Abstract
Failure of the mimic muscles as a cause of facial nerve paralysis may result in significant asymmetry, which can be addressed by surgical reanimation procedures. Among those, the temporalis muscle transfer as advocated by McLaughlin is a single-stage technique for the dynamic reanimation of the mouth. Despite increasing research directed at women’s health, the gender-specific differences of this technique have not yet been addressed. Thus, we retrospectively reviewed the medical records of patients who underwent this operation between 2001 and 2021 for gender-specific differences concerning the postoperative outcome. In total, 28 women and 17 men were included. The two cohorts were statistically comparable with respect to etiological characteristics such as age, duration and etiology of paralysis, and preoperative degree of symptoms. After a median follow up of 15 months, restoration of smiling and elevation of the oral commissure was more often achieved among women than men. A statistically significant difference, however, could only be shown for the latter. Resting symmetry was restored in about 50% of both genders. There were no differences concerning postoperative complications or reoperations. The McLaughlin’s dynamic muscle support effectively re-establishes the elevation of the oral commissure and ability to smile among both genders, albeit women tend to be more likely to achieve the desired results.
1. Introduction
Facial paralysis displays a devastating condition with significant functional and aesthetic implications, as well as emotional and psychosocial sequela [1,2]. The dysfunction of the mimic muscles deprives the patient of individual facial expressions and may cause severe asymmetry, particularly when smiling.
The challenging goal for reconstructive surgery is to re-establish facial symmetry and a coordinated animation of the paralyzed face, wherefore an individualized treatment approach depending on the etiology and duration of paralysis as well as patients’ expectations is imperative [3]. The optimum management, however, has not been defined yet due to the lack of ability to compare results. Contemporary reconstructive options mainly include microsurgical techniques involving cross-facial nerve grafting and nerve transfer or, rather, free neurovascular muscle transplantation. Some drawbacks of these procedures, such as delayed or failed nerve regeneration, long operative time or, rather, a multi-stage approach, risk of flap failure and a bulky appearance of the face with a resultant asymmetric and unaesthetic appearance, explain why their use cannot be considered for all patients, such as those suffering from severe comorbidities or who request an immediate reconstructive result.
As an alternative, the temporalis muscle transfer by McLaughlin is a relatively minimal invasive, single-stage technique for the dynamic reanimation of the oral commissure [4]. The antegrade transposition of the muscle tendon takes advantage of the full contractile force and does not result in a hollowing of the temple fossa or bulging contour at the zygomatic arch as opposed to antidromic procedures [5]. When simultaneously combined with Gillies myoplasty, the temporalis muscle may provide both the active restoration of eyelid closure and the excursion of the oral commissure, which consequently enables smiling [4,6,7].
Within the last few years, the concept of gender dimorphism has also been recognized in facial paralysis reanimation. According to Hontanilla and Marre, women are more likely to accomplish an effortless and reflective smile following reanimation with microvascular gracilis transfer neurotized to the masseteric nerve [8]. Despite increasing research directed at women’s health, gender dimorphism has never been addressed in relation to dynamic muscle transfer techniques such as the McLaughlin’s procedure. Thus, the aim of this study was to retrospectively analyze a consecutive cohort of patients for gender-specific differences.
2. Materials and Methods
We retrospectively reviewed patients who underwent facial reanimation by McLaughlin’s dynamic muscle support either alone or in combination with the Gillies procedure at our institution between 2001 and 2021. Minimum follow-up was set as 3 months postoperatively. Facial paralysis resulted from various etiologies such as trauma, neoplasm, congenital disorders, as well as iatrogenic or idiopathic conditions. All patients suffered from irreversible facial paralysis for more than 12 months prior to surgery. Therefore, neurotization or cross-face nerve graft techniques were not applicable. As an alternative, microvascular free muscle transfer was offered but either rejected by the patients or not indicated due to severe comorbidities or the request for an immediate reconstructive result.
Demographic and surgical data were recorded from medical records. For outcome evaluation, postoperative complications and functional assessment were reviewed. The latter was obtained from clinical records, in which variables such as facial symmetry at rest, movement of the mouth corner, ability to smile, and eye protection by means of complete eyelid closure were assessed. Functional outcome was further evaluated by standardized photographs, which were routinely taken of every consenting patient, pre- and postoperatively, to document the degree of paralysis before and after the surgery.
2.1. Operative Technique
All procedures were performed unilaterally and under general anesthesia. Both techniques described in this study aim to reanimate the paralyzed face; while McLaughlin’s dynamic muscle support is used to correct the drooping oral commissure, the temporalis muscle transfer by Gillies reanimates the paralytic eye, causing lagophthalmos [9]. Before the operation, the function of the temporalis muscle, which is innervated by the mandibular nerve (V3), is tested clinically by observing and palpating for contraction of the muscle in the temple area during mastication.
