Abstract
Urinary As (uAs) is a biomarker of As exposure. Urinary creatinine (uCr) or specific gravity (SG) are used to correct uAs for urine dilution. However, uCr is correlated with As methylation, whereas SG has limitations in individuals with kidney damage. We aimed to evaluate which urine dilution correction methods for uAs most accurately predicted blood As (bAs). We used data from the Folic Acid and Creatine Trial (FACT; N = 541) and Folate and Oxidative Stress (FOX; N = 343) study in Bangladesh. Three linear regression models were assessed using uAs (1) adjusted for uCr or SG as separate covariates, (2) standardized for uCr or SG, i.e., uAs/uCr, and (3) adjusted for residual corrected uCr or SG following adjustment for age, sex and BMI. Median uAs/bAs for FACT and FOX were 114/8.4 and 140/12.3 µg/L. In FACT, two-fold increases in uAs adjusted for uCr or SG were related to 34% and 22% increases in bAs, respectively, with similar patterns in FOX. Across methods, models with uCr consistently had lower AIC values than SG. The uAs associations with bAs were stronger after adjustment for uCr vs. SG. Decisions regarding urine dilution methods should consider whether the study outcomes are influenced by factors such as methylation or medical conditions.
Keywords:
arsenic; urine dilution; environmental exposure; metals; water; blood; creatinine; specific gravity 1. Background
Arsenic (As) exposure affects hundreds of millions of people worldwide. Urinary As (uAs) is an established biomarker of As exposure that integrates multiple sources of individuals’ As consumption, including water and food. In Bangladesh and many other countries, the primary As sources are water and rice intake. Characterizing the health effects of As exposure is of great interest for As risk assessment and for protecting populations from pervasive As exposure. Arsenic is filtered through the kidney and excreted in the urine, with some differences across arsenic species as dimethylated As species are more rapidly excreted compared to inorganic As. Urine can be collected non-invasively and analytical methods to quantify uAs are highly sensitive; therefore, spot uAs is the biomarker of choice in most epidemiological studies where uAs is often modeled as a predictor of health outcomes. However, urine dilution, which is affected by recent fluid intake and hydration status, strongly influences the short-term variability of uAs concentrations in individuals. This short-term variability in urine dilution is a major source of measurement error that needs to be corrected for in epidemiological studies using urinary biomarkers, including As [1,2,3]. However, the best method for correcting urinary measurements of metals and metalloids for urine dilution requires further research.
Blood As (bAs) is a biomarker of As exposure and internal dose that does not require adjustment for hydration status, as blood dilution is relatively constant [4]. However, blood is more difficult to collect, and As concentrations in blood are markedly lower compared to urine. Water As (wAs) is a good environmental marker of As exposure, however, wAs does not reflect all potential sources of exposure. While wAs is often measured at the household or community level, estimating an individual’s exposure might be affected by a substantial amount of measurement error, as it is difficult to identify all water sources a person utilizes for drinking and cooking, and to quantify their daily use.
Urinary creatinine (uCr) is a breakdown product of creatine phosphate, a metabolite found in muscle and in other tissues with high energy requirements, such as the heart and brain, where it is used to regenerate adenosine triphosphate (the main carrier of energy in cells) from adenosine diphosphate [5]. Due to previous evidence that uCr is excreted at a relatively constant rate within individuals in urine, uCr is commonly used to correct uAs and other solutes in urine for variability in urine dilution. However, recent studies have found evidence that uCr is excreted at an inconstant rate with intra- and inter-individual variability of uCr over time [2,6,7]. The final step in creatine synthesis is a methylation reaction, whereby S-adenosylmethionine (SAM) donates a methyl group to guanidinoacetate; this process is a major consumer of SAM [8,9]. The metabolism of creatinine and As are thus closely interconnected as SAM is also used to methylate inorganic As (InAs) into mono-arsenical species (MMAs) and di-methyl arsenical species (DMAs) in a process that facilitates urinary As elimination [10]. For reasons that are not entirely understood, uCr is correlated with the relative proportion of InAs and DMAs in urine [11,12,13,14,15]. The major short-term determinant of uCr concentrations is urine dilution. Additional factors such as meat intake and muscle mass also influence uCr levels, some of which are illustrated in a directed acyclic graph (DAG) in Figure 1.
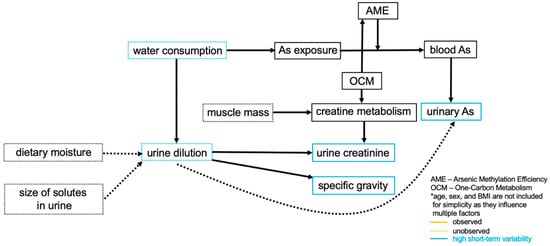
Figure 1.
Conceptual diagram of arsenic biomarkers and urine dilution adjustment methods.
