Role of Intra-Parotid Lymph Node Metastasis in Primary Parotid Carcinoma
Abstract
:1. Introduction
2. Distribution of Lymph Nodes within the Parotid Gland
3. Implications of Intra-Glandular Lymph Node Metastasis
4. Assessment of Intra-Parotid Lymph Nodes in the UICC Staging System
5. Locations of Parotid Malignancies and Intra-Parotid Lymph Node Metastasis
6. Intra-Parotid Node Metastases: An Indicator of Prognosis
7. Importance of Collaborations with Pathologists
8. Importance of Evaluations of Intra-Parotid Lymph Nodes in the Local Control of Parotid Carcinoma
9. Intra-Parotid and Cervical Lymph Node Metastasis in Primary Parotid Carcinoma
10. Surgery for Parotid Carcinoma from the Viewpoint of Intra-Glandular Lymph Nodes—Lower Half Resection
10.1. Concept
10.2. Indications
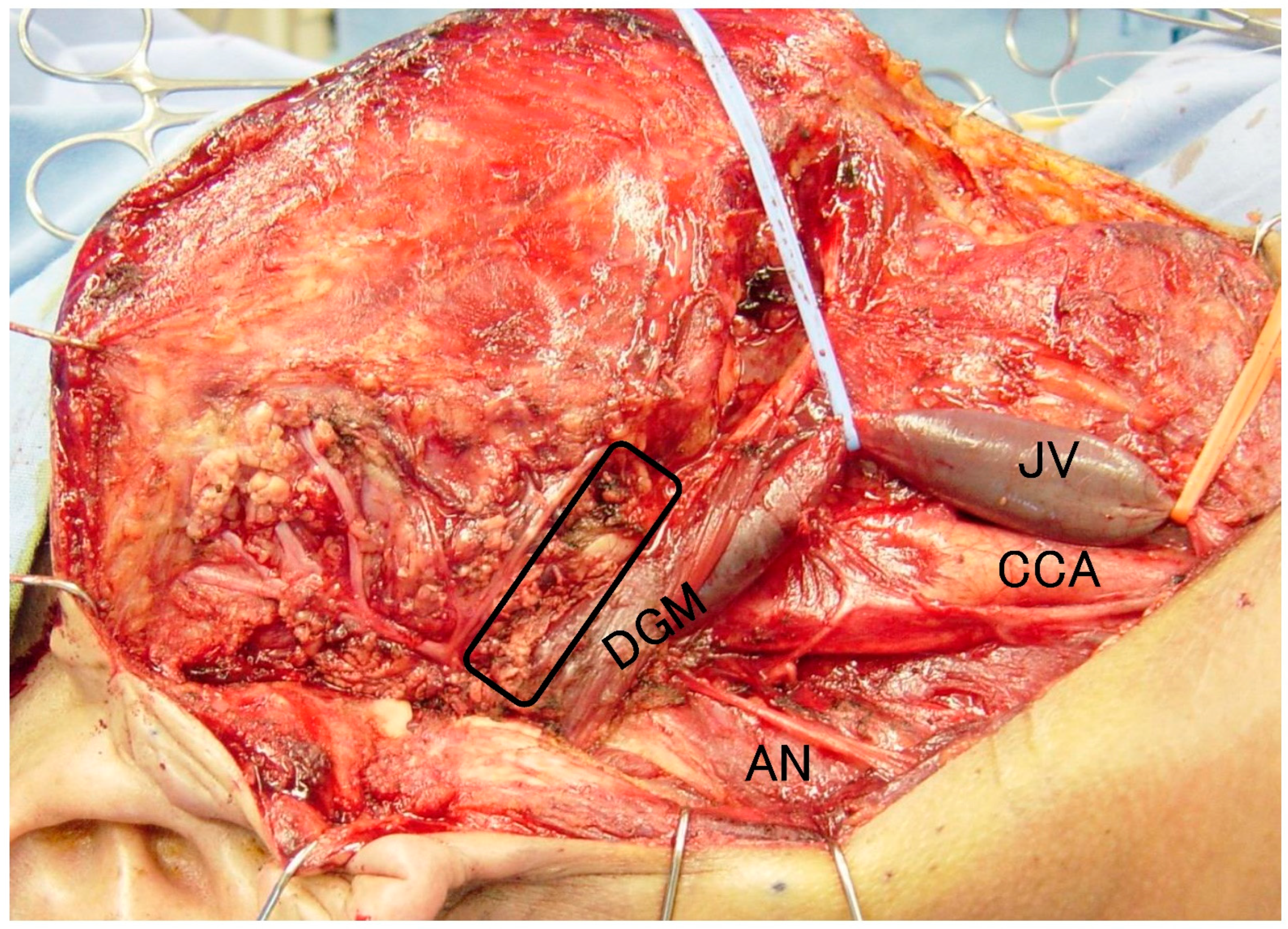
10.3. Surgical Technique
11. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
References
- Holsinger, F.C.; Bui, D.T. Anatomy, function, and evaluation of the salivary glands. In Salivary Gland Disorders; Myers, E.N., Ferris, R.L., Eds.; Springer: Berlin/Heidelberg, Germany, 2007; pp. 1–16. [Google Scholar]
- Som, P.M.; Miletich, I. The embryology of the salivary glands: An update. Neurographics 2015, 5, 167–177. [Google Scholar] [CrossRef]
- Boahene, D.K.; Olsen, K.D.; Lewis, J.E.; Pinheiro, A.D.; Pankratz, V.S.; Bagniewski, S.M. Mucoepidermoid carcinoma of the parotid gland: The Mayo clinic experience. Arch. Otolaryngol. Head Neck Surg. 2004, 130, 849–856. [Google Scholar] [CrossRef] [Green Version]
- Klussmann, J.P.; Ponert, T.; Mueller, R.P.; Dienes, H.P.; Guntinas-Lichius, O. Patterns of lymph node spread and its influence on outcome in resectable parotid cancer. Eur. J. Surg. Oncol. 2008, 34, 932–937. [Google Scholar] [CrossRef]
- Lim, C.M.; Gilbert, M.R.; Johnson, J.T.; Kim, S. Clinical significance of intra-parotid lymph node metastasis in primary parotid cancer. Head Neck 2014, 36, 1634–1637. [Google Scholar] [CrossRef]
- Feng, Y.; Liu, F.; Cheng, G.; Fang, Q.; Niu, X.; He, W. Significance of intra-parotid node metastasis in predicting local control in primary parotid cancer. Laryngoscope 2019, 129, 2309–2312. [Google Scholar] [CrossRef] [PubMed]
- Neisse, R. Über den Einschluss von Parotislappchen in Lymphknoten. Anat. Hefte 1898, 10, 287–306. [Google Scholar] [CrossRef]
- Marks, N.J. The anatomy of the lymph nodes of the parotid gland. Clin. Otolaryngol. Allied Sci. 1984, 9, 271–275. [Google Scholar] [CrossRef] [PubMed]
