Is There a Link between COVID-19 Infection, Periodontal Disease and Acute Myocardial Infarction?
Abstract
:1. Inflammation, Atherosclerosis and Acute Coronary Syndromes
2. Periodontal Disease—The Local Inflammatory Disease Increasing Cardiovascular Risk
3. Inflammatory Biomarkers in Cardiovascular Disease and Periodontal Disease
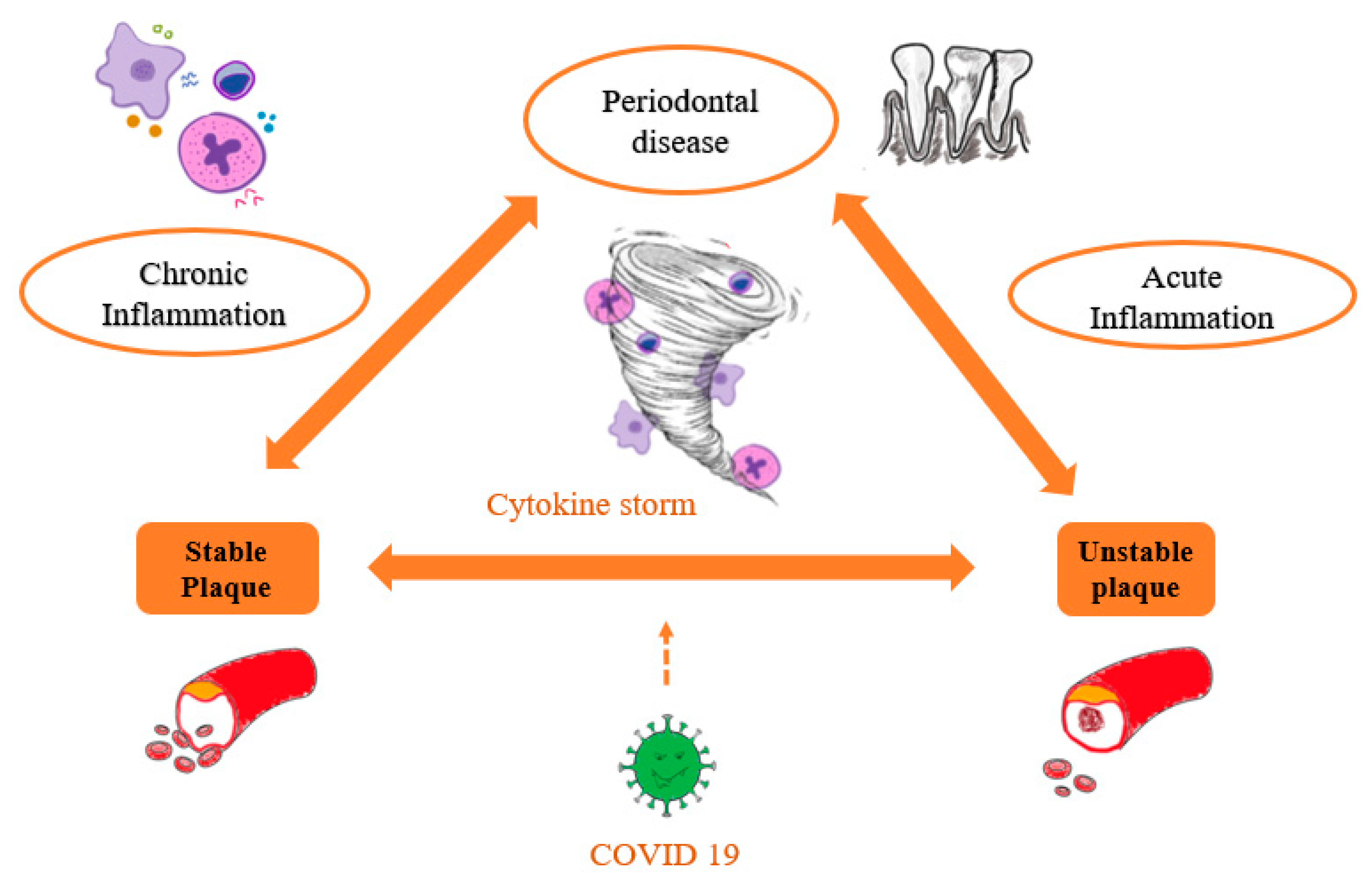
4. COVID-19—The New Trigger of Systemic Inflammation
5. The Inflammatory Link between Periodontal Disease, Acute Coronary Syndrome and COVID-19 Infection
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Gode, S.; Sarp, T.Z.; Saribas, S.; Ergin, S.; Kasnak, G.; Dinc, H.O.; Caliskan, R.; Akkus, S.; Tokman, H.B.; Kocak, B.T.; et al. The prevalence of periodontal pathogenic bacteria in atherosclerotic cardiovascular disease. Clin. Lab. 2020, 66, 893–900. [Google Scholar] [CrossRef]
- Beck, J.D.; Philips, K.; Moss, K.; Sen, S.; Morelli, T.; Preisser, J.; Pankow, J. Periodontal disease classifications and incident coronary heart disease in the Atherosclerosis Risk in Communities study. J. Periodontol. 2020, 91, 1409–1418. [Google Scholar] [CrossRef] [PubMed]
- Schiavone, M.; Gobbi, C.; Biondi-Zoccai, G.; D’Ascenzo, F.; Palazzuoli, A.; Gasperetti, A.; Mitacchione, G.; Viecca, M.; Galli, M.; Fedele, F.; et al. Acute Coronary Syndromes and Covid-19: Exploring the Uncertainties. J. Clin. Med. 2020, 9, 1683. [Google Scholar] [CrossRef] [PubMed]
- Díaz, C.M.; Bullon, B.; Ruiz-Salmerón, R.J.; Fernández-Riejos, P.; Fernández-Palacín, A.; Battino, M.; Cordero, M.D.; Quiles, J.L.; Varela-López, A.; Bullón, P. Molecular inflammation and oxidative stress are shared mechanisms involved in both myocardial infarction and periodontitis. J. Periodontal. Res. 2020, 55, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Winning, L.; Patterson, C.C.; Linden, K.; Evans, A.; Yarnel, J.; McKeown, P.P.; Kee, F.; Linden, G.J. Periodontitis and risk of prevalent and incident coronary heart disease events. J. Clin. Periodontol. 2020, 47, 1446–1456. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; del Castillo, A.M.; Jepsen, S.; Gonzalez-Juanatey, J.R.; D’Aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 2020, 47, 268–288. [Google Scholar] [CrossRef]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef]
- Byon, M.J.; Kim, S.Y.; Kim, J.S.; Kim, H.N.; Kim, J.B. Association of periodontitis with atherosclerotic cardiovascular diseases: A nationwide population-based retrospective matched cohort study. Int. J. Environ. Res. Public Health 2020, 17, 7261. [Google Scholar] [CrossRef]
- Zhang, T.Y.; Zhao, Q.; Liu, Z.S.; Zhang, C.Y.; Yang, J.; Meng, K. Relationship between monocyte/lymphocyte ratio and non-culprit plaque vulnerability in patients with acute coronary syndrome: An optical coherence tomography study. Medicine 2020, 99, e21562. [Google Scholar] [CrossRef]
