Herbal Cannabis Use Is Not Associated with Changes in Levels of Endocannabinoids and Metabolic Profile Alterations among Older Adults
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Procedures
2.3. Assessments and Outcomes
2.4. Endocannabinoid Measurements
2.5. Statistical Analysis
3. Results
3.1. Cohort Characteristics
3.2. Blood Tests and Metabolic Parameters
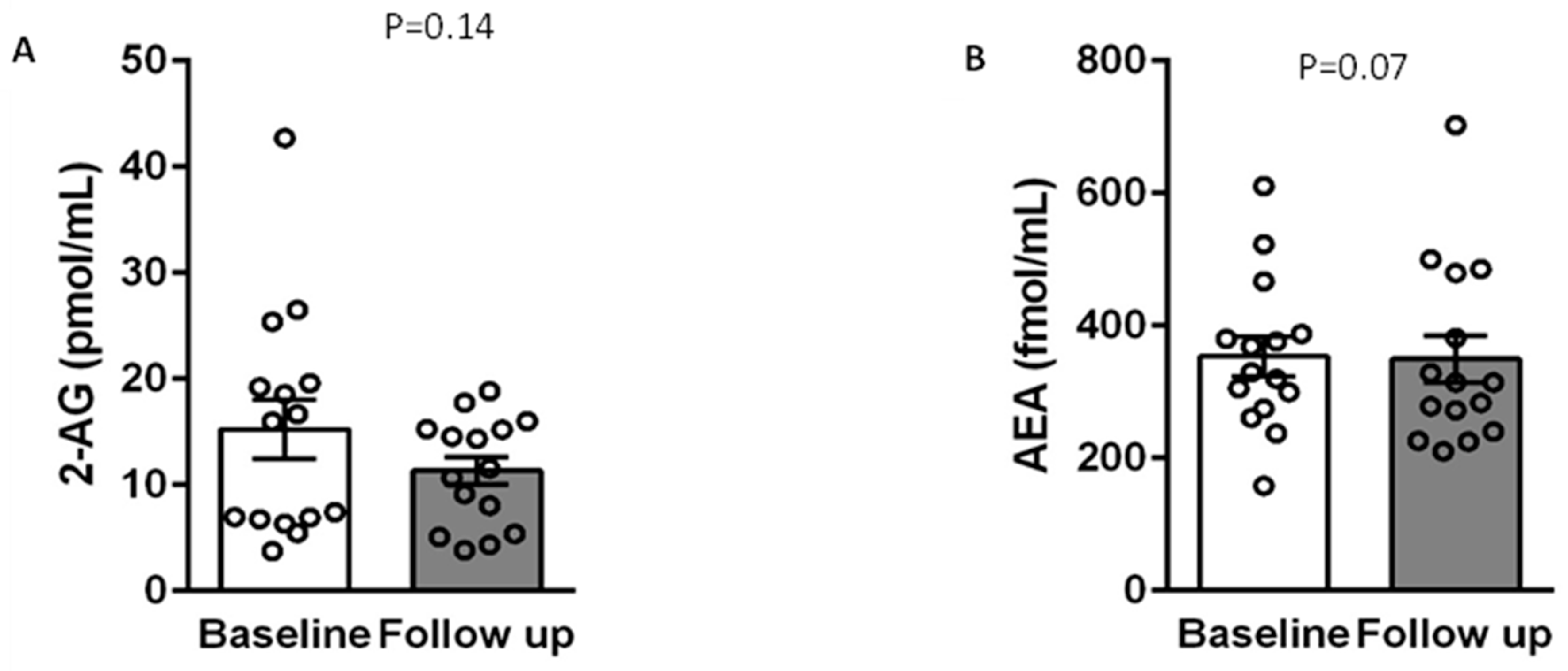
3.3. Correlations between Endocannabinoids, Metabolic Parameters, and Exogenic Cannabis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2021 Update A Report from the American Heart Association. Circulation 2021, 143, E254–E743. [Google Scholar] [CrossRef] [PubMed]
- Mazier, W.; Saucisse, N.; Gatta-Cherifi, B.; Cota, D. The Endocannabinoid System: Pivotal Orchestrator of Obesity and Metabolic Disease. Trends Endocrinol. Metab. 2015, 26, 524–537. [Google Scholar] [CrossRef]
- Joshi, N.; Onaivi, E.S. Endocannabinoid System Components: Overview and Tissue Distribution. Adv. Exp. Med. Biol. 2019, 1162, 1–12. [Google Scholar] [PubMed]
- Simon, V.; Cota, D. Mechanisms in endocrinology: Endocannabinoids and metabolism: Past, present and future. Eur. J. Endocrinol. 2017, 176, R309–R324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veilleux, A.; Di Marzo, V.; Silvestri, C. The Expanded Endocannabinoid System/Endocannabinoidome as a Potential Target for Treating Diabetes Mellitus. Curr. Diabetes Rep. 2019, 19, 117. [Google Scholar] [CrossRef]
- Matias, I.; Gatta-Cherifi, B.; Tabarin, A.; Clark, S.; Leste-Lasserre, T.; Marsicano, G.; Piazza, P.V.; Cota, D. Endocannabinoids measurement in human Saliva as potential biomarker of obesity. PLoS ONE 2012, 7, e42399. [Google Scholar] [CrossRef] [Green Version]
- Van Den Elsen, G.A.H.; Ahmed, A.I.A.; Verkes, R.J.; Feuth, T.; Van Der Marck, M.A.; Rikkert, M.G.M.O. Tetrahydrocannabinol in Behavioral Disturbances in Dementia: A Crossover Randomized Controlled Trial. Am. J. Geriatr. Psychiatry 2015, 23, 1214–1224. [Google Scholar] [CrossRef]
