Homologous Use of Allogeneic Umbilical Cord Tissue to Reduce Knee Pain and Improve Knee Function
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. VAS Scores with Activity
- Mean VAS scores with activity at baseline were statistically different (higher) than the mean VAS scores with activity for every post-injection time interval;
- The p-value for the ANOVA for VAS scores with activity was 1.18 × 10−15;
- Overall, there was a decrease in the mean for VAS with activity scores after the injection.
3.2. VAS Scores at Rest
- Mean VAS scores at rest were statistically different (higher) than the mean VAS scores at rest for every time interval;
- The p-value for the ANOVA for VAS scores at rest was 0.000561;
- Overall, there was a decrease in the mean for VAS at rest scores after the injection.
- 30% (n = 9) of the patients studied never took medication throughout the course of the study period;
- 13.3% (n = 4) of the patients studied continued to take medications throughout the entire course of the study period;
- 20% (n = 6) of the patients studied went from daily medication use to no medication use by the end of the study period;
- 13.3% (n = 4) of the patients studied reduced their medication frequency from daily to occasional by the end of the study period;
- 13.3% (n = 4) of the patients studied reduced their medication frequency from occasional to none by the end of the study period;
- One person went from using no medications to using CBD oil on the knee at the end of the study period. Although that patient had decreasing WOMAC and VAS at rest scores throughout the study period, their VAS with activity score did not change significantly throughout the study period (VAS range: 3–4);
- One person went from using no medications to occasionally using acetaminophen at the end of the study. This patient’s VAS and WOMAC scores remained consistent throughout the study;
- One person went from using no medications to using acetaminophen or ibuprofen daily. This person’s VAS and WOMAC scores initially decreased after the injection, but increased back up over time to pre-injection scores;
- The number of patients using opioids decreased by 16.7% from pre-injection to 24-week follow-ups, and the number of patients using NSAID decreased by 46.1% from pre-injection to 24 weeks follow.
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

References
- Wallace, I.J.; Worthington, S.; Felson, D.T.; Jurmain, R.D.; Wren, K.T.; Maijanen, H.; Woods, R.J.; Lieberman, D.E. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc. Natl. Acad. Sci. USA 2017, 114, 9332–9336. Available online: www.pnas.org/content/114/35/9332 (accessed on 23 February 2021). [CrossRef] [Green Version]
- Arthritis-Related Disabilities and Limitations. Available online: www.cdc.gov/arthritis/data_statistics/disabilities-limitations.htm (accessed on 23 February 2021).
- Arthritis-Related Statistics. Available online: www.cdc.gov/arthritis/data_statistics/arthritis-related-stats.htm (accessed on 23 February 2021).
- Michaud, C.M.; McKenna, M.T.; Begg, S.; Tomijima, N.; Majmudar, M.; Bulzacchelli, M.T.; Ebrahim, S.E.; Ezzati, M.; Salomon, J.A.; Kreiser, J.G.; et al. The burden of disease and injury in the United States 1996. Popul. Health Metr. 2006, 4, 11. Available online: http://pophealthmetrics.biomedcentral.com/articles/10.1186/1478-7954-4-11 (accessed on 23 February 2021). [CrossRef] [PubMed] [Green Version]
- Fukutani, N.; Iijima, H.; Aoyama, T.; Yamamoto, Y.; Hiraoka, M.; Miyanobu, K.; Jinnouchi, M.; Kaneda, E.; Tsuboyama, T.; Matsuda, S. Knee Pain during Activities of Daily Living and Its Relationship with Physical Activity in Patients with Early and Severe Knee Osteoarthritis. Clinical Rheumatology; U.S. National Library of Medicine: Bethesda, MA, USA, 2016. Available online: Pubmed.ncbi.nlm.nih.gov/27041381/ (accessed on 23 February 2021).
