Abstract
This study aimed to compare the antibiotic resistance levels of the indicator bacteria Escherichia coli in wastewater samples collected from two hospitals and two urban communities. Antimicrobial susceptibility testing was performed on 81 E. coli isolates (47 from hospitals and 34 from communities) using the disc diffusion method according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) methodology. Ten antibiotics from nine different classes were chosen. The strains isolated from the community wastewater, compared to those from the hospital wastewater, were not resistant to gentamicin (p = 0.03), but they showed a significantly higher susceptibility—increased exposure to ceftazidime (p = 0.001). Multidrug resistance was observed in 85.11% of the hospital wastewater isolates and 73.53% of the community isolates (p > 0.05). The frequency of the presumed carbapenemase-producing E. coli was higher among the community isolates (76.47% compared to 68.09%) (p > 0.05), whereas the frequency of the presumed extended-spectrum beta-lactamase (ESBL)-producing E. coli was higher among the hospital isolates (21.28% compared to 5.88%) (p > 0.05). The antibiotic resistance rates were high in both the hospital and community wastewaters, with very few significant differences between them, so the community outlet might be a source of resistant bacteria that is at least as important as the well-recognised hospitals.
1. Introduction
As a result of many years of antibiotic use and abuse, the parent compounds and their functional metabolites, antimicrobial-resistant bacteria (ARB) as well as their resistance genes (ARG) are common and widespread contaminants in many environments [1,2,3,4]. Human and animal excreta and wastewater are recognised and documented as major sources of the previously mentioned compounds and bacteria [1]. Although treatment processes can reduce the concentrations of pathogens in wastewater, wastewater treatment plant effluents do not show appreciable removal of ARB and ARG in general [5,6], and large amounts of resistant bacteria, possibly of hospital origin, are released into the recipient waters [7]. Wastewater effluents are considered co-contributors to the extended-spectrum beta-lactamases-producing bacteria (ESBL) in recreational waters, so they can represent a possible exposure route for the population [8]. In many countries, facilities to treat municipal wastewater that may harbour large pathogens as Giardia duodenalis and Cryptosporidium spp. are absent or inadequate [9], so retaining or neutralising smaller molecules such as antibiotics, antibiotic-resistant bacteria and their resistance genes becomes even more difficult to achieve through the currently available treatments [1]. Another common problem for many countries, including Romania, which may lead to population exposure to resistant bacteria is aged infrastructure and the fact that leaking sewers are often co-located with municipal drinking water distribution pipes [1]. On the contrary, other authors claim that there is no evidence for selection for antibiotic resistance in wastewater treatment plants [10].
It has been suggested that the specific hotspots for antibiotic-resistant bacteria and resistance genes are the waste discharges and wastewaters from pharmaceutical production facilities, hospitals and other healthcare facilities [11]. People in hospitals are constantly and extensively treated with antibiotics, and their faecal and liquid wastes have been documented as important sources contributing to the release and subsequent spread of antibiotic residues, ARB and ARG in the environment [5,11,12]. Even though hospitals are under close examination, they provide relatively controlled environments for the usage of antibiotics, and resistance evolution is relatively easy to track (i.e., testing of hospital effluent) and subsequently curb. In contrast, antibiotic usage by the general populace is largely unsupervised [4].
The evolution of resistance in the human gut microbiome (and other microbiomes), via in-home usage of antibiotics, can be due to overuse, inappropriate use or incomplete treatment, resulting in sub-inhibitory antibiotic concentrations in situ [4]. Monitoring antimicrobial resistance (AMR) through national and international surveillance programs has increased knowledge of the dissemination of resistant bacteria. For example, in the veterinary field, the European Food Safety Authority (EFSA) runs such a surveillance program focused on monitoring antimicrobial resistance of commensal bacteria in faecal samples collected from healthy animals [13]. Because it is more difficult to obtain large numbers of faecal samples from healthy humans, less is known about the role of normal human microbiota as a reservoir of antimicrobial-resistant bacteria [13]. According to Kühn et al. [13] and Paulshus et al. [14] an alternative method of sampling hundreds of individuals in the population can be measuring levels of antibiotic resistance in commensal indicators, such as E. coli, from untreated wastewater samples [13,14]. This method can also be used as an early warning system for the emergence of new or rare antibiotic resistance patterns in the corresponding population, as proposed in the 1970s by Linton et al. [15] and confirmed recently by Paulshus et al. [13] as well as by others [16,17,18].