- McKean, M.E.; Lee, K.; McGregor, I.A. The distribution of lymph nodes in and around the parotid gland: An anatomical study. Br. J. Plast. Surg. 1985, 38, 1–5. [Google Scholar] [CrossRef]
- Garatea-Crelgo, J.; Gay-Escoda, C.; Bermejo, B.; Buenechea-Imaz, R. Morphological study of the parotid lymph nodes. J. Cranio-Maxillofac. Surg. 1993, 21, 207–209. [Google Scholar] [CrossRef]
- Sönmez Ergün, S.; Gayretli, O.; Büyükpınarbaşılı, N.; Yıldız, K.; Gürses, I.A.; Avşar, A.; Cavlak, M. Determining the number of intra-parotid lymph nodes: Postmortem examination. J. Cranio-Maxillofac. Surg. 2014, 42, 657–660. [Google Scholar] [CrossRef]
- Sönmez, S.; Orhan, K.S.; Kara, E.; Büyük, M.; Aydemir, L.; Asliyüksek, H. Determining the number and distribution of intra-parotid lymph nodes according to parotidectomy classification of European Salivary Gland Society: Cadaveric study. Head Neck 2020, 42, 3685–3692. [Google Scholar] [CrossRef] [PubMed]
- Quer, M.; Guntinas-Lichius, O.; Marchal, F.; Vander Poorten, V.; Chevalier, D.; León, X.; Eisele, D.; Dulguerov, P. Classification of parotidectomies: A proposal of the European Salivary Gland Society. Eur. Arch. Otorhinolaryngol. 2016, 273, 3307–3312. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.K.; Shetty, S. Classification of parotidectomy: A proposed modification to the European Salivary Gland Society classification system. Eur. Arch. Otorhinolaryngol. 2017, 274, 3175–3181. [Google Scholar] [CrossRef] [PubMed]
- Guntinas-Lichius, O.; Thielker, J.; Robbins, K.T.; Olsen, K.D.; Shaha, A.R.; Mäkitie, A.A.; de Bree, R.; Vander Poorten, V.; Quer, M.; Rinaldo, A.; et al. Prognostic role of intra-parotid lymph node metastasis in primary parotid cancer: Systematic review. Head Neck 2021, 43, 997–1008. [Google Scholar] [CrossRef]
- Schneider, S.; Kotowski, U.; Kadletz, L.; Brunner, M.; Stanisz, I.; Heiduschka, G.; Lill, C. Intra-parotid and cervical lymph nodes metastasis in primary parotid gland carcinoma-impact on clinical outcome. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 129, 570–574. [Google Scholar] [CrossRef]
- Seng, D.; Fang, Q.; Liu, F.; Luo, R.; Liu, S. Intra-parotid lymph node metastasis decreases survival in pediatric patients with parotid cancer. J. Oral Maxillofac. Surg. 2020, 78, e1–e852. [Google Scholar] [CrossRef]
