A Review on SARS-CoV-2 Genome in the Aquatic Environment of Africa: Prevalence, Persistence and the Future Prospects
Abstract
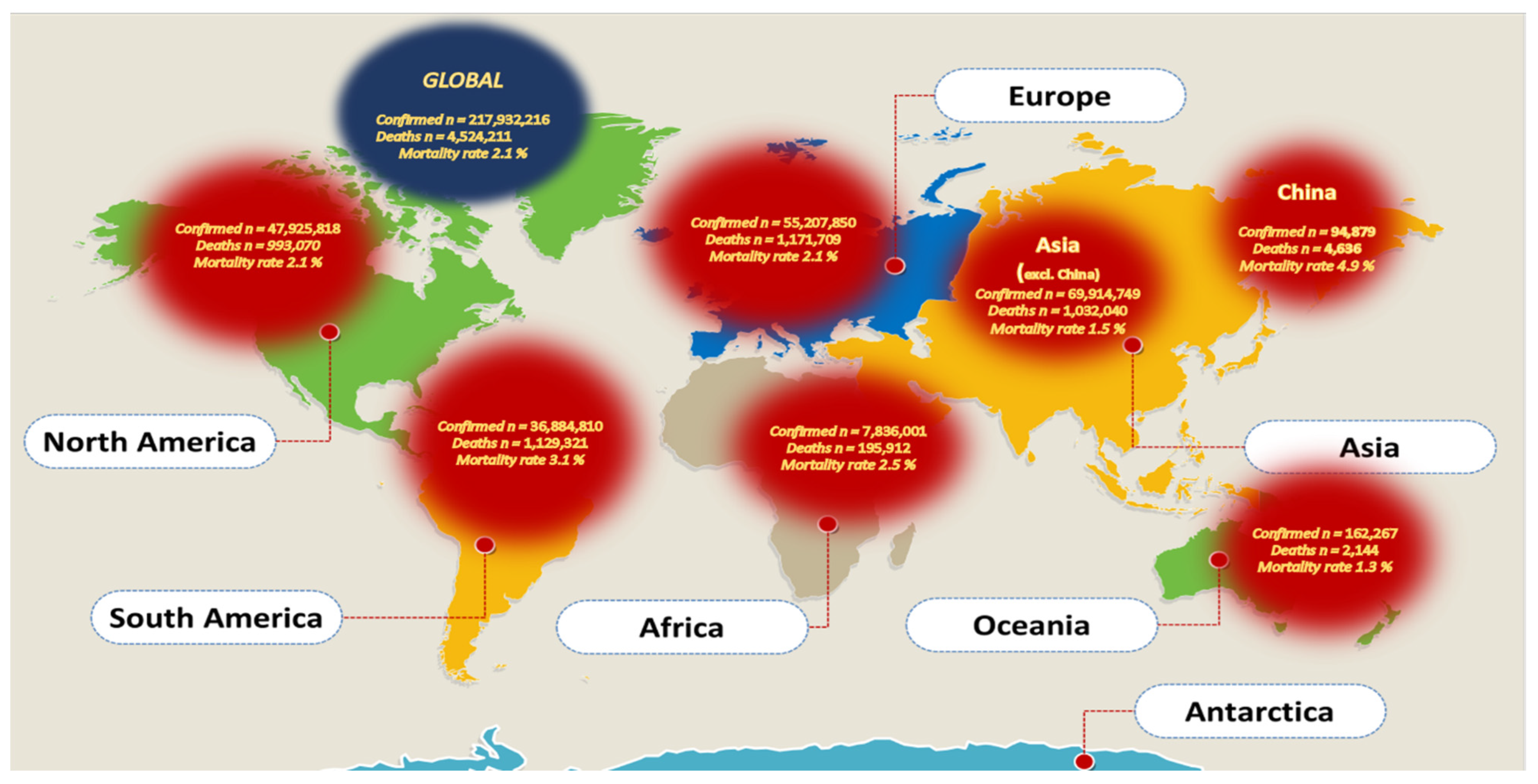
:1. Introduction
2. Monitoring COVID-19 Using Wastewater-Based Epidemiology (WBE)
Increased Waste Production
3. Reduction in Waste Management
4. Ecological Impacts of COVID-19
4.1. Other Indirect Effects of SARS-CoV-2 Genome on the Ecosystem
4.2. Sewer Networks as Red Flags in the Proliferation of SARS-CoV-2
5. Analysis of SARS-CoV-2 Genome in Environmental Niches
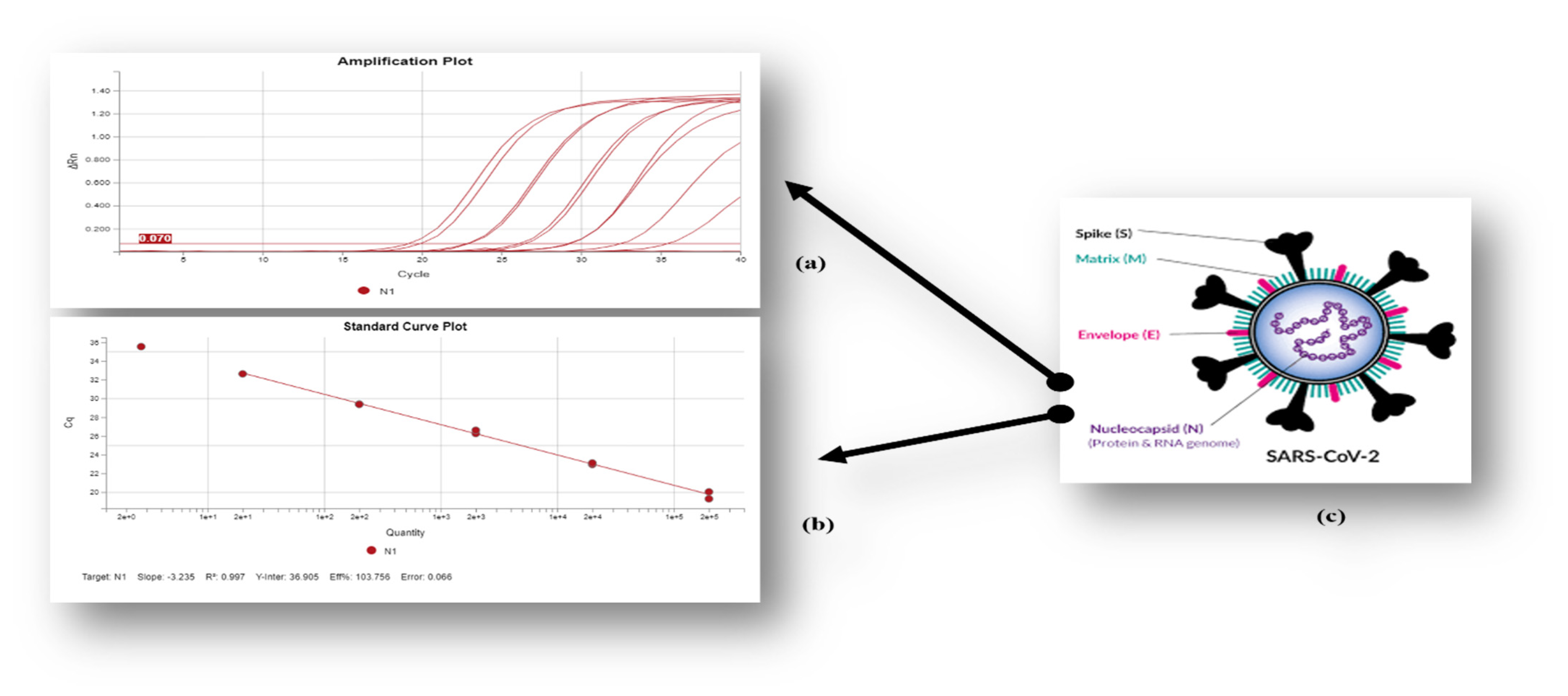
Nucleocapsid (N) Gene, Standard Curve and Ct Value as an Indicator of the Viral Load
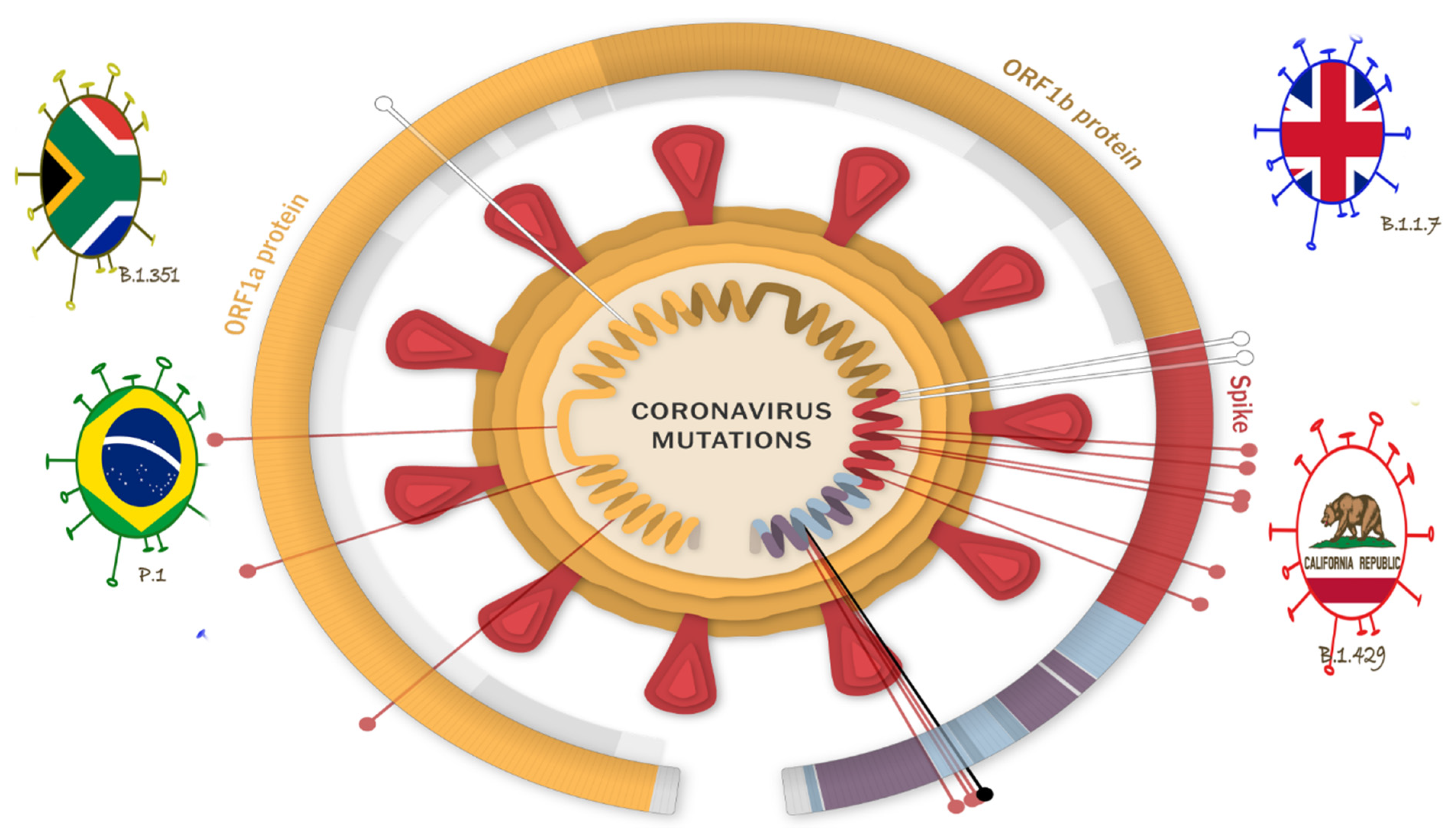
6. Emerging Variants and the Impending COVID Waves
7. Progress on the Development of Therapeutics for COVID-19
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Elliott, R.M. Emerging viruses: The Bunyaviridae. Mol. Med. 1997, 3, 572–577. [Google Scholar] [CrossRef]
- Genersch, E.; Aubert, M. Emerging and re-emerging viruses of the honey bee (Apis mellifera L.). Vet. Res. 2010, 41, 54. [Google Scholar] [CrossRef] [Green Version]
- Siegel, D.; Hui, H.C.; Doerffler, E.; Clarke, M.O.; Chun, K.; Zhang, L.; Neville, S.; Carra, E.; Lew, W.; Ross, B.; et al. Discovery and synthesis of a phosphoramidate prodrug of a pyrrolo [2, 1-f][triazin-4-amino] adenine C-nucleoside (GS-5734) for the treatment of Ebola and emerging viruses. J. Med. Chem. 2017, 60, 1648–1661. [Google Scholar] [CrossRef] [Green Version]
- Katze, M.G.; Fornek, J.L.; Palermo, R.E.; Walters, K.A.; Korth, M.J. Innate immune modulation by RNA viruses: Emerging insights from functional genomics. Nat. Rev. Immunol. 2008, 8, 644–654. [Google Scholar] [CrossRef]
- Mandl, J.N.; Ahmed, R.; Barreiro, L.B.; Daszak, P.; Epstein, J.H.; Virgin, H.W.; Feinberg, M.B. Reservoir host immune responses to emerging zoonotic viruses. Cell 2015, 160, 20–35. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.L.; Wang, Y.Q.; Liao, C.H.; Kuang, Y.Q.; Zheng, Y.T.; Su, B. Adaptive evolution of primate TRIM5α, a gene restricting HIV-1 infection. Gene 2005, 362, 109–116. [Google Scholar] [CrossRef]
- Xu, J.; Zhao, S.; Teng, T.; Abdalla, A.E.; Zhu, W.; Xie, L.; Wang, Y.; Guo, X. Systematic comparison of two animal-to-human transmitted human coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses 2020, 12, 244. [Google Scholar] [CrossRef] [Green Version]
