In Stent Neo-Atherosclerosis: Pathophysiology, Clinical Implications, Prevention, and Therapeutic Approaches
Abstract
:1. Introduction
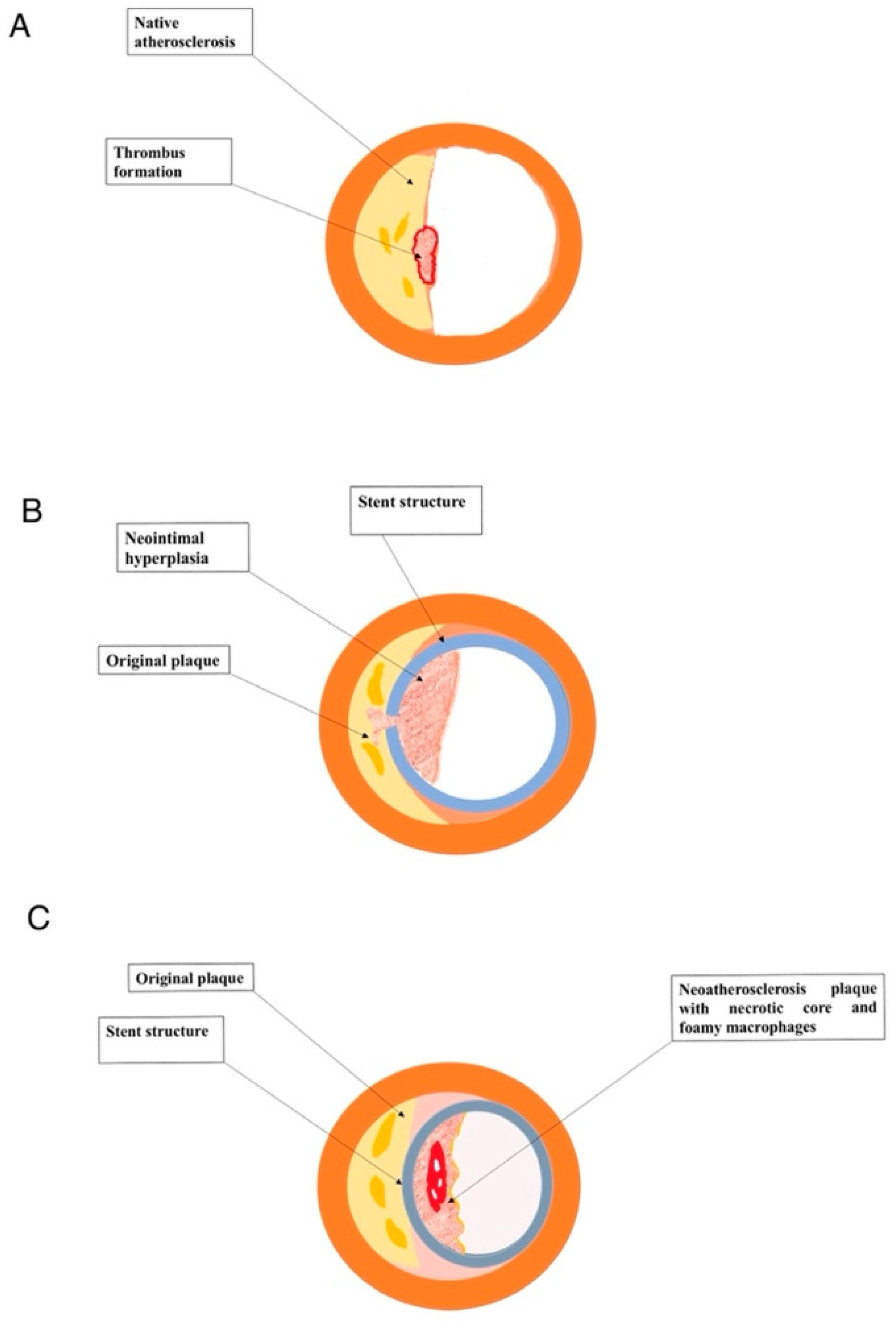
2. Pathophysiology of Native Atherosclerosis, In-Stent Restenosis and Neo-Atherosclerosis
3. Clinical Impact of Neo-Atherosclerosis
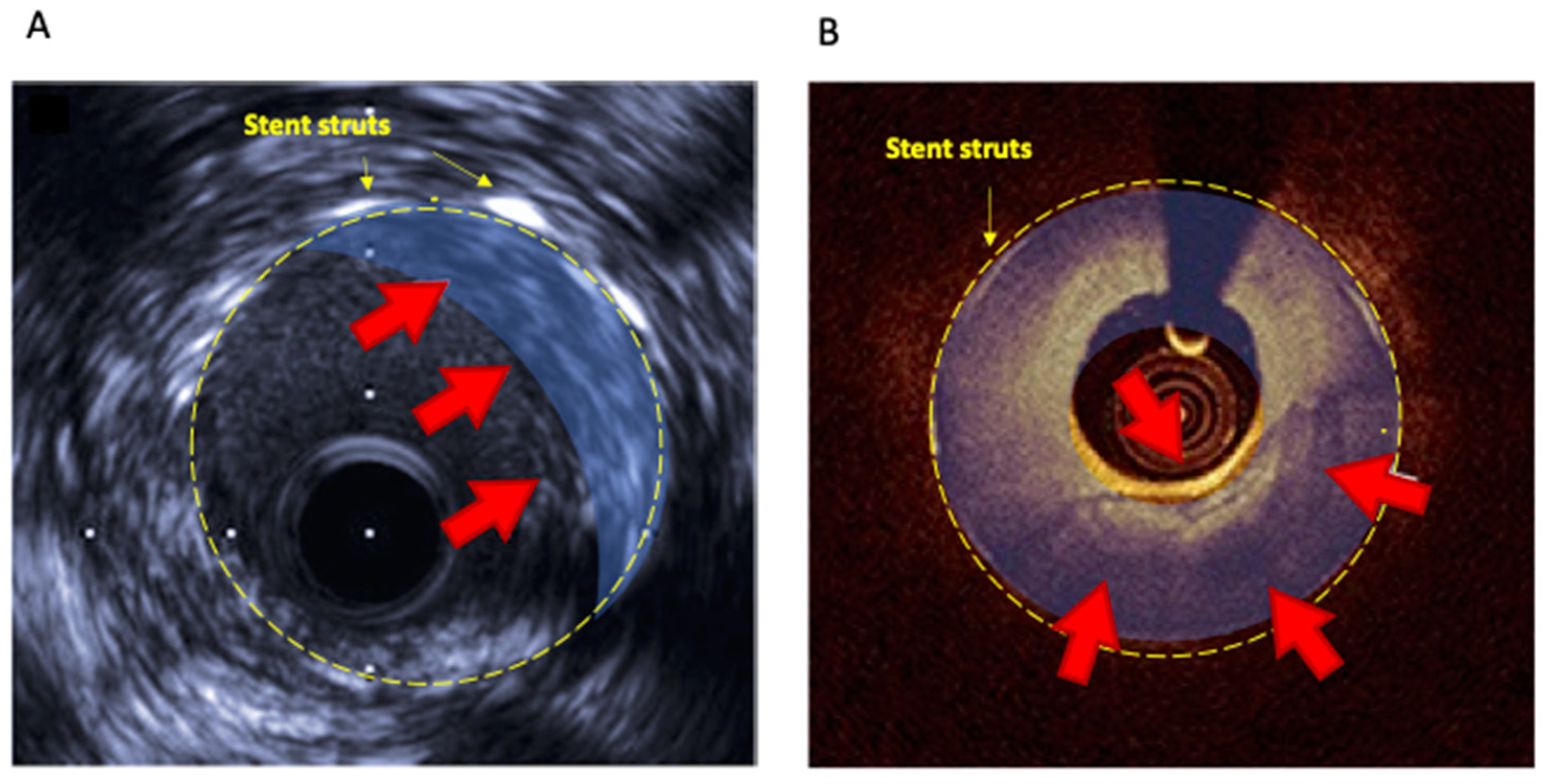
4. In-Stent Restenosis and Neo-Atherosclerosis: The Pivotal Role of Intra-Coronary Imaging
4.1. Intravascular Ultrasound (IVUS)
4.2. Optical Coherence Tomography (OCT)
5. Prevention and Treatment of Neo-Atherosclerosis
5.1. Pharmacological Strategies
5.1.1. Lipid-Lowering Therapy
5.1.2. Antiplatelet Therapies
5.1.3. Targeting Inflammation and Oxidative Pathways
5.2. Device-Based Strategies
5.2.1. Drug-Eluting Balloons and Repeat Drug-Eluting Stent Implantation
5.2.2. Debulking Strategies
5.2.3. Bioresorbable Vascular Scaffolds
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Yahagi, K.; Kolodgie, F.D.; Otsuka, F.; Finn, A.V.; Davis, H.R.; Joner, M.; Virmani, R. Pathophysiology of native coronary, vein graft, and in-stent atherosclerosis. Nat. Rev. Cardiol. 2016, 13, 79–98. [Google Scholar] [CrossRef] [PubMed]
- Lespérance, J.; Bourassa, M.G.; Schwartz, L.; Hudon, G.; Laurier, J.; Eastwood, C.; Kazim, F. Definition and measurement of restenosis after successful coronary angioplasty: Implications for clinical trials. Am. Heart J. 1993, 125, 1394–1408. [Google Scholar] [CrossRef]
- Komatsu, R.; Ueda, M.; Naruko, T.; Kojima, A.; Becker, A.E. Neointimal tissue response at sites of coronary stenting in humans: Macroscopic, histological, and immunohistochemical analyses. Circulation 1998, 98, 224–233. [Google Scholar] [CrossRef] [Green Version]
- Nakazawa, G.; Otsuka, F.; Nakano, M.; Vorpahl, M.; Yazdani, S.K.; Ladich, E.; Kolodgie, F.D.; Finn, A.V.; Virmani, R. The pathology of neoatherosclerosis in human coronary implants bare-metal and drug-eluting stents. J. Am. Coll. Cardiol. 2011, 57, 1314–1322. [Google Scholar] [CrossRef] [Green Version]
- Spadaccio, C.; Antoniades, C.; Nenna, A.; Chung, C.; Will, R.; Chello, M.; Gaudino, M.F.L. Preventing treatment failures in coronary artery disease: What can we learn from the biology of in-stent restenosis, vein graft failure, and internal thoracic arteries? Cardiovasc. Res. 2020, 116, 505–519. [Google Scholar] [CrossRef]
- Piccirillo, F.; Carpenito, M.; Verolino, G.; Chello, C.; Nusca, A.; Lusini, M.; Spadaccio, C.; Nappi, F.; Di Sciascio, G.; Nenna, A. Changes of the coronary arteries and cardiac microvasculature with aging: Implications for translational research and clinical practice. Mech. Ageing Dev. 2019, 184, 111161. [Google Scholar] [CrossRef]
