Novel Insights into Pathophysiology of Orbital Inflammatory Diseases and Progression to Orbital Lymphoma by Pathway Enrichment Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. RNA Extraction
2.3. Digital Gene Expression Analysis
2.4. NanoString Data Processing
2.5. Statistical Evaluation
3. Results
3.1. Gene Set Enrichment Analysis (GSEA):
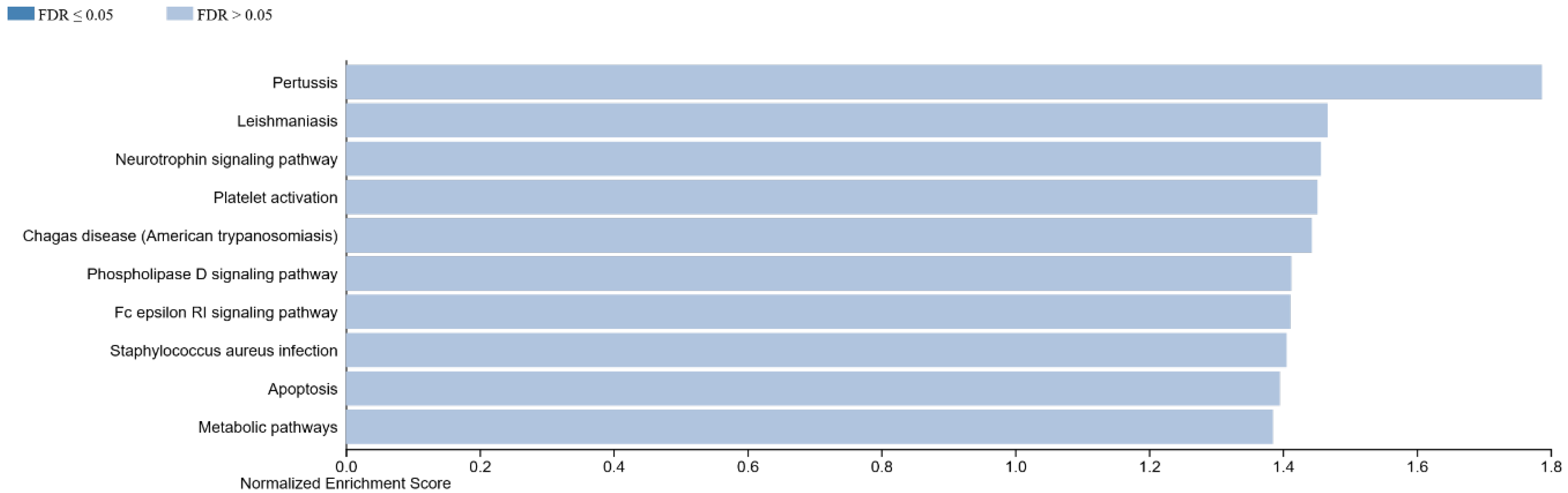
3.1.1. GSEA in Non-Specific Orbital Inflammation
- Innate immune pathways providing general response to foreign bodies:
- pertussis (normalized enrichment score, NES: 1.79; p-value: 0.001), Chagas disease (NES: 1.44; p = 0.03), Staphylococcus aureus infection (NES: 1.41; p = 0.05), phospholipase D signaling pathway (NES: 1.41; p = 0.06) and the neurotrophin signaling pathway (NES: 1.46; p = 0.04)
- Metabolic pathway part of an effector cascade:
- apoptosis (NES: 1.40; p = 0.066), Fc epsilon RI signaling pathway (NES: 1.41; p = 0.056), platelet activation (NES: 1.45; p = 0.037).
3.1.2. GSEA in MALT Lymphoma
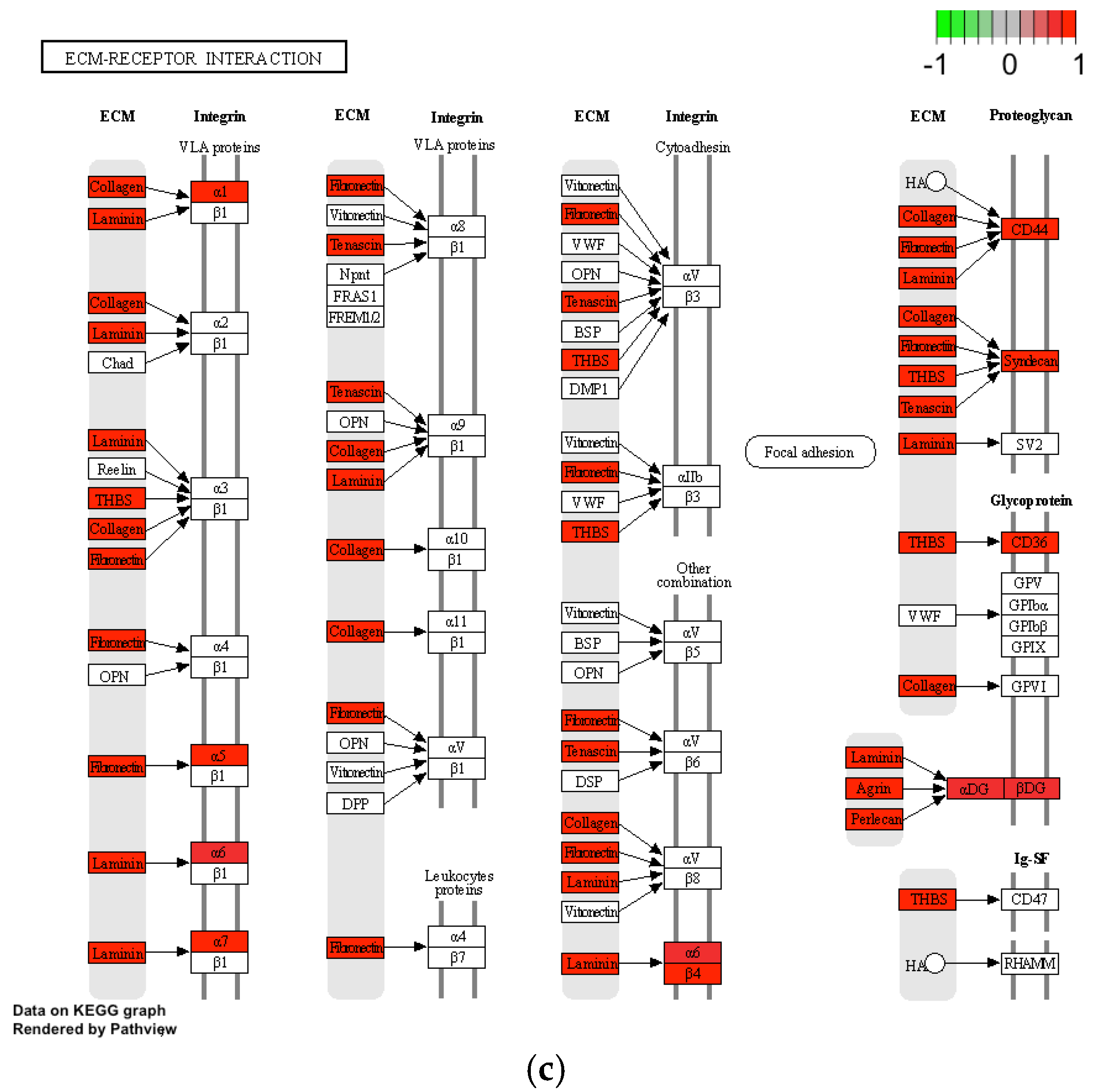
- Focal surface regulatory pathways: protein digestion and absorption (NES: 1.95; p < 0.001), ECM (extracellular matrix)–receptor interaction (NES: 1.58; p = 0.002), complement and coagulation cascades (NES: 1.36; p = 0.054) and focal adhesion (NES: 1.28; p = 0.063), amoebiasis (NES: 1.58; p = 0.011)
- Effector pathways with systematic impact: complement and coagulation cascades (NES: 1.36; p- = 0.054), AGE-RAGE signaling pathway in diabetic complications (NES: 1.34; p = 0.055), small-cell lung cancer (NES: 1.36; p = 0.080), relaxin signaling pathway (NES: 1.38; p = 0.05)
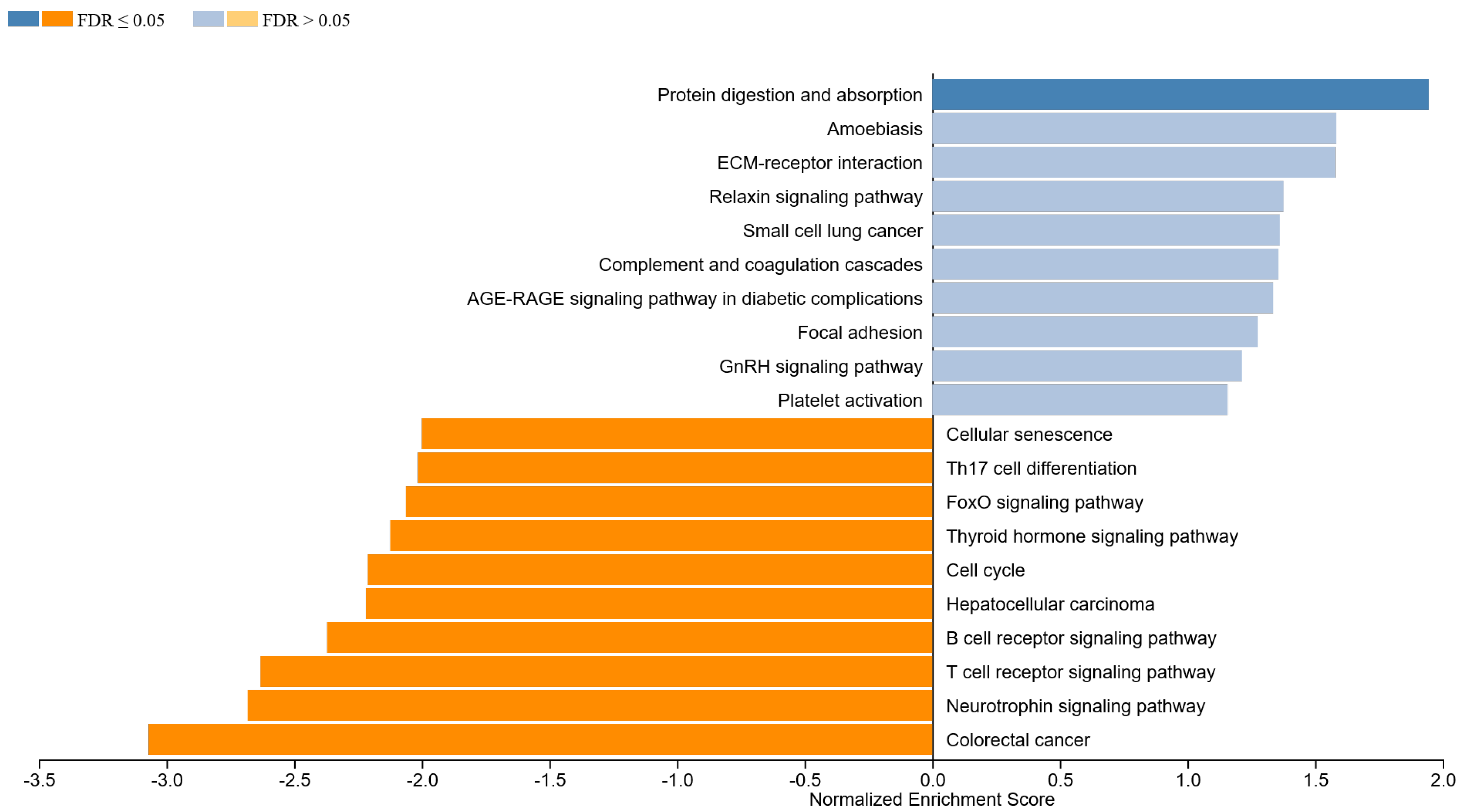
- Focal surface regulatory pathways: B-cell receptor signaling pathway (NES: −2.37; p < 0.001), T-cell receptor signaling pathway (NES: −2.63; p < 0.001), neurotrophin signaling pathway (NES: −2.68; p < 0.001), thyroid hormone signaling pathway (NES: −2.12; p < 0.001 and Th17 cell differentiation (NES: −2.02; p < 0.001)
- Effector pathways with systematic impact: cell cycle (NES: −2.21; p < 0.001), hepatocellular carcinoma (NES: −2.22; p-value: <0.001) and FoxO signaling pathway (NES: −2.06; p < 0.001)
3.1.3. GSEA in IgG4-ROD
- Innate immune pathways providing general focal response to foreign bodies:
- NOD-like receptor signaling pathway (NES: 1.44; p = 0.043), complement and coagulation cascades (NES: 1.35; p = 0.091), ECM–receptor interaction (NES: 1.28; p = 0.126), Salmonella infection (NES: 1.26; p = 0.16) as well as cytokine–cytokine receptor interaction (NES: 1.20; p = 0.20)
- Effector pathways with systematic impact: hematopoietic cell lineage (NES: 1.29; p = 0.129) herpes simplex infection (NES: 1.44; p = 0.047), and rheumatoid arthritis (NES: 1.22; p = 0.182)
- Fc gamma R-mediated phagocytosis (NES: −1.21; p = 0.19), B-cell receptor signaling pathway (NES: −1.14; p = 0.193), T-cell receptor signaling pathway (NES: −1.21; p = 0.214), neurotrophin signaling pathway (NES: −1.15; p = 0.21), platelet activation (NES: −1.12; p = 0.34), insulin signaling pathway (NES: −1.15; p = 0.350), phospholipase D signaling pathway (NES: −1.26; p = 0.111), as well as the thyroid hormone signaling pathway (NES: −1.22; p = 0.14)

