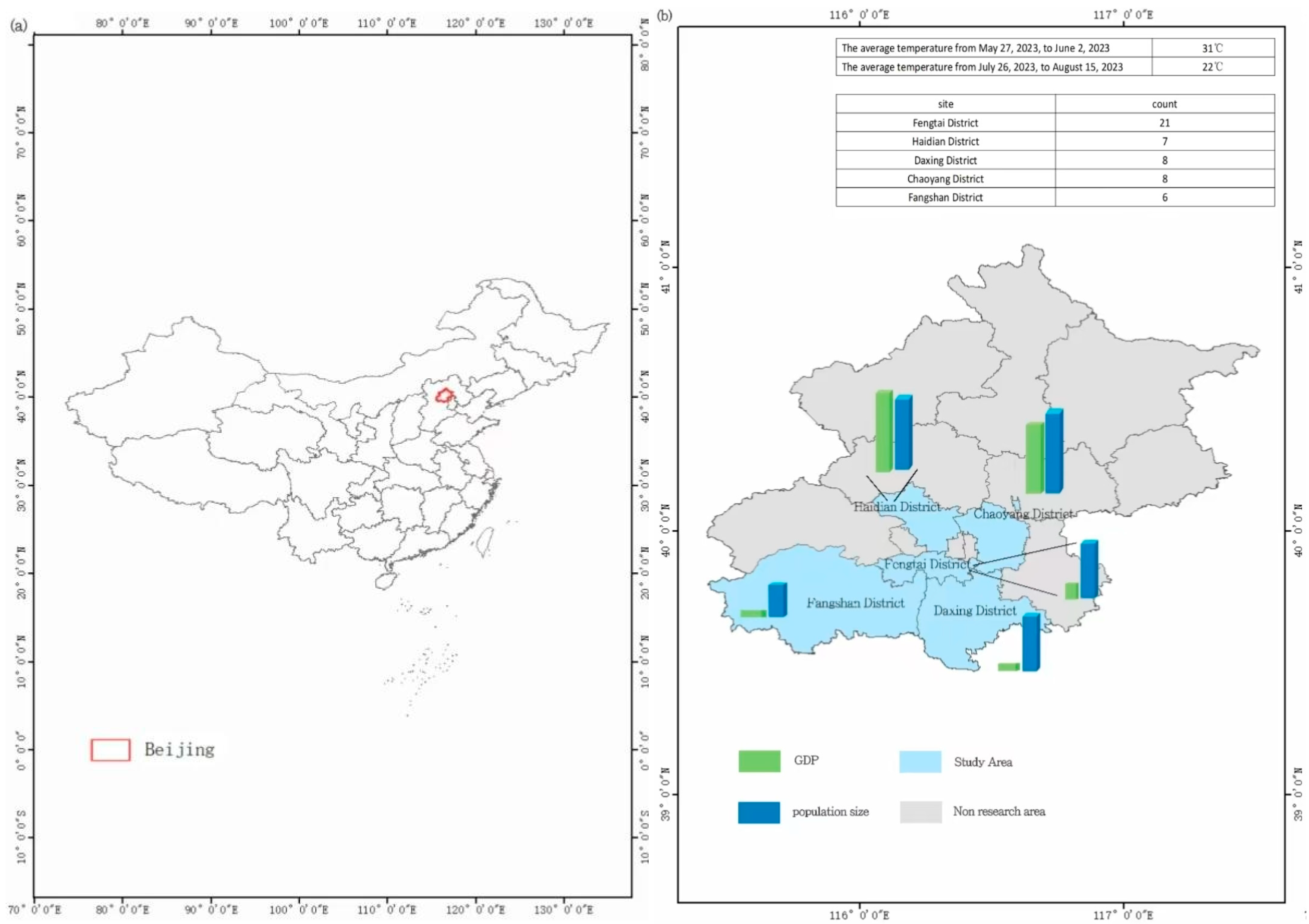
2.1. Study Area
2.2. Instruments and Data
2.3. Technical Approach
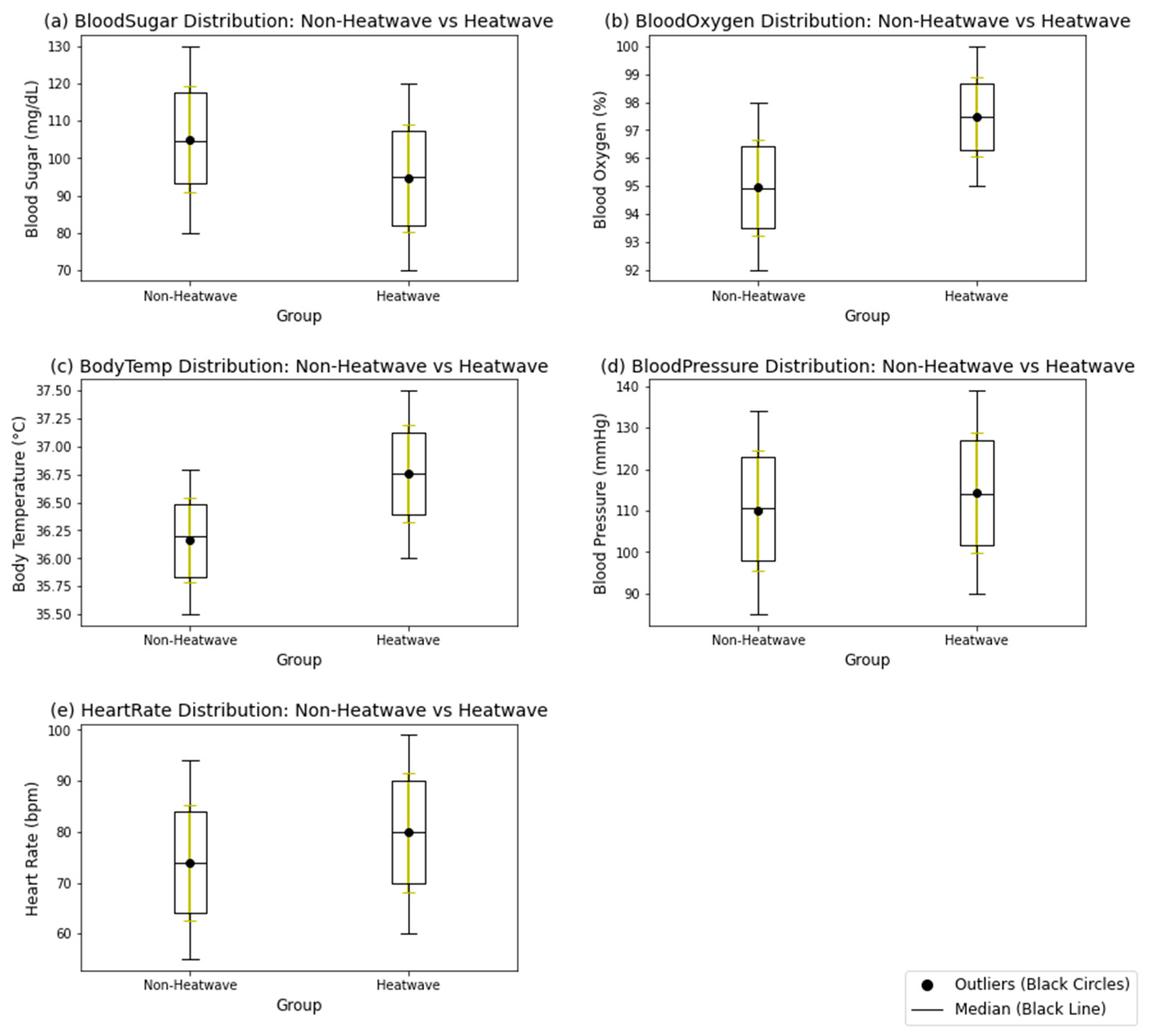
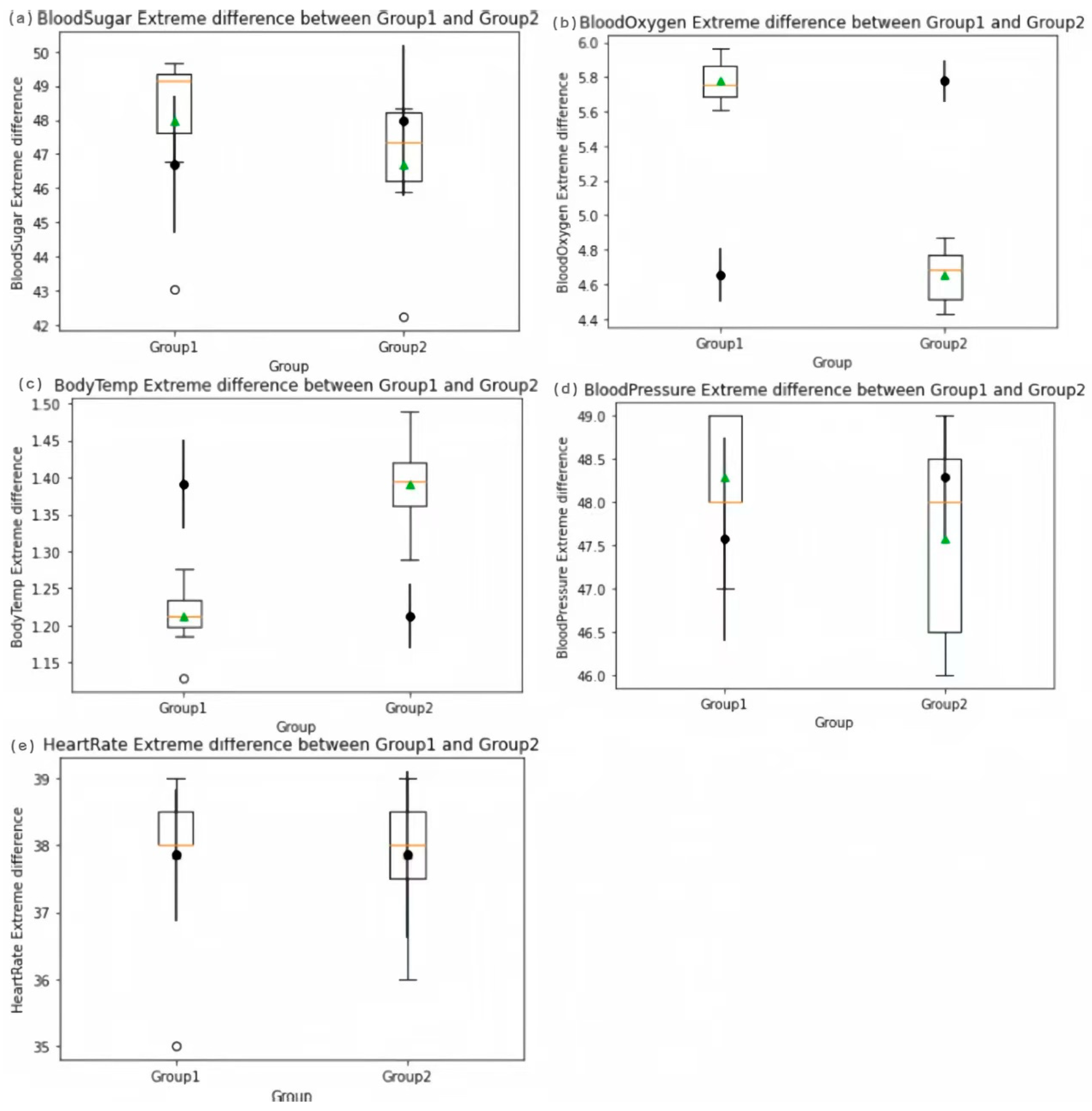
3. Results
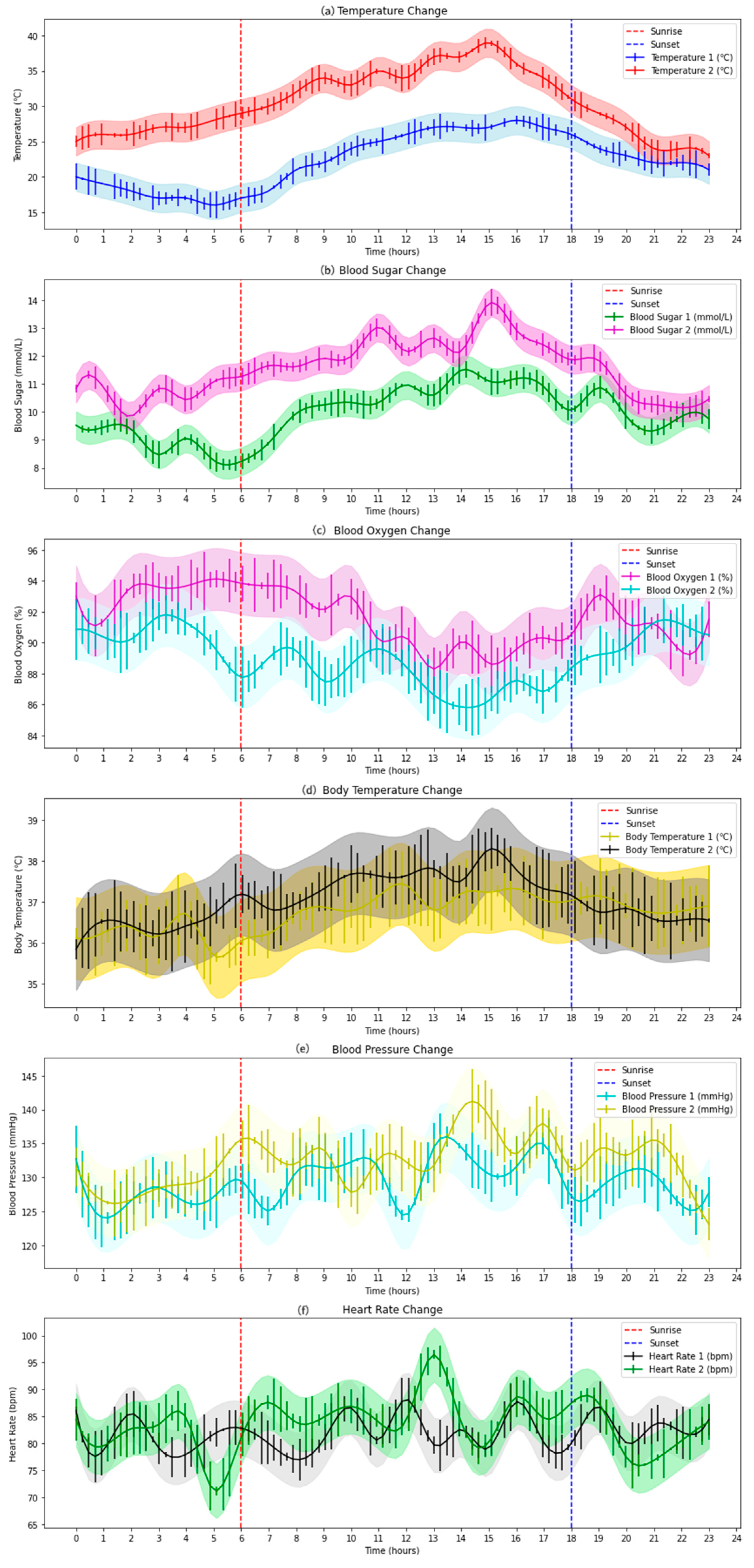
3.1. Daily and Weekly Variations of Human Physiological Parameters
3.1.1. Changes in Daily Average Values of Human Physiological Parameters
3.1.2. Changes in Weekly Average Values of Human Physiological Parameters
Study of Daily Variations
Study of Weekly Variations
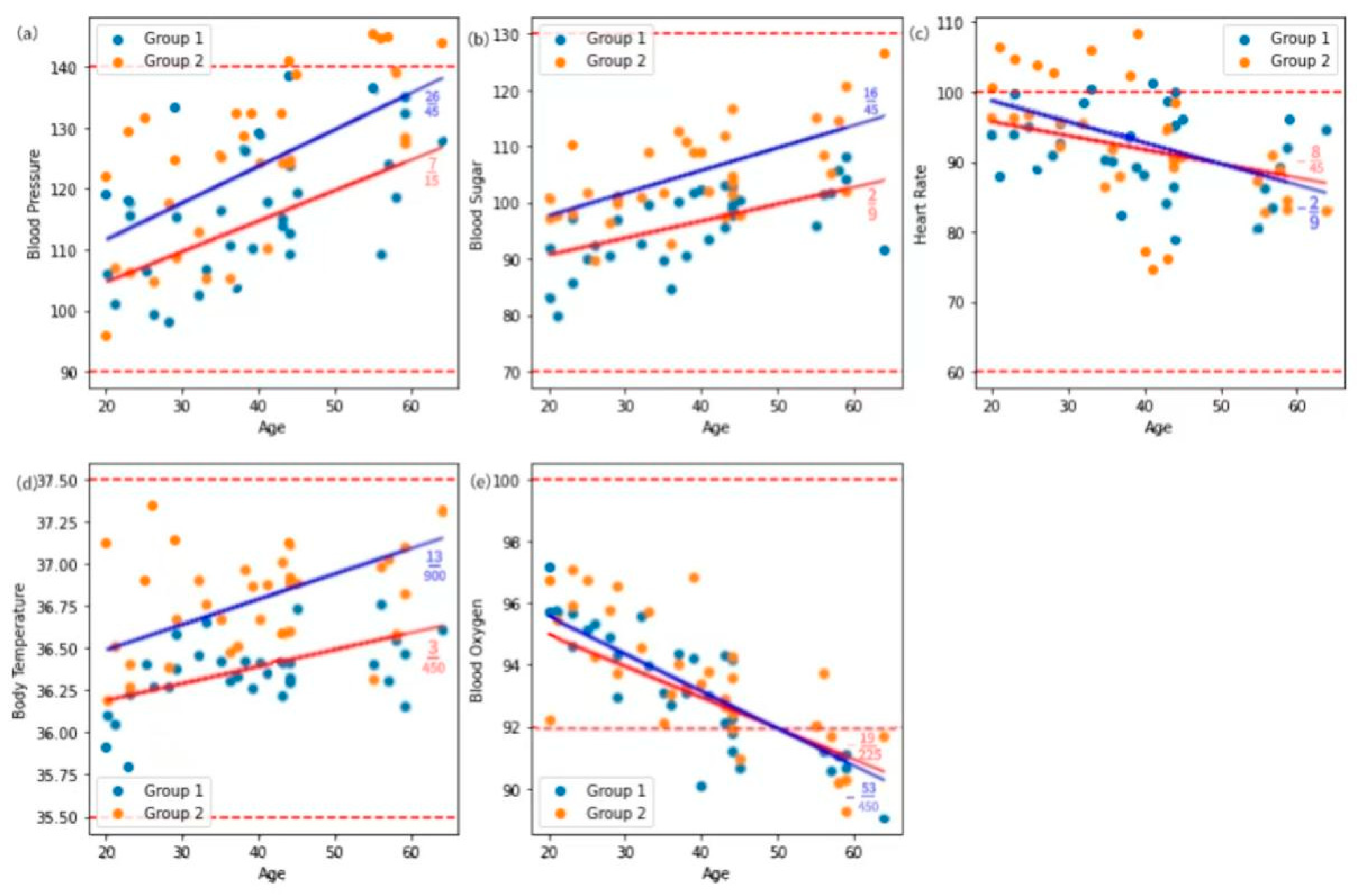
3.2. Relationship Between Human Physiological Parameters and Age
3.2.1. Relationship Between Blood Pressure and Age
3.2.2. Relationship Between Blood Glucose and Age
3.2.3. Relationship Between Heart Rate and Age
3.2.4. Relationship Between Body Temperature and Age
3.2.5. Relationship Between Blood Oxygen and Age
3.2.6. Variation of Physiological Parameters in Age
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Romanello, M.; Napoli, C.D.; Drummond, P.; Green, C.; Kennard, H.; Lampard, P.; Scamman, D.; Walawender, M.; Ali, Z.; Ameli, N.; et al. The 2023 Report of the Lancet Countdown on Health and Climate Change: The Imperative for a Health-Centred Response in a World Facing Irreversible Harms. Lancet 2023, 402, 2346–2394. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Sun, Y. Long-Term Changes in Summer Extreme Wet Bulb Globe Temperature over China. J. Meteorol. Res. 2021, 35, 975–986. [Google Scholar] [CrossRef]
- Hsiang, S.M.; Burke, M. Temperature and mortality: An analysis of the United States from 2000 to 2019. JAMA 2021, 326, 1039–1049. [Google Scholar]
- Climate Change Is Bad for Health but Climate Services Save Lives. WMO News. 2 November 2023. Available online: https://wmo.int/media/news/climate-change-bad-health-climate-services-save-lives (accessed on 11 December 2023).