- Nakashima, Y.; Chen, Y.X.; Kinukawa, N.; Sueishi, K. Distributions of diffuse intimal thickening in human arteries: Preferential expression in atherosclerosis-prone arteries from an early age. Virchows Arch. 2002, 441, 279–288. [Google Scholar] [CrossRef]
- Yahagi, K.; Zarpak, R.; Sakakura, K.; Otsuka, F.; Kutys, R.; Ladich, E.; Fowler, D.R.; Joner, M.; Virmani, R. Multiple simultaneous plaque erosion in 3 coronary arteries. JACC Cardiovasc. Imaging 2014, 7, 1172–1174. [Google Scholar] [CrossRef] [Green Version]
- Kolodgie, F.D.; Burke, A.P.; Farb, A.; Weber, D.K.; Kutys, R.; Wight, T.N.; Virmani, R. Differential accumulation of proteoglycans and hyaluronan in culprit lesions: Insights into plaque erosion. Arterioscler. Thromb. Vasc. Biol. 2002, 22, 1642–1648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otsuka, F.; Byrne, R.A.; Yahagi, K.; Mori, H.; Ladich, E.; Fowler, D.R.; Kutys, R.; Xhepa, E.; Kastrati, A.; Virmani, R.; et al. Neoatherosclerosis: Overview of histopathologic findings and implications for intravascular imaging assessment. Eur. Heart J. 2015, 36, 2147–2159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otsuka, F.; Sakakura, K.; Yahagi, K.; Joner, M.; Virmani, R. Has our understanding of calcification in human coronary atherosclerosis progressed? Arterioscler. Thromb. Vasc. Biol. 2014, 34, 724–736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ando, H.; Amano, T.; Takashima, H.; Harada, K.; Kitagawa, K.; Suzuki, A.; Kunimura, A.; Shimbo, Y.; Harada, K.; Yoshida, T.; et al. Differences in tissue characterization of restenotic neointima between sirolimus-eluting stent and bare-metal stent: Integrated backscatter intravascular ultrasound analysis for in-stent restenosis. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 996–1001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakazawa, G.; Nakano, M.; Otsuka, F.; Wilcox, J.N.; Melder, R.; Pruitt, S.; Kolodgie, F.D.; Virmani, R. Evaluation of polymer-based comparator drug-eluting stents using a rabbit model of iliac artery atherosclerosis. Circ. Cardiovasc. Interv. 2011, 4, 38–46. [Google Scholar] [CrossRef] [Green Version]
- Nakazawa, G.; Torii, S.; Ijichi, T.; Nagamatsu, H.; Ohno, Y.; Kurata, F.; Yoshikawa, A.; Nakano, M.; Shinozaki, N.; Yoshimachi, F.; et al. Comparison of Vascular Responses Following New-Generation Biodegradable and Durable Polymer-Based Drug-Eluting Stent Implantation in an Atherosclerotic Rabbit Iliac Artery Model. J. Am. Heart Assoc. 2016, 5, e003803. [Google Scholar] [CrossRef] [Green Version]