The resistance rates in the bacteria isolated from urban wastewater were found to correlate positively with the frequency of the antibiotic resistance in the corresponding human population [18]. Iversen et al. [19] found a possible transmission route for ampicillin- and ciprofloxacin-resistant Enterococcus faecicum from patients in hospital-to-hospital and urban sewage, further through wastewater treatment plants to surface water and possibly back to humans. Because the strain was found enriched in untreated and treated sewage, and also in many surface water samples, it can be assumed that hospital wastewater is not the only source for these clones, that the community could be involved as well and/or this strain can better survive the bacterial-reduction process in treatment plants than other enterococci strains [19]. Thus, it may be of great importance to identify wastewater outlets, other than hospitals, which can act as hotspots for antibiotic-resistant bacteria [20].
In the present study, we analysed the antimicrobial resistance patterns of the indicator bacterium Escherichia coli in wastewater samples collected from hospitals and urban communities connected to the sewage system of Timisoara, Romania. The aim of this study was to compare the antibiotic resistance levels of these two sites in order to improve the knowledge of the occurrence and spread of antibiotic-resistant bacteria in the resident population and to identify whether any of these two outlets may act as a hotspot for such bacteria.
2. Materials and Methods
Hospital wastewater was collected directly from the wastewater treatment system of two hospitals in Timisoara; more precisely, from the treated effluent stocked in a tank before being transported to the urban wastewater treatment plant. Community wastewater was collected from the sewer system, from two specific points selected based on the city’s sewer system map, in order to provide wastewater with no contributions from health care institutions (human or veterinary) and agricultural or zootechnical sources (Figure 1).
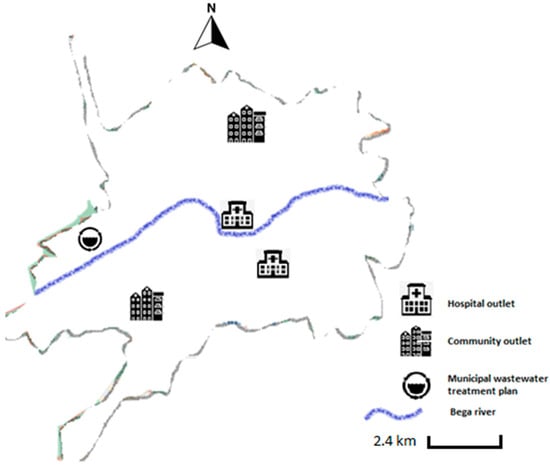
Figure 1.
Wastewater sampling sites and their approximate geographical locations in Timisoara city.
Wastewater was collected on the same days from all four locations, five times from October 2018 to March 2019, in sterile 750 mL glass vials. Samples were kept at +4 °C and analysed within 4 h. From each sample, aliquots of 100 µL were plated on 90 mm Petri dishes containing Tryptone Bile X-glucuronide chromogenic agar for E. coli (Chromocult® TBX agar, Merck KGaA, Darmstadt, Germany) (3 plates for each sample). The plates were incubated for an initial period of 4 h at 37 °C (to reduce potential cellular stress) and then, for the next 20 h, at 44 ± 1 °C. Blue or blue-to-green (turquoise) colonies were regarded as E. coli. Three to five colonies corresponding to each sample were picked from the TBX agar with sterile plastic loops and recultured for proper storage in order to be further analysed. A total of 81 E. coli strains (47 from hospitals and 34 from communities) were subjected to antimicrobial susceptibility testing using the disc diffusion method, according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) methodology [21]. Ten antibiotics from nine different classes were chosen based on the EUCAST recommendations [22] and the World Health Organization list of Critically Important Antimicrobials for Human Medicine—WHO CIA list [23]:
- Highest-priority critically important antimicrobials: cefotaxime (CTX 30 µg), ceftazidime (CAZ 30 µg), ciprofloxacine (CIP 5 µg);
- High-priority critically important antimicrobials: ampicillin (AMP 10 µg), meropenem (MRP 10 µg), aztreonam (AT 30 µg), fosfomycine (FO 200 µg), gentamicine (GEN 10 µg);
- Highly important antimicrobials: sulfamethoxazole-trimethoprim (SXT 25 µg);
- Important antimicrobials: nitrofurantoine (NIT 100 µg) (Liofilchem®, Roseto degli Abruzzi, Teramo, Italy).
- The diameter of the inhibition zone was interpreted according to the latest EUCAST recommendations [22,24,25]. The strains were classified as:
- Susceptible, standard dosing regimen (S)—refers to microorganisms against which there is a high probability of therapeutic success when the antimicrobial agent is used in standard (usual) doses;
- Susceptible, increased exposure (the old intermediate “I” category)—refers to microorganisms against which there is a high probability of therapeutic success when exposure to the agent is increased by adjusting the dosing regimen or by its concentration at the site of infection;
- Resistant (R)—refers to microorganisms against which there is a high probability of therapeutic failure even when there is increased exposure [25].