- Rus, V.A.; Chitu, M.; Cernea, S.; Benedek, I.; Hodas, R.; Zavate, R.; Nyulas, T.; Hintea, M.; Benedek, T. Altered nutritional status, inflammation and systemic vulnerability in patients with acute myocardial infarction undergoing percutaneous coronary revascularisation: A prospective study in a level 3 cardiac critical care unit. Nutr. Diet. 2020, 77, 212–222. [Google Scholar] [CrossRef]
- Benedek, T.; Rodean, I.; Ratiu, M.; Rat, N.; Eremie, L.Y.; Biriș, C.; Lazăr, L.; Păcurar, M.; Benedek, I. Periodontal Disease, Inflammation and Atherosclerosis Progression in Patients with Acute Coronary Syndromes—The ATHERODENT Study. J. Cardiovasc. Emerg. 2018, 4, 17–23. [Google Scholar] [CrossRef] [Green Version]
- Musher, D.M.; Abers, M.S.; Corrales-Medina, V.F. Acute Infection and Myocardial Infarction. N. Engl. J. Med. 2019, 380, 171–176. [Google Scholar] [CrossRef]
- Stepniakowski, K.T.; Goodfriend, T.L.; Egan, B.M. Fatty acids enhance vascular alpha-adrenergic sensitivity. Hypertension 1995, 25, 774–778. [Google Scholar] [CrossRef]
- Fuster, V.; Badimon, L.; Badimon, J.J.; Chesebro, J.H. The pathogenesis of coronary artery disease and the acute coronary syndrome. N. Engl. J. Med. 1992, 4, 242–250. [Google Scholar]
- Choi, S.Y.; Mintz, G.S. What have we learned about plaque rupture in acute coronary syndromes? Curr. Cardiol. Rep. 2010, 12, 338–343. [Google Scholar] [CrossRef]
- Czesnikiewicz-Guzik, M.; D’Aiuto, F.; Deanfield, J.E. Understanding residual inflammatory risk sheds new light on the clinical importance of periodontitis in cardiovascular disease. Eur. Heart J. 2020, 41, 818–819. [Google Scholar] [CrossRef]
- Priyamvara, A.; Dey, A.K.; Bandyopadhyay, D.; Katikineni, V.; Zaghlol, R.; Basyal, B.; Barssoum, K.; Amarin, R.; Bhatt, D.L.; Lavie, C.J. Periodontal Inflammation and the Risk of Cardiovascular Disease. Curr. Atheroscler. Rep. 2020, 22, 28. [Google Scholar] [CrossRef] [PubMed]
- Pitones-Rubio, V.; Chávez-Cortez, E.G.; Hurtado-Camarena, A.; González-Rascón, A.; Serafín-Higuera, N. Is periodontal disease a risk factor for severe COVID-19 illness? Med. Hypotheses 2020, 144, 109969. [Google Scholar] [CrossRef]
- Wojtkowska, A.; Zapolski, T.; Wysokińska-Miszczuk, J.; Wysokiński, A.P. The inflammation link between periodontal disease and coronary atherosclerosis in patients with acute coronary syndromes: Case-control study. BMC Oral Health 2021, 21, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Gomes-Filho, I.S.; Coelho, J.M.F.; Miranda, S.S.; Cruz, S.S.; Trindade, S.C.; Cerqueira, E.M.M.; Passos-Soares, J.S.; Costa, M.D.C.N.; Vianna, M.I.P.; Figueiredo, A.C.M.G.; et al. Severe and moderate periodontitis are associated with acute myocardial infarction. J. Periodontol. 2020, 91, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Rodean, I.P.; Lazăr, L.; Halațiu, V.B.; Biriș, C.; Benedek, I.; Benedek, T. Periodontal Disease Is Associated with Increased Vulnerability of Coronary Atheromatous Plaques in Patients Undergoing Coronary Computed Tomography Angiography—Results from the Atherodent Study. J. Clin. Med. 2021, 10, 1290. [Google Scholar] [CrossRef] [PubMed]
