The Loss of Symmetry in Unilateral Bony Syngnathia: Case Report and Literature Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Review of Literature
2.2. Case Report
3. Results
3.1. Review of Literature
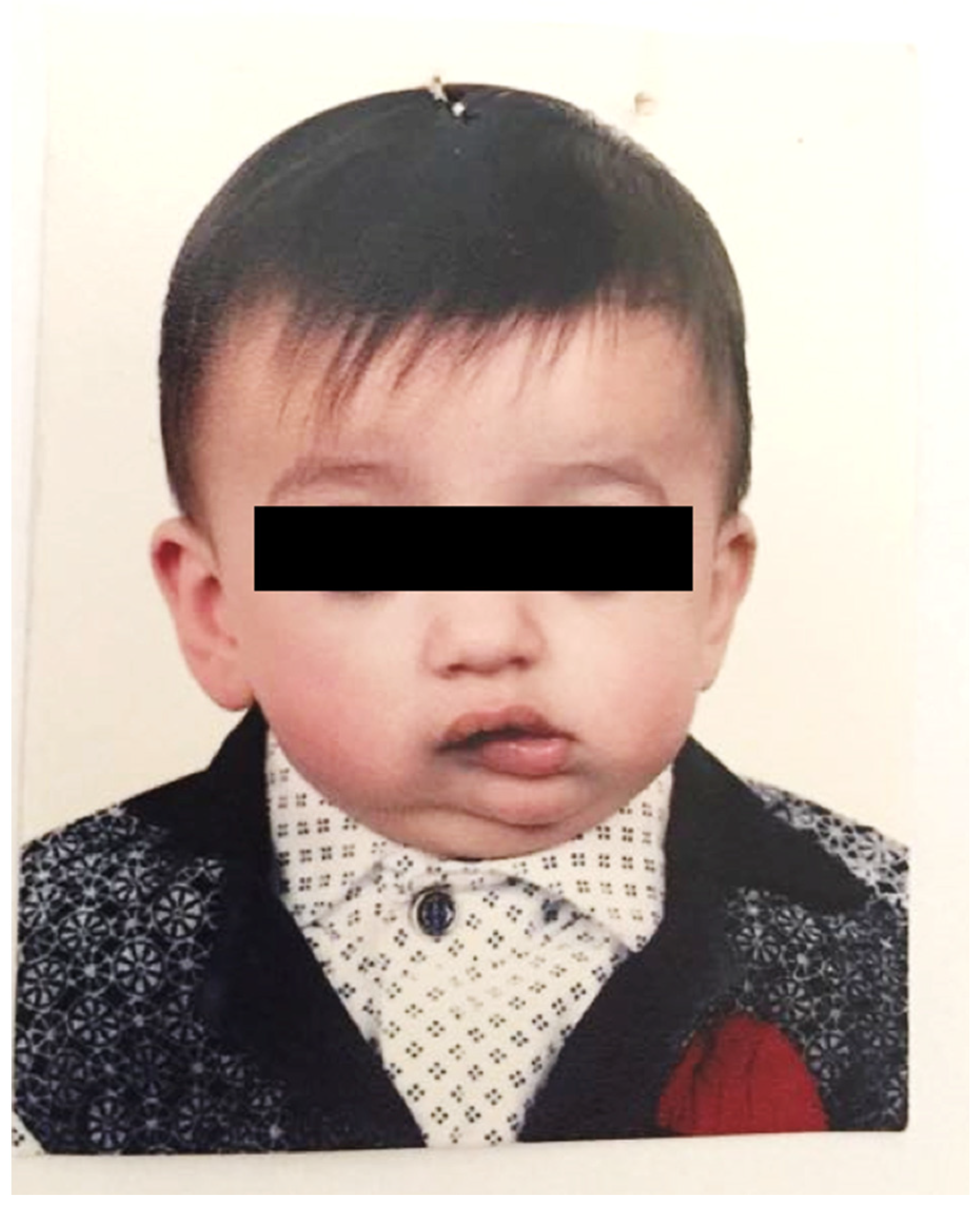
3.2. Case Report
4. Discussion
- (1)
- Planning the surgical field through a three-dimensional reconstructed CT, the only radiograph showing the entity of the bony fusion. Moreover, a facial angio-CT scan can be performed to study the cervical vascular anatomy and discard anatomical variants [22].
