Morphometric Evaluation of Detailed Asymmetry for the Proximal Humerus in Korean Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics and Cadaver CT Data
2.2. Methods
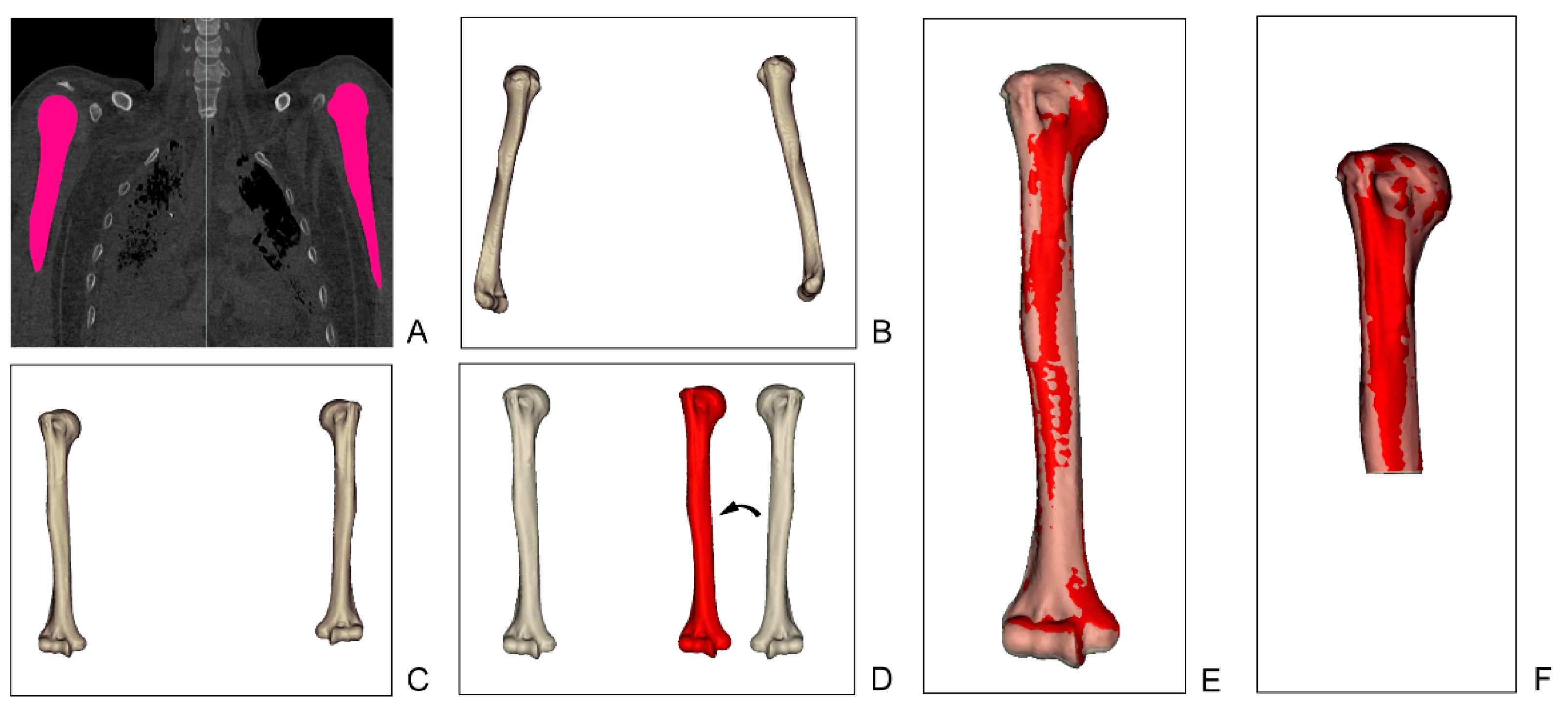
2.2.1. 3D Modeling Process
2.2.2. 3D Model Alignment and Registration
2.2.3. Measurements
2.2.4. Statistical Analysis and Data Reproducibility
3. Results
3.1. Realiability of Alighment and Registration
3.2. Length, Volume, and Surface Area of the Humerus
3.3. Shape Differences of the Humerus
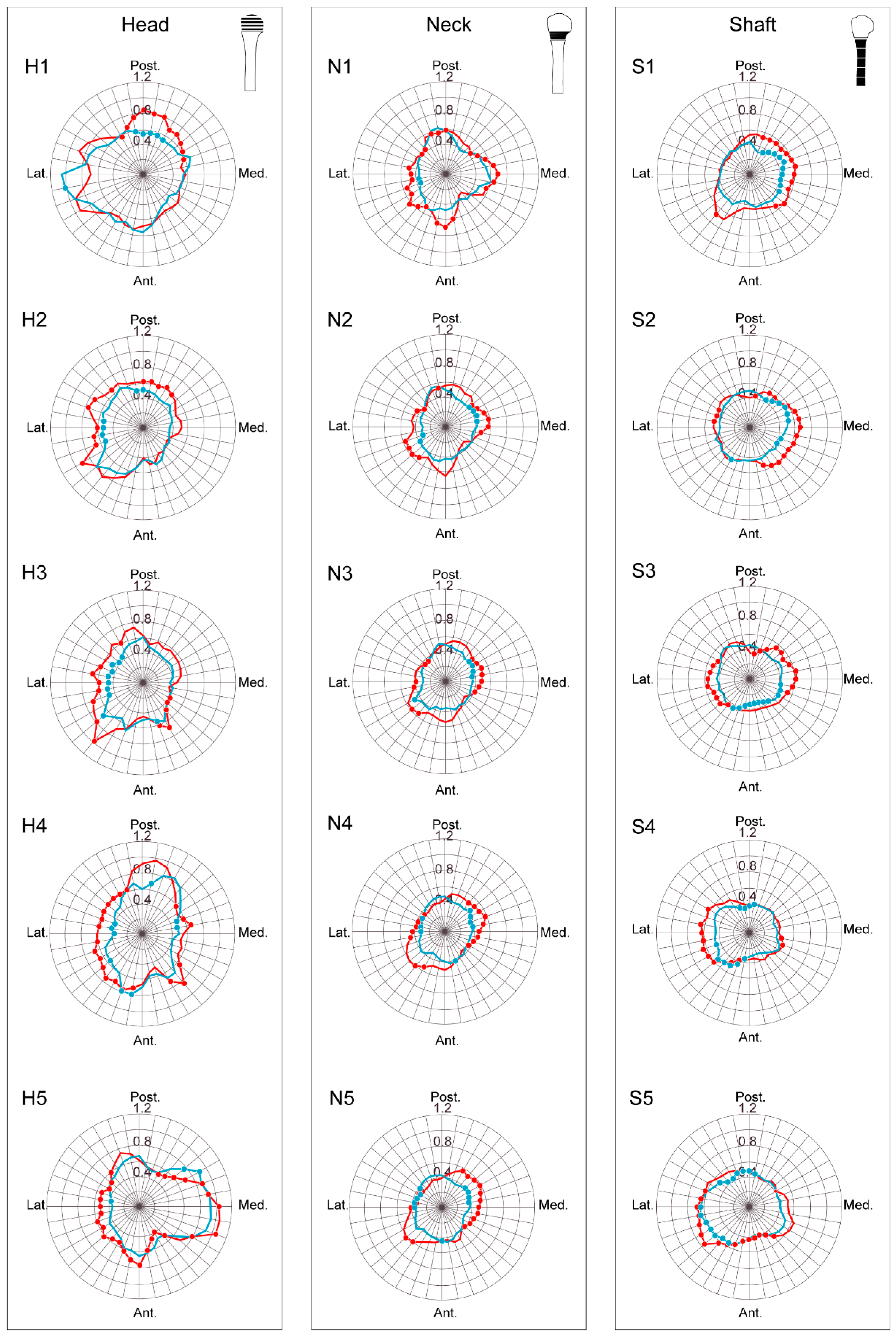
3.3.1. Head
3.3.2. Neck
3.3.3. Shaft
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rhodes, J.A.; Knüsel, C.J. Activity-related skeletal change in medieval humeri: Cross-sectional and architectural alterations. Am. J. Phys. Anthropol. 2005, 128, 536–546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kubicka, A.M.; Nowaczewska, W.; Balzeau, A.; Piontek, J. Bilateral asymmetry of the humerus in Neandertals, Australian aborigines and medieval humans. Am. J. Phys. Anthropol. 2018, 167, 46–60. [Google Scholar] [CrossRef]
- Auerbach, B.M.; Ruff, C.B. Limb bone bilateral asymmetry: Variability and commonality among modern humans. J. Hum. Evol. 2006, 50, 203–218. [Google Scholar] [CrossRef] [Green Version]
- Delude, J.A.; Bicknell, R.T.; MacKenzie, G.A.; Ferreira, L.M.; Dunning, C.E.; King, G.J.; Johnson, J.A.; Drosdowech, D.S. An anthropometric study of the bilateral anatomy of the humerus. J. Shoulder Elb. Surg. 2007, 16, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Kubicek, J.; Tomanec, F.; Cerny, M.; Vilimek, D.; Kalova, M.; Oczka, D. Recent Trends, Technical Concepts and Components of Computer-Assisted Orthopedic Surgery Systems: A Comprehensive Review. Sensors 2019, 19, 5199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugano, N. Computer-assisted orthopedic surgery. J. Orthop. Sci. 2003, 8, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Amiot, L.-P.; Poulin, F. Computed Tomography-Based Navigation for Hip, Knee, and Spine Surgery. Clin. Orthop. Relat. Res. 2004, 421, 77–86. [Google Scholar] [CrossRef] [PubMed]
- McDonald, C.P.; Beaton, B.J.; King, G.J.; Peters, T.M.; Johnson, J.A. The effect of anatomic landmark selection of the distal humerus on registration accuracy in computer-assisted elbow surgery. J. Shoulder Elb. Surg. 2008, 17, 833–843. [Google Scholar] [CrossRef] [PubMed]