- Joshi, C.; Bapat, R.; Anderson, W.; Dawson, D.; Hijazi, K.; Cherukara, G. Detection of periodontal microorganisms in coronary atheromatous plaque specimens of myocardial infarction patients: A systematic review and meta-analysis. Trends Cardiovasc. Med. 2021, 31, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Viafara-García, S.M.; Morantes, S.J.; Chacon-Quintero, Y.; Castillo, D.M.; Lafaurie, G.I.; Buitrago, D.M. Repeated Porphyromonas gingivalis W83 exposure leads to release pro-inflammatory cytokynes and angiotensin II in coronary artery endothelial cells. Sci. Rep. 2019, 9, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lund Håheim, L.; Schwarze, P.E.; Thelle, D.S.; Nafstad, P.; Rønningen, K.S.; Olsen, I. Low levels of antibodies for the oral bacterium Tannerella forsythia predict cardiovascular disease mortality in men with myocardial infarction: A prospective cohort study. Med. Hypotheses 2020, 138, 109575. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Tang, Q.; Nie, J.; Zhang, C.; Zhou, X.; Yu, S.; Sun, J.; Cheng, X.; Dong, N.; Hu, Y.; et al. Bmal1-downregulation aggravates porphyromonas gingivalis-induced atherosclerosis by encouraging oxidative stress. Circ. Res. 2020, 126, E15–E29. [Google Scholar] [CrossRef] [PubMed]
- Schulz, S.; Schlitt, A.; Hofmann, B.; Schaller, H.G.; Reichert, S. Periodontal pathogens and their role in cardiovascular outcome. J. Clin. Periodontol. 2020, 47, 173–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bostanci, N.; Bao, K.; Greenwood, D.; Silbereisen, A.; Belibasakis, G.N. Periodontal disease: From the lenses of light microscopy to the specs of proteomics and next-generation sequencing. Adv. Clin. Chem. 2019, 93, 263–290. [Google Scholar] [PubMed]
- Feres, M.; Retamal-Valde, B.; Gonçalves, C.; Cristina Figueiredo, L.; Teles, F. Did Omics change periodontal therapy? Periodontol. 2000 2021, 85, 182–209. [Google Scholar] [CrossRef]
- Seneviratne, C.J.; Balan, P.; Suriyanarayanan, T.; Lakshmanan, M.; Lee, D.Y.; Rho, M.; Jakubovics, N.; Brandt, B.; Crielaard, W.; Zaura, E. Oral microbiome-systemic link studies: Perspectives on current limitations and future artificial intelligence-based approaches. Crit. Rev. Microbiol. 2020, 46, 288–299. [Google Scholar] [CrossRef]
- Choi, H.; Dey, A.K.; Priyamvara, A.; Aksentijevich, M.; Bandyopadhyay, D.; Dey, D.; Dani, S.; Guha, A.; Nambiar, P.; Nasir, K.; et al. Role of Periodontal Infection, Inflammation and Immunity in Atherosclerosis. Curr. Probl. Cardiol. 2021, 46, 100638. [Google Scholar] [CrossRef]
- Schenkein, H.A.; Papapanou, P.N.; Genco, R.; Sanz, M. Mechanisms underlying the association between periodontitis and atherosclerotic disease. Periodontol. 2000 2020, 83, 90–106. [Google Scholar] [CrossRef] [PubMed]
- Herrera, D.; Molina, A.; Buhlin, K.; Klinge, B. Periodontal diseases and association with atherosclerotic disease. Periodontol. 2000 2020, 83, 66–89. [Google Scholar] [CrossRef] [PubMed]