Isolates showing resistance to both CTX and CAZ were regarded as the presumed extended-spectrum beta-lactamases (ESBL) producers [13,26,27]. Those exhibiting an inhibition zone diameter to MRP smaller than 28 mm were regarded as presumed carbapenemases producers [26], and the isolates showing resistance to at least three antibiotics from three different classes were regarded as multidrug-resistant [28].
Comparisons between the prevalence of antibiotic-resistant E. coli in hospitals and community wastewater were performed using the Chi-square test with Yates correction at a level of significance set at p < 0.05. Where the requirements for Chi-square testing were unmet, Fischer’s exact test was performed with a two-side p value of >0.05, which is considered to be significant.
3. Results
3.1. Antibiotic Susceptibility of E. coli Isolates from Hospital Wastewater and Community Wastewater
All 81 E. coli isolates were tested for their susceptibility using a panel of ten antibiotics (from nine different classes). The most commonly found antibiotics to which the isolates were resistant (over 50%) were: ampicillin (58/81; 72%), fosfomycin (51/81; 63%), ceftazidime (47/81; 58%) and sulfamethoxazole/trimethoprim (44/81; 54%). Less than 50% of the strains showed resistance to: aztreonam (35/81; 43%), ciprofloxacin (29/81; 36%), nitrofurantoin (26/81; 32%), cefotaxime (23/81; (28%), gentamicin (6/81; 7%) and meropenem (3/81; 4%) (Figure 2).
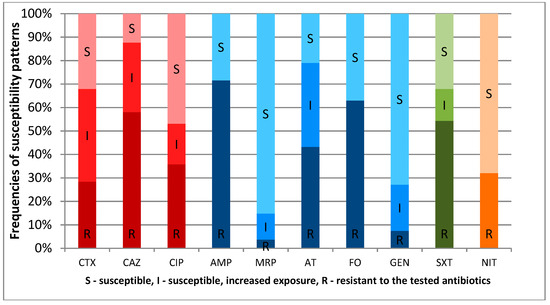
Figure 2.
Susceptibility pattern of E. coli strains to critically important antimicrobials—highest priority (RED) and high priority (BLUE) and highly important (GREEN) and important (ORANGE) antimicrobials for human medicine.
The highest frequency of susceptibility at increased exposure (old intermediate category I), was found for cefotaxime (32/81; 39.5%), followed by aztreonam (29/81; 36%), ceftazidime (24/81; 30%), gentamicin (16/81; 20%), ciprofloxacin (14/81; 17%), sulfamethoxazole/trimethoprim (11/81; 14%) and meropenem (9/81; 11%) (Figure 2).
Resistance was more common among the isolates from the hospital wastewater for the following six out of ten antibiotics: MRP, CTX, CAZ, AT, GEN, SXT with a significant difference only in the case of gentamicin (p = 0.03). The strains isolated from the community wastewater showed a higher resistance rate to AMP, CIP, FO and NIT without any significant difference (p > 0.05) (Table 1).

Table 1.
Antibiotic resistance patterns for E. coli isolates from hospital wastewater (HW) and community wastewater (CW).
Susceptibility at increased exposure was more common among the isolates from the hospital wastewater only for the following three antibiotics: MRP, CIP and GEN without any significant difference. The isolates from the community wastewater showed a higher susceptibility at increased exposure to CTX, CAZ, AT and SXT with significant differences in the case of ceftazidime (p = 0.001) (Table 1).
3.2. The Proportion of Multidrug-Resistant E. coli Recovered from Hospital Wastewater and Community Wastewater
The isolates showing resistance to at least three antibiotics belonging to three different classes were regarded as multidrug-resistant (MDR) [27]. It was found that the proportion of MDR E. coli recovered from HW (85.11%), even if higher, was not statistically significant compared to those recovered from CW (73.53%) Χ2 (1, N = 81) = 1.75; p > 0.05 (Figure 3).
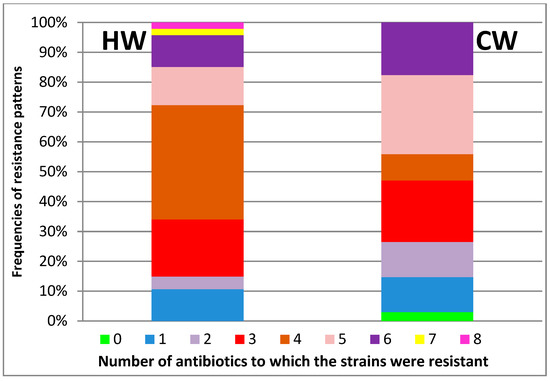
Figure 3.
The proportion of multidrug-resistant E. coli (resistance to at least three antibiotics from three different classes—starting from no. 3) in hospital wastewater (HW) and community wastewater (CW).