- Van den Elsen, G.A.H.; Ahmed, A.I.A.; Verkes, R.-J.; Kramers, C.; Feuth, T.; Rosenberg, P.B.; van der Marck, M.A.; Rikkert, M.G.M.O. Tetrahydrocannabinol for neuropsychiatric symptoms in dementia: A randomized controlled trial. Neurology 2015, 84, 2338–2346. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, A.I.A.; van den Elsen, G.A.H.; Colbers, A.; van der Marck, M.A.; Burger, D.M.; Feuth, T.B.; Rikkert, M.G.M.O.; Kramers, C. Safety and pharmacokinetics of oral delta-9-tetrahydrocannabinol in healthy older subjects: A randomized controlled trial. Eur. Neuropsychopharmacol. 2014, 24, 1475–1482. [Google Scholar] [CrossRef]
- Haleem, A.; Hwang, Y.J.; Elton-Marshall, T.; Rehm, J.; Imtiaz, S. The longitudinal relationship between cannabis use and hypertension. Drug Alcohol. Rev. 2021, 40, 914–919. [Google Scholar] [CrossRef]
- Sultan, S.R.; O’Sullivan, S.E.; England, T.J. The effects of acute and sustained cannabidiol dosing for seven days on the haemodynamics in healthy men: A randomised controlled trial. Br. J. Clin. Pharmacol. 2020, 86, 1125–1138. [Google Scholar] [CrossRef] [PubMed]
- Jadoon, K.A.; Tan, G.D.; O’sullivan, S.E. A single dose of cannabidiol reduces blood pressure in healthy volunteers in a randomized crossover study. JCI insight 2017, 2, e93760. [Google Scholar] [CrossRef] [PubMed]
- Vandrey, R.; Umbricht, A.; Strain, E.C. Increased blood pressure after abrupt cessation of daily cannabis use. J. Addict. Med. 2011, 5, 16–20. [Google Scholar] [CrossRef]
- Muniyappa, R.; Sable, S.; Ouwerkerk, R.; Mari, A.; Gharib, A.M.; Walter, M.; Courville, A.; Hall, G.; Chen, K.Y.; Volkow, N.D.; et al. Metabolic effects of chronic cannabis smoking. Diabetes Care 2013, 36, 2415–2422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kearney-Ramos, T.; Herrmann, E.S.; Belluomo, I.; Matias, I.; Vallée, M.; Monlezun, S.; Piazza, P.V.; Haney, M. The Relationship Between Circulating Endogenous Cannabinoids and the Effects of Smoked Cannabis. Cannabis Cannabinoid Res. 2022. [Google Scholar] [CrossRef]
- Park, J.Y.; Wu, L.T. Prevalence, reasons, perceived effects, and correlates of medical marijuana use: A review. Drug Alcohol. Depend. 2017, 177, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Fairman, B.J. Trends in registered medical marijuana participation across 13 US states and District of Columbia. Drug Alcohol. Depend. 2016, 159, 72–79. [Google Scholar] [CrossRef]
- Hamilton, H.A.; Brands, B.; Ialomiteanu, A.R.; Mann, R.E. Therapeutic use of cannabis: Prevalence and characteristics among adults in Ontario, Canada. Can. J. Public Health 2017, 108, e282–e287. [Google Scholar] [CrossRef]