- (2)
- Management of upper airways and surgical time.
- (3)
- Long-term post-operative physiotherapy [3].
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ugurlu, K.; Karsidag, S.; Huthut, I.; Yildiz, K.; Bas, L. Congenital fusion of the maxilla and mandible. J. Craniofacial Surg. 2005, 16, 287–291. [Google Scholar] [CrossRef]
- Burket, L.W. Congenital bony temporomandibular ankylosis and facial hemiatrophy: Review of the literature and report of a case. J. Am. Med. Assoc. 1936, 106, 1719–1722. [Google Scholar] [CrossRef]
- Hegab, A.; ElMadawy, A.; Shawkat, W. Congenital maxillomandibular fusion: A report of three cases. Int. J. Oral Maxillofac. Surg. 2012, 41, 1248–1252. [Google Scholar] [CrossRef]
- Inman, K.E.; Purcell, P.; Kume, T.; Trainor, P.A. Interaction between Foxc1 and Fgf8 during mammalian jaw patterning and in the pathogenesis of syngnathia. PLoS Genet. 2013, 9, e1003949. [Google Scholar] [CrossRef]
- Mohan, A. Syngnathia—Congenital maxillomandibular fusion: Case report and literature review. J. Oral Maxillofac. Surg. 2018, 76, 1096.e1–1096.e6. [Google Scholar] [CrossRef]
- Campobasso, A.; Cosola, M.D.; Testa, N.F.; Lacarbonara, V.; Dioguardi, M.; Muzio, L.L.; Muzio, E.L.; Scarpa, M.; Covelli, M.; Crincoli, V.; et al. The influence of abnormal head posture on facial asymmetry. J. Biol. Regul. Homeost. Agents 2022, 36, 325–335. [Google Scholar]
- Choi, J.; Min, C.; Myoung, H.; Hwang, S.; Kim, M.; Lee, J. Acquired syngnathia. Br. J. Oral Maxillofac. Surg. 2004, 42, 448–450. [Google Scholar] [CrossRef]
- Dawson, K.H.; Gruss, J.S.; Myall, R.W. Congenital bony syngnathia: A proposed classification. Cleft Palate-Craniofacial J. 1997, 34, 141–146. [Google Scholar] [CrossRef]
- Laster, Z.; Temkin, D.; Zarfin, Y.; Kushnir, A. Complete bony fusion of the mandible to the zygomatic complex and maxillary tuberosity: Case report and review. Int. J. Oral Maxillofac. Surg. 2001, 30, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Tauro, D.P.; Kallappanavar, N.; Kiran, H.; Girhe, V.J. Congenital zygomatico-mandibular fusion (pseudo-syngnathia?) in conjunction with unilateral anophthalmia: Review of terminology and classification. Cleft Palate-Craniofacial J. 2012, 49, 626–629. [Google Scholar] [CrossRef] [PubMed]
- Olusanya, A.; Akadiri, O. Congenital syngnathia: Review of clinical profile and proposal of a new classification-based management protocol. Int. J. Oral Maxillofac. Surg. 2020, 49, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Rattan, V.; Rai, S. Congenital maxillomandibular syngnathia: Review of literature and proposed new classification system. J. Maxillofac. Oral Surg. 2021, 20, 19–36. [Google Scholar] [CrossRef]
- Broome, M.; Vial, Y.; Jacquemont, S.; Sergi, C.; Kamnasaran, D.; Giannoni, E. Complete maxillo-mandibular syngnathia in a newborn with multiple congenital malformations. Pediatrics Neonatol. 2016, 57, 65–68. [Google Scholar] [CrossRef]
- Vahidi, K.; Joe, B.N.; Glenn, O.A.; Barkovich, A.J.; Filly, R.; Ball, R.; Coakley, F.V. Prenatal imaging of congenital maxillomandibular fusion: Case report and review of the literature. J. Ultrasound Med. 2007, 26, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.; Oak, S.; Wagh, M.; Kulkarni, B. Congenital midline palatomandibular bony fusion with a mandibular cleft and a bifid tongue. Br. J. Plast. Surg. 1997, 50, 139–141. [Google Scholar] [CrossRef]