The isolates resistant to three, five and six antibiotics were more frequently identified in the CW: 21% compared with 19% (HW), 26% compared with 13% and 18% compared with 11% (p > 0.05). The isolates resistant to four antibiotics were significantly more common in HW: 38% compared with 9%, Χ2 (1, N = 81) = 8.92; p < 0.05. The only two isolates resistant to seven (2%) and eight (2%) antibiotics were also isolated from the HW. The single isolate susceptible to all antibiotics was identified in the community wastewater (Figure 3).
3.3. Presumed ESBL- and Carbapenemase-Producing E. coli Recovered from HW and CW
The frequency of presumed carbapenemase-producing E. coli (IZD < 28 mm for meropenem) was higher among the CW isolates (76.47%) than the HW isolates (68.09%) (p > 0.05). In contrast, two isolates from the hospital outlet (4.26%) were clearly resistant to meropenem (IZD < 16 mm) and to one of the third-generation cephalosporins compared to one isolate from the community outlet (2.94%) (p > 0.05) (Table 1). The proportion of the isolates resistant to one of the cephalosporins was slightly higher in the community outlet (55.88% compared with 53.19%), and the prevalence of those resistant to both cephalosporins (the presumed ESBL-producing E. coli) was higher in the hospital outlets (21.28% compared with 5.88%). In both situations, the differences were statistically nonsignificant (p > 0.05) (Table 1).
4. Discussion
We compared E. coli in wastewater from hospital and non-hospital outlets with regard to their prevalence of antibiotic resistance. To our knowledge, no previous studies have investigated ARB in wastewaters in Romania, the country with the second-highest consumption of antibacterials for systemic use in Europe [29].
In our study, we found the following prevalences of resistance to critically important antimicrobials for human medicine: highest priority—CAZ (58%), CIP (36%) and high priority—AMP (72%), FO (63%). According to WHO, antibiotics within the critically important category (highest and priority antimicrobials) should be included in antibiotic resistance monitoring programs [23]. Currently, this category includes quinolones; third-, fourth- and fifth-generation cephalosporins; macrolides and ketolides; polymyxins; and glycopeptides. On the one hand, these drugs must be used with caution and great discernment, as the loss of their effectiveness due to the emergence of resistance would result in the lack of therapeutic options and, thus, in the impossibility of treating life-threatening infections in humans [23]. On the other hand, these medicines are also used to treat diseases caused by bacteria other than those of human origin, and, often, these infections can be difficult to manage because of the improper use of antibiotics in veterinary medicine and other fields [23]. Additionally, commensal microorganisms from non-human sources (animals, water, food or the environment), as well as transmitting antimicrobial resistance genes to pathogenic bacteria of human origin, can themselves become pathogenic for immunosuppressed hosts [23].
The increased resistance to ampicillin (72%) can be attributed to the fact that it is among the most frequently used drugs in the EU for the treatment of respiratory, abdominal, soft tissue and urinary tract infections [30]. Currently, in Romania, beta-lactams (potentiated or not) are the favourite “weapon” of both doctors and veterinarians, conduct that inevitably leads to an increase in the resistant bacteria population and an increased amount of drug residues in wastewater. It is known that antibiotic residues present in wastewater can cause resistance in susceptible bacterial populations [31]. Moreover, selective pressure caused by the presence of antibiotics can lead to the occurrence of antibiotic resistance mainly in the form of cross-resistance [13]. In the case of the extended beta-lactam antibiotics class, the presence of cross-resistance between amoxicillin and third-generation cephalosporins is an undeniable fact [32]. The occurrence of cross-resistance can explain the increased resistance to ceftazidime (58%) and the increased intermediate behaviour towards cefotaxime (39.5%) revealed by the present study.
The second-highest frequency of resistance was to fosfomycin (63%). At the time of the research, this antibiotic was placed in the Reserve group. Its use should be limited to urinary tract infections with ESBL-producing E. coli strains. Resistance to aztreonam, which has the same indications as fosfomycin, was lower (43%), but it is still considered high given that it replaced fosfomycin in the WHO Model List of Essential Medicines in 2017 [23,33].
Only 3 out of 81 strains (4%) exhibited clear resistance to meropenem (IZD < 16 mm). The low resistance rate to meropenem could be due to the fact that it is included in the Watch group: it remains an antibiotic reserved for in-hospital patients, is given mainly parenterally and is not used in any situation as the first therapeutic option but only as a second option (for serious conditions such as acute bacterial meningitis in newborns, complicated and severe abdominal infections as well as high-risk febrile neutropenia) [33].
Although sulfonamides or therapeutic combinations containing sulfonamides have been used less and less in the treatment of bacterial infections in recent years in human medicine, we found a high-resistance frequency to SXT (54%).