- Pal, M.; Berhanu, G.; Desalegn, C.; Kandi, V. Severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2): An update. Cureus 2020, 12, e7423. [Google Scholar] [CrossRef] [Green Version]
- Audi, A.; AlIbrahim, M.; Kaddoura, M.; Hijazi, G.; Yassine, H.M.; Zaraket, H. Seasonality of Respiratory Viral Infections: Will COVID-19 Follow Suit? Front. Public Health 2020, 8, 576. [Google Scholar] [CrossRef]
- Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020, 5, 536–544. [Google Scholar] [CrossRef] [Green Version]
- Bchetnia, M.; Girard, C.; Duchaine, C.; Laprise, C. The outbreak of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): A review of the current global status. J. Infect. Public Health 2020, 13, 1601–1610. [Google Scholar] [CrossRef]
- Petrosillo, N.; Viceconte, G.; Ergonul, O.; Ippolito, G.; Petersen, E. COVID-19, SARS and MERS: Are they closely related? Clin. Microbiol. Infect. 2020, 26, 729–734. [Google Scholar] [CrossRef]
- Song, Y.; Liu, P.; Shi, X.L.; Chu, Y.L.; Zhang, J.; Xia, J.; Gao, X.Z.; Qu, T.; Wang, M.Y. SARS-CoV-2 induced diarrhoea as onset symptom in patient with COVID-19. Gut 2020, 69, 1143–1144. [Google Scholar] [CrossRef] [Green Version]
- Park, S.E. Epidemiology, virology, and clinical features of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clin. Exp. Pediatrics 2020, 63, 119. [Google Scholar] [CrossRef] [Green Version]
- Giannis, D.; Ziogas, I.A.; Gianni, P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J. Clin. Virol. 2020, 127, 104362. [Google Scholar] [CrossRef]
- Xu, X.W.; Wu, X.X.; Jiang, X.G.; Xu, K.J.; Ying, L.J.; Ma, C.L.; Xu, X.W.; Wu, X.X.; Jiang, X.G.; Xu, K.J.; et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: Retrospective case series. BMJ 2020, 368, m606. [Google Scholar] [CrossRef] [Green Version]
- Peeri, N.C.; Shrestha, N.; Rahman, M.S.; Zaki, R.; Tan, Z.; Bibi, S.; Baghbanzadeh, M.; Aghamohammadi, N.; Zhang, W.; Haque, U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? Int. J. Epidemiol. 2020, 49, 717–726. [Google Scholar] [CrossRef] [Green Version]
- Abduljali, J.M.; Abduljali, B.M. Epidemiology, genome and clinical features of the pandemic SARS-CoV-2: A recent view. New Microbes New Infect. 2020, 35, 100672. [Google Scholar] [CrossRef]
- Alwaqfi, N.R.; Ibrahim, K.S. COVID-19: An update and cardiac involvement. J. Cardiothorac. Surg. 2020, 15, 239. [Google Scholar] [CrossRef]
- McKibbin, W.J. Fernando, R. The global macroeconomic impacts of COVID-19: Seven scenarios. Asian Econ. Pap. 2021, 20, 1–30. [Google Scholar] [CrossRef]