- Hasegawa, K.; Tamai, H.; Kyo, E.; Kosuga, K.; Ikeguchi, S.; Hata, T.; Okada, M.; Fujita, S.; Tsuji, T.; Takeda, S.; et al. Histopathological findings of new in-stent lesions developed beyond five years. Catheter. Cardiovasc. Interv. 2006, 68, 554–558. [Google Scholar] [CrossRef]
- Chaabane, C.; Otsuka, F.; Virmani, R.; Bochaton-Piallat, M.L. Biological responses in stented arteries. Cardiovasc. Res. 2013, 99, 353–363. [Google Scholar] [CrossRef]
- Davies, P.F. Hemodynamic shear stress and the endothelium in cardiovascular pathophysiology. Nat. Clin. Pract. Cardiovasc. Med. 2009, 6, 16–26. [Google Scholar] [CrossRef] [Green Version]
- Nakano, M.; Otsuka, F.; Yahagi, K.; Sakakura, K.; Kutys, R.; Ladich, E.R.; Finn, A.V.; Kolodgie, F.D.; Virmani, R. Human autopsy study of drug-eluting stents restenosis: Histomorphological predictors and neointimal characteristics. Eur. Heart J. 2013, 34, 3304–3313. [Google Scholar] [CrossRef] [Green Version]
- Nakazawa, G.; Finn, A.V.; Vorpahl, M.; Ladich, E.R.; Kolodgie, F.D.; Virmani, R. Coronary responses and differential mechanisms of late stent thrombosis attributed to first-generation sirolimus- and paclitaxel-eluting stents. J. Am. Coll. Cardiol. 2011, 57, 390–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoshino, M.; Yonetsu, T.; Kanaji, Y.; Usui, E.; Yamaguchi, M.; Hada, M.; Hamaya, R.; Kanno, Y.; Murai, T.; Lee, T.; et al. Impact of baseline plaque characteristic on the development of neoatherosclerosis in the very late phase after stenting. J. Cardiol. 2019, 74, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Kang, S.J.; Virmani, R.; Nakano, M.; Ueda, Y. In-stent neoatherosclerosis: A final common pathway of late stent failure. J. Am. Coll. Cardiol. 2012, 59, 2051–2057. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joner, M.; Finn, A.V.; Farb, A.; Mont, E.K.; Kolodgie, F.D.; Ladich, E.; Kutys, R.; Skorija, K.; Gold, H.K.; Virmani, R. Pathology of drug-eluting stents in humans: Delayed healing and late thrombotic risk. J. Am. Coll. Cardiol. 2006, 48, 193–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuramitsu, S.; Sonoda, S.; Ando, K.; Otake, H.; Natsuaki, M.; Anai, R.; Honda, Y.; Kadota, K.; Kobayashi, Y.; Kimura, T. Drug-eluting stent thrombosis: Current and future perspectives. Cardiovasc. Interv. Ther. 2021, 36, 158–168. [Google Scholar] [CrossRef]