- Campbell-Lendrum, D.; Neville, T.; Schweizer, C.; Neira, M. Climate change and health: Three grand challenges. Nat. Med. 2023, 29, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Kjellstrom, T.; Holmer, I.; Lemke, B. Workplace Heat Stress, Health, and Productivity. J. Occup. Environ. Med. 2016, 58, e86–e91. [Google Scholar]
- Gonzalez-Alonso, J.; Crandall, C.G.; Johnson, J.M. The Cardiovascular Challenge of Exercising in the Heat. J. Appl. Physiol. 2008, 105, 682–688. [Google Scholar] [CrossRef]
- Ha, C.-M.; Park, S.; Choi, Y.-K.; Jeong, J.-Y.; Oh, C.J.; Bae, K.-H.; Lee, S.J.; Kim, J.-H.; Park, K.-G.; Jun, D.Y.; et al. Activation of nrf2 by dimethyl fumarate improves vascular calcification. Vasc. Pharmacol. 2014, 63, 29–36. [Google Scholar] [CrossRef]
- Wang, M.-Z.; Zhang, S.; Wang, S.-G. Research Progress of Influence of High Temperature and Heat Wave on Human Health. J. Environ. Health 2012, 29, 662–664. [Google Scholar]
- He, Z. Geoengineering: Proactive Measures to Tackle Climate Change. Natl. Sci. Rev. 2024, 11, 299–304. [Google Scholar]
- Yan, Y.; Zhang, H. Tackling Climate Change: China in Action. China Today 2024, 73, 26–31. [Google Scholar]
- He, B. High-Temperature Work and Human Thermal Response: Factors and Assessment of Heat Stress. Ph.D. Thesis, Chongqing University, Chongqing, China, 2023. (In Chinese). [Google Scholar]
- Wang, Y.; Zou, Y.; Li, Z. Emerging intelligent wearable devices for cardiovascular health monitoring. Nano Today 2024, 59, 102544. [Google Scholar] [CrossRef]
- Knudsen, M.T.; Hoyer, S.; Frost, F. Prehabilitation in Urological Oncology: A Systematic Review. BJU Int. 2020, 125, 483–493. [Google Scholar]
- Gustafsson, U.O.; Scott, M.J.; Schwenk, W.; Demartines, N.; Roulin, D.; Francis, N.; McNaught, C.E.; MacFie, J.; Liberman, A.S.; Soop, M.; et al. Guidelines for Perioperative Care in Elective Colonic Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J. Surg. 2011, 35, 245–256. [Google Scholar]