Regarding nitrofurantoin, which is also no longer commonly used, there is, however, a low resistance rate (32%). It is included in the Access group and should be one of the first therapeutic options in the treatment of uncomplicated urinary tract infections in women, including those caused by ESBL-producing Enterobacteriaceae [30,33]. The reluctance to prescribe nitrofurantoin is probably due to the associated risks [30,34]. It is known that, in animal populations, decreased exposure to a particular antibiotic may reduce the incidence of resistance [35], as was probably the case with nitrofurantoin, and also that the phenomenon may be irreversible [30], which would explain the evolution of resistance to sulfamethoxazole/trimethoprim.
The frequency of antibiotic resistance in E. coli isolates from the HW compared with the CW in the present study is somehow predictable, given that ampicillin and ciprofloxacin are among the most often prescribed antibiotics in ambulatory care. In contrast, meropenem, gentamicin and third-generation cephalosporins are reserved for in-hospital treatment of serious infections. Gentamicin is used as a monotherapy or in various combinations in the treatment of severe infections with not only Gram-negative bacteria in general, but also Gram-positive (e.g., endocarditis caused by S. aureus). Further, perhaps the most important aspect, which mainly explains the second-lowest resistance rate (after meropenem) in all strains (7%), is that it is only available for parenteral administration (except for eye drops), which makes it less attractive for both the doctor and patient [30,33].
The results obtained by this study, according to which there are no significant differences between the antibiotic resistance rates of the bacteria isolated from the HW and those isolated from the CW, are reinforced by the findings of other studies. In their study conducted in Oslo, Norway, Paulshus et al. [13] concluded that the levels of antibiotic-resistant E. coli in the hospital wastewater relative to the community and urban wastewater (entering the urban treatment plant), even if they were higher, were insufficient to recommend the implementation of local treatment measures. They also agreed that the majority of the antibiotic-resistant bacteria in the influent entering the urban wastewater treatment plant were likely derived from the presence of such bacteria in the total population of the urban society, as the relative contribution of the hospital wastewater was low [13].
If testing for susceptibility to meropenem and an inhibition zone diameter of less than 28 mm is obtained, the EUCAST recommends that the strain should be subjected to additional testing procedures in order to detect carbapenemase production [26]. The presumed carbapenemase production is strengthened by the concomitant resistance to meropenem and a third-generation cephalosporin. Moreover, resistance and/or susceptibility at increased exposure (intermediate) to cefotaxime and/or ceftazidime is a phenotypic criterion for further investigations in order to detect ESBLs and acquired AmpC beta-lactamases in bacteria belonging to the Enterobacteriaceae family. However, the same authority points out that screening for these resistance mechanisms is important for infection control and public health, but that the phenotypical expression of these enzymes is not always associated with clinical resistance, especially in Gram-negative bacteria producing ESBL and carbapenemases [26].
The epidemiological importance of the detection of carbapenemase secretion lies in the following: these enzymes can generate resistance to practically all beta-lactams; resistance is easily transferable between bacterial strains; infections with such bacteria belonging to the Enterobacteriaceae group result in high mortality rates [36], especially when low susceptibility to carbapenems occurs [26]. The lack of response to carbapenems may be due not only to carbapenemase production but also to the presence of ESBLs or AmpCs in combination with decreased permeability due to porin loss [37]. Same as carbapenemases, ESBLs hydrolyse most penicillin and cephalosporins, including oxyimino compounds (cefuroxime, third- and fourth-generation cephalosporins as well as aztreonam) but do not hydrolyse cephamycins (cefoxitin) and carbapenems and are inhibited by classical inhibitors (clavulanic acid, sulbactam and tazobactam) and diazabicyclooctanone (avibactam) [38]. Except for the strains isolated from patients with various infections, ESBL production was also detected in bacterial strains isolated from healthy carriers, sick and healthy animals as well as food of animal origin throughout the entire European community, suggesting that both horizontal gene transfer resistance, through plasmids, in addition to chromosomal transmission of resistance, is achieved at a fast pace among bacterial populations [26].