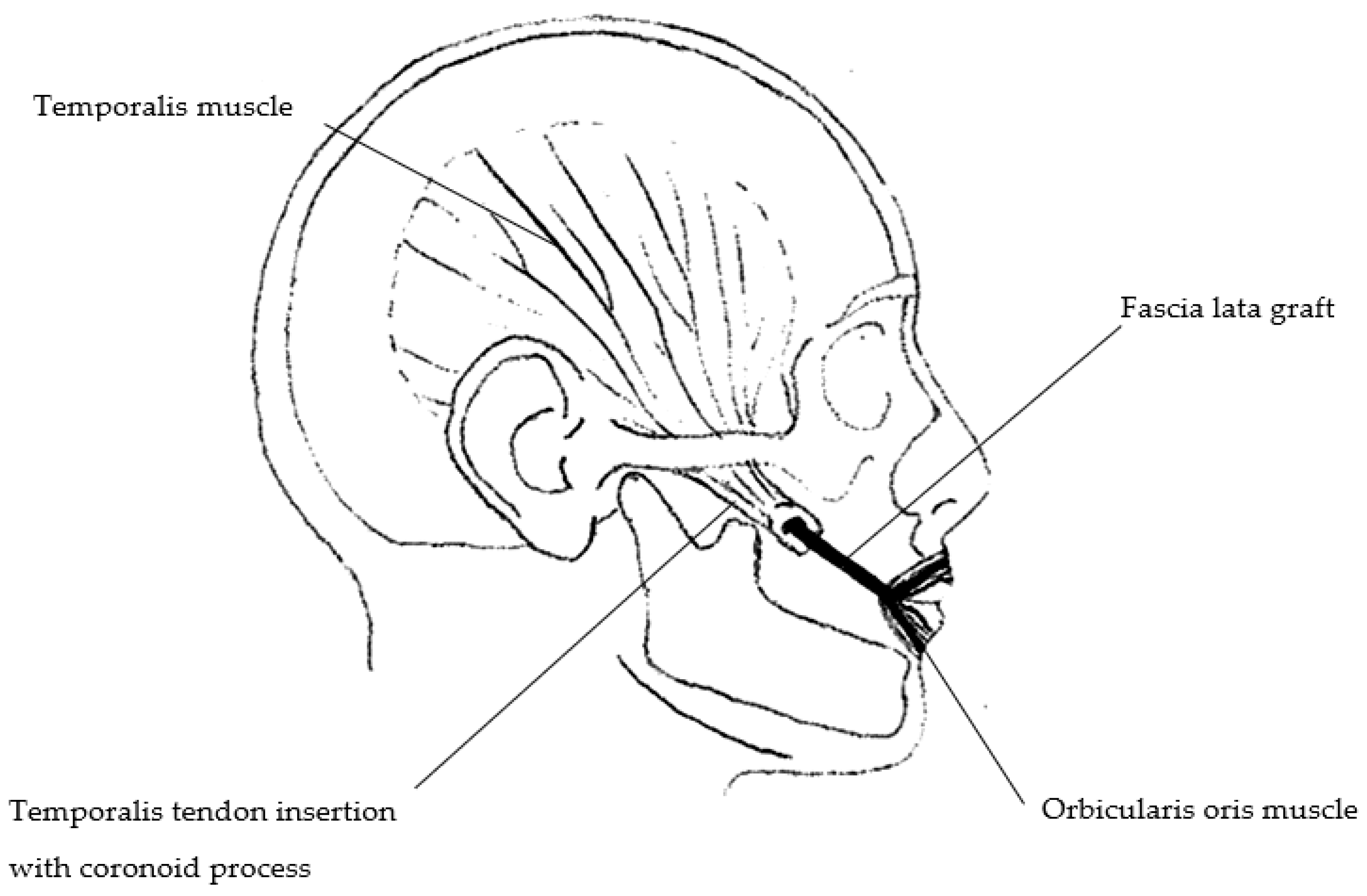
In 1953, McLaughlin first described the antegrade transposition of the coronoid process with the attached temporalis tendon to the lateral corner of the ipsilateral modiolus, as shown in Figure 1 [4]. The osteotomy of the coronoid process can be performed either via intraoral or extraoral (preauricular) incision [10,11]. Another incision is made next to the modiolus, then a subcutaneous tunnel is formed between both incisions by blunt dissection through the buccal space. Following osteotomy, the temporalis muscle tendon is lengthened by a strip of facia lata to reach the modiolus and the most medial parts of the upper and lower lip, respectively, where it is anchored to the orbicularis oris muscle on three key locations, which are defined preoperatively.
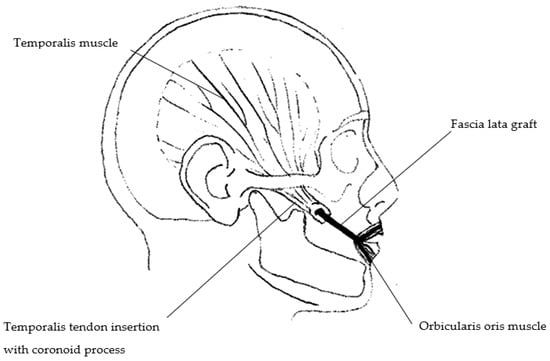
Figure 1.
