Abstract
Manual handling tasks, both in daily activities and at work, require high dexterity and the ability to move objects of different shapes and sizes. However, musculoskeletal disorders that can arise due to aging, disabilities, overloading, or strenuous work can impact the natural capabilities of the hand with serious repercussions both in working and daily activities. To address this, researchers have been developing and proving the benefits of wrist exoskeletons. This paper, which is Part II of a study on wrist exoskeletons, presents and summarizes wearable wrist exoskeleton devices intended for use in rehabilitation, assistance, and occupational fields. Exoskeletons considered within the study are those available either in a prototyping phase or on the market. These devices can support the human wrist by relieving pain or mitigating fatigue while allowing for at least one movement. Most of them have been designed to be active (80%) for higher force/torque transmission, and soft for better kinematic compliance, ergonomics, and safety (13 devices out of 24, more than 50%). Electric motors and cable transmission (respectively 11 and 9 devices, out of 24, i.e., almost 50% and 40%) are the most common due to their simplicity, controllability, safety, power-to-weight ratio, and the possibility of remote actuation. As sensing technologies, position and force sensors are widely used in all devices (almost 90%). The control strategy depends mainly on the application domain: for rehabilitation, CPM (control passive motion) is preferred (35% of devices), while for assistance and occupational purposes, AAN (assistance-as-needed) is more suitable (38% of the devices). What emerges from this analysis is that, while rehabilitation and training are fields in which exoskeletons have grown more easily and gained some user acceptance (almost 18 devices, of which 4 are available on the market), relatively few devices have been designed for occupational purposes (5, with only 2 available on the market) due to difficulties in meeting the acceptance and needs of users. In this perspective, as a result of the state-of-the-art analysis, the authors propose a conceptual idea for a portable soft wrist exoskeleton for occupational assistance.
1. Introduction
Manual handling tasks, such as opening a jar, lifting a weight, or manipulating objects of different shapes and sizes in daily activities and at work, require high hand/wrist dexterity and the application of force. These actions, when performed for a prolonged time or when they are violent, irregular, repetitive, and/or involve awkward postures, contribute to the development and aggravation of musculoskeletal discomforts in the arms, wrists, and hands [1]. Musculoskeletal disorders (MSD) affect joints, bones, muscles, tendons, or ligaments. They can range from mild to severe and can lead to episodic or chronic diseases that alter the quality of life of individuals by reducing mobility and dexterity in activities of daily living (ADL). They can also arise as a result of aging, disabilities, and injuries.
Work-related musculoskeletal disorders (WRMSDs) have been recognized for a long time, with early literature dating back to the work of Bernardino Ramazzini, an 18th-century Italian physician and scientist, who is considered the father of occupational medicine [2]. His studies on workers in Padova, Italy, identified more than 50 methods for preventing harm at work and pointed out that “workers’ diseases” were attributable to the working environment, and prolonged, violent, irregular movements and postures [3,4,5].
Nowadays, as reported by the World Health Organization (WHO), approximately 1.71 billion people have MSD worldwide, most of which involve pain in the lower back and upper limbs [6]. In Italy, a report from the Italian Workers Compensatory Authority (INAIL) [7] confirms this, noting that 51.6% of all Italian workers suffer from back pain problems, while 46.7% have upper limb-related problems [8].
Fortunately, exoskeletons are increasingly being shown to provide benefits to the human body by transferring loads from the most vulnerable areas, and through the effective transfer of energy between the human and the robotic system. The number of projects involving these devices has increased dramatically since the 2000s and has involved different sectors, such as military, medical, and industrial [9], although many of the very first examples were for military programs, such as DARPA’s “Exoskeleton for human performance augmentation”. The key early developments also focused on static devices for rehabilitation in clinical settings to help recover functionalities of the limb and reduce pain after injuries [10,11]. However, today, the growing impact of WRMSD is placing more emphasis on occupational exoskeletons (OEs). Crea et al. [12] produced a roadmap for the large-scale adoption of OEs, highlighting the costs and benefits of these technologies in real-world scenarios. Only in the past 12 years have commercial wearable solutions entered the market to assist workers in burdensome and repetitive tasks [11]. Although this growth has been substantial, few have focused on the wrist, despite this being considered the fourth most common site for musculoskeletal pain in the upper limb [10,11,12,13,14]. This is due to design difficulties in the one-to-one correspondence with the human body. As presented and explained in Part I of this work [15], these devices have to meet a variety of requirements, including the biomechanics and pain factors of human joints; the application field, the kinematic compliance with the human limbs and joints, the dynamic compliance according to the forces/torques required to perform certain tasks, the stiffness of the mechanism, the ergonomics, and the safety of the device, all of which must combine to ensure the system’s adoption in real scenarios and its overall acceptance.
Different design structures have been explored by researchers and are still under development in the areas of rehabilitation and assistance [13,14,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33], as well as occupational [11,34,35,36] exoskeletons. Those structures, as shown in Part I [15], can be classified according to the stiffness, actuation type, power source, power transmission methods, and sensing and control strategies. Rigid devices [13,16,17,18,31,32], mostly made of hard and stiff materials (e.g., stiff linkages and gears), are preferred for better reliability in motion control and force/torque transmission. But soft or compliant structures are also seen to have benefits when there is a demand for more comfortable, lighter, safer devices that can overcome axis mismatches [11,14,19,20,21,22,23,24,25,26,27,28,29,30,33,34,35,36,37,38]. Soft devices are composed of materials, such as textiles, foam, rubber, or silicon, and have the advantages of being more comfortable and ergonomic, not hindering the natural movement of human joints. While compliant devices are increasingly seen as a good compromise between entirely rigid or soft devices, they consist of a system of compliant structures, cables, and springs, which are partly stiff and partly soft [15]. With respect to actuation type, a critical distinction can be made between passive and active exoskeletons. Passive devices, which are by far the most common, often use springs that store potential energy typically extracted from the motion of the user [18,28,31,33,36]; active units can use a variety of different sources of power, such as electrical [11,13,14,16,17,18,19,23,29,30,32,35], pneumatic [20,21,22,34,37], and thermal [24,25,26,27,38]. Electrical motors are the most preferred due to their robust controllability, good power-to-weight ratio, and price. The type of power transmission influences the rigidity of the system. Various methods have been explored involving rigid structures (such as direct drive, rigid links, or gears) [13,16,17,18,27,31,32], tendons or Bowden cables [11,14,19,23,26,29,35,38], or compliant elements (such as springs, artificial muscles, or flexible joint-less structures) [20,21,22,24,25,26,28,30,33,34,36,37]. To function correctly, providing feedback for and to the human body, all wearable devices need sensing and control paradigms, and usually adopt more than one type of sensor and control strategy. In wrist exoskeletons, the key sensing parameters are position-detected by encoders, potentiometers, IMU or flex sensors, forces/torques measured using load cells, pressure sensors, force resistive sensors (FSR), and bio-signals recorded using electromyography (EMG). Controllers can be designed to exert predefined trajectories and forces/torques based on a control passive motion (CPM) strategy. This is mainly used in rehabilitation protocols for passive users or to provide assistance-as-needed (AAN) control, which guarantees a higher adaptability to the user’s needs. Furthermore, controllers can work in an active resistance mode by adjusting the stiffness of some springs to impose forces/torques that resist the motion of the subject and improve rehabilitation training.
Although Part I has already focused on the human wrist anatomy and biomechanics, relevant musculoskeletal disorders, and the requirements and issues guiding the design of wrist exoskeletons, it does not cover how these aspects can be implemented into effective robotic devices. Therefore, as a continuation of Part I, Part II aims to describe how various technologies and requirements were combined to create effective wrist exoskeletons. This article underscores the point of view presented in [39]. Frequently diagnosed wrist injuries include carpal tunnel syndrome (CTS), ganglion cysts, sprains, tendinitis, and tenosynovitis, often resulting from the repetitiveness and speed of tasks, awkward postures, and the use of force in lifting and transporting loads, holding objects, or using different working tools [15]. Thus, all the devices discussed in this article are designed to support the wrist by facilitating the execution of certain movements following the human wrist kinematics, and reducing pressure on the bones, ligaments, and tendons of the wrist by providing assistance force. This helps lower the strain on the forearm muscles, thereby decreasing the risk of injury due to the aforementioned problems.
This Part II paper differs from the available literature [10,12,40,41,42,43,44,45,46] as it focuses on wearable and portable wrist exoskeletons designed since the 2000s and available both as prototypes and as commercial devices.
With respect to the previous work (Part I), it highlights the features of each device more clearly, by analyzing their mechanical design, control, and functionalities, highlighting the pros and cons, and providing general suggestions on industrializing effective devices. The reported devices are grouped on the basis of structural stiffness (rigid, soft, and compliant) and the field of application (rehabilitation, assistance, and occupational). The criteria for categorizing exoskeletons into rehabilitation, assistance, and occupational are mainly associated with required force/torque values, depending on the aim to be addressed, as can be deduced from Part I. In rehabilitation, because of impairments, muscular spasticity, or bone weaknesses, the limb does not function properly. Therefore, the forces and torques must be low to avoid the worsening of medical conditions, and movements must be slow and gently controlled to restore natural functions. In the occupational field, mid-high forces and torques are usually required. The limb is fully and correctly functioning, so the device should provide additional force to support the user by reducing the workload. The assistance domain may be considered as somewhat in between the rehabilitation and occupational fields. The user may come from a post-rehabilitation phase and still have a weak limb that is not as fully functional as it should be. Thus, mid–low forces/torques are usually required to help users in daily activities.
This paper seeks to identify the disparity between marketed and prototype products by examining the technical distinctions and peculiarities, determining the most suitable features for creating effective devices that meet user needs, and exploring the obstacles that can prevent their commercialization. It is organized as follows: In Section 2, we provide an explanation and schematization of the materials and data selection protocol adopted. In Section 3 and Section 4, we provide detailed descriptions of available wearable and portable wrist devices, respectively, in a prototyping phase and in the market, intended for rehabilitation, assistance, or occupational purposes. As a result of the state-of-the-art analysis, in Section 5, we propose a conceptual idea of a novel portable soft wrist exoskeleton for occupational assistance. Finally, Section 6 summarizes the most significant findings of the review paper and future trends of wrist exoskeletons. To simplify the gathering of information by the reader, a summary table Table A1 in Appendix A provides details on the devices and their characteristics. All acronyms are listed and defined after the appendix in the Abbreviations.
2. Materials and Methods
The methodological approach behind this review paper involved searching the market and several databases, including Google Scholar, MDPI, Scopus, Frontiers, Elsevier, ResearchGate, IEEE/ASME, ScienceDirect, Sage, Wiley, and Taylor & Francis, for all technologies explored and implemented since the 2000s regarding wrist exoskeletons.
The main keywords used for conducting the research were “Wrist exoskeletons”, designed to be “Wearable” and “Portable”, for “Rehabilitation”, “Assistance”, or “Occupational” purposes. To ensure that the results best reflected the goals of the study, a set of specific inclusion and exclusion criteria were implemented to refine the search domain.
Inclusion criteria consist of:
- Upper limb exoskeletons, which include the wrist in their designs;
- Devices able to relieve pain or mitigate fatigue by supporting at least one wrist movement;
- Devices intended for rehabilitation, assistance, and occupational purposes;
- Portable devices;
- All studies must be accessible by the authors in English.
Exclusion criteria consist of:
- Prosthesis or exoskeletons that do not allow free wrist movements;
- Military devices;
- Fixed/grounded devices;
- Studies in other languages or with insufficient information, which made the analysis unclear.
The methodological approach used, and shown in Figure 1, is similar to that in Part I [15], and focuses on describing, in detail, the design, control, and assessment of wearable and portable wrist exoskeletons.
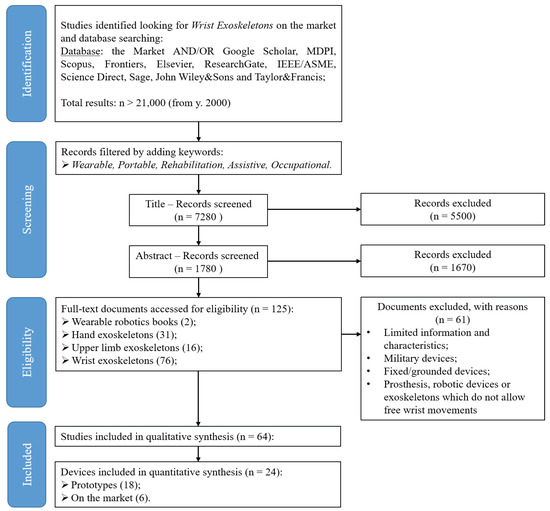
Figure 1.
The flow chart methodology adopted to identify and screen all information available from online databases and to conduct our review. This is in line with the preferred reporting items for systematic reviews and meta-analysis (PRISMA) flowchart.
3. Research and Pre-Commercial Devices
As with all developmental cycles, with exoskeletons, there is an early phase of the prototype design for research and pre-commercial testing. While the end goals for these devices may fully align with eventual commercial systems, they are often more complex in terms of hardware and software, may have unrealistic costs, or may not fully conform to strict commercial mandatory regulations. Nonetheless, these devices often form the basis for designs that will eventually become industry standards, and a full and comprehensive study and analysis of these systems is vital in any detailed review. This section provides a detailed study of wearable and portable wrist exoskeleton prototypes with, where appropriate, an assessment of the integrated actuation, electronics, control system and batteries, the ease of donning and doffing, and the potential application scenarios. All devices are shown in Figure 2 and grouped according to structural rigidity criteria.
Based on the requirements proposed in [15], the schematic shown in Figure 3 provides relevant information about research and pre-commercial wrist exoskeletons.
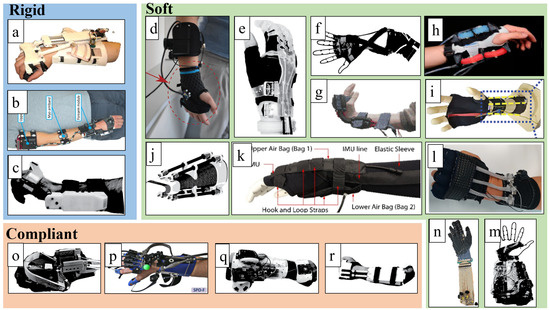
Figure 2.
All wearable exoskeleton prototypes for wrist assistance. Devices are grouped by stiffness criteria in rigid (a–c), soft (d–n), and compliant (o–r). From the top left to the bottom right, it is possible to find: (a) a portable wrist exoskeleton (PWE) designed by [47]; (b) an eWrist designed by [13,17]; (c) a wrist exoskeleton designed by [18]; (d) an exosuit designed by [11] and already reported on in [15]; (e) an Exo-Wrist designed by [19]; (f) soft orthosis designed by [20]; (g) an active support splint for the wrist (ASSIST) designed by [21]; (h) a soft origami-patterned actuator (SOA)-based wrist exoskeleton designed by [22]; (i) a soft wrist exoskeleton designed by [23]; (j) a pneumatic soft wrist exoskeleton (Exo-Wrist) designed by [37]; (k) a soft robotic device designed by [34]; (l) a soft wrist assist (SWA) designed by [24,25]; (m) a wearable wrist and forearm exoskeleton developed by [26]; (n) an advanced service robot (ASR) a shape memory alloy (SMA)-based hand exoskeleton designed by [38]; (o) SMA-based wrist exoskeleton designed by [27]; (p) SCRIPT passive wrist orthosis (SCRIPT-SPO) designed by [28], as reported in [15]; (q) a hand and wrist exoskeleton designed by [14,29]; (r) and a low-profile wrist exoskeleton designed by [30].
3.1. Rigid Devices
3.1.1. Development of a Portable Wrist Exoskeleton (PWE)
Xiao et al. [16,47] investigated the design and control of a 2 DoF (flexion/extension and radial/ulnar deviation) portable, active, and rigid wrist exoskeleton, shown in Figure 4. This exoskeleton was intended for post-stroke rehabilitation at home or for use by workers to provide assistance in industrial settings.
The portable wrist exoskeleton (PWE) has a rigid kinematic chain made of ABS plastic and weighs 360 g. To avoid harm to the user, foam pads are inserted between the rigid parts and the skin. To increase safety and prevent possible injuries, mechanical stoppers limit the RoM to ° for flexion/extension, and ° for radial/ulnar deviation. The power is transferred from the actuator (Pololu 298:1 micro DC geared motor), located on the forearm brace, to the hand brace through gears and links. The maximum torque generated is 2.3 Nm for flexion/extension and 2.5 Nm for ulnar/radial deviation, which are sufficient for rehabilitation applications, yet they may not be adequate for industrial use.
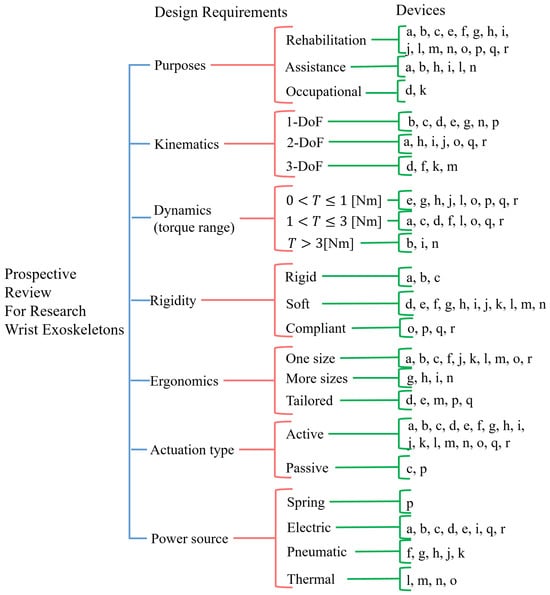
Figure 3.
