The Effect of Vibration Massage on Fatigue of the Upper Trapezius Muscle during Different Tasks
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Apparatus
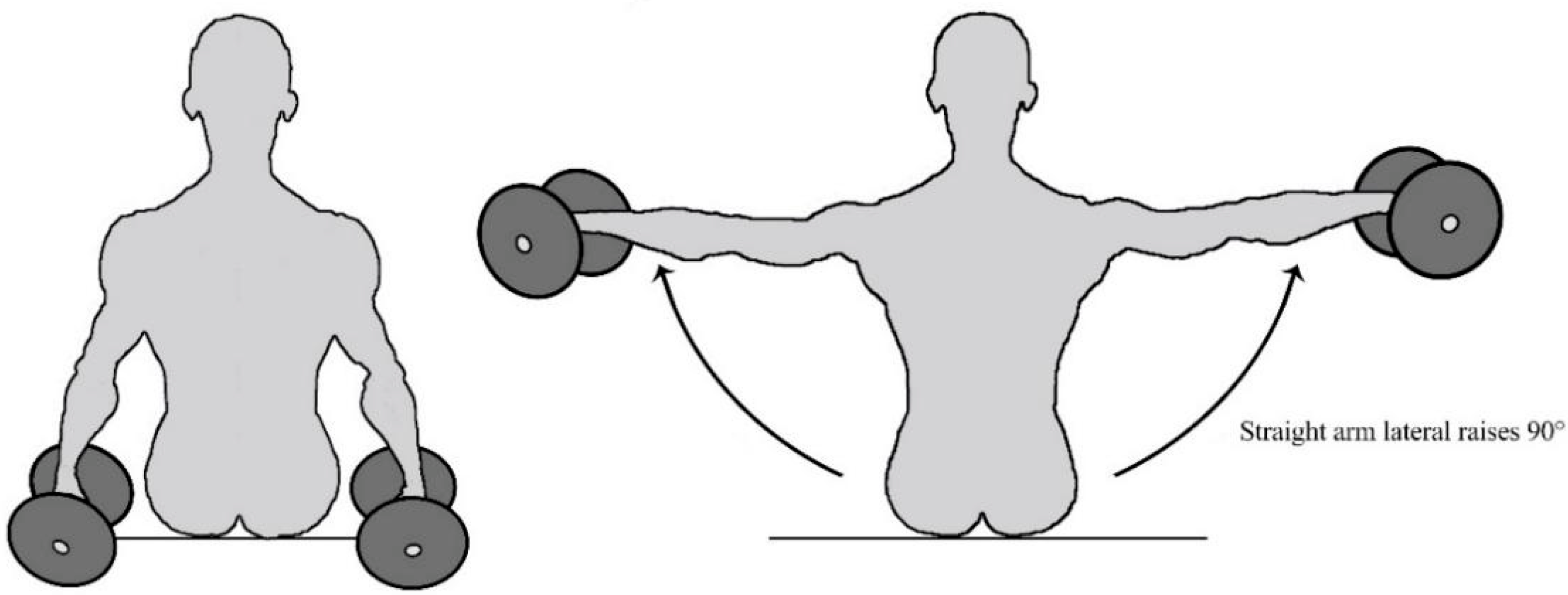
2.3. Experimental Design and Procedure
2.4. Data Analysis and Processing
2.4.1. Selection of Features
2.4.2. Feature Extraction
2.4.3. Statistical Analysis
2.4.4. Classification Models
3. Results
3.1. Analysis of UT Muscle Fatigue and Vibration Massage Intensity Results
3.2. Massage Scheme Recognition Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Santos, J.; Baptista, J.S.; Monteiro, P.R.R.; Miguel, A.S.; Santos, R.; Vaz, M.A. The influence of task design on upper limb muscles fatigue during low-load repetitive work: A systematic review. Int. J. Ind. Ergon. 2016, 52, 78–91. [Google Scholar] [CrossRef] [Green Version]
- Mathiassen, S.E. Diversity and variation in biomechanical exposure: What is it, and why would we like to know? Appl. Ergon. 2006, 37, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Nussbaum, M.A.; Clark, L.L.; Lanza, M.A.; Rice, K.M. Fatigue and Endurance Limits During Intermittent Overhead Work. AIHAJ Am. Ind. Hyg. Assoc. 2001, 62, 446–456. [Google Scholar] [CrossRef]
- Lomond, K.V.; Côté, J.N. Shoulder functional assessments in persons with chronic neck/shoulder pain and healthy subjects: Reliability and effects of movement repetition. Work 2011, 38, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Telaprolu, N.; Anne, S.D. Physical and psychological work demands as potential risk factors for musculoskeletal disorders among workers in weaving operations. Indian J. Occup. Environ. Med. 2014, 18, 129–134. [Google Scholar] [CrossRef] [Green Version]
- Gangopadhyay, S.; Ghosh, T.; DAS, T.; Ghoshal, G.; DAS, B.B. Prevalence of Upper Limb Musculo Skeletal Disorders among Brass Metal Workers in West Bengal, India. Ind. Health 2007, 45, 365–370. [Google Scholar] [CrossRef] [Green Version]
- Luger, T.; Bosch, T.; Hoozemans, M.; De Looze, M.; Veeger, D. Task variation during simulated, repetitive, low-intensity work—Influence on manifestation of shoulder muscle fatigue, perceived discomfort and upper-body postures. Ergonomics 2015, 58, 1851–1867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mork, P.J.; Westgaard, R.H. Long-term electromyographic activity in upper trapezius and low back muscles of women with moderate physical activity. J. Appl. Physiol. 2005, 99, 570–578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarker, P.; Norasi, H.; Koenig, J.; Hallbeck, M.S.; Mirka, G. Effects of break scheduling strategies on subjective and objective measures of neck and shoulder muscle fatigue in asymptomatic adults performing a standing task requiring static neck flexion. Appl. Ergon. 2020, 92, 103311. [Google Scholar] [CrossRef] [PubMed]