- Slottow, T.L.P.; Waksman, R. Overview of the 2006 Food and Drug Administration Circulatory System Devices Panel meeting on drug-eluting stent thrombosis. Catheter. Cardiovasc. Interv. 2007, 69, 1064–1074. [Google Scholar] [CrossRef]
- Tada, T.; Byrne, R.A.; Simunovic, I.; King, L.A.; Cassese, S.; Joner, M.; Fusaro, M.; Schneider, S.; Schulz, S.; Ibrahim, T.; et al. Risk of stent thrombosis among bare-metal stents, first-generation drug-eluting stents, and second-generation drug-eluting stents: Results from a registry of 18,334 patients. JACC Cardiovasc. Interv. 2013, 6, 1267–1274. [Google Scholar] [CrossRef] [Green Version]
- Sabaté, M.; Brugaletta, S.; Cequier, A.; Iñiguez, A.; Serra, A.; Hernádez-Antolín, R.; Mainar, V.; Valgimigli, M.; Tespili, M.; Den Heijer, P.; et al. The examination trial (everolimus-eluting stents versus bare-metal stents in st-segment elevation myocardial infarction): 2-year results from a multicenter randomized controlled trial. JACC Cardiovasc. Interv. 2014, 7, 64–71. [Google Scholar] [CrossRef] [Green Version]
- Spaulding, C.; Teiger, E.; Commeau, P.; Varenne, O.; Bramucci, E.; Slama, M.; Beatt, K.; Tirouvanziam, A.; Polonski, L.; Stella, P.R.; et al. Four-year follow-up of TYPHOON (Trial to assess the use of the CYPHer sirolimus-eluting coronary stent in acute myocardial infarction treated with BallOON angioplasty). JACC Cardiovasc. Interv. 2011, 4, 14–23. [Google Scholar] [CrossRef] [Green Version]
- Violini, R.; Musto, C.; De Felice, F.; Nazzaro, M.S.; Cifarelli, A.; Petitti, T.; Fiorilli, R. Maintenance of Long-Term Clinical Benefit With Sirolimus-Eluting Stents in Patients With ST-Segment Elevation Myocardial Infarction. 3-Year Results of the SESAMI (Sirolimus-Eluting Stent Versus Bare-Metal Stent In Acute Myocardial Infarction) Trial. J. Am. Coll. Cardiol. 2010, 55, 810–814. [Google Scholar] [CrossRef] [Green Version]
- Räber, L.; Yamaji, K.; Kelbæk, H.; Engstrøm, T.; Baumbach, A.; Roffi, M.; Von Birgelen, C.; Taniwaki, M.; Moschovitis, A.; Zaugg, S.; et al. Five-year clinical outcomes and intracoronary imaging findings of the COMFORTABLE AMI trial: Randomized comparison of biodegradable polymer-based biolimus-eluting stents with bare-metal stents in patients with acute ST-segment elevation myocardial infarct. Eur. Heart J. 2019, 40, 1909–1919. [Google Scholar] [CrossRef] [PubMed]