- Torrungruang, K.; Katudat, D.; Mahanonda, R.; Sritara, P.; Udomsak, A. Periodontitis is associated with elevated serum levels of cardiac biomarkers—Soluble ST2 and C-reactive protein. J. Clin. Periodontol. 2019, 46, 809–818. [Google Scholar] [CrossRef] [PubMed]
- Montenegro, M.M.; Ribeiro, I.W.J.; Kampits, C.; Saffi, M.A.L.; Furtado, M.V.; Polanczyk, C.A.; Haas, A.N.; Rösing, C.K. Randomized controlled trial of the effect of periodontal treatment on cardiovascular risk biomarkers in patients with stable coronary artery disease: Preliminary findings of 3 months. J. Clin. Periodontol. 2019, 46, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Antoniades, C.; Antonopoulos, A.S.; Deanfield, J. Imaging residual inflammatory cardiovascular risk. Eur. Heart J. 2020, 41, 748–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khurshid, Z.; Mali, M.; Adanir, N.; Zafar, M.S.; Khan, R.S.; Latif, M. Periostin: Immunomodulatory Effects on Oral Diseases. Eur. J. Dent. 2020, 14, 462–466. [Google Scholar] [CrossRef] [PubMed]
- Oka, T.; Xu, J.; Kaiser, R.A.; Melendez, J.; Hambleton, M.; Sargent, M.A.; Lorts, A.; Brunskill, E.W.; Dorn, G.W.; Conway, S.J.; et al. Genetic manipulation of periostin expression reveals a role in cardiac hypertrophy and ventricular remodeling. Circ. Res. 2007, 101, 313–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taniyama, Y.; Katsuragi, N.; Sanada, F.; Azuma, J.; Iekushi, K.; Koibuchi, N.; Okayama, K.; Ikeda-Iwabu, Y.; Muratsu, J.; Otsu, R.; et al. Selective Blockade of Periostin Exon 17 Preserves Cardiac Performance in Acute Myocardial Infarction. Hypertension 2016, 67, 356–361. [Google Scholar] [CrossRef]
- Chen, Z.; Xie, J.; Hao, H.; Lin, H.; Wang, L.; Zhang, Y.; Chen, L.; Cao, S.; Huang, X.; Liao, W.; et al. Ablation of periostin inhibits post-infarction myocardial regeneration in neonatal mice mediated by the phosphatidylinositol 3 kinase/glycogen synthase kinase 3β/cyclin D1 signalling pathway. Cardiovasc. Res. 2017, 113, 620–632. [Google Scholar] [CrossRef] [Green Version]
- Azharuddin, M.; Adil, M.; Ghosh, P.; Kapur, P.; Sharma, M. Periostin as a novel biomarker of cardiovascular disease: A systematic evidence landscape of preclinical and clinical studies. J. Evid. Based Med. 2019, 12, 325–336. [Google Scholar] [CrossRef]
- Wang, F.; Yang, C.; Song, Y.; Jiang, Y.; Ding, Z. Periostin gene polymorphisms, protein levels and risk of incident coronary artery disease. Mol. Biol. Rep. 2012, 39, 359–367. [Google Scholar] [CrossRef]
- Cheng, C.W.; Wang, C.H.; Lee, J.F.; Kuo, L.T.; Cherng, W.J. Levels of blood periostin decrease after acute myocardial infarction and are negatively associated with ventricular function after 3 months. J. Investig. Med. 2012, 60, 523–528. [Google Scholar] [CrossRef]
- Ling, L.; Cheng, Y.; Ding, L.; Yang, X. Association of serum periostin with cardiac function and short-term prognosis in acute myocardial infarction patients. PLoS ONE 2014, 9, 1–8. [Google Scholar] [CrossRef]