- Van Rijn, R.M.; Huisstede, B.M.; Koes, B.; Burdorf, A. Associations between work-related factors and specific disorders of the shoulder—A systematic review of the literature. Scand. J. Work. Environ. Health 2010, 36, 189–201. [Google Scholar] [CrossRef]
- Kim, J.Y.; Park, J.S.; Kim, D.J.; Im, S. Evaluation of fatigue patterns in individual shoulder muscles under various external conditions. Appl. Ergon. 2020, 91, 103280. [Google Scholar] [CrossRef] [PubMed]
- Côté, J.N. Adaptations to Neck/Shoulder Fatigue and Injuries. In Progress in Motor Control. Vol 826. Advances in Experimental Medicine and Biology; Levin, M.F., Ed.; Springer: New York, NY, USA, 2014; pp. 205–228. [Google Scholar] [CrossRef]
- Keir, P.J.; Sanei, K.; Holmes, M.W. Task rotation effects on upper extremity and back muscle activity. Appl. Ergon. 2011, 42, 814–819. [Google Scholar] [CrossRef]
- Lee, C.-L.; Lu, S.-Y.; Sung, P.-C.; Liao, H.-Y. Working height and parts bin position effects on upper limb muscular strain for repetitive hand transfer. Int. J. Ind. Ergon. 2015, 50, 178–185. [Google Scholar] [CrossRef]
- Nimbarte, A.D. Risk of neck musculoskeletal disorders among males and females in lifting exertions. Int. J. Ind. Ergon. 2014, 44, 253–259. [Google Scholar] [CrossRef]
- Lee, S.; Choi, Y.-H.; Kim, J. Effects of the cervical flexion angle during smartphone use on muscle fatigue and pain in the cervical erector spinae and upper trapezius in normal adults in their 20s. J. Phys. Ther. Sci. 2017, 29, 921–923. [Google Scholar] [CrossRef] [Green Version]
- Richter, H.O.; Zetterberg, C.; Forsman, M. Trapezius muscle activity increases during near work activity regardless of accommodation/vergence demand level. Eur. J. Appl. Physiol. 2015, 115, 1501–1512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fei-Ruo, Z.; Li-Hua, H.; Shan-Shan, W.; Jing-Yun, L.; Kang-Pin, Y.; Sheng, W. Quantify work load and muscle functional activation patterns in neck-shoulder muscles of female sewing machine operators using surface electromyogram. Chin. Med. J. 2011, 124, 3731–3737. [Google Scholar]
- Padilha, U.C.; Vieira, A.; Vieira, D.C.L.; De Lima, F.D.; Junior, V.A.R.; Tufano, J.J.; Bottaro, M. Could inter-set stretching increase acute neuromuscular and metabolic responses during resistance exercise? Eur. J. Transl. Myol. 2019, 29, 8579. [Google Scholar] [CrossRef] [PubMed]
- Mika, A.; Mika, P.; Fernhall, B.; Unnithan, V.B. Comparison of Recovery Strategies on Muscle Performance After Fatiguing Exercise. Am. J. Phys. Med. Rehabil. 2007, 86, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Hohenauer, E.; Taeymans, J.; Baeyens, J.-P.; Clarys, P.; Clijsen, R. The Effect of Post-Exercise Cryotherapy on Recovery Characteristics: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0139028. [Google Scholar] [CrossRef] [PubMed]