In a similar study conducted by Paulshus et al. [13], the isolates showing resistance to cefotaxime and cefpodoxime were regarded as ESBL-producing E. coli (ESBL-EC). The prevalence of ESBL-EC was 11.5% for the hospital wastewater and 6.9% for the community wastewater [13]. In another study in Stockholm, 14.9% of the hospital wastewater isolates were suspected ESBL-EC and resistant to at least one of the antibiotics cefotaxime or ceftazidime. Moreover, 14% were resistant to cefotaxime, ceftazidime and cefpodoxime. After the confirmation of ESBL production using an AREB (antibiotic resistance in environmental bacteria) test for 75 of the isolates (hospital and urban wastewater) that were resistant to all three cephalosporins, 73 (97%) of these were confirmed to harbour an ESBL gene (including qAmpC) [27]. In another study conducted in Spain on wastewater samples of human and animal origin, E. coli from chicken wastewater showed the highest percentage of ESBL producers (21%), followed by 4% in humans and 0% in cow and pig wastewater [39]. The prevalence of ESBL-producing E. coli isolated from the hospital wastewater in our study (21.28%) was lower compared to a situation in Poland where ESBL-EC constituted 37% of the examined hospital wastewater isolates [12].
Thus, to answer whether hospital effluents should be additionally treated, it is essential to define the risks associated with MDR bacteria in the wastewater outlets specific to each country. Additionally, the present study presents limitations, such as the low sample size and the small number of isolates, which may interfere with the statistical results. The lack of the molecular characterisation of the isolates is also an issue when it comes to demonstrating that a certain antibiotic resistance phenotype is not due to the spread of specific clones among the E. coli population isolated from our samples.
Despite these limitations, the finding that the community outlets might be a source of resistant bacteria at least as important as the well-recognised hospital outlets raises new questions about how the phenomenon of antibiotic resistance escalates within the population. Measuring levels of antibiotic resistance in faecal bacteria from wastewater can be used as an early warning system for changes in the human or animal population’s resistance patterns.
5. Conclusions
Even if the resistance rate (for six out of ten antibiotics tested), the frequency of multidrug-resistant bacteria and the prevalence of ESBL producing E. coli were higher overall among the hospital wastewater isolates compared to the community isolates, the differences were statistically insignificant.
Thus, the community outlet might be a source of resistant bacteria at least as important as the well-recognised hospitals.
Author Contributions
Conceptualization, C.-M.G. and I.Ţ.; data curation, M.B.; formal analysis, C.F.L.; investigation, C.-M.G.; methodology, C.-M.G.; resources, M.B.; supervision, M.B.; validation, L.T.C., C.F.L. and M.P.; visualization, I.Ţ.; writing—original draft, C.-M.G., L.T.C., C.F.L., I.Ţ., M.P. and M.B.; writing—review and editing, I.Ţ. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sobsey, M.; Abebe, L.; Andremont, A.; Ashbolt, N.; de Roda Husman, A.M.; Gin, K.; Hunter, P.; Meschke, J.; Vilchez, S. Briefing note—Antimicrobial Resistance: An Emerging Water, Sanitation and Hygiene Issue; WHO: Geneva, Switzerland, 2014. [Google Scholar] [CrossRef]
- Kümmerer, K. Antibiotics in the aquatic environment—A review—Part I. Chemosphere 2009, 75, 417–434. [Google Scholar] [CrossRef] [PubMed]
- Kolár, M.; Urbánek, K.; Látal, T. Antibiotic selective pressure and development of bacterial resistance. Int. J. Antimicrob. Agents 2001, 17, 357–363. [Google Scholar] [CrossRef]
- Kraemer, S.A.; Ramachandran, A.; Perron, G.G. Antibiotic Pollution in the Environment: From Microbial Ecology to Public Policy. Microorganisms 2019, 7, 180. [Google Scholar] [CrossRef] [PubMed]
- Leclercq, R.; Oberle, K.; Galopin, S.; Cattoir, V.; Budzinski, H.; Petit, F. Changes in enterococcal populations and related antibiotic resistance along a medical center–wastewater treatment plant–river continuum. Appl. Environ. Microbiol. 2013, 79, 2428–2434. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Okoh, A.I.; Igbinosa, E.O. Antibiotic susceptibility profiles of some Vibrio strains isolated from wastewater final effluents in a rural community of the Eastern Cape Province of South Africa. BMC Microbiol. 2010, 10, 143. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, L.; Manaia, C.; Merlin, C.; Schwartz, T.; Dagot, C.; Ploy, M.C.; Michael, I.; Fatta-Kassinos, D. Urban wastewater treatment plants as hotspots for antibiotic resistant bacteria and genes spread into the environment: A review. Sci. Total Environ. 2013, 447, 345–360. [Google Scholar] [CrossRef]