- Perlman, A.I.; McLeod, H.M.; Ventresca, E.C.; Salinas, M.G.; Post, P.J.; Schuh, M.J.; Abu Dabrh, A.M. Medical Cannabis State and Federal Regulations: Implications for United States Health Care Entities. Mayo Clin. Proc. 2021, 96, 2671–2681. [Google Scholar] [CrossRef]
- Abuhasira, R.; Shbiro, L.; Landschaft, Y. Medical use of cannabis and cannabinoids containing products—Regulations in Europe and North America. Eur. J. Intern. Med. 2018, 49, 2–6. [Google Scholar] [CrossRef]
- Abuhasira, R.; Haviv, Y.S.; Leiba, M.; Leiba, A.; Ryvo, L.; Novack, V. Cannabis is associated with blood pressure reduction in older adults—A 24-hours ambulatory blood pressure monitoring study. Eur. J. Intern. Med. 2021, 86, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Aran, A.; Eylon, M.; Harel, M.; Polianski, L.; Nemirovski, A.; Tepper, S.; Schnapp, A.; Cassuto, H.; Wattad, N.; Tam, J. Lower circulating endocannabinoid levels in children with autism spectrum disorder. Mol. Autism 2019, 10, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matalon, S.T.; Azar, S.; Meiri, D.; Hadar, R.; Nemirovski, A.; Jabal, N.A.; Konikoff, F.M.; Drucker, L.; Tam, J.; Naftali, T. Endocannabinoid Levels in Ulcerative Colitis Patients Correlate With Clinical Parameters and Are Affected by Cannabis Consumption. Front. Endocrinol. 2021, 12, 685289. [Google Scholar] [CrossRef] [PubMed]
- Azar, S.; Sherf-Dagan, S.; Nemirovski, A.; Webb, M.; Raziel, A.; Keidar, A.; Goitein, D.; Sakran, N.; Shibolet, O.; Tam, J.; et al. Circulating Endocannabinoids Are Reduced Following Bariatric Surgery and Associated with Improved Metabolic Homeostasis in Humans. Obes. Surg. 2019, 29, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Moradi, H.; Park, C.; Igarashi, M.; Streja, E.; Argueta, D.A.; Soohoo, M.; Daglian, J.; You, A.S.; Rhee, C.M.; Kashyap, M.L.; et al. Serum endocannabinoid levels in patients with end-stage renal disease. J. Endocr. Soc. 2019, 3, 1869–1880. [Google Scholar] [CrossRef]
- Moradi, H.; Park, C.; Streja, E.; Argueta, D.A.; Dipatrizio, N.V.; You, A.S.; Rhee, C.M.; Vaziri, N.D.; Kalantar-Zadeh, K.; Piomelli, D. Circulating endocannabinoids and mortality in hemodialysis patients. Am. J. Nephrol. 2020, 51, 86–95. [Google Scholar] [CrossRef]
