Is Preterm Birth a Risk Factor for Subsequent Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder in Children with Febrile Seizure?—A Retrospective Study
Abstract
:1. Introduction
2. Methods and Approach
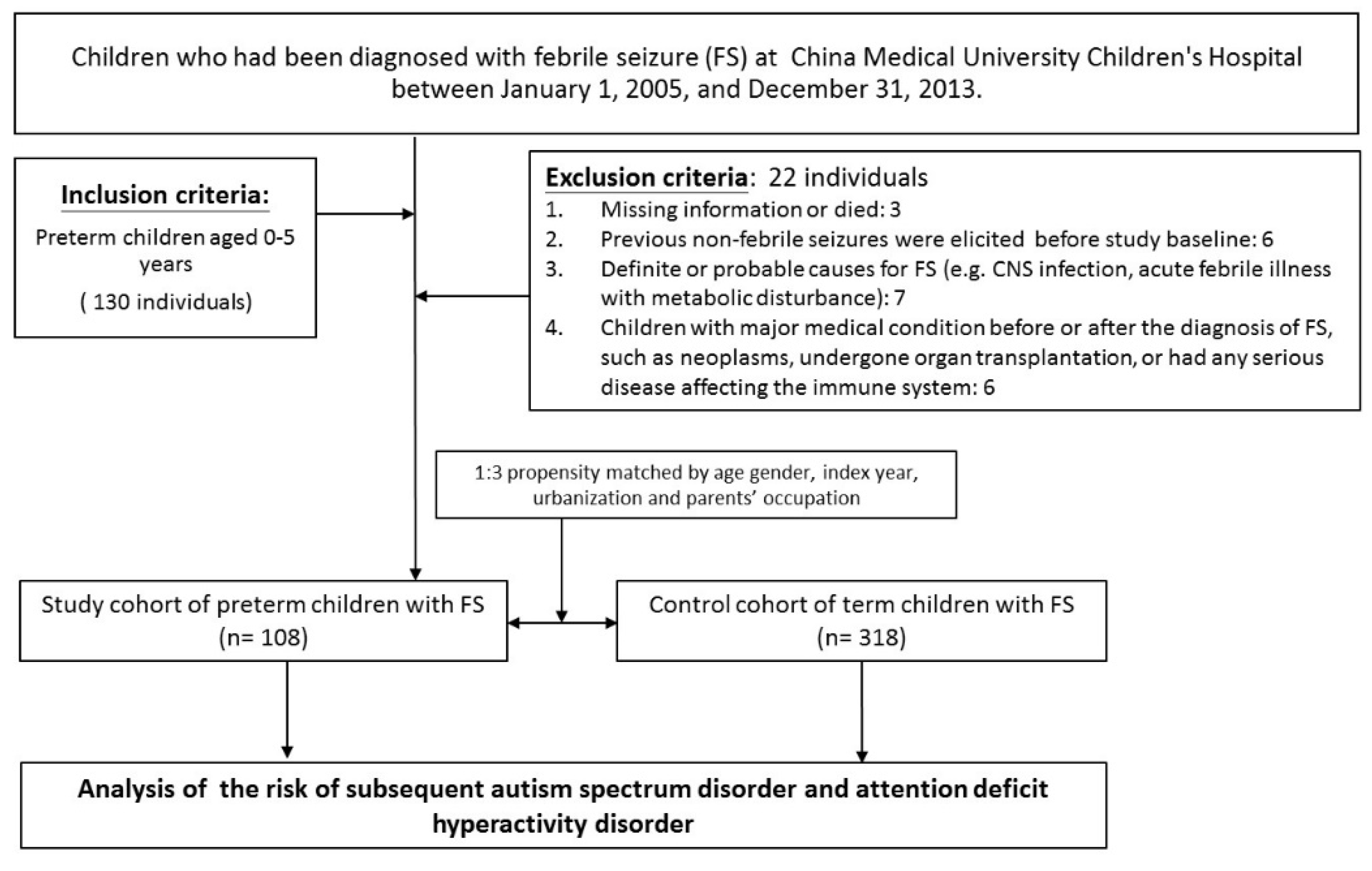
Patient Population
3. Statistical Analysis
4. Results
Data Analysis
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADHD | Attention Deficit Hyperactivity Disorder |
| ASD | Autism Spectrum Disorder |
| CI | Confidence Interval |
| DSM | Diagnostic and Statistical Manual of Mental Disorders |
| FS | Febrile Seizure |
| MR | Mental Retardation |
| NDDs | Neurodevelopmental Disorders |
| OR | Odds Ratio |
| TS | Tourette Syndrome |
References
- Lung, F.-W.; Chiang, T.-L.; Lin, S.-J.; Lee, M.-C.; Shu, B.-C. Advanced Maternal Age and Maternal Education Disparity in Children with Autism Spectrum Disorder. Matern. Child. Health J. 2018, 22, 941–949. [Google Scholar] [CrossRef]
- Janecka, M.; Hansen, S.N.; Modabbernia, A.; Browne, H.A.; Buxbaum, J.; Schendel, D.E.; Reichenberg, A.; Parner, E.; Grice, D.E. Parental Age and Differential Estimates of Risk for Neuropsychiatric Disorders: Findings from the Danish Birth Cohort. J. Am. Acad. Child. Adolesc. Psychiatry 2019, 58, 618–627. [Google Scholar] [CrossRef] [PubMed]
- Russell, A.E.; Ford, T.; Williams, R.; Russell, G. The Association Between Socioeconomic Disadvantage and Attention Deficit/Hyperactivity Disorder (ADHD): A Systematic Review. Child. Psychiatry Hum. Dev. 2015, 47, 440–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durkin, M.S.; Yeargin-Allsopp, M. Socioeconomic Status and Pediatric Neurologic Disorders: Current Evidence. Semin. Pediatr. Neurol. 2018, 27, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Wang, Y.; Zhang, L.; Zheng, Z.; Zhu, T.; Qu, Y.; Mu, D. Maternal Smoking and Attention-Deficit/Hyperactivity Disorder in Offspring: A Meta-analysis. Pediatrics 2017, 141, e20172465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, Y.; Lee, A.M.; McKee, S.A.; Picciotto, M.R. Maternal smoking and autism spectrum disorder: Meta-analysis with population smoking metrics as moderators. Sci. Rep. 2017, 7, 1–10. [Google Scholar] [CrossRef]
- Hagan, J.F.; Balachova, T.; Bertrand, J.; Chasnoff, I.; Dang, E.; Fernandez-Baca, D.; Kable, J.; Kosofsky, B.; Senturias, Y.N.; Singh, N.; et al. Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure. Pediatrics 2016, 138, e20151553. [Google Scholar] [CrossRef] [Green Version]
- Vestergaard, M.; Pedersen, M.G.; Østergaard, J.R.; Pedersen, C.B.; Olsen, J.; Christensen, J. Death in children with febrile seizures: A population-based cohort study. Lancet 2008, 372, 457–463. [Google Scholar] [CrossRef]