- Yin, F.; Hongsen, N.; Shin, Y.K.; Li, Y.; Kim, E.S.; Kim, N.Y. A wearable device based on the ionic liquid decorated sponge-like ultraviolet-curable resin for recognizing human mental health conditions. Nano Energy 2023, 118 Pt B, 109039. [Google Scholar] [CrossRef]
- Contini, M.S.; Martins, L.E.G. Wearable Device Sensing Technologies: A Systematic Literature Review. Res. Biomed. Eng. 2024, 40, 69–84. [Google Scholar] [CrossRef]
- Ichwana, D.; Ikhlas, R.Z.; Ekariani, S. Heart Rate Monitoring System During Physical Exercise for Fatigue Warning Using Non-invasive Wearable Sensor. In Proceedings of the International Conference on Information Technology Systems and Innovation (ICITSI 2008), Bandung, Indonesia, 22 October 2008; pp. 497–502. [Google Scholar] [CrossRef]
- Vonteddu, S.N.R.; Nunna, P.; Jain, S.; Diwakar, G. Smart Wearable Wristband for Patients’ Health Monitoring System through IoT. In Proceedings of the International Conference on Power, Energy, Control and Transmission Systems (ICPECTS 2022), Chennai, India, 8 December 2022; pp. 1–6. [Google Scholar] [CrossRef]
- Masoumian Hosseini, M.; Masoumian Hosseini, S.T.; Qayumi, K.; Hosseinzadeh, S.; Sajadi Tabar, S.S. Smartwatches in Healthcare Medicine: Assistance and Monitoring; A Scoping Review. BMC Med. Inform. Decis. Mak. 2023, 23, 248. [Google Scholar] [CrossRef]
- Andersen, Z.J.; Vicedo-Cabrera, A.M.; Hoffmann, B.; Melén, E. Climate Change and Respiratory Disease: Clinical Guidance for Healthcare Professionals. Breathe 2023, 19, 220222. [Google Scholar] [CrossRef] [PubMed]
- Vedantam, D.; Poman, D.S.; Motwani, L.; Asif, N.; Patel, A.; Anne, K.K. Stress-Induced Hyperglycemia: Consequences and Management. Cureus 2022, 14, e26714. [Google Scholar] [CrossRef]
- Romanovsky, A.A. Skin Temperature: Its Role in Thermoregulation. Acta Physiol. 2014, 210, 498–507. [Google Scholar] [CrossRef]