- Norum, H.M.; Broch, K.; Michelsen, A.E.; Lunde, I.G.; Lekva, T.; Abraityte, A.; Dahl, C.P.; Fiane, A.E.; Andreassen, A.K.; Christensen, G.; et al. The Notch Ligands DLL1 and Periostin Are Associated with Symptom Severity and Diastolic Function in Dilated Cardiomyopathy. J. Cardiovasc. Transl. Res. 2017, 10, 401–410. [Google Scholar] [CrossRef]
- Landry, N.M.; Cohen, S.; Dixon, I.M.C. Periostin in cardiovascular disease and development: A tale of two distinct roles. Basic Res. Cardiol. 2018, 113, 1. [Google Scholar] [CrossRef] [PubMed]
- Ţolescu, C.; Gerculy, R.; Libenciuc, C.; Kovacs, I. Differential Diagnosis of Myocardial Injury in the SARS-CoV-2 Era—Myocarditis Versus Acute Coronary Syndrome. J. Cardiovasc. Emerg. 2020, 6, 98–103. [Google Scholar] [CrossRef]
- Ponti, G.; Maccaferri, M.; Ruini, C.; Tomasi, A.; Ozben, T. Biomarkers associated with COVID-19 disease progression. Crit. Rev. Clin. Lab. Sci. 2020, 57, 389–399. [Google Scholar] [CrossRef]
- Ueland, T.; Holter, J.C.; Holten, A.R.; Müller, K.E.; Lind, A.; Bekken, G.K.; Dudman, S.; Aukrust, P.; Dyrhol-Riise, A.M.; Heggelund, L. Distinct and early increase in circulating MMP-9 in COVID-19 patients with respiratory failure: MMP-9 and respiratory failure in COVID-19. J. Infect. 2020, 81, e41–e43. [Google Scholar] [CrossRef] [PubMed]
- Jøntvedt Jørgensen, M.; Holter, J.C.; Christensen, E.E.; Schjalm, C.; Tonby, K.; Pischke, S.E.; Jenum, S.; Skeie, L.G.; Nur, S.; Lind, A.; et al. Increased interleukin-6 and macrophage chemoattractant protein-1 are associated with respiratory failure in COVID-19. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef]
- Lo, M.W.; Kemper, C.; Woodruff, T.M. COVID-19: Complement, Coagulation, and Collateral Damage. J. Immunol. 2020, 205, 1488–1495. [Google Scholar] [CrossRef]
- Galvan-Roman, J.M.; Rodriguez-Garcia, S.C.; Roy-Vallejo, E.; Marcos-Jimenez, A.; Sanzhez-Alonso, S.; Fernandez-Diaz, C.; Alcaraz-Serna, A.; Mateu-Albero, T.; Rodriguez-Cortez, P.; Sanchez-Cerrillo, I.; et al. IL-6 serum levels predict severity and response to tocilizumab in COVID-19: An observational study. J. Allergy Clin. Immunol. 2021, 147, 72–80. [Google Scholar] [CrossRef]
- Gao, Y.; Li, T.; Han, M.; Li, X.; Wu, D.; Xu, Y.; Zhu, Y.; Liu, Y.; Wang, X.; Wang, L. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J. Med. Virol. 2020, 92, 791–796. [Google Scholar] [CrossRef]
- Liu, F.; Li, L.; Xu, M.; Wu, J.; Luo, D.; Zhu, Y.; Li, B.; Song, X.; Zhou, X. Prognostic value, of IL-6, CRP, and PCT in patients with COVID-19. J. Clin. Virol. 2020, 127, 104370. [Google Scholar] [CrossRef]
- Coomes, E.A.; Haghbayan, H. Interleukin-6 in Covid-19: A systematic review and meta-analysis. Rev. Med. Virol. 2020, 30, 1–9. [Google Scholar] [CrossRef]
- Xie, Y.; You, Q.; Wu, C.; Cao, S.; Qu, G.; Yan, X.; Han, X.; Wang, C.; Zhang, H. Impact of cardiovascular disease on clinical characteristics and outcomes of coronavirus disease 2019. Circ. J. 2020, 84, 1277–1283. [Google Scholar] [CrossRef]