Adjusting for variability in urine dilution using uCr in As analyses may introduce bias. For example, it has been proposed that collider bias can occur when the study outcome is obesity or obesity-related [16]. An alternative method utilizes specific gravity (SG), defined as the ratio of the density of urine to the density of water, which also reflects urine dilution. However, SG is influenced by the presence of glucose and protein in urine and as such has limitations in individuals with kidney damage and diabetes. Furthermore, SG is less precise than uCr, as it has a relatively narrow range with generally only one informative numeric digit.
Urine volume fluctuates with fluid intake, perspiration, physical activity, and respiratory rate. Both uCr concentrations and SG primarily reflect urine volume and the amount of water consumed. A study in rural Bangladesh assessed urine dilution methods for uAs analyses in a malnourished population (N = 1466) and found that uCr can be related to a number of factors that may not influence SG. These include age, gender, body size, muscle mass, and dietary meat intake (i.e., the predominant dietary source of creatine, which is generally low in rural Bangladesh) [2]. The use of SG as a proxy for hydration status also requires considerations regarding factors that influence major solutes in urine, such as age, sex, albuminuria and diabetes status. Although uAs analyses most commonly adjust for uCr in models, few studies have directly compared multiple urine dilution correction methods to determine the best approach [17,18]. In a recent analysis by Hoet et al., uAs in spot urine samples corrected for SG seemed to be more reliable than corrections for uCr as compared to the “gold standard” of 24 h urine samples [1]. However, it should be noted that 24 h urine samples are subject to substantial measurement error and may require urine dilution corrections as well [19]. Currently, there is not a clear consensus as to which (1) biomarker (uCr or SG) and (2) modeling approach is the most appropriate to use for urine dilution correction in uAs analyses. The objective of our study was to remove the influence of variability of urine dilution on uAs by correcting for uCr and SG, and then to compare the performance of both methods versus bAs, a biomarker of As exposure that is unaffected by hydration status, or to wAs concentration, which is the primary source of As in this population. Additionally, we compared three common linear regression modeling approaches to unadjusted models: (1) Adjusted models—either uCr or SG are added as covariates in the models, (2) Standardized models—a new standardized uAs variable is created by correcting uAs for uCr or SG, and this standardized uAs is used in the models, or (3) Covariate adjusted standardized (residual corrected) models—residual corrected uCr or SG are added as covariates in the models. Comparing these urine dilution correction methods is crucial for determining which approach introduces the least amount of bias and accounts for most of the variability of urine, without overcorrecting.
2. Methods
2.1. Study Populations
This study leveraged data and samples previously collected from participants of the Folic Acid and Creatine Trial (FACT) and Folate and Oxidative Stress (FOX) study, both of which were conducted in Araihazar, Bangladesh. These studies recruited participants from the Health Effects of Arsenic Longitudinal Study (HEALS), a prospective cohort study which followed more than 12,000 participants starting in 2000 [20].
Full descriptions of these studies have previously been reported [20,21,22]. Briefly, all study participants resided in Araihazar, a region of Bangladesh 25 km2 southeast of Dhaka, where well water As concentrations vary widely. The Columbia University Institutional Review Board and the Ethical Committee of the Bangladesh Medical Research Council approved all study protocols. The eligibility criteria for HEALS participants were: (1) married adults aged 20–65 years old, (2) area residents for at least 5 years, and (3) drinking water primarily from the same household well for at least 3 years. Starting in 2009, participants in FACT were randomly selected from HEALS participants who had been drinking from a household well with water As > 50 µg/L, for at least 1 year. The exclusion criteria for FACT were: (1) women who were pregnant, (2) participants taking nutritional supplements, and (3) participants with known diabetes, cardiovascular, or renal disease, or other known health issues [21]. The inclusion/exclusion criteria for FOX were similar to those of FACT, but study participants were selected in 2008 according to their water As exposure: participants were recruited from each of five well water As concentration categories: <10 (n = 76), 10–100 (n = 104), 101–200 (n = 86), 201–300 (n = 67), and >300 µg/L (n = 45) [22].
2.2. Demographic Characteristics
Age and sex were recorded during baseline interviews. BMI was computed based on weight and height measured by trained examiners following a standardized protocol.
2.3. Arsenic Measurements
Tube well water As. Water As concentrations were measured at Columbia University’s Lamont Doherty Earth Observatory using inductively coupled plasma-mass spectrometry (ICP-MS) as described [23]. The intra-assay coefficients of variation (CVs) were for FACT and FOX were 2.0% and 6.0%, respectively. The inter-assay CVs for FACT and FOX were 2.6% and 3.8%, respectively. The limit of detection (LOD) was <0.2 µg/L; no samples were below the LOD.