Schematic of research-wrist exoskeletons grouped by design requirements. Devices, named from (a) to (r), are the same as reported in Figure 2.
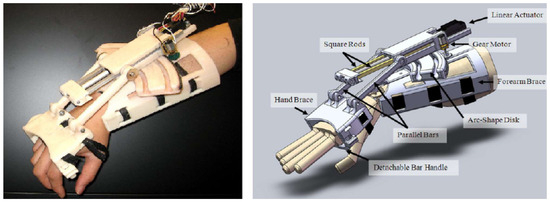
Figure 4.
An older version of the portable wrist exoskeleton (PWE) [47].
Two different control modalities have been implemented: position control for passive, repetitive, pre-programmed movements, suitable for rehabilitation applications; and torque control designed for torque amplification applications, such as for workers’ assistance. As part of the control strategy, the feasibility of classifying surface electromyography (sEMG) signals using a neural network (NN) and support vector machine (SVM) was investigated The experiment involved measuring the sEMG amplitude and torque exerted by the main wrist muscles of a healthy subject. This subject gradually applied maximum voluntary contraction in all wrist directions while having the forearm and hand placed on a rig. The SVM predicted and followed the wrist movement in real time with the greatest accuracy (up to 80.44%), exerting different levels of torque depending on the wrist position. This study suggests that machine learning techniques for motion prediction could be beneficial when performing highly dynamic tasks. However, the requirement for sEMG signals makes it hard to apply in industrial settings, where workers must wear them in contact with the skin.
3.1.2. The eWrist—A Wearable Wrist Exoskeleton
Lambelet et al. [13,17] presented eWrist, a portable and rigid 1-DoF wrist exoskeleton to support flexion/extension in rehabilitation and training. The device, shown in Figure 5, aims to enhance wrist muscle activity in ADLs by measuring the residual sEMG amplitude of stroke patients through a Myo armband, a commercially available sEMG device.
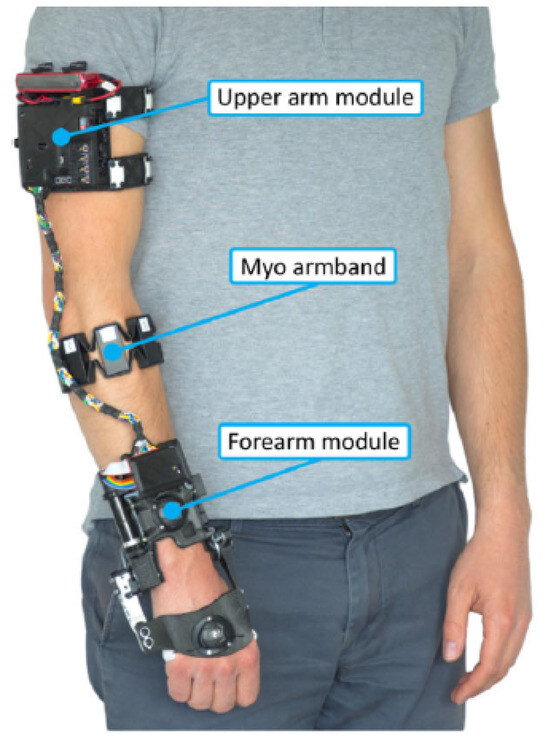
Figure 5.
The eWrist: The first prototype attempt of a wrist exoskeleton for rehabilitation and training designed by [13,17]. It is made of a rigid mechanism and powered by a rotary motor placed on the side of the forearm. It is intended for wrist flexion/extension.
The whole device consists of a kinematic chain made of rigid and soft 3D printed parts, and weighs 556 g, including the battery (80 g) and the Myo armband [17]. A boa closure is used as the tightening system and allows quick and easy one-handed placement. The actuation system incorporates a 12V DC brushless rotary motor (Maxon EC 16) with a total reduction ratio of 475:1, making it difficult to back-drive. Therefore, mechanical transparency is obtained through active control. A two-channel Hall effect sensor, integrated within the motor, determines joint angular velocity and position. A load cell, mounted between the bevel gear and the hand fixation, determines the torque. The battery can power the device for about 125 min in normal use.
A real-time PD controller, integrated into a Raspberry Pi Zero, implements an assistance-as-needed (AAN) support strategy. This adjusts the position and torque output based on several inputs: raw sEMG data from the Myo, force from the load cell, and angular velocity. Two different dynamic behaviors for different rehabilitation settings are available: transparent or resistive. In transparency mode, users can move freely and rapidly with low interaction torques (up to 0.34 Nm); in resistive modality, movements are constrained by higher torque values (up to 1.59 Nm).
The device was characterized based on standardized metrics for rehabilitation devices and, subsequently, tested with healthy and stroke participants. A total of 15 healthy subjects (7 females and 8 males, mean age: 26 ± 3.4) and 2 stroke survivors were recruited (both males, age: 68 and 52 years). Tests performed on healthy subjects showed that it can provide a RoM of 154°, a maximum output torque of 3.7 Nm, a maximum output velocity close to 520°/s, and an average set-up time of 37.3 s. Observations from questionnaires showed that the eWrist was positively received: it helped impaired subjects achieve an RoM comparable to that of healthy subjects; all participants were able to use it independently; and the fixation systems were evaluated as being efficient, secure, and easy to handle. However, some limitations remain in terms of aesthetics, physical proportions, and weight distribution. Some subjects felt discomfort due to a wrong size, alignment mismatch between mechanical and biological joints, and skin pain caused by fixations.
3.1.3. Robotic Orthosis for Wrist Assistance
Sangha et al. [18] presented a wearable 1 DoF robotic orthosis to assist wrist flexion and extension in rehabilitation. The device, shown in Figure 6, weighs 330 g and consists of a rigid aluminum kinematic chain, secured at the palm and forearm by C-shaped clamps and Velcro straps, and 3D printed ABS plastics that cover all the electronics. The actuator is a DC rotary motor with a custom gearbox with a high reduction ratio (1700:1). It provides a nominal torque of 1.12 Nm, and a stall torque of 8 Nm. The device can operate in three different modes according to the patient’s impairment: passive, active resistive, and active assistive. The passive mode assists the wrist movements based on predefined parameters and the patient’s RoM. It is useful for those with muscle weaknesses. The active mode assists wrist movements to augment brain plasticity and decrease muscle spasticity. Assistance is provided after detecting muscular effort with eight force-sensitive resistors (FSR) to record force myography (FMG) signals from the forearm. A neural network (NN) is implemented in Arduino software to process the FMG signals and send the control command to the motor.

Figure 6.
One DoF rigid wrist exoskeleton designed by [18]. Image adapted from [18].
Tested on a healthy volunteer, it has an RoM from 0° (full flexion) to 120° (full extension), a nominal torque of 1.12 Nm, and a battery life of 150 min. Despite its interesting performances and features, such as working modalities, compactness, lightweightness, and cost, further investigations are required to test its efficacy in real scenarios with more subjects (both healthy and impaired).
3.2. Soft Devices
3.2.1. Soft Wrist Exosuit
Chiaradia et al. [11] developed a novel 1-DoF wrist exosuit for assistance at work. It is made up of a soft wrist orthosis and two 3D-printed ABS supports (one for the back and one for the palm), which help to distribute pressure on large areas, bearing cable tension and sensors. The wearable parts, as shown in Figure 7, weigh 300 g. The system is actuated remotely using a Bowden cable transmission and a Kollmorgen motor (AKM23F) with an Apex Dynamics planetary gear drive (PG II 040), and a gear ratio of 10:1. This helps reduce the weight on the human joint and the metabolic impact. A load cell measures cable tension, and 9 DoF inertial measurement units (IMUs) estimate wrist flexion: one on the back of the hand and one on the forearm. The control strategy is based on admittance control for transparency and gravity compensation. The torque exerted on the wrist is compensated for by evaluating an estimated torque (knowing the wrist angle and the cable force). The addition of a PID controller on the angular velocity gives faster assistance by capturing the user’s motion intention.
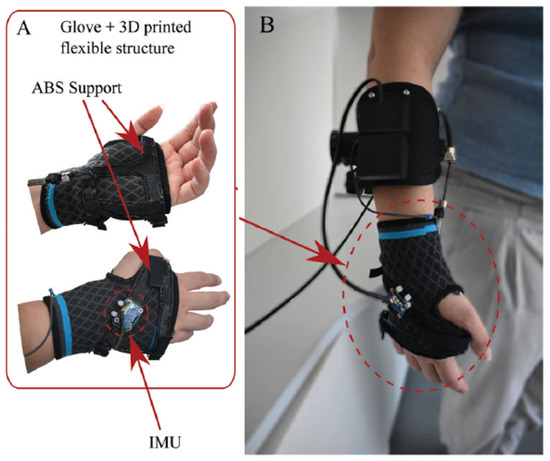
Figure 7.
Soft wrist exosuit designed and developed by [11]. The exosuit comprises a glove that is reinforced through a flexible 3D-printed structure (A) and a strap that wraps around the forearm (B). These two act as anchor points for Bowden cables’. An inertial measurement unit (A) sense the interaction force, the wrist flexion angle, and angular speed.
The device was tested on four healthy participants (all males, aged 28.0 ± 4.0) under both isometric and dynamic conditions. In the isometric test, the participants were asked to keep their forearm and hand parallel to the ground for 3 min while holding a 1.5 kg weight. The dynamic test required the participant to track a minimum jerk trajectory (MJT) that involved a wrist flexion, from 0° to 60° at two different speeds (35 and 70°/s), with and without exosuit assistance, while performing 15 repetitions with a 1.5 kg weight. Overall, the device enhances wrist movement in a range of 150° (70° for flexion and 80° for extension) and can provide 3 Nm torque, sufficient enough to hold 3.0 kg. However, it adopts an external heavy DC motor, which makes it difficult to wear, and the reduction in muscle activation seems lower than with other devices.
Despite its limitations, this prototype is worthy of attention due to its characteristics, such as industrial applications, softness (because of the tendon-driven actuation), comfort, and customization (as the rigid parts are designed following a 3D scan of a human hand). Future developments may include full wearable actuation and control systems, improving the transmission efficiency with a control strategy for friction management and comfort.
3.2.2. Exo-Wrist—A Soft Tendon-Driven Wrist Wearable Robot for a Dart-Throwing Motion
Choi et al. [19] presented a new soft wearable wrist robot called Exo-Wrist, shown in Figure 8. This active device is designed to restore wrist functionalities in weakened upper limbs after injuries, with a focus on the dart-throwing motion (DTM), the most natural wrist movement [48,49,50,51]. It is expected to be used both in clinics and outside of them. The Exo-Wrist consists of a golf glove, a forearm active anchor, and a wrist armlet. On the back of the glove, tendons are placed to transmit forces. The forearm anchoring consists of a truncated cone shape made of soft and flexible materials. This compresses the forearm only when assistance is needed to reduce force losses through friction. The wrist armlet is a silicon-based 3D printed part and is customizable, based on the wrist width, wrist height, and the DTM orientation plane. The use of soft materials and cables makes the whole device comfortable with an overall weight of 1 kg. The DTM plane and wrist kinematics of each individual were measured by using 3D motion-capture sensors (Vicon) to define the tendon path and correctly apply assistive force.
Figure 8.
Soft tendon-driven wearable wrist robot for a dart-throwing motion designed and developed by [19]. Image adapted from [19].
The robot was assessed on three healthy subjects through three experiments, evaluating, respectively, the following: the efficacy of the anchoring system, the motion tracking performance, and the ability not to hinder other movements. Participants sat on chairs with their elbows extended, forearms pronated, and wrists in a neutral position. For the first experiment, each participant was asked to wear the anchor and place their forearm on the setup, which restricted forearm movement. Then the maximum displacement of the forearm anchor was measured at different anchoring wire tensions. For the motion tracking control, participants were instructed not to exert any volitional effort on their wrists while the robot pulled them. The last experiment involved the comparison between the average maximum ROM of the finger joints (by using a goniometer) and the grasp force before and after the actuation of the robot. The results show that without the active anchor, the robot could not provide proper assistance. When the anchoring point was activated and properly tightened, the robot could assist by more than 0.5 Nm, otherwise, it could not generate more than 0.2 Nm, which is less than what is required for ADLs (0.35 Nm). The robot could extend the wrist along the DTM plane for more than 50°, which is more than what is needed for constraint-induced movement therapy (CIMT, 0–20°), and it did not affect movements at the elbow, shoulder, and fingers.
3.2.3. A Soft Robotic Orthosis for Wrist Rehabilitation
Bartlett et al. [20] proposed a home wrist rehabilitation soft device designed for patients suffering from hemiparesis after a stroke. The device shown in Figure 9 is pneumatically actuated, portable, and soft; it weighs 2.26 kg. It consists of a glove, an elbow sleeve, and a Boa ratchet tensioning mechanism, which facilitates donning and doffing with one hand and adaptation to different arm lengths. The actuation mechanism consists of pneumatic artificial muscles (McKibben actuators) anchored on both the palm and the back of the hand. The size is crucial: a tube diameter of 1/2 in. (approx. 12.5 mm) can exert a contractile force close to 120 N, at a pressure of 30 PSI (approx. 200 kPa), which is enough for rehabilitation. The anchoring points determine the initial actuator length and, thus, affect contraction length, RoM, and force direction.

Figure 9.
Soft robotic wrist orthosis [20]. Image adapted from [20].
The device works on the agonist-antagonist principle: a single movement can be generated by activating a pair of actuators (e.g., the two in the palm for flexion, and the two in the back for extension, etc.). The air pressure of each actuator is constantly monitored and modulated by a controller, which reads the status of pressure sensors and gives the input signal to a pump and relevant valves. The device is tested on a mannequin hand and on a healthy subject for assessment. The user was instructed to fully relax his wrist while the robot is actuated. The results show that it can support all wrist DoFs by providing assistance over a range of 91° in flexion/extension, 78° in pronation/supination, and 32° in radial/ulnar deviation. When presented to a group of stroke patients, the participants provided positive feedback regarding its use in therapy.
3.2.4. Active Support Splint Driven by a Pneumatic Soft Actuator (ASSIST)
Sasaki et al. [21] developed ASSIST, an active soft wrist splint used to assist the elderly or people in need of care, making them more independent. The device is shown in Figure 10.
Figure 10.
Outlook of the ASSIST device from [21]. Image adapted from [21].
Two different types of ASSIST were created: one for assistance in the whole RoM (type I), and the other for increasing muscular endurance (type II). They differ in the McKibben structure of artificial muscle actuators. Both devices consist of plastic interfaces, on the palm and back, to which two rotary soft pneumatic actuators are attached. Reinforcements at the ends allow the actuators to bend circumferentially, providing enough bending angle and torque for wrist assistance. The devices weigh almost 390 g. ASSIST is controlled by measuring the wrist angle with flex sensors and keeping the inner pressure constant. At 400 kPa pressure, type II provides almost 80° rotation and 1 Nm of torque; while type I allows the same bending angle with a lower torque (0.25 Nm). In contrast, the torque of type II decreases faster as the bending angle increases.
These devices were assessed on five male subjects by measuring their performance. In these experiments, the human wrist was bent by ASSIST without any human muscular effort. To evaluate the effectiveness of the assistance, both the bending angle at the human wrist and the amplitude of sEMG signals at the flexor carpi ulnaris were measured. The results showed their suitability in correctly bending the wrist, and reducing muscular effort while lifting 3 kg. Although the results are not statistically significant, these devices have promising capabilities for industrial applications. However, there are drawbacks; further analyses and more data are needed to verify the benefits of prolonged use, make the devices fully wearable with a pressure tank and compressor above 400 kPa, and assess the reliability and control of the actuators’ behavior.
3.2.5. A Soft Robotic Wrist Brace with Origami Actuators
Liu S. et al. [22] designed a low-profile, active, and soft robotic (SR) wrist brace that is pneumatically driven and has 2-DoF (flexion/extension and radial/ulnar deviation).
It consists of eight modular soft origami-patterned actuators (SOAs), a commercial wrist brace, and rigid anchors made of fabric to fix the actuators and transmit forces, as shown in Figure 11. Due to the inherent compliance of its materials, the SR brace enables safe interaction, is lightweight, compact, comfortable, and can accommodate various wrist sizes. The part worn on the wrist weighs 214 g (each SOA weighs approximately 1.9 g), but the overall device weighs almost 1.76 kg, including the actuation system and batteries.
The actuation system includes four identical two-SOA units and two diaphragm air pumps. The device works by alternately contracting and expanding the actuators (e.g., during flexion, actuators on the dorsal side of the wrist elongate, while those on the palmar side contract). The axial deformation exhibited when pressurized is converted into significant bending due to anchoring constraints. The control architecture consists of a high-level and a low-level controller. The high-level controller estimates the wrist position, depending on the pressure feedback from each actuator, and compares it with the desired motion. Thus, a pressure command is sent to the low-level controller to regulate the SOA pressure and elongation.
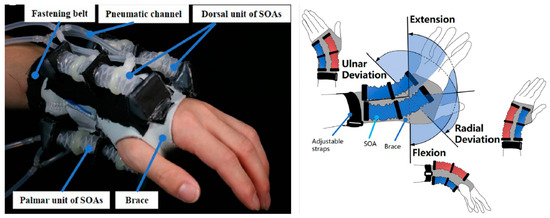
Figure 11.
A robotic wrist brace with origami actuators, developed by [22]. The actuators are placed on both the dorsal and palmar hand sides. Their elongation and contraction states are marked, respectively, in red and blue.