- Vestergaard, M.; Pedersen, C.B.; Sidenius, P.; Olsen, J.; Christensen, J. The Long-Term Risk of Epilepsy after Febrile Seizures in Susceptible Subgroups. Am. J. Epidemiol. 2007, 165, 911–918. [Google Scholar] [CrossRef] [Green Version]
- Gillberg, C.; Lundström, S.; Fernell, E.; Nilsson, G.; Neville, B. Febrile Seizures and Epilepsy: Association with Autism and Other Neurodevelopmental Disorders in the Child and Adolescent Twin Study in Sweden. Pediatr. Neurol. 2017, 74, 80–86.e2. [Google Scholar] [CrossRef] [Green Version]
- Baumann, R.J.; Duffner, P.K. Treatment of children with simple febrile seizures: The aap practice parameter. Pediatr. Neurol. 2000, 23, 11–17. [Google Scholar] [CrossRef]
- Ku, Y.-C.; Muo, C.-H.; Ku, C.-S.; Chen, C.-H.; Lee, W.-Y.; Shen, E.-Y.; Chang, Y.-J.; Kao, C.-H. Risk of subsequent attention deficit-hyperactivity disorder in children with febrile seizures. Arch. Dis. Child. 2013, 99, 322–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertelsen, E.N.; Larsen, J.T.; Petersen, L.V.; Christensen, J.; Dalsgaard, S. Childhood Epilepsy, Febrile Seizures, and Subsequent Risk of ADHD. Pediatrics 2016, 138, e20154654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarjour, I.T. Neurodevelopmental Outcome After Extreme Prematurity: A Review of the Literature. Pediatr. Neurol. 2015, 52, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Ask, H.; Gustavson, K.; Ystrom, E.; Havdahl, A.; Tesli, M.; Askeland, R.B.; Reichborn-Kjennerud, T. Association of Gestational Age at Birth with Symptoms of Attention-Deficit/Hyperactivity Disorder in Children. JAMA Pediatr. 2018, 172, 749–756. [Google Scholar] [CrossRef]
- Sucksdorff, M.; Lehtonen, L.; Chudal, R.; Suominen, A.; Joelsson, P.; Gissler, M.; Sourander, A. Preterm Birth and Poor Fetal Growth as Risk Factors of Attention-Deficit/Hyperactivity Disorder. Pediatrics 2015, 136, e599–e608. [Google Scholar] [CrossRef] [Green Version]
- Pourhoseingholi, M.A.; Baghestani, A.; Vahedi, M. How to control confounding effects by statistical analysis. Gastroenterol. Hepatol. Bed Bench 2012, 5, 79–83. [Google Scholar] [PubMed]
- Pavlidou, E.; Panteliadis, C. Prognostic factors for subsequent epilepsy in children with febrile seizures. Epilepsia 2013, 54, 2101–2107. [Google Scholar] [CrossRef] [PubMed]
- Dreier, J.W.; Li, J.; Sun, Y.; Christensen, J. Evaluation of Long-term Risk of Epilepsy, Psychiatric Disorders, and Mortality Among Children with Recurrent Febrile Seizures. JAMA Pediatr. 2019, 173, 1164–1170. [Google Scholar] [CrossRef]