Total Urinary As. Urinary As was measured in the Columbia University Trace Metals Core Laboratory using a Perkin-Elmer Analyst 600 GFAA as previously described [24]. The intra-assay CVs for FACT and FOX were 3.1% and 3.8%, respectively. The inter-assay CVs for FACT and FOX were 5.4%, and 5.1%, respectively. The LOD for uAs was 5 µg/L. None of the samples for FACT or FOX were below the LOD.
Total Blood As. Venous blood samples collected in EDTA vacutainer tubes were used for bAs analyses using a PerkinElmer Elan DRC II ICP-MS with an AS93+ autosampler [4]. The intra-assay CVs for FACT and FOX were 2.7% and 3.2%, respectively. The inter-assay CVs for FACT and FOX were 5.7% and 5.7%, respectively. The LOD for bAs was 0.5 µg/L of blood and no samples were below the LOD in FACT or FOX.
Creatinine and Specific Gravity. In FACT and FOX, uCr concentrations were measured by a method based on the Jaffe reaction [25]. SG was measured using a handheld refractometer (TS 400, Reichert, Depew, NY, USA) [26].
2.4. Statistical Analyses
All variables were assessed for normality. Statistical analyses were conducted using R 3.6.3 [27]. We examined 610 participants from the Folic Acid and Creatine Trial (FACT) study and 378 participants from the FOX study separately. Urine samples with SG ≤ 1.001 or SG ≥ 1.02, outside the normal range [28], were removed from the dataset (N = 46 out of 610 samples from FACT and N = 33 out of 379 samples from FOX). Urine samples with uiAs% ≥ 55%, outside the normal range were removed from the dataset (N = 1 out of 564 samples in FACT). Participants with missing bAs, wAs, SG, or BMI measurements were excluded, resulting in 541 participants in FACT and 343 participants in FOX.
Correction Method Calculations. A classic method used to correct for urine dilution is to standardize uAs for uCr by dividing as uAs (ug) per gram of uCr (uAs/uCr). To standardize uAs for SG (uAs-SG), we used the following formula: uAs × (overall mean SG − 1)/(measured SG − 1), as previously described [29]. As an alternative method, covariate adjusted uCr was calculated by first regressing uCr onto age, sex, and BMI, extracting the residuals from this linear regression, and then adding the mean creatinine values to these residuals—resulting in a residual-based measure of uCr that is independent of age, sex, and BMI. This method was also used to calculate a residual-based measure of SG that is also independent of age, sex, and BMI.
The two studies were used to analyze the association between log2-transformed total bAs or log2-transformed wAs and log2-transformed uAs with adjustments for the three urine dilution methods listed below. Unadjusted models did not include adjustment for urine dilution.
- Adjusted models included log2-transformed uAs with further adjustments for either log2-transformed uCr or log2-transformed SG in separate models;
- Standardized models were adjusted for either log2-transformed uAs standardized for uCr (uAs/uCr) or log2-transformed uAs standardized for SG (uAs-SG) as described above in separate models;
- Covariate adjusted standardized (residual corrected) models included log2-transformed uAs with further adjustments for either log2-transformed residual corrected uCr or log2-transformed residual corrected SG in separate models.
Unadjusted, adjusted, and standardized models were all further adjusted for age, sex, and BMI, while covariate adjusted standardized models accounted for age, sex, and BMI for calculation of the residuals.
To quantify the relative quality of the models, Akaike information criteria (AIC) were calculated using the formula , where is the number of parameters in the model and is the log likelihood. Therefore, when comparing the AIC values of two separate models, those with lower AIC values indicate a better model fit, with a difference of −2 or more revealing significant difference between models.
Another method to estimate the differences between the models was to calculate the percent change as compared to the unadjusted model, which was calculated as follows: .
For sensitivity analyses, we used lasso and elastic net regression for variable selection to assess whether uCr or SG were necessary for the predictive accuracy of uAs in the unadjusted and adjusted models previously mentioned.
3. Results
3.1. Participant Characteristics
By design, about 50% of the study participants were female in both studies (Table 1). The median ages were 38 and 42 years old in FACT and FOX, respectively. The mean BMI was 19.8 (2.7) and 20.4 (3.4) kg/m2 (SD) in FACT and FOX, respectively. Median uAs concentrations were 114 and 140 µg/L in FACT and FOX, respectively. Median bAs/wAs concentrations were 8.4/103 and 12.3/114 µg/L in FACT and FOX, respectively. Median uCr (mg/dL)/SG levels were 50.0/1.007 and 43.8/1.007 in FACT and FOX, respectively. Urinary creatinine and SG were highly correlated with each other in FACT (Spearman correlation = 0.86, p < 0.0001) and FOX (Spearman correlation = 0.90, p < 0.0001). The distributions of uCr and SG (Figure A1) show the sparsity of values for SG, where the third decimal place is important for detecting differences across individuals.

Table 1.