The device assessment was based on the RoM, output force, wearing position adaptivity, and performance. The RoM was measured with and without external loads (100, 200, and 300 g). The maximum values, at = 160 kPa pressure, were 30° in extension, 31° in flexion, 33° in radial deviation, and 22° in ulnar deviation. They decreased as the load increased. The force exerted achieved up to 7.5 N in flexion/extension, and 6 N in radial/ulnar deviation. The torque reached up to 0.76 Nm and met the functional requirement for rehabilitation therapy. The performance, assessed with an IMU sensor, showed that the device consistently followed the planned flexion/extension, while it had less stability in ulnar/radial directions. Although the results are promising and comparable to existing devices, future work will aim to optimize the design, improve compactness and portability, and validate the effectiveness and side effects of specific rehabilitation therapies.
3.2.6. Bioinspired Musculoskeletal Model-Based Soft Wrist Exoskeleton
Ning Li et al. [23] describe a novel soft wrist exoskeleton for stroke rehabilitation and ADLs, as shown in Figure 12.
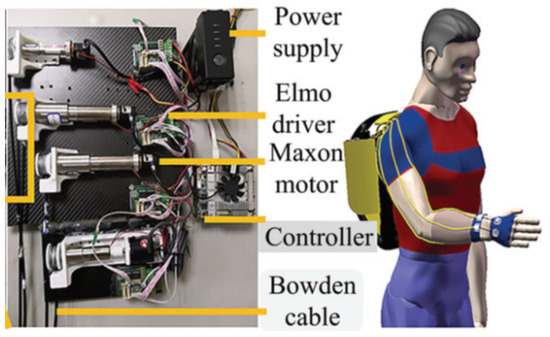
Figure 12.
A soft wrist exoskeleton developed by [23]. The model comes from OpenSim simulation software.
They used commercially available components (motors, commercial body protectors, sensors, power supply) and investigated the distribution of muscle tension lines to identify the most efficient path along which artificial tendons should be placed to correctly move the wrist. They analyzed the kinematics of wrist muscles and simplified this to four main muscles: extensor carpi radialis longus (ECRL), extensor carpi ulnaris (ECU), flexor carpi radialis (FCR), and flexor carpi ulnaris (FCU), which were arranged to form a quadrilateral around the wrist. This design guarantees a more natural interaction with the user. To compare the exoskeleton movements with a real wrist, a Vicon tracking system was used to capture the wrist trajectories of healthy subjects and those produced by the exoskeleton mounted on a hand mannequin.
The assessment was conducted in simulation (OpenSim software), and on healthy and impaired subjects. One healthy volunteer and three stroke (hemorrhagic) survivors (three males, age range 32–57 years) were enrolled for clinical trials. First, tests were conducted on a healthy subject to have a baseline. The wrist motions were captured by Vicon, and sEMG signals at the forearm were measured when lifting a 5 kg weight during wrist flexion with and without exoskeleton assistance. Then, tests on stroke patients were carried out to verify the clinical assistance effects. Overall, the device was able to cover the daily RoM requirements with a flexion/extension range of 115°, and a radial/ulnar deviation range of 70°. When tested on stroke patients, the device demonstrated an average 90.3% ability to recover healthy wrist motions in ADLs (e.g., drinking action was selected to evaluate the assistance effect of the exoskeleton). Moreover, by measuring the forearm sEMG signals from a healthy subject during the 5 kg lift, the exo exhibited more than a 40% reduction in muscle activation. The overall results are consistent both in simulation and real scenarios, and pave the way for new and even better-performing soft wrist exoskeletons. Although it is designed for rehabilitation and daily life assistance, the halving of muscle effort in lifting 5 kg is a great achievement and similar solutions could also be adopted in industry.
3.2.7. Exo-Wrist: A Wrist Exoskeleton Actuated by Pneumatic Muscle Actuators
Andrikopoulos et al. [37] developed a novel soft 2-DoF robotic wrist exoskeleton for rehabilitation, powered by pneumatic muscle actuators (McKibben actuators).
The device, shown in Figure 13, consists of a wearable elastic neoprene-based glove. It adopts four pneumatic muscle actuators (PMAs), symmetrically distributed around the forearm, to function antagonistically and generate wrist flexion/extension and radial/ulnar deviation. PMA is like a tube, fixed to the glove with plastic supports, and it is characterized by a decrease in length when pressurized. The design uses a few hard materials and enhances lightness, comfort, and safety, with a total weight of approximately 430 g.
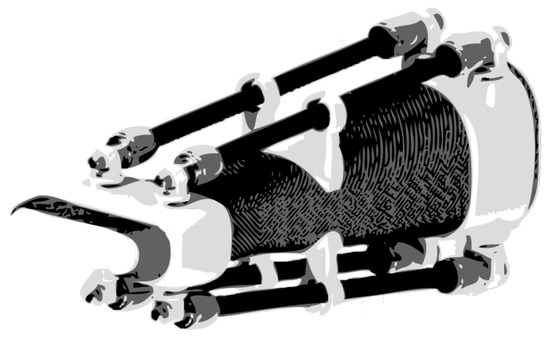
Figure 13.
Soft wrist exoskeleton driven by pneumatic actuators and developed by [37]. Image adapted from [37].
Exo-Wrist’s performance was evaluated on a healthy, passive male volunteer without any medical history of hand and arm issues, to demonstrate its motion capabilities and safety. The motion test involved executing wrist flexion/extension and ulnar/radial deviation movements, with the patient’s arm lying parallel to the floor. To achieve the maximum RoM, PMA should first be inflated to half its maximum stroke. The device, measured with an IMU placed on the back of the hand, can reach ° in both flexion/extension and radial/ulnar deviation in less than 1 s. The pressure range is 0 to 8 bar, with a maximum operating pressure reaching 630 N of the delivered force. The control strategy adopts an advanced nonlinear PID (ANPID) algorithm, which allows tracking of pre-defined sinusoidal motions with smooth, fast, and accurate PMA responses. The safety was assessed by placing FSR force sensors between PMA connections and the human skin to measure the contact forces, as they are the main sources of torque. The shear forces generated remain low, not exceeding 2.2 N, and the respective generated torques remain under 0.055 Nm. The results prove that the Exo-Wrist has potential in rehabilitation scenarios. However, there is a need for further improvement, especially in the actuation system, to make the device fully wearable, portable, and safe, since high levels of pressure are required and must be supplied from a compressor or high-pressure tank.
3.2.8. Carpal Tunnel Syndrome Soft Relief Device
Zhu et al. [34] proposed a novel device to alleviate carpal tunnel syndrome (CTS) strains and pain by actively adjusting the wrist angle when operating in awkward postures for a prolonged time, e.g., while typing on a keyboard.
The device, shown in Figure 14, consists of an elastic fabric sleeve that can be worn like a glove, and two thermoplastic (TPU) airbag actuators (eight-flanged bladders) sewn onto it. They are located at the lower and top part of the sleeve to extend and flex the wrist, respectively, by dynamically pressurizing and depressurizing them.

Figure 14.
Soft wrist exoskeleton designed by [34] to alleviate CTS: (a) the whole device; (b) the airbag actuators.
The performances were assessed on a hand mannequin by lifting the hand, with an external load of 200 g, to a height similar to that of a keyboard (1.9 cm). The device was able to lift the hand above 2 cm under a pressure of 31 kPa and from 0° to around 65° in 9 s, under a maximum pressure of 62 kPa. Although this device has interesting characteristics, such as soft actuation, breathable material, safety, ease, and a compact design, it needs further development regarding the design, control, and experimental evaluation with subjects. CTS problems are highly topical and need special attention for the well-being of workers.
3.2.9. Wrist-Assisting Soft Wearable Robot with Integrated SMA Muscle
Jeong et al. [24,25] proposed a novel shape memory alloy (SMA)-based wearable robot that assists 2-DoF (flexion/extension and radial/ulnar deviation) wrist motions in performing ADLs.
SMA actuators are metallic alloys that deform when heated above their transformation temperature and reduce their length to between 3 and 5%, depending on the type and shape of the alloy chosen. SMA has potential properties as artificial muscles since it can produce high forces and can be fairly rapidly actuated via Joule heating. Furthermore, if shaped as a coil spring, it can produce forces up to 10 N, a contraction ratio of 40%, and strains over 200%, achieving performances higher than that of SMA shaped as wires [27].
The device, shown in Figure 15, named soft wrist assist (SWA), consists of a fingerless glove, a forearm Velcro strap, and an elbow-anchoring Velcro strap to adapt to different users’ sizes, and prevent and improve dislocation and slip [24]. Moreover, to transmit forces properly, actuators are fixed on the glove with non-stretchable fabric. Five muscle-like actuators are attached at various positions: three to the back of the hand, and two on the palm. They are designed as coil springs, integrated into an active and stretchable coolant vessel, and filled with mineral oil, for improved heating and cooling response. The wearable parts weigh 300 g, while the total mass, including the pump and radiator, is around 1.92 kg.
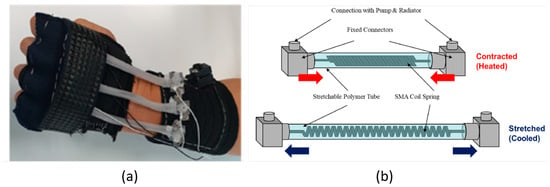
Figure 15.
SMA-based wrist wearable robot developed by [24]: (a) the real device; (b) the SMA actuator design.
The device can produce combined wrist movements, such as radial extension and ulnar flexion by selectively activating the actuators. First, the overall RoM, torque, mechanical performance, wearability, and set-up time were assessed on a hand mannequin, and then on five healthy subjects (three males and two females). The ROM was measured through absolute magnetic encoders that were attached to the wrist joint. The average RoMs were 38°, 50°, 34°, and 35°, respectively, for flexion, extension, radial, and ulnar deviation. The maximum torques, measured on a 3D-printed arm mannequin, were 1.32 Nm during extension, while greater than 0.5 Nm for the other motions. Tests with external loads (1.5 kg and 3 kg) have shown that the torque assistance provided an average increase in support of 62.81%, 101.65%, 58.11%, and 44.23% in flexion, extension, radial and ulnar deviation, respectively. The average wearing time was 87 s (if self-worn), and 75 s (if assisted by another person).
These performances are in line with rehabilitation targets. However, some issues still have to be solved: the anchoring system (Velcro straps) could not perfectly prevent dislocation and should be modified to ensure stronger fixation and faster locking. The robot’s size and shape should be optimized for all users, reducing discomfort due to actuator misalignments. Full wearability can be guaranteed by reducing weights and keeping working temperatures as low as possible to prevent the burning of the user’s skin.
3.2.10. Wearable SMA-Based Wrist and Forearm Exoskeleton
Hope and McDaid [26] proposed a novel 3-DoF (flexion/extension, radial/ulnar deviation, pronation/supination) wearable and portable wrist–forearm SMA-actuated exoskeleton, for rehabilitation at home, or to help people perform ADLs.
The exoskeleton, shown in Figure 16, is active, soft, compact, has a low profile, is lightweight (950 g), and has low noise. It is attached to the user at three points: hand, wrist, and forearm. Forces/torques are transferred from SMA actuators to the limb by tendon–pulley mechanisms, which adopt wheels of different radii for force amplification, arranged around the forearm. Each DoF is controlled independently through a tendon module and an SMA actuator, for a total of six tendons and related mechanisms. This arrangement allows complex combinations of movements (e.g., DTM) based on agonist–antagonist principles by varying SMA lengths through Joule heating. The wire tension is released after cooling, which occurs through conduction and forced convection heat transfer with fans. The tendon length is selected to permit free movements, covering the maximum RoM; moreover, a potentiometer, fitted into the amplification wheel, measures the SMA wire linear displacement. Six force sensors, arranged around the hand, provide information on flexion/extension and radial/ulnar deviations. A variable stiffness model and active stiffness control of SMA actuators were implemented. The stress and position of SMA wires are determined by potentiometer and force sensors. A closed-loop PID controller modulates the duty cycle of the voltage applied to each actuator, according to a target strain/position.
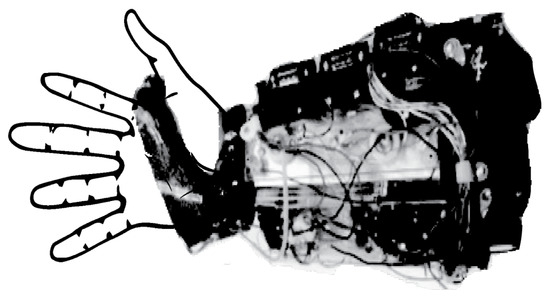
Figure 16.
SMA wrist–forearm exoskeleton for home rehabilitation developed by [26]. Image adapted from [26].
Two prototypes were tested: one using an SMA actuator and a compensation spring, and another using SMA actuators in differential configuration. The assessment was done by measuring tendon displacement on a test bench while lifting a variable load and tracking different trajectories (step, sinusoidal, and triangle waves). The expected displacement of the actuators in the spring-bias configuration covers 40% of the expected RoM, while the differential module covers 65%. In both cases, the major issues are related to friction (especially at lower strain rates and duty cycles), tolerances in the mechanical components, and the uncontrolled pre-stresses on the SMA wires. Further potential improvements could include a quantitative analysis of system friction to generate better and smoother control; a more effective cooling system rather than miniature fans, integration of sEMG sensors on the forearm cover as an additional sensing method; and the redesign of each module to reduce the overall weight and fit different sizes.
3.2.11. ASR: A Wearable Glove for Hand Grasping
Hadi et al. [38] presented the ASR (advanced service robot), a 5-fingered SMA-based hand exoskeleton for grasping rehabilitation and assistance, for use in clinics and at home.
ASR, as shown in Figure 17, is active, portable, light (300 g without electronics and batteries), compact, and noiseless. Its actuation system consists of two fishing wires for each finger (attached to the proximal and distal phalanges), an SMA actuator for each fishing wire (for a total of 10 SMA), and guides for connecting wires and transferring the force. The SMAs are fastened to a rigid platform on the forearm, and use 1 m of Flexinol with a diameter of 0.38 mm, which can produce 22.5 N force. When the actuators are heated up with a current of 2.2 A, their tension force and length variation are transformed into the motion of the phalanges and hand grasping.

Figure 17.
ASR: An SMA-based hand exoskeleton designed for grasping assistance [38]. Image adapted from [38].
A theoretical model that correlates tendon tension and grasping force was developed and experimentally assessed by using two load cells to measure fingertip and tendon forces, a signal amplifier, and an Arduino Uno microcontroller to record data. The results show good agreement between theoretical and experimental values. The device was assessed on a volunteer. The force exerted on the fingertip is 35% of the force produced by the SMA actuator. The total grasping force is more than 40 N, which is sufficient for typical ADLs (18 N). The overall speed of hand closure is 3 s, while it takes about 4 s to open by cooling down the actuators using air fans. Although not directly intended for wrist assistance, due to motion synergies between the hand and wrist, problems at the wrist level reduce grasping ability; therefore, this device could be considered a valuable wrist support. Current drawbacks include a lack of full wearability, due to the integration of sensing and control systems not yet being implemented, along with the absence of user trials. Moreover, the high currents required (2.2 A) might pose risks for real-world applications.
3.3. Compliant Devices
3.3.1. SMA-Based Wrist Exoskeleton
Serrano et al. [27] proposed a rehabilitation-wearable wrist exoskeleton with 2-DoF (flexion/extension and radial/ulnar deviation) based on SMA actuators. The device, shown in Figure 18, is a hybrid, due to the rigid kinematic chain around the joint actuated by remotely placed flexible materials.
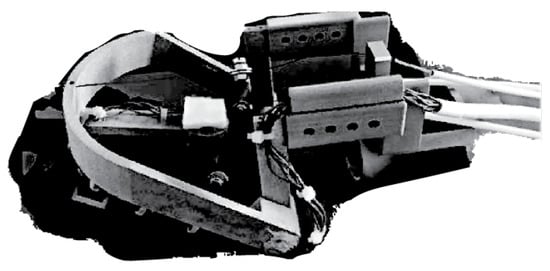
Figure 18.
SMA wrist exoskeleton for rehabilitation developed by [27]. Image adapted from [27].
Flexinol® is used as an SMA actuator (0.51 mm of diameter), which can exert 35.6 N of force and more than 0.5 Nm of torque. One SMA wire is used for each movement, except flexion, which is left under gravity. The exoskeleton is made of simple and low-cost parts through 3D-sintering polyamide with aluminum powder. The rigid interfaces are sewn on a glove to ease wearability. The device is symmetrical and can be worn both on the right and left hands. The overall weight, considering the actuators, is less than 1 kg, and the price is approximately USD 1060.
The feasibility of the system was first tested on a simulator and then in real cases. Biomechanics of Bodies (BoB) software was used to select the proper actuation systems, and evaluate human body biomechanics, mechanical designs, and control algorithms. Subsequently, a pilot study was conducted on three healthy subjects. The results showed the device allowed a RoM between + 40° and −10° in flexion/extension; and between + 30° and −10° in radial/ulnar deviation. In both cases, the exoskeleton could follow a reference movement with little error. For a proper displacement of the wrist, 2.2 m-long SMA wires are needed for extension, and 1.7 m for radial/ulnar deviation.
The main difficulty involved when controlling SMA actuators is their hysteresis, which introduces non-linearity in the system. Thus, a BPID controller (a combination of a standard linear PID controller with a bilinear compensator) has been used for a single SMA wire. This device could serve as a noiseless and low-cost alternative to current rehabilitation robots. While its inherent flexibility allows easy adaptation to the body, wearability remains an issue due to the encumbrance of long cables and the high temperature required to activate the actuators.
3.3.2. Script: A Passive Orthosis
Ates et al. [28] developed a hand and wrist exoskeleton for post-stroke rehabilitation at home, which provides compliant and adaptable extension assistance during ADLs.