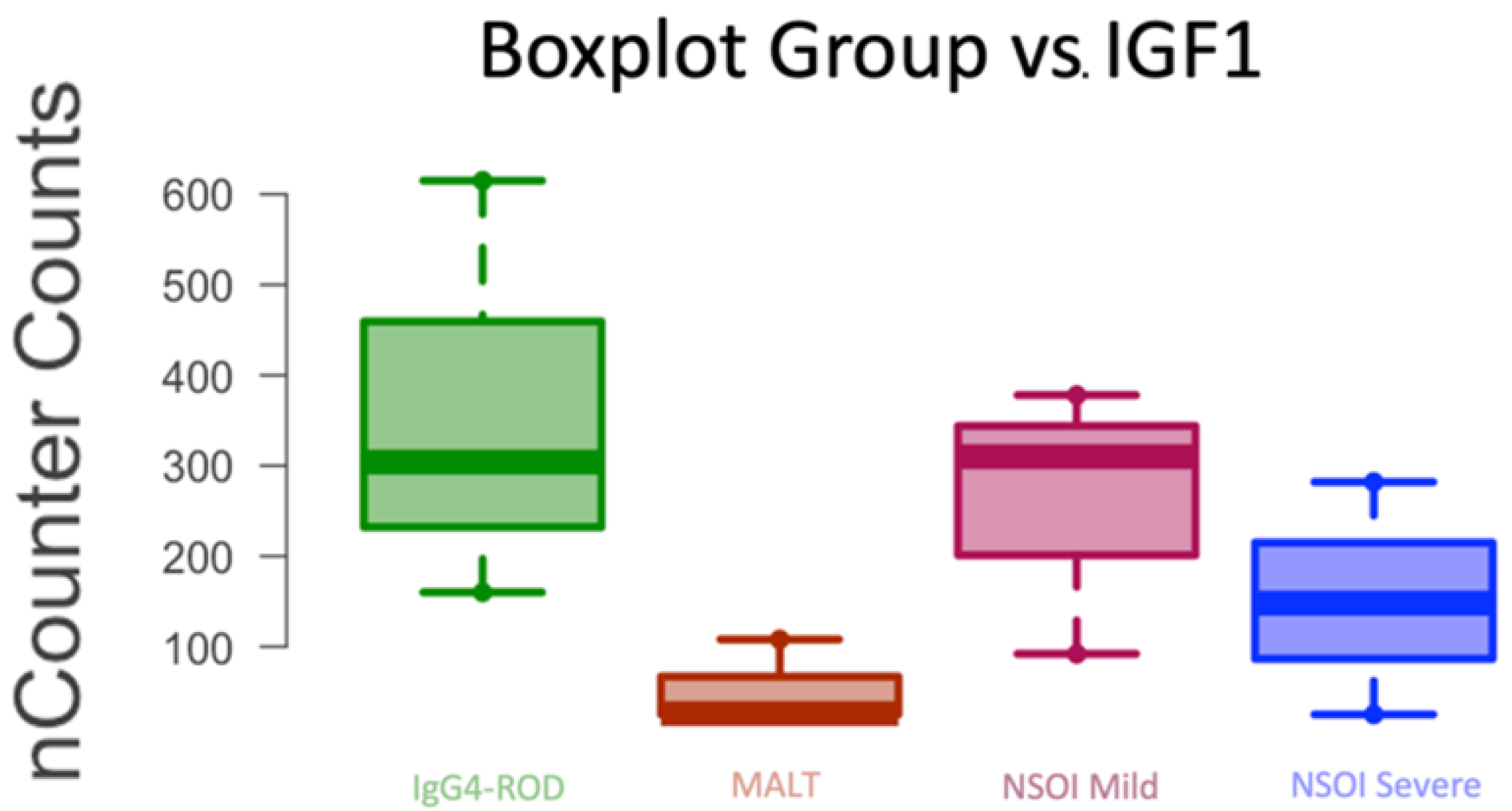
3.2. Re-Identification of Genes with Relevant Expression
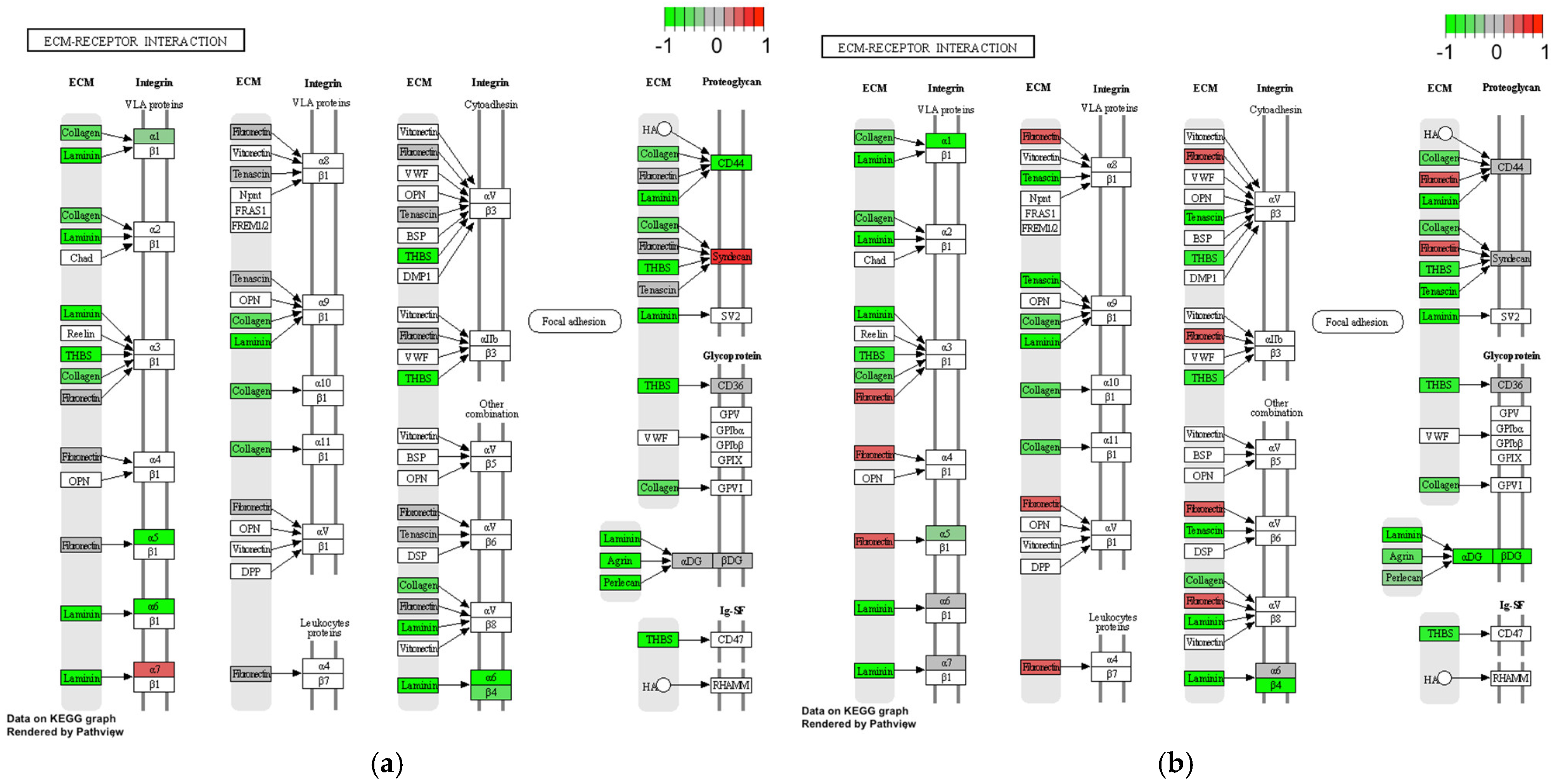
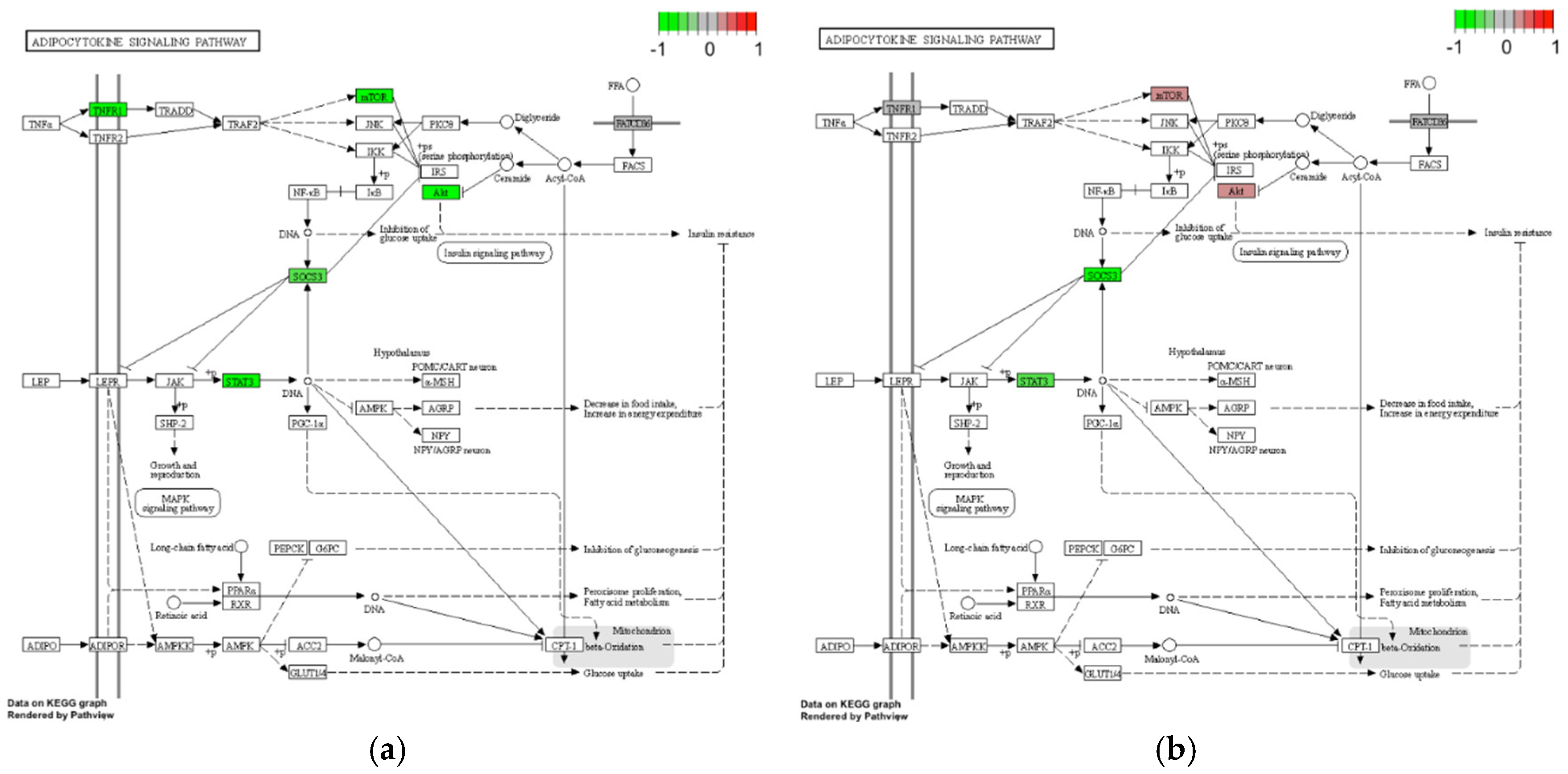
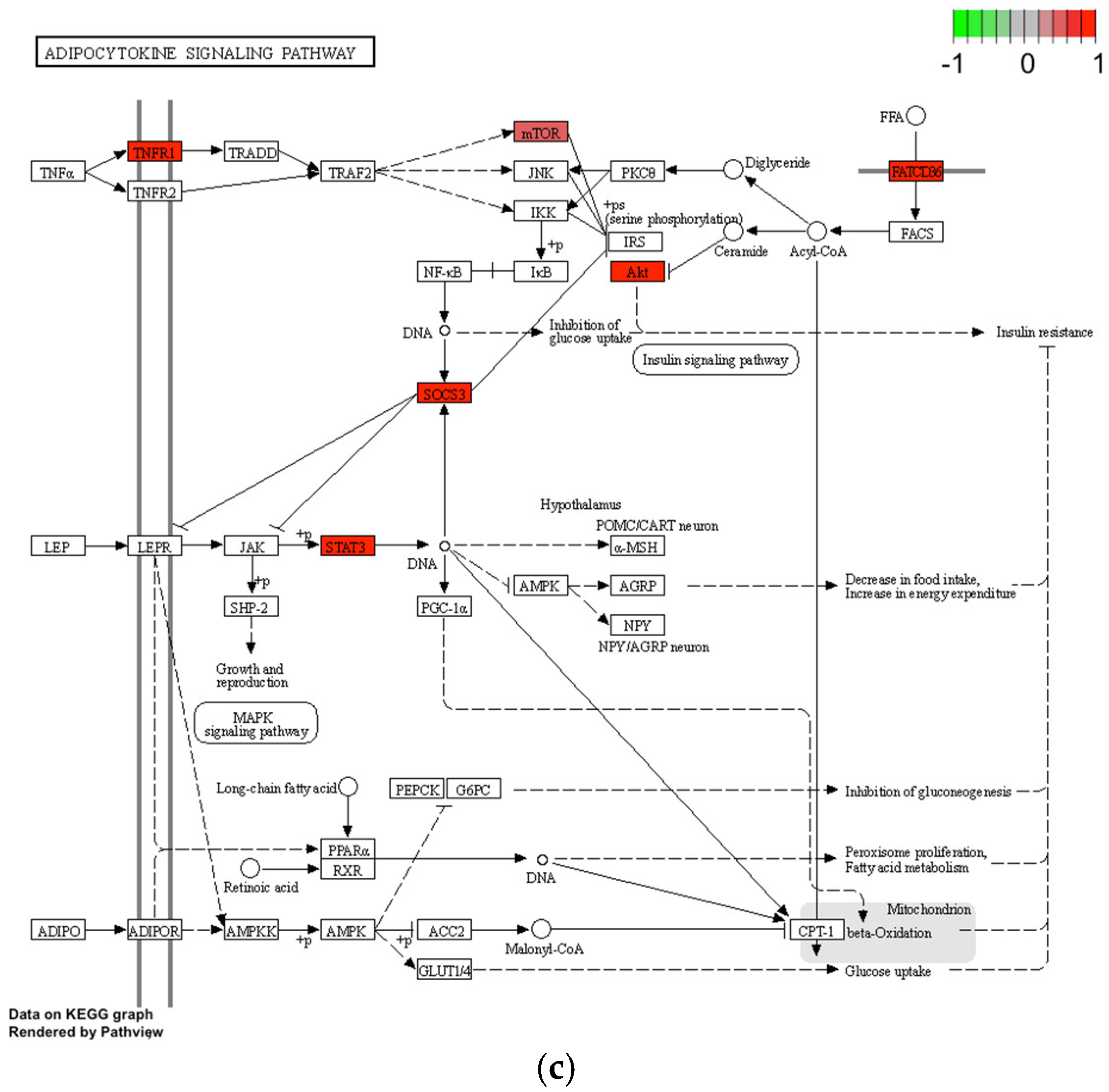
ECM–Receptor Interaction and Adipocytokine Signaling Pathway
4. Discussion
4.1. ECM–Receptor Interaction and Adipocytokine Signaling Pathway
4.2. NOD-like Receptor Signaling Pathway
4.3. Outlook into B- and T-Cell Receptor Signaling
4.3.1. B-Cell Receptor Signaling in MALT
4.3.2. B-Cell Receptor Signaling in IgG4-ROD
4.3.3. T-Cell Receptor Signaling and Cytokine Induced Proliferation
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Krieger, C.C.; Place, R.F.; Bevilacqua, C.; Marcus-Samuels, B.; Abel, B.S.; Skarulis, M.C.; Kahaly, G.J.; Neumann, S.; Gershengorn, M.C. TSH/IGF-1 Receptor Cross Talk in Graves’ Ophthalmopathy Pathogenesis. J. Clin. Endocrinol. Metab. 2016, 101, 2340–2347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morshed, S.A.; Davies, T.F. Graves’ Disease Mechanisms: The Role of Stimulating, Blocking, and Cleavage Region TSH Receptor Antibodies. Horm. Metab. Res. 2015, 47, 727–734. [Google Scholar] [PubMed] [Green Version]
- Tsui, S.; Naik, V.; Hoa, N.; Hwang, C.J.; Afifiyan, N.F.; Sinha Hikim, A.; Gianoukakis, A.G.; Douglas, R.S.; Smith, T.J. Evidence for an association between thyroid-stimulating hormone and insulin-like growth factor 1 receptors: A tale of two antigens implicated in Graves’ disease. J. Immunol. 2008, 181, 4397–4405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krieger, C.C.; Neumann, S.; Place, R.F.; Marcus-Samuels, B.; Gershengorn, M.C. Bidirectional TSH and IGF-1 receptor cross talk mediates stimulation of hyaluronan secretion by Graves’ disease immunoglobins. J. Clin. Endocrinol. Metab. 2015, 100, 1071–1077. [Google Scholar] [CrossRef]
- Stohr, M.; Oeverhaus, M.; Lytton, S.D.; Horstmann, M.; Zwanziger, D.; Moller, L.; Stark, A.; Fuhrer-Sakel, D.; Bechrakis, N.; Berchner-Pfannschmidt, U.; et al. Predicting the Course of Graves’ Orbitopathy Using Serially Measured TSH-Receptor Autoantibodies by Automated Binding Immunoassays and the Functional Bioassay. Horm. Metab. Res. 2021, 53, 435–443. [Google Scholar]
- Plohn, S.; Edelmann, B.; Japtok, L.; He, X.; Hose, M.; Hansen, W.; Schuchman, E.H.; Eckstein, A.; Berchner-Pfannschmidt, U. CD40 Enhances Sphingolipids in Orbital Fibroblasts: Potential Role of Sphingosine-1-Phosphate in Inflammatory T-Cell Migration in Graves’ Orbitopathy. Investig. Ophthalmol. Vis. Sci. 2018, 59, 5391–5397. [Google Scholar] [CrossRef]
- Lee, A.C.H.; Kahaly, G.J. Pathophysiology of thyroid-associated orbitopathy. Best Pract. Res. Clin. Endocrinol. Metab. 2022, 101620, in press. [Google Scholar] [CrossRef]