Participant Characteristics in FACT and FOX stratified by sex.
3.2. Blood Arsenic Adjusted Models
Adjustment for uCr compared to adjustment for SG in log2–log2 linear regression models resulted in a stronger association of uAs with bAs in both FACT and FOX, as indicated by both higher geometric mean ratios and lower AIC values in the model adjusted for uCr (Table 2 top). In models that were unadjusted, adjusted for uCr, or adjusted for SG, geometric mean ratios (95% CI) of bAs per doubling of uAs were 1.34 (1.30, 1.38), 1.79 (1.75, 1.83), and 1.64 (1.59, 1.68), respectively, in FACT participants. Consistent with FACT, in FOX participants, the corresponding geometric mean ratios (95% CI) were 1.26 (1.21, 1.32), 1.78 (1.73, 1.84), and 1.55 (1.49, 1.61), respectively. Both in FACT and FOX, the associations between uAs and bAs were consistent for men and women separately in all models (Table 3 top). Compared to the unadjusted uAs model, uAs in models with uCr and SG adjustments resulted in 34% and 22% improvement in estimating bAs concentrations in FACT, and 36% and 23% improvement in FOX, respectively.

Table 2.
Geometric mean ratio for blood and water arsenic levels per two-fold increase in urine arsenic levels.

Table 3.
Geometric mean ratio for blood arsenic levels per two-fold increase in urine arsenic levels stratified by sex (Top). Geometric mean ratio for water arsenic levels per two-fold increase in urine arsenic levels stratified by sex (Bottom).
All unadjusted, adjusted, and standardized models included adjustments for age, sex, and BMI. Covariate adjusted standardized models were further adjusted for the corresponding dilution correction method.
3.3. Water Arsenic Adjusted Models
Adjustment for uCr compared to adjustment for SG in log2–log2 linear regression models also resulted in a stronger association of uAs with wAs (Table 2 bottom). The geometric mean ratios (95% CI) per doubling of uAs in wAs models that were unadjusted, adjusted for uCr and adjusted for SG, respectively, were stronger for males (1.42 (1.30, 1.55), 1.71 (1.52, 1.92), and 1.62 (1.45, 1.81)) than females (1.30 (1.21, 1.39), 1.55 (1.42, 1.68), and 1.46 (1.35, 1.58)) in FACT, and to some extent also in FOX (Table 3 bottom). Compared to the unadjusted uAs model, uAs in models with uCr and SG adjustments resulted in 30% and 20% improvements in estimating wAs levels in FACT, and 36% and 23% improvements in FOX, respectively.
3.4. Standardized Models
Crude log–log linear models with total uAs standardized for either uCr or SG had a strong positive association with bAs in both studies, with FOX having slightly wider 95% confidence intervals (as shown in gray around the regression line) than FACT (Figure 2a). Similar linear associations were observed between total uAs standardized for either uCr or SG and wAs (Figure 2b). Adjustment for uCr or SG resulted in narrower 95% confidence intervals for all outcomes compared to models that did not account for urine dilution, with the model standardized for uCr having steeper regression lines and narrower confidence intervals overall.
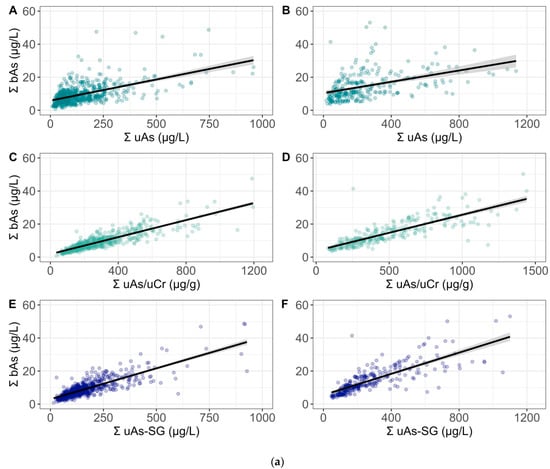
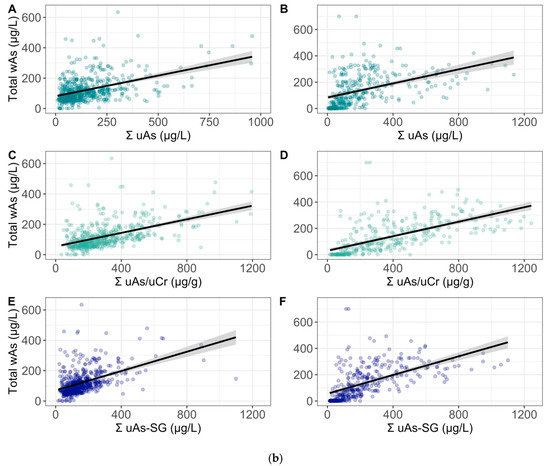
Figure 2.