SCRIPT was designed with both passive and active actuation. However, even though the active systems offer more benefits, their architecture is more complex, heavier (1.5 kg), and bulkier. Thus, the authors focused on improving the passive mechanisms with dynamic interaction. The device in Figure 19 is called SPO-F, and represents the final achievement after four design architectures described in [28]. It is a hybrid solution involving a rigid kinematic chain with a soft actuation system (springs and cables). It provides assistance along 1-DoF wrist and finger extension to overcome the hyper-flexion problems and restore a more functional position. The finger mechanisms consist of 3D-printed stiff levers connected with digit caps via a Dyneema cable, and actuated via an extension spring. The wrist mechanism is a 3D-printed double parallelogram that transfers the torque to the hand plate thanks to an extension spring. Each spring force can be adjusted by individual ball chains. As rigid interfaces, off-the-shelf ergonomic components from SaeboFlex [33] are used and are available in different sizes (S, M, L, XL) to ensure a better fit for each subject.

Figure 19.
SCRIPT passive orthosis. The SPO-F design developed by [28].
The device RoM was assessed by using rotary position sensors (potentiometers), an Arduino Nano micro-controller, and a visual marker on the hand plate for motion tracking. The results show that the device can rotate up to 45° in flexion and 30° in extension. Assistance is proportional to hand flexion, spring stiffness (k), lever length, and placement. The forces and torques are measured, via force sensors for different stiffness values and pre-tensioning forces at fixed k = 0.5 N/mm. In all cases, the minimum torque is higher than 0.5 Nm, while the maximum is 2 Nm at 60° of extension.
The first SPO orthosis was tested on 33 stroke patients in 3 different EU countries. This helped address the final design of SPO-F, which looks lighter (650 g), safer, more professional, comfortable, compliant, simple, easy to wear, and able to satisfy rehabilitation requirements according to a stroke patient. Despite the great achievements obtained over the years, the design should be further improved in compactness due to its vertical profile. Furthermore, the extension force applied on the digits should be assessed with more patients because the compression applied might cause some finger pain.
3.3.3. Hand and Wrist Actuated Exoskeleton for Rehabilitation and Training
Dragusanu et al. [14,29] developed a 2-DoF (flexion/extension and radial/ulnar deviation) active and hybrid exoskeleton to allow people with disabilities to regain autonomy.
The device, shown in Figure 20, consists of a tendon-actuated mechanism with thermoplastic interfaces, which allows remote actuation and user adaptation. All actuation and electronic components are placed on the forearm, and data are transmitted via Bluetooth. The device is composed of two independent rigid parts tailored to the user: one on the hand and the other one on the forearm. Three tendons, wrapped around three pulleys, connect the motors on the forearm to the hand plate. Dynamixe XL-320 DC rotary motors are selected, with a stall torque of up to 0.39 Nm at 7.4 V, which is suitable for rehabilitation applications. The whole system weighs almost 300 g, and costs about USD 150. The control consists of tracking wrist movements by measuring the orientation of the hand with respect to the forearm using IMUs (on the hand and forearm). A Matlab GUI interface was developed to guide the users during rehabilitation, making the whole process easier to set and less boring.
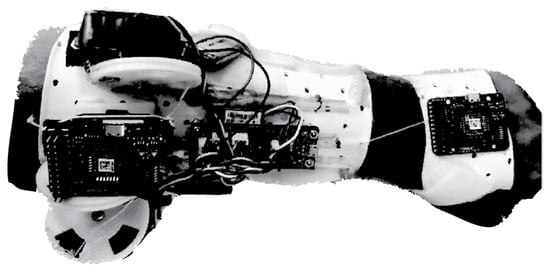
Figure 20.
Exoskeleton for wrist rehabilitation developed by [29]. Image adapted from [29].
This wrist exoskeleton has become a module of a full hand/wrist exoskeleton developed by the same authors [14], which can actuate finger flexion/extension, work for about 3 h, and has an overall weight of 500 g. The updated version of the wrist comes from user feedback on wearability and anatomical adaptability. Subsequently, all rigid interfaces and the actuation module were redesigned with a parametric approach: pulleys connected to the motor shafts are reduced in dimensions; external support is added to wrap the excess wire; an automatic closure for the forearm module is designed to ease and halve the wearing time. The structure and control are developed to guarantee the use of hand and wrist modulus independently.
The device’s performance was assessed by having a patient execute three exercises: flexion/extension, radial/ulnar deviation, and recording and reproducing a movement performed by a physiotherapist. A predefined set of movements was generated. Among the 60 trials, the average root-mean-square (RMS) errors in the following flexion/extension and radial/ulnar deviation movements were found to be not normally distributed, and had statistically significant differences for different motor speeds (). This device has interesting features and great potential for use in rehabilitation. It can assist all wrist movements, is portable, wearable, affordable, lightweight, easy to control and manage autonomously, and has a TRL of 4. However, some improvements could be made to reduce the overall encumbrance and weight, and improve the torque provided.
3.3.4. Low-Profile Two-DoF Wrist Exoskeleton
Higuma et al. [30] developed a 2-DoF rigid wrist exoskeleton for rehabilitation, which allows flexion/extension and radial/ulnar deviation movements.
The mechanism, shown in Figure 21 consists of a hand back support, a forearm base where two linear actuators are placed, and two steel spring blades that connect the motors to the hand. The device is inherently flexible thanks to elastic elements, which can deform during motion and adapt to the wrist center of rotation while transmitting forces. Each linear actuator moves a spring blade independently, back and forth, allowing bidirectional force transmission. The device is made up of 3D-printed resin, it is 310 mm in length and weighs 509.5 g.
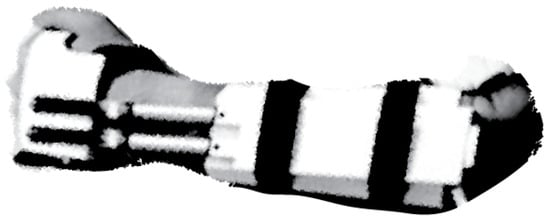
Figure 21.
Low profile 2-DoF wrist exoskeleton for rehabilitation developed by [30]. Image adapted from [30].
Performances measured on a test bench showed a RoM that is in good agreement with finite element analysis (FEA) results, encompassing the range seen in healthy subjects: 56.7° in flexion, 68.1° in extension, 39.5° in radial deviation, and 13.8° in ulnar deviation. The constraints are mainly due to the limited stroke of the actuators. The torque varies from 0.26 Nm (max flexion) to 2.47 Nm (max extension), with an average of nearly 0.65 Nm for radial and ulnar deviations. The maximum load applied perpendicular to the wrist is 10.24 N for flexion/extension, with a shear force of 7.98 N; while for radial and ulnar deviations, it is 4.26 N, with a shear force of 4.14 N. Despite small interaction forces, a human evaluation is required to verify whether it harms the user.
Overall, it is a simple mechanism with a fairly soft structure, reducing the strain on the wrist during movement However, since linear actuators are not manually back driven, when turned off, the fixed position of the blades may exert some shear force on the user’s skin. Moreover, the absence of a defined center of rotation could make the springs deform in unwanted ways, increasing discomfort.
4. Commercial Devices
When searching online, one can observe how difficult is to find devices designed to assist workers’ wrists. Most of them are designed for rehabilitation and training, or are still prototypes that are unable to jump out from research labs and hit the market. In 2020, Forbes published an article titled “The Number Of Companies Making Industrial Exoskeletons Has Been Quietly Increasing For The Past Five Years” [52]. One of the main contributors was Borislav Marinov, a founder of the ExR—Exoskeleton Report website [53]. Borislav pointed out that a comprehensive definition of what constitutes an “industrial exoskeleton” has to be defined [52]. The Wearable Robotics Association (WearRA) estimated that the total number of businesses engaged in manufacturing or distributing industrial exoskeletons increased by 350% between 2015 and 2020, increasing from 16 to 56 companies (as shown in Figure 22), and exceeding 700% to date, with almost 120 companies around the World [52,53].
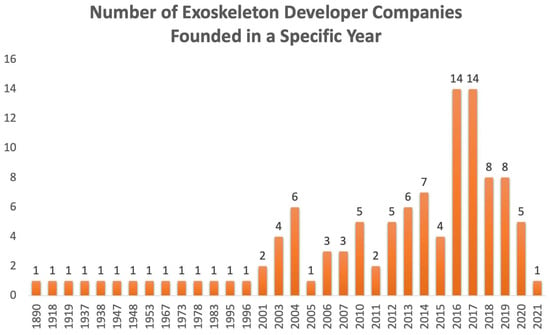
Figure 22.
Statistics from the resources available on the ExR—Exoskeleton Report website [53].
One reason behind this increase may depend on a recent shift in the perception of the exoskeleton, not as something that makes people either “superhuman” or “better”, but rather as a specific tool, which could be worn and help workers complete physically repetitive tasks safer and more efficiently.
To gain an understanding of the exoskeletons that have been introduced to the market in the last decade, the website ExR—Exoskeleton Report (https://exoskeletonreport.com/product-category/exoskeleton-catalog/, accessed on 14 March 2023) has become relevant. It could be regarded as the widest repository/catalog of exoskeleton devices for all application domains [53]. Examining the body area section, one could observe a lack of devices intended for wrist assistance. These deficiencies make the research and development phases more difficult since there is very little information. Hereafter, we propose a list of devices, already available on the market, which involve the wrist in their assisted segments. All devices taken into account, which will be described in the following sub-sections, are shown in Figure 23, and are grouped according to structural stiffness criteria. Moreover, based on the wrist exoskeleton requirements proposed in [15], the schematic shown in Figure 24 provides relevant information about commercial wrist exoskeletons.
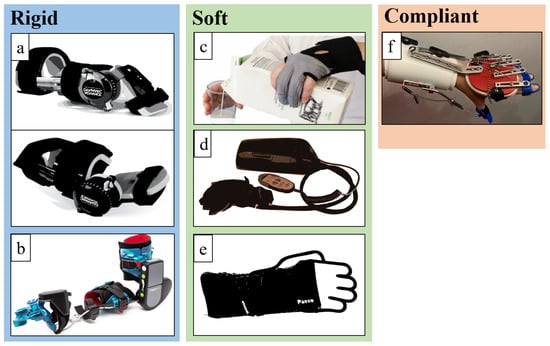
Figure 23.
All commercial wearable exoskeletons for wrist assistance. Devices are grouped by stiffness criteria in rigid (a,b), soft (c–e), and compliant (f). From top left to bottom right, it is possible to find (a) JAS wrists from Joint Active Systems [31]. Re-edited images; (b) MyoPro designed by Myomo [32]. Image used with the permission of the Myomo company; (c) Carbonhand designed by Bioservo [54]; (d) Ironhand designed by Bioservo [55]. Re-edited image; (e) Paexo Wrist designed by Ottobock [36]. Re-edited image; (f) soft orthosis designed by Saebo [56].
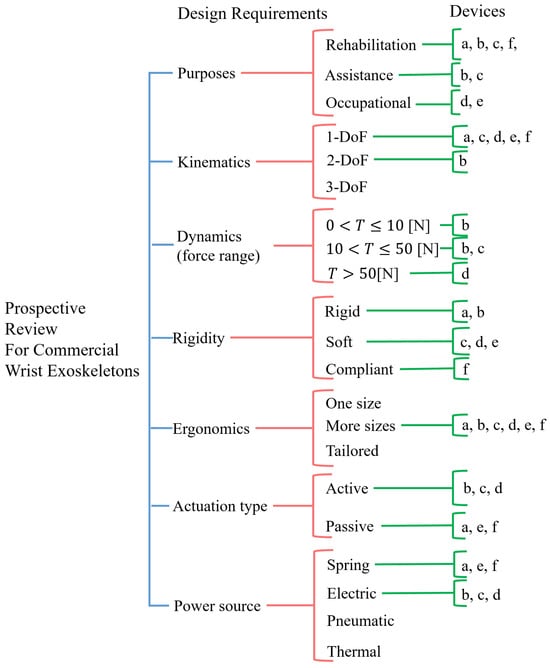
Figure 24.
Schematic of commercial wrist exoskeletons grouped by design requirements. The devices, from (a) to (f), are the same as reported in Figure 23.
4.1. Rigid Devices
4.1.1. JAS Wrists
These products are developed by Joint Active Systems, Inc. (JAS), which is a leading company in the US for range-of-motion therapy for patients with motion loss. They provide a wide range of options for assisting different limbs and joints, to meet the needs of each patient; moreover, they provide some open-source data/analyses that demonstrate the effectiveness of these devices. The company proposes a well-structured protocol for starting ROM therapy after an injury or surgery. Their pioneering device for wrist support is the JAS static progressive stretch (SPS) wrist. It utilizes the proven principles of SPS to achieve permanent restoration of joint ROM. It is intended for injuries, such as distal radius/ulnar fractures, carpal fractures, and ligament/tendon repairs. Clinical studies carried out in more than 60 patients with deficits in wrist flexion or extension ROM, or healed distal radius fractures, have shown an increase in ROM and grip strength after six months of therapy [57,58].
However, among all their products oriented to the wrist joint, we would like to focus more on the devices known as advanced dynamic wrist flexion and extension [31], as shown in Figure 25, as they seem more practical and comfortable for use outside of clinics, such as at home to enhance therapy, during sleep, or during periods of rest to achieve permanent RoM gains. These devices are ready-to-fit, low-profile, and lightweight passive rehabilitation orthoses. They include integrated tension control, allowing patients to optimize spring tension by simply rotating a lever by hand.

Figure 25.
Dynamic wrist orthosis for wrist flexion and extension recovery by JAS, Inc. [31]. Re-edited image.
There are not many studies reporting on the Advanced Dynamic JAS Wrist application. In [59], the concept of dynamic splints/wrist extension was tested on 133 patients (78 women, 55 men; mean age 53 ± 17.6), in both surgical and non-surgical patients (respectively, 42 and 91 subjects), following distal radius fractures. The results showed a 62% recovery in active range of motion within 3 to 20 weeks of treatment, with no significant differences between genders, or among patients who received previous surgical intervention. Based on clinical and published evidence, some articles described their safety, usefulness in effectively increasing and restoring RoM for all levels of joint stiffness (e.g., wrist arthrofibrosis), and patient satisfaction [60,61].
4.1.2. MyoPro Orthosis
MyoPro Orthosis originated in 2006 thanks to the work conducted at MIT and Harvard Medical School; it was then commercialized by Myomo, Inc.
The product is a wearable active powered arm orthosis (includes the elbow–wrist–hand) that is designed to restore functionality to a paralyzed or weakened arm, for patients suffering from neuromuscular and neurological diseases or injuries (e.g., stroke arm paralysis, brachial plexus injury, cerebral palsy, multiple sclerosis). The MyoPro weighs approximately 1.8 kg, provides almost 0° to 130° of motion, 7 Nm of torque at the elbow, and 1–2.7 Nm torque for the fingers, ensuring the lifting of approximately 2.3–3.6 kg [62]. The device works by reading faint nerve signals from the skin through sEMG; it then amplifies them and activates motors to move the limb as the user intends, as shown in Figure 26. The wrist joint is intended to improve dexterity and facilitate the recovery of muscle tone and functionality.

Figure 26.
MyoPro device by Myomo, Inc., Boston, Massachusetts, US [32]. Images reproduced with permission from the company.
Since 2017, several experiments have been conducted to evaluate its impact on both in-clinic and at-home rehabilitation for patients with arm weakness resulting from neurological diseases. Over fifty individuals who have been diagnosed with upper limb paralysis caused by spinal cord injury (SCI), chronic stroke, or traumatic brain injury (TBI) have taken part in clinical trials. In [62], a 62-year-old U.S. Army veteran with upper extremity paresis and chronic stroke was involved in the study. He was monitored for three years. During the first year, he primarily received traditional occupational therapy (OT) without an orthosis. This therapy included electrical stimulation, mirror therapy, the use of a massage wand, active assisted and passive ROM, and task-oriented interventions. Starting from the second year, his therapy incorporated the use of a functional grasp MyoPro Arm, both in clinical settings and at home. By the end of the study, he was able to independently open his hand (by 75%), which indicates substantial improvements in ADLs using his paretic left arm, and in his level of independence. In [63,64], two adult males (respectively, 75 and 31 years old) with SCI were involved in the study. The experimental protocol consisted of evaluating the active hand-grip angular position, hand-grip force, and sEMG from the finger flexor and extensor muscles, by having the participants squeeze and open their hands over 18 training sessions at a rehabilitation research center, conducted three times per week (almost 60 min/session). In [65], 18 stroke subjects were selected (11 males, 7 females; average age 55.5 (±21.5) years old) in a single-day-session study to evaluate the device usability, functionality, and efficacy. Most participants were able to don/doff, use the device without any assistance, and hold up to 1 kg weights for 2 min. In [66], 13 volunteers (5 males, 8 females; average age 50.9 (±19.9) years old), including 7 stroke survivors and 6 individuals with TBI, were involved in a pilot study that lasted about 18 weeks. This study involved both in-clinic sessions and home exercise therapy using the MyoPro arm. In-clinic therapy consisted of 2 weekly sessions, with each lasting 1.5 h under the direction of a physical therapist. In [67], 18 stroke patients participated in a 3-month-long home rehabilitation trial (13 males and 5 females; average age 52.5 (±14.7) years old). Before receiving their MyoPro, participants underwent a baseline session where their performance on a range of functional tasks was evaluated (e.g., move the object to the mouth, hold the object in space, stabilize the object, etc.); these tasks were aimed at assessing their capabilities with their paretic side.
Overall, participants showed a high level of satisfaction using the device, and significant improvement in overall task completion (time and correctness in execution); furthermore, compared to the baseline measurements (without the device), they were able to perform bi-manual tasks for prolonged periods; there was an increase in their independence in ADLs, enhanced force while grasping, improved lateral pinch strength, and increased wrist RoM. The use of the device also helped in avoiding the development of wrist ulnar and radial deviations. Notably, no serious adverse events, such as the hyperextension of joints, pain caused by the device, or skin breakdown, were recorded [62,63,64,65,66,67,68].
