Post-Infectious Guillain–Barré Syndrome Related to SARS-CoV-2 Infection: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Literature Search
2.3. Data Extraction and Management
3. Results
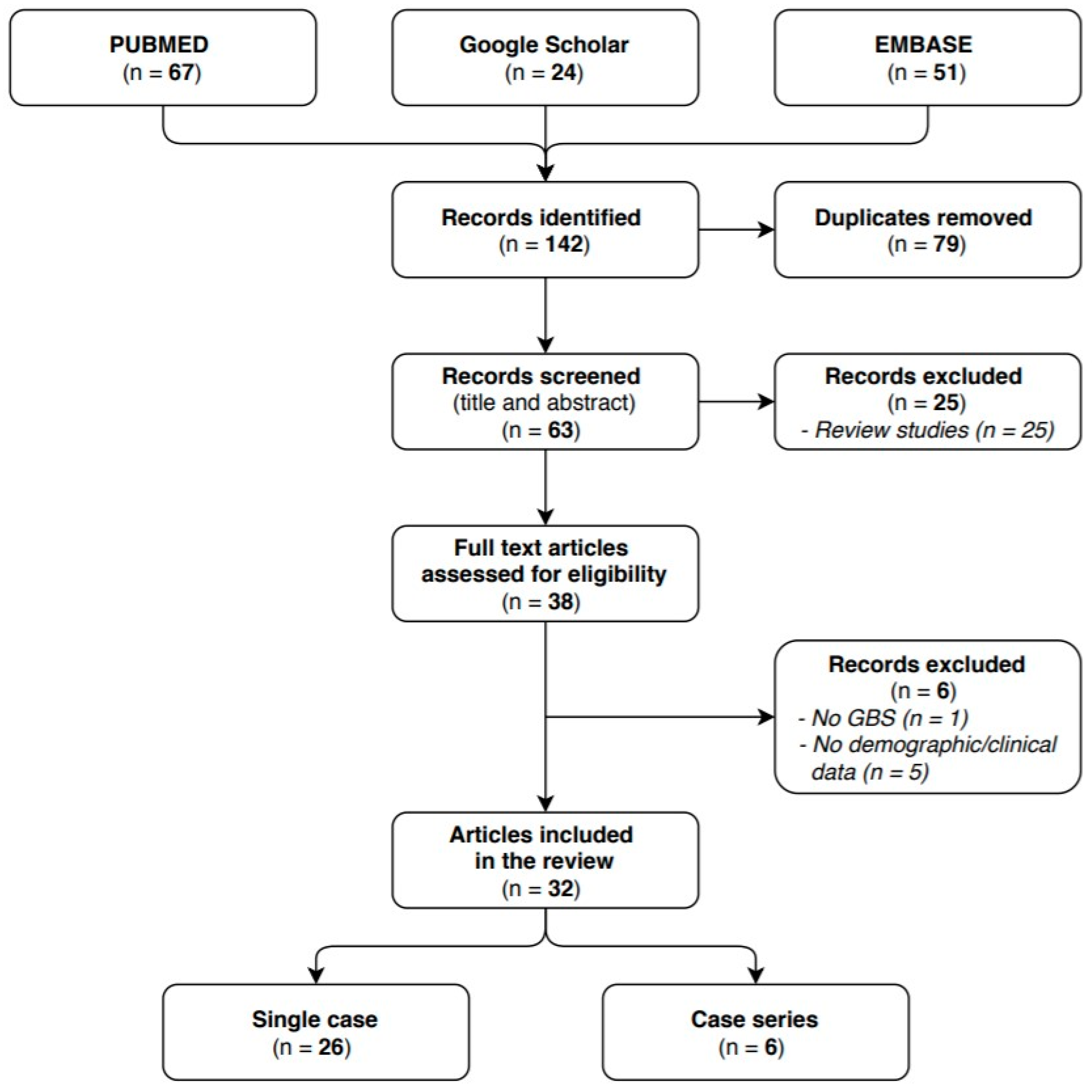
3.1. Study Selection
3.2. Study Characteristics
3.3. Patient Characteristics
3.3.1. Demographics
3.3.2. Certainty Levels of GBS Diagnosis and Infection
3.3.3. Clinical Characteristics
3.4. Diagnostic Investigations
3.5. Treatment and Disease Progression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Sejvar, J.J.; Baughman, A.L.; Wise, M.; Morgan, O.W. Population incidence of Guillain-Barre’ syndrome: A systematic review and meta-analysis. Neuroepidemiology 2011, 36, 123–133. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, B.C.; Rothbarth, P.H.; Van der Meché, F.G.A.; Herbrink, P.; Schmitz, P.I.M.; De Klerk, M.A.; Van Doorn, P.A. The spectrum of antecedent infections in Guillain-Barre’ syndrome: A case-control study. Neurology 1998, 51, 1110–1115. [Google Scholar] [CrossRef]
- Whittaker, A.; Anson, M.; Harky, A. Neurological Manifestations of COVID-19: A systematic review and current update. Acta Neurol. Scand. 2020, 142, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Willison, H.J.; Jacobs, B.C.; van Doorn, P.A. Guillain-Barré syndrome. Lancet 2016, 388, 717–727. [Google Scholar] [CrossRef] [Green Version]
- Dimachkie, M.M.; Barohn, R.J. Guillain-Barré syndrome and variants. Neurol. Clin. 2013, 31, 491–510. [Google Scholar] [CrossRef] [Green Version]
- Leonhard, S.E.; Mandarakas, M.R.; Gondim, F.A.; Bateman, K.; Ferreira, M.L.; Cornblath, D.R.; van Doorn, P.A.; Dourado, M.E.; Hughes, R.A.C.; Islam, B.; et al. Diagnosis and management of Guillain-Barré syndrome in ten steps. Nat. Rev. Neurol. 2019, 15, 671–683. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fokke, C.; van den Berg, B.; Drenthen, J.; Walgaard, C.; van Doorn, P.A.; Jacobs, B.C. Diagnosis of Guillain-Barré syndrome and validation of Brighton criteria. Brain 2014, 37, 33–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diagnostic Testing for SARS-CoV-2. Available online: https://www.who.int/publications/i/item/diagnostic-testing-for-sars-cov-2 (accessed on 24 September 2020).
