Neurosurgical CSF Diversion in Idiopathic Intracranial Hypertension: A Narrative Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Neurosurgical Involvement in IIH
3.1.1. CSF Diversion Strategies
3.1.2. LP Shunt
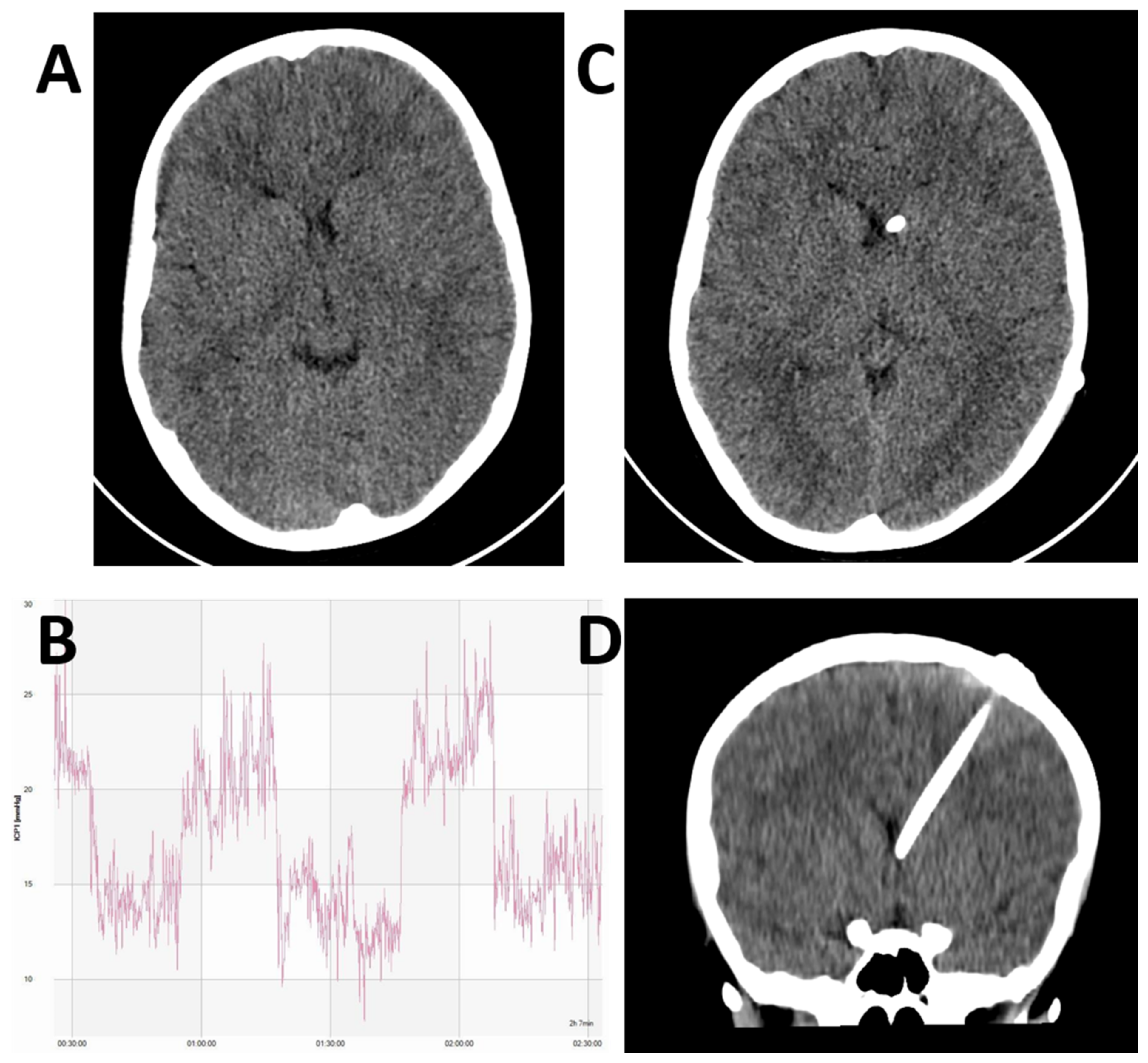
3.1.3. Cranial CSF Shunts
3.2. Complications
3.2.1. Surgical
3.2.2. Shunt Failure
3.2.3. Over-Drainage
3.2.4. Management of Suspected Shunt Malfunction, Obstruction, or Over-Drainage
3.3. Shunt Valve Selection
3.3.1. Flow Control vs. Differential Pressure
3.3.2. Programmable Valves
3.3.3. Anti-Siphon Devices and Gravitational Valves
3.4. Experience from the BASICS Trial
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Durcan, F.J.; Corbett, J.J.; Wall, M. The Incidence of Pseudotumor Cerebri. Arch. Neurol. 1988, 45, 875–877. [Google Scholar] [CrossRef]
- Ball, A.K.; Clarke, C.E. Idiopathic intracranial hypertension. Lancet Neurol. 2006, 5, 433–442. [Google Scholar] [CrossRef] [Green Version]
- Kilgore, K.P.; Lee, M.S.; Leavitt, J.A.; Mokri, B.; Hodge, D.O.; Frank, R.D.; Chen, J.J. Re-evaluating the Incidence of Idiopathic Intracranial Hypertension in an Era of Increasing Obesity. Ophthalmology 2017, 124, 697–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curry, W.T.; Butler, W.E.; Barker, F.G. Rapidly Rising Incidence of Cerebrospinal Fluid Shunting Procedures for Idiopathic Intracranial Hypertension in the United States, 1988–2002. Neurosurgery 2005, 57, 97–108. [Google Scholar] [CrossRef]
- Mollan, S.P.; Aguiar, M.; Evison, F.; Frew, E.; Sinclair, A.J. The expanding burden of idiopathic intracranial hypertension. Eye 2019, 33, 478–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sinclair, A.J.; Kuruvath, S.; Sen, D.; Nightingale, P.G.; Burdon, M.A.; Flint, G. Is cerebrospinal fluid shunting in idiopathic intracranial hypertension worthwhile? A 10-year review. Cephalalgia 2011, 31, 1627–1633. [Google Scholar] [CrossRef] [PubMed]
- Dandy, W.E. Intracranial pressure without brain tumor. Ann. Surg. 1937, 106, 492–513. [Google Scholar] [CrossRef] [PubMed]
- Quincke, H. Ueber Meningitis serosa und verwandte Zustände. J. Neurol. 1896, 9, 149–168. [Google Scholar] [CrossRef] [Green Version]
- Galgano, M.A.; Deshaies, E.M. An update on the management of pseudotumor cerebri. Clin. Neurol. Neurosurg. 2013, 115, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, K.; Thacker, A.K.; Bohlaga, N.H.; Maloo, J.C.; Gerryo, S.E. Epidemiology of idiopathic intracranial hypertension: A prospective and case-control study. J. Neurol. Sci. 1993, 116, 18–28. [Google Scholar] [CrossRef]
- Friedman, D.I.; Liu, G.T.; Digre, K.B. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 2013, 81, 1159–1165. [Google Scholar] [CrossRef] [PubMed]
- Mollan, S.P.; Davies, B.; Silver, N.C.; Shaw, S.; Mallucci, C.L.; Wakerley, B.R.; Krishnan, A.; Chavda, S.V.; Ramalingam, S.; Edwards, J.; et al. Idiopathic intracranial hypertension: Consensus guidelines on management. J. Neurol. Neurosurg. Psychiatry 2018, 89, 1088–1100. [Google Scholar] [CrossRef] [Green Version]