- Di Lorenzo, E.; Sauro, R.; Varricchio, A.; Capasso, M.; Lanzillo, T.; Manganelli, F.; Carbone, G.; Lanni, F.; Pagliuca, M.R.; Stanco, G.; et al. Randomized comparison of everolimus-eluting stents and sirolimus-eluting stents in patients with ST elevation myocardial infarction: RACES-MI trial. JACC Cardiovasc. Interv. 2014, 7, 849–856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Räber, L.; Magro, M.; Stefanini, G.G.; Kalesan, B.; van Domburg, R.T.; Onuma, Y.; Wenaweser, P.; Daemen, J.; Meier, B.; Jüni, P.; et al. Very Late Coronary Stent Thrombosis of a Newer Generation Everolimus-Eluting Stent Compared with Early Generation Drug-Eluting Stents: A Prospective Cohort Study. Circulation 2012, 125, 1979–1983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otsuka, F.; Vorpahl, M.; Nakano, M.; Foerst, J.; Newell, J.B.; Sakakura, K.; Kutys, R.; Ladich, E.; Finn, A.V.; Kolodgie, F.D.; et al. Pathology of second-generation everolimus-eluting stents versus first-generation sirolimus- and paclitaxel-eluting stents in humans. Circulation 2014, 129, 211–223. [Google Scholar] [CrossRef] [Green Version]
- Natsuaki, M.; Morimoto, T.; Furukawa, Y.; Nakagawa, Y.; Kadota, K.; Yamaji, K.; Ando, K.; Shizuta, S.; Shiomi, H.; Tada, T.; et al. Late adverse events after implantation of sirolimus-eluting stent and bare-metal stent: Long-term (5–7 years) follow-up of the Coronary Revascularization Demonstrating Outcome study-Kyoto registry Cohort-2. Circ. Cardiovasc. Interv. 2014, 7, 168–179. [Google Scholar] [CrossRef] [Green Version]
- Brener, S.J.; Kereiakes, D.J.; Simonton, C.A.; Rizvi, A.; Newman, W.; Mastali, K.; Wang, J.C.; Caputo, R.; Smith, R.S.; Ying, S.W.; et al. Everolimus-eluting stents in patients undergoing percutaneous coronary intervention: Final 3-year results of the Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System in the Treatment of Subjects With de Novo Native Coronary Artery. Am. Heart J. 2013, 166, 1035–1042. [Google Scholar] [CrossRef]
- Camenzind, E.; Wijns, W.; Mauri, L.; Kurowski, V.; Parikh, K.; Gao, R.; Bode, C.; Greenwood, J.P.; Boersma, E.; Vranckx, P.; et al. Stent thrombosis and major clinical events at 3 years after zotarolimus-eluting or sirolimus-eluting coronary stent implantation: A randomised, multicentre, open-label, controlled trial. Lancet 2012, 380, 1396–1405. [Google Scholar] [CrossRef]
- Sumino, Y.; Yonetsu, T.; Ueno, H.; Nogami, K.; Misawa, T.; Hada, M.; Yamaguchi, M.; Hoshino, M.; Kanaji, Y.; Sugiyama, T.; et al. Clinical significance of neoatherosclerosis observed at very late phase between 3 and 7 years after coronary stent implantation. J. Cardiol. 2021, 78, 58–65. [Google Scholar] [CrossRef]