- Blaak, H.; van Hoek, A.H.; Veenman, C.; van Leeuwen, A.E.D.; Lynch, G.; van Overbeek, W.M.; de Roda Husman, A.M. Extended spectrum β-lactamase- and constitutively AmpC-producing Enterobacteriaceae on fresh produce and in the agricultural environment. Int. J. Food Microbiol. 2014, 168–169, 8–16. [Google Scholar] [CrossRef]
- Imre, K.; Morar, A.; Ilie, M.S.; Plutzer, J.; Imre, M.; Tîrziu, E.; Herbei, M.V.; Dărăbuș, G. Survey of the Occurrence and Human Infective Potential of Giardia duodenalis and Cryptosporidium spp. in Wastewater and Different Surface Water Sources of Western Romania. Vector Borne Zoonotic Dis. 2017, 17, 685–691. [Google Scholar] [CrossRef]
- Flach, C.F.; Genheden, M.; Fick, J.; Larsson, J.D.G. A comprehensive screening of Escherichia coli isolates from Scandinavia’s largest sewage treatment plant indicates no selection for antibiotic resistance. Environ. Sci. Technol. 2018, 52, 11419–11428. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Qiu, S.; Wang, Y.; Qi, L.; Hao, R.; Liu, X.; Shi, Y.; Hu, X.; An, D.; Li, Z.; et al. Higher isolation of NDM-1 producing Acinetobacter baumannii from the sewage of the hospitals in Beijing. PLoS ONE 2013, 8, e64857. [Google Scholar] [CrossRef]
- Korzeniewska, E.; Korzeniewska, A.; Harnisz, M. Antibiotic resistant Escherichia coli in hospital and municipal sewage and their emission to the environment. Ecotoxicol. Environ. Saf. 2013, 91, 96–102. [Google Scholar] [CrossRef]
- Paulshus, E.; Kühn, I.; Möllby, R.; Colque, P.; O’Sullivan, K.; Midtvedt, T.; Lingaas, E.; Holmstad, R.; Sørum, H. Diversity and antibiotic resistance among Escherichia coli populations in hospital and community wastewater compared to wastewater at the receiving urban treatment plant. Water Res. 2019, 161, 232–241. [Google Scholar] [CrossRef]
- Kühn, I.; Iversen, A.; Burman, L.G.; Olsson-Liljequist, B.; Franklin, A.; Finn, M.; Aarestrup, F.; Seyfarth, A.M.; Blanch, A.R.; Vilanova, X.; et al. Comparison of enterococcal populations in animals, humans, and the environment—A European study. Int. J. Food Microbiol. 2003, 88, 133–145. [Google Scholar] [CrossRef]
- Linton, K.B.; Richmond, M.H.; Bevan, R.; Gillespie, W.A. Antibiotic resistance and R factors in coliform bacilli isolated from hospital and domestic sewage. J. Med. Microbiol. 1974, 7, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Kümmerer, K.; Henninger, A. Promoting resistance by the emission of antibiotics from hospitals and households into effluent. Clin. Microbiol. Infect. 2003, 9, 1203–1214. [Google Scholar] [CrossRef] [PubMed]
- Munir, M.; Wong, K.; Xagoraraki, I. Release of antibiotic resistant bacteria and genes in the effluent and biosolids of five wastewater utilities in Michigan. Water Res. 2011, 45, 681–693. [Google Scholar] [CrossRef] [PubMed]
- Reinthaler, F.F.; Galler, H.; Feierl, G.; Haas, D.; Leitner, E.; Mascher, F.; Melkes, A.; Posch, J.; Pertschy, B.; Winter, I.; et al. Resistance patterns of Escherichia coli isolated from sewage sludge in comparison with those isolated from human patients in 2000 and 2009. J. Water Health 2013, 11, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Iversen, A.; Kühn, I.; Rahman, M.; Franklin, A.; Burman, L.G.; Olsson-Liljequist, B.; Torell, E.; Mollby, R. Evidence for transmission between humans and the environment of a nosocomial strain of Enterococcus faecium. Environ. Microbiol. 2004, 6, 55–59. [Google Scholar] [CrossRef]
- Berendonk, T.U.; Manaia, C.M.; Merlin, C.; Fatta-Kassinos, D.; Cytryn, E.; Walsh, F.; Bürgmann, H.; Sørum, H.; Norstrom, M.; Pons, M.N.; et al. Tackling antibiotic resistance: The environmental framework. Nat. Rev. Microbiol. 2015, 13, 310–317. [Google Scholar] [CrossRef] [PubMed]
- The European Committee on Antimicrobial Susceptibility Testing. Antimicrobial Susceptibility Testing–EUCAST Disk Diffusion Method. Version 7.0. 2019. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Disk_test_documents/2019_manuals/Manual_v_7.0_EUCAST_Disk_Test_2019.pdf (accessed on 2 May 2019).
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 9.0. 2019. Available online: https://eucast.org/clinical_breakpoints/ (accessed on 2 May 2019).
- World Health Organization. Critically Important Antimicrobials for Human Medicine, 6th ed.; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- The European Committee on Antimicrobial Susceptibility Testing. Reading Guide–EUCAST Disk Diffusion Method for Antimicrobial Susceptibility Testing. Version 6.0. 2019. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Disk_test_documents/2017_manuals/Manual_v_6.0_EUCAST_Disk_Test_final.pdf (accessed on 2 May 2019).