- Wu, J.; Fang, Q.; Liu, F.; Zhang, X. Intra-parotid node metastases in adults with parotid mucoepidermoid cancer: An indicator of prognosis? Br. J. Oral Maxillofac. Surg. 2020, 58, 525–529. [Google Scholar] [CrossRef]
- Niu, X.; Fang, Q.; Liu, F. Role of intra-parotid node metastasis in mucoepidermoid carcinoma of the parotid gland. BMC Cancer. 2019, 19, 417. [Google Scholar] [CrossRef]
- Nisa, L.; Salmina, C.; Dettmer, M.S.; Arnold, A.; Aebersold, D.M.; Borner, U.; Giger, R. Implications of intraglandular lymph node metastases in primary carcinomas of the parotid gland. Laryngoscope 2015, 125, 2099–2106. [Google Scholar] [CrossRef]
- Walvekar, R.R.; Filho, P.A.A.; Seethala, R.R.; Gooding, W.E.; Heron, D.E.; Johnson, J.T.; Ferris, R.L. Clinicopathologic features as stronger prognostic factors than histology or grade in risk stratification of primary parotid malignancies. Head Neck 2011, 33, 225–231. [Google Scholar] [CrossRef]
- Lee, D.Y.; Park, M.W.; Oh, K.H.; Cho, J.G.; Kwon, S.Y.; Woo, J.S.; Jung, K.Y.; Baek, S.K. Clinicopathologic factors associated with recurrence in low- and high-grade parotid cancers. Head Neck 2016, 38 (Suppl. 1), E1788–E1793. [Google Scholar] [CrossRef] [PubMed]
- Ellis, M.A.; Graboyes, E.M.; Day, T.A.; Neskey, D.M. Prognostic factors and occult nodal disease in mucoepidermoid carcinoma of the oral cavity and oropharynx: An analysis of the National Cancer Database. Oral Oncol. 2017, 72, 174–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shang, X.; Fang, Q.; Liu, F.; Wu, J.; Luo, R.; Qi, J. Deep Parotid Lymph Node Metastasis Is Associated With Recurrence in High-Grade Mucoepidermoid Carcinoma of the Parotid Gland. J. Oral Maxillofac. Surg. 2019, 77, 1505–1509. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef]
- O’Brien, C.J.; McNeil, E.B.; McMahon, J.D.; Pathak, I.; Lauer, C.S.; Jackson, M.A. Significance of clinical stage, extent of surgery, and pathologic findings in metastatic cutaneous squamous carcinoma of the parotid gland. Head Neck 2002, 24, 417–422. [Google Scholar] [CrossRef]
- Erovic, B.M.; Shah, M.D.; Bruch, G.; Johnston, M.; Kim, J.; O’Sullivan, B.; Perez-Ordonez, B.; Weinreb, I.; Atenafu, E.G.; de Almeida, J.R.; et al. Outcome analysis of 215 patients with parotid gland tumors: A retrospective cohort analysis. J. Otolaryngol. Head Neck Surg. 2015, 44, 43. [Google Scholar] [CrossRef] [Green Version]
- Lau, V.H.; Aouad, R.; Farwell, D.G.; Donald, P.J.; Chen, A.M. Patterns of nodal involvement for clinically N0 salivary gland carcinoma: Refining the role of elective neck irradiation. Head Neck 2014, 36, 1435–1439. [Google Scholar] [CrossRef]