- Velavan, T.P.; Meyer, C.G. The COVID-19 epidemic. Trop. Med. Int. Health 2020, 25, 278. [Google Scholar] [CrossRef] [Green Version]
- Yan, J.; Guo, J.; Fan, C.; Juan, J.; Yu, X.; Li, J. Coronavirus disease 2019 (COVID-19) in pregnant women: A report based on 116 cases. Am. J. Obstet. Gynecol. 2020, 223, 111.e1–111.e14. [Google Scholar] [CrossRef]
- Indra, S.; Vijayasankari, A.; Kalpana, S. Current scenario for management on COVID-19—A global review. Int. J. Med. Biomed. Stud. 2020, 4. [Google Scholar] [CrossRef]
- Valk, S.J.; Piechotta, V.; Chai, K.L.; Doree, C.; Monsef, I.; Wood, E.M.; Lamikanra, A.; Kimber, C.; McQuilten, Z.; So-Osman, C.; et al. Convalescent plasma or hyperimmune immunoglobulin for people with COVID-19: A rapid review. Cochrane Database Syst. Rev. 2020, 5, CD013600. [Google Scholar]
- Lai, C.C.; Shih, T.P.; Ko, W.C.; Tang, H.J.; Hsueh, P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents 2020, 55, 105924. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Rahman, M.S.; Islam, M.R.; Hoque, M.N.; Alam, A.S.M.R.U.; Akther, M.; Puspo, J.A.; Akter, S.; Anwar, A.; Sultana, M.; Hossain, M.A. Comprehensive annotations of the mutational spectra of SARS-CoV-2 spike protein: A fast and accurate pipeline. Transbound. Emerg. Dis. 2021, 68, 1625–1638. [Google Scholar] [CrossRef]
- Okoh, A.I.; Sibanda, T.; Gusha, S.S. Inadequately treated wastewater as a source of human enteric viruses in the environment. Int. J. Environ. Res. Public Health 2010, 7, 2620–2637. [Google Scholar] [CrossRef] [Green Version]
- Okeyo, A.N.; Nontongana, N.; Fadare, T.O.; Okoh, A.I. Vibrio species in wastewater final effluents and receiving watershed in South Africa: Implications for public health. Int. J. Environ. Res. Public Health 2018, 15, 1266. [Google Scholar] [CrossRef] [Green Version]
- Ibekwe, A.M.; Murinda, S.E. Linking microbial community composition in treated wastewater with water quality in distribution systems and subsequent health effects. Microorganisms 2019, 7, 660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, R.; Muller, C.J.F.; Ghoor, S.; Louw, J.; Archer, E.; Surujlal-Naicker, S.; Berkowitz, N.; Volschenk, M.; Bröcker, L.H.L.; Wolfaardt, G.; et al. Qualitative and quantitative detection of SARS-CoV-2 RNA in untreated wastewater in Western Cape Province, South Africa. S. Afr. Med. J. 2021, 111, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Walker, D.B.; Baumgartner, D.J.; Gerba, C.P.; Fitzsimmons, K. Surface water pollution. In Environmental and Pollution Science; Academic Press: Cambridge, MA, USA, 2019; pp. 261–292. [Google Scholar]
