Evaluation of Medical Carrying Capacity for Megacities from a Traffic Analysis Zone View: A Case Study in Shenzhen, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area
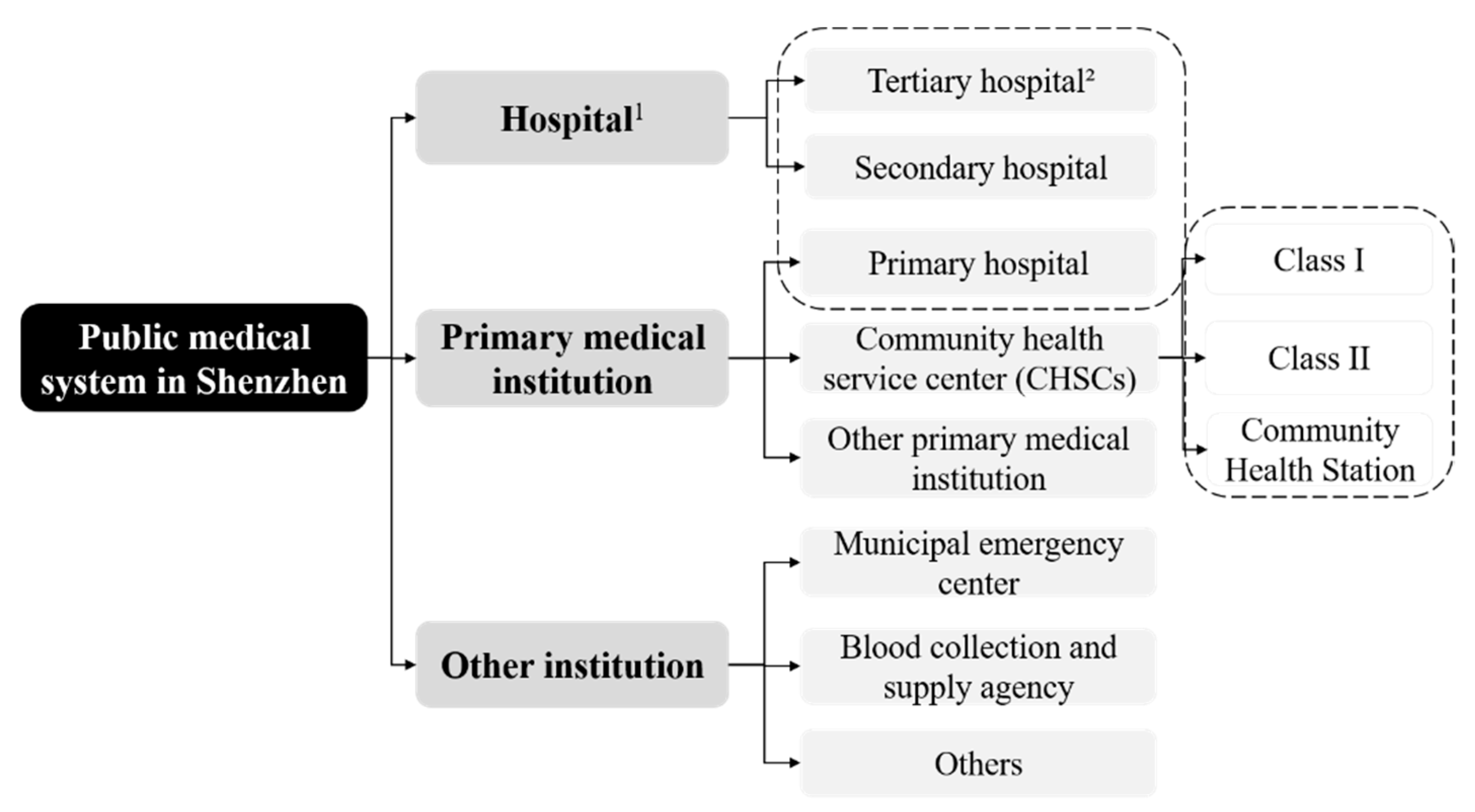
2.2. Data Sources
2.3. Methods
2.3.1. Kernel Density Estimation
2.3.2. Spatial Autocorrelation Model
2.3.3. Improved Potential Model
2.3.4. Carrying-Capacity Evaluation Model
3. Results
3.1. Spatial Differentiation Characteristics of Public Medical Facilities
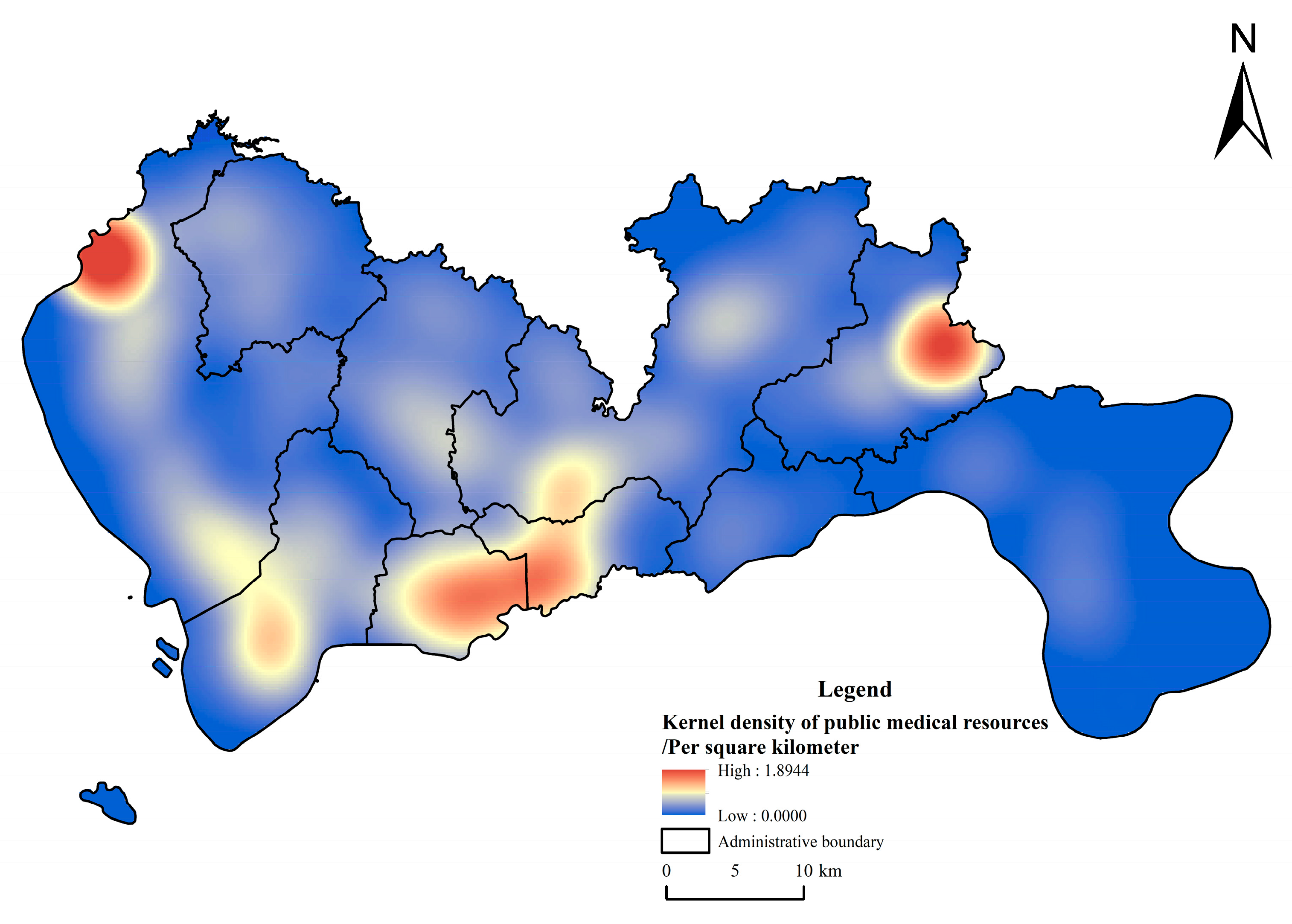
3.1.1. Density Distribution Characteristics of Public Medical Facilities
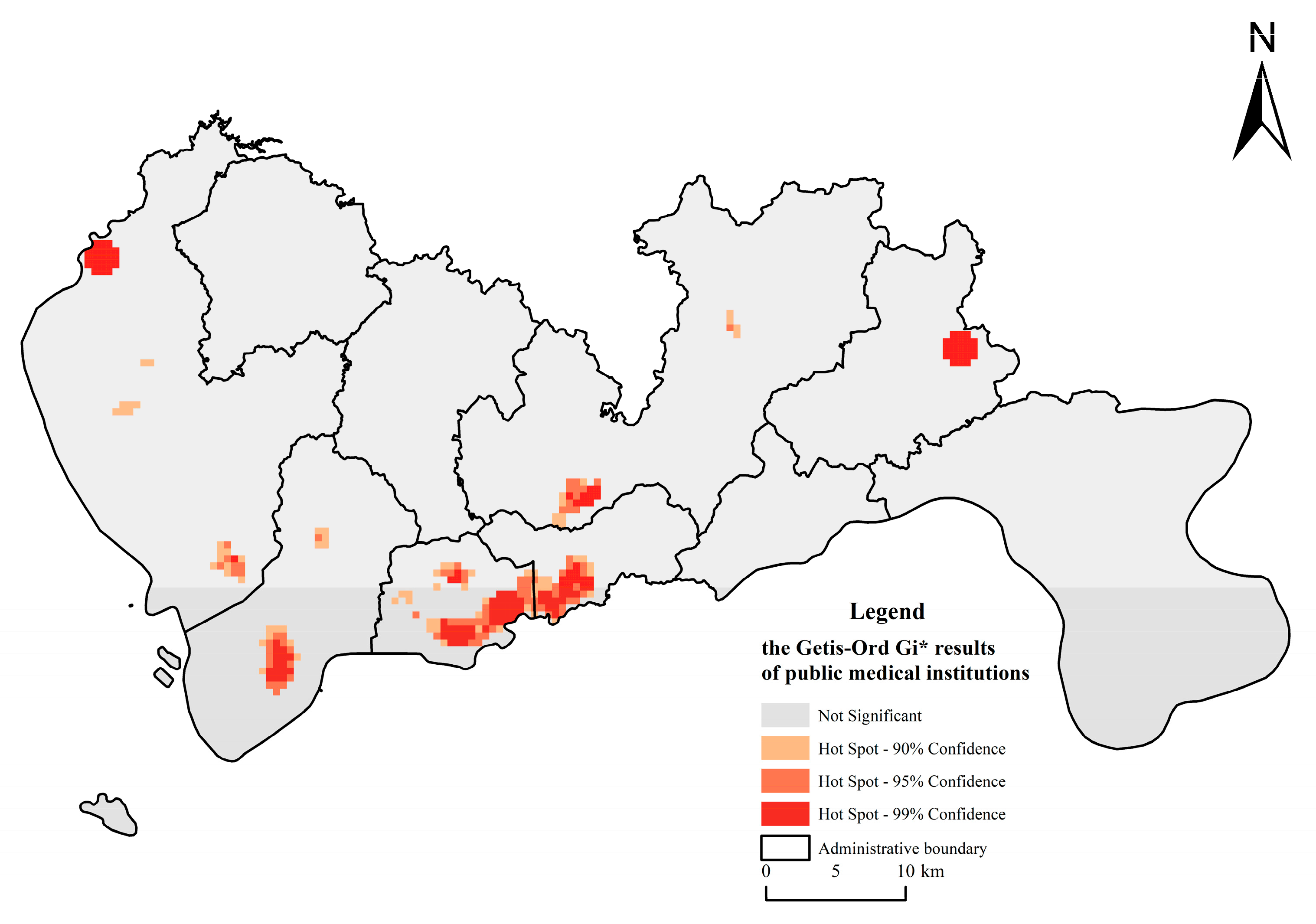
3.1.2. Cold and Hotspot Distribution Characteristics of Public Healthcare Facilities