- McDonald, C.P.; Peters, T.M.; King, G.J.; Johnson, J.A. Computer assisted surgery of the distal humerus can employ contralateral images for pre-operative planning, registration, and surgical intervention. J. Shoulder Elb. Surg. 2009, 18, 469–477. [Google Scholar] [CrossRef]
- Berg, P.W.L.T.; Dobbe, J.G.G.; Van Wolfswinkel, G.; Strackee, S.D.; Streekstra, G.J. Validation of the contralateral side as reference for selecting radial head implant sizes. Surg. Radiol. Anat. 2016, 38, 801–807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luenam, S.; Kosiyatrakul, A.; Hansudewechakul, C.; Phakdeewisetkul, K.; Lohwongwatana, B.; Puncreobutr, C. The Patient-Specific Implant Created with 3D Printing Technology in Treatment of the Irreparable Radial Head in Chronic Persistent Elbow Instability. Case Rep. Orthop. 2018, 2018, 9272075. [Google Scholar] [CrossRef]
- Kurki, H.K. Bilateral Asymmetry in the Human Pelvis. Anat. Rec. 2017, 300, 653–665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferràs-Tarragó, J.; Sanchis-Alfonso, V.; Ramírez-Fuentes, C.; Roselló-Añón, A.; Baixauli-García, F. A 3D-CT Analysis of Femoral Symmetry—Surgical Implications. J. Clin. Med. 2020, 9, 3546. [Google Scholar] [CrossRef]
- Mopin, C.; Chaumoître, K.; Signoli, M.; Adalian, P. Developmental stability and environmental stress: A geometric morphometrics analysis of asymmetry in the human femur. Am. J. Phys. Anthropol. 2018, 167, 144–160. [Google Scholar] [CrossRef]
- Canale, S.T.; Beaty, J.H. Campbell’s Operative Orthopaedics e-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Sanders, R. Core Knowledge in Orthopaedics: Trauma; Elsevier: Amsterdam, The Netherlands, 2008. [Google Scholar]
- Neer, C.S. Displaced proximal humeral fractures. I. Classification and evaluation. J. Bone Jt. Surg. Am. 1970, 52, 1077–1089. [Google Scholar] [CrossRef]
- Tallman, S.D.; Blanton, A.I. Distal Humerus Morphological Variation and Sex Estimation in Modern Thai Individuals. J. Forensic Sci. 2020, 65, 361–371. [Google Scholar] [CrossRef]
- Robertson, D.D.; Yuan, J.; Bigliani, L.U.; Flatow, E.L.; Yamaguchi, K. Three-Dimensional Analysis of the Proximal Part of the Humerus: Relevance to Arthroplasty. J. Bone Jt. Surg. Am. 2000, 82, 1594–1602. [Google Scholar] [CrossRef]