(a) Crude Log–Log linear models of the sum of blood arsenic species (Σ bAs) with the sum of urinary arsenic species (Σ uAs) that is unadjusted, adjusted for creatinine (uCr) and adjusted for specific gravity (SG) in FACT (A,C,E) and FOX (B,D,F), respectively. (b) Crude Log–Log linear models of total water arsenic (wAs) with the sum of urinary arsenic species (Σ uAs) that is unadjusted, adjusted for creatinine (uCr) and adjusted for specific gravity (SG) in FACT (A,C,E) and FOX (B,D,F), respectively.
Consistently, across all of the adjusted and standardized log2–log2 linear regression models, uCr and SG had similar patterns of association regardless of the outcome or dilution correction method (Table 2). In FACT, the AIC values for the bAs models with uAs standardized for uCr and SG were 270.0 and 613.9, respectively. In FOX, the models standardized for uCr and SG had AIC values of 180.8 and 271.5, respectively. Water As models resulted in similar patterns, with lower AIC values for models standardized for uCr as compared to SG. Stratification by sex did not change these patterns of association; however, AIC values were more similar across models within the same sex (Table 3).
3.5. Residual Corrected Models
Consistent with all of the previous models, residual corrected uCr models resulted in lower AIC values than residual corrected SG models (Table 2). Overall, these models were most similar to uCr and SG adjusted models, but with wider confidence intervals.
In FACT, the lowest AIC values from the bAs models were from the uCr standardized model. In FOX, the lowest AIC values from the bAs models were from the uCr adjusted models. The AIC values for wAs models had similar patterns across models.
3.6. Sensitivity Analyses
In sensitivity analyses, both uCr and SG were relevant variables for the predictive accuracy of uAs in models fully adjusted for both variables. In comparing the mean squared error (MSE) for each model with separate adjustments for uCr and SG, models adjusted for uCr consistently had slightly lower MSE values than models adjusted for SG (Table A1).
4. Discussion
Our objective was to compare biomarkers of urine dilution—uCr and SG—and to assess three statistical urine dilution correction methods in order to evaluate which approach most accurately predicts bAs and wAs concentrations in a Bangladeshi population having high exposure to As-contaminated drinking water. Three linear regression models were assessed using uAs (1) adjusted for uCr or SG as separate model covariates, (2) standardized for uCr or SG, i.e., uAs/uCr, and (3) adjusted for residual corrected values for uCr or SG following adjustment for age, sex and BMI. Overall, we found that the associations of uAs with bAs and wAs were stronger in models that utilized uCr as compared to SG to adjust for urine dilution. Models with uCr consistently had lower AIC values than models with SG regardless of which of the three regression models was employed, suggesting that uCr outperformed SG, particularly in terms of predicting bAs concentrations (Table 2). However, it should be noted that all three models that accounted for urine dilution—either with uCr or SG—consistently had higher geometric mean ratios and lower AIC values than models that did not account for urine dilution (unadjusted models), underscoring the importance of urine dilution adjustments in uAs analyses.
As a biomarker of exposure, bAs captures all sources of exposure, and wAs is a less precise measure of exposure, due to the fact that people typically drink from more than one well, consume varying amounts of water, and ingest various foods containing As. Consequently, differences across models with uCr and SG adjusted uAs were smaller when wAs was the outcome as compared to bAs. Additionally, AIC values for wAs (but not for bAs) were consistently higher for males than for females. This could be a result of more measurement error in male exposure data, as males in this region have more opportunities to drink water from different sources, such as job sites [30].
The availability of data on concentrations of As in blood, urine and water in the FACT and FOX studies provided a unique opportunity to evaluate three commonly used statistical methods and two proxy variables to account for dilution in uAs. The models were developed to reflect real-world applications, where uAs is adjusted or standardized for uCr or SG and may be used to predict an outcome of interest. However, a full evaluation of the potential impact of these approaches for urine dilution adjustment requires analyses of studies with a health outcome and consideration of other factors that impact uCr and SG as these may introduce bias via confounding. Long-term predictors of uCr such as muscle mass and body mass index change slowly over time, generally resulting in differences across individuals but not within individuals. However, these and other factors that influence uCr and/or SG might be relevant for the health outcome of interest and therefore the choice of urine dilution adjustment method may introduce bias.