- Knoll, B.; Karas, D.; Persing, J.A.; Shin, J. Complete congenital bony syngnathia in a case of oromandibular limb hypogenesis syndrome. J. Craniofacial Surg. 2000, 11, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.K.; Jadhav, V.; Gupta, A.; Sanghvi, B.; Shah, H.; Parelkar, S. Congenital alveolar fusion. J. Pediatric Surg. 2008, 43, 1421–1425. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, B.; Agrawal, K.; Panda, K. Congenital fusion of the jaws: A management protocol. Int. J. Oral Maxillofac. Surg. 2010, 39, 925–929. [Google Scholar] [CrossRef] [PubMed]
- El-Hakim, I.; Al-Sebaei, M.; Abuzennada, S.; AlYamani, A. Congenital fusion of the maxilla and mandible (congenital bony syngnathia). Int. J. Oral Maxillofac. Surg. 2010, 39, 933–936. [Google Scholar] [CrossRef]
- Konas, E.; Aliyev, A.; Tunçbilek, G. Congenital maxillomandibular syngnathia: A new management technique using distraction techniques. J. Craniofacial Surg. 2015, 26, e68–e70. [Google Scholar] [CrossRef] [PubMed]
- Desai, J.; Smit, C.; Naidoo, S. Release of syngnathia by anticlockwise rotation and mandibular advancement using bilateral alloplastic temporomandibular joint prostheses: A new approach. Br. J. Oral Maxillofac. Surg. 2018, 56, 750–752. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Palau, J.; Prieto-Gundin, A.; de Abreu Graterol, L.M.; Vercruysse Jr, H. Maxillomandibular syngnathia: 3D planning and review of the literature. Craniomaxillofacial Trauma Reconstr. 2018, 11, 124–130. [Google Scholar] [CrossRef]
- Alfery, D.D.; Ward, C.; HARWOOD, I.R.; MANNINO, F.L. Airway management for a neonate with congenital fusion of the jaws. J. Am. Soc. Anesthesiol. 1979, 51, 340–342. [Google Scholar] [CrossRef]
- Brown, T.; Dwyer, M. The problems of anaesthesia for a neonate with fused jaws. Anaesthesia 1985, 40, 597–598. [Google Scholar] [CrossRef] [PubMed]
- Mattos, C.; Vilani, G.; Sant’Anna, E.; Ruellas, A.; Maia, L. Effects of orthognathic surgery on oropharyngeal airway: A meta-analysis. Int. J. Oral Maxillofac. Surg. 2011, 40, 1347–1356. [Google Scholar] [CrossRef]
- Ciavarella, D.; Parziale, V.; Mastrovincenzo, M.; Palazzo, A.; Sabatucci, A.; Suriano, M.M.; Bossù, M.; Cazzolla, A.P.; Lo Muzio, L.; Chimenti, C. Condylar Position Indicator and T-Scan system II in clinical evaluation of temporomandibular intracapsular disease. J. Cranio-Maxillofac. Surg. 2012, 40, 449–455. [Google Scholar] [CrossRef] [PubMed]




| Authors | Country | Gender | Age | Dawson | Laster | Notes | |
|---|---|---|---|---|---|---|---|
| 1 | Burket L.W. (1936) [2] | USA | Male | Newborn | 2b | 2b | Association with Horner syndrome and hemifacial hemiatrophy |
| 2 | Patterson G. (1961) | Sweden | Male | 1 day | 2a | 2b | Association with hypoglossia |
| 3 | Salleh N.M. (1965) | Malaysia | Female | N.S. | 1 | N.S. | / |
| 4 | Hoggins G.S. (1969) | Jamaica | Male | Newborn | 2a | 1b | Association with aglossia and syndactylia |
| 5 | Alvarez G.E. (1976) | N.S. | N.S. | Newborn | 2a | 2b | Association with aglossia-adactylia syndrome |