- Cho, S.W.; Jharia, T.K.; Moon, Y.L.; Sim, S.W.; Shin, D.S.; Bigliani, L.U. Three-dimensional templating arthroplasty of the humeral head. Surg. Radiol. Anat. 2013, 35, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-I.; Kwak, D.-S.; Han, S.-H. Sex determination using discriminant analysis of the medial and lateral condyles of the femur in Koreans. Forensic Sci. Int. 2013, 233, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.-J.; Kwak, D.-S.; Kim, I.-B. Morphometric Evaluation of Korean Femurs by Geometric Computation: Comparisons of the Sex and the Population. BioMed Res. Int. 2015, 2015, 730538. [Google Scholar] [CrossRef] [Green Version]
- Cho, H.-J.; Kim, S.; Kwak, D.-S. Morphological Study of the Anterior Surface of the Distal Radius. BioMed Res. Int. 2017, 2017, 8963768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.; Kwak, D.-S.; Kim, I.-B. Morphometric Analysis and Classification of the Cross-Sectional Shape of the C2 Lamina. BioMed Res. Int. 2017, 2017, 7276946. [Google Scholar] [CrossRef] [Green Version]
- Gray, H. Gray’s Anatomy; Arcturus Publishing: London, UK, 2009. [Google Scholar]
- Hingsammer, A.M.; Vlachopoulos, L.; Meyer, D.C.; Fürnstahl, P. Three-dimensional corrective osteotomies of mal-united clavicles-is the contralateral anatomy a reliable template for reconstruction? Clin. Anat. 2015, 28, 865–871. [Google Scholar] [CrossRef]
- Byrne, A.-M.; Impelmans, B.; Bertrand, V.; Van Haver, A.; Verstreken, F. Corrective Osteotomy for Malunited Diaphyseal Forearm Fractures Using Preoperative 3-Dimensional Planning and Patient-Specific Surgical Guides and Implants. J. Hand Surg. 2017, 42, 836.e1–836.e12. [Google Scholar] [CrossRef] [PubMed]
- Lalone, E.A.; Deluce, S.R.; Shannon, H.; King, G.J.; Johnson, J.A. Design of Anatomical Population-Based and Patient-Specific Radial Head Implants. J. Hand Surg. 2017, 42, 924.e1–924.e11. [Google Scholar] [CrossRef] [PubMed]
- Roner, S.; Bersier, P.; Fürnstahl, P.; Vlachopoulos, L.; Schweizer, A.; Wieser, K. 3D planning and surgical navigation of clavicle osteosynthesis using adaptable patient-specific instruments. J. Orthop. Surg. Res. 2019, 14, 115. [Google Scholar] [CrossRef]
- Power, J.; Loveridge, N.; Kröger, H.; Parker, M.; Reeve, J. Femoral neck cortical bone in female and male hip fracture cases: Differential contrasts in cortical width and sub-periosteal porosity in 112 cases and controls. Bone 2018, 114, 81–89. [Google Scholar] [CrossRef]