- Eguchi, Y.; Jinde, M.; Murooka, K.; Konno, Y.; Ohta, M.; Yamato, H. Stretching versus transitory icing: Which is the more effective treatment for attenuating muscle fatigue after repeated manual labor? Eur. J. Appl. Physiol. 2014, 114, 2617–2623. [Google Scholar] [CrossRef] [PubMed]
- Lau, W.Y.; Nosaka, K. Effect of Vibration Treatment on Symptoms Associated with Eccentric Exercise-Induced Muscle Damage. Am. J. Phys. Med. Rehabil. 2011, 90, 648–657. [Google Scholar] [CrossRef] [PubMed]
- Oliveri, D.J.; Lynn, K.; Hong, C.-Z. Increased Skin Temperature after Vibratory Stimulation. Am. J. Phys. Med. Rehabil. 1989, 68, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Hausswirth, C.; Le Meur, Y. Physiological and nutritional aspects of post-exercise recovery: Specific recommendations for female athletes. Sports Med. 2011, 41, 861–882. [Google Scholar] [CrossRef] [PubMed]
- Iii, E.B.L.; Sackiriyas, K.S.B.; Bains, G.S.; Calandra, G.; Lobo, C.; Nakhro, D.; Malthankar, G.; Paul, S. A comparison of whole body vibration and moist heat on lower extremity skin temperature and skin blood flow in healthy older individuals. Med. Sci. Monit. 2012, 18, CR415–CR424. [Google Scholar] [CrossRef] [Green Version]
- Chwała, W.; Pogwizd, P.; Rydzik, Ł.; Ambroży, T. Effect of Vibration Massage and Passive Rest on Recovery of Muscle Strength after Short-Term Exercise. Int. J. Environ. Res. Public Health 2021, 18, 11680. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.; Zhao, Y.; Hu, S.; Wang, Q.; Semeah, L.M.; Jia, H.; Lv, T.; Li, X.; Wang, R. Immediate Effect of Local Vibration Therapy for Sport-induced Fatigue Based on Traditional Chinese Medicine’s Holistic Theory. J. Multidiscip. Health 2020, 13, 1993–2001. [Google Scholar] [CrossRef]
- Lurie, R.C.; Cimino, S.R.; Gregory, D.E.; Brown, S. The effect of short duration low back vibration on pain developed during prolonged standing. Appl. Ergon. 2018, 67, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Koumantakis, G.A.; Roussou, E.; Angoules, G.A.; Angoules, N.A.; Alexandropoulos, T.; Mavrokosta, G.; Nikolaou, P.; Karathanassi, F.; Papadopoulou, M. The immediate effect of IASTM vs. Vibration vs. Light Hand Massage on knee angle repositioning accuracy and hamstrings flexibility: A pilot study. J. Bodyw. Mov. Ther. 2020, 24, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Pournot, H.; Tindel, J.; Testa, R.; Mathevon, L.; Lapole, T. The Acute Effect of Local Vibration as a Recovery Modality from Exercise-Induced Increased Muscle Stiffness. J. Sports Sci. Med. 2016, 15, 142–147. [Google Scholar] [PubMed]