- Di Marzo, V.; Côté, M.; Matias, I.; Lemieux, I.; Arsenault, B.J.; Cartier, A.; Piscitelli, F.; Petrosino, S.; Alméras, N.; Després, J.P. Changes in plasma endocannabinoid levels in viscerally obese men following a 1 year lifestyle modification programme and waist circumference reduction: Associations with changes in metabolic risk factors. Diabetologia 2009, 52, 213–217. [Google Scholar] [CrossRef] [Green Version]
- Zelber-Sagi, S.; Azar, S.; Nemirovski, A.; Webb, M.; Halpern, Z.; Shibolet, O.; Tam, J. Serum levels of endocannabinoids are independently associated with nonalcoholic fatty liver disease. Obesity 2017, 25, 94–101. [Google Scholar] [CrossRef]
- Marchioni, C.; Santos-Lobato, B.L.; Queiroz, M.E.C.; Crippa, J.A.S.; Tumas, V. Endocannabinoid levels in patients with Parkinson’s disease with and without levodopa-induced dyskinesias. J. Neural Transm. 2020, 127, 1359–1367. [Google Scholar] [CrossRef]
- Thanabalasingam, S.J.; Ranjith, B.; Jackson, R.; Wijeratne, D.T. Cannabis and its derivatives for the use of motor symptoms in Parkinson’s disease: A systematic review and meta-analysis. Ther. Adv. Neurol. Disord. 2021, 14, 17562864211018560. [Google Scholar] [CrossRef]
- Remiszewski, P.; Jarocka-Karpowicz, I.; Biernacki, M.; Jastrząb, A.; Schlicker, E.; Toczek, M.; Harasim-Symbor, E.; Pędzińska-Betiuk, A.; Malinowska, B. Chronic cannabidiol administration fails to diminish blood pressure in rats with primary and secondary hypertension despite its effects on cardiac and plasma endocannabinoid system, oxidative stress and lipid metabolism. Int. J. Mol. Sci. 2020, 21, 1295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thieme, U.; Schelling, G.; Hauer, D.; Greif, R.; Dame, T.; Laubender, R.P.; Bernhard, W.; Thieme, D.; Campolongo, P.; Theiler, L. Quantification of anandamide and 2-arachidonoylglycerol plasma levels to examine potential influences of tetrahydrocannabinol application on the endocannabinoid system in humans. Drug Test. Anal. 2014, 6, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.; Ferreirós, N.; Bishay, P.; Geisslinger, G.; Tegeder, I.; Lötsch, J. Exogenous Delta9-tetrahydrocannabinol influences circulating endogenous cannabinoids in humans. J. Clin. Psychopharmacol. 2013, 33, 699–705. [Google Scholar] [CrossRef]