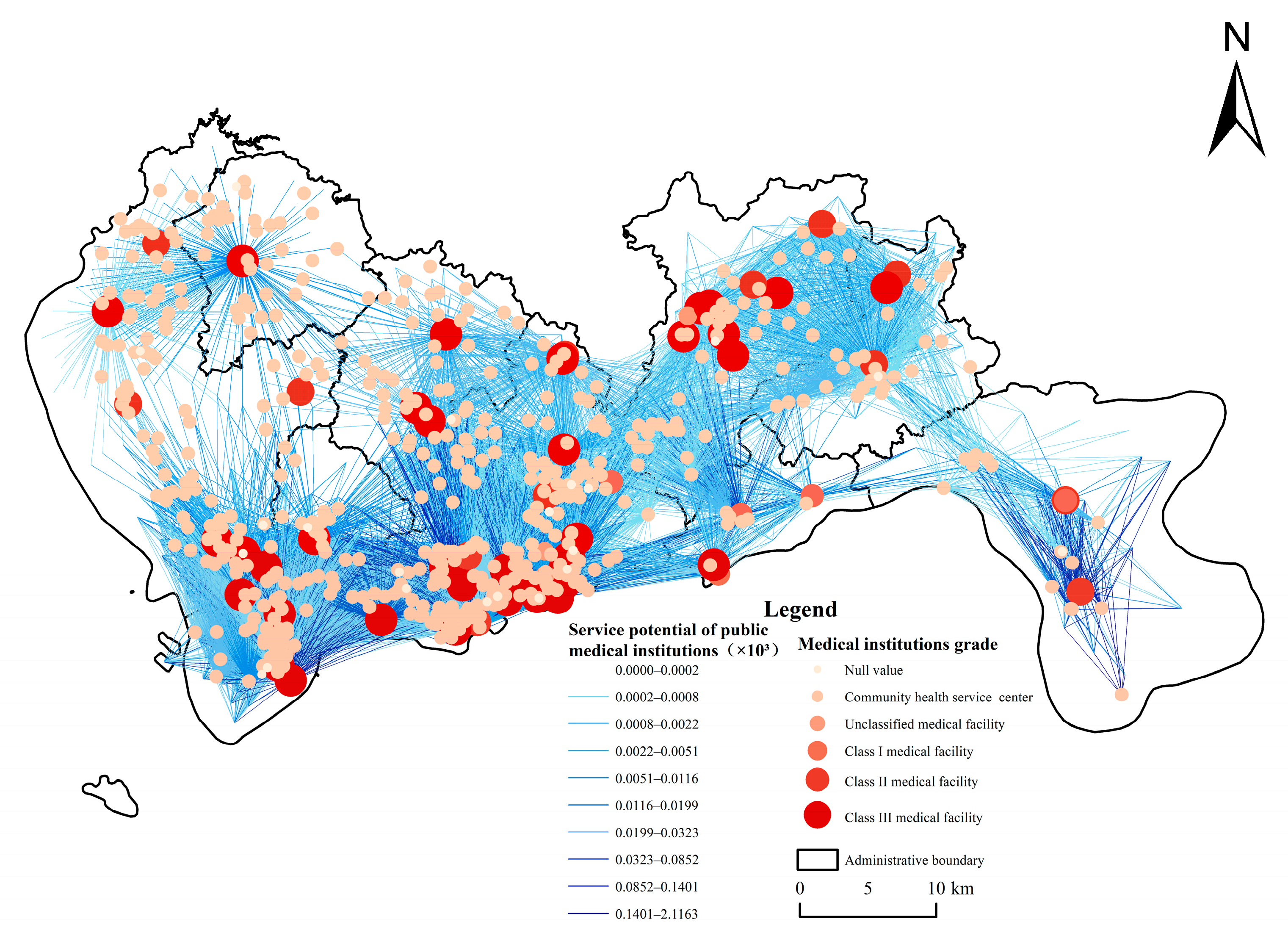
3.2. Service Potential Characteristics of Public Medical Facilities
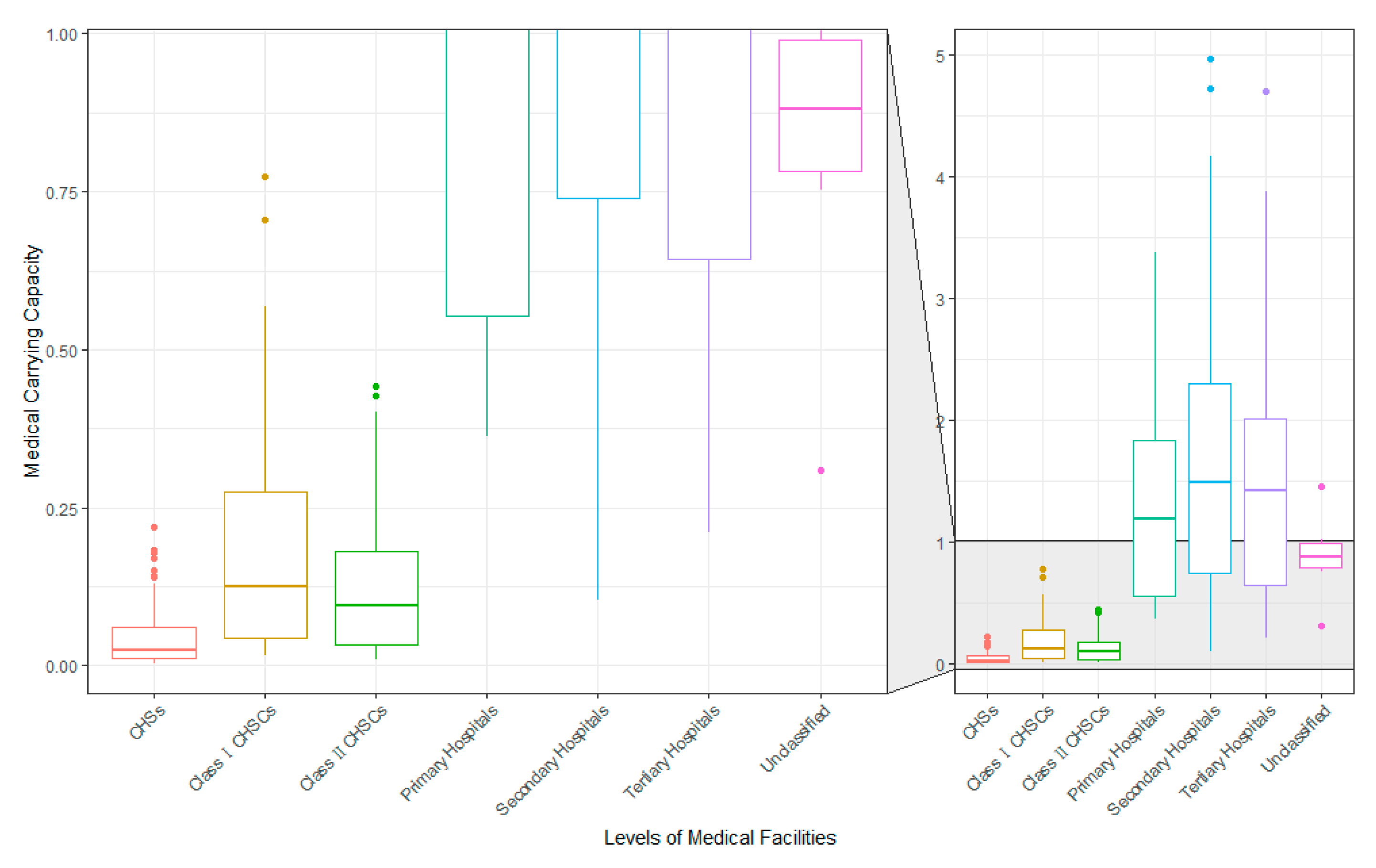
3.3. Evaluation of the Service Carrying Capacity of Public Medical Facilities
4. Discussion
4.1. Characteristics of Healthcare Resources Carrying in Shenzhen
4.2. Refined Population Portrayal
4.3. Outlook and Limitations of the Study
4.4. Policy Recommendations
5. Conclusions
- (1)
- The spatial distribution of public medical resources in Shenzhen is uneven. Medical resources generally show a blocklike aggregation and a multicenter and hierarchical development pattern, and local aggregation hotspots are scattered in different districts of the city. Specifically, these districts include the northern and southern parts of the Bao’an District, the central part of Nanshan District, Futian District, the western part of Luohu District, the northeastern part of Pingshan District, and some parts of the Longgang District.
- (2)
- The service potential of public medical facilities in Shenzhen has obvious geographical variations at the regional level due to the quality of services and the size of the radiated population. Specifically, the southwestern part of Shenzhen, such as the Futian and Nanshan Districts, and the eastern part of Shenzhen, such as the Dapeng New District, show the characteristics of a high-level gravitational value cluster. The northwestern Guangming, Bao’an, and Longhua Districts have lower gravitational value for their medical facilities.
- (3)
- Overall, public medical facilities in Shenzhen are not empty, but several public medical facilities in each district of Shenzhen, except for the Dapeng New District, are overloaded with service demands. The current spatial allocation of medical facilities is unreasonable, with large swaths of CHSCs lightly loaded due to a mismatch between residents’ preferences for medical care and the supply and demand for medical resource services. It is likely to become necessary to merge or cancel low-grade medical facilities such as CHSCs and to add high-grade medical institutions to optimize the spatial allocation pattern.