- Hasan, F.; Marsia, S.; Patel, K.; Agrawal, P.; Razzak, J.A. Effective Community-Based Interventions for the Prevention and Management of Heat-Related Illnesses: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 8362. [Google Scholar] [CrossRef]
- Ma, Y.; Lu, L.; Xiao, D.; Cai, M.; Ren, C.; Zhou, M.; Hui, W.; Li, Q. Urban Thermal Environment Analysis by Local Climate Zone in Beijing. J. Beijing Norm. Univ. (Nat. Sci.) 2022, 58, 901–909. [Google Scholar] [CrossRef]
- Hernandez, N.; Castro, L.; Medina-Quero, J.; Favela, J.; Michán, L.; Mortenson, W.B. Scoping Review of Healthcare Literature on Mobile, Wearable, and Textile Sensing Technology for Continuous Monitoring. J. Healthc. Inform. Res. 2021, 5, 270–299. [Google Scholar] [CrossRef] [PubMed]
- Nehra, K.A.; Gettman, T.M.; Rivera, E.M.; Agarwal, D.; O’Neil, D.; Jenkins, S.; Viers, B. Patients Are Willing to Utilize Wearable Devices for Their Care: A Survey of Perceptions and Acceptance of Wearable Technology for Health Monitoring in a Urological Patient Population. Urol. Pract. 2017, 4, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Xie, M.; Feng, Q.; Li, Z.; Chu, L.; Liu, Q. Heat Risk of Residents in Different Types of Communities from Urban Heat-Exposed Areas. Sci. Total Environ. 2021, 768, 145052. [Google Scholar] [CrossRef]
- Liu, Q.; Xie, M.; Wu, R.; Xue, Q.; Chen, B.; Li, Z.; Li, X. From Expanding Areas to Stable Areas: Identification, Classification, and Determinants of Multiple Frequency Urban Heat Islands. Ecol. Indic. 2021, 130, 108046. [Google Scholar] [CrossRef]
- Xuecheng, F.; Lei, Y.; Shuo, S. Accessing the Heat Exposure Risk in Beijing–Tianjin–Hebei Region Based on Heat Island Footprint Analysis. Atmosphere 2022, 13, 739. [Google Scholar] [CrossRef]