- Douglas, R.S.; Kahaly, G.J.; Ugradar, S.; Elflein, H.; Ponto, K.A.; Fowler, B.T.; Dailey, R.; Harris, G.J.; Schiffman, J.; Tang, R.; et al. Teprotumumab Efficacy, Safety, and Durability in Longer-Duration Thyroid Eye Disease and Re-treatment: OPTIC-X Study. Ophthalmology 2022, 129, 438–449. [Google Scholar] [CrossRef]
- Douglas, R.S.; Kahaly, G.J.; Patel, A.; Sile, S.; Thompson, E.H.Z.; Perdok, R.; Fleming, J.C.; Fowler, B.T.; Marcocci, C.; Marino, M.; et al. Teprotumumab for the Treatment of Active Thyroid Eye Disease. N. Engl. J. Med. 2020, 382, 341–352. [Google Scholar] [CrossRef]
- Oeverhaus, M.; Stohr, M.; Moller, L.; Fuhrer, D.; Eckstein, A. Graves’ Orbitopathy: Current Concepts for Medical Treatment. Klin. Monbl. Augenheilkd. 2021, 238, 24–32. [Google Scholar]
- Andrew, N.; Kearney, D.; Selva, D. IgG4-related orbital disease: A meta-analysis and review. Acta Ophthalmol. 2013, 91, 694–700. [Google Scholar] [CrossRef]
- Lee, M.J.; Planck, S.R.; Choi, D.; Harrington, C.A.; Wilson, D.J.; Dailey, R.A.; Ng, J.D.; Steele, E.A.; Hamilton, B.E.; Khwarg, S.I.; et al. Non-specific orbital inflammation: Current understanding and unmet needs. Prog. Retin. Eye Res. 2021, 81, 100885. [Google Scholar] [CrossRef]
- McNab, A.A. Orbital Myositis: A Comprehensive Review and Reclassification. Ophthalmic. Plast. Reconstr. Surg. 2020, 36, 109–117. [Google Scholar] [CrossRef]
- Higgs, B.W.; Liu, Y.; Guo, J.; Sebastian, Y.; Morehouse, C.; Zhu, W.; Ren, L.; Liu, M.; Du, Y.; Yu, G.; et al. High-throughput RNA sequencing reveals distinct gene signatures in active IgG4-related disease. Sci. Rep. 2017, 7, 17567. [Google Scholar] [CrossRef] [Green Version]
- Asakage, M.; Usui, Y.; Nezu, N.; Shimizu, H.; Tsubota, K.; Umazume, K.; Yamakawa, N.; Umezu, T.; Suwanai, H.; Kuroda, M.; et al. Comprehensive Gene Analysis of IgG4-Related Ophthalmic Disease Using RNA Sequencing. J. Clin. Med. 2020, 9, 3458. [Google Scholar] [CrossRef]
- Rosenbaum, J.T.; Choi, D.; Harrington, C.A.; Wilson, D.J.; Grossniklaus, H.E.; Sibley, C.H.; Salek, S.S.; Ng, J.D.; Dailey, R.A.; Steele, E.A.; et al. Gene Expression Profiling and Heterogeneity of Nonspecific Orbital Inflammation Affecting the Lacrimal Gland. JAMA Ophthalmol. 2017, 135, 1156–1162. [Google Scholar] [CrossRef]
- Verma, R.; Choi, D.; Chen, A.J.; Harrington, C.A.; Wilson, D.J.; Grossniklaus, H.E.; Dailey, R.A.; Ng, J.; Steele, E.A.; Planck, S.R.; et al. Enrichment of IGF-1R and PPARgamma signalling pathways in orbital inflammatory diseases: Steps toward understanding pathogenesis. Br. J. Ophthalmol. 2022, 106, 1012–1017. [Google Scholar] [CrossRef]
- Goto, H.; Takahira, M.; Azumi, A.; Japanese Study Group for Ig, G.R.O.D. Diagnostic criteria for IgG4-related ophthalmic disease. Jpn. J. Ophthalmol. 2015, 59, 1–7. [Google Scholar] [CrossRef]
- Mombaerts, I.; Ramberg, I.; Coupland, S.E.; Heegaard, S. Diagnosis of orbital mass lesions: Clinical, radiological, and pathological recommendations. Surv. Ophthalmol. 2019, 64, 741–756. [Google Scholar] [CrossRef]