- Alberti, P.; Beretta, S.; Piatti, M.; Karantzoulis, A.; Piatti, M.L.; Santoro, P.; Viganò, M.; Giovannelli, G.; Pirro, F.; Montisano, D.A.; et al. Guillain-Barré syndrome related to COVID-19 infection. Neurol. Neuroimmunol. Neuroinflamm. 2020, 7, e741. [Google Scholar] [CrossRef]
- Arnaud, S.; Budowski, C.; Tin, S.N.W.; Degos, B. Post SARS-CoV-2 Guillain-Barré syndrome. Clin. Neurophysiol. 2020, 131, 1652–1654. [Google Scholar] [CrossRef]
- Assini, A.; Benedetti, L.; Di Maio, S.; Schirinzi, E.; Del Sette, M. New clinical manifestation of COVID-19 related Guillain-Barrè syndrome highly responsive to intravenous immunoglobulins: Two Italian cases. Neurol. Sci. 2020, 41, 1657–1658. [Google Scholar] [CrossRef] [PubMed]
- Bigaut, K.; Mallaret, M.; Baloglu, S.; Nemoz, B.; Morand, P.; Baicry, F.; Godon, A.; Voulleminot, P.; Kremer, L.; Chanson, J.-B.; et al. Guillain-Barré syndrome related to SARS-CoV-2 infection. Neurol. Neuroimmunol. Neuroinflamm. 2020, 7, e785. [Google Scholar] [CrossRef] [PubMed]
- Juliao Caamaño, D.S.; Alonso Beato, R. Facial diplegia, a possible atypical variant of Guillain-Barré Syndrome as a rare neurological complication of SARS-CoV-2. J. Clin. Neurosci. 2020, 77, 230–232. [Google Scholar] [CrossRef] [PubMed]
- Camdessanche, J.P.; Morel, J.; Pozzetto, B.; Paul, S.; Tholance, Y.; Botelho-Nevers, E. COVID-19 may induce Guillain-Barré syndrome. Rev. Neurol. 2020, 176, 516–518. [Google Scholar] [CrossRef] [PubMed]
- Coen, M.; Jeanson, G.; Almeida, L.A.C.; Hübers, A.; Stierlin, F.; Najjar, I.; Ongaro, M.; Moulin, K.; Makrygianni, M.; Leemann, B. Guillain-Barré syndrome as a complication of SARS-CoV-2 infection. Brain Behav. Immun. 2020, 87, 111–112. [Google Scholar] [CrossRef]
- Dinkin, M.; Gao, V.; Kahan, J.; Bobker, S.; Simonetto, M.; Wechsler, P.; Harpe, J.; Greer, C.; Mints, G.; Salama, G.; et al. COVID-19 presenting with ophthalmoparesis from cranial nerve palsy. Neurology 2020, 95, 221–223. [Google Scholar] [CrossRef] [PubMed]
- El Otmani, H.; El Moutawakil, B.; Rafai, M.A.; El Benna, N.; El Kettani, C.; Soussi, M.; El Mdaghri, N.; Barrou, H.; Afif, H. Covid-19 and Guillain-Barré syndrome: More than a coincidence! Rev. Neurol. 2020, 176, 518–519. [Google Scholar] [CrossRef]
- Fernández-Domínguez, J.; Ameijide-Sanluis, E.; García-Cabo, C.; García-Rodríguez, R.; Mateos, V. Miller-Fisher-like syndrome related to SARS-CoV-2 infection (COVID 19). J. Neurol. 2020, 267, 2495–2496. [Google Scholar] [CrossRef] [PubMed]
- Velayos Galán, A.; Del Saz Saucedo, P.; Peinado Postigo, F.; Botia Paniagua, E. Guillain-Barré syndrome associated with SARS-CoV-2 infection. Neurologia 2020, 35, 268–269. [Google Scholar] [CrossRef] [PubMed]
- Granger, A.; Omari, M.; Jakubowska-Sadowska, K.; Boffa, M.; Zakin, E. SARS-CoV-2-Associated Guillain-Barre Syndrome With Good Response to Plasmapheresis. J. Clin. Neuromuscul. Dis. 2020, 22, 58–59. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Ortiz, C.; Méndez-Guerrero, A.; Rodrigo-Rey, S.; San Pedro-Murillo, E.; Bermejo-Guerrero, L.; Gordo-Mañas, R.; de Aragón-Gómez, F.; Benito-León, J. Miller Fisher syndrome and polyneuritis cranialis in COVID-19. Neurology 2020, 95, e601–e605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lantos, J.E.; Strauss, S.B.; Lin, E. COVID-19-Associated Miller Fisher Syndrome: MRI Findings. AJNR Am. J. Neuroradiol. 2020, 41, 1184–1186. [Google Scholar] [CrossRef] [PubMed]
- Manganotti, P.; Pesavento, V.; Stella, A.B.; Bonzi, L.; Campagnolo, E.; Bellavita, G.; Fabris, B.; Luzzati, R. Miller Fisher syndrome diagnosis and treatment in a patient with SARS-CoV-2. J. Neurovirol. 2020, 26, 605–606. [Google Scholar] [CrossRef]