Illustration showing the anatomy of the temporalis muscle after osteotomy of the coronoid process and lengthening by a strip of fascia lata. The fascial strip is anchored to the orbicularis oris muscle on three defined locations (modiolus, upper and lower lip—“three-point-fixation”). The fixation of the lip should be located in the midline to include innervated muscle from the contralateral side.
The Gillies procedure uses a central strip of the temporalis muscle of about 2 cm in width, which is transposed anteriorly and again lengthened by a small fascial strip [6]. The fascial part is then divided into two equal slips, which are sutured to the medial and lateral canthal region after preparation of pretarsal subcutaneous tunnels. The resulting sling around the eye enables active lid closure of both the upper and lower eyelid when the temporalis muscle is contracted.
For both procedures, muscle-retraining exercises in terms of active training of mouth elevation and closure of the eyelid by clenching of the teeth can be started immediately after the operation. In our opinion, early mobilization is pivotal to minimize tendon adhesions and scar formations. After discharge, patients are advised to pursue the instructed exercises in front of a mirror several times a day to achieve the desired result and to regain a symmetric appearance. For two weeks postoperatively, patients are further placed on a soft diet to reduce the maximum force on the sutures during mastication.
2.2. Statistical Analysis
Continuously coded variables of patients’ demographics and operative characteristics were either reported as mean and standard deviation (SD) or median and interquartile range (IQR) when the normality of the data was not confirmed. Categorical variables were displayed as frequencies and proportions. For the analysis of group differences between men and women, the chi-squared test and the Student’s t-test, or the nonparametric equivalent, when appropriate, were used.
All analyses were conducted with IBM SPSS Statistics for Windows, Version 26.0 (Armonk, NY, USA: IBM Corp.). Statistical testing was two-sided and the significance was set at p < 0.05.
3. Results
In total, 45 patients underwent McLaughlin’s dynamic muscle reanimation at our institution between 2001 and 2021. Approximately two thirds of all patients were females (62.2%).
Table 1 outlines the epidemiological characteristics of the entire study group, as well as according to each gender. The mean age of all patients was about 52 years (range 18–77). For most patients (84.4%), unilateral paralysis was diagnosed more than 24 months preoperatively. Females showed a slightly shorter mean duration of paralysis compared to men (110.2 vs. 116.9 months, respectively), yet this difference did not reach statistical significance (p = 0.944).

Table 1.
Epidemiological characteristics.
Both male and female patients most often suffered from facial paralysis secondary to surgical interventions (84.4%), which involved the excision of acoustic neuroma in most cases. Congenital and iatrogenic conditions affected one, or rather two, patients of each gender, while facial paralysis resulting from penetrating trauma was documented once in a male patient; despite these differences, the distribution of etiologies did not follow a gender-related pattern.
Pre-existing medical conditions were documented in a total of 17 patients (37.8%) which again were equally distributed among men and women.
3.1. Operative Details
Except for four patients (8.9%, one male and three females), all others had undergone previous reanimation procedures, which did not reach a functionally or aesthetically pleasing condition, wherefore the indication for McLaughlin’s procedure, either alone (n= 16) or in combination with Gillies myoplasty (n = 29) was made. Among both genders, the combined procedure was undertaken more often than the singular muscle transposition by McLaughlin (Table 2).

Table 2.
Operative details.
When the McLaughlin’s procedure was performed alone, patients either underwent a previous correction of eyelid closure in terms of lid loading with a gold or platinum chain implant and/or canthoplasty (n = 7) or did not require surgical correction due to sufficient eyelid closure at the time of operation (n = 9).
Osteotomy of the coronoid process was predominantly performed following an extraoral access via preauricular or, rather, face-lift incision (91.1%). In only two cases of each gender, an intraoral access was used.
The rate of additional corrective procedures while performing McLaughlin’s dynamic muscle reanimation was equally distributed between male and female patients, with 23.5% vs. 25%, respectively. Among those, concomitant ophthalmologic interventions for correction of lower lid ectropium were most often performed. Additionally, female patients underwent simultaneous brow lift in three cases and symmetrizing facelift of the contralateral side in one case. These procedures were not undertaken among men.
3.2. Outcome
Before surgery all patients displayed significant facial asymmetry, which further included the inability of smiling (n = 40, 89.0%) and restricted movement of the oral commissure, causing a drooping appearance (n = 39, 86.7%). The ability of asymmetric smiling without teeth exposure was preoperatively documented in three females (6.7%).