- Jones, D.L.; Baluja, M.Q.; Graham, D.W.; Corbishley, A.; McDonald, J.E.; Malham, S.K.; Hillary, L.S.; Connor, T.R.; Gaze, W.H.; Moura, I.B.; et al. Shedding of SARS-CoV-2 in feces and urine and its potential role in person-to-person transmission and the environment-based spread of COVID-19. Sci. Total Environ. 2020, 749, 141364. [Google Scholar] [CrossRef]
- Nzouebet, W.A.L.; Kengne, E.S.; Wafo, G.V.D.; Wanda, C.; Rechenburg, A.; Noumsi, I.M.K. Assessment of the faecal sludge management practices in households of a sub-Saharan Africa urban area and the health risks associated: The case study of Yaoundé, Cameroon. Int. J. Biol. Chem. Sci. 2019, 13, 1–23. [Google Scholar] [CrossRef]
- Umahi, E.N.; Obiano, E.C.; Joel, R.U. A Preview of Water, Sanitation and Hygiene Practices in Kofai Community of Taraba State, Nigeria. Cent. Afr. J. Public Health 2020, 6, 213. [Google Scholar] [CrossRef]
- Yao, M.; Zhang, L.; Ma, J.; Zhou, L. On airborne transmission and control of SARS-Cov-2. Sci. Total Environ. 2020, 139178. [Google Scholar] [CrossRef]
- Guerrero-Latorre, L.; Ballesteros, I.; Villacrés-Granda, I.; Granda, M.G.; Freire-Paspuel, B.; Ríos-Touma, B. SARS-CoV-2 in river water: Implications in low sanitation countries. Sci. Total Environ. 2020, 743, 140832. [Google Scholar] [CrossRef]
- Langone, M.; Petta, L.; Cellamare, C.M.; Ferraris, M.; Guzzinati, R.; Mattioli, D.; Sabia, G. SARS-CoV-2 in water services: Presence and impacts. Environ. Pollut. 2021, 268, 115806. [Google Scholar] [CrossRef]
- Zambrano-Monserrate, M.A.; Ruano, M.A.; Sanchez-Alcalde, L. Indirect effects of COVID-19 on the environment. Sci. Total Environ. 2020, 728, 138813. [Google Scholar] [CrossRef]
- Ramteke, S.; Sahu, B.L. Novel coronavirus disease 2019 (COVID-19) pandemic: Considerations for the biomedical waste sector in India. Case Stud. Chem. Environ. Eng. 2020, 2, 100029. [Google Scholar] [CrossRef]
- Balaraman, V.; Drolet, B.S.; Mitzel, D.N.; Wilson, W.C.; Owens, J.; Gaudreault, N.N.; Meekins, D.A.; Bold, D.; Trujillo, J.D.; Noronha, L.E.; et al. Mechanical transmission of SARS-CoV-2 by house flies. Parasites Vectors 2021, 14, 214. [Google Scholar] [CrossRef] [PubMed]