- Mahdavi, N.; Motamedzade, M.; Jamshidi, A.A.; Darvishi, E.; Moghimbeygi, A.; Heidarimoghadam, R. Upper trapezius fatigue in carpet weaving: The impact of a repetitive task cycle. Int. J. Occup. Saf. Ergon. 2016, 24, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-Y.; Yu, I.-Y.; Oh, J.-S.; Kang, M.-H. Effects of Intended Scapular Posterior Tilt Motion on Trapezius Muscle Electromyography Activity. Int. J. Environ. Res. Public Health 2021, 18, 9147. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Song, D.; Park, D.; Kim, H.; Shin, G. Reflexive Response of Neck Muscle to Sudden Perturbation after Prolonged Smartphone Use. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2021, 65, 1250–1253. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirst, M.A. Effects of Tool Weight on Fatigue and Performance during Short Cycle Overhead Work Operations. Ph.D. Thesis, Virginia Tech, Blacksburg, VA, USA, 1999. [Google Scholar]
- Kleine, B.-U.; Schumann, N.-P.; Stegeman, D.F.; Scholle, H.-C. Surface EMG mapping of the human trapezius muscle: The topography of monopolar and bipolar surface EMG amplitude and spectrum parameters at varied forces and in fatigue. Clin. Neurophysiol. 2000, 111, 686–693. [Google Scholar] [CrossRef]
- Farina, D.; Madeleine, P.; Graven-Nielsen, T.; Merletti, R.; Arendt-Nielsen, L. Standardising surface electromyogram recordings for assessment of activity and fatigue in the human upper trapezius muscle. Eur. J. Appl. Physiol. 2002, 86, 469–478. [Google Scholar] [CrossRef]
- Jensen, C.; Westgaard, R.H. Functional subdivision of the upper trapezius muscle during low-level activation. Eur. J. Appl. Physiol. 1997, 76, 335–339. [Google Scholar] [CrossRef]
- Jensen, C.; Vasseljen, O.; Westgaard, R.H. The influence of electrode position on bipolar surface electromyogram recordings of the upper trapezius muscle. Eur. J. Appl. Physiol. 1993, 67, 266–273. [Google Scholar] [CrossRef]
- Johansen, T.I.; Samani, A.; Antle, D.M.; Côté, J.N.; Madeleine, P. Gender effects on the coordination of subdivisions of the trapezius muscle during a repetitive box-folding task. Eur. J. Appl. Physiol. 2012, 113, 175–182. [Google Scholar] [CrossRef]
- Öberg, T. Muscle fatigue and calibration of EMG measurements. J. Electromyogr. Kinesiol. 1995, 5, 239–243. [Google Scholar] [CrossRef]
- Borstad, J.D.; Szucs, K.; Navalgund, A. Scapula kinematic alterations following a modified push-up plus task. Hum. Mov. Sci. 2009, 28, 738–751. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, R.H.; Reaz, M.B.I.; Ali, M.A.B.M.; Bakar, A.A.A.; Chellappan, K.; Chang, T.G. Surface Electromyography Signal Processing and Classification Techniques. Sensors 2013, 13, 12431–12466. [Google Scholar] [CrossRef] [PubMed]