Careful consideration of which approach (e.g., urine dilution unadjusted or adjusted models, using uCr or SG) will provide models that more accurately reflect the associations between As and the outcome of interest. For example, consider testing the hypothesis that the methylation of As is saturable, such that at higher levels of As exposure, a greater percentage of As is excreted in urine as InAs. In the FACT study, using total bAs as a biomarker of As exposure, the correlation between bAs and InAs% in urine is 0.21 (p < 0.0001). Using uAs/uCr as the exposure, the correlation with iAs% is smaller, at 0.16 (p = 0.0001). As mentioned previously, uCr is itself a predictor of As methylation capacity, and in FACT, the correlation between uCr and InAs% is −0.27 (p < 0.0001). In this example, when using uAs/uCr as the exposure variable, uCr is itself capturing a part of the variability of InAs% and therefore the effect size of As exposure on the saturation of As methylation capacity is underestimated. Additionally, when studying sex-specific effects of As exposure on an outcome, it is important to also consider conducting sensitivity analyses that include models without any adjustment for urine dilution, as correcting for uCr or SG could introduce potential bias.
One approach to aid in the decision of which urine dilution approach is most appropriate for a given As-related research question is to create a DAG, or conceptual diagram a priori, such as that presented in Figure 1. In this figure, only a subset of variables that influence uCr concentrations are shown, and although the number of predictors of uCr is greater than that of SG, uCr was still a better proxy of hydration status in these analyses predicting bAs concentrations. Note that the figure does not include age, sex, and BMI because they influence multiple factors in the conceptual diagram. Thus, adjusting for age, sex, and BMI in models may capture the variability of other factors in Figure 1 that influence uCr, resulting in improved uCr model estimates.
In conclusion, decisions regarding which urine dilution method is most appropriate for a given study and/or exposure should consider whether the exposure and the study outcomes are influenced by factors such as age, sex, BMI, As methylation, kidney function, muscle mass, ethnicity, season, pregnancy state and others, which may be associated with uCr and/or SG [1]. Additional studies are needed in populations with different levels of As exposure and sociodemographic characteristics to evaluate the consistency of the findings and the optimization of urine dilution adjustment methods studies linking As exposure to As-related health outcomes.
Author Contributions
Conceptualization, A.A., A.N.-A. and M.V.G.; methodology, A.A., J.G., A.N.-A. and M.V.G.; formal analysis, A.A.; investigation, F.P., T.I., J.H.G. and M.V.G.; resources, M.V.G.; data curation, A.A. and N.L.; writing—original draft preparation, A.A.; writing—review and editing, A.A., J.G., J.B.H., J.H.G., A.N.-A. and M.V.G.; visualization, A.A.; supervision, A.N.-A. and M.V.G.; project administration, M.V.G.; funding acquisition, J.H.G. and M.V.G. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by US National Institutes of Health (NIH) grants including, National Cancer Institute R01 CA133595, National Institute of Environmental Health Sciences (NIEHS) P42 ES010349, NIEHS R01ES030945, National Institute of Health P30 ES0090089, National Institute of General Medical Sciences R25 GM062454, and NIEHS F31 ES032321.
Institutional Review Board Statement
The FACT and FOX studies were conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Columbia University Medical Center and the Bangladesh Research Council (FACT protocol AAAC86218, with the original approval date of 25 January 2006; FOX protocol AAAB8701, with the original approval date of 28 February 2008).
Informed Consent Statement
Informed consent was obtained from all participants involved in both studies. Participants of both studies also consented for the use of their data in future studies.
Acknowledgments
The authors would like to thank all of the FACT and FOX participants and staff who made this work possible.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
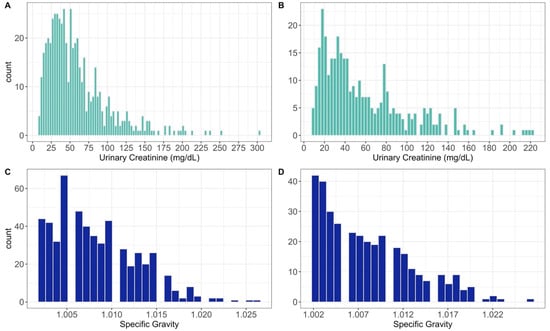
Figure A1.
Distribution of urine creatinine and specific gravity in FACT (A,C) and FOX (B,D), respectively.

Table A1.
Sensitivity analyses using lasso and elastic net regression to predict blood and water arsenic in FACT and FOX.
Table A1.
Sensitivity analyses using lasso and elastic net regression to predict blood and water arsenic in FACT and FOX.
| FACT | FOX | ||||
|---|---|---|---|---|---|
| Outcome | Urine Dilution Method | Lasso (MSE) | Elastic Net (MSE) | Lasso (MSE) | Elastic Net (MSE) |
| Blood Arsenic | Unadjusted | 0.093 | 0.093 | 0.092 | 0.094 |
| Adjusted for uCr | 0.101 | 0.101 | 0.101 | 0.098 | |
| Adjusted for SG | 0.190 | 0.190 | 0.188 | 0.189 | |
| Water Arsenic | Unadjusted | 1.16 | 1.16 | 0.418 | 0.418 |
| Adjusted for uCr | 1.16 | 1.16 | 0.418 | 0.418 | |
| Adjusted for SG | 1.19 | 1.19 | 0.461 | 0.461 | |
All models were adjusted for total uAs, age, sex, and BMI, with further adjustments for uCr and SG where indicated.