| 6 | Shah R.M. (1977) | Canada | Male | Embryo | 2a | 2b | Association with partial aglossia and cleft palate |
| 7 | Myskiniar S.A. (1979) | Iran | Female | 3 weeks | 1 | 1a | / |
| 8 | Dobrow B. (1983) | N.S. | Female | Newborn | 2a | N.S. | Association with aglossia, coloboma, right choanal stenosis, hemivertebrae |
| 9 | Brown T.C.K. (1984) | USA | Male | 6 months | N.S. | N.S. | Association with hypoglossia |
| 10 | Simpson J.R., Maves M.D. (1985) | USA | Female | Newborn | 2b | 2b | Association with hypoglossia and asymmetry of calvarium |
| 11 | Nwoku A.L., Kekere-Ekun T.A. (1986) | Nigeria | Female | 12 days | 1 | 2a | / |
| 12 | Goodacre T.E., Wallace A.F. (1990) | Holland | Female | 39 years | 1 | 1b | / |
| 13 | Brown D.M., Marsh J.L. (1990) | USA | Male | Newborn | 2b | 2b | Association with low-set dysplastic ears, Dandy–Walker malformation, tetralogy of Fallot |
| 14 | Agrawal K. et al. (1993) | India | Female | Newborn | 1 | 1a | / |
| 15 | Gartlan M.G. et al. (1993) | USA | Female | Newborn | 2a | 2b | / |
| 16 | Arshad A.R., Goh C.S. (1994) | Malaysia | Male | 7 days | 2b | 1a | Association with hypoglossia congenita |
| 17 | Behnia H., Shamse M.G. (1996) | Iran | Male | 5 days | 2b | 2b | Association with pectus excavatum and other facial anomalies |
| 18 | Kamata S. et al. (1996) | Japan | Male | 18 months | 2b | 2a | Association with low-set ears |
| 19 | Dawson K.H. et al. (1997) [8] | USA | Male | 5 years | 2a | 2b | Association with aglossia-adctylia syndrome |
| 20 | Dawson K.H. et al. (1997) [8] | USA | Male | 1 week | 2b | 2a | Association with hemifacial microsomia, trisomy 8, hypothyroidism, type I diabetes |
| 21 | Dawson K.H. et al. (1997) [8] | USA | Male | Newborn | 2b | 2b | Association with hemifacial hypoplasia |
| 22 | Dawson K.H. et al. (1997) [8] | USA | Male | Newborn | 2b | 2b | Association with hemifacial hypoplasia |
| 23 | Dawson K.H. et al. (1997) [8] | USA | Female | 6 months | 2b | 2b | Association with Nager syndrome |
| 24 | Rao S. et al. (1997) [15] | India | Female | Newborn | 2b | 2a | Association with mandibular cleft and bifid tongue |
| 25 | Ugurlu K. et al. (1999) | Turkey | Male | Newborn | 1 | 1a | Consanguineous parents. Association with hypoglossia and hypertelorism |
| 26 | Knoll B. et al. (2000) [16] | USA | Female | Newborn | 2a | 1b | Association with oromandibuar limb hypogenesis syndrome |
| 27 | Yazdi I., Fakhraee A.H. (2000) | Iran | Female | Newborn | 1 | 1a | / |
| 28 | Laster Z. et al. (2001) [9] | Israel | Male | Newborn | 2b | 2b | Association with other craniofacial deformities |
| 29 | Verloes A. et al. (2004) | France | Female | Newborn | 2b | 2b | Association with Dobrow syndrome |
| 30 | Daniels J.S. (2004) | USA | Female | Newborn | 1 | 2a | Association with micrognathism and proptosis of both eyes |
| 31 | Ugurlu K. et al. (2005) | Turkey | Male | 4 years | 2b | 2a | Association with mandible hypoplasia |
| 32 | Mir M. et al. (2006) | India | Male | Newborn | 1 | 1a | Consanguineous parents |
| 33 | Shams M.G. et al. (2006) | Iran | Male | 1 year | 1 | 1a | / |
| 34 | Nikolic S. et al. (2006) | Serbia and Montenegro | Male | 20 days | 1 | 1a | / |
| 35 | Trigg D.J. et al. (2007) | USA | Female | Newborn | 2a | 1b | Association with aglossia |