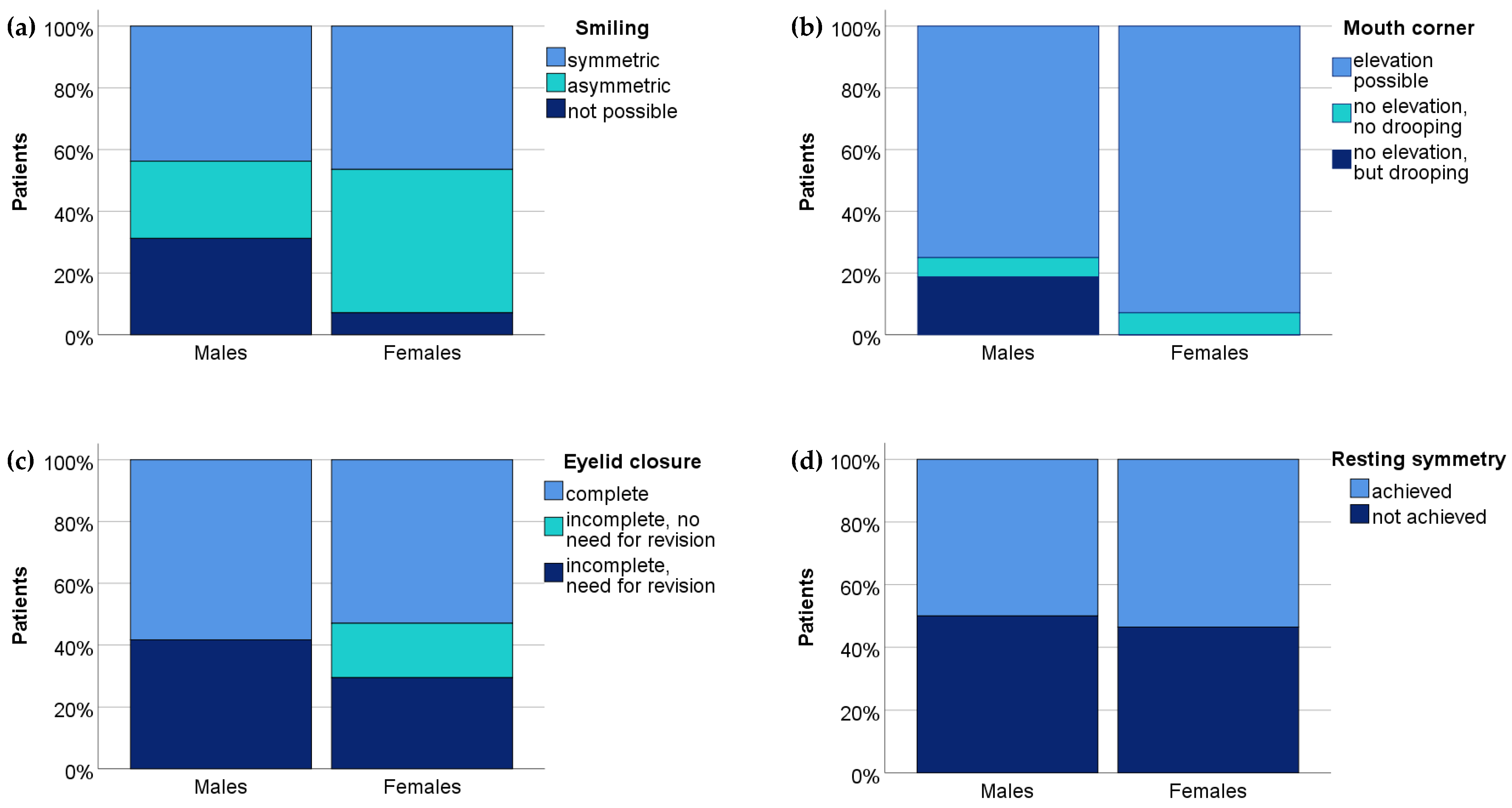
Among all patients, the median duration of follow-up was 15.0 months (range 3–228, p = 0.349). Figure 2 summarizes the postoperative results concerning the ability to smile, elevation of the mouth corner, eye protection by means of eyelid closure (in patients who underwent the combined procedure) and resting symmetry. Apart from resting symmetry, restoration of function was postoperatively more often achieved among females than males. A significant difference between both genders, however, could only be shown for the elevation of the mouth corner (p = 0.045). As for smiling, there was no gender-related statistical difference (p = 0.086), even though more females than males regained smiling activity (26 out of 28, 92.8% vs. 12 out of 17, 70.5%), which was considered symmetric in about 45% of both genders.
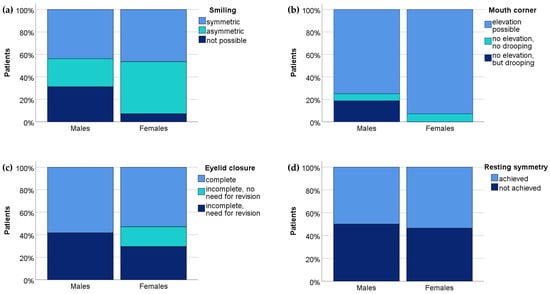
Figure 2.
Postoperative evaluation of (a) smiling activity, (b) elevation of the mouth corner, (c) eyelid closure (in case of combined McLaughlin and Gillies procedure) and (d) resting symmetry according to each gender. Data are given in percentage. Gender-specific comparison revealed a statistically significant difference for the elevation of the mouth corner (p = 0.045), even though women also achieved better results concerning the restoration of smiling and eyelid closure.