- Tkach, D.; Huang, H.; Kuiken, T.A. RSetseuardchy of stability of time-domain features for electromyographic pattern recognition. J. Neuroeng. Rehabil. 2010, 7, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moussavi, Z.K.; Cooper, J.E.; Shwedyk, E. Fatigue pattern of trapezius muscle in relation to its functional role. In Proceedings of the 18th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Amsterdam, The Netherlands, 31 October–3 November 1996; Volume 4, pp. 1451–1453. [Google Scholar] [CrossRef]
- Lavender, S.A.; Marras, W.S. An electromyographic analysis of an ergonomic intervention with the jackleg drill. Appl. Ergon. 1990, 21, 90–100. [Google Scholar] [CrossRef]
- Sharon, H.; Elamvazuthi, I.; Lu, C.-K.; Parasuraman, S.; Natarajan, E. Development of Rheumatoid Arthritis Classification from Electronic Image Sensor Using Ensemble Method. Sensors 2019, 20, 167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alam, M.M.; Khan, A.A.; Farooq, M. Effects of vibratory massage therapy on grip strength, endurance time and forearm muscle performance. Work 2021, 68, 619–632. [Google Scholar] [CrossRef]
- Rittweger, J.; Mutschelknauss, M.; Felsenberg, D. Acute changes in neuromuscular excitability after exhaustive whole body vibration exercise as compared to exhaustion by squatting exercise. Clin. Physiol. Funct. Imaging 2003, 23, 81–86. [Google Scholar] [CrossRef]
- Torvinen, S.; Kannus, P.; Sievänen, H.; Jarvinen, T.A.H.; Pasanen, M.; Kontulainen, S.; Järvinen, T.L.N.; Järvinen, M.; Oja, P.; Vuori, I. Effect of a vibration exposure on muscular performance and body balance. Randomized cross-over study: Effects of vibration on perfor-mance and balance. Clin. Physiol. Funct. Imaging 2002, 22, 145–152. [Google Scholar] [CrossRef]
- Diego, M.A.; Field, T.; Sanders, C.; Hernandez-Reif, M. Massage therapy of moderate and light pressure and vibrator effects on EEG and heart rate. Int. J. Neurosci. 2004, 114, 31–44. [Google Scholar] [CrossRef]
- Barnes, M.J.; Perry, B.G.; Mündel, T.; Cochrane, D.J. The effects of vibration therapy on muscle force loss following eccentrically induced muscle damage. Eur. J. Appl. Physiol. 2011, 112, 1189–1194. [Google Scholar] [CrossRef]
- Fuller, J.T.; Thomson, R.L.; Howe, P.R.; Buckley, J.D. Vibration Therapy Is No More Effective Than the Standard Practice of Massage and Stretching for Promoting Recovery from Muscle Damage After Eccentric Exercise. Clin. J. Sport Med. 2015, 25, 332–337. [Google Scholar] [CrossRef]
- Merletti, R.; Sabbahi, M.A.; De Luca, C.J. Median frequency of the myoelectric signal. Eur. J. Appl. Physiol. Occup. Physiol. 1984, 52, 258–265. [Google Scholar] [CrossRef]
- Farina, D.; Kallenberg, L.A.C.; Merletti, R.; Hermens, H.J. Effect of side dominance on myoelectric manifestations of muscle fatigue in the human upper trapezius muscle. Eur. J. Appl. Physiol. 2003, 90, 480–488. [Google Scholar] [CrossRef]