- Marta-Enguita, J.; Rubio-Baines, I.; Gastón-Zubimendi, I. Fatal Guillain-Barre syndrome after infection with SARS-CoV-2. Neurologia 2020, 35, 265–267. [Google Scholar] [CrossRef]
- Naddaf, E.; Laughlin, R.S.; Klein, C.J.; Toledano, M.; Theel, E.S.; Binnicker, M.J. Guillain-Barré Syndrome in a Patient with Evidence of Recent SARS-CoV-2 Infection. Mayo Clin. Proc. 2020, 95, 1799–1801. [Google Scholar] [CrossRef]
- Oguz-Akarsu, E.; Ozpar, R.; Mirzayev, H.; Acet-Ozturk, N.A.; Hakyemez, B.; Ediger, D.; Karli, N. Guillain-Barré Syndrome in a Patient with Minimal Symptoms of COVID-19 Infection. Muscle Nerve. 2020, 62, E54–E57. [Google Scholar] [CrossRef]
- Ottaviani, D.; Boso, F.; Tranquillini, E.; Gapeni, I.; Pedrotti, G.; Cozzio, S.; Guarrera, G.M.; Giometto, B. Early Guillain-Barré syndrome in coronavirus disease 2019 (COVID-19): A case report from an Italian COVID-hospital. Neurol. Sci. 2020, 41, 1351–1354. [Google Scholar] [CrossRef]
- Padroni, M.; Mastrangelo, V.; Asioli, G.M.; Pavolucci, L.; Abu-Rumeileh, S.; Piscaglia, M.G.; Querzani, P.; Callegarini, C.; Foschi, M. Guillain-Barré syndrome following COVID-19: New infection, old complication? J. Neurol. 2020, 267, 1877–1879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paybast, S.; Gorji, R.; Mavandadi, S. Guillain-Barré Syndrome as a Neurological Complication of Novel COVID-19 Infection: A Case Report and Review of the Literature. Neurologist 2020, 25, 101–103. [Google Scholar] [CrossRef]
- Pfefferkorn, T.; Dabitz, R.; von Wernitz-Keibel, T.; Aufenanger, J.; Nowak-Machen, M.; Janssen, H. Acute polyradiculoneuritis with locked-in syndrome in a patient with Covid-19. J. Neurol. 2020, 267, 1883–1884. [Google Scholar] [CrossRef]
- Rana, S.; Lima, A.A.; Chandra, R.; Valeriano, J.; Desai, T.; Freiberg, W.; Small, G. Novel Coronavirus (COVID-19)-Associated Guillain-Barré Syndrome: Case Report. J. Clin. Neuromuscul. Dis. 2020, 21, 240–242. [Google Scholar] [CrossRef] [PubMed]
- Ray, A. Miller Fisher syndrome and COVID-19: Is there a link? BMJ Case Rep. 2020, 13, e236419. [Google Scholar] [CrossRef]
- Riva, N.; Russo, T.; Falzone, Y.M.; Strollo, M.; Amadio, S.; Del Carro, U.; Locatelli, M.; Filippi, M.; Fazio, R. Post-infectious Guillain-Barré syndrome related to SARS-CoV-2 infection: A case report. J. Neurol. 2020, 267, 2492–2494. [Google Scholar] [CrossRef]
- Scheidl, E.; Canseco, D.D.; Hadji-Naumov, A.; Bereznai, B. Guillain-Barré syndrome during SARS-CoV-2 pandemic: A case report and review of recent literature. J. Peripher Nerv. Syst. 2020, 25, 204–207. [Google Scholar] [CrossRef]
- Sedaghat, Z.; Karimi, N. Guillain Barre syndrome associated with COVID-19 infection: A case report. J. Clin. Neurosci. 2020, 76, 233–235. [Google Scholar] [CrossRef] [PubMed]
- Su, X.W.; Palka, S.V.; Rao, R.R.; Chen, F.S.; Brackney, C.R.; Cambi, F. SARS-CoV-2-associated Guillain-Barré syndrome with dysautonomia. Muscle Nerve. 2020, 62, E48–E49. [Google Scholar] [CrossRef]
- Tiet, M.Y.; Al Shaikh, N. Guillain-Barré syndrome associated with COVID-19 infection: A case from the UK. BMJ Case Rep. 2020, 13, e236536. [Google Scholar] [CrossRef] [PubMed]
- Toscano, G.; Palmerini, F.; Ravaglia, S.; Ruiz, L.; Invernizzi, P.; Cuzzoni, M.G.; Baldanti, F.; Postorino, P. Guillain-Barré Syndrome Associated with SARS-CoV-2. N. Engl. J. Med. 2020, 382, 2574–2576. [Google Scholar] [CrossRef]
- Webb, S.; Wallace, V.C.; Martin-Lopez, D.; Yogarajah, M. Guillain-Barré syndrome following COVID-19: A newly emerging post-infectious complication. BMJ Case Rep. 2020, 13, e236182. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Shen, D.; Zhou, H.; Liu, J.; Chen, S. Guillain-Barré syndrome associated with SARS-CoV-2 infection: Causality or coincidence? Lancet Neurol. 2020, 19, 383–384. [Google Scholar] [CrossRef]