3.3. Complications
Most patients (n = 36, 80.0%) experienced an uneventful postoperative course. Local infection (n = 4) and wound healing disturbance (n = 2) were both treated conservatively in all cases and exclusively limited to patients who had undergone an extra-oral access for osteotomy of the coronoid process. Operative revisions due to hematoma or acute bleeding were undertaken in three cases (two males and one woman). Despite the male predominance in postoperative complications (23.5% vs. 17.9%), no gender-specific difference could be found (p = 0.505).
Among the entire cohort, there were no donor-site complications recorded neither in the temple region, nor in the lateral part of the thigh where the fascia lata was harvested. Combining the McLaughlin and Gillies procedures did not result in an increase of postoperative complications or higher donor-site morbidity among both genders.
4. Discussion
Facial expression is the key to social interaction and the ability to show emotions, which is imperative for interpersonal communication [12]. For these reasons, various surgical techniques have been developed for the treatment of the paralyzed face tailored to the needs of the patients or, rather, the time of presentation and etiology of paralysis.
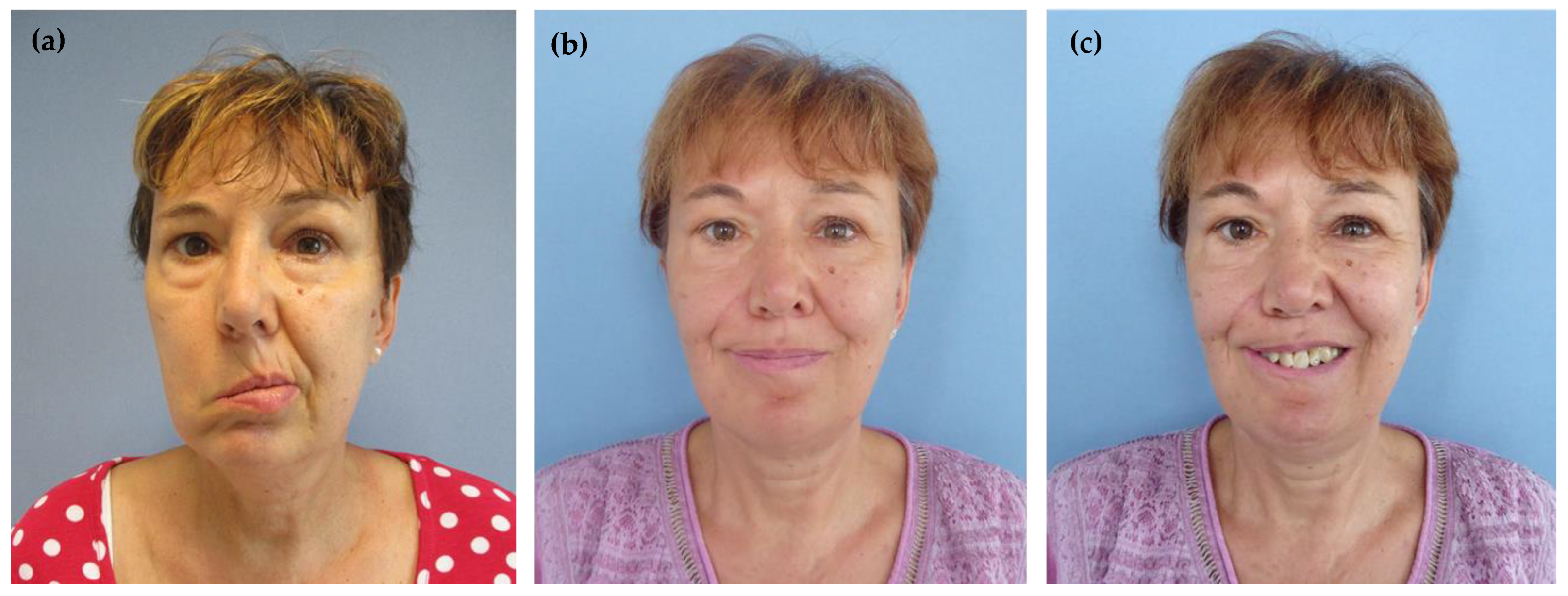
The temporalis muscle transfer as advocated by McLaughlin is a simple and relatively minimal invasive single-stage technique for restoring the elevation of the oral commissure and smiling ability [4,13,14]. It can be performed irrespectively of the duration of facial paralysis since it is the third branch of the trigeminus nerve, which is responsible for the motor innervation of the temporalis muscle, enabling the dynamic correction. Due to its low morbidity, the McLaughlin’s procedure is associated with quick postoperative recovery and, thus, can also be considered for elderly patients with comorbidities or who have a poor prognosis [15,16]. A further benefit is the relatively short duration of the procedure, which is completed in about 4 h in our clinics. Most importantly, however, it produces an immediate postoperative result, which means that patients are quickly advanced to actively engage the temporalis muscle in oral commissure excursion. After the instruction of specific exercises, diligent practice in front of a mirror will further improve the dynamics of the oral commissure and specifically train the different smiling functions, ultimately leading to a symmetric appearance as illustrated in Figure 3 [5,11]. In our study, women more often regained the ability to smile, and adequate excursion of the mouth corner compared to men. These results are in accordance with authors who observed that women were more likely to achieve an effortless and symmetric smile following cross-face nerve grafting or free muscle transfer neurotized to the masseteric nerve [8,17]. In this regard, it has been hypothesized that women develop brain plasticity to a greater extent than men, especially for actions considered important in social behavior [18]. Given the fact that women more often smile than men—under both natural and experimental conditions—this association does not seem surprising and may be further transferred to the observations of this study [19,20]. In other words, women may consider smiling more important than men and, therefore, the motivation to regain smiling activity by constant exercising is higher in the female population [17]. The role of sex hormones for this association as mentioned by Hontanilla et al. remains merely speculative, however [17].