- Zhang, J.; Yu, J.; Liu, C.; Tang, C.; Zhang, Z. Modulation in Elastic Properties of Upper Trapezius with Varying Neck Angle. Appl. Bionics Biomech. 2019, 2019, 6048562. [Google Scholar] [CrossRef] [Green Version]
- Uthaikhup, S.; Bsc, N.W.; Kummaung, P. Effects of gender and hand dominance on size of the lower trapezius muscle: Lower Trapezius Size. Muscle Nerve 2015, 52, 576–579. [Google Scholar] [CrossRef]
- Januario, L.B.; França, D.B.; Moreira, R.D.F.C.; Oliveira, A.B. Comparison of muscle activity from upper trapezius and wrist extensors between dominant and non-dominant upper limbs during computer-based tasks. Work 2018, 61, 295–301. [Google Scholar] [CrossRef]
- Diederichsen, L.P.; Nørregaard, J.; Dyhre-Poulsen, P.; Winther, A.; Tufekovic, G.; Bandholm, T.; Rasmussen, L.R.; Krogsgaard, M. The effect of handedness on electromyographic activity of human shoulder muscles during movement. J. Electromyogr. Kinesiol. 2007, 17, 410–419. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-G. Correlation between Scapular Asymmetry and Differences in Left and Right Side Activity of Muscles Adjacent to the Scapula. Osong Public Health Res. Perspect. 2017, 8, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Marker, R.J.; Balter, J.E.; Nofsinger, M.L.; Anton, D.; Fethke, N.B.; Maluf, K.S. Upper trapezius muscle activity in healthy office workers: Reliability and sensitivity of occupational exposure measures to differences in sex and hand dominance. Ergonomics 2016, 59, 1205–1214. [Google Scholar] [CrossRef] [PubMed]
- Shiezadeh, Z.; Sajedi, H.; Aflakie, E. Diagnosis of rheumatoid arthritis using an ensemble learning approach. Comput. Sci. Inf. Technol. 2015, 5, 139–148. [Google Scholar] [CrossRef]
- Das, R.; Sengur, A. Evaluation of ensemble methods for diagnosing of valvular heart disease. Expert Syst. Appl. 2010, 37, 5110–5115. [Google Scholar] [CrossRef]

| Degree | Task | Side | Intervention Group (Difference 95%CI) | Control Group (Difference 95%CI) | p-Value |
|---|---|---|---|---|---|
| Level-1 (36 Hz) | Fatigue 30 s | R | 24.80 (19.47–30.14) | 33.04 (27.19–38.87) | 0.043 * |
| L | 31.21 (25.61–36.81) | 37.64 (31.50–43.78) | 0.122 | ||
| Fatigue 60 s | R | 31.17 (26.26–36.08) | 40.48 (35.11–45.86) | 0.015 * | |
| L | 37.19 (32.11–42.27) | 38.73 (32.52–44.94) | 0.911 | ||
| Fatigue 90 s | R | 39.43 (34.15–44.69) | 46.89 (41.12–52.66) | 0.060 * | |
| L | 39.19 (33.51–44.86) | 43.64 (38.07–49.21) | 0.090 | ||
| Level-3 (46 Hz) | Fatigue 30 s | R | 30.18 (25.84–34.52) | 39.15 (34.38–43.91) | 0.010 * |
| L | 31.48 (27.08–35.88) | 35.05 (30.23–39.87) | 0.267 | ||
| Fatigue 60 s | R | 32.57 (27.63–37.79) | 40.64 (34.93–46.36) | 0.043 * | |
| L | 31.88 (25.99–37.77) | 36.83 (30.38–43.29) | 0.252 | ||