- Kumar, H.; Azad, A.; Gupta, A.; Sharma, J.; Bherwani, H.; Labhsetwar, N.K.; Kumar, R. COVID-19 Creating another problem? Sustainable solution for PPE disposal through LCA approach. Environ. Dev. Sustain. 2021, 23, 9418–9432. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.M.; Ahmed, S.A.; Rahman, K.A.; Biswas, T.K. Pattern of medical waste management: Existing scenario in Dhaka City, Bangladesh. BMC Public Health 2008, 8, 36. [Google Scholar] [CrossRef] [Green Version]
- Vining, J.; Ebreo, A. Predicting recycling behavior from global and specific environmental attitudes and changes in recycling opportunities 1. J. Appl. Soc. Psychol. 1992, 22, 1580–1607. [Google Scholar] [CrossRef]
- Ma, B.; Li, X.; Jiang, Z.; Jiang, J. Recycle more, waste more? When recycling efforts increase resource consumption. J. Clean. Prod. 2019, 206, 870–877. [Google Scholar] [CrossRef]
- Espejo, W.; Celis, J.E.; Chiang, G.; Bahamonde, P. Environment and COVID-19: Pollutants, impacts, dissemination, management and recommendations for facing future epidemic threats. Sci. Total Environ. 2020, 747, 141314. [Google Scholar] [CrossRef]
- Tabish, M.; Khatoon, A.; Alkahtani, S.; Alkahtane, A.; Alghamdi, J.; Ahmed, S.A.; Mir, S.S.; Albasher, G.; Almeer, R.; Al-Sultan, N.K.; et al. Approaches for prevention and environmental management of novel COVID-19. Environ. Sci. Pollut. Res. 2021, 28, 40311–40321. [Google Scholar] [CrossRef]
- Ogunleye, O.O.; Basu, D.; Mueller, D.; Sneddon, J.; Seaton, R.A.; Yinka-Ogunleye, A.F.; Wamboga, J.; Miljković, N.; Mwita, J.C.; Rwegerera, G.M.; et al. Response to the novel corona virus (COVID-19) pandemic across Africa: Successes, challenges and implications for the future. Front. Pharmacol. 2020, 11, 1205. [Google Scholar] [CrossRef]
- Lindberg, L.D.; VandeVusse, A.; Mueller, J.; Kirstein, M. Early Impacts of the COVID-19 Pandemic: Findings from the 2020 Guttmacher Survey of Reproductive Health Experiences; Guttmacher Institute: New York, NY, USA, 2020. [Google Scholar]
- Singh, J.A.; Moodley, K. Critical care triaging in the shadow of COVID-19: Ethics considerations. SAMJ S. Afr. Med. J. 2020, 110, 355–359. [Google Scholar]
- Shadmi, E.; Chen, Y.; Dourado, I.; Faran-Perach, I.; Furler, J.; Hangoma, P.; Hanvoravongchai, P.; Obando, C.; Petrosyan, V.; Rao, K.D.; et al. Health equity and COVID-19: Global perspectives. Int. J. Equity Health 2020, 19, 104. [Google Scholar] [CrossRef]
- World Health Organization. Critical Preparedness, Readiness and Response Actions for COVID-19: Interim Guidance, 4 November 2020 (No. WHO/COVID-19/Community_Actions/2020.5); World Health Organization: Geneva, Switzerland, 2020.