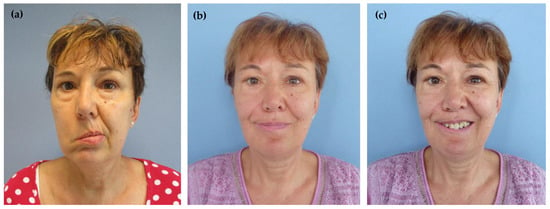
Figure 3.
(a) Preoperative picture of 56-year-old women with complete facial palsy on the right side after acoustic neuroma excision (b,c) Postoperative pictures of the same patient: symmetric smiling without and with teeth exposure following McLaughlin’s procedure.
As for brain plasticity, it has been hypothesized to be causative for the ability to smile, not only voluntarily by active clenching of the teeth but also spontaneously without biting [5,21,22]. Yet, the lack of spontaneity is regarded a main limitation of dynamic muscle reanimation procedures such as the McLaughlin’s technique. Therefore, it needs to be reconsidered if it is indeed a “spontaneous” action or rather an “invisible” muscular contraction which has been perfectly trained to give the impression of being effortless and reflexive. In other words, some patients might diligently do the instructed exercises and by maintaining the right tension for achieving a symmetric appearance, it may become a “constant habit”, which is then automatically carried out in social interactions later. This mechanistic background might explain the re-establishment of facial symmetry at rest in 50% of our patients. In this regard, we recommend slightly overcorrecting the position of the oral commissure intraoperatively (of about 6–8 mm compared to the uninjured side) since the repair site will slip a few millimeters after the operation [9]. In our opinion, the risk of overcorrection is lower than the risk of a failed reconstruction. When determining the right estimation of length-tension relationship, we further recommend the use of intraoperative electrical stimulation to achieve the desired functional range of motion.
Respecting the biomechanics of muscle tendon transfer, Boahene states that one single tendon should be used to restore one single function [23]. This principle, however, is not necessarily applicable to the temporalis muscle since it can effectively provide dynamic support for the paralyzed eyelid and the oral commissure at the same time. We did not observe any difference concerning the reanimation of the oral commissure or smiling when the McLaughlin procedure was combined with the Gillies technique, neither among men nor among women.
Against the opinion that direct transfer of the muscle tendon unit generates a more effective contraction (as performed in the Labbé’s procedure), biomechanical studies have shown that lengthening the temporalis tendon by fascia lata (as advocated by McLaughlin) generates an adequate force of contraction and additionally avoids the overstretching of the muscle [23,24]. Our experience with the McLaughlin’s temporal myoplasty has been very good so far and its complication profile can be regarded low, as shown in this study (rate of operative revision: 6%, rate of conservatively treated complication: 13.3%). Labbé’s technique, however, is associated with extensive dissection and mobilization of the muscle, which can not only potentially damage the neurovascular structures but also result in a consequent risk of scarring [10,25]. In a retrospective investigation by Panossian, who performed this procedure in 18 children, revision surgery was needed in about 64% due to tendon adhesions and further 11.1% required blood transfusion during an average operative time of about 7 h [26]. As an alternative, a less invasive approach, as proposed by Choudhary et al., could be considered, which is classified as the suprazygomatic aponeurotic myoplasty [25]. Their technique is a modification of the McLaughlin procedure but does not involve any osteotomy. Outcome evaluation demonstrated good to excellent results among all patients (n = 12), with an average range of modiolus excursion of 12.6 mm, no complications, and no need for revision surgery. Yet, follow-up was limited to a maximum of 3 months, wherefore further evaluation is necessary to draw a conclusion.
Ultimately, the temporalis tendon transfer can be considered as an option to upgrade nerve grafting procedures or nerve transfers, as advocated by Viterbro et al. [5]. While acting as a substitute during nerve regeneration, the simultaneous transfer can significantly reduce the time of functional loss. Even though our clinics offer the combined procedure, we did not include these patients in the presented study to clearly assess the outcome that can be reached by McLaughlin’s procedure. Otherwise, it would have been impossible to distinguish to what extent McLaughlin’s procedure or the regenerating nerve had restored the function of the oral commissure or, rather, the smiling ability.