- Kuroda, M.; Otake, H.; Shinke, T.; Takaya, T.; Nakagawa, M.; Osue, T.; Taniguchi, Y.; Iwasaki, M.; Kinutani, H.; Konishi, A.; et al. The impact of in-stent neoatherosclerosis on long-term clinical outcomes: An observational study from the Kobe University Hospital optical coherence tomography registry. EuroIntervention 2016, 12, e1366–e1374. [Google Scholar] [CrossRef] [Green Version]
- Nair, A.; Kuban, B.D.; Tuzcu, E.M.; Schoenhagen, P.; Nissen, S.E.; Vince, D.G. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation 2002, 106, 2200–2206. [Google Scholar] [CrossRef] [Green Version]
- Fineschi, M.; Carrera, A.; Gori, T. Atheromatous degeneration of the neointima in a bare metal stent: Intravascular ultrasound evidence. J. Cardiovasc. Med. 2009, 10, 572–573. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.J.; Mintz, G.S.; Park, D.W.; Lee, S.W.; Kim, Y.H.; Lee, C.W.; Han, K.H.; Kim, J.J.; Park, S.W.; Park, S.J. Tissue characterization of in-stent neointima using intravascular ultrasound radiofrequency data analysis. Am. J. Cardiol. 2010, 106, 1561–1565. [Google Scholar] [CrossRef] [PubMed]
- Kimura, T.; Yokoi, H.; Nakagawa, Y.; Tamura, T.; Kaburagi, S.; Sawada, Y.; Sato, Y.; Yokoi, H.; Hamasaki, N.; Nosaka, H.; et al. Three-year follow-up after implantation of metallic coronary-artery stents. N. Engl. J. Med. 1996, 334, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Nobuyoshi, M.; Kimura, T.; Ohishi, H.; Horiuchi, H.; Nosaka, H.; Hamasaki, N.; Yokoi, H.; Kim, K. Restenosis after percutaneous transluminal coronary angioplasty: Pathologic observations in 20 patients. J. Am. Coll. Cardiol. 1991, 17, 433–439. [Google Scholar] [CrossRef]
- Kimura, T.; Abe, K.; Shizuta, S.; Odashiro, K.; Yoshida, Y.; Sakai, K.; Kaitani, K.; Inoue, K.; Nakagawa, Y.; Yokoi, H.; et al. Long-term clinical and angiographic follow-up after coronary stent placement in native coronary arteries. Circulation 2002, 105, 2986–2991. [Google Scholar] [CrossRef] [Green Version]
- Hong, S.J.; Lee, S.Y.; Hong, M.K. Clinical Implication of Optical Coherence Tomography-Based Neoatherosclerosis. J. Korean Med. Sci. 2017, 32, 1056–1061. [Google Scholar] [CrossRef] [Green Version]
- Gonzalo, N.; Serruys, P.W.; Okamura, T.; van Beusekom, H.M.; Garcia-Garcia, H.M.; van Soest, G.; van der Giessen, W.; Regar, E. Optical coherence tomography patterns of stent restenosis. Am. Heart J. 2009, 158, 284–293. [Google Scholar] [CrossRef]
- Miura, K.; Tada, T.; Habara, S.; Kuwayama, A.; Shimada, T.; Ohya, M.; Murai, R.; Amano, H.; Kubo, S.; Otsuru, S.; et al. Optical Coherence Tomography Predictors for Recurrent Restenosis After Paclitaxel-Coated Balloon Angioplasty for Drug-Eluting Stent Restenosis. Circ. J. 2018, 82, 2820–2828. [Google Scholar] [CrossRef] [Green Version]