- Varchetta, S.; Mele, D.; Oliviero, B.; Mantovani, S.; Ludovisi, S.; Cerino, A.; Bruno, R.; Castelli, A.; Mosconi, M.; Vecchia, M. Unique immunological profile in patients with COVID-19. Cell. Mol. Immunol. 2021, 18, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Al-Samkari, H.; Karp Leaf, R.S.; Dzik, W.H.; Carlson, J.; Fogerty, A.E.; Waheed, A.; Goodarzi, K.; Bendapudi, P.K.; Bornikova, L.; Gupta, S. COVID-19 and coagulation: Bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood 2020, 136, 489–500. [Google Scholar] [CrossRef]
- Huang, Y.; Guo, H.; Zhou, Y.; Guo, J.; Wang, T.; Zhao, X.; Li, H.; Sun, Y.; Bian, X.; Fang, C. The associations between fasting plasma glucose levels and mortality of COVID-19 in patients without diabetes. Diabetes Res. Clin. Pract. 2020, 169, 108448. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.; Zhou, L.; Hu, Z.; Zhang, S. Dysregulation of immune response in patients with COVID-19 in Wuhan, China Chuan. J. Chem. Inf. Model 2017, 53, 1689–1699. [Google Scholar]
- Zhang, J.J.; Dong, X.; Cao, Y.Y.; Yuan, Y.D.; Yang, Y.B.; Yan, Y.Q.; Akdis, C.A.; Gao, Y.D. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy Eur. J. Allergy Clin. Immunol. 2020, 75, 1730–1741. [Google Scholar] [CrossRef] [PubMed]
- Valizadeh, H.; Abdolmohammadi-Vahid, S.; Danshina, S.; Ziya Gencer, M.; Ammari, A.; Sadeghi, A.; Roshangar, L.; Aslani, S.; Esmaeilzadeh, A.; Ghaebi, M. Nano-curcumin therapy, a promising method in modulating inflammatory cytokines in COVID-19 patients. Int. Immunopharmacol. 2020, 89, 107088. [Google Scholar] [CrossRef]
- Venet, F.; Cour, M.; Rimmelé, T.; Viel, S.; Yonis, H.; Coudereau, R.; Amaz, C.; Abraham, P.; Monard, C.; Casalegno, J.S.; et al. Longitudinal assessment of IFN-I activity and immune profile in critically ill COVID-19 patients with acute respiratory distress syndrome. Crit. Care 2021, 25, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hashemian, S.R.; Aliannejad, R.; Zarrabi, M.; Soleimani, M.; Vosough, M.; Hosseini, S.E.; Hossieni, H.; Keshel, S.H.; Naderpour, Z.; Hajizadeh-Saffar, E.; et al. Mesenchymal stem cells derived from perinatal tissues for treatment of critically ill COVID-19-induced ARDS patients: A case series. Stem Cell Res. Ther. 2021, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury with Mortality in Hospitalized Patients with COVID-19 in Wuhan, China. JAMA 2020, 5, 802–810. [Google Scholar] [CrossRef] [Green Version]
- Al-Wahaibi, K.; Al-Wahshi, Y.; Elfadil, O.M. Myocardial Injury Is Associated with Higher Morbidity and Mortality in Patients with 2019 Novel Coronavirus Disease (COVID-19). SN Compr. Clin. Med. 2020, 2, 2514–2520. [Google Scholar] [CrossRef]
- Rose, J.J.; Voora, D.; Cyr, D.D.; Lucas, J.E.; Zaas, A.K.; Woods, C.W.; Newby, L.K.; Kraus, W.E.; Ginsburg, G.S. Gene expression profiles link respiratory viral infection, platelet response to aspirin, and acute myocardial infarction. PLoS ONE 2015, 10, 1–15. [Google Scholar]