- (4)
- The incorporation of the medical institution rank factor can better express the difference in service quality provided by different levels of hospitals. In the future, merging low-utility, lightly loaded CHSCs and increasing the number of high-grade medical services will be the main direction of policy formulation. At the same time, the improved potential model and infrastructure carrying-capacity evaluation model based on the population data of mobile signaling of the TAZ can effectively express the residents’ medical behavior, and then evaluate the infrastructure carrying capacity of megacities such as Shenzhen, guide future infrastructure construction, and provide the basis for building sustainable cities and communities.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, J.; Bai, Y.; Zhang, P.; Qiu, J.; Hu, Y.; Wang, T.; Xu, C.; Gong, P. A Spatial Distribution Equilibrium Evaluation of Health Service Resources at Community Grid Scale in Yichang, China. Sustainability 2020, 12, 52. [Google Scholar] [CrossRef]
- Zhang, D.; Huang, J.; Luo, C. From “Hospital Runs” to “Health Care for All”: The Impact of the Public Health Policy Change. China J. Econ. 2021, 8, 182–206. (In Chinese) [Google Scholar] [CrossRef]
- Yin, G.; Song, H.; Wang, J.; Nicholas, S.; Maitland, E. The COVID-19 Run on Medical Resources in Wuhan China: Causes, Consequences and Lessons. Healthcare 2021, 9, 1362. [Google Scholar] [CrossRef] [PubMed]
- Carroll, N.; Conboy, K. Normalising the “New Normal”: Changing Tech-Driven Work Practices under Pandemic Time Pressure. Int. J. Inf. Manag. 2020, 55, 102186. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chen, W. The Development and Transformation of China’s Human Resource Service Industry in the Post-Epidemic Era: Based on the Context Analysis of Policies about Human Resources Service under the Normalization of Epidemic Prevention and Control. Hum. Resour. Dev. China 2020, 37, 18–32. (In Chinese) [Google Scholar] [CrossRef]
- Wu, T.; Tang, C.; Zhang, R.; Wang, X. GDCL Evaluation Method for Service Carrying Capacity of Medical Facilities from the Perspective of Residents’Choice Behavior: A Case Study of Basic Public Health Service. Geogr. Geo-Inf. Sci. 2020, 36, 64–69. [Google Scholar] [CrossRef]
- Zhang, D.; Zhang, G.; Zhou, C. Differences in Accessibility of Public Health Facilities in Hierarchical Municipalities and the Spatial Pattern Characteristics of Their Services in Doumen District, China. Land 2021, 10, 1249. [Google Scholar] [CrossRef]
- Xia, T.; Song, X.; Zhang, H.; Song, X.; Kanasugi, H.; Shibasaki, R. Measuring Spatio-Temporal Accessibility to Emergency Medical Services through Big GPS Data. Health Place 2019, 56, 53–62. [Google Scholar] [CrossRef]
- Ye, K.-H.; Lee, W.-S. Medical Accessibility Analysis by Optical Store and Ophthalmic Clinic Distribution (Centering on Special and Metropolitan Cities). J. Korean Ophthalmic Opt. Soc. 2016, 21, 159–171. [Google Scholar] [CrossRef]
- Han, C.; Wang, Y.; Qu, D.; Han, K.; Wang, J.; Zhang, Z. Study on the Dynamic Impact of the Gap between Urban and Rural Medical and Health Resources Allocation in China Based on State Space Model. Chin. J. Health Stat. 2020, 37, 757–760. (In Chinese) [Google Scholar]
- Withanachchi, N.; Uchida, Y.; Nanayakkara, S.; Samaranayake, D.; Okitsu, A. Resource Allocation in Public Hospitals: Is It Effective? Health Policy 2007, 80, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Ren, X.; Zhang, Q.; He, J.; Chen, Y. Spatial Analysis of Rural Medical Facilities Using Huff Model: A Case Study of Lankao County, Henan Province. Int. J. Smart Home 2015, 9, 161–168. [Google Scholar] [CrossRef]
- Yang, S.; Tian, S. Analysis of Health Resource Allocation Efficiency of Township Hospitals in China. Proc. J. Phys. Conf. Ser. 2021, 1774, 12021. [Google Scholar] [CrossRef]
- Chen, Y.; Yin, Z.; Xie, Q. Suggestions to Ameliorate the Inequity in Urban/Rural Allocation of Healthcare Resources in China. Int. J. Equity Health 2014, 13, 34. [Google Scholar] [CrossRef]
- Roadevin, C.; Hill, H. How Can We Decide a Fair Allocation of Healthcare Resources during a Pandemic? J. Med. Ethics 2021, 47, 84. [Google Scholar] [CrossRef]
- Fu, S.; Liu, Y.; Fang, Y. Measuring the Differences of Public Health Service Facilities and Their Influencing Factors. Land 2021, 10, 1225. [Google Scholar] [CrossRef]
- MacInko, J.; Lima-Costa, M.F. Horizontal Equity in Health Care Utilization in Brazil, 1998–2008. Int. J. Equity Health 2012, 11, 33. [Google Scholar] [CrossRef]
- Bai, X.; Cheng, Y. Differences in Regional Medical Resources Allocation, Medical Condition, and Individual Health. J. Xi’an Jiaotong Univ. (Soc. Sci.) 2019, 39, 80–89. [Google Scholar] [CrossRef]
- Wang, J.; Liu, Y. Spatial Layout Analysis of General Hospitals in Central City Districts of Tianjin Based on GIS. Geogr. Geo-Inf. Sci. 2018, 34, 25–30. (In Chinese) [Google Scholar] [CrossRef]
- Zhang, C.; Zhao, X.; Ni, J.; Wu, Y.; Li, X. Fairness Analysis of Health Resources Allocation in Sichuan Province Based on Agglomeration Degree. Mod. Prev. Med. 2020, 47, 3530–3535. (In Chinese) [Google Scholar]