- Whitmarsh, T.; Otake, Y.; Uemura, K.; Takao, M.; Sugano, N.; Sato, Y. A cross-sectional study on the age-related cortical and trabecular bone changes at the femoral head in elderly female hip fracture patients. Sci. Rep. 2019, 9, 305. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Cheng, X.G.; Su, Y.B.; Brown, K.; Xu, L.; Li, K.; Zhang, C.X.; Duanmu, Y.Y.; Wu, X.B. Sex-related variations in cortical and trabecular bone of the femoral neck in an elderly Chinese population. Osteoporos. Int. 2017, 28, 2391–2399. [Google Scholar] [CrossRef]
- Blackburn, A. Bilateral asymmetry of the humerus during growth and development. Am. J. Phys. Anthropol. 2011, 145, 639–646. [Google Scholar] [CrossRef]
- Inyang, A.O.; Roche, S.; Sivarasu, S. An interpopulation comparison of 3-dimensional morphometric measurements of the proximal humerus. JSES Int. 2020, 4, 453–463. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yuan, B.; Wang, C.; Liu, Z. Comparison of anatomical shoulder prostheses and the proximal humeri of Chinese people. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2007, 221, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Milner, G.R.; Boldsen, J.L. Humeral and Femoral Head Diameters in Recent White American Skeletons. J. Forensic Sci. 2012, 57, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, N.; Oki, S.; Ogawa, K.; Iwamoto, T.; Ochi, K.; Sato, K.; Nagura, T. Three-dimensional anthropometric analysis of the glenohumeral joint in a normal Japanese population. J. Shoulder Elb. Surg. 2016, 25, 493–501. [Google Scholar] [CrossRef] [PubMed]

| Female | Male | Combined | |
|---|---|---|---|
| Number | 51 | 50 | 101 |
| Average age | 61.1 | 57.8 | 59.5 |
| Minimum age | 38 | 22 | 22 |
| Maximum age | 96 | 95 | 96 |
| Female | Male | Combined | p | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Length (mm) | 283.97 | 14.14 | 305.69 | 15.62 | 294.72 | 18.42 | <0.01 |
| Volume (mm3) | 119,290.83 | 16,445.40 | 170,174.38 | 25,065.72 | 144,480.71 | 33,102.80 | <0.01 |
| Surface area (mm2) | 23,101.57 | 2164.79 | 28,743.46 | 2794.92 | 25,894.58 | 3768.14 | <0.01 |
| Female | Male | |||||
|---|---|---|---|---|---|---|
| Younger (n = 20) | Elder (n = 31) | p | Younger (n = 32) | Elder (n = 18) | p | |
| Length (mm) | 279.91 | 284.32 | 0.28 | 303.48 | 307.40 | 0.40 |
| Surface area (mm2) | 22,603.87 | 23,204.86 | 0.34 | 8,325,382.89 | 5,147,540.32 | 0.08 |
| Female | Male | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Right | Left | p | Right | Left | p | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||