- Lei, J.; Xie, M.; Chen, B.; Su, W.; Zhao, X.; Wu, R. Key areas and measures to mitigate heat exposure risk in highly urbanized city: A case study of Beijing, China. Urban Clim. 2024, 53, 101748. [Google Scholar]
- Qunfang, H. Variation Characteristics of Summer High Temperature and Its Influence on Urban Heat Island Intensity in Beijing. Meteorol. Sci. Technol. 2023, 51, 66–74. (In Chinese) [Google Scholar] [CrossRef]
- Liu, Q.; Xie, M.; Peng, J.; Zhou, X.; Yang, K.; Zhu, R.; Liu, Y. Revealing the Urban Heat Exposure Risk Network: Exploring the Possibility of Mitigating Heat-Related Risks from a Network Perspective. Sustain. Cities Soc. 2024, 112, 105592. [Google Scholar] [CrossRef]
- Lu, S.; Jia, W.; Shuping, C. Population Spatial Distribution Based on Luojia 1-01 Nighttime Light Image: A Case Study of Beijing. Chin. Geogr. Sci. 2021, 31, 966–978. [Google Scholar]
- Chen, Y.; Qin, X. The Impact of Extreme Temperature Shocks on the Health Status of the Elderly in China. Int. J. Environ. Res. Public Health 2022, 19, 15729. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ren, Y.; Song, L.; Xiang, Y. Responses of extreme high temperatures to urbanization in the Beijing–Tianjin–Hebei urban agglomeration in the context of a changing climate. Meteorol. Appl. 2021, 28, e2024. [Google Scholar]
- Cai, F.; Liu, C.; Gerten, D.; Yang, S.; Zhang, T.; Lin, S.; Kurths, J. Pronounced Spatial Disparity of Projected Heatwave Changes Linked to Heat Domes and Land-Atmosphere Coupling. npj Clim. Atmos. Sci. 2024, 7, 225. [Google Scholar] [CrossRef]
- Jiayan, L.; Ranhao, S.; Jialei, L.; Yongfu, M.; Meng, Z.; Liding, C. Human Extreme Heat Protective Behaviours: The Effects of Physical Risks, Psychological Perception, and Public Measures. Humanit. Soc. Sci. Commun. 2024, 11, 327. [Google Scholar]
- Parati, G.; Ochoa, J.; Lombardi, C.; Bilo, G. Assessment and Management of Blood-Pressure Variability. Nat. Rev. Cardiol. 2013, 10, 143–155. [Google Scholar] [CrossRef]