- Gencpinar, P.; Yavuz, H.; Bozkurt, Ö.; Haspolat, Ş.; Duman, Ö. The risk of subsequent epilepsy in children with febrile seizure after 5 years of age. Seizure 2017, 53, 62–65. [Google Scholar] [CrossRef] [Green Version]
- Chiang, L.-M.; Huang, G.-S.; Sun, C.-C.; Hsiao, Y.-L.; Hui, C.K.; Hu, M.-H. Association of developing childhood epilepsy subsequent to febrile seizure: A population-based cohort study. Brain Dev. 2018, 40, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.K.; Hon, K.L.; Leung, T.N. Febrile seizures: An overview. Drugs Context 2018, 7, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Salehi, B.; Yousefichaijan, P.; Arian, S.S.; Ebrahimi, S.; Naziri, M. Comparison of Relation between Attention Deficit Hyperactivity Disorder in Children with and without Simple Febrile Seizure Admitted in Arak Central Iran. Iran. J. Child Neurol. 2016, 10, 56–61. [Google Scholar]
- Chang, Y.-C.; Guo, N.-W.; Huang, C.-C.; Wang, S.-T.; Tsai, J.-J. Neurocognitive attention and behavior outcome of school-age children with a history of febrile convulsions: A population study. Epilepsia 2000, 41, 412–420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Besag, F.M. Current controversies in the relationships between autism and epilepsy. Epilepsy Behav. 2015, 47, 143–146. [Google Scholar] [CrossRef]
- Kanner, A.M.; Scharfman, H.; Jette, N.; Anagnostou, E.; Bernard, C.; Camfield, C.; Camfield, P.; Legg, K.; Dinstein, I.; Giacobbe, P.; et al. Epilepsy as a Network Disorder (1): What can we learn from other network disorders such as autistic spectrum disorder and mood disorders? Epilepsy Behav. 2017, 77, 106–113. [Google Scholar] [CrossRef]
- Richard, A.E.; Scheffer, I.E.; Wilson, S.J. Features of the broader autism phenotype in people with epilepsy support shared mechanisms between epilepsy and autism spectrum disorder. Neurosci. Biobehav. Rev. 2017, 75, 203–233. [Google Scholar] [CrossRef] [Green Version]
- Keller, R.; Basta, R.; Salerno, L.; Elia, M. Autism, epilepsy, and synaptopathies: A not rare association. Neurol. Sci. 2017, 38, 1353–1361. [Google Scholar] [CrossRef]
- McCue, L.M.; Flick, L.H.; Twyman, K.A.; Xian, H.; Conturo, T.E. Prevalence of non-febrile seizures in children with idiopathic autism spectrum disorder and their unaffected siblings: A retrospective cohort study. BMC Neurol. 2016, 16, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Peralta-Carcelen, M.; Schwartz, J.; Carcelen, A.C. Behavioral and Socioemotional Development in Preterm Children. Clin. Perinatol. 2018, 45, 529–546. [Google Scholar] [CrossRef]