- Wall, M.; George, D. Idiopathic intracranial hypertension. A prospective study of 50 patients. Brain 1991, 114, 155–180. [Google Scholar]
- Sinclair, A.J.; Burdon, M.A.; Nightingale, P.G.; Ball, A.K.; Good, P.; Matthews, T.D.; Jacks, A.; Lawden, M.; Clarke, C.E.; Stewart, P.M.; et al. Low energy diet and intracranial pressure in women with idiopathic intracranial hypertension: Prospective cohort study. BMJ 2010, 341, c2701. [Google Scholar] [CrossRef] [Green Version]
- Mollan, S.P.; Ali, F.; Hassan-Smith, G.; Botfield, H.; Friedman, D.I.; Sinclair, A.J. Evolving evidence in adult idiopathic intracranial hypertension: Pathophysiology and management. J. Neurol. Neurosurg. Psychiatry 2016, 87, 982–992. [Google Scholar] [CrossRef]
- Wall, M. Idiopathic intracranial hypertension (Pseudotumor cerebri). Curr. Neurol. Neurosci. Rep. 2008, 8, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Giridharan, N.; Patel, S.K.; Ojugbeli, A.; Nouri, A.; Shirani, P.; Grossman, A.W.; Cheng, J.; Zuccarello, M.; Prestigiacomo, C.J. Understanding the complex pathophysiology of idiopathic intracranial hypertension and the evolving role of venous sinus stenting: A comprehensive review of the literature. Neurosurg. Focus 2018, 45, E10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalyvas, A.V.; Hughes, M.; Koutsarnakis, C.; Moris, D.; Liakos, F.; Sakas, D.E.; Stranjalis, G.; Fouyas, I. Efficacy, complications and cost of surgical interventions for idiopathic intracranial hypertension: A systematic review of the literature. Acta Neurochir. 2017, 159, 33–49. [Google Scholar] [CrossRef] [PubMed]
- Thurtell, M.J.; Bruce, B.B.; Newman, N.J.; Biousse, V. An update on idiopathic intracranial hypertension. Rev. Neurol. Dis. 2010, 7, e56–e68. [Google Scholar] [PubMed]
- Schirmer, C.M.; Hedges, T.R. Mechanisms of visual loss in papilledema. Neurosurg. Focus 2007, 23, E5. [Google Scholar] [CrossRef]
- Brazis, P.W. Clinical Review: The Surgical Treatment of Idiopathic Pseudotumour Cerebri (Idiopathic Intracranial Hypertension). Cephalalgia 2008, 28, 1361–1373. [Google Scholar] [CrossRef] [PubMed]
- Wall, M. Update on Idiopathic Intracranial Hypertension. Neurol. Clin. 2017, 35, 45–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thambisetty, M.; Lavin, P.J.; Newman, N.J.; Biousse, V. Fulminant idiopathic intracranial hypertension. Neurology 2007, 68, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Ball, A.K.; Howman, A.; Wheatley, K.; Burdon, M.A.; Matthews, T.; Jacks, A.S.; Lawden, M.; Sivaguru, A.; Furmston, A.; Howell, S.; et al. A randomised controlled trial of treatment for idiopathic intracranial hypertension. J. Neurol. 2010, 258, 874–881. [Google Scholar] [CrossRef]
- Kessler, L.A.; Novelli, P.M.; Reigel, D.H. Surgical Treatment of Benign Intracranial Hypertension—Subtemporal Decompression Revisited. Surg. Neurol. 1998, 50, 73–76. [Google Scholar] [CrossRef]
- Horrax, G. The Subtemporal Decompression: Present Day Indications and Technique. Surg. Clin. N. Am. 1956, 36, 555–566. [Google Scholar] [CrossRef]