- Finsterer, J.; Stollberger, C. Update on the neurology of COVID-19. J. Med. Virol. 2020, 92, 2316–2318. [Google Scholar] [CrossRef]
- Finsterer, J.; Scorza, F.A.; Ghosh, R. COVID-19 polyradiculitis in 24 patients without SARS-CoV-2 in the cerebro-spinal fluid. J. Med. Virol. 2020, 4, 10. [Google Scholar] [CrossRef]
- Sun, X.; Wang, T.; Cai, D.; Hu, Z.; Chen, J.; Liao, H.; Zhi, L.; Wei, H.; Zhang, Z.; Qiu, Y.; et al. Cytokine storm intervention in the early stages of COVID-19 pneumonia. Cytokine Growth Factor Rev. 2020, 53, 38–42. [Google Scholar] [CrossRef]
- Yuki, N.; Susuki, K.; Koga, M.; Nishimoto, Y.; Odaka, M.; Hirata, K.; Taguchi, K.; Miyatake, T.; Furukawa, K.; Kobata, T.; et al. Carbohydrate mimicry between human ganglioside GM1 and Campylobacter jejuni lipooligosaccharide causes Guillain-Barre syndrome. Proc. Natl. Acad. Sci. USA 2004, 101, 11404–11409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paniz-Mondolfi, A.; Bryce, C.; Grimes, Z.; Gordon, R.E.; Reidy, J.; Lednicky, J.; Sordillo, E.M.; Fowkes, M. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J. Med. Virol. 2020, 92, 699–702. [Google Scholar] [CrossRef] [Green Version]
- van den Berg, B.; Walgaard, C.; Drenthen, J.; Fokke, C.; Jacobs, B.C.; van Doorn, P.A. Guillain-Barré syndrome: Pathogenesis, diagnosis, treatment, and prognosis. Nat. Rev. Neurol. 2014, 10, 469–482. [Google Scholar] [CrossRef] [PubMed]
- Domingues, R.B.; Fernandes, G.B.P.; Leite, F.B.V.D.M.; Tilbery, C.P.; Thomaz, R.B.; Silva, G.S.; Mangueira, C.L.P.; Soares, C.A.S. The cerebrospinal fluid in multiple sclerosis: Far beyond the bands. Einstein 2017, 15, 100–104. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.H.; Jiang, D.; Huang, J.T. SARS-CoV-2 Detected in Cerebrospinal Fluid by PCR in a Case of COVID-19 Encephalitis. Brain Behav. Immun. 2020, 87, 149. [Google Scholar] [CrossRef]
- Al Saiegh, F.; Ghosh, R.; Leibold, A.; Avery, M.B.; Schmidt, R.F.; Theofanis, T.; Mouchtouris, N.; Philipp, L.; Peiper, S.C.; Wang, Z.-X.; et al. Status of SARS-CoV-2 in cerebrospinal fluid of patients with COVID-19 and stroke. J. Neurol. Neurosurg Psychiatry 2020, 91, 846–848. [Google Scholar] [CrossRef]
- Khan, S.; Gomes, J. Neuropathogenesis of SARS-CoV-2 infection. Elife 2020, 9, e59136. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Xu, Y.; Gao, R.; Lu, R.; Han, K.; Wu, G.; Tan, W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA 2020, 323, 1843–1844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hughes, R.A.C.; Swan, A.V.; van Doorn, P.A. Intravenous immunoglobulin for Guillain-Barré syndrome. Cochrane Database Syst. Rev. 2014, 9, CD002063. [Google Scholar] [CrossRef] [PubMed]
- Raphaël, J.C.; Chevret, S.; Hughes, R.A.; Annane, D. Plasma exchange for Guillain-Barré syndrome. Cochrane Database Syst. Rev. 2002, CD001798. [Google Scholar] [CrossRef]
- Hughes, R.A.C.; Brassington, R.; Gunn, A.A.; van Doorn, P.A. Corticosteroids for Guillain-Barré syndrome. Cochrane Database Syst. Rev. 2016, 10, CD001446. [Google Scholar] [CrossRef] [PubMed]


| Authors, Year | Country | Sex, Age (Years) | COVID-19 Related Symptoms | COVID-19 Diagnosis | Neurological Symptoms | GBS Diagnosis | GBS Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Alberti P. et al., 2020 [10] | Italy | M, 71 | Fever. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Paresthesia at limb extremities and distal weakness. Flaccid severe tetraparesis. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AIDP. | IVIg (0.4 g/kg/d) for 5 days. | Died. |
| Arnaud S. et al., 2020 [11] | France | M, 64 | Cough, fever, dyspnea and diarrhea. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Distal weakness, flaccid paraparesis, decreased proprioceptive length-dependent sensitivity involving the four limbs. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AIDP. | IVIg (?) for 5 days. | Recovery. |