- Yang, L.; Li, S. Influencing Factors and Improvement of Unbalanced Allocation of Urban and Rural Medical Resources. Econ. Perspect. 2016, 9, 57–68. (In Chinese) [Google Scholar]
- Lei, P.; Feng, Z.; Ding, J.; Duan, R.; Yu, H.; Liu, Q. Evaluation of the Status Quo of Medical Resource Allocation and Service Utilization in China. Health Econ. Res. 2019, 36, 50–55. (In Chinese) [Google Scholar]
- Zhu, L.; Zhong, S.; Tu, W.; Zheng, J.; He, S.; Bao, J.; Huang, C. Assessing Spatial Accessibility to Medical Resources at the Community Level in Shenzhen, China. Int. J. Environ. Res. Public Health 2019, 16, 242. [Google Scholar] [CrossRef] [PubMed]
- Yin, C.; He, Q.; Liu, Y.; Chen, W.; Gao, Y. Inequality of Public Health and Its Role in Spatial Accessibility to Medical Facilities in China. Appl. Geogr. 2018, 92, 50–62. [Google Scholar] [CrossRef]
- Tao, Z.; Yao, Z.; Kong, H.; Duan, F.; Li, G. Spatial Accessibility to Healthcare Services in Shenzhen, China: Improving the Multi-Modal Two-Step Floating Catchment Area Method by Estimating Travel Time via Online Map APIs. BMC Health Serv. Res. 2018, 18, 345. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.; Tao, L.; Lian, Y.; Huang, W. Measuring Spatial Accessibility of Urban Medical Facilities: A Case Study in Changning District of Shanghai in China. Int. J. Environ. Res. Public Health 2021, 18, 9598. [Google Scholar] [CrossRef]
- Qu, X.; Qi, X.; Wu, B. Disparities in Dental Service Utilization among Adults in Chinese Megacities: Do Health Insurance and City of Residence Matter? Int. J. Environ. Res. Public Health 2020, 17, 6851. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Li, S.; Liu, D. Unequable Spatial Accessibility to Hospitals in Developing Megacities: New Evidence from Beijing. Health Place 2020, 65, 102406. [Google Scholar] [CrossRef]
- Luo, J.; Chen, G.; Li, C.; Xia, B.; Sun, X.; Chen, S. Use of an E2SFCA Method to Measure and Analyse Spatial Accessibility to Medical Services for Elderly People in Wuhan, China. Int. J. Environ. Res. Public Health 2018, 15, 1503. [Google Scholar] [CrossRef]
- Cheng, L.; Yang, M.; De Vos, J.; Witlox, F. Examining Geographical Accessibility to Multi-Tier Hospital Care Services for the Elderly: A Focus on Spatial Equity. J. Transp. Health 2020, 19, 100926. [Google Scholar] [CrossRef]
- Xin, J. Measurement of Construction for Elderly-Care Facilities Based on 15-Minute Community Living Circle Planning. Remote Sens. Inf. 2019, 34, 118–223. (In Chinese) [Google Scholar] [CrossRef]
- Chen, P.T. Medical Big Data Applications: Intertwined Effects and Effective Resource Allocation Strategies Identified through IRA-NRM Analysis. Technol. Forecast. Soc. Chang. 2018, 130, 150–164. [Google Scholar] [CrossRef]
- Kong, X.; Liu, Y.; Wang, Y.; Tong, D.; Zhang, J. Investigating Public Facility Characteristics from a Spatial Interaction Perspective: A Case Study of Beijing Hospitals Using Taxi Data. ISPRS Int. J. Geo-Inf. 2017, 6, 38. [Google Scholar] [CrossRef]
- Zhou, N. Research on Urban Spatial Structure Based on the Dual Constraints of Geographic Environment and POI Big Data. J. King Saud Univ.-Sci. 2022, 34, 101887. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, N.; Luo, Y.; He, H.; Wu, L.; Wang, H.; Wang, Q.; Wu, J. Quantification of Ecosystem Services Supply-Demand and the Impact of Demographic Change on Cultural Services in Shenzhen, China. J. Environ. Manag. 2022, 304, 114280. [Google Scholar] [CrossRef]
- Tong, D.; Sun, Y.; Xie, M. Evaluation of Green Space Accessibility Based on Improved Gaussian Two-Step Floating Catchment Area Method:A Case Study of Shenzhen City, China. Prog. Geogr. 2021, 40, 1113–1126. (In Chinese) [Google Scholar] [CrossRef]
- Xu, Y.; Zhou, R.; Dai, L.; Wang, Y.; Wang, X. Spatial Differences and the Impacts of the Separation between Jobs and Residential Locations: Evidence from Household Survey Data in Luohe City. Urban Dev. Stud. 2014, 21, 52–58. (In Chinese) [Google Scholar] [CrossRef]
- Lv, Y.; Qin, Y.; Jia, L.; Dong, H.; Jia, X.; Sun, Z. Dynamic Traffic Zone Partition Based on Cluster Analysis of Taxi GPS Data. Logist. Technol. 2010, 29, 86–88. (In Chinese) [Google Scholar] [CrossRef]
- Li, X.; Yang, X.; Chen, H. Study on Traffic Zone Division Based on Spatial Clustering Analysis. Comput. Eng. Appl. 2009, 45, 19–22. [Google Scholar] [CrossRef]
- Song, L.; Zhu, J.; Liu, X.; Chen, J.; Xian, K. Optimization Method of Traffic Analysis Zones Division in Public Transit Corridor. J. Transp. Syst. Eng. Inf. Technol. 2020, 20, 34–40. (In Chinese) [Google Scholar] [CrossRef]
- Xing, X.; Huang, W.; Song, G.; Xie, K. Traffic Zone Division Using Mobile Billing Data. In Proceedings of the 2014 11th International Conference on Fuzzy Systems and Knowledge Discovery, FSKD 2014, Xiamen, China, 19–21 August 2014; pp. 692–697. [Google Scholar]
- Cheng, G.; Zeng, X.; Duan, L.; Lu, X.; Sun, H.; Jiang, T.; Li, Y. Spatial Difference Analysis for Accessibility to High Level Hospitals Based on Travel Time in Shenzhen, China. Habitat Int. 2016, 53, 485–494. [Google Scholar] [CrossRef]
- Shenzhen Bureau of Statistics. Data of the Seventh National Census of Shenzhen in 2020; Shenzhen Bureau of Statistics: Shenzhen, China, 2020. [Google Scholar]