- Shi, S.; Fang, Q.; Liu, F.; Zhong, M.; Sun, C. Prognostic factors and survival rates for parotid duct carcinoma patients. J. Craniomaxillofac. Surg. 2014, 42, 1929–1931. [Google Scholar] [CrossRef]
- Cheng, G.; Liu, F.; Niu, X.; Fang, Q. Role of the pretreatment neutrophil-to-lymphocyte ratio in the survival of primary parotid cancer patients. Cancer Manag. Res. 2019, 11, 2281–2286. [Google Scholar] [CrossRef] [Green Version]
- Seethala, R.R.; Altemani, A.; Ferris, R.L.; Fonseca, I.; Gnepp, D.R.; Ha, P.; Nagao, T.; Skalova, A.; Stenman, G.; Thompson, L.D.R. Data set for the reporting of carcinomas of the major salivary glands: Explanations and Recommendations of the Guidelines from the International Collaboration on Cancer Reporting. Arch. Pathol. Lab. Med. 2019, 143, 578–586. [Google Scholar] [CrossRef]
- Sood, S.; McGurk, M.; Vaz, F. Management of salivary gland tumours: United Kingdom National Multidisciplinary Guidelines. J. Laryngol. Otol. 2016, 130, S142–S149. [Google Scholar] [CrossRef] [PubMed]
- Olsen, K.D.; Quer, M.; de Bree, R.; Vander Poorten, V.; Rinaldo, A.; Ferlito, A. Deep lobe parotidectomy-why, when, and how? Eur. Arch. Otorhinolaryngol. 2017, 274, 4073–4078. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stenner, M.; Molls, C.; Luers, J.C.; Beutner, D.; Klussmann, J.P.; Huettenbrink, K.B. Occurrence of lymph node metastasis in early-stage parotid gland cancer. Eur. Arch. Otorhinolaryngol. 2012, 269, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Poorten, V.V.; Hart, A.; Vauterin, T.; Jeunen, G.; Schoenaers, J.; Hamoir, M.; Balm, A.; Stennert, E.; Guntinas-Lichius, O.; Delaere, P. Prognostic index for patients with parotid carcinoma: International external validation in a Belgian-German database. Cancer 2009, 115, 540–550. [Google Scholar] [CrossRef] [PubMed]
- Terhaard, C.H.; Lubsen, H.; Van der Tweel, I.; Hilgers, F.J.; Eijkenboom, W.M.; Marres, H.A.; Tjho-Heslinga, R.E.; de Jong, J.M.; Roodenburg, J.L. Dutch Head and Neck Oncology Cooperative Group. Salivary gland carcinoma: Independent prognostic factors for locoregional control, distant metastases, and overall survival: Results of the Dutch head and neck oncology cooperative group. Head Neck 2004, 26, 681–692; discussion 692–693. [Google Scholar] [CrossRef] [PubMed]