- Mombaerts, I.; Rose, G.E.; Garrity, J.A. Orbital inflammation: Biopsy first. Surv. Ophthalmol. 2016, 61, 664–669. [Google Scholar] [CrossRef]
- Reis, P.P.; Waldron, L.; Goswami, R.S.; Xu, W.; Xuan, Y.; Perez-Ordonez, B.; Gullane, P.; Irish, J.; Jurisica, I.; Kamel-Reid, S. mRNA transcript quantification in archival samples using multiplexed, color-coded probes. BMC Biotechnol. 2011, 11, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrew, N.H.; Sladden, N.; Kearney, D.J.; Selva, D. An analysis of IgG4-related disease (IgG4-RD) among idiopathic orbital inflammations and benign lymphoid hyperplasias using two consensus-based diagnostic criteria for IgG4-RD. Br. J. Ophthalmol. 2015, 99, 376–381. [Google Scholar] [CrossRef]
- Yan, J.; Wu, Z.; Li, Y. The differentiation of idiopathic inflammatory pseudotumor from lymphoid tumors of orbit: Analysis of 319 cases. Orbit 2004, 23, 245–254. [Google Scholar] [CrossRef]
- Du, M.Q. MALT lymphoma: A paradigm of NF-kappaB dysregulation. Semin. Cancer Biol. 2016, 39, 49–60. [Google Scholar] [CrossRef] [Green Version]
- Schattner, E.J. Apoptosis in lymphocytic leukemias and lymphomas. Cancer Investig. 2002, 20, 737–748. [Google Scholar] [CrossRef]
- Gong, S.; Crane, G.M.; McCall, C.M.; Xiao, W.; Ganapathi, K.A.; Cuka, N.; Davies-Hill, T.; Xi, L.; Raffeld, M.; Pittaluga, S.; et al. Expanding the Spectrum of EBV-positive Marginal Zone Lymphomas: A Lesion Associated with Diverse Immunodeficiency Settings. Am. J. Surg. Pathol. 2018, 42, 1306–1316. [Google Scholar] [CrossRef]
- Ferreri, A.J.; Govi, S.; Ponzoni, M. Marginal zone lymphomas and infectious agents. Semin. Cancer Biol. 2013, 23, 431–440. [Google Scholar] [CrossRef]
- Al-Ghazzawi, K.; Baum, S.H.; Pfortner, R.; Philipp, S.; Bechrakis, N.; Gortz, G.; Eckstein, A.; Mairinger, F.D.; Oeverhaus, M. Evaluation of Orbital Lymphoproliferative and Inflammatory Disorders by Gene Expression Analysis. Int. J. Mol. Sci. 2022, 23, 8609. [Google Scholar] [CrossRef]
- Walter, R.F.; Mairinger, F.D.; Wohlschlaeger, J.; Worm, K.; Ting, S.; Vollbrecht, C.; Schmid, K.W.; Hager, T. FFPE tissue as a feasible source for gene expression analysis--a comparison of three reference genes and one tumor marker. Pathol. Res. Pract. 2013, 209, 784–789. [Google Scholar] [CrossRef]
- Walter, R.F.H.; Werner, R.; Vollbrecht, C.; Hager, T.; Flom, E.; Christoph, D.C.; Schmeller, J.; Schmid, K.W.; Wohlschlaeger, J.; Mairinger, F.D. ACTB, CDKN1B, GAPDH, GRB2, RHOA and SDCBP Were Identified as Reference Genes in Neuroendocrine Lung Cancer via the nCounter Technology. PLoS ONE 2016, 11, e0165181. [Google Scholar] [CrossRef] [Green Version]