- Hu, W.; Li, L.; Su, M. Spatial Inequity of Multi-Level Healthcare Services in a Rapid Expanding Immigrant City of China: A Case Study of Shenzhen. Int. J. Environ. Res. Public Health 2019, 16, 3441. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Du, Q.; Ren, F.; Ma, X. Assessing Spatial Accessibility to Hierarchical Urban Parks by Multi-Types of Travel Distance in Shenzhen, China. Int. J. Environ. Res. Public Health 2019, 16, 1038. [Google Scholar] [CrossRef]
- Chang, Z.; Diao, M. Inter-City Transport Infrastructure and Intra-City Housing Markets: Estimating the Redistribution Effect of High-Speed Rail in Shenzhen, China. Urban Stud. 2021, 59, 870–889. [Google Scholar] [CrossRef]
- Jin, M.; Liu, L.; Tong, D.; Gong, Y.; Liu, Y. Evaluating the Spatial Accessibility and Distribution Balance of Multi-Level Medical Service Facilities. Int. J. Environ. Res. Public Health 2019, 16, 1150. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Fu, J.; Wang, H.; Zhao, Y.; Yi, T. Identifying Spatial Matching between the Supply and Demand of Medical Resource and Accessing Carrying Capacity: A Case Study of Shenzhen, China. Int. J. Environ. Res. Public Health 2022, 19, 2354. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xie, Y.; Liu, R.; Zhang, H. Population Prediction and Resource Allocation in Megacities from the Optimum Population Perspective:A Case Study of Beijing, Shanghai, Guangzhou and Shenzhen. Acta Geogr. Sin. 2021, 76, 352–366. [Google Scholar] [CrossRef]
- Duffy, C.; Newing, A.; Górska, J. Evaluating the Geographical Accessibility and Equity of COVID-19 Vaccination Sites in England. Vaccines 2022, 10, 50. [Google Scholar] [CrossRef]
- Shenzhen Municipal Health Commission. Medical Institution Establishment Planning in Shenzhen (2016–2020); Shenzhen Municipal Health Commission: Shenzhen, China, 2017. [Google Scholar]
- He, D.; Wang, J.; Wang, X.; Xie, C.; Jin, C. The Status Quo of Development on Private Medical Institutions in China. Chin. J. Health Policy 2014, 7, 8–13. [Google Scholar] [CrossRef]
- Shenzhen Municipal Health Commission Summary of Health Statistics of Shenzhen in 2020. Available online: http://wjw.sz.gov.cn/ (accessed on 7 October 2021). (In Chinese)
- Li, X.; Chen, Y.; Zhu, Y.; Feng, J.; Liu, Z. Private Hospitals Operated in DEA-Tobit Model in Shenzhen: Operating Efficiency and Influencing Factors. Chin. J. Hosp. Adm. 2017, 33, 876–880. [Google Scholar] [CrossRef]
- Li, X.; Chen, Y.; Zhu, Y.; Feng, J.; Yang, Y.; Gao, Y.; Feng, Z. PEST-SWOT Analysis of the Development for Private Hospitals in Shenzhen City. Chin. Hosp. Manag. 2017, 37, 36–38. [Google Scholar]
- Xiao, J.; Yang, H.; Liu, R.; Chen, Q. Study on Ecological Environment of Private Hospitals. Chin. Health Econ. 2013, 32, 59–62. [Google Scholar]
- Zhao, Y.; Zhu, M. Development Trend, Difficulties and Opportunities of Private Hospitals in China. Her. Med. 2019, 38, 276–278. [Google Scholar]
- Xiao, J.; Yang, Y.; Liu, R.; Guo, J.; Chen, Q. Analysis on the Cognition of Urban Residents to Private Hospitals in the Pearl River Delta. Health Econ. Res. 2013, 3, 45–46. (In Chinese) [Google Scholar] [CrossRef]
- Shenzhen Center for Prehospital Care Introduction to Shenzhen Emergency Center. Available online: http://wjw.sz.gov.cn/szsjjzx/jggk_161338/zxjj_161339/content/post_3130351.html (accessed on 1 June 2022).
- Anderson, T.K. Kernel Density Estimation and K-Means Clustering to Profile Road Accident Hotspots. Accid. Anal. Prev. 2009, 41, 359–364. [Google Scholar] [CrossRef]
- Feng, Y.; Chen, X.; Gao, F.; Liu, Y. Impacts of Changing Scale on Getis-Ord Gi* Hotspots of CPUE: A Case Study of the Neon Flying Squid (Ommastrephes Bartramii) in the Northwest Pacific Ocean. Acta Oceanol. Sin. 2018, 37, 67–76. [Google Scholar] [CrossRef]
- Getis, A.; Aldstadt, J. Constructing the Spatial Weights Matrix Using a Local Statistic. Geogr. Anal. 2004, 36, 90–104. [Google Scholar] [CrossRef]
- Cheng, M.; Lian, Y. Spatial Accessibility of Urban Medical Facilities Based on Improved Potential Model: A Case Study of Yangpu District in Shanghai. Prog. Geogr. 2018, 37, 266–275. (In Chinese) [Google Scholar]
- Mirzahossein, H.; Sedghi, M.; Motevalli Habibi, H.; Jalali, F. Site Selection Methodology for Emergency Centers in Silk Road Based on Compatibility with Asian Highway Network Using the AHP and ArcGIS (Case Study: I. R. Iran). Innov. Infrastruct. Solut. 2020, 5, 1–14. [Google Scholar] [CrossRef]
- Song, Z.; Cheng, W.; Che, Q.; Zhang, L. Measurement of Spatial Accessibility to Health Care Facilities and Defining Health Professional Shortage Areas Based on Improved Potential Model—A Case Study of Rudong County in Jiangsu Province. Sci. Geogr. Sin. 2010, 30, 213–219. [Google Scholar] [CrossRef]
- Yang, Z.; Chen, Y.; Qian, Q.; Hu, Y.; Huang, Q. Evaluation of the Matching Degree of Public Medical Service Level Based on Population Spatialization:A Case Study of Guangzhou. Geogr. Geo-Inf. Sci. 2019, 35, 74–82. [Google Scholar] [CrossRef]
- Tong, S.; Chen, H. Evaluation of Accessibility of Medical Facilities Based on Street Scale—A Case Study in Shenzhen City. Health Econ. Res. 2017, 2, 31–34. (In Chinese) [Google Scholar] [CrossRef]