- Buxton, N.; Punt, J. Subtemporal Decompression: The Treatment of Noncompliant Ventricle Syndrome. Neurosurgery 1999, 44, 513–518. [Google Scholar] [CrossRef]
- Mcgirt, M.J.; Woodworth, G.; Thomas, G.; Miller, N.; Williams, M.; Rigamonti, D. Cerebrospinal fluid shunt placement for pseudotumor cerebri—associated intractable headache: Predictors of treatment response and an analysis of long-term outcomes. J. Neurosurg. 2004, 101, 627–632. [Google Scholar] [CrossRef]
- Wang, V.Y.; Barbaro, N.M.; Lawton, M.T.; Pitts, L.; Kunwar, S.; Parsa, A.T.; Gupta, N.; McDermott, M.W. Complications of lumboperitoneal shunts. Neurosurgery 2007, 60, 1045–1049. [Google Scholar] [CrossRef]
- Menger, R.P.; Connor, D.E.; Thakur, J.D.; Sonig, A.; Smith, E.; Guthikonda, B.; Nanda, A. A comparison of lumboperitoneal and ventriculoperitoneal shunting for idiopathic intracranial hypertension: An analysis of economic impact and complications using the Nationwide Inpatient Sample. Neurosurg. Focus 2014, 37, E4. [Google Scholar] [CrossRef] [Green Version]
- Abubaker, K.; Ali, Z.; Raza, K.; Bolger, C.; Rawluk, D.; O’Brien, D. Idiopathic intracranial hypertension: Lumboperitoneal shunts versus ventriculoperitoneal shunts—Case series and literature review. Br. J. Neurosurg. 2011, 25, 94–99. [Google Scholar] [CrossRef]
- Alkosha, H.M.; Zidan, A.S. Role of Lumbopleural Shunt in Management of Idiopathic Intracranial Hypertension. World Neurosurg. 2016, 88, 113–118. [Google Scholar] [CrossRef]
- Burgett, R.A.; Purvin, V.A.; Kawasaki, A. Lumboperitoneal shunting for pseudotumor cerebri. Neurology 1997, 49, 734–739. [Google Scholar] [CrossRef] [PubMed]
- Eggenberger, E.R.; Miller, N.R.; Vitale, S. Lumboperitoneal shunt for the treatment of pseudotumor cerebri. Neurology 1996, 46, 1524–1530. [Google Scholar] [CrossRef]
- Yadav, Y.R.; Parihar, V.; Agarwal, M.; Bhatele, P.R.; Saxena, N. Lumbar peritoneal shunt in idiopathic intra cranial hypertension. Turk. Neurosurg. 2011, 22, 21–26. [Google Scholar] [CrossRef]
- Karabatsou, K.; Quigley, G.; Buxton, N.; Foy, P.; Mallucci, C. Lumboperitoneal shunts: Are the complications acceptable? Acta Neurochir. 2004, 146, 1193–1197. [Google Scholar] [CrossRef]
- Bynke, G.; Zemack, G.; Bynke, H.; Romner, B. Ventriculoperitoneal shunting for idiopathic intracranial hypertension. Neurology 2004, 63, 1314–1316. [Google Scholar] [CrossRef] [PubMed]
- Tarnaris, A.; Toma, A.K.; Watkins, L.D.; Kitchen, N.D. Is there a difference in outcomes of patients with idiopathic intracranial hypertension with the choice of cerebrospinal fluid diversion site: A single centre experience. Clin. Neurol. Neurosurg. 2011, 113, 477–479. [Google Scholar] [CrossRef]