References
- Hoet, P.; Deumer, G.; Bernard, A.; Lison, D.; Haufroid, V. Urinary Trace Element Concentrations in Environmental Settings: Is There a Value for Systematic Creatinine Adjustment or Do We Introduce a Bias? J. Expo. Sci. Environ. Epidemiol. 2016, 26, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Nermell, B.; Lindberg, A.-L.; Rahman, M.; Berglund, M.; Persson, L.Å.; el Arifeen, S.; Vahter, M. Urinary Arsenic Concentration Adjustment Factors and Malnutrition. Environ. Res. 2008, 106, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-K.; Song, J.-W.; Park, J.D.; Choi, B.-S. A Comparison of the Adjustment Methods for Assessing Urinary Concentrations of Cadmium and Arsenic: Creatinine Vs. Specific Gravity. Korean J. Environ. Health Sci. 2011, 37, 450–459. [Google Scholar] [CrossRef][Green Version]
- Hall, M.; Chen, Y.; Ahsan, H.; Slavkovich, V.; Van Geen, A.; Parvez, F.; Graziano, J. Blood Arsenic as a Biomarker of Arsenic Exposure: Results from a Prospective Study. Toxicology 2006, 225, 225–233. [Google Scholar] [CrossRef]
- Wyss, M.; Kaddurah-Daouk, R. Creatine and Creatinine Metabolism. Physiol. Rev. 2000, 80, 1107–1213. [Google Scholar] [CrossRef]
- Garde, A.H.; Hansen, Å.M.; Kristiansen, J.; Knudsen, L.E. Comparison of Uncertainties Related to Standardization of Urine Samples with Volume and Creatinine Concentration. Ann. Occup. Hyg. 2004, 48, 171–179. [Google Scholar]
- De Keyzer, W.; Huybrechts, I.; Dekkers, A.L.M.; Geelen, A.; Crispim, S.; Hulshof, P.J.M.; Andersen, L.F.; Rehurková, I.; Ruprich, J.; Volatier, J.-L.; et al. Predicting Urinary Creatinine Excretion and Its Usefulness to Identify Incomplete 24 H Urine Collections. Br. J. Nutr. 2012, 108, 1118–1125. [Google Scholar] [CrossRef]
- Mudd, S.H.; Poole, J.R. Labile Methyl Balances for Normal Humans on Various Dietary Regimens. Metab. Clin. Exp. 1975, 24, 721–735. [Google Scholar] [CrossRef]
- Brosnan, J.T.; da Silva, R.P.; Brosnan, M.E. The Metabolic Burden of Creatine Synthesis. Amino Acids 2011, 40, 1325–1331. [Google Scholar] [CrossRef]
- Challenger, F. Biological Methylation. Chem. Rev. 1945, 36, 315–361. [Google Scholar] [CrossRef]
- Gamble, M.V.; Liu, X.; Ahsan, H.; Pilsner, J.R.; Ilievski, V.; Slavkovich, V.; Parvez, F.; Levy, D.; Factor-Litvak, P.; Graziano, J.H. Folate, Homocysteine, and Arsenic Metabolism in Arsenic-Exposed Individuals in Bangladesh. Environ. Health Perspect. 2005, 113, 1683–1688. [Google Scholar] [CrossRef] [PubMed]
- Gamble, M.V.; Liu, X.; Ahsan, H.; Pilsner, J.R.; Ilievski, V.; Slavkovich, V.; Parvez, F.; Chen, Y.; Levy, D.; Factor-Litvak, P.; et al. Folate and Arsenic Metabolism: A Double-Blind, Placebo-Controlled Folic Acid-Supplementation Trial in Bangladesh. Am. J. Clin. Nutr. 2006, 84, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.N.; Liu, X.; Slavkovich, V.; Ilievski, V.; Pilsner, J.R.; Alam, S.; Factor-Litvak, P.; Graziano, J.H.; Gamble, M.V. Folate, Cobalamin, Cysteine, Homocysteine, and Arsenic Metabolism among Children in Bangladesh. Environ. Health Perspect. 2009, 117, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Mitra, S.; Chung, J.; Mazumder, D.N.G.; Ghosh, N.; Kalman, D.; von Ehrenstein, O.S.; Steinmaus, C.; Liaw, J.; Smith, A.H. Creatinine, Diet, Micronutrients, and Arsenic Methylation in West Bengal, India. Environ. Health Perspect. 2011, 119, 1308–1313. [Google Scholar] [CrossRef] [PubMed]
- Kile, M.L.; Hoffman, E.; Hsueh, Y.-M.; Afroz, S.; Quamruzzaman, Q.; Rahman, M.; Mahiuddin, G.; Ryan, L.; Christiani, D.C. Variability in Biomarkers of Arsenic Exposure and Metabolism in Adults over Time. Environ. Health Perspect. 2009, 117, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Bulka, C.M.; Bulka, C.M.; Mabila, S.L.; Lash, J.P.; Turyk, M.E. Arsenic and Obesity: A Comparison of Urine Dilution Adjustment Methods. Environ. Health Perspect. 2017, 125, 87020. [Google Scholar] [CrossRef]