4.2. Soft Devices
4.2.1. Carbonhand®
Carbonhand, as shown in Figure 27 is an assistive soft robotic glove for use outside of clinical settings; it is built on Soft Extra Muscle (SEMTM) technology [35,69]. It is sold by Bioservo for nearly USD 7000.

Figure 27.
The Bioservo Carbonhand® device and examples of related applications [54]. Legend: (1) SEM unit; (2) cord; (3) arm strap; (4) slap wrap: (5) glove, three-finger version.
It is designed as a glove with pressure sensors in the fingertips to measure contact forces during interactions with objects or tools. Power is applied when the user initiates gripping, ensuring a firm grip. Thus, it activates one degree of freedom: the gripping (or finger flexion). It enhances human capabilities by applying a force of up to 20 N per finger (involving only three fingers). The overall device weighs 685 g (glove plus control unit), but since the control unit and the battery can be placed wherever the user prefers on their body, weight should not be an issue. Batteries are designed to last approximately 8 h and the device is available in different sizes (XS, S, M, L, XL) for both right and left hands. The device is intended for rehabilitation and assistance at home by helping people with reduced hand functions perform ADLs independently [35,69]. This device has garnered our attention because, due to motion synergies, hand dexterity is related to wrist motion and resistance capabilities: problems at the wrist level reduce grasping ability. Therefore, this device could be considered valuable wrist support.
A pilot study in [70] involved 15 participants (18–65 years old) with chronic SCI and impaired hand function. They were given instructions on how to use the device at home for 12 weeks for at least 4 h a day during regular ADLs, while executing task-specific activities, such as squeezing and releasing a softball, simulated drinking, eating a meal, and writing. Participants were asked to keep a diary of their activities. They returned for reassessment after week 6 and week 12 to evaluate grip strength and hand function. Most participants reported that they used the glove 0.3–6 h daily, and the average grip strength across subjects improved from the initial measurement (9.9 ± 2.9 kg) to week 6 (14.0 ± 3.0 kg) to week 12 (14.0 ± 3.2 kg). Recently, it was evaluated over six weeks in a study involving 63 participants (between 18 and 90 years old) with impaired hand functions [71]. The protocol consisted of five assessments for each participant: three pre-assessments over three weeks as baselines before the intervention, a post-assessment within one week of the intervention’s conclusion, and a follow-up assessment four weeks later to gauge the retention of effects. The participants were patients experiencing limitations in hand function and were asked to use the glove for at least 180 min per week during ADLs at home (such as lifting and carrying items, performing hobbies, cleaning, and cooking). The outcome measures included hand grip strength, arm and hand functional abilities, the amount of glove use, and quality of life. Preliminary results have shown promising improvements in grip strength (+27%), pinch strength (+15%), and hand functionality (+12%). Since 2022, it has been approved as a medical device, according to the European Medical Device Regulation (EU-MDR).
4.2.2. Ironhand®
Ironhand® is a soft active exoskeleton designed for grasping assistance and augmentation, built on Soft Extra Muscle (SEMTM) technology, Bioservo Technologies AB, Torshamnsgatan, Sweden. Initially, the development of SEMTM technology (e.g., Carbonhand®) was intended to rehabilitate patients with impaired hand function. Today, Bioservo Technologies is also focusing on preventing injuries at work. The product has undergone long-term testing with various industrial partners, which have become key factors for its quick development since its first release in 2019 for nearly USD 6500 [35,55]. Ironhand 2.0 (https://www.bioservo.com/professional, accessed on 14 March 2023), shown in Figure 28, consists of a sensorized glove, a backpack (containing control and battery units), and a hip-carry, with everything designed in different sizes (S, M, L, XL) to better fit the user’s body. The whole system weighs almost 2.75 kg, with the glove alone weighing 50 g. The lithium battery in the backpack is the ‘sore point’ for the weight, with a full-charge duration of nearly 6–8 h. The glove has force sensors (FSRs) on the fingertips and the palm, and it is innervated with artificial tendons (e.g., Bowden cables), which enhance finger flexion and gripping thanks to the push–pull action of linear DC motors. Enabled when force sensors detect certain pressure levels, the tendon-driven system can generate a maximum force of 16 N per finger (80 N in total) [35,55], adjustable to adapt to different needs and applications, as shown in Figure 29. The device can collect and share data through Bluetooth, 4G, and Wi-Fi among different devices (e.g., tablet, control equipment), and save the data in local storage or the cloud (BioCloudTM); see Figure 29. The collected data can be used to assess the wearer’s risk of developing injuries.
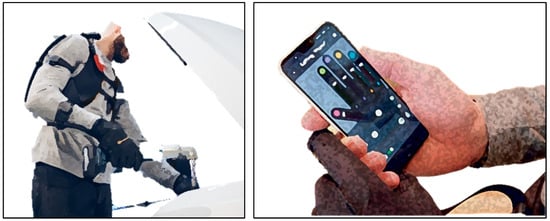
Figure 28.
The Bioservo Ironhand® system and application. Image revised from [35].
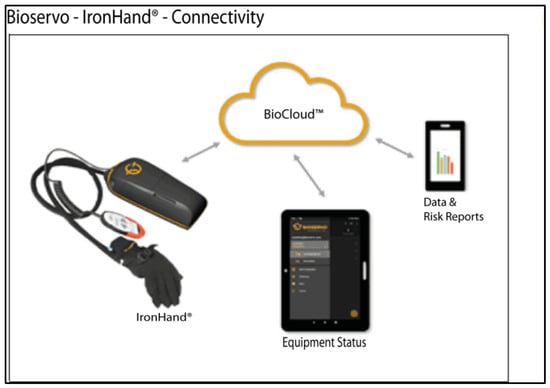
Figure 29.
The Bioservo Ironhand® system control and connectivity. Image revised from [55].
Several clinical trials were conducted on SEM technology over a period of months [54,55,70,71]. The first preliminary study on the effects of Ironhand in working tasks (automotive assembly) was published in [72]. Eight participants (four males and four females) were identified by a General Motors (GM) ergonomist based on the task, which required the hand to be active for most of the work cycle, gripping efforts to manipulate parts/tools, and willingness to use the device for 2 weeks. Muscle activity was recorded using sEMG from the main forearm muscles. For each participant, sEMG was collected on the first day without Ironhand, and on the second day with it. Once all electrodes were properly placed, participants performed muscle-specific isometric maximum voluntary contractions (MVCs) for 3 s. Controlling task, repetition, and cycle variables across participants was not feasible, as each one performed different tasks within a work cycle (approximately 120 s) on the assembly line during an 8-h shift. Examples of these tasks include curtain airbag installation and securing, floor-pan securing, overhead fastener securing, and carrying and installing engine splash guards). Overall, the results have indicated significant reductions in forearm muscle activity, along with improvements in gross hand grip strength, pinch strength, and all hand functions (such as grip, grasp, precise movements, writing, etc.). Further evaluation demonstrated that 59% of the recorded cycles resulted in a reduction in at least one muscle’s activity and 41% resulted in an increase in activity. Thus, when compared to no exoskeleton, Ironhand produced both increases and decreases in forearm muscle activity, depending on the individual and the specific tasks. Therefore, specific use cases need to be carefully determined, with the device optimized for each individual to ensure benefits.
Even if it is a hand exoskeleton designed for grasping augmentation, due to motion synergies, it is safe to assume that grip force and wrist fatigue are, in a sense, correlated. The stronger the grasping, the more compression will be transmitted to the hand ligaments and wrist. However, despite these promising results, in our opinion, this does not mean that reducing grasping fatigue will guarantee the same reduction in wrist workload. Rather, it will reduce the probability of sustaining injuries, inflammation (such as carpal tunnel syndrome), and pain in the wrist joint.
4.2.3. Paexo Wrist®
Paexo Wrist is a commercial passive wrist exoskeleton developed and sold by Ottobock for nearly USD 160. In practice, it is an orthosis that aims to support the wrist while moving loads, as well as prevent injuries and inflammations. It can be used when holding a screwdriver, riveting tool, or welding equipment, and for carrying loads. By looking at the Paexo.com website (https://paexo.com/paexo-wrist/?lang=it, accessed on 14 March 2023) and the user manual, the device adopts innovative solutions: materials for thermal regulation tested in space (provided by Outlast Material), a Pull-2-Lock mechanism for quick one-handed donning in a few seconds, and a metal splint inside the garment, which fulfills the function of a flexible beam to absorb and transfer loads away from the wrist. For better versatility, the device can fit both left and right hands and is available in different sizes (S, M, L) to satisfy different users. No sensors and control strategies have been implemented. The device and its application are shown in Figure 30.

Figure 30.
Paexo Wrist device [36]. Images taken and revised from the Ottobock official website.
The company mentions that the Paexo Wrist is designed to relieve muscles and tendons during prolonged periods of work with tools and in assembly; this is achieved by stabilizing the wrist and ensuring optimal distribution of the workload. Unfortunately, we have not found additional technical details or analyses regarding its positive effects on workers’ health. Thus, we cannot quantify its usefulness compared to other devices.
4.3. Compliant Devices
SaeboFlex
SaeboFlex, shown in Figure 31, is a custom-fabricated wrist, hand, and finger orthosis [73], developed and sold by Saebo, Inc., for nearly USD 600 [33]. It is designed to improve mobility in individuals with hand/wrist weakness or spasticity due to neurological or orthopedic conditions.
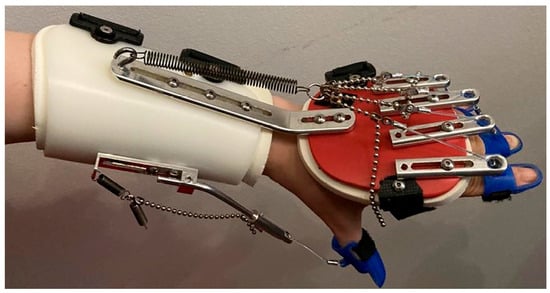
Figure 31.
SaeboFlex device [56].
It is a passive device made of resistive springs and is intended for therapy both in clinics and at home. No sensors or control strategies have been implemented. The primary goal is to position the impaired wrist and fingers into the extension for proper functional grip and release training [73]. The optimum wrist angle is measured at 35° of extension, which is considered the position where maximum grip effort begins. This value can be adjusted according to the patient’s impairment.
Pilot studies [74,75,76] were conducted to explore the feasibility, as well as patients’ and therapists’ experiences, of SaeboFlex training. In [74], ten stroke patients were recruited from a rehabilitation hospital. The experimental group consisted of five patients (three males and two females); the control group included five patients (four males and one female). Subjects in the experimental group underwent four weeks of training using SaeboFlex for one hour per day, five times a week. Each session included nine task-oriented practice sessions involving the hemiparetic arm, such as moving a softball side-to-side and diagonally, reaching a target, and grasping and releasing a softball. Each subject in the control group wore the same orthosis for 1 h per day but did not participate in any upper extremity training. In [75], eight stroke participants (four males and four females; 70 ± 15 years old) with upper limb extremity weaknesses were recruited for 12 weeks of rehabilitation. A battery of measurements was taken at baseline, and then at 4, 8, and 12 weeks. Participants were trained once or twice a day, with sessions lasting anywhere from 5 to 105 min per day. The number of grasp and release repetitions varied between 12 and 500 per day. In [76], the authors focused more on the experiences of patients and therapists using SaeboFlex, utilizing both quantitative and qualitative data from previous clinical trials. Eleven stroke participants (seven males and five females; mean age was 60.2 ± 7.89) were recruited to answer questionnaires following their training program with the device. The questions pertained to the psychosocial impacts of assistive device scales, and how the SaeboFlex supported their ability to do, be, become, and belong. Furthermore, five therapists were enrolled and asked to complete reflective responses for their work with clients. In [56], a 43-year-old woman with left upper extremity spasticity following a stroke underwent a treatment combining botulinum toxin injections and SaeboFlex training. The 16-week program comprised three 50-min sessions daily, focusing on grasping and releasing exercises both with and without the splint. The patient was evaluated before the botulinum toxin injection and again after 6, 12, and 16 weeks. After completing the program, the treatment was found to reduce disability and improve quality of life. However, further investigation is needed.
Overall results from clinical trials and questionnaires conducted over several months on patients who suffered from strokes, as seen in [56,74,75,76,77,78], have proven that the device is safe, improves hand grip strength and dexterity in moving objects, increases wrist extension RoM by 5–6 degrees, facilitates clinically significant improvements in upper limb function, coordination, and velocity, enhances participation and independence in ADLs, and reduces carer burden and associated costs.
5. Design Proposal for a Portable Wrist Exoskeleton
Based on the literature and our experience, in this section, we propose a conceptual idea (TRL 1–2) of a technological device to assist all wrist movements, provide sufficient force support, and guarantee good user acceptance in industrial settings. Softness, lightness, and customization are essential. Although obvious, these are factors that often emerge from user evaluation questionnaires [13,14,19,68]. Therefore, we will design a wrist exoskeleton on a glove to meet comfort requirements. We will customize the device to the user by taking anatomical measurements and utilizing 3D scanning technologies for the hand/wrist shape [11].
The device should facilitate the main movements of the wrist (flexion/extension and radial/ulnar deviation), as well as their combinations, in a controlled way. This would help during activities such as screwing, holding, hammering, and lifting. However, the RoM must be limited to prevent overstretching the human joint and causing pain. This is in line with the safety requirements of a wearable device [15].
Gripping is also important; the stronger the grasp, the more compression occurs between the wrist ligaments, and the higher the probability of obtaining carpal tunnel inflammation.
To allow these movements, the idea is to use cable transmissions. Soft plastic supports/saddles (thick purple shapes in Figure 32 and Figure 33) would be sewn on a glove to hold steel or fiber cables (tiny light blue lines in Figure 32 and Figure 33) on the back, palm, and lateral sides of the hand and fingers, as shown in Figure 32 and Figure 33, where forces would be applied. The shape of the cable supports will be based on the 3D hand/wrist profile. The cables from the actuators should be routed around the hand, passing through Teflon sleeves (black in Figure 32 and Figure 33) along the forearm to reduce friction. Care should be taken to avoid sharp edges or bending angles (e.g., 90° or more), as these cause friction losses along the cable’s path. One cable would be used to actuate a single wrist movement, except for grasping, where all cables around the fingers would be actuated simultaneously.
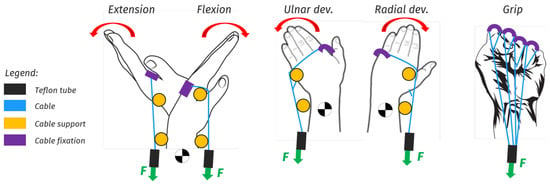
Figure 32.
Hand and wrist movements to be assisted.
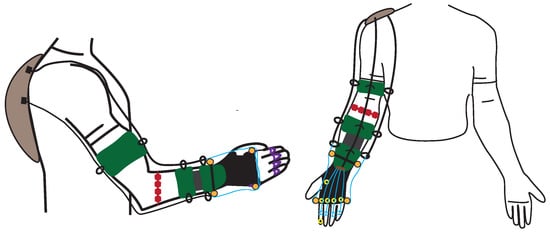
Figure 33.
Conceptual idea of a portable wrist exoskeleton. Grey: backpack containing actuators and electronics; green: webbing; red: sEMG sensors; black lines: Teflon tubes; light blue lines: steel or fiber cables; Orange: rigid cable supports; Yellow: FSR sensors; black: glove; purple: soft plastic cable holders.
A rotary actuator, equipped with a proper reduction transmission, would facilitate agonist and antagonist movements by pulling two cables (for flexion/extension and radial/ulnar deviation) and would ensure backdrivability. For grasping, a linear motor would be used to pull and close all fingers simultaneously. Forces (green arrow in Figure 32) would be applied through cables attached to actuators placed remotely, e.g., on a backpack. This would help redistribute localized weights on the hand/wrist.
In terms of dynamic requirements [15], the device should ideally be capable of holding objects weighing up to 5 kg with minimal muscular effort. This could be beneficial in both rehabilitation and industrial sectors when handling loads. Actuators and transmissions have to be sized according to the weight to be handled. Consider a weight of 5 kg held on the palm, 10 cm from the wrist joint. This would produce a force of nearly 50 N and a torque of 5 Nm, which has to be compensated for by the exoskeleton. Considering that standard normal-sized men’s wrists have a circumference of 16 to 18 cm, the wrist radius is estimated to be between 2.5 to 2.8 cm. Therefore, the cable force required to produce 5 Nm torque around the wrist should be approximately 180 N. This can be improved with special supports that raise the cable, increasing its radius relative to the wrist. These supports (orange in Figure 32 and Figure 33) would also prevent cables from unwinding, prevent the force vector from passing through the wrist CoR without producing effective torque, as shown in Figure 34, and reduce compression forces on the wrist. In fact, without these supports, the cable may become loose during pulling, causing the force to be closer to the wrist’s center of rotation, thus reducing the momentum and augmenting wrist compression (in Figure 34, the distances d, d’, and d” represent the pulling force arm in the neutral, flexion, and extension positions, respectively). With cable supports, cable unwinding is limited, and there is always a minimum distance, similar to that in the neutral position, ensuring a minimum effective momentum even when the wrist is flexed (the worst position).
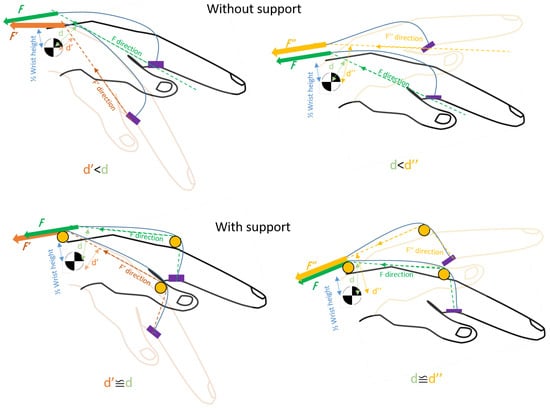
Figure 34.