- Chen, L.; Li, X.; Chen, M.; Feng, Y.; Xiong, C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with, SARS-CoV-2. Cardiovasc. Res. 2020, 116, 1097–1100. [Google Scholar] [CrossRef] [Green Version]
- Larvin, H.; Wilmott, S.; Wu, J.; Kang, J. The Impact of Periodontal Disease on Hospital Admission and Mortality During COVID-19 Pandemic. Front. Med. 2020, 7, 1–7. [Google Scholar] [CrossRef]
- Larvin, H.; Wilmott, S.; Kang, J.; Aggarwal, V.R.; Pavitt, S.; Wu, J. Additive Effect of Periodontal Disease and Obesity on COVID-19 Outcomes. J. Dent. Res. 2021, 16, 220345211029638. [Google Scholar]
- Kara, C.; Çelen, K.; Dede, F.Ö.; Gökmenoğlu, C.; Kara, N.B. Is periodontal disease a risk factor for developing severe Covid-19 infection? The potential role of Galectin-3. Exp. Biol. Med. 2020, 245, 1425–1427. [Google Scholar] [CrossRef]
- Mancini, L.; Quinzi, V.; Mummolo, S.; Marzo, G.; Marchetti, E. Angiotensin-converting enzyme 2 as a possible correlation between COVID-19 and periodontal disease. Appl. Sci. 2020, 10, 6224. [Google Scholar] [CrossRef]
- Roganović, J. Downregulation of microRNA-146a in diabetes, obesity and hypertension may contribute to severe COVID-19. Med. Hypotheses 2021, 146, 2. [Google Scholar] [CrossRef]
- Kass, D.A.; Duggal, P.; Cingolani, O. Obesity could shift severe COVID-19 disease to younger ages. Lancet 2020, 395, 1544–1545. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, X.; Jia, X.; Li, J.; Hu, K.; Chen, G.; Wei, J.; Gong, Z.; Zhou, C.; Yu, H.; et al. Risk factors for disease severity, unimprovement, and mortality in COVID-19 patients in Wuhan, China. Clin. Microbiol. Infect. 2020, 26, 767–772. [Google Scholar] [CrossRef] [PubMed]
- Bortone, F.; Scandiffio, L.; Marcuzzo, S.; Bonanno, S.; Frangiamore, R.; Motta, T.; Antozzi, C.; Mantegazza, R.; Cavalcante, P.; Bernasconi, P. miR-146a in Myasthenia Gravis Thymus Bridges Innate Immunity with Autoimmunity and Is Linked to Therapeutic Effects of Corticosteroids. Front. Immunol. 2020, 11, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, J.L.; Yang, W.; Ito, K.; Matte, T.D.; Shaman, J.; Kinney, P.L. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. 2016, 1, 274–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwong, J.C.; Schwartz, K.L.; Campitelli, M.A.; Chung, H.; Crowcroft, N.S.; Karnauchow, T.; Katz, K.; Ko, D.T.; McGeer, A.J.; McNally, D.; et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N. Engl. J. Med. 2018, 378, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, S. SARS-Cov2 Enables Anaerobic Bacteria (Prevotella; et al.) to Colonize the Lungs Disrupting Homeostasis, Causing Long-Drawn Chronic Symptoms, and Acute Severe Symptoms (ARDS, Septic Shock, Clots, Arterial Stroke) which Finds Resonance, with Key Differences, in the ‘Forgotten Disease’ Lemierre Syndrome, Enabled by Epstein Barr Virus. Available online: https://osf.io/usztn/ (accessed on 12 August 2021).