- Jacobson, M.R.; Watts, J.J.; Boileau, I.; Tong, J.; Mizrahi, R.; Jacobson, M.R.; Watts, J.J. A systematic review of phytocannabinoid exposure on the endocannabinoid system: Implications for psychosis. Eur. Neuropsychopharmacol. 2019, 29, 330–348. [Google Scholar] [CrossRef] [PubMed]
- Tischmann, L.; Drummen, M.; Joris, P.J.; Gatta-Cherifi, B.; Raben, A.; Fogelholm, M.; Matias, I.; Cota, D.; Mensink, R.P.; Westerterp-Plantenga, M.S.; et al. Effects of a High-Protein Diet on Cardiometabolic Health, Vascular Function, and Endocannabinoids—A Preview Study. Nutrients 2020, 12, 1512. [Google Scholar] [CrossRef] [PubMed]
- Lazarte, J.; Hegele, R.A. Cannabis effects on lipoproteins. Curr. Opin. Lipidol. 2019, 30, 140–146. [Google Scholar] [CrossRef]
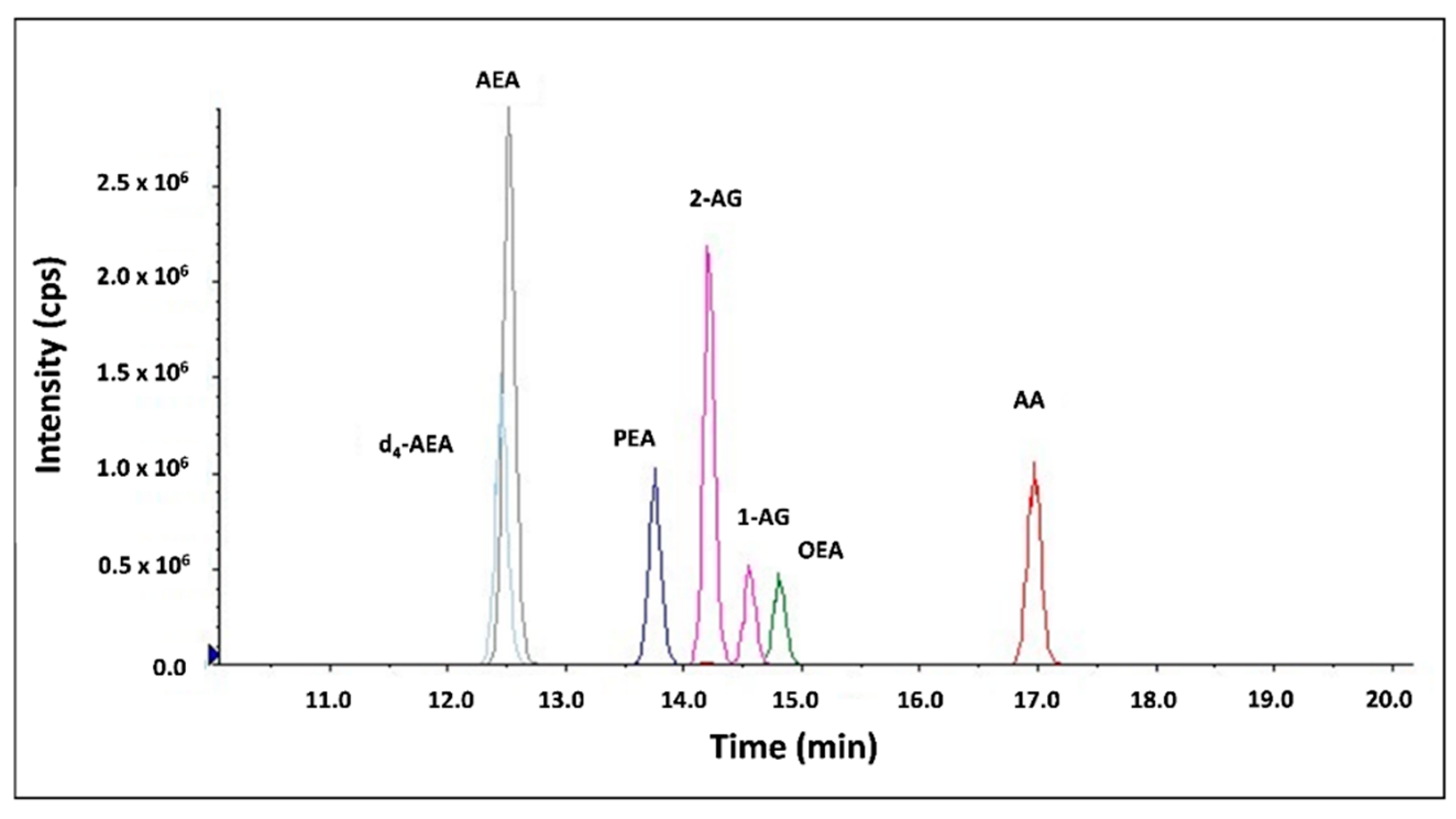

| Compound | Molecular Ion [M+H]+ (m/z) | Fragment (m/z) | DP (volts) | CE (volts) | CXP (volts) |
|---|---|---|---|---|---|
| 2-AG | 379.2 | 287.1 (quantifier) | 70 | 19 | 14 |
| 91 (qualifier) | 70 | 67 | 10 | ||
| AEA | 348.2 | 287.1 (quantifier) | 26 | 13 | 16 |
| 62 (qualifier) | 26 | 13 | 8 | ||
| PEA | 300.3 | 283.2 (quantifier) | 130 | 19 | 24 |
| 62 (qualifier) | 130 | 17 | 8 | ||
| AA | 305.3 | 91 (quantifier) | 1 | 49 | 10 |
| 287.1 (qualifier) | 1 | 13 | 22 | ||
| OEA | 326.3 | 61.9 (quantifier) | 146 | 21 | 24 |
| 309.1 (qualifier) | 146 | 21 | 42 | ||
| d4-AEA | 352.3 | 287.1 (quantifier) | 66 | 15 | 20 |
| 66 (qualifier) | 66 | 21 | 8 |
| Variable | Reference Range | Before Treatment | After Treatment | p-Value |
|---|---|---|---|---|
| Age (years, median, IQR) | 69 (66–72) | – | – | |
| Male (n, %) | 8 (53.3%) | – | – | |
| Indication for cannabis (n, %) | – | – | ||
| Neuropathic pain | 5 (33.3%) | – | – | |
| Parkinson’s Disease-associated pain | 7 (46.7%) | – | – | |
| Other indication | 3 (20.0%) | – | – | |
| Mode of cannabis administration | – | – | ||
| Oil | 11 (73.3%) | – | – | |
| Smoking | 3 (20.0%) | – | – | |
| Oil and smoking | 1 (6.7%) | – | – | |
| CBD and THC composition of cannabis products at treatment initiation (n, %) | – | – | ||
| THC 5%/CBD 10% | 5 (23.8%) | – | – | |
| THC 10%/CBD 2% | 7 (33.3%) | – | – | |
| THC 10%/CBD 10% | 3 (14.3%) | – | – | |
| THC 1%/CBD 20% | 1 (4.8%) | – | – | |
| THC 3%/CBD 15% | 1 (4.8%) | – | – | |
| THC 15%/CBD 3% | 2 (9.5%) | – | – | |