| Assini A. et al., 2020 [12] | Italy | M, 55 | Anosmia, ageusia, fever and cough. | - Nasal swab: RT-PCR + | Bilateral eyelid ptosis, dysphagia, and dysphonia. | - CSF: Total protein level normal. SARS-CoV-2 neg. - Reflex: general hyporeflexia. - EMG: AIDP. | IVIg (0.4 g/kg/d) for 5 days. | Recovery. |
| M, 60 | Fever and cough. | - Nasal swab: RT-PCR + - CT scan: interstitial pneumonia. | Distal weakness, gastroplegia, paralytic ileus, and loss of blood pressure control. | - CSF: total protein level normal. SARS-CoV-2 neg. - Reflex: hyporeflexia. - EMG: AMSAN. | IVIg (0.4 g/kg/d) for 5 days. | Recovery. | ||
| Bigaut K. et al., 2020 [13] | France | M, 43 | Cough, asthenia, myalgia, anosmia, ageusia, diarrhea. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Paraesthesia, hypoesthesia, and distal weakness in the lower limbs. Ataxia. Right peripheral facial palsy. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes (exept left biceps reflex). - EMG: AMAN. | IVIg (2 g/kg). | Recovery. |
| F, 70 | Anosmia, ageusia, diarrhea, mild asthenia. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Flaccid tetraparesis, generalized areflexia, forelimb paresthesia, respiratory failure | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AMSAN. | IVIg (2 g/kg). | Recovery. | ||
| Caamaño DSJ et al., 2020 [14] | Spain | M, 61 | Cough, fever. | - Nasal swab: RT-PCR + | Peripheral facial nerve palsy. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Normal. - EMG: Not performed. | Prednisone. | Recovery. |
| Camdessanche JP et al., 2020 [15] | France | M, 64 | Cough, fever. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Paresthesia, flaccid severe tetraparesia. Swallowing disturbance. | - CSF: ACD. - Reflex: Absent deep tendon reflexes. - EMG: AIDP. | IVIg (0.4 g/kg/d) for 5 days. | ? |
| Coen M et al., 2020 [16] | Switzerland | M, 70 | Myalgia, fatigue, cough. | - Nasal swab: RT-PCR + - Anti-SARS-CoV-2 IgA and IgG + | Paraparesis, distal allodynia, difficulties in voiding, constipation. | - CSF: ACD. - Reflex: Absent deep tendon reflexes. - EMG: AIDP. | IVIg (0.4 g/kg/d) for 5 days. | Recovery. |
| Dinkin M et al., 2020 [17] | U.S. | M, 36 | Fever, cough, and myalgias. | - Nasal swab: RT-PCR + | Left ptosis, diplopia, and bilateral distal leg paresthesias. | - CSF: Total protein level normal. SARS-CoV-2 neg. - Reflex: General hyporeflexia. - EMG: Not performed. | IVIg (2g/kg) for 3 days. | Recovery. |
| F, 71 | Cough and fever. | - Nasal swab: RT-PCR + | Diplopia. | - CSF: Normal. - Reflex: Not performed. - EMG: Not performed. | None. | Recovery. | ||
| El Otmani H et al., 2020 [18] | Marocco | F, 70 | Cough. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Weakness and tingling sensation in four extremities. Quadriplegia and hypotonia. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AMSAN | IVIg (2 g/kg) for 5 days. | No significant neurological improvement after one week. |
| Fernandez-Dominguez J et al., 2020 [19] | Spain | F, 74 | Respiratory symptoms. | - Nasal swab: RT-PCR + | Gait impairment, blurred vision. | - CSF: ACD. - Reflex: Absent deep tendon reflexes. - EMG: ? | IVIg (20 g/d) for 5 days. | Recovery. |
| Galan AV et al., 2020 [20] | Spain | F, 43 | Diarrhea and respiratory symptoms. | - Nasal swab: RT-PCR + | Distal weakness and gait impairment. Facial palsy and dysphagia. | - CSF: Not performed. - Reflex: General hyporeflexia. - EMG: AIDP | IVIg (?) for 5 days. | Recovery. |
| Granger A et al., 2020 [21] | U.S. | M, 48 | Viral syndrome. | - Nasal swab: RT-PCR + | Progressive and symmetric sensorimotor deficits involving the face, extremities, and trunk. Right facial paralysis. | - CSF: ACD. - Reflex: Absent deep tendon reflexes. - EMG: AMSAN. | PLEX (5 sessions). | Recovery. |