- Gamble, M.; Liu, X. Urinary Creatinine and Arsenic Metabolism. Environ. Health Perspect. 2005, 113, A442. [Google Scholar] [CrossRef][Green Version]
- Barr, D.B.; Wilder, L.C.; Caudill, S.P.; Gonzalez, A.J.; Needham, L.L.; Pirkle, J.L. Urinary Creatinine Concentrations in the U.S. Population: Implications for Urinary Biologic Monitoring Measurements. Environ. Health Perspect. 2005, 113, 192–200. [Google Scholar] [CrossRef]
- Miler, M.; Simundić, A.M. Low Level of Adherence to Instructions for 24-Hour Urine Collection among Hospital Outpatients. Biochem. Med. 2013, 23, 316–320. [Google Scholar] [CrossRef]
- Ahsan, H.; Chen, Y.; Faruque, P.; Argos, M.; Iftikhar, H.A.; Hassina, M.; Levy, D.; van Green, A.; Howe, G.; Graziano, J. Health Effects of Arsenic Longitudinal Study (Heals): Description of a Multidisciplinary Epidemiologic Investigation. J. Expo. Sci. Environ. Epidemiol. 2006, 16, 191–205. [Google Scholar] [CrossRef]
- Peters, B.A.; Hall, M.N.; Liu, X.; Parvez, F.; Sanchez, T.R.; van Geen, A.; Mey, J.L.; Siddique, A.B.; Hasan, S.; Nasir Udin, M.; et al. Folic Acid and Creatine as Therapeutic Approaches to Lower Blood Arsenic: A Randomized Controlled Trial. Environ. Health Perspect. 2015, 123, 1294. [Google Scholar] [CrossRef]
- Hall, M.N.; Niedzwiecki, M.; Liu, X.; Harper, K.N.; Alam, S.; Slavkovich, V.; Ilievski, V.; Levy, D.; Siddique, A.B.; Faruque, P.; et al. Chronic Arsenic Exposure and Blood Glutathione and Glutathione Disulfide Concentrations in Bangladeshi Adults. Environ. Health Perspect. 2013, 121, 1068. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Zheng, Y.; Mortlock, R.; van Geen, A. Rapid Multi-Element Analysis of Groundwater by High-Resolution Inductively Coupled Plasma Mass Spectrometry. Anal. Bioanal. Chem. 2004, 379, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Nixon, D.E.; Mussmann, G.V.; Eckdahl, S.J.; Moyer, T.P. Total Arsenic in Urine: Palladium-Persulfate Vs Nickel as a Matrix Modifier for Graphite Furnace Atomic Absorption Spectrophotometry. Clin. Chem. 1991, 37, 1575. [Google Scholar] [CrossRef] [PubMed]
- Slot, C. Plasma Creatinine Determination. A New and Specific Jaffe Reaction Method. Scand. J. Clin. Lab. Investig. 1965, 17, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Harper, K.N.; Liu, X.; Hall, M.N.; Ilievski, V.; Oka, J.; Calancie, L.; Slavkovich, V.; Levy, D.; Siddique, A.; Alam, S.; et al. A Dose-Response Study of Arsenic Exposure and Markers of Oxidative Damage in Bangladesh. J. Occup. Environ. Med. 2014, 56, 652–658. [Google Scholar] [CrossRef][Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Miller, R.C.; Brindle, E.; Holman, D.J.; Shofer, J.; Klein, N.A.; Soules, M.R.; O’Connor, K.A. Comparison of Specific Gravity and Creatinine for Normalizing Urinary Reproductive Hormone Concentrations. Clin. Chem. 2004, 50, 924–932. [Google Scholar] [CrossRef]
- Cone, E.J.; Caplan, Y.H.; Moser, F.; Robert, T.; Shelby, M.K.; Black, D.L. Normalization of Urinary Drug Concentrations with Specific Gravity and Creatinine. J. Anal. Toxicol. 2009, 33, 1–7. [Google Scholar] [CrossRef]
- Huhmann, L.B.; Harvey, C.F.; Navas-Acien, A.; Graziano, J.; Slavkovich, V.; Chen, Y.; Argos, M.; Ahsan, H.; van Geen, A. A Mass-Balance Model to Assess Arsenic Exposure from Multiple Wells in Bangladesh. J. Expo. Sci. Environ. Epidemiol. 2021, 1–9. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).