- Goldring, M.B.; Otero, M. Inflammation in osteoarthritis. Curr. Opin. Rheumatol. 2011, 23, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Murphy, L.; Helmick, C.G. The impact of osteoarthritis in the United States: A population-health perspective. Am. J. Nurs. 2012, 112 (Suppl. 1), S13–S19. [Google Scholar] [CrossRef] [PubMed]
- Hochberg, M.C.; Cisternas, M.G.; Watkins-Castillo, S.I. Osteoarthritis. BMUS: The Burden of Musculoskeletal Diseases in the United States. Available online: www.boneandjointburden.org/fourth-edition/iiib10/osteoarthritis (accessed on 27 March 2021).
- Find Help: ATOD. SAMHSA. Available online: https://www.samhsa.gov/find-help/atod (accessed on 23 February 2021).
- Understanding the Epidemic. Available online: www.cdc.gov/drugoverdose/epidemic/index.html (accessed on 17 March 2021).
- Lanas, A.; Perez-Aisa, M.A.; Feu, F.; Ponce, J.; Saperas, E.; Santolaria, S.; Rodrigo, L.; Balanzo, J.; Bajador, E.; Almela, P.; et al. A nationwide study of mortality associated with hospital admission due to severe gastrointestinal events and those associated with nonsteroidal antiinflammatory drug use. Am. J. Gastroenterol. 2005, 100, 1685–1693. Available online: Pubmed.ncbi.nlm.nih.gov/16086703/ (accessed on 23 February 2021). [CrossRef] [PubMed]
- Weigard, T.J.; Vernetti, C.M. Nonsteroidal Anti-inflammatory Drug (NSAID) Toxicity. 2020. Available online: http://emedicine.medscape.com/article/816117-overview (accessed on 10 July 2021).
- Datta, A.; Flynn, N.R.; Barnette, D.A.; Woeltje, K.F.; Miller, G.P.; Swamidass, S.J. Machine Learning Liver-Injuring Drug Interactions with Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) from a retrospective electronic health record (EHR) cohort. PLoS Comput. Biol. 2021, 17, e1009053. Available online: https://journals.plos.org/ploscompbiol/article?id=10.1371%2Fjournal.pcbi.1009053 (accessed on 24 January 2022). [CrossRef] [PubMed]
- Epidural Corticosteroid Injections. Johns Hopkins Medicine. Available online: www.hopkinsmedicine.org/health/conditions-and-diseases/epidural-corticosteroid-injections (accessed on 23 February 2021).
- RA Medications: What Are Disease Modifying Antirheumatic Drugs? Available online: https://www.rheumatoidarthritis.org/treatment/medications/dmards/ (accessed on 10 July 2021).
- Viscosupplementation for Knee Osteoarthritis. Cleveland Clinic. Available online: https://my.clevelandclinic.org/health/articles/14982-viscosupplementation-for-osteoarthritis-of-the-knee (accessed on 27 January 2022).
- Arutyunyan, I.; Fatkhudinov, T.; Sukhikh, G. Umbilical cord tissue cryopreservation: A short review. Stem Cell Res. Ther. 2018, 9, 236. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.E.; Walker, J.T.; Keating, A. Concise review: Wharton’s jelly: The rich, but enigmatic, source of mesenchymal stromal cells. Stem Cells Transl. Med. 2017, 6, 1620–1630. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; El-Amin, S.F., III; Levy, H.J.; Sze-Tu, R.; Ibim, S.E.; Mafulli, N. Umbilical cord-derived Wharton’s jelly for regenerative medicine applications. J. Orthop. Surg. Res. 2020, 15, 49. Available online: Josr-online.biomedcentral.com/articles/10.1186/s13018-020-1553-7 (accessed on 23 February 2021). [CrossRef] [PubMed] [Green Version]
- Fernandes, J.C.; Martel-Pelletier, J.; Pelletier, J.P. The role of cytokines in osteoarthritis pathophysiology. Biorheology 2002, 39, 237–246. [Google Scholar] [PubMed]
- Frisbie, D.D.; Ghivizzani, S.C.; Robbins, P.D.; Evans, C.H.; McIlwraith, C.W. Treatment of experimental equine osteoarthritis by in vivo delivery of the equine interleukin-1 receptor antagonist gene. Gene Ther. 2002, 9, 12–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heusinkveld, M.; de Vos van Steenwijk, P.J.; Goedemans, R.; Ramwadhdoebe, T.H.; Gorter, A.; Welters, M.J.P.; van Hall, T.; van der Burg, S.H. M2 macrophages induced by prostaglandin E2 and Il-6 from cervical carcinoma are switched to activated M1 macrophages by CD4+ Th1 cells. J. Immunol. 2011, 187, 1157–1165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Acevedo, P. Successful treatment of painful chronic wounds with amniotic and umbilical cord tissue: A case series. In SAGE Open Medical Case Reports; U.S. National Library of Medicine: Bethesda, MA, USA, 2020. Available online: Pubmed.ncbi.nlm.nih.gov/32477550/ (accessed on 20 March 2021).