| Gutierrez-Ortiz C et al., 2020 [22] | Spain | M, 50 | Cough, malaise, headache, low back pain, fever. | - Nasal swab: RT-PCR + - Chest X-ray: normal. | Vertical diplopia, perioral paresthesias, and gait instability. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: Not performed. | IVIg (0.4 g/kg) for 5 days. | Recovery. |
| M, 39 | Diarrhea and fever. | - Nasal swab: RT-PCR + - Chest X-ray: normal. | Diplopia. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: Not performed. | None. | Recovery. | ||
| Lantos JE et al., 2020 [23] | U.S. | M, 36 | Fevers, chills, and myalgia. | - Nasal swab: RT-PCR + | Left eye drooping, blurry vision, reduced sensation and paresthesia in both legs. Ophthalmoparesis and ataxia. | - CSF: Not performed. - Reflex: general hyporeflexia. - EMG: Not performed. | IVIg (?) | Recovery. |
| Manganotti P et al., 2020 [24] | Italy | F, 50 | Fever, cough and augesia. | - ? | Diplopia and facial paresthesia. Ataxia and gait impairment. | - CSF: ACD. - Reflex: ? - EMG: not performed. | IVIg (0.4 g/kg) for 5 days. | Recovery. |
| Marta-Enguita J et al., 2020 [25] | Spain | F. 74 | Fever. | - Nasal swab: RT-PCR + - CT scan: interstitial pneumonia. | Progressive tetraparesis with distal paresthesias. Dysphagia. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: Not performed. | ? | Died. |
| Naddaf E et al., 2020 [26] | U.S. | F, 58 | Dysgeusia, fever, myalgia, and asthenia. | - Nasal swab: RT-PCR - - Anti-SARS-CoV-2 IgA and IgG + | Progressive bilateral paraparesis, imbalance, severe lower thoracic pain and gait difficulty. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent in the legs and decreased in the upper extremities. - EMG: AIDP. | PLEX (5 sessions). | Slightly ataxic. |
| Oguz-Akarsu E et al., 2020 [27] | Turkey | F, 53 | Fever. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Dysarthria, progressive weakness and numbness of the lower extremities. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent in the legs. - EMG: AIDP. | PLEX (5 sessions). | Recovery. |
| Ottaviani D et al., 2020 [28] | Italy | F, 66 | Fever and cough. Pruriginous dorsal rash. | - Nasal swab: RT-PCR – (I°), then + (II°). - CT scan: ground-glass opacities. | Difficulty walking and acute fatigue. Paraparetic with a rapidly progressive symmetric weakness in the upper and lower limbs. | - CSF: ACD. - Reflex: Absent deep tendon reflexes. - EMG: AIDP/AMAN | IVIg ( 0,4 g/kg) for 5 days. | Multiple Organ Failure. |
| Padroni M et al., 2020 [29] | Italy | F, 70 | Fever and cough. | - Nasal swab: RT-PCR + (I°), then - (II°). - CT scan: ground-glass opacities. | Asthenia, hands and feet paresthesia and gait difficulties. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AIDP | IVIg (400 mg/d) for 5 days. | Respiratory failure. |
| Paybast S et al., 2020 [30] | Iran | M, 38 | Viral syndrome | ? | Ascending paresthesia, bilateral facial droop. Autonomic features (tachycardia and blood pressure instability). Swallowing disturbance. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AIDP/AMAN. | PLEX (5 sessions). | ? |
| F, 14 | Headaches and dizziness. | ? | Ascending quadripareshtesia. Lower limb weakness. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Hypoactive in upper limbs and absent in lower limbs. - EMG: Not preformed. | IVIg (20 g/d) for 5 days. | ? | ||
| Pfefferkorn T et al., 2020 [31] | Germany | M, 51 | Fever and flu-like symptoms with marked fatigue and cough. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Progressive upper and lower limb weakness and acral paresthesias. Respiratory faiulure. Peripheral locked-in syndrome with tetraplegia. | - CSF: Total protein level normal. SARS-CoV-2 neg. - Reflex: General hyporeflexia. - EMG: AMSAN. | IVIg (30 g/d) for 5 days. PLEX (14 sessions). | Rehabilitation. |