Description of the modality, according to which the direction of the force changes when the cable supports (orange in the picture) are either present or absent. On the left, the wrist goes from neutral to flexion, while on the right, it goes from neutral to extension. Green: force vector direction in neutral position (F); Light green: distance (d) of F from the wrist center of rotation; Copper-coloured: force vector direction in flexion position (F′); Light copper-coloured: distance (d′) of F′ from the wrist center of rotation; Yellow: force vector direction in extension position (F″); Light yellow: distance (d″) of F″ from the wrist center of rotation; Blue: cable; Light blue: half height of the wrist center of rotation; Purple: cable holder.
We implement sEMG sensors (red in Figure 33) to detect electrical muscle spikes and muscle fatigue when the user moves their wrist. Moreover, FSR sensors (yellow in Figure 33) are placed in the palm to detect when an object is grasped and to measure the gripping pressure. The control system is based on state-of-the-art controllers that utilize machine learning strategies to predict hand/wrist movements according to muscle activation. It uses a PID controller to generate the required pulling forces on the cables [16,79,80,81,82]. The control scheme is structured on two levels, as depicted in Figure 35, to guarantee that the user can move freely as intended and experience assistive forces with appropriate timing and intensity. The high-level strategy determines wrist movement based on muscular activation, decides the necessary amount of assistive force/torque, and generates reference signals accordingly. At the low level, a closed-loop force/torque controller tracks these reference signals at each actuator. EMG signals are recorded by the high-level controller, segmented, and classified using methods such as neural networks or support vector machine classifiers. This process is designed to establish the intensity of muscular activity, identify which muscles are active, and predict hand/wrist movement. Additionally, FSR sensors in the palm assist in assessing the applied grasp force. This force is correlated with the amplitude of the EMG signals to determine the level of support to be provided. As a result, force/torque and pulling direction reference signals are generated by the high-level control and sent to the low-level controller. There, a PID controller determines which motor to activate based on the anticipated movement of the wrist. It also regulates the output force/torque at each motor by tracking the reference force/torque signal, ensuring precise and responsive control.
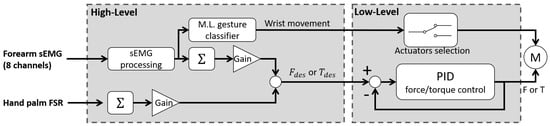
Figure 35.
Control scheme articulated in two levels. The high-level is responsible for the assistance to be given within appropriate timing. The low-level determines which actuators to switch on and regulates the force/torque output references at the actuators.
The objective is to design a device that enables the user to handle at least 5 kg effortlessly, while being as soft and light as possible (less than 1 kg); it should be comfortable, portable, equipped with a 6–8 h battery, and feature an affordable and user-friendly command interface (UCI). We are inspired by existing commercial and research products that exhibit the most promising characteristics and are well-received by patients and workers. We aim to contribute to the research by creating a new wrist exoskeleton for occupational purposes, designed to support all wrist movements during activities that can be detrimental to wrist health.
6. Discussion and Conclusions
Over the past few decades, researchers have been dedicated to developing exoskeletons with enhanced capabilities and “intelligence” levels, to address challenges related to aging, disabilities, physical overload, and strenuous work, which can impede normal life, leading to marginalization in both work and private life.
These devices are expected to play an important role in human health, particularly in the areas of rehabilitation, assistive technologies, and human power augmentation. They achieve this by transferring loads away from the human body and assisting in specific tasks. There have already been some positive results and approvals in the field of rehabilitation, while other applications, particularly in the occupational sector, require further investigation. The recent increase in disabilities caused by musculoskeletal disorders (with more than 1.7 billion cases worldwide) has raised concerns for the European Commission and the WHO, who have been leading awareness campaigns on this issue. Only in the last decade have wearable commercial solutions entered the market to assist workers in burdensome and repetitive tasks. However, as reported by Tiboni et al. [44], relatively few of these solutions focus on the wrist, even though it is considered the fourth most common site of musculoskeletal pain in the upper limbs.
This paper provides a comprehensive summary of several types of wearable and portable wrist exoskeletons, which are available both in the market and in research, as shown in Table A1 (see Appendix A). The aim is to gather sufficient information to develop critical thinking about what distinguishing features can determine the design of effective exoskeletons, depending on the field of application and the requirements to be met. We described and compared devices intended for different applications (rehabilitation, assistance, and occupational), by focusing on their technologies (hardware and control), functions, potential, and limitations. Macroscopic classifications of wrist exoskeletons can be based on several aspects, as described in [15], including purpose (rehabilitation, assistance, or occupational), stiffness (rigid, soft, compliant), type of actuation, power source, power transmission, sensing, control strategies, and technology readiness level (TRL), as shown in Figure 36 and Figure 37.
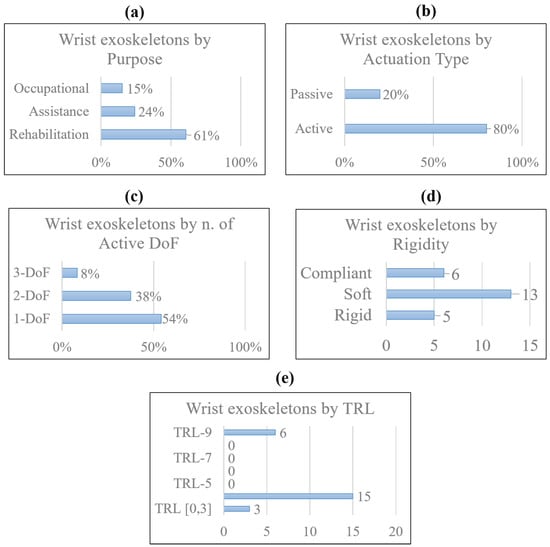
Figure 36.
Different classifications by purpose (a), actuation type (b), number of active DoFs (c), stiffness (d), and TRL (e), of wearable wrist exoskeletons taken into consideration. The amount of devices considered is 24. In some graphs, the percentage is preferred because some devices were designed for more than one application or could be used both as passive or active. Only 6 devices out of 24 passed conformity tests and entered the market.
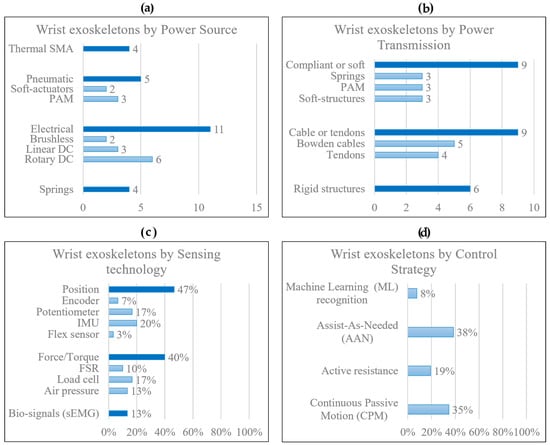
Figure 37.
Different classifications by power source (a), power transmission (b), sensing technologies (c), and control strategies (d) of wearable wrist exoskeletons taken into consideration. The total amount of devices considered is 24. In some graphs, the percentage is preferred because some devices adopt more than one sensing technology and control strategy.
A total of 24 wearable and portable wrist exoskeletons were designed: almost 18 devices for rehabilitation and assistance, and 5 for occupational tasks, as shown in Figure 36 and Figure 38.
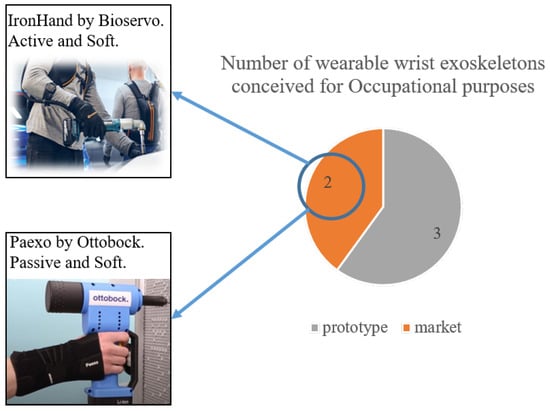
Figure 38.
Classification by TRL of wearable wrist exoskeletons intended for occupational purposes. Only two devices are available in the market: Ironhand designed by Bioservo (active device) and Paexo Wrist designed by Ottobock (passive device).
Looking at those data and Table A1, a strong prevalence of active devices emerged as they provide greater forces/torques, ensuring a wider range of applications. The most widespread actuation systems are electrical motors due to their robust controllability, great power-to-weight ratio, reliability, and price. For power transmission, cables and tendons are preferred because of high-force transmission and remote actuation, with a better redistribution of weight along the human body. However, they suffer from friction loss with non-linear behavior, making their control difficult. To ensure better control of the device, a lot of sensors are implemented. Position (encoder, potentiometer, IMU, flexible sensors) and force sensors (FSR, load cell, pressure gauge) are the most used. Position sensors enhance device performance by estimating wrist motion parameters (angle, position, velocity, and acceleration), enabling the determination of which movement has been performed and the application of drive parameters to provide assistance as quickly as possible. However, these solutions may experience time delays, discretization-related effects if speed is derived from position differentiation, or drift problems. Therefore, they often require additional sensors for more accurate kinematic evaluation. Force sensors are useful for the proper functioning of a device as they estimate the external loads applied to the wrist, thus determining the necessary torque/force to compensate for these loads and provide the required level of assistance at a specific time. Yet, they come with limitations. Load cells, while robust, very accurate, and pre-calibrated, are challenging to integrate into wearables due to their bulkiness, rigidity, heaviness, and the need for expensive signal conditioning. In contrast, FSRs are a viable alternative as they are easy to integrate, inexpensive, and lightweight. However, they are not very accurate, require calibration, are highly sensitive to environmental conditions and aging, and are prone to damage.
Nowadays, new control methods based on biofeedback signals (e.g., sEMG), directly related to user motion intentions, have also been tested. These sensors still have limitations in unstructured environments, as they must be attached directly to human skin and suffer from external noises. The main control strategies adopted are control passive motion (CPM) and assistance-as-needed (AAN). The former consists of controlling the movement of the exoskeleton according to predefined trajectories; the latter evaluates the actual external load or muscle effort to modulate the assistance provided by the robotic device. AAN is strongly recommended in unstructured environments, where the user could perform different activities. Moreover, new control techniques are being developed based on machine learning (ML) algorithms to predict user motion intention, and reduce the number of sensors adopted.
In terms of ergonomics and safety, the design features sought include kinematic compliance with human joints (by choosing an appropriate number of both active and passive degrees of freedom), covering and protection systems for electronics and moving parts, wearability, customization, and lightness. Wearability and comfort are achieved using soft materials, textiles, and foams, especially at the human–robot interfaces. These materials act as shock absorbers or coatings for rigid parts. Three-dimensional (3D) scanning technologies are considered a reliable and increasingly common approach for customized design, gathering information on the shape, dimensions, and metrics of a real object. To achieve lightness, the focus is on selecting design materials and creating low-profile shapes for the parts that wrap around the limb. In active devices, remote actuation is beneficial for locally reducing and better distributing weights and pressure points on the human body by positioning the actuators away from the actuated joints/limbs. Safety is usually guaranteed by introducing mechanical limit stops to prevent excessive joint excursions that could harm the user, covering open or restricted areas of the robot, avoiding floating cables, implementing emergency shutoff switches, and employing multiple control routines in the software. These routines monitor sensor status, joint angles, and joint torques to prevent sudden and unexpected movements and limit maximum torque.
It is not easy to design wrist exoskeletons because of the complex anatomy of the joint. It can move in a 3D space while supporting high forces in a very compact size. This creates difficulties in reproducing and assisting such kinematics and dynamics, without hindering human movement. Moreover, the requirements and specifications needed in certain applications lead to different design approaches. The majority of the devices reviewed are still in development, with promising practical outcomes, but have only been tested and used in a laboratory setting. By looking at these, as presented in Section 5, the authors are working on developing a novel portable wrist exoskeleton for occupational purposes. To facilitate user acceptance and accelerate the industrialization phase, starting with a soft device based on a glove is the initial approach. Tendon mechanisms, actuated remotely via DC motors, will be the first to be tested as they offer more reliable, robust, lightweight, safe, and cost-effective solutions. For sensing, position and force sensors will be distributed throughout the glove to detect wrist movements and applied forces/torques. In terms of control strategies, advanced machine learning algorithms for the AAN will be implemented. These algorithms will detect motion intentions and provide assistance based on the wrist’s position and overload.
The main limitations of this study, which may affect the generalizability of the findings, include a small number of trials conducted on subjects in real conditions in both rehabilitation and occupational settings, especially for non-commercial devices; a limited number of commercial devices designed for workers that can be compared; and a limited amount of accessible information on clinical data and experimentation on subjects, particularly for commercial devices. This makes it difficult to quantitatively evaluate the benefits of devices and their technologies, showing that real limits only allow speculation on what the most effective solutions might be.
Like all products, technological and economic barriers, as well as communication biases, are open issues opposed to acceptance and industrialization. The main obstacles could be identified as the high costs and long research and development times, often incompatible with the views of stakeholders and consumers; lack of interest from stakeholders, making it difficult to justify development; a lack of market competitors, hindering the identification of their pros and cons, and finding more advanced solutions; and the need for CE, FDA, or similar certifications. Furthermore, for occupational aims, challenges specific to user needs and acceptance may involve: physiological factors (e.g., personal history of physical complaints, wearing comfort), psycho-social factors (e.g., perceived usefulness, openness to innovation, feeling in control, safety), work-related factors (e.g., compatibility with tasks, storage, durability, reliability), and policy-related and implementation-related factors (e.g., WRMD prevention, costs, ease of use, training). Moreover, if the development of a device is driven by specific end-user needs and collaborations, the results greatly improve acceptability. This makes it more likely that exoskeletons are adopted rather than deserted after an initial period of testing. Although various frameworks based on existing technology acceptance models for industrial exoskeletons with potential end users [83], a grounded framework is still lacking.
Even though it is difficult to justify the effectiveness of exoskeletons, due to the lack of long-term experimental tests (more than 3 months), and the need for standardized products, evaluation protocols, and regulations, these devices bring both benefits and limitations [83,84]. Some studies have highlighted the potential and effectiveness of exoskeletons in reducing muscle demand and addressing the pathophysiological mechanisms underlying MSDs during load handling tasks, static bending postures, and elevating postures. However, the use of exoskeletons could lead to compensations in antagonist muscles and/or spinal imbalance, as well as changes in postural strategies and muscle coordination (such as inertia, force, and speed trajectory). These changes could counterproductively increase tendinopathies and the risk of injuries [84]. The current state of knowledge does not allow unreserved endorsement of the use of these devices as preventive technologies because many questions still need to be investigated and clarified, particularly the occurrence of muscle fatigue and chronic adaptations, skin pain, the impact of movement assistance on neuromuscular coordination, and joint kinematics. In view of emerging health and industrial needs, and thanks to the latest research findings, the authors expect an increase in the demand for progress and development in the field of portable wrist exoskeletons in the coming decades. There is hope for the same positive results as seen with other devices, improving working conditions and people’s health.
Author Contributions
Conceptualization, R.F.P., D.P., G.B. and J.O.; methodology, R.F.P., D.P., G.B. and J.O.; formal analysis, R.F.P. and D.P.; investigation, R.F.P.; resources, R.F.P.; writing—original draft preparation, R.F.P.; writing—review and editing, R.F.P., D.P., D.G.C., G.B. and J.O.; visualization, D.P., D.G.C., G.B. and J.O.; supervision, D.P., D.G.C., G.B. and J.O.; project administration, D.G.C. and J.O.; funding acquisition, D.G.C. and J.O. All authors have read and agreed to the published version of the manuscript.
Funding
This work is funded by the Italian Workers Compensation Authority (INAIL). Unique Project Code (CUP): J59C20001570005.
Data Availability Statement
Data sharing is not applicable to this review paper. No new data was created in this study.
Acknowledgments
Our thanks go out to INAIL (Italian Workers Compensation Authority) for its ongoing support, collaboration, and funding in the development of novel types of industrial exoskeletons, under the Collaborative Exoskeletons–EC-2 project in collaboration with Istituto Italiano di Tecnologia (IIT) and the University of Genoa.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MSD | musculoskeletal disorder |
| WRMSD | work-related musculoskeletal disorder |
| WHO | World Health Organization |
| INAIL | Italian Workers Compensatory Authority |
| DARPA | Defense Advanced Research Projects Agency |
| OE | occupational exoskeleton |
| CTS | carpal tunnel syndrome |
| DoF | degree of freedom |
| RoM | range of motion |
| CoR | center of rotation |
| ADL | activities of daily living |
| DTM | dart-throwing motion |
| TRL | technology readiness level |
| ICR | instantaneous center of rotation |
| OA | hand osteoarthritis |
| HAL | hand activity level |
| IMU | inertial magnetic unit |
| FSR | force resistive sensor |
| sEMG | surface electromyography signal |
| CPM | continuous passive motion |
| AAN | assistance-as-needed |
| ML | machine learning |
| PRISMA | preferred reporting items for systematic reviews and meta-analysis |
| WearRA | Wearable Robotics Association |
| SEM | soft extra muscle |
| SCI | spinal cord injury |
| JAS | Joint Active Systems, Inc. |
| PWE | portable wrist exoskeleton |
| NN | neural network |
| SVM | support vector machine |
| FMG | force myography signal |
| CIMT | constraint-induced movement therapy |
| MVC | maximum voluntary contraction |
| SOA | soft origami actuator |
| PMA | pneumatic muscle actuator |
| SMA | shape memory alloy |
| SWA | soft wrist assist |
| RMSE | root mean squared error |
| SPS | static progressive stretch |
| TBI | traumatic brain injury |
| OT | occupational therapy |
Appendix A

Table A1.