- Patel, J.; Woolley, J. Necrotizing periodontal disease: Oral manifestation of COVID-19. Oral Dis. 2021, 27, 768–769. [Google Scholar] [CrossRef] [PubMed]
- Martín Carreras-Presas, C.; Amaro Sánchez, J.; López-Sánchez, A.F.; Jané-Salas, E.; Somacarrera Pérez, M.L. Oral vesiculobullous lesions associated with SARS-CoV-2 infection. Oral Dis. 2021, 27, 710–712. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Watanabe, N.; Kamio, N.; Kobayashi, R.; Iinuma, T.; Imai, K. Aspiration of periodontopathic bacteria due to poor oral hygiene potentially contributes to the aggravation of COVID-19. J. Oral Sci. 2021, 63, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Marouf, N.; Cai, W.; Said, K.N.; Daas, H.; Diab, H.; Chinta, V.R.; Hssain, A.A.; Nicolau, B.; Sanz, M.; Tamimi, F. Association between periodontitis and severity of COVID-19 infection: A case-control study. J. Clin. Periodontol. 2021, 48, 483–491. [Google Scholar] [CrossRef] [PubMed]
| Study | Pro-Inflammatory Cytokine | Main Findings | Statistical Relevance |
|---|---|---|---|
| Galvan-Roman J.M. et al. [51] | IL 6 | IL6 baseline level are directly correlated with the COVID-19 severity and the necessity of invasive ventilation | p < 0.0001 |
| Gao Y. et al. [52] | IL6 | IL 6 is an independent risk factor | p = 0.005 |
| Liu F. et al. [53] | IL 6 | The IL6 level predicts the COVID-19 severity | p < 0.001 |
| Coomes E., Haghbayan H. [54] | IL 6 | The IL 6 levels are strongly correlated with COVID-19 adverse clinical outcomes | |
| Xie Y. et al. [55] | IL6 | IL 6 level was higher in patients with CVD and COVID-19. Moreover, the higher the IL 6 level, the more severe the COVID -19 form is | p < 0.05 |
| Varchetta S. et al. [56] | IL 6 | Increased levels of IL 6 were found in serum of COVID-19 patients with severe forms. Moreover, IL 6 level was higher in non-survivor vs. survivors | p < 0.0001 p < 0.05 |
| Al-Samkari H. et al. [57] | CRP | Elevated CRP level is a predictor of thrombosis in patients with COVID-19 | OR 2.71, CI 95%, 1.26–5.86 |
| Huang Y. et al. [58] | CRP | The CRP level was higher in COVID-19 non-survivor patients | p < 0.0001 |
| Qin C. et al. [59] | CRP | CRP level is increased in severe vs. non-severe COVID 19 forms | p < 0.001 |
| Zhang J.J. et al. [60] | CRP | In severe COVID-19 group CRP levels are higher | p < 0.001 |
| Valizadeh H. et al. [61] | Tumor necrosis factor α | In COVID-19 group, NF was higher compared with control group | p < 0.0001 |
| Venet F. et al. [62] | Tumor necrosis factor α | Higher values of NF were found in non-survivor vs. survivors | |
| Hashemian S.R. et al. [63] | Tumor necrosis factor α | Lower levels of NF were associated with survivor status | p < 0.01 |
| Author, Journal, Year | Study Population | Mortality | Association with Myocardial Injury | Mortality in Patients with Myocardial Injury |
|---|---|---|---|---|
| Huang et al., Lancet, 2020 [64] | n = 41 | 6 (15.00%) | 5 (12.20%) | N.A. |
| Wang et al., JAMA, 2020 [65] | n = 138 | 6 (4.35%) | 10 (7.25%) | N.A. |
| Zhou et al., Lancet, 2020 [66] | n = 191 | 54 (28.27%) | 33 (17.28%) | 32 (16.75%) |
| Shi et al., JAMA, 2020 [67] | n = 416 | 57 (13.67%) | 82 (19.71%) | 42 (10.10%) |
| Al-Wahaibi et al., SN Compr Clin Med, 2020 [68] | n = 143 | 24 (16.78%) | 31 (21.68%) | 16 (11.19%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodean, I.-P.; Biriș, C.-I.; Halațiu, V.-B.; Modiga, A.; Lazăr, L.; Benedek, I.; Benedek, T. Is There a Link between COVID-19 Infection, Periodontal Disease and Acute Myocardial Infarction? Life 2021, 11, 1050. https://doi.org/10.3390/life11101050
Rodean I-P, Biriș C-I, Halațiu V-B, Modiga A, Lazăr L, Benedek I, Benedek T. Is There a Link between COVID-19 Infection, Periodontal Disease and Acute Myocardial Infarction? Life. 2021; 11(10):1050. https://doi.org/10.3390/life11101050
Chicago/Turabian StyleRodean, Ioana-Patricia, Carmen-Ioana Biriș, Vasile-Bogdan Halațiu, Andrei Modiga, Luminița Lazăr, Imre Benedek, and Theodora Benedek. 2021. "Is There a Link between COVID-19 Infection, Periodontal Disease and Acute Myocardial Infarction?" Life 11, no. 10: 1050. https://doi.org/10.3390/life11101050
APA StyleRodean, I.-P., Biriș, C.-I., Halațiu, V.-B., Modiga, A., Lazăr, L., Benedek, I., & Benedek, T. (2021). Is There a Link between COVID-19 Infection, Periodontal Disease and Acute Myocardial Infarction? Life, 11(10), 1050. https://doi.org/10.3390/life11101050