- Hickman, S.J.; Raoof, N.; Panesar, H.; McMullan, J.M.; Pepper, I.M.; Sharrack, B. Visual Outcomes from Shunting for Idiopathic Intracranial Hypertension. Neuroophthalmology 2014, 38, 310–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bjornson, A.; Tapply, I.; Nabbanja, E.; Lalou, A.-D.; Czosnyka, M.; Czosnyka, Z.; Muthusamy, B.; Garnett, M. Ventriculo-peritoneal shunting is a safe and effective treatment for idiopathic intracranial hypertension. Br. J. Neurosurg. 2019, 33, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.O.; Garrity, J.A.; Meyer, F.B. Refractory idiopathic intracranial hypertension treated with stereotactically planned ventriculoperitoneal shunt placement. Neurosurg. Focus 2001, 10, 1–4. [Google Scholar] [CrossRef]
- Abu-Serieh, B.; Ghassempour, K.; Duprez, T.; Raftopoulos, C. Stereotactic ventriculoperitoneal shunting for refractory idiopathic intracranial hypertension. Neurosurgery 2007, 60, 1039–1044. [Google Scholar] [CrossRef]
- Woodworth, G.F.; McGirt, M.J.; Elfert, P.; Sciubba, D.M.; Rigamonti, D. Frameless Stereotactic Ventricular Shunt Placement for Idiopathic Intracranial Hypertension. Ster. Funct. Neurosurg. 2005, 83, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Mallucci, C.L.; Jenkinson, M.D.; Conroy, E.J.; Hartley, J.C.; Brown, M.; Dalton, J.; Kearns, T.; Moitt, T.; Griffiths, M.J.; Culeddu, G.; et al. Antibiotic or silver versus standard ventriculoperitoneal shunts (BASICS): A multicentre, single-blinded, randomised trial and economic evaluation. Lancet 2019, 394, 1530–1539. [Google Scholar] [CrossRef] [Green Version]
- Kandasamy, J.; Hayhurst, C.; Clark, S.; Jenkinson, M.D.; Byrne, P.; Karabatsou, K.; Mallucci, C.L. Electromagnetic Stereotactic Ventriculoperitoneal CSF Shunting for Idiopathic Intracranial Hypertension: A Successful Step Forward? World Neurosurg. 2011, 75, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Tulipan, N.; Lavin, P.J.; Copeland, M. Stereotactic ventriculoperitoneal shunt for idiopathic intracranial hypertension: Technical note. Neurosurgery 1998, 43, 175–176. [Google Scholar] [CrossRef]
- Hayhurst, C.; Beems, T.; Jenkinson, M.D.; Byrne, P.; Clark, S.; Kandasamy, J.; Goodden, J.; Tewarie, R.D.N.; Mallucci, C.L. Effect of electromagnetic-navigated shunt placement on failure rates: A prospective multicenter study. J. Neurosurg. 2010, 113, 1273–1278. [Google Scholar] [CrossRef] [Green Version]
- Khan, N.R.; Decuypere, M.; Vaughn, B.N.; Klimo, P. Image Guidance for Ventricular Shunt Surgery: An Analysis of Ventricular Size and Proximal Revision Rates. Neurosurgery 2018, 84, 624–635. [Google Scholar] [CrossRef] [PubMed]
- Sampath, R.; Wadhwa, R.; Tawfik, T.; Nanda, A.; Guthikonda, B. Stereotactic Placement of Ventricular Catheters: Does It Affect Proximal Malfunction Rates. Ster. Funct. Neurosurg. 2012, 90, 97–103. [Google Scholar] [CrossRef]
- Hayhurst, C.; Byrne, P.; Eldridge, P.R.; Mallucci, C.L. Application of electromagnetic technology to neuronavigation: A revolution in image-guided neurosurgery. J. Neurosurg. 2009, 111, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Paff, M.; Alexandru-Abrams, D.; Muhonen, M.; Loudon, W. Ventriculoperitoneal shunt complications: A review. Interdiscip. Neurosurg. 2018, 13, 66–70. [Google Scholar] [CrossRef]