Comparison of all wearable and portable wrist exoskeletons, highlighting their characteristics.
Table A1.
Comparison of all wearable and portable wrist exoskeletons, highlighting their characteristics.
| Image | Reference | Device Name | Application Field | Actuation Type | Power Source | Power Transmission | Force/Torque Output [N][Nm] | Active DoF | Assisted Motion | RoM | Sensing | Control | TRL | Weight | Price ($) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | [16] | PWE | Rehab/Assistance | Active | DC motor | Links, gears | 2.3 Nm | 2 | Flex/Extension | ±60° | Potentiometer | CPM | ** 4 | 0.36 kg | - |
| Occupational | 2.5 Nm | Rad/Ulnar dev. | ±25° | sEMG | M.L. | ||||||||||
 | [13,17] | eWrist | Rehab/Assistance | Active | DC motor | Links, gears | up to 3.7 Nm | 1 | Flex/Extension | range 154° | sEMG, load cell, | AAN | ** 4 | 0.56 kg | - |
| encoder | |||||||||||||||
 | [18] | * - | Rehabilitation | Passive | DC motor | Links, gears | up to 1.12 Nm | 1 | Flex/Extension | range 120° | Triggered | CPM | ** 4 | 0.33 kg | * - |
| Active | Force (FSR) | M.L. | |||||||||||||
 | [11] | Wrist exosuit | Occupational | Active | Brushless motor | Bowden cables | 3 Nm | 1 | Flex/Extension | 70°/80° | Load cell, IMU | AAN | ** 4 | 0.3 kg (hand) | - |
 | [19] | Exo-Wrist | Rehabilitation | Active | DC motor | Bowden cables | ≥0.5 Nm | 1 | Extension | ≥50° | sEMG | AAN | ** 4 | 1 kg | - |
 | [20] | * - | Rehabilitation | Active | Pneumatic | Artificial muscles | 120 N | 3 | Flex/Extension | 91° | Pressure | Triggered | ** 4 | 2.26 kg | - |
| Rad/Ulnar dev. | 32° | ||||||||||||||
| Pron/supination | 78° | ||||||||||||||
 | [21] | ASSIST | Rehabilitation | Active | Pneumatic | Artificial muscles | up to 1 Nm | 1 | Flex/Extension | 80° | Flex sensor | AAN | ** 4 | 0.39 kg | - |
| Pressure | |||||||||||||||
 | [22] | SOA-wrist | Rehab/Assistance | Active | Pneumatic | Flexible joint-less | up to 0.76 Nm | 2 | Flex/Extension | 31°/30° | Pressure, | AAN | ** 4 | 1.76 kg | - |
| structures | Rad/Ulnar dev. | 33°/22° | IMU | ||||||||||||
 | [23] | * - | Rehab/Assistance | Active | Brushless motors | Bowden cables | ** ≥5 Nm | 2 | Flex/Extension | range 115° | IMU | CPM | ** 4 | 0.65 kg | - |
| Rad/Ulnar dev. | range 70° | ||||||||||||||
 | [37] | Exo-Wrist | Rehabilitation | Active | Pneumatic | Artificial muscles | 630 N | 2 | Flex/Extension | ±30° | IMU | CPM | ** 4 | 0.43 kg | - |
| Rad/Ulnar dev. | ±30° | ||||||||||||||
 | [34] | * - | Occupational | Active | Pneumatic | Flexible joint-less | * - | 1 | Flex/Extension | ±65° | IMU | AAN | ** 3 | * - | - |
| structure | Pressure | ||||||||||||||
 | [24,25] | SWA | Rehab/Assistance | Active | Thermal SMA | Compliant | up to 1.32 Nm | 2 | Flex/Extension | 38°/50° | Encoder | AAN | ** 4 | 1.9 kg | - |
| ≥0.6 Nm | Rad/Ulnar dev. | 34°/35° | Load cell | ||||||||||||
 | [26] | * - | Rehabilitation | Active | Thermal SMA | Pulley-tendons | * - | 3 | Flex/Extension | ** up to 50°/48° | Potentiometer | CPM | ** 3 | 0.95 kg | * - |
| Rad/Ulnar dev. | ** up to 16°/29° | Load cell | |||||||||||||
| Pron/Supination | ** up to 52° | ||||||||||||||
 | [38] | ASR | Rehab/Assistance | Active | Thermal SMA | Tendons | 40 N | 1 | Gripping | - | Load cell | Triggered | ** 3 | 300 g | - |
 | [27] | SMA-wrist exo | Rehabilitation | Active | Thermal SMA | Linkages | ≥0.5 Nm | 2 | Flex/Extension | range 50° | Potentiometer | CPM | ** 4 | 1 kg | 1060 |
| Rad/Ulnar dev. | range 40° | ||||||||||||||
 | [28] | SCRIPT | Rehabilitation | Passive | Springs | Links, tendons | 0.5–2 Nm | 1 | Flex/Extension | 45°/30° | Potentiometer | - | ** 4 | 0.65 kg | - |
 | [14,29] | * - | Rehabilitation | Active | DC motor | Tendons | 0.4 Nm | 2 | Flex/Extension | All | IMU | CPM | 4 | 0.3 kg | 160 |
| Rad/Ulnar dev. | |||||||||||||||
 | [30] | * - | Rehabilitation | Active | Linear DC motor | Leaf springs | 0.26 to 2.47 Nm | 2 | Flex/Extension | 57°/68 | Potentiometer | CPM | ** 4 | 0.51 kg | - |
| 0.65 Nm | Rad/Ulnar dev. | 40°/14° | |||||||||||||
 | [31] | JAS wrist | Rehabilitation | Passive | ** Springs | Links | - | 1 | Flex/Extension | up to 95° | - | - | 9 | * - | * - |
 | [32] | MyoPro orthosis | Rehab/Assistance | Active | DC motor | Linkages | 10 to 20 N | 2 | Flex/Extension | improve up to 35° | sEMG | AAN | 9 | 1.8 kg | 10,000 |
| Rad/Ulnar dev. | |||||||||||||||
 | [35] | Carbonhand | Assistance | Active | DC motor | Bowden cables | ** 60 N | 1 | Gripping | All | Force (FSR) | AAN | 9 | 0.7 kg | 7000 |
 | [35] | Ironhand | Occupational | Active | DC motor | Bowden cables | 80 N | 1 | Gripping | All | Force (FSR) | AAN | 9 | 2.5 kg | 6500 |
 | [36] | Paexo Wrist | Occupational | Passive | Leaf spring | Elastic | - | * 1 | Holding | All | - | - | 9 | * - | 160 |
 | [33] | SaeboFlex | Rehabilitation | Passive | Springs | Links, elastics | - | 1 | Flex/Extension | improve up to 6° | - | - | 9 | 1.6 kg | 600 |
Note: * no information; ** hypothesized according to its characteristics.

Table A2.
Number of clinical trials, number of subjects involved, age, gender, setting, and testing period for each device. The authors wish to emphasize that the information below may not be exhaustive, as it only refers to documentation accessible online, and does not include confidential data held by companies, especially for commercial devices.
Table A2.
Number of clinical trials, number of subjects involved, age, gender, setting, and testing period for each device. The authors wish to emphasize that the information below may not be exhaustive, as it only refers to documentation accessible online, and does not include confidential data held by companies, especially for commercial devices.
| Experimental Tests Conducted on the Device in a Real Environment or Laboratory | ||||||
|---|---|---|---|---|---|---|
| Reference | Subjects | Age | Gender | Clinical Condition | Setting | Testing Period |
| Research prototypes | ||||||
| [16] | 1 | n.d. | n.d. | Healthy | Lab. | n.d. |
| [13,17] | 15 | 26 ± 3.4 | 7 M, 8 F | Healthy | Lab. | n.d. |
| 2 | 60 ± 8 | M | Stroke | Lab. | n.d. | |
| [18] | 1 | n.d. | n.d. | Healthy | Lab. | n.d. |
| [11] | 4 | 28 ± 4.0 | M | Healthy | Lab. | n.d. |
| [19] | 3 | n.d. | n.d. | Healthy | Lab. | n.d. |
| [20] | 1 | n.d. | n.d. | Healthy | Lab. | n.d. |
| [21] | 5 | n.d. | M | Healthy | Lab. | n.d. |
| [22] | - | n.d. | n.d. | n.d. | Lab. | n.d. |
| [23] | 1 | n.d. | n.d. | Healthy | Lab. | n.d. |
| 3 | 47 ± 10.0 | M | Stroke | Lab. | ||
| [37] | 1 | n.d. | M | Healthy | Lab. | n.d. |
| [34] | - | n.d. | n.d. | n.d. | Lab. | n.d. |
| [24,25] | 5 | n.d. | 3 M, 2 F | Healthy | Lab. | n.d. |
| [26] | - | n.d. | n.d. | n.d. | Lab. | n.d. |
| [38] | 1 | n.d. | M | Healthy | Lab. | n.d. |
| [27] | 3 | n.d. | M | Healthy | Lab. | n.d. |
| [28] | 33 | n.d. | n.d. | Stroke | Lab. | n.d. |
| [14,29] | 1 | n.d. | M | Impaired Hand | Lab. | 60 trials |
| [30] | - | n.d. | n.d. | n.d. | Lab. | n.d. |
| Commercial devices | ||||||
| [31,59,60,61] | 133 | 53 ± 17.6 | 55 M, 78 F | Radius fractures | Clinic | 3–20 weeks |
| [32,62,63,64,65,66,67,68] | 1 | 62 | M | Stroke | Clinic/Home | 3 years |
| 2 | 53 ± 22 | M | SCI | Clinic | 6 weeks | |
| 18 | 55.5 ± 21.5 | 11 M, 7 F | Stroke | Clinic | A day | |
| 13 | 51 ± 19.9 | 5 M, 8 F | 7 Stroke, 6 TBI | Clinic/Home | 18 weeks | |
| 18 | 52.5 ± 14.7 | 13 M, 5 F | Stroke | Home | 3 months | |
| [35,70,71] | 15 | 41.5 ± 23.5 | n.d. | SCI | Home | 12 weeks |
| 63 | 54 ± 36 | n.d. | Impaired Hand | Home | 6 weeks | |
| [35,72] | 8 | n.d. | 4 M, 4 F | Healthy | Industry | 2 weeks |
| [36] | - | n.d. | n.d. | n.d. | Industry | n.d. |
| [33,56,74,75,76,77,78] | 10 | n.d. | 7 M, 3 F | Stroke | Clinic | 4 weeks |
| 8 | 70 ± 15 | 4 M, 4 F | Stroke | Clinic | 12 weeks | |
| 11 | 60.2 ± 7.89 | 7 M, 5 F | Stroke | Clinic | n.d. | |
| 1 | 43 | F | Stroke | Clinic | 16 weeks | |
n.d. = not defined, M = male, F = female.
References
- Gonçalves, H.; Cardoso, A.; Mattos, D.; Deola Borges, G.; Anacleto, P.; Colim, A.; Carneiro, P.; Arezes, P.M. Assessment of Work-Related Musculoskeletal Disorders by Observational Methods in Repetitive Tasks—A Systematic Review. In Occupational and Environmental Safety and Health III; Springer: Cham, Switzerland, 2022; pp. 455–463. [Google Scholar] [CrossRef]
- Ramazzini, B. De morbis artificum diatriba [diseases of workers]. Am. J. Public Health 2001, 91, 1380–1382. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, T.J.; Fine, L.J.; Goldstein, S.A.; Lifshitz, Y.R.; Silverstein, B.A. Ergonomics considerations in hand and wrist tendinitis. J. Hand Surg. 1987, 12, 830–837. [Google Scholar] [CrossRef] [PubMed]
- Sluiter, J.K.; Rest, K.M.; Frings-Dresen, M.H. Criteria document for evaluating the work-relatedness of upper-extremity musculoskeletal disorders. Scand. J. Work Environ. Health 2001, 27, 1–102. Available online: http://www.jstor.org/stable/40967163 (accessed on 31 March 2022). [CrossRef] [PubMed]
- Franco, G.; Franco, F. Bernardino Ramazzini: The father of occupational medicine. Am. J. Public Health 2001, 91, 1382. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Musculoskeletal Conditions, Key Facts. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 14 July 2022).
- INAIL-Italian Workers’ Compensatory Authority. Occupational Exoskeletons: Wearable Robotic Devices to Prevent Work Related Musculoskeletal Disorders in the Workplace of the Future. 2020. Available online: http://www.osha.europa.eu (accessed on 1 November 2021).
- European Agency for Safety and Health at Work (EU-OSHA). Work-Related Musculoskeletal Disorders—Facts and Figures; Standard, European Agency for Safety and Health at Work (EU-OSHA); Publications Office of the European Union: Luxembourg, 2020. [CrossRef]
- Pons, J.L. Wearable Robots: Biomechatronic Exoskeletons; John Wiley & Sons Ltd.: Chichester, UK, 2008; pp. 4, 11, 219, 332. ISBN 9780470512944. [Google Scholar]
- du Plessis, T.; Djouani, K.; Oosthuizen, C. Review of Active Hand Exoskeletons for Rehabilitation and Assistance. Robotics 2021, 10, 40. [Google Scholar] [CrossRef]
- Chiaradia, D.; Tiseni, L.; Xiloyannis, M.; Solazzi, M.; Masia, L.; Frisoli, A. An assistive soft wrist exosuit for flexion movements with an ergonomic reinforced glove. Front. Robot. AI 2021, 7, 595862. [Google Scholar] [CrossRef] [PubMed]
- Crea, S.; Beckerle, P.; De Looze, M.; De Pauw, K.; Grazi, L.; Kermavnar, T.; Masood, J.; O’Sullivan, L.W.; Pacifico, I.; Rodriguez-Guerrero, C.; et al. Occupational exoskeletons: A roadmap toward large-scale adoption. Methodology and challenges of bringing exoskeletons to workplaces. Wearable Technol. 2021, 2, e11. [Google Scholar] [CrossRef]
- Lambelet, C.; Temiraliuly, D.; Siegenthaler, M.; Wirth, M.; Woolley, D.G.; Lambercy, O.; Gassert, R.; Wenderoth, N. Characterization and wearability evaluation of a fully portable wrist exoskeleton for unsupervised training after stroke. J. Neuro Eng. Rehabil. 2020, 17, 132. [Google Scholar] [CrossRef]
- Dragusanu, M.; Iqbal, M.Z.; Baldi, T.L.; Prattichizzo, D.; Malvezzi, M. Design, Development, and Control of a Hand/Wrist Exoskeleton for Rehabilitation and Training. IEEE Trans. Robot. 2022, 38, 1472–1488. [Google Scholar] [CrossRef]
- Pitzalis, R.F.; Park, D.; Caldwell, D.G.; Berselli, G.; Ortiz, J. State of the Art in Wearable Wrist Exoskeletons Part I: Background Needs and Design Requirements. Machines 2023, 11, 458. [Google Scholar] [CrossRef]
- Xiao, Z.G.; Menon, C. Towards the development of a portable wrist exoskeleton. In Proceedings of the 2011 IEEE International Conference on Robotics and Biomimetics, Karon Beach, Thailand, 7–11 December 2011; pp. 1884–1889. [Google Scholar] [CrossRef]
- Lambelet, C.; Lyu, M.; Woolley, D.; Gassert, R.; Wenderoth, N. The eWrist—A wearable wrist exoskeleton with sEMG-based force control for stroke rehabilitation. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 726–733. [Google Scholar] [CrossRef]
- Sangha, S.; Elnady, A.M.; Menon, C. A compact robotic orthosis for wrist assistance. In Proceedings of the 2016 6th IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob), Singapore, 26–29 June 2016; pp. 1080–1085. [Google Scholar] [CrossRef]
- Choi, H.; Kang, B.B.; Jung, B.K.; Cho, K.J. Exo-wrist: A soft tendon-driven wrist-wearable robot with active anchor for dart-throwing motion in hemiplegic patients. IEEE Robot. Autom. Lett. 2019, 4, 4499–4506. [Google Scholar] [CrossRef]
- Bartlett, N.W.; Lyau, V.; Raiford, W.A.; Holland, D.; Gafford, J.B.; Ellis, T.D.; Walsh, C.J. A soft robotic orthosis for wrist rehabilitation. J. Med. Devices 2015, 9, 030918. [Google Scholar] [CrossRef]
- Sasaki, D.; Noritsugu, T.; Takaiwa, M. Development of active support splint driven by pneumatic soft actuator (ASSIST). In Proceedings of the 2005 IEEE international Conference on Robotics and Automation, Barcelona, Spain, 18–22 April 2005; pp. 520–525. [Google Scholar] [CrossRef]
- Liu, S.; Fang, Z.; Liu, J.; Tang, K.; Luo, J.; Yi, J.; Hu, X.; Wang, Z. A compact soft robotic wrist brace with origami actuators. Front. Robot. AI 2021, 8, 34. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Yang, T.; Yang, Y.; Yu, P.; Xue, X.; Zhao, X.; Song, G.; Elhajj, I.H.; Wang, W.; Xi, N.; et al. Bioinspired musculoskeletal model-based soft wrist exoskeleton for stroke rehabilitation. J. Bionic Eng. 2020, 17, 1163–1174. [Google Scholar] [CrossRef]
- Jeong, J.; Yasir, I.B.; Han, J.; Park, C.H.; Bok, S.K.; Kyung, K.U. Design of shape memory alloy-based soft wearable robot for assisting wrist motion. Appl. Sci. 2019, 9, 4025. [Google Scholar] [CrossRef]
- Jeong, J.; Hyeon, K.; Han, J.; Park, C.H.; Ahn, S.Y.; Bok, S.K.; Kyung, K.U. Wrist assisting soft wearable robot with stretchable coolant vessel integrated SMA muscle. IEEE/ASME Trans. Mechatronics 2021, 27, 1046–1058. [Google Scholar] [CrossRef]
- Hope, J.; McDaid, A. Development of wearable wrist and forearm exoskeleton with shape memory alloy actuators. J. Intell. Robot. Syst. 2017, 86, 397. [Google Scholar] [CrossRef]
- Serrano, D.; Copaci, D.S.; Moreno, L.; Blanco, D. SMA based wrist exoskeleton for rehabilitation therapy. In Proceedings of the 2018 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Madrid, Spain, 1–5 October 2018; pp. 2318–2323. [Google Scholar] [CrossRef]
- Ates, S.; Haarman, C.J.; Stienen, A.H. SCRIPT passive orthosis: Design of interactive hand and wrist exoskeleton for rehabilitation at home after stroke. Auton. Robot. 2017, 41, 711–723. [Google Scholar] [CrossRef]
- Dragusanu, M.; Baldi, T.L.; Iqbal, Z.; Prattichizzo, D.; Malvezzi, M. Design, development, and control of a tendon-actuated exoskeleton for wrist rehabilitation and training. In Proceedings of the 2020 IEEE International Conference on Robotics and Automation (ICRA), Paris, France, 31 May–31 August 2020; pp. 1749–1754. [Google Scholar] [CrossRef]
- Higuma, T.; Kiguchi, K.; Arata, J. Low-profile two-degree-of-freedom wrist exoskeleton device using multiple spring blades. IEEE Robot. Autom. Lett. 2017, 3, 305–311. [Google Scholar] [CrossRef]
- JAS-Joint Active Systems. JAS Wrist. 2017. Available online: https://www.jointactivesystems.com/products/areas/wrist (accessed on 5 August 2022).