- Mairinger, F.; Bankfalvi, A.; Schmid, K.W.; Mairinger, E.; Mach, P.; Walter, R.F.; Borchert, S.; Kasimir-Bauer, S.; Kimmig, R.; Buderath, P. Digital Immune-Related Gene Expression Signatures in High-Grade Serous Ovarian Carcinoma: Developing Prediction Models For Platinum Response. Cancer Manag. Res. 2019, 11, 9571–9583. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.; Wang, J.; Jaehnig, E.J.; Shi, Z.; Zhang, B. WebGestalt 2019: Gene set analysis toolkit with revamped UIs and APIs. Nucleic Acids Res. 2019, 47, W199–W205. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Vasaikar, S.; Shi, Z.; Greer, M.; Zhang, B. WebGestalt 2017: A more comprehensive, powerful, flexible and interactive gene set enrichment analysis toolkit. Nucleic Acids Res. 2017, 45, W130–W137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Duncan, D.; Shi, Z.; Zhang, B. WEB-based GEne SeT AnaLysis Toolkit (WebGestalt): Update 2013. Nucleic Acids Res. 2013, 41, W77–W83. [Google Scholar] [CrossRef] [Green Version]
- Zhang, B.; Kirov, S.; Snoddy, J. WebGestalt: An integrated system for exploring gene sets in various biological contexts. Nucleic Acids Res. 2005, 33, W741–W748. [Google Scholar] [CrossRef]
- Wixon, J.; Kell, D. The Kyoto encyclopedia of genes and genomes—KEGG. Yeast 2000, 17, 48–55. [Google Scholar]
- Saxena, N.K.; Anania, F.A. Adipocytokines and hepatic fibrosis. Trends Endocrinol. Metab. 2015, 26, 153–161. [Google Scholar] [CrossRef] [Green Version]
- Philipp, S.; Horstmann, M.; Hose, M.; Daser, A.; Gortz, G.E.; Jesenek, C.; Flogel, U.; Hansen, W.; Bechrakis, N.; Banga, J.P.S.; et al. An Early Wave of Macrophage Infiltration Intertwined with Antigen-Specific Proinflammatory T Cells and Browning of Adipose Tissue Characterizes the Onset of Orbital Inflammation in a Mouse Model of Graves’ Orbitopathy. Thyroid 2022, 32, 283–293. [Google Scholar] [CrossRef]
- D’Alessandro, M.; Bergantini, L.; Refini, R.M.; Cameli, P.; Perillo, F.; Landi, C.; Icorne, F.; Perrone, A.; Sestini, P.; Bonella, F.; et al. Adiponectin and leptin levels in idiopathic pulmonary fibrosis: A new method for BAL and serum assessment. Immunobiology 2020, 225, 151997. [Google Scholar] [CrossRef]
- Jaspars, L.H.; Beljaards, R.C.; Bonnet, P.; Willemze, R.; Meijer, C.J. Distinctive adhesion pathways are involved in epitheliotropic processes at different sites. J. Pathol. 1996, 178, 385–392. [Google Scholar] [CrossRef]
- Rosenbaum, J.T.; Choi, D.; Wilson, D.J.; Grossniklaus, H.E.; Harrington, C.A.; Dailey, R.A.; Ng, J.D.; Steele, E.A.; Czyz, C.N.; Foster, J.A.; et al. Fibrosis, gene expression and orbital inflammatory disease. Br. J. Ophthalmol. 2015, 99, 1424–1429. [Google Scholar] [CrossRef] [Green Version]
- Hynes, R.O. Integrins: Bidirectional, allosteric signaling machines. Cell 2002, 110, 673–687. [Google Scholar] [CrossRef] [Green Version]
- Yoshioka, T.; Otero, J.; Chen, Y.; Kim, Y.M.; Koutcher, J.A.; Satagopan, J.; Reuter, V.; Carver, B.; de Stanchina, E.; Enomoto, K.; et al. beta4 Integrin signaling induces expansion of prostate tumor progenitors. J. Clin. Investig. 2013, 123, 682–699. [Google Scholar]
- Kajiji, S.; Tamura, R.N.; Quaranta, V. A novel integrin (alpha E beta 4) from human epithelial cells suggests a fourth family of integrin adhesion receptors. EMBO J. 1989, 8, 673–680. [Google Scholar] [CrossRef]