| Humerus | Length (mm) | 285.34 | 14.21 | 282.59 | 14.09 | 0.324 | 307.10 | 15.73 | 304.89 | 15.43 | 0.612 |
| Volume (mm3) | 117,981.70 | 20,744.26 | 117,117.84 | 18,799.50 | 0.550 | 171,242.23 | 25,012.86 | 168,751.88 | 24,031.55 | 0.433 | |
| Surface area (mm2) | 23,879.15 | 3843.24 | 23,312.96 | 3345.61 | 0.539 | 30,328.04 | 4729.69 | 29,310.09 | 3759.95 | 0.436 | |
| Female | Male | Combined | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Minimum | Maximum | Mean | Minimum | Maximum | Mean | Minimum | Maximum | |
| H1 | 0.62 | 0.39 | 1.02 | 0.67 | 0.50 | 0.94 | 0.65 | 0.49 | 0.91 |
| H2 | 0.48 | 0.34 | 0.76 | 0.57 | 0.35 | 0.90 | 0.53 | 0.36 | 0.83 |
| H3 | 0.47 | 0.35 | 0.66 | 0.56 | 0.33 | 0.97 | 0.51 | 0.36 | 0.77 |
| H4 | 0.55 | 0.35 | 0.83 | 0.64 | 0.44 | 0.96 | 0.59 | 0.44 | 0.84 |
| H5 | 0.59 | 0.35 | 0.94 | 0.62 | 0.37 | 1.05 | 0.60 | 0.42 | 0.99 |
| N1 | 0.44 | 0.33 | 0.59 | 0.50 | 0.30 | 0.67 | 0.47 | 0.35 | 0.63 |
| N2 | 0.39 | 0.29 | 0.54 | 0.46 | 0.29 | 0.62 | 0.43 | 0.33 | 0.52 |
| N3 | 0.37 | 0.28 | 0.49 | 0.44 | 0.29 | 0.55 | 0.40 | 0.32 | 0.50 |
| N4 | 0.37 | 0.30 | 0.46 | 0.44 | 0.32 | 0.58 | 0.40 | 0.33 | 0.49 |
| N5 | 0.37 | 0.30 | 0.44 | 0.44 | 0.32 | 0.60 | 0.41 | 0.33 | 0.51 |
| S1 | 0.40 | 0.30 | 0.46 | 0.48 | 0.35 | 0.61 | 0.44 | 0.36 | 0.54 |
| S2 | 0.44 | 0.38 | 0.52 | 0.49 | 0.40 | 0.63 | 0.46 | 0.41 | 0.56 |
| S3 | 0.40 | 0.31 | 0.51 | 0.47 | 0.35 | 0.58 | 0.44 | 0.35 | 0.51 |
| S4 | 0.39 | 0.28 | 0.53 | 0.44 | 0.34 | 0.61 | 0.42 | 0.32 | 0.55 |
| S5 | 0.47 | 0.37 | 0.64 | 0.52 | 0.37 | 0.74 | 0.49 | 0.37 | 0.66 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, E.; Kwak, D.-S.; Kim, I.-B. Morphometric Evaluation of Detailed Asymmetry for the Proximal Humerus in Korean Population. Symmetry 2021, 13, 862. https://doi.org/10.3390/sym13050862
Hong E, Kwak D-S, Kim I-B. Morphometric Evaluation of Detailed Asymmetry for the Proximal Humerus in Korean Population. Symmetry. 2021; 13(5):862. https://doi.org/10.3390/sym13050862
Chicago/Turabian StyleHong, Eunah, Dai-Soon Kwak, and In-Beom Kim. 2021. "Morphometric Evaluation of Detailed Asymmetry for the Proximal Humerus in Korean Population" Symmetry 13, no. 5: 862. https://doi.org/10.3390/sym13050862
APA StyleHong, E., Kwak, D.-S., & Kim, I.-B. (2021). Morphometric Evaluation of Detailed Asymmetry for the Proximal Humerus in Korean Population. Symmetry, 13(5), 862. https://doi.org/10.3390/sym13050862