- Koivusalo, M.; Vartiainen, T. Drinking water chlorination by-products and cancer. Rev. Environ. Health 1997, 12, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Shafi, M.; Liu, J.; Ren, W. Impact of COVID-19 pandemic on micro, small, and medium-sized Enterprises operating in Pakistan. Res. Glob. 2020, 2, 100018. [Google Scholar] [CrossRef]
- Donthu, N.; Gustafsson, A. Effects of COVID-19 on business and research. J. Business Res. 2020, 117, 284–289. [Google Scholar] [CrossRef]
- Hoseinzadeh, E.; Javan, S.; Farzadkia, M.; Mohammadi, F.; Hossini, H.; Taghavi, M. An updated min-review on environmental route of the SARS-CoV-2 transmission. Ecotoxicol. Environ. Saf. 2020, 202, 111015. [Google Scholar] [CrossRef] [PubMed]
- Mourya, D.T.; Yadav, P.D.; Ullas, P.T.; Bhardwaj, S.D.; Sahay, R.R.; Chadha, M.S.; Shete, A.M.; Jadhav, S.; Gupta, N.; Gangakhedkar, R.R.; et al. Emerging/re-emerging viral diseases & new viruses on the Indian horizon. Indian J. Med. Res. 2019, 149, 447–467. [Google Scholar] [PubMed]
- Feldman, C. Potential impact of SARS-CoV-2 infection in HIV-positive patients in South Africa. Wits J. Clin. Med. 2020, 2, 19–24. [Google Scholar] [CrossRef] [Green Version]
- Vadiati, M.; Beynaghi, A.; Bhattacharya, P.; Bandala, E.R.; Mozafari, M. Indirect effects of COVID-19 on the environment: How deep and how long? Sci. Total Environ. 2022, 810, 152255. [Google Scholar] [CrossRef]
- García-Ávila, F.; Valdiviezo-Gonzales, L.; Cadme-Galabay, M.; Gutiérrez-Ortega, H.; Altamirano-Cárdenas, L.; Zhindón-Arévalo, C.; del Pino, L.F. Considerations on water quality and the use of chlorine in times of SARS-CoV-2 (COVID-19) pandemic in the community. Case Stud. Chem. Environ. Eng. 2020, 2, 100049. [Google Scholar] [CrossRef]
- Crawford, D.H. Viruses: A Very Short Introduction; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Zamparini, J.; Venturas, J.; Shaddock, E.; Edgar, J.; Naidoo, V.; Mahomed, A.; Mer, M.; Bolon, S.; Smith, O.; Motara, F.; et al. Clinical characteristics of the first 100 COVID-19 patients admitted to a tertiary hospital in Johannesburg, South Africa. Wits J. Clin. Med. 2020, 2, 105–114. [Google Scholar] [CrossRef]
- Singh, A.K.; Jena, A.; Kumar-M, P.; Sharma, V.; Sebastian, S. Risk and outcomes of coronavirus disease in patients with inflammatory bowel disease: A systematic review and meta-analysis. UEG J. 2021, 9, 159–176. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Adelodun, B.; Ajibade, F.O.; Ibrahim, R.G.; Bakare, H.O.; Choi, K.S. Snowballing transmission of COVID-19 (SARS-CoV-2) through wastewater: Any sustainable preventive measures to curtail the scourge in low-income countries? Sci. Total Environ. 2020, 742, 140680. [Google Scholar] [CrossRef] [PubMed]
- Amoah, I.D.; Pillay, L.; Deepnarian, N.; Awolusi, O.; Pillay, K.; Ramlal, P.; Kumari, S.; Bux, F. Detection of SARS-CoV-2 on contact surfaces within shared sanitation facilities and assessment of the potential risks for COVID-19 infections. Int. J. Hyg. Environ. Health 2021, 236, 113807. [Google Scholar] [CrossRef] [PubMed]
- Elsamadony, M.; Fujii, M.; Miura, T.; Watanabe, T. Possible transmission of viruses from contaminated human feces and sewage: Implications for SARS-CoV-2. Sci. Total Environ. 2020, 755, 142575. [Google Scholar] [CrossRef]
- Gwenzi, W. Leaving no stone unturned in light of the COVID-19 faecal-oral hypothesis? A water, sanitation and hygiene (WASH) perspective targeting low-income countries. Sci. Total Environ. 2020, 753, 141751. [Google Scholar] [CrossRef]
- Street, R.; Malema, S.; Mahlangeni, N.; Mathee, A. Wastewater surveillance for Covid-19: An African perspective. Sci. Total Environ. 2020, 743, 140719. [Google Scholar] [CrossRef]
- Ahmed, W.; Angel, N.; Edson, J.; Bibby, K.; Bivins, A.; O’Brien, J.W.; Choi, P.M.; Kitajima, M.; Simpson, S.L.; Li, J.; et al. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: A proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020, 738, 138764. [Google Scholar] [CrossRef]
- Thompson, J.R.; Nancharaiah, Y.V.; Gu, X.; Lee, W.L.; Rajal, V.B.; Haines, M.B.; Girones, R.; Ng, L.C.; Alm, E.J.; Wuertz, S. Making waves: Wastewater surveillance of SARS-CoV-2 for population-based health management. Water Res. 2020, 184, 116181. [Google Scholar] [CrossRef]