- Carrillo, J.F.; Vázquez, R.; Ramírez-Ortega, M.C.; Cano, A.; Ochoa-Carrillo, F.J.; Oñate-Ocaña, L.F. Multivariate prediction of the probability of recurrence in patients with carcinoma of the parotid gland. Cancer 2007, 109, 2043–2051. [Google Scholar] [CrossRef]
- Kouka, M.; Koehler, B.; Buentzel, J.; Kaftan, H.; Boeger, D.; Mueller, A.H.; Wittig, A.; Schultze-Mosgau, S.; Ernst, T.; Schlattmann, P.; et al. Role of Intraparotid and Neck Lymph Node Metastasis in Primary Parotid Cancer Surgery: A Population-Based Analysis. Cancers 2022, 14, 2822. [Google Scholar] [CrossRef]
- Li, C.; Matthies, L.; Hou, X.; Knipfer, C.; Gosau, M.; Friedrich, R.E. A meta-analysis of the pros and cons of partial superficial parotidectomy versus superficial parotidectomy for the treatment of benign parotid neoplasms. J. Craniomaxillofac. Surg. 2020, 48, 590–598. [Google Scholar] [CrossRef]
- Stathopoulos, P.; Igoumenakis, D.; Smith, W.P. Partial Superficial, Superficial, and Total Parotidectomy in the Management of Benign Parotid Gland Tumors: A 10-Year Prospective Study of 205 Patients. J. Oral Maxillofac. Surg. 2018, 76, 455–459. [Google Scholar] [CrossRef]
- Ichihara, T.; Kawata, R.; Higashino, M.; Terada, T.; Haginomori, S. A more appropriate clinical classification of benign parotid tumors: Investigation of 425 cases. Acta Otolaryngol. 2014, 134, 1185–1191. [Google Scholar] [CrossRef]
- Kawata, R.; Kinoshita, I.; Omura, S.; Higashino, M.; Nishikawa, S.; Terada, T.; Haginomori, S.-I.; Kurisu, Y.; Hirose, Y.; Tochizawa, T. Risk Factors of Postoperative Facial Palsy for Benign Parotid Tumors: Outcome of 1018 Patients. Layngoscope 2021, 131, E2857–E2864. [Google Scholar] [CrossRef] [PubMed]
| Intra-Parotid Lymph Nodes |
|---|
| Known facts |
|
| Need to know and consider |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Terada, T.; Kawata, R. Role of Intra-Parotid Lymph Node Metastasis in Primary Parotid Carcinoma. Life 2022, 12, 2053. https://doi.org/10.3390/life12122053
Terada T, Kawata R. Role of Intra-Parotid Lymph Node Metastasis in Primary Parotid Carcinoma. Life. 2022; 12(12):2053. https://doi.org/10.3390/life12122053
Chicago/Turabian StyleTerada, Tetsuya, and Ryo Kawata. 2022. "Role of Intra-Parotid Lymph Node Metastasis in Primary Parotid Carcinoma" Life 12, no. 12: 2053. https://doi.org/10.3390/life12122053
APA StyleTerada, T., & Kawata, R. (2022). Role of Intra-Parotid Lymph Node Metastasis in Primary Parotid Carcinoma. Life, 12(12), 2053. https://doi.org/10.3390/life12122053