- Arora, N.K.; Nair, M.K.C.; Gulati, S.; Deshmukh, V.; Mohapatra, A.; Mishra, D.; Patel, V.; Pandey, R.M.; Das, B.C.; Divan, G.; et al. Neurodevelopmental disorders in children aged 2–9 years: Population-based burden estimates across five regions in India. PLoS Med. 2018, 15, e1002615. [Google Scholar] [CrossRef] [PubMed]
- El-Dib, M.; Massaro, A.N.; Glass, P.; Aly, H. Neurodevelopmental assessment of the newborn: An opportunity for prediction of outcome. Brain Dev. 2011, 33, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Vieira, M.E.B.; Linhares, M.B.M. Developmental outcomes and quality of life in children born preterm at preschool- and school-age. J. Pediatr. 2011, 87, 281–291. [Google Scholar] [CrossRef] [Green Version]
- Rogers, C.E.; Lean, R.E.; Wheelock, M.D.; Smyser, C.D. Aberrant structural and functional connectivity and neurodevelopmental impairment in preterm children. J. Neurodev. Disord. 2018, 10, 38. [Google Scholar] [CrossRef] [PubMed]
- Moster, D.; Lie, R.T.; Markestad, T. Long-Term Medical and Social Consequences of Preterm Birth. N. Engl. J. Med. 2008, 359, 262–273. [Google Scholar] [CrossRef] [Green Version]
- Fezer, G.F.; Matos, M.B.; Nau, A.L.; Zeigelboim, B.S.; Marques, J.M.; Liberalesso, P.B.N. Perinatal Features of Children with Autism Spectrum Disorder. Rev. Paul. Pediatr. 2017, 35, 2. [Google Scholar] [CrossRef] [Green Version]
- Kuzniewicz, M.W.; Wi, S.; Qian, Y.; Walsh, E.M.; Armstrong, M.A.; Croen, L.A. Prevalence and Neonatal Factors Associated with Autism Spectrum Disorders in Preterm Infants. J. Pediatr. 2014, 164, 20–25. [Google Scholar] [CrossRef]
- Lubsen, J.; Vohr, B.; Myers, E.; Hampson, M.; Lacadie, C.; Schneider, K.C.; Katz, K.H.; Constable, R.; Ment, L.R. Microstructural and Functional Connectivity in the Developing Preterm Brain. Semin. Perinatol. 2011, 35, 34–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feenstra, B.; Pasternak, B.; Geller, F.; Carstensen, L.; Wang, T.-F.; Huang, H.; Eitson, J.L.; Hollegaard, M.V.; Svanström, H.; Vestergaard, M. Common variants associated with general and MMR vaccine–related febrile seizures. Nat. Genet. 2014, 46, 1274–1282. [Google Scholar] [CrossRef] [Green Version]
- Fry, A.E.; Rees, E.; Thompson, R.; Mantripragada, K.; Blake, P.; Jones, G.; Morgan, S.; Jose, S.; Mugalaasi, H.; Archer, H.; et al. Pathogenic copy number variants and SCN1A mutations in patients with intellectual disability and childhood-onset epilepsy. BMC Med. Genet. 2016, 17, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Papp-Hertelendi, R.; Tényi, T.; Hadzsiev, K.; Hau, L.; Benyus, Z.; Csábi, G. First report on the association of SCN1A mutation, childhood schizophrenia and autism spectrum disorder without epilepsy. Psychiatry Res. 2018, 270, 1175–1176. [Google Scholar] [CrossRef] [PubMed]