- Bogler, A.; Packman, A.; Furman, A.; Gross, A.; Kushmaro, A.; Ronen, A.; Dagot, C.; Hill, C.; Vaizel-Ohayon, D.; Morgenroth, E.; et al. Rethinking wastewater risks and monitoring in light of the COVID-19 pandemic. Nat. Sustain. 2020, 3, 981–990. [Google Scholar] [CrossRef]
- Alygizakis, N.; Markou, A.N.; Rousis, N.I.; Galani, A.; Avgeris, M.; Adamopoulos, P.G.; Scorilas, A.; Lianidou, E.S.; Paraskevis, D.; Tsiodras, S.; et al. Analytical methodologies for the detection of SARS-CoV-2 in wastewater: Protocols and future perspectives. TrAC Trends Anal. Chem. 2021, 134, 116125. [Google Scholar] [CrossRef]
- Shao, L.; Ge, S.; Jones, T.; Santosh, M.; Silva, L.F.; Cao, Y.; Oliveira, M.L.; Zhang, M.; BéruBé, K. The role of airborne particles and environmental considerations in the transmission of SARS-CoV-2. Geosci. Front. 2021, 12, 101189. [Google Scholar] [CrossRef]
- La Rosa, G.; Mancini, P.; Ferraro, G.B.; Veneri, C.; Iaconelli, M.; Lucentini, L.; Bonadonna, L.; Brusaferro, S.; Brandtner, D.; Fasanella, A.; et al. Rapid screening for SARS-CoV-2 variants of concern in clinical and environmental samples using nested RT-PCR assays targeting key mutations of the spike protein. Water Res. 2021, 197, 117104. [Google Scholar] [CrossRef] [PubMed]
- Morrison, C.; Atkinson, A.; Zamyadi, A.; Kibuye, F.; McKie, M.; Hogard, S.; Mollica, P.; Jasim, S.; Wert, E.C. Critical review and research need of ozone applications related to virus inactivation: Potential implications for SARS-CoV-2. Ozone Sci. Eng. 2021, 43, 2–20. [Google Scholar] [CrossRef]
- Zhao, L.; Seth-Pasricha, M.; Stemate, D.; Crespo-Bellido, A.; Gagnon, J.; Draghi, J.; Duffy, S. Existing host range mutations constrain further emergence of RNA viruses. J. Virol. 2019, 93, e01385-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, X.; Hao, Q.; Mu, Y.; Timani, K.A.; Ye, L.; Zhu, Y.; Wu, J. Nucleocapsid protein of SARS-CoV activates the expression of cyclooxygenase-2 by binding directly to regulatory elements for nuclear factor-kappa B and CCAAT/enhancer binding protein. Int. J. Biochem. Cell Biol. 2006, 38, 1417–1428. [Google Scholar] [CrossRef] [PubMed]
- Sherchan, S.P.; Shahin, S.; Ward, L.M.; Tandukar, S.; Aw, T.G.; Schmitz, B.; Ahmed, W.; Kitajima, M. First detection of SARS-CoV-2 RNA in wastewater in North America: A study in Louisiana, USA. Sci. Total Environ. 2020, 743, 140621. [Google Scholar] [CrossRef]
- Afzal, A. Molecular diagnostic technologies for COVID-19: Limitations and challenges. J. Adv. Res. 2020, 26, 149–159. [Google Scholar] [CrossRef]
- Reed, K.D. Viral Zoonoses. Ref. Modul. Biomed. Sci. 2018. [Google Scholar] [CrossRef]
- Recovery Collaborative Group. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N. Engl. J. Med. 2020, 383, 2030–2040. [Google Scholar] [CrossRef]
- Hsu, J. Covid-19: What now for remdesivir? BMJ 2020, 371, m4457. [Google Scholar] [CrossRef]
- Sisay, M. Available evidence and ongoing clinical trials of remdesivir: Could it be a promising therapeutic option for COVID-19? Front. Pharmacol. 2020, 11, 791. [Google Scholar] [CrossRef] [PubMed]
- Ailabouni, N.J.; Hilmer, S.N.; Kalisch, L.; Braund, R.; Reeve, E. COVID-19 pandemic: Considerations for safe medication use in older adults with multimorbidity and polypharmacy. J. Gerontol. Ser. A 2020, 76, 1068–1073. [Google Scholar] [CrossRef] [PubMed]
- Davoudi-Monfared, E.; Rahmani, H.; Khalili, H.; Hajiabdolbaghi, M.; Salehi, M.; Abbasian, L.; Kazemzadeh, H.; Yekaninejad, M.S. Efficacy and safety of interferon beta-1a in treatment of severe COVID-19: A randomized clinical trial. medRxiv 2020. [Google Scholar] [CrossRef]
- Pacheco, T.J.A.; da Silva, V.C.M.; de Souza, D.G. Nano COVID-19 Vaccines: The firsts RNA lipid nanoparticle vaccines being approved from history-Review. Res. Soc. Dev. 2020, 9, e20191211123. [Google Scholar] [CrossRef]
- Haque, A.; Pant, A.B. Efforts at COVID-19 Vaccine Development: Challenges and Successes. Vaccines 2020, 8, 739. [Google Scholar] [CrossRef]
- Knoll, M.D.; Wonodi, C. Oxford–AstraZeneca COVID-19 vaccine efficacy. Lancet 2020, 397, 72–74. [Google Scholar] [CrossRef]
- Bell, B.P. ACIP COVID-19 Vaccines Work Group. 2020. Available online: https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-09/COVID-01-Bell-508.pdf (accessed on 30 March 2022).