- The European Committee on Antimicrobial Susceptibility Testing. Redefining Susceptibility Testing Categories S, I and R. 2019. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/EUCAST_Presentations/2018/EUCAST_-_Intermediate_category_-_information_for_all.pdf (accessed on 2 May 2019).
- The European Committee on Antimicrobial Susceptibility Testing. EUCAST Guidelines for Detection of Resistance Mechanism and Specific Resistance of Clinical and/or Epidemiological Importance. Version 2.0. 2017. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Resistance_mechanisms/EUCAST_detection_of_resistance_mechanisms_170711.pdf (accessed on 2 May 2019).
- Kwak, Y.K.; Colque, P.; Byfors, S.; Giske, C.G.; Mollby, R.; Kühn, I. Surveillance antimicrobial resistance among Escherichia coli in wastewater in Stockholm during 1 year: Does it reflect the resistance trends in the society? Int. J. Antimicrob. Agents 2015, 45, 25–32. [Google Scholar] [CrossRef]
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. ECDC Country Visit to Romania to Discuss Antimicrobial Resistance Issues; ECDC: Stockholm, Sweden, 2018. [Google Scholar]
- The European Medicines Agency. Answer to the Request from the European Commission for Updating the Scientific Advice on the Impact on Public Health and Animal Health of the Use of Antibiotics in Animals-Categorisation of Antimicrobials (Draft) EMA/CVMP/CHMP. 2019. Available online: https://www.ema.europa.eu/en/documents/other/answer-request-european-commission-updating-scientific-advice-impact-public-health-animal-health-use_en.pdf (accessed on 1 October 2019).
- Garcia, S.; Wade, B.; Bauer, C.; Craig, C.; Nakaoka, K.; Lorowitz, W. The effect of wastewater treatment on antibiotic resistance in Escherichia coli and Enterococcus sp. Water Environ. Res. 2007, 79, 2387–2395. [Google Scholar] [CrossRef] [PubMed]
- Persoons, D.; Dewulf, J.; Smet, A.; Herman, L.; Heyndrickx, M.; Martel, A.; Catry, B.; Butaye, P.; Haesebrouck, F. Antimicrobial use in Belgian broiler production. Prev. Vet. Med. 2012, 105, 320–325. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Model List of Essential Medicines, 21st ed.; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- The European Medicines Agency. Concluzii Științifice și Motive Pentru Modificarea Condițiilor Autorizației/Autorizațiilor de Punere pe Piață-Nitrofurantoină, Nifurtoinol. 2018. Available online: https://www.ema.europa.eu/en/documents/psusa/nitrofurantoin-nifurtoinol-cmdh-scientificconclusions-grounds-variation-amendments-product/00002174/201802_ro.pdf (accessed on 1 October 2019).
- Hanon, J.-B.; Jaspers, S.; Butaye, P.; Wattiau, P.; Méroc, E.; Aerts, M.; Imberechts, H.; Vermeersch, K.; Van der Stede, Y. A trend analysis of antimicrobial resistance in commensal Escherichia coli from several livestock species in Belgium (2011–2014). Prev. Vet. Med. 2015, 122, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Souli, M.; Galani, I.; Antoniadou, A.; Papadomichelakis, E.; Poulakou, G.; Panagea, T.; Vourli, S.; Zerva, L.; Armaganidis, A.; Kanellakopoulou, K.; et al. An outbreak of infection due to β-lactamase Klebsiella pneumoniae carbapenemase 2-producing K. pneumoniae in a Greek University Hospital: Molecular characterization, epidemiology, and outcomes. Clin. Infect. Dis. 2010, 50, 364–373. [Google Scholar] [CrossRef] [PubMed]
- Doumith, M.; Ellington, M.J.; Livermore, D.M.; Woodford, N. Molecular mechanisms disrupting porin expression in ertapenem-resistant Klebsiella and Enterobacter spp. clinical isolates from the UK. J. Antimicrob. Chemother. 2009, 63, 659–667. [Google Scholar] [CrossRef]
- Bush, K.; Jacoby, G.A.; Medeiros, A.A. A functional classification scheme for β -lactamases and its correlation with molecular structure. Antimicrob. Agents Chemother. 1995, 39, 211–1233. [Google Scholar] [CrossRef]
- Sabaté, M.; Prats, G.; Moreno, E.; Ballesté, E.; Blanch, A.R.; Andreu, A. Virulence and antimicrobial resistance profiles among Escherichia coli strains isolated from human and animal wastewater. Res. Microbiol. 2008, 159, 288–293. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).