| Rana S et al., 2020 [32] | U.S. | M, 54 | Rhinorrhea, odynophagia, fevers, chills, and night sweats. | - Nasal swab: RT-PCR + | Ascending limb weakness and numbness. Difficulty voiding urine. Respiratory faiulure. Facial diplegia, quadriparesis and mild ophthalmoparesis. | - CSF: Not performed. - Reflex: Absent deep tendon reflexes. - EMG: AIDP/AMAN | IVIg (400 mg/kg/d). | Rehabilitation. |
| Ray A, 2020 [33] | UK | M, 63 | Fever. | - Nasal swab: RT-PCR + | Diplopia, perioral paresthesias, finger tingling and gait impairment. | - CSF: ACD. - Reflex: Absent deep tendon reflexes. - EMG: Not performed. | None. | Recovery. |
| Riva N et al., 2020 [34] | Italy | M, 60 | Fever, headache, myalgia, anosmia and ageusia. | - Nasal swab: RT-PCR - - Anti-SARS-CoV-2 IgG+ - CT scan: ground-glass opacities. | Progressive limb weakness and distal paresthesia at four-limbs. Facial diplegia, hypophonia and dysarthria. | - CSF: Normal. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AIDP. | IVIg (0.4 g/kg/d) for 5 days. | Recovery. |
| Scheidl E et al., 2020 [35] | Germany | F, 54 | Anosmia and ageusia. | - Nasal swab: RT-PCR + | Proximally and symmetric paraparesis. Numbness and tingling of all extremities. | - CSF: ACD. - Reflex: Absent deep tendon reflexes. - EMG: AIDP. | IVIg (0.4 g/kg/d) for 5 days. | Recovery. |
| Sedaghat Z et al., 2020 [36] | Iran | M, 65 | Cough, fever and dyspnea. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Acute progressive symmetric ascending quadriparesis, facial paresis and dysphagia. | - CSF: Not performed. - Reflex: Absent deep tendon reflexes. - EMG: AMSAN. | IVIg (0.4 g/kg/d) for 5 days. | ? |
| Su XW et al., 2020 [37] | U.S. | M, 72 | Diarrhea, anorexia and chills. | - Nasal swab: RT-PCR + | Symmetric paresthesias and ascending appendicular weakness. Respiratory faiulure. Dysautonomia with hypotension alternating with hypertension and tachycardia. SIADH. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AIDP. | IVIg (2 g/kg) for 4 days. | Severe weakness. |
| Tiet MY et al., 2020 [38] | U.K. | M, 49 | Shortness of breath, headache and cough. | - Nasal swab: RT-PCR + | Distal lower limb paraesthesia resulting in difficulty mobilising, facial diplegia, weakness and dysaesthesia in lower limbs. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AIDP. | IVIg (0.4 g/kg/d) for 5 days. | Recovery. |
| Toscano G et al., 2020 [39] * - Nasal swab: RT-PCR + (n = 4) - IgG + (n = 1) ** EMG: AIDP (n = 2); AMAN (n = 3) | Italy | Fever, cough, and ageusia | - Nasal swab: RT-PCR + (n=4); - IgG + (n=1). | Flaccid areflexic tetraplegia. Facial weakness, upper-limb paresthesia and respiratory faiure. | - CSF: I°) normal; II°) ACD. SARS-CoV-2 neg. - EMG: * | IVIg (?) | Severe upper-limb weakness, dysphagia, and lower-limb paraplegia. | |
| Fever and pharyngitis. | Facial diplegia and lower limb paresthesia with ataxia. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: * | IVIg (?) | Recovery. | ||||
| Fever and cough. | Flaccid tetraparesis and facial weakness. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: * | IVIg (?) | Respiratory failure and flaccid tetraplegia. | ||||
| Cough and hyposmia. | Flaccid tetraparesis and ataxia. | - CSF: normal. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: * | IVIg (?) | Mild improvement. | ||||
| Cough, ageusia, and anosmia. | Facial weakness and flaccid paraplegia. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: * | IVIg (?) PLEX (?) | Bacterial pneumonia. | ||||
| * EMG: AIDP (n = 2); AMAN (n = 3) | ||||||||