- Fatisson, J.; Oswald, V.; Lalonde, F. Influence Diagram of Physiological and Environmental Factors Affecting Heart Rate Variability: An Extended Literature Overview. Heart Int. 2016, 11, e32–e40. [Google Scholar] [CrossRef]
- Lv, Y.; Huo, Z. Special Environmental Physiology; Military Medical Science Press: Beijing, China, 2003. (In Chinese) [Google Scholar]
- Hu, Y.; Zhang, P.; Ding, B.; Cao, X.; Zhong, Y.; Lee, K.O.; Ma, J.H. Response of Blood Glucose and GLP-1 to Different Food Temperature in Normal Subjects and Patients with Type 2 Diabetes. Nutr. Diabetes 2022, 12, 28. [Google Scholar] [CrossRef]
- Pastor, M.C. Hyperthermia Decreases the Response to Vasoconstrictors in Rat Portal Veins. Eur. J. Pharmacol. 2004, 494, 191–197. [Google Scholar]
- Wolsk, E.; Bakkestrom, R.; Thomsen, H.J.; Balling, L.; Andersen, M.J.; Dahl, J.S.; Hassager, C.; Møller, J.E.; Gustafsson, F. The Influence of Age on Hemodynamic Parameters During Rest and Exercise in Healthy Individuals. JACC Heart Fail. 2016, 5, 337–346. [Google Scholar]
- Suzuki, Y.; Kaneko, H.; Yano, Y.; Okada, A.; Itoh, H.; Matsuoka, S.; Fujiu, K.; Yamaguchi, S.; Michihata, N.; Jo, T.; et al. Age-Dependent Relationship of Hypertension Subtypes With Incident Heart Failure. J. Am. Heart Assoc. 2022, 11, e025406. [Google Scholar] [CrossRef]
- Ou, Q.; Wu, R. The Relationship Between Blood Sugar and Age. Intermed. Med. J. 1996, 3, 18–19. (In Chinese) [Google Scholar]
- Sun, S.; Guo, Y.; Ruan, Y.; Zheng, Y.; Huang, Z.Z.; Shi, Y.; Wu, F. Association Between Quality of Life and Physical Activity Among People Aged 50 Years and Over. Chin. J. Epidemiol. 2019, 40, 1245–1251. [Google Scholar] [CrossRef]