- Murata, N.; Takayama, T.; Hiro, T.; Hirayama, A. Balloon pin-hole rupture during percutaneous coronary intervention for recurrent, calcified in-stent restenosis: A case report. Catheter. Cardiovasc. Interv. 2018, 91, 1287–1290. [Google Scholar] [CrossRef]
- Yamamoto, W.; Fujii, K.; Otsuji, S.; Takiuchi, S.; Kakishita, M.; Shimatani, Y.; Hasegawa, K.; Ishibuchi, K.; Tamaru, H.; Ishii, R.; et al. Effect of neointimal tissue morphology on vascular response to balloon angioplasty in lesions with in-stent restenosis after drug-eluting stent deployment: An optical coherence tomography analysis. Heart Vessel. 2020, 35, 1193–1200. [Google Scholar] [CrossRef]
- Nagoshi, R.; Shinke, T.; Otake, H.; Shite, J.; Matsumoto, D.; Kawamori, H.; Nakagawa, M.; Kozuki, A.; Hariki, H.; Inoue, T.; et al. Qualitative and quantitative assessment of stent restenosis by optical coherence tomography: Comparison between drug-eluting and bare-metal stents. Circ. J. 2013, 77, 652–660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamaguchi, H.; Arikawa, R.; Takaoka, J.; Miyamura, A.; Atsuchi, N.; Ninomiya, T.; Atsuchi, Y.; Ohishi, M.; Terashima, M.; Kaneda, H. Association of morphologic characteristics on optical coherence tomography and angiographic progression patterns of late restenosis after drug-eluting stent implantation. Cardiovasc. Revasculariz. Med. 2015, 16, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, N.; Ito, Y.; Yamawaki, M.; Araki, M.; Sakai, T.; Obokata, M.; Sakamoto, Y.; Mori, S.; Tsutsumi, M.; Nauchi, M.; et al. Differences between first-generation and second-generation drug-eluting stent regarding in-stent neoatherosclerosis characteristics: An optical coherence tomography analysis. Int. J. Cardiovasc. Imaging 2018, 34, 1521–1528. [Google Scholar] [CrossRef] [PubMed]
- Joner, M.; Koppara, T.; Byrne, R.A.; Castellanos, M.I.; Lewerich, J.; Novotny, J.; Guagliumi, G.; Xhepa, E.; Adriaenssens, T.; Godschalk, T.C.; et al. Neoatherosclerosis in Patients With Coronary Stent Thrombosis: Findings From Optical Coherence Tomography Imaging (A Report of the PRESTIGE Consortium). JACC Cardiovasc. Interv. 2018, 11, 1340–1350. [Google Scholar] [CrossRef]