| Webb S et al., 2020 [40] | U.K. | M, 57 | Cough, headache, myalgia and malaise. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Progressive limb weakness and foot dysaesthesia. Respiratory faiulure. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Hyporeflexia. - EMG: AIDP. | IVIg (2 g/kg/d) for 5 days. | Mild improvement. |
| Zhao H et al., 2020 [41] | China | F, 61 | Cough and fever. | - Nasal swab: RT-PCR + - CT scan: ground-glass opacities. | Acute weakness in both legs and severe fatigue. | - CSF: ACD. SARS-CoV-2 neg. - Reflex: Absent deep tendon reflexes. - EMG: AIDP | IVIg (?) | Recovery. |
| Neurological Symptoms | N | N/GBS Cases * (%) |
| Dysphagia | 7 | 17.1 |
| Dysarthria | 4 | 9.8 |
| Diplopia | 9 | 21.9 |
| Neurological Signs | N | N/GBS Cases * (%) |
| Facial palsy | 13 | 31.7 |
| Bulbar palsy | 4 | 9.8 |
| Ocular palsy | 7 | 17.1 |
| Tetraparesis | 11 | 26.8 |
| Paraparesis | 7 | 17.1 |
| Paresthesia | 26 | 63.4 |
| Areflexia or hyporeflexia | 34 | 82.9 |
| Ataxia | 12 | 29.3 |
| Respiratory dysfunction | 7 | 17.1 |
| Dysautonomia | 5 | 12.2 |
| SARS-CoV-2 virus Certainty Level | Cases (%) | ||
| Confirmed | 40/41 (97.6%) | ||
| Probable | 1/41 (2.4%) | ||
| Suspected | 0/41 | ||
| Arboviral Tests | Cases (%) | ||
| SARS-CoV-2 virus | Total | Pos. | Neg. |
| PCR (Nasopharyngeal swab test) | 36/41 (87.8%) | 33/36 (91.7%) | 3/36 (8.3%) |
| PCR (Oropharyngeal swab test) | 4/41 (9.7%) | 4/4 (100%) | 0/4 |
| IgA serum | 2/41 (4.9%) | 2/2 (100%) | 0/2 |
| IgG serum | 4/41 (9.7%) | 4/4 (100%) | 0/4 |
| PCR CSF | 24/41 (58.5%) | 0/24 | 24/24 (100%) |
| Serological test (Campylobacter jejuni, HIV, syphilis, CMV, and EBV) | 11/41 (26.8%) | 0/11 | 11/11 (100%) |
| Radiology Test | Cases (%) | ||
| COVID-19 radiologiac features | Total | Pos. | Neg. |
| Chest X-ray | 11/40 (27.5%) | 5/11 (45.5%) | 6/11 (54.5%) |
| Chest CT | 15/40 (37.5%) | 15/15 (100%) | 0/15 |
| CSF Analysis | |||
| Increased protein level | 1/31 (3.2%) | ||
| ACD | 26/31 (83.9%) | ||
| Normal | 4/31 (12.9%) | ||
| Electrophysiological Exam | |||
| AIDP | 17/30 (56.7%) | ||
| AMAN | 4/30 (13.3%) | ||
| AMSAN | 5/30 (16.7%) | ||
| Equivocal | 3/30 (10.0%) | ||
| Inconclusive | 1/30 (3.3%) | ||
| Immunomodulatory Treatment | |||
| IVIg | 30/36 (83.3%) | ||
| Plasma exchange | 4/36 (11.1%) | ||
| IVIg and plasma exchange | 2/36 (5.6%) | ||
| Disease Progression | |||
| Admission to ICU | 14/41 (34.1%) | ||
| Mechanical ventilation | 14/41 (34.1%) | ||
| Died | 2/41 (4.9%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sansone, P.; Giaccari, L.G.; Aurilio, C.; Coppolino, F.; Esposito, V.; Fiore, M.; Paladini, A.; Passavanti, M.B.; Pota, V.; Pace, M.C. Post-Infectious Guillain–Barré Syndrome Related to SARS-CoV-2 Infection: A Systematic Review. Life 2021, 11, 167. https://doi.org/10.3390/life11020167
Sansone P, Giaccari LG, Aurilio C, Coppolino F, Esposito V, Fiore M, Paladini A, Passavanti MB, Pota V, Pace MC. Post-Infectious Guillain–Barré Syndrome Related to SARS-CoV-2 Infection: A Systematic Review. Life. 2021; 11(2):167. https://doi.org/10.3390/life11020167
Chicago/Turabian StyleSansone, Pasquale, Luca Gregorio Giaccari, Caterina Aurilio, Francesco Coppolino, Valentina Esposito, Marco Fiore, Antonella Paladini, Maria Beatrice Passavanti, Vincenzo Pota, and Maria Caterina Pace. 2021. "Post-Infectious Guillain–Barré Syndrome Related to SARS-CoV-2 Infection: A Systematic Review" Life 11, no. 2: 167. https://doi.org/10.3390/life11020167
APA StyleSansone, P., Giaccari, L. G., Aurilio, C., Coppolino, F., Esposito, V., Fiore, M., Paladini, A., Passavanti, M. B., Pota, V., & Pace, M. C. (2021). Post-Infectious Guillain–Barré Syndrome Related to SARS-CoV-2 Infection: A Systematic Review. Life, 11(2), 167. https://doi.org/10.3390/life11020167