| THC 20%/CBD 1% | 1 (4.8%) | – | – | |
| Cannabis dosing | – | – | – | |
| Cannabis administration once a day (n, %) | 5 (33.3%) | – | – | |
| Cannabis administration twice a day (n, %) | 6 (40%) | – | – | |
| Cannabis administration ≥3 times a day (n, %) | 4 (26.7%) | – | – | |
| Total THC dose per day (mg, median, IQR) | 22.2 (13.5–40.0) | – | – | |
| Total CBD dose per day (mg, median, IQR) | 30.0 (5.5–39.5) | – | – | |
| Blood test values | – | – | ||
| Urea (mg/dL, mean ± SD) | 17–43 | 50.11 ± 21.7 | 51.19 ± 27.04 | 0.13 |
| Uric acid (mg/dL, mean ± SD) | 3.5–7.2 (male) | 5.62 ± 1.41 | 5.54 ± 1.58 | 0.89 |
| 2.6–6 (female) | ||||
| Creatinine (mg/dL, mean ± SD) | 0.67–1.17 (male) | 0.93 ± 0.27 | 0.88 ± 0.31 | 0.1 |
| 0.51–0.95 (female) | ||||
| Sodium (mEq/L, mean ± SD) | 135–145 | 139.93 ± 1.62 | 140 ± 1.85 | 0.84 |
| Potassium (mEq/L, mean ± SD) | 3.5–5.1 | 4.66 ± 0.43 | 5.05 ± 1.16 | 0.46 |
| Chloride (mEq/L, mean ± SD) | 98–106 | 103.87 ± 3.25 | 104 ± 3.09 | 0.34 |
| Calcium (mg/dL, mean ± SD) | 8.5–10.5 | 9.61 ± 0.34 | 9.37 ± 0.5 | 0.03 |
| Total cholesterol (mg/dL, mean ± SD) | 164.27 ± 57.7 | 164.07 ± 38.61 | 0.73 | |
| Non-HDL cholesterol (mg/dL, mean ± SD) | 113.4 ± 53.94 | 112.33 ± 33.54 | 1 | |
| LDL cholesterol (mg/dL, mean ± SD) | 78.86 ± 38.89 | 87.67 ± 31.93 | 0.57 | |
| HDL cholesterol (mg/dL, mean ± SD) | 50.8 ± 12.39 | 51.93 ± 14.3 | 0.55 | |
| LDL/HDL Ratio | 1.56 ± 0.66 | 1.75 ± 0.6 | 0.47 | |
| Triglycerides (mg/dL, mean ± SD) | 137.13 ± 75.22 | 123.07 ± 42.87 | 0.46 | |
| Fasting plasma glucose (mg/dL, mean ± SD) | 70–100 | 119.33 ± 30.01 | 112.93 ± 35.46 | 0.12 |
| Hemoglobin A1C (%, mean ± SD) | 4–5.7 | 6.15 ± 0.86 | 6.09 ± 0.88 | 0.86 |
| Fasting insulin (mU/mL, mean ± SD) | 5–25 | 14.32 ± 8.37 | 12.04 ± 8.53 | 0.21 |
| HOMA-IR | 4.55 ± 3.31 | 3.56 ± 2.9 | 0.1 | |
| C-reactive protein (mg/dL, mean ± SD) | 0.02–0.5 | 0.65 ± 0.76 | 0.9 ± 1.31 | 0.89 |
| Endocannabinoids | ||||
| 2-AG (pmol/mL, mean ± SD) | 15.23 ± 10.73 | 11.35 ± 5.1 | 0.07 | |
| AEA (fmol/mL, mean ± SD) | 353.41 ± 114.5 | 349.57 ± 137.46 | 0.39 | |
| AA (pmol/mL, mean ± SD) | 974.1 ± 216.13 | 859.27 ± 407.94 | 0.14 | |
| OEA (pmol/mL, mean ± SD) | 5.65 ± 4.16 | 5.15 ± 3.5 | 0.65 | |
| PEA (pmol/mL, mean ± SD) | 7.16 ± 3.11 | 7.06 ± 3.33 | 0.46 |
| Parameter | 2-AG | AEA | AA | OEA | PEA |