- Rubinstein, M.; Patowary, A.; Stanaway, I.B.; McCord, E.; Nesbitt, R.R.; Archer, M.; Scheuer, T.; Nickerson, D.; Raskind, W.H.; Wijsman, E.M.; et al. Association of rare missense variants in the second intracellular loop of NaV1.7 sodium channels with familial autism. Mol. Psychiatry 2016, 23, 231–239. [Google Scholar] [CrossRef] [Green Version]
- Tang, L.; Lu, X.; Tao, Y.; Zheng, J.; Zhao, P.; Li, K.; Li, L. SCN1A rs3812718 polymorphism and susceptibility to epilepsy with febrile seizures: A meta-analysis. Gene 2014, 533, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Audenaert, D.; Claes, L.; Ceulemans, B.; Lofgren, A.; Van Broeckhoven, C.; De Jonghe, P. A deletion in SCN1B is associated with febrile seizures and early-onset absence epilepsy. Neurology 2003, 61, 854–856. [Google Scholar] [CrossRef] [PubMed]

| Demographic and Clinical Characteristics | Group | ||
|---|---|---|---|
| FS+/Preterm+ (n = 108) | FS+/Preterm− (n = 318) | p | |
| Mean 1st FS onset age (yrs) (SD) * | 2.30 (1.14) | 2.19 (1.10) | 0.62 |
| Gender (%) | 0.99 | ||
| Male | 72 (66.7) | 212 (66.7) | |
| Female | 36 (33.3) | 106 (33.3) | |
| GA (mean) (SD) * | 29.9 (6.00) | 38.4 (1.07) | <0.001 |
| BBW (gm) (SD) * | 1420 (591) | 3053 (395) | <0.001 |
| Stratified by age (yrs) (%) | 0.86 | ||
| 0–1 | 30 (27.8) | 93 (29.3) | |
| 1–5 | 78 (72.2) | 225 (70.7) | |
| Mean 1st FS duration (mins) (SD) * | 8.69 (10.05) | 5.81 (5.58) | 0.03 |
| No. of FS (SD) | 1.44 (0.65) | 1.35 (0.62) | 0.47 |
| Brain condition within 6 months of age (%) | <0.001 | ||
| Negative | 45 (41.6) | 312 | |
| IVH | 45 (41.6) | - | |
| HCP or VM | 6 (5.5) | 6 | |
| WM or PVL | 12 (11.1) | - | |
| Others (HCC, microcephaly) | 6 (5.5) | - | |
| Neurodevelopmental disabilities (%) | <0.001 | ||
| Epilepsy | 12 (11.1) | 15 (4.71) | |
| ASD | 15 (13.8) | 3 (0.94) | |
| ADHD | 30 (27.7) | 18 (5.66) | |
| Group | Epilepsy | ADHD | ASD | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Event (No.) | IR (%, N) | OR (95% CI) | Event (No.) | IR (%, N) | OR (95% CI) | Event (No.) | IR (%, N) | OR (95% CI) | |
| Term children with FS (N = 318) | 15 | 4.71 | Reference | 18 | 5.66 | Reference | 3 | 0.94 | Reference |
| Age (yrs, n) | |||||||||
| 0–1 (93) | 3 | 0.94 | Reference | 6 | 1.88 | Reference | 1 | 0.31 | Reference |
| 1–5 (225) | 12 | 3.77 | Reference | 12 | 3.77 | Reference | 2 | 0.62 | Reference |
| No of FS | |||||||||
| 1 (225) | 0 | 0 | - | 15 | 4.71 | Reference | 1 | 0.31 | Reference |
| >1 (93) | 15 | 4.71 | Reference | 3 | 0.94 | Reference | 2 | 0.62 | Reference |
| Preterm children with FS (N = 108) | 12 | 11.1 | 2.52 (1.14, 5.58) * | 30 | 27 | 6.41 (3.39, 12.09) *** | 15 | 13.9 | 16.9 (4.79, 59.7) *** |