- Ackley, J.F.; Kolosky, M.; Gurin, D.; Hampton, R.; Masin, R.; Krahe, D. Cryopreserved amniotic membrane and umbilical cord particulate matrix for partial rotator cuff tears: A case series. Medicine 2019, 98, e16569. Available online: https://europepmc.org/article/MED/31348285#free-full-text (accessed on 20 March 2021). [CrossRef] [PubMed]
- DeMill, S.L.; Granata, J.D.; McAlister, J.E.; Berlet, G.C.; Hyer, C.F. Safety analysis of cryopreserved amniotic membrane/umbilical cord tissue in foot and ankle surgery: A consecutive case series of 124 patients. Surg. Technol. Int. 2014, 25, 257–261. [Google Scholar] [PubMed]
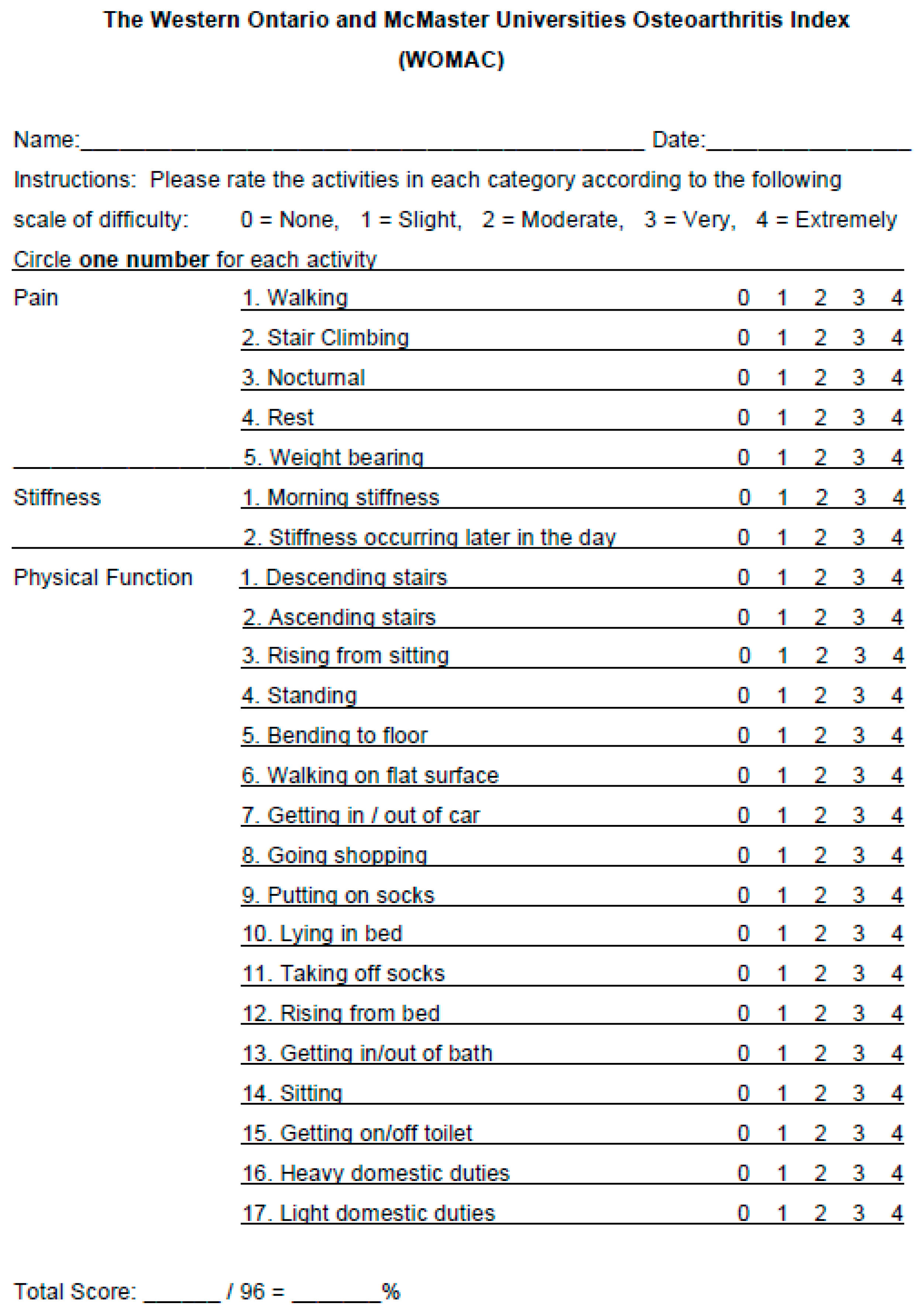
- Woolacott, N.F.; Corbett, M.S.; Rice, S.J.C. The use and reporting of WOMAC in the assessment of the benefit of physical therapies for the pain of osteoarthritis of the knee: Findings from a systematic review of clinical trials. Rheumatology 2012, 51, 1440–1446. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Age (Years) | Overall | Female | Male |
|---|---|---|---|
| Sample Size | 30 | 19 | 11 |
| Mean Age | 63 | 64.2 | 61 |
| Min Age | 36 | 36 | 49 |
| Max Age | 84 | 84 | 78 |
| Std. Dev | 10.94 | 12.10 | 8.75 |
| Injection Site | Overall | Female | Male |
|---|---|---|---|
| Sample Size | 30 | 19 | 11 |
| Right Knee | 20 | 12 | 8 |