The main limitations of this observational study are its retrospective study design and small study population. Therefore, the generalizability of the results must be handled with caution. We further acknowledge a certain inhomogeneity concerning the depiction of patients’ clinical course, which may have influenced outcome evaluation. The lack of a standardized protocol in assessing functional outcome following facial reanimation is a well-known limitation of other studies, which limits precise comparison of the different techniques. The use of a computer-based assessment tool (e.g., eFACE) would have been desirable to overcome the subjective nature of any clinical measure [27]. Thus, the gender-related difference in this study could, in part, be influenced by the fact that the female face was interpreted differently than the male when evaluating postoperative facial movement. Ultimately, it would be interesting to assess if gender-specific differences also need to be considered for interrater reliability; in other words, does the assessors’ gender have an impact on the perception of clinical outcome regarding facial symmetry?
Opposed to other retrospective investigations, we minimized the rate of missing data, since patients were exclusively considered for study inclusion when all variables of interest for evaluating the preoperative degree of symptoms and postoperative results were given. Since our study is one of the few focusing on gender dimorphism, further research regarding gender-specific differences in facial reanimation surgery is highly recommended, and should overcome the limitations mentioned above to conclude evidence-based recommendations.
5. Conclusions
Dynamic reanimation of the face due to facial paralysis remains a challenging goal for reconstructive surgery, wherefore a wide range of techniques have been introduced to date. The benefit of the orthodromic temporalis muscle transfer by McLaughlin is the immediate restoration of dynamic action of the mouth, which consequently enables smiling and contributes to the reestablishment of facial symmetry. This study indicates that women tend to be more likely to achieve the functional dynamics, albeit further investigation is needed to profoundly evaluate this finding.
Author Contributions
Conceptualization, I.A.E. and U.M.R.; methodology, I.A.E., J.R. and L.K.; software, I.A.E. and T.S.; validation, R.S., K.E., J.R. and U.M.R.; formal analysis, K.E., L.K. and J.R.; investigation, I.A.E., L.K., T.S. and R.S.; resources, I.A.E., K.E. and T.S.; data curation, I.A.E., L.K. and T.S.; writing—original draft preparation, I.A.E. and L.K.; writing—review and editing, K.E., R.S., T.S., J.R. and U.M.R.; visualization, I.A.E. and U.M.R.; supervision, U.M.R. and J.R.; project administration, U.M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the rules of the Declaration of Helsinki 1975 and approved by the Institutional Ethics Committee.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All presented data are available upon reasonable request to the corresponding author Ederer IA. Reuse is only permitted after agreement of all co-authors of this study.
Acknowledgments
We kindly thank Vanessa Behrend for her contribution to the drawing of the illustration and Thomas K. Villiger for his technical support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lyford-Pike, S.; Nellis, J.C. Perceptions of Patients with Facial Paralysis: Predicting Social Implications and Setting Goals. Facial Plast. Surg. Clin. North Am. 2021, 29, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Ishii, L.E.; Nellis, J.C.; Boahene, K.D.; Byrne, P.; Ishii, M. The Importance and Psychology of Facial Expression. Otolaryngol. Clin. North Am. 2018, 51, 1011–1017. [Google Scholar] [CrossRef]
- Pinkiewicz, M.; Dorobisz, K.; Zatoński, T. A Comprehensive Approach to Facial Reanimation: A Systematic Review. J. Clin. Med. 2022, 11, 2890. [Google Scholar] [CrossRef] [PubMed]
- Mclaughlin, c.r. surgical support in permanent facial paralysis. Plast. Reconstr. Surg. 1953, 11, 302–314. [Google Scholar] [CrossRef] [PubMed]
- Viterbo, F.; Romão, A.; Brock, R.S.; Joethy, J. Facial Reanimation Utilizing Combined Orthodromic Temporalis Muscle Flap and End-to-Side Cross-Face Nerve Grafts. Aesthetic Plast. Surg. 2014, 38, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Gillies, H. Experiences with Fascia Lata Grafts in the Operative Treatment of Facial Paralysis: (Section of Otology and Section of Laryngology). Proc. R. Soc. Med. 1934, 27, 1372–1382. [Google Scholar]