| 36 | Vahidi K. et al. (2007) [14] | USA | Female | Newborn | 2b | 2a | / |
| 37 | Gupta R.K. et al. (2007) [17] | India | Female | Newborn | 1 | 1a | / |
| 38 | Ramachandra Reddy G.V. et al. (2008) | India | Female | 2 years | 1 | 1a | / |
| 39 | Ajike S.O. et al. (2008) | Nigeria | Female | Newborn | 2a | 1a | Association with pectus excavatum and craniosynostosis |
| 40 | Foroutan H.R. et al. (2009) | Iran | Male | Newborn | 1 | 2b | / |
| 41 | Villaneuva-Garcia et al. (2009) | Mexico | Female | Newborn | 2a | 2b | Consanguineous parents |
| 42 | Naikmasur V.G. et al. (2009) | India | Female | 60 years | 1 | 1a | / |
| 43 | Poovazhagi V. et al. (2009) | India | N.S. | Newborn | 1 | 1a | Consanguineous parents |
| 44 | Koeda S. et al. (2010) | Japan | Female | 8 years | 1 | 2a | Association with congenital corneal opacity |
| 45 | Subramanian B. et al. (2010) [18] | India | Female | 9 months | 1 | 1a | / |
| 46 | Subramanian B. et al. (2010) [18] | India | Male | 3 months | 1 | 1a | / |
| 47 | Subramanian B. et al. (2010) [18] | India | Male | 2 days | 1 | 1a | / |
| 48 | Subramanian B. et al. (2010) [18] | India | Male | 2 days | 1 | 1b | / |
| 49 | Fallahi H.R. et al. (2010) | Iran | Female | 6 months | 2b | 2a | Association with earlobe deformity and abnormal lateral chantal fissure |
| 50 | El-Hakim I.E. et al. (2010) [19] | Saudi Arabia | Male | 2 years | 2b | 2a | / |
| 51 | Halli R. et al. (2010) | India | Male | 8 years | 2b | 2b | Association with hemifacial hypoplasia, everted lower lip |
| 52 | Martin L.P. et al. (2011) | Spain | Female | 2 months | 2b | 2b | Association with frontonasal malformation, macrostomia, retrognathia, bifid tongue, hypophyseal duplication, corpus callosum agenesis |
| 53 | Hegab A. et al. (2012) [3] | Egypt | Female | 4 months | 2b | 2a | Consanguineous parents |
| 54 | Hegab A. et al. (2012) [3] | Egypt | Male | 3 months | 1 | 1a | Consanguineous parents |
| 55 | Hegab A. et al. (2012) [3] | Egypt | Male | 3 years | 2b | 2a | / |
| 56 | Tauro D.P. et al. (2012) [10] | India | Male | 18 days | 2b | 2a | Association with unilateral anophthalmia |
| 57 | Kim CH, KimMY (2012) | Korea | Female | 74 years | 1 | 1a | / |
| 58 | Rahaman M.M. et al. (2013) | Bangladesh | Female | 11 years | 1 | 2a | Consanguineous parents |
| 59 | Broome M. et al. (2013) | Africa | Male | Newborn | 2b | 2b | Association with cleft palate, choanal atresia, deafness, delayed cerebral white matter development and genital and limb malformations. |
| 60 | Shao X., Yang G. (2014) | China | Female | 42 days | 1 | 1a | / |
| 61 | Hamed M.S., Prasad P. (2014) | UAE | Male | Newborn | 1 | 1a | Consanguineous parents |
| 62 | El-Madi A., Bouabdallah Y. (2014) | Morocco | Female | Newborn | 1 | 1a | Association with hypoplasia of the ascending branches of the mandible |
| 63 | Konas E. et al. (2015) [20] | Turkey | Female | 12 days | 2b | 2b | Association with hypoglossia |
| 64 | Al-Mahdi A.H. (2015) | Iraq | Male | Newborn | 2b | 2a | Consanguineous parents |
| 65 | Shukri Raban M. et al. (2015) | South Africa | Male | Newborn | 2b | 2a | Association with craniosynostosis, ventriculomegaly, microcephaly, bilateral cataracts, facial dysmorphism, small kidneys, hypoplastic prepuce of the genitalia and bilateral syndactyly of toes 2, 3 and 4 |