- Mehrotra, D.V.; Janes, H.E.; Fleming, T.R.; Annunziato, P.W.; Neuzil, K.M.; Carpp, L.N.; Benkeser, D.; Brown, E.R.; Carone, M.; Cho, I.; et al. Clinical endpoints for evaluating efficacy in COVID-19 vaccine trials. Ann. Intern. Med. 2021, 174, 221–228. [Google Scholar] [CrossRef]
- Available online: https://www.npr.org/sections/coronavirus-live-updates (accessed on 10 March 2021).
- Langel, S.N.; Paim, F.C.; Lager, K.M.; Vlasova, A.N.; Saif, L.J. Lactogenic immunity and vaccines for porcine epidemic diarrhoea virus (PEDV): Historical and current concepts. Virus Res. 2016, 226, 93–107. [Google Scholar] [CrossRef] [Green Version]
- Available online: https://perkinelmer-appliedgenomics.com/ (accessed on 25 December 2020).

| Treatment Administered/Vaccines Used | Country of Origin | Benefits/Limitations | Shelf Life | Storage | References |
|---|---|---|---|---|---|
| Hydroxychloroquine | USA | Little or no effect on overall mortality. | NA | NA | Recovery Collaborative Group, [83] |
| Remdesivir | Currently not approved for marketing in any country | It is an inhibitor of the viral RNA-dependent, RNA polymerase with in vitro inhibitory action against SARS-CoV. It has little to no effect on COVID patients. | NA | NA | Hsu, [84]; Sisay, [85] |
| Lopinavir/Ritonavir | USA | Harsh side-effects may consist of pancreatitis, liver problems and high blood sugar | NA | NA | Ailabouni et al. [86] |
| Interferon | Currently available for sale in countries besides USA | Possible hepatotoxicity | NA | NA | Davoudi-Monfared et al. [87] |
| Pfizer-BioNTech COVID-19 vaccine | Authorized and recommended by CDC to prevent COVID-19. Originally developed in the USA | 95% effective; mRNA-based vaccine that produces T-cell responses specific to SARS-CoV-2 proteins. Being administered. | NA | NA | Pacheco et al. [88] |
| Moderna COVID-19 vaccine | USA is the first country to greenlight its use | Produces T-cell responses specific to SARS-CoV-2 proteins | NA | NA | Haque and Pant, [89] |
| Oxford-AstraZeneca vaccine | University of Oxford, UK | Being administered | NA | NA | Knoll and Wonodi, [90] |
| Janssen COVID-19 vaccine | Belgium | Clinical trials in progress | NA | NA | Bell, [91] |
| Novavax COVID-19 vaccine | Gaithersburg, Maryland, USA | Clinical trials in progress | NA | NA | Mehrotra et al. [92] |
| Johnson and Johnson vaccine | USA | Being administered | 2 years | −20 °C | [93] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ebomah, K.E.; Msolo, L.; Okoh, A.I. A Review on SARS-CoV-2 Genome in the Aquatic Environment of Africa: Prevalence, Persistence and the Future Prospects. Water 2022, 14, 2020. https://doi.org/10.3390/w14132020
Ebomah KE, Msolo L, Okoh AI. A Review on SARS-CoV-2 Genome in the Aquatic Environment of Africa: Prevalence, Persistence and the Future Prospects. Water. 2022; 14(13):2020. https://doi.org/10.3390/w14132020
Chicago/Turabian StyleEbomah, Kingsley Ehi, Luyanda Msolo, and Anthony Ifeanyi Okoh. 2022. "A Review on SARS-CoV-2 Genome in the Aquatic Environment of Africa: Prevalence, Persistence and the Future Prospects" Water 14, no. 13: 2020. https://doi.org/10.3390/w14132020
APA StyleEbomah, K. E., Msolo, L., & Okoh, A. I. (2022). A Review on SARS-CoV-2 Genome in the Aquatic Environment of Africa: Prevalence, Persistence and the Future Prospects. Water, 14(13), 2020. https://doi.org/10.3390/w14132020