- Merkler, A.E.; Ch’Ang, J.; Parker, W.E.; Murthy, S.B.; Kamel, H. The Rate of Complications after Ventriculoperitoneal Shunt Surgery. World Neurosurg. 2017, 98, 654–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padmanabhan, R.; Crompton, D.; Burn, D.; Birchall, D. Acquired Chiari 1 malformation and syringomyelia following lumboperitoneal shunting for pseudotumour cerebri. J. Neurol. Neurosurg. Psychiatry 2005, 76, 298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bari, M.E.; Khan, F.; Rehman, A.; Shamim, M.S. Factors affecting ventriculoperitoneal shunt survival in adult patients. Surg. Neurol. Int. 2015, 6, 25. [Google Scholar] [CrossRef]
- Wu, M.Y.; Green, B.N.L.; Wrensch, P.M.R.; Zhao, M.S.; Gupta, M.N. Ventriculoperitoneal shunt complications in california. Neurosurgery 2007, 61, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Reddy, G.K.; Bollam, P.; Caldito, G. Long-Term Outcomes of Ventriculoperitoneal Shunt Surgery in Patients with Hydrocephalus. World Neurosurg. 2014, 81, 404–410. [Google Scholar] [CrossRef]
- Craven, C.L.; Pradini-Santos, L.; Goel, A.; Thorne, L.; Watkins, L.D.; Toma, A.K. Approach to Slitlike Ventricles: Parietal-Occipital versus Frontal Burr Catheter Entry Sites. World Neurosurg. 2020, 135, e447–e451. [Google Scholar] [CrossRef]
- Gutowski, P.; Gölz, L.; Rot, S.; Lemcke, J.; Thomale, U.-W. Gravitational shunt valves in hydrocephalus to challenge the sequelae of over-drainage. Expert Rev. Med. Devices 2020, 17, 1155–1168. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.J.; Dillon, W.P.; Chin, C.T.; McDermott, M.W.; Horton, J.C. Intracranial hypotension caused by leakage of cerebrospinal fluid from the thecal sac after lumboperitoneal shunt placement. J. Neurosurg. 2007, 107, 173–177. [Google Scholar] [CrossRef] [Green Version]
- Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [CrossRef]
- Paldino, M.; Mogilner, A.Y.; Tenner, M.S. Intracranial hypotension syndrome: A comprehensive review. Neurosurg. Focus 2003, 15, 1–8. [Google Scholar] [CrossRef]
- Koerner, J.C.; Friedman, D.I. Inpatient and Emergency Service Utilization in Patients With Idiopathic Intracranial Hypertension. J. Neuro-Ophthalmol. 2014, 34, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Liu, A.; Elder, B.D.; Sankey, E.W.; Goodwin, C.R.; Jusué-Torres, I.; Rigamonti, D. The Utility of Computed Tomography in Shunted Patients with Idiopathic Intracranial Hypertension Presenting to the Emergency Department. World Neurosurg. 2015, 84, 1852–1856. [Google Scholar] [CrossRef]
- Liu, A.; Elder, B.D.; Sankey, E.W.; Goodwin, C.R.; Jusué-Torres, I.; Rigamonti, D. Are shunt series and shunt patency studies useful in patients with shunted idiopathic intracranial hypertension in the emergency department? Clin. Neurol. Neurosurg. 2015, 138, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Aschoff, A.; Kremer, P.; Hashemi, B.; Kunze, S. The scientific history of hydrocephalus and its treatment. Neurosurg. Rev. 1999, 22, 67–93. [Google Scholar] [CrossRef]