| 66 | Mehdizadeh M. et al. (2015) | Afghanistan | Female | Newborn | 1 | 1a | / |
| 67 | Kumar S. et al. (2016) | India | Female | 25 years | 1 | 2a | / |
| 68 | Rough J. et al. (2016) | USA | Male | Newborn | 2b | 2a | Association with abdominal omphalocele and with grade III heart murmur and atrial septal defect |
| 69 | Khasgiwala A. et al. (2016) | India | Male | Newborn | 1 | 1b | Association with tracheoesophageal fistula |
| 70 | Patel K., Ponde V. (2016) | India | Female | 4 months | 1 | 1a | / |
| 71 | James O. et al. (2016) | Nigeria | Female | 40 years | 1 | 2b | / |
| 72 | Sarin Y.K. et al. (2017) | India | Female | Newborn | 2b | 2b | / |
| 73 | Rubio-Palau J. et al. (2017) | Senegal | Male | 15 years | 2b | 2b | Association with palatal cleft and hemifacial microsomia. Consanguineous parents |
| 74 | Ozel A. et al. (2017) | Turkey | Male | Newborn | 2b | 2a | Consanguineous parents |
| 75 | Desai J. et al. (2018) [21] | South Africa | Male | 19 years | 2b | 2b | Association with Pierre Robin syndrome |
| 76 | Mohan A. (2018) [5] | Iran | Female | 6 months | 2b | 2a | Association with earlobe deformity |
| 77 | Olusanya A.A. et al. (2018) | Nigeria | Female | Newborn | 1 | 1a | / |
| 78 | Martinez-Tafalla Lopez et al. (2018) | Spain | N.S. | Newborn | 1 | 1a | Article in Spanish |
| 79 | Duro A.E. et al. (2018) | Argentina | Female | 40 weeks | 2a | 2b | Association with low set ears |
| 80 | Cespedes Casas M.C. et al. (2018) | Taiwan | N.S. | Newborn | N.S. | N.S. | Association with agenesis of corpus callosum |
| 81 | Khan M.N. et al. (2018) | Pakistan | Female | 8 months | N.S. | N.S. | / |
| 82 | Lin L.Q. et al. (2019) | China | Female | 7 months | 2b | 2b | / |
| 83 | Decaux J. et al. (2019) | Africa | Male | Newborn | 2b | 2a | Mother HIV + |
| 84 | Zhu W. et al. (2020) | USA | N.S. | Newborn | 2b | 2a | / |
| 85 | Maximo G. et al. (2020) | Brazil | Female | 41 days | 1 | 1a | Association with oromandibular hypogenesis syndrome |
| 86 | DeMarsh S.J. et al. (2021) | USA | Male | Newborn | 2b | 2b | Association with X-linked Cornelia de Large syndrome |
| 87 | Raiteb M. et al. (2021) | Morocco | Female | 14 months | 2b | 2a | Association with low set ears. Consanguineous parents |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crincoli, V.; Cortelazzi, R.; De Biase, C.; Cazzolla, A.P.; Campobasso, A.; Dioguardi, M.; Piancino, M.G.; Mattia, L.; Di Comite, M. The Loss of Symmetry in Unilateral Bony Syngnathia: Case Report and Literature Review. Symmetry 2022, 14, 2008. https://doi.org/10.3390/sym14102008
Crincoli V, Cortelazzi R, De Biase C, Cazzolla AP, Campobasso A, Dioguardi M, Piancino MG, Mattia L, Di Comite M. The Loss of Symmetry in Unilateral Bony Syngnathia: Case Report and Literature Review. Symmetry. 2022; 14(10):2008. https://doi.org/10.3390/sym14102008
Chicago/Turabian StyleCrincoli, Vito, Roberto Cortelazzi, Corrado De Biase, Angela Pia Cazzolla, Alessandra Campobasso, Mario Dioguardi, Maria Grazia Piancino, Luigi Mattia, and Mariasevera Di Comite. 2022. "The Loss of Symmetry in Unilateral Bony Syngnathia: Case Report and Literature Review" Symmetry 14, no. 10: 2008. https://doi.org/10.3390/sym14102008