|---|---|---|---|---|---|
| Mean diastolic blood pressure (mm Hg) | 0.08 | 0.25 | 0.45 * | −0.12 | −0.01 |
| Mean heart rate (bpm) | −0.16 | 0.19 | 0.25 | −0.32 | −0.21 |
| Mean systolic blood pressure (mm Hg) | 0.01 | 0.10 | 0.25 | −0.23 | −0.08 |
| Body mass index | −0.09 | −0.18 | −0.21 | −0.30 | 0.00 |
| Waist-to-hip ratio | 0.23 | −0.11 | 0.05 | 0.02 | 0.02 |
| Total THC per day (mg) | −0.05 | 0.26 | 0.07 | −0.01 | −0.20 |
| Total CBD per day (mg) | −0.04 | 0.04 | −0.02 | −0.40 * | −0.44 * |
| Total cholesterol (mg/dL) | −0.13 | 0.00 | −0.06 | −0.10 | −0.21 |
| LDL cholesterol (mg/dL) | −0.30 | 0.06 | 0.01 | −0.28 | −0.39 |
| HDL cholesterol (mg/dL) | −0.20 | 0.18 | 0.16 | 0.24 | 0.09 |
| Non-HDL Cholesterol (mg/dL) | −0.03 | −0.05 | 0.05 | −0.16 | −0.24 |
| LDL/HDL Ratio | −0.19 | −0.05 | −0.03 | −0.47 * | −0.45 * |
| C-reactive protein (mg/dL) | −0.14 | 0.26 | 0.39 * | −0.01 | −0.05 |
| Triglycerides (mg/dL) | 0.47 * | 0.10 | 0.20 | −0.01 | 0.03 |
| Hemoglobin A1C (%) | 0.16 | 0.36 | 0.20 | 0.13 | 0.18 |
| Fasting plasma glucose (mg/dL) | 0.12 | 0.04 | −0.06 | 0.00 | −0.10 |
| HOMA-IR | 0.14 | −0.12 | 0.05 | −0.01 | −0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abuhasira, R.; Azar, S.; Nemirovski, A.; Tam, J.; Novack, V. Herbal Cannabis Use Is Not Associated with Changes in Levels of Endocannabinoids and Metabolic Profile Alterations among Older Adults. Life 2022, 12, 1539. https://doi.org/10.3390/life12101539
Abuhasira R, Azar S, Nemirovski A, Tam J, Novack V. Herbal Cannabis Use Is Not Associated with Changes in Levels of Endocannabinoids and Metabolic Profile Alterations among Older Adults. Life. 2022; 12(10):1539. https://doi.org/10.3390/life12101539
Chicago/Turabian StyleAbuhasira, Ran, Shahar Azar, Alina Nemirovski, Joseph Tam, and Victor Novack. 2022. "Herbal Cannabis Use Is Not Associated with Changes in Levels of Endocannabinoids and Metabolic Profile Alterations among Older Adults" Life 12, no. 10: 1539. https://doi.org/10.3390/life12101539
APA StyleAbuhasira, R., Azar, S., Nemirovski, A., Tam, J., & Novack, V. (2022). Herbal Cannabis Use Is Not Associated with Changes in Levels of Endocannabinoids and Metabolic Profile Alterations among Older Adults. Life, 12(10), 1539. https://doi.org/10.3390/life12101539