- Aschoff, A. In-Depth View: Functional Characteristics of CSF Shunt Devices (Pros and Cons). In Textbook of Pediatric Neuro-surgery; Di Rocco, C., Pang, D., Rutka, J.T., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 1–40. [Google Scholar] [CrossRef]
- Mallucci, C.; Sgouros, S. Cerebrospinal Fluid Disorders; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Wetzel, C.; Goertz, L.; Noé, P.; Von Spreckelsen, N.; Penner, M.; Kabbasch, C.; Goldbrunner, R.; Krischek, B. Flow-regulated versus differential pressure valves for idiopathic normal pressure hydrocephalus: Comparison of overdrainage rates and neurological outcome. Acta Neurochir. 2019, 162, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Ulivieri, S.; Oliveri, G.; Georgantzinou, M.; Fruschelli, M.; Motolese, P.; Menicacci, F.; Motolese, I.; Motelese, E. Long-term effectiveness of lumboperitoneal flow-regulated shunt system for idiopathic intracranial hypertension. J. Neurosurg. Sci. 2009, 53, 107–111. [Google Scholar]
- Zemack, G.; Romner, B. Seven-year clinical experience with the Codman Hakim programmable valve: A retrospective study of 583 patients. Neurosurg. Focus 1999, 7, E10. [Google Scholar] [CrossRef] [Green Version]
- Toma, A.K.; Dherijha, M.; Kitchen, N.D.; Watkins, L.D. Use of lumboperitoneal shunts with the Strata NSC valve: A single-center experience. J. Neurosurg. 2010, 113, 1304–1308. [Google Scholar] [CrossRef] [PubMed]
- Nadkarni, T.D.; Rekate, H.L.; Wallace, D. Concurrent use of a lumboperitoneal shunt with programmable valve and ventricular access device in the treatment of pseudotumor cerebri: Review of 40 cases. J. Neurosurg. Pediatr. 2008, 2, 19–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petersen, L.G.; Petersen, J.C.G.; Andresen, M.; Secher, N.H.; Juhler, M. Postural influence on intracranial and cerebral perfusion pressure in ambulatory neurosurgical patients. Am. J. Physiol. Integr. Comp. Physiol. 2016, 310, R100–R104. [Google Scholar] [CrossRef] [PubMed]
- Kurtom, K.H.; Magram, G. Siphon regulatory devices: Their role in the treatment of hydrocephalus. Neurosurg. Focus 2007, 22, 1–8. [Google Scholar] [CrossRef]
- Freimann, F.B.; Kimura, T.; Stockhammer, F.; Schulz, M.; Rohde, V.; Thomale, U.-W. In vitro performance and principles of anti-siphoning devices. Acta Neurochir. 2014, 156, 2191–2199. [Google Scholar] [CrossRef] [PubMed]
- Gehlen, M.; Eklund, A.; Kurtcuoglu, V.; Malm, J.; Daners, M.S. Comparison of anti-siphon devices—how do they affect CSF dynamics in supine and upright posture? Acta Neurochir. 2017, 159, 1389–1397. [Google Scholar] [CrossRef]
- Azad, T.D.; Zhang, Y.; Varshneya, K.; Veeravagu, A.; Ratliff, J.K.; Li, G. Lumboperitoneal and Ventriculoperitoneal Shunting for Idiopathic Intracranial Hypertension Demonstrate Comparable Failure and Complication Rates. Neurosurgery 2019, 86, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Wang, Z.; Liu, F.; Tan, G.; Zhu, H.; Chen, D. Programmable shunt valves for the treatment of hydrocephalus: A systematic review. Eur. J. Paediatr. Neurol. 2013, 17, 454–461. [Google Scholar] [CrossRef]