- Ruan, S.; Lin, M.; Zhu, Y.; Lum, L.; Thakur, A.; Jin, R.; Shao, W.; Zhang, Y.; Hu, Y.; Huang, S.; et al. Integrin beta4-Targeted Cancer Immunotherapies Inhibit Tumor Growth and Decrease Metastasis. Cancer Res. 2020, 80, 771–783. [Google Scholar] [CrossRef] [Green Version]
- Caruso, R.; Warner, N.; Inohara, N.; Nunez, G. NOD1 and NOD2: Signaling, host defense, and inflammatory disease. Immunity 2014, 41, 898–908. [Google Scholar] [CrossRef] [Green Version]
- Bertin, J.; Nir, W.J.; Fischer, C.M.; Tayber, O.V.; Errada, P.R.; Grant, J.R.; Keilty, J.J.; Gosselin, M.L.; Robison, K.E.; Wong, G.H.; et al. Human CARD4 protein is a novel CED-4/Apaf-1 cell death family member that activates NF-kappaB. J. Biol. Chem. 1999, 274, 12955–12958. [Google Scholar] [CrossRef] [Green Version]
- Ogura, Y.; Inohara, N.; Benito, A.; Chen, F.F.; Yamaoka, S.; Nunez, G. Nod2, a Nod1/Apaf-1 family member that is restricted to monocytes and activates NF-kappaB. J. Biol. Chem. 2001, 276, 4812–4818. [Google Scholar] [CrossRef] [Green Version]
- Harb, A.A.; Chen, Y.; Ben-Ami, J.R.; Francke, M.; Hur, C.; Turk, A.T.; Gudis, D.A. Acute Vision Loss From IgG4-Related and Bacterial Rhinosinusitis After COVID-19. JAMA Otolaryngol. Head Neck. Surg. 2021, 147, 914–915. [Google Scholar] [CrossRef]
- Hamano, H.; Kawa, S.; Horiuchi, A.; Unno, H.; Furuya, N.; Akamatsu, T.; Fukushima, M.; Nikaido, T.; Nakayama, K.; Usuda, N.; et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N. Engl. J. Med. 2001, 344, 732–738. [Google Scholar] [CrossRef]
- Zhao, A.; Wu, F.; Wang, Y.; Li, J.; Xu, W.; Liu, H. Analysis of Genetic Alterations in Ocular Adnexal Mucosa-Associated Lymphoid Tissue Lymphoma With Whole-Exome Sequencing. Front. Oncol. 2022, 12, 817635. [Google Scholar] [CrossRef]
- Fowler, N.; Davis, E. Targeting B-cell receptor signaling: Changing the paradigm. Hematol. Am. Soc. Hematol. Educ. Program. 2013, 2013, 553–560. [Google Scholar] [CrossRef] [Green Version]
- Craig, V.J.; Arnold, I.; Gerke, C.; Huynh, M.Q.; Wundisch, T.; Neubauer, A.; Renner, C.; Falkow, S.; Muller, A. Gastric MALT lymphoma B cells express polyreactive, somatically mutated immunoglobulins. Blood 2010, 115, 581–591. [Google Scholar] [CrossRef] [Green Version]
- Lucas, P.C.; Yonezumi, M.; Inohara, N.; McAllister-Lucas, L.M.; Abazeed, M.E.; Chen, F.F.; Yamaoka, S.; Seto, M.; Nunez, G. Bcl10 and MALT1, independent targets of chromosomal translocation in malt lymphoma, cooperate in a novel NF-kappa B signaling pathway. J. Biol. Chem. 2001, 276, 19012–19019. [Google Scholar] [CrossRef]
- Nakamura, S.; Aoyagi, K.; Furuse, M.; Suekane, H.; Matsumoto, T.; Yao, T.; Sakai, Y.; Fuchigami, T.; Yamamoto, I.; Tsuneyoshi, M.; et al. B-cell monoclonality precedes the development of gastric MALT lymphoma in Helicobacter pylori-associated chronic gastritis. Am. J. Pathol. 1998, 152, 1271–1279. [Google Scholar]
- Liu, Y.C.; Ohyashiki, J.H.; Ito, Y.; Iwaya, K.; Serizawa, H.; Mukai, K.; Goto, H.; Usui, M.; Ohyashiki, K. Chlamydia psittaci in ocular adnexal lymphoma: Japanese experience. Leuk. Res. 2006, 30, 1587–1589. [Google Scholar] [CrossRef]