| Fatigue 90 s | R | 37.65 (32.25–43.11) | 46.78 (40.82–52.74) | 0.030 * | |
| L | 33.37 (28.86–37.89) | 43.16 (38.21–48.11) | 0.007 * |
| Task | Side | Intervention Group | Control Group | ||||
|---|---|---|---|---|---|---|---|
| Before (Mean (SD)) | After (Mean (SD)) | p-Value | Before (Mean (SD)) | After (Mean (SD)) | p-Value | ||
| Fatigue 30 s | R1 | 35.65 ± 3.45 | 25.25 ± 3.52 | 0.022 * | 34.05 ± 3.83 | 32.49 ± 3.23 | 1.000 |
| L1 | 39.39 ± 3.09 | 31.33 ± 2.51 | 0.076 | 38.49 ± 2.61 | 37.49 ± 3.11 | 1.000 | |
| Fatigue 60 s | R2 | 41.23 ± 3.56 | 31.14 ± 4.49 | 0.005 * | 41.29 ± 3.02 | 40.51 ± 2.10 | 1.000 |
| L2 | 42.94 ± 1.81 | 36.94 ± 2.79 | 1.000 | 40.90 ± 2.49 | 39.42 ± 2.09 | 1.000 | |
| Fatigue 90 s | R3 | 45.12 ± 2.41 | 39.55 ± 3.61 | 0.049 * | 44.73 ± 2.61 | 46.74 ± 2.08 | 1.000 |
| L3 | 44.87 ± 5.10 | 38.05 ± 3.75 | 0.345 | 41.98 ± 2.95 | 42.61 ± 3.80 | 1.000 | |
| Task | Side | Intervention Group | Control Group | ||||
|---|---|---|---|---|---|---|---|
| Before (Mean (SD)) | After (Mean (SD)) | p-Value | Before (Mean (SD)) | After (Mean (SD)) | p-Value | ||
| Fatigue 30 s | R1 | 35.19 ± 2.61 | 28.83 ± 3.07 | 0.116 | 39.77 ± 2.19 | 40.77 ± 1.69 | 1.000 |
| L1 | 38.11 ± 3.36 | 31.88 ± 3.00 | 0.301 | 36.54 ± 3.12 | 34.57 ± 2.50 | 1.000 | |
| Fatigue 60 s | R2 | 40.04 ± 3.28 | 31.38 ± 3.83 | 0.033 * | 43.22 ± 2.48 | 42.08 ± 2.99 | 1.000 |
| L2 | 40.40 ± 3.43 | 32.82 ± 3.75 | 0.274 | 37.31 ± 3.56 | 35.71 ± 3.53 | 1.000 | |
| Fatigue 90 s | R3 | 49.04 ± 3.91 | 38.98 ± 3.93 | 0.028 * | 44.42 ± 2.67 | 45.22 ± 2.30 | 1.000 |
| L3 | 43.17 ± 14.33 | 35.05 ± 3.56 | 0.040 * | 38.00 ± 3.72 | 41.15 ± 3.73 | 1.000 | |
| Model | Accuracy | Precision | Recall | F1-Score |
|---|---|---|---|---|
| SVM | 0.855 | 0.774 | 0.784 | 0.779 |
| KNN | 0.829 | 0.740 | 0.762 | 0.751 |
| DT | 0.764 | 0.640 | 0.693 | 0.665 |
| Bagging | 0.860 | 0.782 | 0.814 | 0.797 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, L.; Fang, M.; Hu, J. The Effect of Vibration Massage on Fatigue of the Upper Trapezius Muscle during Different Tasks. Symmetry 2022, 14, 2158. https://doi.org/10.3390/sym14102158
Wang L, Fang M, Hu J. The Effect of Vibration Massage on Fatigue of the Upper Trapezius Muscle during Different Tasks. Symmetry. 2022; 14(10):2158. https://doi.org/10.3390/sym14102158
Chicago/Turabian StyleWang, Lingyu, Mingzhu Fang, and Jie Hu. 2022. "The Effect of Vibration Massage on Fatigue of the Upper Trapezius Muscle during Different Tasks" Symmetry 14, no. 10: 2158. https://doi.org/10.3390/sym14102158
APA StyleWang, L., Fang, M., & Hu, J. (2022). The Effect of Vibration Massage on Fatigue of the Upper Trapezius Muscle during Different Tasks. Symmetry, 14(10), 2158. https://doi.org/10.3390/sym14102158