- Shenzhen Municipal People’s Government. Shenzhen Urban Planning Standards and Guidelines; Shenzhen Municipal People’s Government: Shenzhen, China, 2014. [Google Scholar]
- Zhao, N.; Shen, J.; Jia, L. An Empirical Study on Infrastructure Carrying Capacity and Carrying Condition of Beijing. Urban Stud. 2009, 16, 68–75. [Google Scholar] [CrossRef]
- Song, Y.; Yu, D. Evaluation of Comprehensive Capacity of Resources and Environments in Poyang Lake Eco-Economic Zone. Chin. J. Appl. Ecol. 2014, 25, 2975–2984. (In Chinese) [Google Scholar]
- Wu, C.; Wang, W. Evaluation of Infrastructure Carrying Capacity of National Central Cities and Diagnosis of Its Obstacles. Bull. Soil Water Conserv. 2020, 40, 260–267. (In Chinese) [Google Scholar] [CrossRef]
- Shenzhen Bureau of Statistics. Shenzhen Statistical Yearbook; China Statistics Press: Shenzhen, China, 2020; ISBN C832.653-54. [Google Scholar]
- Guo, S.; Pei, T.; Xie, S.; Song, C.; Chen, J.; Liu, Y.; Shu, H.; Wang, X.; Yin, L. Fractal Dimension of Job-Housing Flows: A Comparison between Beijing and Shenzhen. Cities 2021, 112, 103120. [Google Scholar] [CrossRef]
- Song, Y.; Chen, Y.; Pan, X. Polycentric Spatial Structure and Travel Mode Choice: The Case of Shenzhen, China. Reg. Sci. Policy Pract. 2012, 4, 479–493. [Google Scholar] [CrossRef]
- Jianatiguli, K.; Wang, X.; Meng, X. Comparative Study of Jobs-Housing Spatial Structure of Beijing and Shenzhen. Comp. Study Jobs-Hous. Spat. Struct. Beijing Shenzhen 2014, 21, 35–44. [Google Scholar] [CrossRef]
- Gharani, P.; Stewart, K.; Ryan, G.L. An Enhanced Approach for Modeling Spatial Accessibility for in Vitro Fertilization Services in the Rural Midwestern United States. Appl. Geogr. 2015, 64, 12–23. [Google Scholar] [CrossRef]
- Pu, Q.; Yoo, E.H.; Rothstein, D.H.; Cairo, S.; Malemo, L. Improving the Spatial Accessibility of Healthcare in North Kivu, Democratic Republic of Congo. Appl. Geogr. 2020, 121, 102262. [Google Scholar] [CrossRef]
- Schuurman, N.; Bérubé, M.; Crooks, V.A. Measuring Potential Spatial Access to Primary Health Care Physicians Using a Modified Gravity Model. Can. Geogr. 2010, 54, 29–45. [Google Scholar] [CrossRef]
- Liu, X.; Lin, Z.; Huang, J.; Gao, H.; Shi, W. Evaluating the Inequality of Medical Service Accessibility Using Smart Card Data. Int. J. Environ. Res. Public Health 2021, 18, 2711. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, F. Measures of Spatial Accessibility to Health Care in a GIS Environment: Synthesis and a Case Study in the Chicago Region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef] [PubMed]
- Peeters, D.; Thomas, I. Distance Predicting Functions and Applied Location-Allocation Models. J. Geogr. Syst. 2000, 2, 167–184. [Google Scholar] [CrossRef]
- Yang, N.; Chen, S.; Hu, W.; Wu, Z.; Chao, Y. Spatial Distribution Balance Analysis of Hospitals in Wuhan. Int. J. Environ. Res. Public Health 2016, 13, 971. [Google Scholar] [CrossRef] [PubMed]



| Name of Data | Contents | Source |
|---|---|---|
| Data on basic characteristics of three-tier hospitals | Including information on the name of the institution, level, category, size, number of beds, number of health technicians, address, administrative division, etc. | http://www.sz.gov.cn/ (accessed on 13 May 2021) |
| Data on basic characteristics of community health service centers (CHSCs) 1 | Including information on the name, level, address, and administrative division of the institution. | http://wjw.sz.gov.cn/ (accessed on 9 May 2021) |
| Healthcare point of interest (POI) data | Latitude and longitude information | https://www.amap.com/ (accessed on 1 May 2021) |
| Shenzhen mobile phone signaling traffic analysis zone (TAZ) data | Including TAZ vector surface data, TAZ number, population number, and population density (person/km2) data. | China Mobile Communications Group Co., Ltd. |
| Road Network Data 2 | Main Road Network | Open Street Map |
| Range of Values | Degree of Medical Resources Carrying Capacity | Status of Medical Resources |
|---|---|---|
| [0, 0.5] | Severely light load | Waste |
| (0.5, 0.8] | Moderately light load | Inefficiency |
| (0.8, 1.2] | Relatively balanced | Good elasticity |
| (1.2, 1.5] | Mild overload | General |
| (1.5, 3] | Moderate overload | Fragility |
| (3, +∞) | Severe overload | Breakdown |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, J.; Yi, T.; Wang, H.; Wang, H.; Fu, J.; Zhao, Y. Evaluation of Medical Carrying Capacity for Megacities from a Traffic Analysis Zone View: A Case Study in Shenzhen, China. Land 2022, 11, 888. https://doi.org/10.3390/land11060888
Wu J, Yi T, Wang H, Wang H, Fu J, Zhao Y. Evaluation of Medical Carrying Capacity for Megacities from a Traffic Analysis Zone View: A Case Study in Shenzhen, China. Land. 2022; 11(6):888. https://doi.org/10.3390/land11060888
Chicago/Turabian StyleWu, Jiansheng, Tengyun Yi, Han Wang, Hongliang Wang, Jiayi Fu, and Yuhao Zhao. 2022. "Evaluation of Medical Carrying Capacity for Megacities from a Traffic Analysis Zone View: A Case Study in Shenzhen, China" Land 11, no. 6: 888. https://doi.org/10.3390/land11060888