- Chanudet, E.; Zhou, Y.; Bacon, C.M.; Wotherspoon, A.C.; Muller-Hermelink, H.K.; Adam, P.; Dong, H.Y.; de Jong, D.; Li, Y.; Wei, R.; et al. Chlamydia psittaci is variably associated with ocular adnexal MALT lymphoma in different geographical regions. J. Pathol. 2006, 209, 344–351. [Google Scholar] [CrossRef]
- Zhu, D.; Ikpatt, O.F.; Dubovy, S.R.; Lossos, C.; Natkunam, Y.; Chapman-Fredricks, J.R.; Fan, Y.S.; Lossos, I.S. Molecular and genomic aberrations in Chlamydophila psittaci negative ocular adnexal marginal zone lymphomas. Am. J. Hematol. 2013, 88, 730–735. [Google Scholar] [CrossRef] [Green Version]
- Maillette de Buy Wenniger, L.J.; Doorenspleet, M.E.; Klarenbeek, P.L.; Verheij, J.; Baas, F.; Elferink, R.P.; Tak, P.P.; de Vries, N.; Beuers, U. Immunoglobulin G4+ clones identified by next-generation sequencing dominate the B cell receptor repertoire in immunoglobulin G4 associated cholangitis. Hepatology 2013, 57, 2390–2398. [Google Scholar] [CrossRef]
- Du, H.; Shi, L.; Chen, P.; Yang, W.; Xun, Y.; Yang, C.; Zhao, L.; Zhou, Y.; Chen, G. Prohibitin Is Involved in Patients with IgG4 Related Disease. PLoS ONE 2015, 10, e0125331. [Google Scholar] [CrossRef]
- Perugino, C.A.; AlSalem, S.B.; Mattoo, H.; Della-Torre, E.; Mahajan, V.; Ganesh, G.; Allard-Chamard, H.; Wallace, Z.; Montesi, S.B.; Kreuzer, J.; et al. Identification of galectin-3 as an autoantigen in patients with IgG4-related disease. J. Allergy Clin. Immunol. 2019, 143, 736–745.e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wallace, Z.S.; Mattoo, H.; Carruthers, M.; Mahajan, V.S.; Della Torre, E.; Lee, H.; Kulikova, M.; Deshpande, V.; Pillai, S.; Stone, J.H. Plasmablasts as a biomarker for IgG4-related disease, independent of serum IgG4 concentrations. Ann. Rheum. Dis. 2015, 74, 190–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khosroshahi, A.; Bloch, D.B.; Deshpande, V.; Stone, J.H. Rituximab therapy leads to rapid decline of serum IgG4 levels and prompt clinical improvement in IgG4-related systemic disease. Arthritis Rheum. 2010, 62, 1755–1762. [Google Scholar] [CrossRef] [PubMed]
- Detiger, S.E.; Karim, A.F.; Verdijk, R.M.; van Hagen, P.M.; van Laar, J.A.M.; Paridaens, D. The treatment outcomes in IgG4-related orbital disease: A systematic review of the literature. Acta Ophthalmol. 2019, 97, 451–459. [Google Scholar] [CrossRef]
- Morita, R.; Schmitt, N.; Bentebibel, S.E.; Ranganathan, R.; Bourdery, L.; Zurawski, G.; Foucat, E.; Dullaers, M.; Oh, S.; Sabzghabaei, N.; et al. Human blood CXCR5(+)CD4(+) T cells are counterparts of T follicular cells and contain specific subsets that differentially support antibody secretion. Immunity 2011, 34, 108–121. [Google Scholar] [CrossRef]
- Rousset, F.; Garcia, E.; Defrance, T.; Peronne, C.; Vezzio, N.; Hsu, D.H.; Kastelein, R.; Moore, K.W.; Banchereau, J. Interleukin 10 is a potent growth and differentiation factor for activated human B lymphocytes. Proc. Natl. Acad. Sci. USA 1992, 89, 1890–1893. [Google Scholar] [CrossRef] [Green Version]