- Papadopulos, N.; Markou, M.A. A modified temporalis transfer technique for facial paralysis in elderly patients. Injury 2020, 51, S88–S92. [Google Scholar] [CrossRef] [PubMed]
- Hontanilla, B.; Marre, D. Differences between sexes in dissociation and spontaneity of smile in facial paralysis reanimation with the masseteric nerve. Head Neck 2014, 36, 1176–1180. [Google Scholar] [CrossRef]
- Exner, K.; Kuhn, T. Gillies and McLaughlin’s Dynamic Muscle Support in Irreversible Facial Palsy. Handchir. Mikrochir. Plast. Chir. 2010, 42, 102–108. [Google Scholar] [CrossRef]
- Aum, J.H.; Kang, D.H.; Oh, S.A.; Gu, J.H. Orthodromic Transfer of the Temporalis Muscle in Incomplete Facial Nerve Palsy. Arch. Plast. Surg. 2013, 40, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Kim, H.J.; Moon, S.Y. Management of the paralyzed face using temporalis tendon transfer via intraoral and transcutaneous approach: Temporalis Tendon Transfer. Maxillofac. Plast. Reconstr. Surg. 2018, 40, 24. [Google Scholar] [CrossRef] [PubMed]
- Dobreva, D.; Gkantidis, N.; Halazonetis, D.; Verna, C.; Kanavakis, G. Smile Reproducibility and Its Relationship to Self-Perceived Smile Attractiveness. Biology 2022, 11, 719. [Google Scholar] [CrossRef] [PubMed]
- Wüster, J.; Kreutzer, K.; Koerdt, S.; Voss, J.O.; Richter, M.; Heiland, M.; Doll, C.; Raguse, J.-D. Modified McLaughlin’s Dynamic Muscle Support in the 21st Century? A Retrospective Study with a Prospective Follow-Up Analysis for Patients With Long Standing Facial Paralysis. J. Craniofacial Surg. 2022, 33, e594–e598. [Google Scholar] [CrossRef] [PubMed]
- Croxson, G.R.; Quinn, M.J.; Coulson, S.E. Temporalis Muscle Transfer for Facial Paralysis: A Further Refinement. Facial Plast. Surg. 2001, 16, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Mabvuure, N.T.; Pinto-Lopes, R.; Fernandez-Diaz, O.; Tzafetta, K. The mini-temporalis turnover flap for midface reanimation: Photogrammetric and patient-rated outcomes. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 2185–2195. [Google Scholar] [CrossRef] [PubMed]
- Hembd, A.; Harrison, B.; Rocha, C.S.M.; Rocha, F.D.S.; Chamseddin, K.; Labbé, D.; Cárdenas-Mejía, A.; Rozen, S.M. Facial Reanimation in the Seventh and Eighth Decades of Life. Plast. Reconstr. Surg. 2018, 141, 1239–1251. [Google Scholar] [CrossRef]
- Hontanilla, B.; Olivas-Menayo, J.; Marré, D.; Cabello, Á.; Aubá, C. Maximizing the Smile Symmetry in Facial Paralysis Reconstruction: An Algorithm Based on Twenty Years’ Experience. Facial Plast. Surg. 2021, 37, 360–369. [Google Scholar] [CrossRef]
- Marre, D.; Hontanilla, B. Gender Differences in Facial Paralysis Reanimation. Plast. Reconstr. Surg. 2012, 129, 190e–192e. [Google Scholar] [CrossRef]
- Ellis, L.; Das, S. Sex differences in smiling and other photographed traits: A theoretical assessment. J. Biosoc. Sci. 2011, 43, 345–351. [Google Scholar] [CrossRef]
- Ellis, L. Gender differences in smiling: An evolutionary neuroandrogenic theory. Physiol. Behav. 2006, 88, 303–308. [Google Scholar] [CrossRef]
- Labbè, D.; Bussu, F.; Iodice, A. Approccio Alle Paralisi Del Facciale Basato Sulla Plastica Di Allungamento Del Muscolo Temporale. Acta Otorhinolaryngol. Ital. 2012, 32, 145–153. [Google Scholar] [PubMed]
- Scaglioni, M.F.; Verdini, F.; Marchesini, A.; Neuendorf, A.D.; Coccia, D.; Leo, T.; Riccio, M. Assessment of functional outcomes of temporalis muscle transfers for patients with longstanding facial paralysis. Head Neck 2016, 38, E1535–E1543. [Google Scholar] [CrossRef]
- Boahene, K.D.O. Principles and biomechanics of muscle tendon unit transfer: Application in temporalis muscle tendon transposition for smile improvement in facial paralysis. Laryngoscope 2013, 123, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Labbe, D. Lengthening Temporalis Myoplasty and Lips Reanimation. Annales de Chirurgie Plastique Esthetique. 1997, 42, 44–47. [Google Scholar] [CrossRef]
- Choudhary, S.; Khanna, S.; Mantri, R.; Arora, P. Suprazygomatic Aponeurotic McLaughlin Myoplasty for Facial Reanimation. Ann. Plast. Surg. 2020, 85, 149–157. [Google Scholar] [CrossRef]
- Panossian, A. Lengthening Temporalis Myoplasty for Single-Stage Smile Reconstruction in Children with Facial Paralysis. Plast. Reconstr. Surg. 2016, 137, 1251–1261. [Google Scholar] [CrossRef] [PubMed]
- Banks, C.A.; Bhama, P.K.; Park, J.; Hadlock, C.R.; Hadlock, T.A. Clinician-Graded Electronic Facial Paralysis Assessment: The eFACE. Plast. Reconstr. Surg. 2015, 136, 223e–230e. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).