- Omidbeigi, M.; Mousavi, M.-S.; Meknatkhah, S.; Edalatfar, M.; Bari, A.; Sharif-Alhoseini, M. Telemetric Intracranial Pressure Monitoring: A Systematic Review. Neurocrit. Care 2021, 34, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Banta, J.T.; Farris, B.K. Pseudotumor cerebri and optic nerve sheath decompression. Ophthalmology 2000, 107, 1907–1912. [Google Scholar] [CrossRef]
- Scherman, D.B.; Dmytriw, A.A.; Nguyen, G.T.; Nguyen, N.T.; Tchantchaleishvili, N.; Maingard, J.; Asadi, H.; Brooks, M.; Griessenauer, C.; Ogilvy, C.; et al. Shunting, optic nerve sheath fenestration and dural venous stenting for medically re-fractory idiopathic intracranial hypertension: Systematic review and meta-analysis. Ann. Eye Sci. 2018, 3, 26. [Google Scholar] [CrossRef]



| Factors |
|---|
| Differential pressure vs. flow regulation |
| Fixed vs. programmable valves |
| Anti-siphon and programmable anti-siphon devices |
| Gravity assisted valves |
| Idiopathic Intracranial Hypertension | Other Aetiologies | |
|---|---|---|
| Total n | 88 | 512 |
| Female n(%) | 78 (88.6) | 271 (52.9) |
| Median Age (IQR) | 31.2 (25.4–37) | 44.6 (26.6–56.3) |
| Total Revisions n(%) | 29 (32.9) | 121 (23.6) |
| Programmable Valve n(%) | 39 (44.3) | 174 (34) |
| Anti-Siphon Device n(%) | 31 (35.2) | 139 (27.1) |
| Revision | Mechanical Failure | Infection | Revision | Mechanical Failure | Infection | |
|---|---|---|---|---|---|---|
| Total n (%) | 29 (32.9) | 24 (27.3) | 5 (5.7) | 121 (23.6) | 101 (19.7) | 20 (3.9) |
| Programmable Valve | ||||||
| Yes n (%) | 11 (28.2) | 10 (25.6) | 1 (2.6) | 35 (20.1) | 30 (17.2) | 5 (2.9) |
| No n (%) | 18 (36.7) | 14 (28.5) | 4 (8.1) | 86 (25.4) | 71 (21.0) | 15 (4.4) |
| Anti-Siphon Device | ||||||
| Yes n (%) | 9 (29.0) | 6 (19.4) | 3 (9.7) | 28 (20.1) | 22 (15.8) | 6 (4.3) |
| No n (%) | 20 (35.0) | 18 (31.6) | 2 (3.5) | 93 (24.9) | 79 (21.2) | 14 (3.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sunderland, G.J.; Jenkinson, M.D.; Conroy, E.J.; Gamble, C.; Mallucci, C.L. Neurosurgical CSF Diversion in Idiopathic Intracranial Hypertension: A Narrative Review. Life 2021, 11, 393. https://doi.org/10.3390/life11050393
Sunderland GJ, Jenkinson MD, Conroy EJ, Gamble C, Mallucci CL. Neurosurgical CSF Diversion in Idiopathic Intracranial Hypertension: A Narrative Review. Life. 2021; 11(5):393. https://doi.org/10.3390/life11050393
Chicago/Turabian StyleSunderland, Geraint J., Michael D. Jenkinson, Elizabeth J. Conroy, Carrol Gamble, and Conor L. Mallucci. 2021. "Neurosurgical CSF Diversion in Idiopathic Intracranial Hypertension: A Narrative Review" Life 11, no. 5: 393. https://doi.org/10.3390/life11050393
APA StyleSunderland, G. J., Jenkinson, M. D., Conroy, E. J., Gamble, C., & Mallucci, C. L. (2021). Neurosurgical CSF Diversion in Idiopathic Intracranial Hypertension: A Narrative Review. Life, 11(5), 393. https://doi.org/10.3390/life11050393