| Left Knee | 10 | 7 | 3 |
| BMI | Overall | Female | Male |
|---|---|---|---|
| Sample Size | 30 | 19 | 11 |
| Mean BMI | 29.2 | 26.9 | 33.1 |
| Min BMI | 18.0 | 18.0 | 23.8 |
| Max BMI | 50.2 | 39.3 | 50.2 |
| Std. Dev. | 6.97 | 5.54 | 7.71 |
| Source | Sum of Squares | df | Mean Square | F-Value | p-Value | |
|---|---|---|---|---|---|---|
| Model | 7.86 | 1 | 7.86 | 1.71 | 0.1927 | Not significant |
| A-Time (Days) | 7.86 | 1 | 7.86 | 1.71 | 0.1927 | |
| Residual | 818.42 | 178 | 4.60 | |||
| Lack of Fit | 7.03 | 4 | 1.76 | 0.3770 | 0.8249 | Not significant |
| Pure Error | 811.38 | 174 | 4.66 | |||
| Cor Total | 826.28 | 179 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Timmons, R.B.; Sugaya, K.; Bane, L.D. Homologous Use of Allogeneic Umbilical Cord Tissue to Reduce Knee Pain and Improve Knee Function. Life 2022, 12, 260. https://doi.org/10.3390/life12020260
Timmons RB, Sugaya K, Bane LD. Homologous Use of Allogeneic Umbilical Cord Tissue to Reduce Knee Pain and Improve Knee Function. Life. 2022; 12(2):260. https://doi.org/10.3390/life12020260
Chicago/Turabian StyleTimmons, Ruben Berrocal, Kiminobu Sugaya, and Lori Deneke Bane. 2022. "Homologous Use of Allogeneic Umbilical Cord Tissue to Reduce Knee Pain and Improve Knee Function" Life 12, no. 2: 260. https://doi.org/10.3390/life12020260