- Mostardi, R.; Kubica, R.; Veicsteinas, A.; Margaria, R. The Effect of Increased Body Temperature Due to Exercise on the Heart Rate and on the Maximal Aerobic Power. Eur. J. Appl. Physiol. 1974, 33, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, S.; Gupta, S.; Mishra, M.K. Electrolytes and Acid-Base Disorders. In Clinical Applications of Biomolecules in Disease Diagnosis; Singh, R.L., Singh, P., Pathak, N., Eds.; Springer: Singapore, 2024; p. 7. [Google Scholar] [CrossRef]
- Kenny, G.P.; Notley, S.R.; Flouris, A.D.; Nybo, L. Effects of Increased Activity Level on Physiological and Subjective Responses at Different High Temperatures. Appl. Ergon. 2021, 93, 103384. [Google Scholar]
- Wang, L.Y.; Feng, M.; Hu, X.Y.; Tang, M.L. Association of Daily Health Behavior and Activity of Daily Living in Older Adults in China. Sci. Rep. 2023, 13, 19484. [Google Scholar] [CrossRef]
- Lim, C.L. Fundamental Concepts of Human Thermoregulation and Adaptation to Heat: A Review in the Context of Global Warming. Int. J. Environ. Res. Public Health 2020, 17, 7795. [Google Scholar] [CrossRef]
- Cramer, M.N.; Gagnon, D.; Laitano, O.; Crandall, C.G. Human Temperature Regulation Under Heat Stress in Health, Disease, and Injury. Physiol. Rev. 2022, 102, 1907–1989. [Google Scholar] [CrossRef]


| Feature/Product Name | Wearing Position | Battery Life | GPS Accuracy | Sleep Quality Monitoring | Heart Rate Monitoring | Body Temperature Monitoring | High-Temperature Alert | Blood Oxygen Monitoring |
|---|---|---|---|---|---|---|---|---|
| ① | Wrist | 5–18 h | × | √ | √ | √ | × | √ |
| ② | Wrist | 3–12 days | × | √ | √ | × | × | √ |
| ③ | Wrist | 3–12 days | × | √ | √ | × | × | √ |
| ④ | Wrist | 7–14 days | √ | √ | √ | √ | × | √ |
| ⑤ | Wrist | 10–14 days | × | √ | √ | × | × | √ |
| ⑥ | Finger | 4–7 days | × | √ | √ | √ | × | √ |
| ⑦ | Wrist | 3–5 days | × | √ | √ | √ | × | √ |
| ⑧ | Wrist | 3–7 days | × | √ | √ | √ | √ | √ |
| ⑨ | Wrist | 10–14 days | × | √ | √ | × | × | √ |
| Factors | Classification | Percentage |
|---|---|---|
| Gender | Male | 77.1% |