- Myomo, Inc. MyoPro Orthosis. 2006. Available online: https://myomo.com/what-is-a-myopro-orthosis/ (accessed on 8 August 2022).
- Saebo Inc. SaeboFlex. Available online: https://www.saebo.com/shop/saeboflex/ (accessed on 30 November 2022).
- Zhu, M.; Adams, W.; Polygerinos, P. Carpal tunnel syndrome soft relief device for typing applications. In Proceedings of the 2017 Design of Medical Devices Conference, Minneapolis, MN, USA, 10–13 April 2017; American Society of Mechanical Engineers: New York, NY, USA, 2017; Volume 40672, p. V001T03A003. [Google Scholar] [CrossRef]
- Bioservo Technologies. Bioservo Strength for Life—Professional and Healthcare. Available online: https://www.bioservo.com/ (accessed on 7 September 2022).
- Ottobock. Paexo Wrist Exoskeleton. Available online: https://paexo.com/paexo-wrist/?lang=it (accessed on 5 August 2022).
- Andrikopoulos, G.; Nikolakopoulos, G.; Manesis, S. Motion control of a novel robotic wrist exoskeleton via pneumatic muscle actuators. In Proceedings of the 2015 IEEE 20th Conference on Emerging Technologies & Factory Automation (ETFA), Luxembourg, 8–11 September 2015; pp. 1–8. [Google Scholar] [CrossRef]
- Hadi, A.; Alipour, K.; Kazeminasab, S.; Elahinia, M. ASR glove: A wearable glove for hand assistance and rehabilitation using shape memory alloys. J. Intell. Mater. Syst. Struct. 2018, 29, 1575–1585. [Google Scholar] [CrossRef]
- Ferguson, R.; Riley, N.D.; Wijendra, A.; Thurley, N.; Carr, A.J.; Dean, B.J.F. Wrist pain: A systematic review of prevalence and risk factors–what is the role of occupation and activity? BMC Musculoskelet. Disord. 2019, 20, 542. [Google Scholar] [CrossRef] [PubMed]
- Noronha, B.; Accoto, D. Exoskeletal devices for hand assistance and rehabilitation: A comprehensive analysis of state-of-the-art technologies. IEEE Trans. Med. Robot. Bionics 2021, 3, 525–538. [Google Scholar] [CrossRef]
- Gopura, R.; Kiguchi, K. Mechanical designs of active upper-limb exoskeleton robots: State-of-the-art and design difficulties. In Proceedings of the 2009 IEEE International Conference on Rehabilitation Robotics, Kyoto, Japan, 23–26 June 2009; pp. 178–187. [Google Scholar] [CrossRef]
- Gopura, R.; Bandara, D.; Kiguchi, K.; Mann, G.K. Developments in hardware systems of active upper-limb exoskeleton robots: A review. Robot. Auton. Syst. 2016, 75, 203–220. [Google Scholar] [CrossRef]
- Nikhil, G.; Yedukondalu, G.; Rao, S. Robotic exoskeletons: A review on development. Int. J. Mech. Prod. Eng. Res. Dev. 2019, 9, 529–542. [Google Scholar]
- Tiboni, M.; Borboni, A.; Vérité, F.; Bregoli, C.; Amici, C. Sensors and actuation technologies in exoskeletons: A review. Sensors 2022, 22, 884. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Jamwal, P.K.; Van Vliet, P.; Ghayesh, M.H. State-of-the-art robotic devices for wrist rehabilitation: Design and control aspects. IEEE Trans. Hum.-Mach. Syst. 2020, 50, 361–372. [Google Scholar] [CrossRef]
- Cornejo, J.; Huamanchahua, D.; Huamán-Vizconde, S.; Terrazas-Rodas, D.; Sierra-Huertas, J.; Janampa-Espinoza, A.; Gonzáles, J.; Cardona, M. Mechatronic exoskeleton systems for supporting the biomechanics of shoulder-elbow-wrist: An innovative review. In Proceedings of the 2021 IEEE International IOT, Electronics and Mechatronics Conference (IEMTRONICS), Toronto, ON, Canada, 21–24 April 2021; pp. 1–9. [Google Scholar] [CrossRef]
- Khokhar, Z.O.; Xiao, Z.G.; Menon, C. Surface EMG pattern recognition for real-time control of a wrist exoskeleton. Biomed. Eng. Online 2010, 9, 41. [Google Scholar] [CrossRef]
- Vardakastani, V.; Bell, H.; Mee, S.; Brigstocke, G.; Kedgley, A.E. Clinical measurement of the dart throwing motion of the wrist: Variability, accuracy and correction. J. Hand Surg. Eur. Vol. 2018, 43, 723–731. [Google Scholar] [CrossRef]
- Braidotti, F.; Atzei, A.; Fairplay, T. Dart-Splint: An innovative orthosis that can be integrated into a scapho-lunate and palmar midcarpal instability re-education protocol. J. Hand Ther. 2015, 28, 329–335. [Google Scholar] [CrossRef]
- Kaufman-Cohen, Y.; Friedman, J.; Levanon, Y.; Jacobi, G.; Doron, N.; Portnoy, S. Wrist plane of motion and range during daily activities. Am. J. Occup. Ther. 2018, 72, 7206205080p1–7206205080p10. [Google Scholar] [CrossRef]
- Brigstocke, G.; Hearnden, A.; Holt, C.; Whatling, G. In-vivo confirmation of the use of the dart thrower’s motion during activities of daily living. J. Hand Surg. Eur. Vol. 2014, 39, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Borislav, M. The Number of Companies Making Industrial Exoskeletons Has Been Quietly Increasing for the Past Five Years. 2020. Available online: https://www.forbes.com/sites/borislavmarinov/2020/09/24/the-number-of-companies-making-industrial-exoskeletons-has-been-quietly-increasing-for-the-past-five-years/?sh=231b1c067bf4 (accessed on 5 August 2022).
- Borislav, M. Updated Directory of Exoskeleton Companies and Industry Statistics. 2021. Available online: https://exoskeletonreport.com/2021/12/updated-directory-of-exoskeleton-companies-and-industry-statistics/ (accessed on 5 August 2022).
- Radder, B.; Prange-Lasonder, G.B.; Kottink, A.I.; Holmberg, J.; Sletta, K.; van Dijk, M.; Meyer, T.; Melendez-Calderon, A.; Buurke, J.H.; Rietman, J.S. Home rehabilitation supported by a wearable soft-robotic device for improving hand function in older adults: A pilot randomized controlled trial. PLoS ONE 2019, 14, e0220544. [Google Scholar] [CrossRef] [PubMed]
- Hyttinge, M.; Einarsson, F. Bioservo Technologies. Technical Report, Redeye, Equity Research and Investment Banking Company, 7 September 2021, Redeye, Mäster Samuelsgatan 42, 10tr, Box 7141, 103 87 Stockholm. Available online: https://www.redeye.se/company/bioservo-technologies (accessed on 1 November 2022).
- Moskiewicz, D.; Mraz, M.; Chamela-Bilińska, D. Botulinum Toxin and Dynamic Splint Restore Grasping Function after Stroke: A Case Report. Int. J. Environ. Res. Public Health 2023, 20, 4873. [Google Scholar] [CrossRef] [PubMed]
- Lucado, A.M.; Li, Z.; Russell, G.B.; Papadonikolakis, A.; Ruch, D.S. Changes in impairment and function after static progressive splinting for stiffness after distal radius fracture. J. Hand Ther. 2008, 21, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Lucado, A.M.; Li, Z. Static progressive splinting to improve wrist stiffness after distal radius fracture: A prospective, case series study. Physiother. Theory Pract. 2009, 25, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Berner, S.H.; Willis, F.B. Dynamic splinting in wrist extension following distal radius fractures. J. Orthop. Surg. Res. 2010, 5, 53. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.A. Static progressive orthoses for the upper extremity: A comprehensive literature review. Hand 2012, 7, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Sodhi, N.; Yao, B.; Anis, H.K.; Khlopas, A.; Sultan, A.A.; Newman, J.M.; Mont, M.A. Patient satisfaction and outcomes of static progressive stretch bracing: A 10-year prospective analysis. Ann. Transl. Med. 2019, 7, 67. [Google Scholar] [CrossRef]
- Dunaway, S.; Dezsi, D.B.; Perkins, J.; Tran, D.; Naft, J. Case report on the use of a custom myoelectric elbow–wrist–hand orthosis for the remediation of upper extremity paresis and loss of function in chronic stroke. Mil. Med. 2017, 182, e1963–e1968. [Google Scholar] [CrossRef]
- Androwis, G.J.; Engler, A.; Rana, S.; Kirshblum, S.; Yue, G.H. The Rehabilitation Effects of Myoelectric Powered Wearable Orthotics on Improving Upper Extremity Function in Persons with SCI. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Virtual, 1–5 November 2021; pp. 4944–4948. [Google Scholar]
- Androwis, G.J.; Engler, A.; Rana, S.; Kirshblum, S.; Yue, G. Upper Extremity Functional Improvements in Persons with SCI Resulted from Daily Utilization of Myoelectric Powered Wearable Orthotics. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Virtual, 1–5 November 2021; pp. 4949–4952. [Google Scholar]
- Hoppe-Ludwig, S.; Armitage, J.; Turner, K.L.; O’Brien, M.K.; Mummidisetty, C.K.; Koch, L.M.; Kocherginsky, M.; Jayaraman, A. Usability, functionality, and efficacy of a custom myoelectric elbow-wrist-hand orthosis to assist elbow function in individuals with stroke. J. Rehabil. Assist. Technol. Eng. 2021, 8, 20556683211035057. [Google Scholar] [CrossRef]
- Pundik, S.; McCabe, J.; Skelly, M.; Salameh, A.; Naft, J.; Chen, Z.; Tatsuoka, C.; Fatone, S. Myoelectric Arm Orthosis in Motor Learning-Based Therapy for Chronic Deficits After Stroke and Traumatic Brain Injury. Front. Neurol. 2022, 13, 19. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.R.; Hofland, N.; Chen, Z.; Tatsuoka, C.; Richards, L.G.; Bruestle, M.; Kovelman, H.; Naft, J. Myoelectric Arm Orthosis Assists Functional Activities: A 3-Month Home Use Outcome Report. Arch. Rehabil. Res. Clin. Transl. 2023, 5, 100279. [Google Scholar] [CrossRef] [PubMed]
- McCabe, J.P.; Henniger, D.; Perkins, J.; Skelly, M.; Tatsuoka, C.; Pundik, S. Feasibility and clinical experience of implementing a myoelectric upper limb orthosis in the rehabilitation of chronic stroke patients: A clinical case series report. PLoS ONE 2019, 14, e0215311. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, M.; Ingvast, J.; Wikander, J.; von Holst, H. The Soft Extra Muscle system for improving the grasping capability in neurological rehabilitation. In Proceedings of the 2012 IEEE-EMBS Conference on Biomedical Engineering and Sciences, Langkawi, Malaysia, 17–19 December 2012; pp. 412–417. [Google Scholar] [CrossRef]
- Osuagwu, B.A.; Timms, S.; Peachment, R.; Dowie, S.; Thrussell, H.; Cross, S.; Heywood, T.; Shirley, R.; Taylor, J. Clinical Trial of the Soft Extra Muscle Glove to Assess Orthotic and Long-Term Functional Gain Following Chronic Incomplete Tetraplegia: Preliminary Functional Results. In Proceedings of the International Conference on NeuroRehabilitation, Pisa, Italy, 16–20 October 2018; Springer: Cham, Switzerland, 2018; pp. 385–389. [Google Scholar] [CrossRef]
- Kottink, A.I.R.; Nikamp, C.D.; Bos, F.P.; van der Sluis, C.K.; van den Broek, M.; Onneweer, B.; Stolwijk-Swüste, J.M.; Brink, S.M.; Voet, N.B.; Buurke, J.B.; et al. Therapeutic Effect of a Soft Robotic Glove for Activities of Daily Living In People with Impaired Hand Strength: Protocol for a Multicenter Clinical Trial (iHand). JMIR Res. Protoc. 2022, 11, e34200. [Google Scholar] [CrossRef] [PubMed]
- Cousins, D.; Porto, R.; Bigelo, A.; Fox, R.; Libs, B.; Holmes, M.; Cort, J. Effects of the Ironhand® Soft Exoskeleton on Forearm Muscle Activity During in Field Automotive Assembly Tasks. Available online: https://ssrn.com/abstract=4559929 (accessed on 2 September 2023).
- Hoffman, H.B.; Blakey, G.L. New design of dynamic orthoses for neurological conditions. NeuroRehabilitation 2011, 28, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.-S.; Woo, Y.-K.; Yi, C.-H.; Kwon, O.-Y.; Jung, M.-Y.; Lee, Y.-H.; Hwang, S.; Choi, B.-R. Effect of intensive training with a pring-assisted hand orthosis on movement smoothness in upper extremity following stroke: A pilot clinical trial. Top. Stroke Rehabil. 2012, 19, 320–328. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stuck, R.A.; Marshall, L.M.; Sivakumar, R. Feasibility of SaeboFlex upper-limb training in acute stroke rehabilitation: A clinical case series. Occup. Ther. Int. 2014, 21, 108–114. [Google Scholar] [CrossRef]
- Andriske, L.; Verikios, D.; Hitch, D. Patient and therapist experiences of the SaeboFlex: A pilot study. Occup. Ther. Int. 2017, 2017, 5462078. [Google Scholar] [CrossRef]
- Barry, J.; Saabye, S.; Baker, D.; Fogarty, J.; Beck, K. Effects of the saeboflex® orthosis and a home exercise program on upper extremity recovery in individuals with chronic. J. Neurol. Phys. Ther. 2006, 30, 207. [Google Scholar] [CrossRef]
- Lannin, N.A.; Cusick, A.; Hills, C.; Kinnear, B.; Vogel, K.; Matthews, K.; Bowring, G. Upper limb motor training using a Saebo™ orthosis is feasible for increasing task-specific practice in hospital after stroke. Aust. Occup. Ther. J. 2016, 63, 364–372. [Google Scholar] [CrossRef]
- Huang, Z.; Liu, J.; Li, Z.; Su, C.Y. Adaptive impedance control of robotic exoskeletons using reinforcement learning. In Proceedings of the 2016 International Conference on Advanced Robotics and Mechatronics (ICARM), Macau, China, 18–20 August 2016; pp. 243–248. [Google Scholar] [CrossRef]
- Ren, J.L.; Chien, Y.H.; Chia, E.Y.; Fu, L.C.; Lai, J.S. Deep learning based motion prediction for exoskeleton robot control in upper limb rehabilitation. In Proceedings of the 2019 International Conference on Robotics and Automation (ICRA), Montreal, QC, Canada, 20–24 May 2019; pp. 5076–5082. [Google Scholar] [CrossRef]
- Rose, L.; Bazzocchi, M.C.; Nejat, G. A model-free deep reinforcement learning approach for control of exoskeleton gait patterns. Robotica 2022, 40, 2189–2214. [Google Scholar] [CrossRef]
- Côté-Allard, U.; Fall, C.L.; Drouin, A.; Campeau-Lecours, A.; Gosselin, C.; Glette, K.; Laviolette, F.; Gosselin, B. Deep learning for electromyographic hand gesture signal classification using transfer learning. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 760–771. [Google Scholar] [CrossRef] [PubMed]
- Theurel, J.; Desbrosses, K. Occupational exoskeletons: Overview of their benefits and limitations in preventing work-related musculoskeletal disorders. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 264–280. [Google Scholar] [CrossRef]
- Elprama, S.A.; Vanderborght, B.; Jacobs, A. An industrial exoskeleton user acceptance framework based on a literature review of empirical studies. Appl. Ergon. 2022, 100, 103615. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).