| Age (yrs, n) | |||||||||
| 0–1 (30) | 3 | 2.77 | 3.33 (0.63, 17.4) | 6 | 5.54 | 3.62 (1.07, 12.2) * | 3 | 2.77 | 10.22 (1.02,102.3) * |
| 1–5 (78) | 9 | 8.33 | 2.31 (0.93, 5.72) | 24 | 22.2 | 7.88 (3.70, 16.7) *** | 12 | 11.1 | 20.27 (4.4,92.8) *** |
| No of FS | |||||||||
| 1 (27) | 3 | 2.77 | - | 15 | 13.9 | 17.5 (6.95, 44.0) *** | 6 | 5.55 | 64.0 (7.35, 557) *** |
| >1 (81) | 9 | 8.33 | 0.65 (0.26, 1.57) | 15 | 13.9 | 6.81 (1.89, 24.5) ** | 9 | 8.33 | 5.68 (1.19, 27.1) * |
| FS+/Preterm+ (n = 108) | ASD | ADHD | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
Sex  | ||||
| F | 0 | 0.99 | 2.50 (0.43, 14.23) | 0.30 |
GA (wks)  | ||||
| 30–35 | 1.11 (0.07, 15.5) | 0.9 | 0.37 (0.04, 2.99) | 0.35 |
| <30 | 0.58 (0.04, 7.91) | 0.68 | 0.26 (0.03, 1.86) | 0.18 |
Brain condition  | ||||
| Abnormal | 1.14 (0.16, 7.89) | 0.88 | 0.67 (0.15, 2.91) | 0.59 |
No. of FS  | ||||
| >1 | 3.15 (0.45, 21.94) | 0.24 | 2.25 (0.5, 10.01) | 0.28 |
1st FS duration (mins)  | ||||
| >10 | 1.04 (0.09,11.09) | 0.97 | 0.37 (0.03, 3.54) | 0.38 |
SGA  | ||||
| Yes | 0 | 0.99 | 2.35 (0.42, 13.18) | 0.33 |
 Reference for sex (male), GA (35–37 weeks); brain condition at birth (normal); number of FSs (1); first FS duration (1–10 min); SGA (No).
Reference for sex (male), GA (35–37 weeks); brain condition at birth (normal); number of FSs (1); first FS duration (1–10 min); SGA (No).Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-H.; Lin, W.-D.; Chou, I.-C.; Lee, I.-C.; Hong, S.-Y. Is Preterm Birth a Risk Factor for Subsequent Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder in Children with Febrile Seizure?—A Retrospective Study. Life 2021, 11, 854. https://doi.org/10.3390/life11080854
Lin C-H, Lin W-D, Chou I-C, Lee I-C, Hong S-Y. Is Preterm Birth a Risk Factor for Subsequent Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder in Children with Febrile Seizure?—A Retrospective Study. Life. 2021; 11(8):854. https://doi.org/10.3390/life11080854
Chicago/Turabian StyleLin, Chien-Heng, Wei-De Lin, I-Ching Chou, Inn-Chi Lee, and Syuan-Yu Hong. 2021. "Is Preterm Birth a Risk Factor for Subsequent Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder in Children with Febrile Seizure?—A Retrospective Study" Life 11, no. 8: 854. https://doi.org/10.3390/life11080854
APA StyleLin, C.-H., Lin, W.-D., Chou, I.-C., Lee, I.-C., & Hong, S.-Y. (2021). Is Preterm Birth a Risk Factor for Subsequent Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder in Children with Febrile Seizure?—A Retrospective Study. Life, 11(8), 854. https://doi.org/10.3390/life11080854