- Pene, J.; Gauchat, J.F.; Lecart, S.; Drouet, E.; Guglielmi, P.; Boulay, V.; Delwail, A.; Foster, D.; Lecron, J.C.; Yssel, H. Cutting edge: IL-21 is a switch factor for the production of IgG1 and IgG3 by human B cells. J. Immunol. 2004, 172, 5154–5157. [Google Scholar] [CrossRef] [Green Version]
- Good, K.L.; Bryant, V.L.; Tangye, S.G. Kinetics of human B cell behavior and amplification of proliferative responses following stimulation with IL-21. J. Immunol. 2006, 177, 5236–5247. [Google Scholar] [CrossRef] [Green Version]
- Chung, Y.; Tanaka, S.; Chu, F.; Nurieva, R.I.; Martinez, G.J.; Rawal, S.; Wang, Y.H.; Lim, H.; Reynolds, J.M.; Zhou, X.H.; et al. Follicular regulatory T cells expressing Foxp3 and Bcl-6 suppress germinal center reactions. Nat. Med. 2011, 17, 983–988. [Google Scholar] [CrossRef]
- Ito, F.; Kamekura, R.; Yamamoto, M.; Takano, K.; Takaki, H.; Yabe, H.; Ikegami, I.; Shigehara, K.; Himi, T.; Takahashi, H.; et al. IL-10(+) T follicular regulatory cells are associated with the pathogenesis of IgG4-related disease. Immunol. Lett. 2019, 207, 56–63. [Google Scholar] [CrossRef]
- Jeannin, P.; Lecoanet, S.; Delneste, Y.; Gauchat, J.F.; Bonnefoy, J.Y. IgE versus IgG4 production can be differentially regulated by IL-10. J. Immunol. 1998, 160, 3555–3561. [Google Scholar]
| Gene | p-Value | FDR-Adjusted p Values | Lower CI | Higher CI |
|---|---|---|---|---|
| Lymphoma by IGF1 | 0.0110 | 0.0224 | −349.7 | −59.2 |
| Lymphoma by IGFBP4 | 0.0008 | 0.0121 | −2204.0 | −783.1 |
| Lymphoma by IGFBP7 | 0.0052 | 0.0165 | −1670 | −407.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Ghazzawi, K.; Mairinger, F.D.; Pförtner, R.; Horstmann, M.; Bechrakis, N.; Mohr, C.; Eckstein, A.; Oeverhaus, M. Novel Insights into Pathophysiology of Orbital Inflammatory Diseases and Progression to Orbital Lymphoma by Pathway Enrichment Analysis. Life 2022, 12, 1660. https://doi.org/10.3390/life12101660
Al-Ghazzawi K, Mairinger FD, Pförtner R, Horstmann M, Bechrakis N, Mohr C, Eckstein A, Oeverhaus M. Novel Insights into Pathophysiology of Orbital Inflammatory Diseases and Progression to Orbital Lymphoma by Pathway Enrichment Analysis. Life. 2022; 12(10):1660. https://doi.org/10.3390/life12101660
Chicago/Turabian StyleAl-Ghazzawi, Karim, Fabian D. Mairinger, Roman Pförtner, Mareike Horstmann, Nikolaos Bechrakis, Christopher Mohr, Anja Eckstein, and Michael Oeverhaus. 2022. "Novel Insights into Pathophysiology of Orbital Inflammatory Diseases and Progression to Orbital Lymphoma by Pathway Enrichment Analysis" Life 12, no. 10: 1660. https://doi.org/10.3390/life12101660
APA StyleAl-Ghazzawi, K., Mairinger, F. D., Pförtner, R., Horstmann, M., Bechrakis, N., Mohr, C., Eckstein, A., & Oeverhaus, M. (2022). Novel Insights into Pathophysiology of Orbital Inflammatory Diseases and Progression to Orbital Lymphoma by Pathway Enrichment Analysis. Life, 12(10), 1660. https://doi.org/10.3390/life12101660