| Female | 22.9% | |
| Age | <30 | 25.7% |
| 30–50 | 51.4% | |
| >50 | 22.9% | |
| Education Level | High school/Technical school or below | 25.7% |
| High school/Technical school | 54.3% | |
| Bachelor’s degree and above | 20.0% | |
| Geographical Location | Fengtai District | 41.4% |
| Haidian District | 14.3% | |
| Daxing District | 15.7% | |
| Chaoyang District | 15.7% | |
| Fangshan District | 12.9% | |
| Outdoor Activity Frequency (Per Day) | None or very little | 51.4% |
| Two hours or more | 11.4% | |
| Six hours or more | 37.2% | |
| Monthly Income | <1000 | 8.6% |
| 1000–5000 | 45.7% | |
| 5000–10,000 | 11.4% | |
| >10,000 | 34.3% | |
| Coping Strategies | Yes | 60.0% |
| No | 40.0% | |
| Social Support | Yes | 62.8% |
| No | 37.2% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheng, T.; Liu, Q.; Kou, Y.; Shang, G.; Xie, M. Differential Impacts on Human Physiological Responses on Heatwave and Non-Heatwave Days: A Comparative Study Using Wearable Devices in Beijing. Atmosphere 2025, 16, 413. https://doi.org/10.3390/atmos16040413
Sheng T, Liu Q, Kou Y, Shang G, Xie M. Differential Impacts on Human Physiological Responses on Heatwave and Non-Heatwave Days: A Comparative Study Using Wearable Devices in Beijing. Atmosphere. 2025; 16(4):413. https://doi.org/10.3390/atmos16040413
Chicago/Turabian StyleSheng, Tong, Qi Liu, Yumeng Kou, Guole Shang, and Miaomiao Xie. 2025. "Differential Impacts on Human Physiological Responses on Heatwave and Non-Heatwave Days: A Comparative Study Using Wearable Devices in Beijing" Atmosphere 16, no. 4: 413. https://doi.org/10.3390/atmos16040413
APA StyleSheng, T., Liu, Q., Kou, Y., Shang, G., & Xie, M. (2025). Differential Impacts on Human Physiological Responses on Heatwave and Non-Heatwave Days: A Comparative Study Using Wearable Devices in Beijing. Atmosphere, 16(4), 413. https://doi.org/10.3390/atmos16040413