- Kang, S.J.; Mintz, G.S.; Akasaka, T.; Park, D.W.; Lee, J.Y.; Kim, W.J.; Lee, S.W.; Kim, Y.H.; Lee, C.W.; Park, S.W.; et al. Optical coherence tomographic analysis of in-stent neoatherosclerosis after drug-eluting stent implantation. Circulation 2011, 123, 2954–2963. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.S.; Hong, M.K.; Shin, D.H.; Kim, B.K.; Ko, Y.G.; Choi, D.; Jang, Y. Quantitative and Qualitative Changes in DES-Related Neointimal Tissue Based on Serial OCT. JACC Cardiovasc. Imaging 2012, 5, 1147–1155. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.S.; Lee, J.H.; Shin, D.H.; Kim, B.K.; Ko, Y.G.; Choi, D.; Jang, Y.; Hong, M.K. Long-term outcomes of neointimal hyperplasia without neoatherosclerosis after drug-eluting stent implantation. JACC. Cardiovasc. Imaging 2014, 7, 788–795. [Google Scholar] [CrossRef] [Green Version]
- Writing Committee Members; Lawton, J.S.; Tamis-Holland, J.E.; Bangalore, S.; Bates, E.R.; Beckie, T.M.; Bischoff, J.M.; Bittl, J.A.; Cohen, M.G.; DiMaio, J.M.; et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2022, 79, 197–215. [Google Scholar] [CrossRef]
- Nakamura, D.; Yasumura, K.; Nakamura, H.; Matsuhiro, Y.; Yasumoto, K.; Tanaka, A.; Matsunaga-Lee, Y.; Yano, M.; Yamato, M.; Egami, Y.; et al. Different Neoatherosclerosis Patterns in Drug-Eluting- and Bare-Metal Stent Restenosis—Optical Coherence Tomography Study. Circ. J. 2019, 83, 313–319. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, W.; Fujii, K.; Otsuji, S.; Takiuchi, S.; Kakishita, M.; Ibuki, M.; Hasegawa, K.; Ishibuchi, K.; Tamaru, H.; Yasuda, S.; et al. Optical coherence tomography characteristics of in-stent restenosis after drug-eluting stent implantation: A novel classification and its clinical significance. Heart Vessel. 2020, 35, 38–45. [Google Scholar] [CrossRef]
- Yoshizane, T.; Tanaka, S.; Abe, S.; Ueno, T.; Goto, Y.; Kojima, T.; Iwama, M.; Arai, M.; Noda, T.; Kawasaki, M. Impact of neointimal tissue characterization and heterogeneity of bare-metal stents and drug-eluting stents on the time course after stent implantation evaluated by integrated backscatter intravascular ultrasound. Heart Vessel. 2019, 34, 1639–1649. [Google Scholar] [CrossRef] [PubMed]
- Habara, M.; Terashima, M.; Nasu, K.; Kaneda, H.; Inoue, K.; Ito, T.; Kamikawa, S.; Kurita, T.; Tanaka, N.; Kimura, M.; et al. Difference of tissue characteristics between early and very late restenosis lesions after bare-metal stent implantation: An optical coherence tomography study. Circ. Cardiovasc. Interv. 2011, 4, 232–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yonetsu, T.; Kato, K.; Kim, S.J.; Xing, L.; Jia, H.; McNulty, I.; Lee, H.; Zhang, S.; Uemura, S.; Jang, Y.; et al. Predictors for neoatherosclerosis a retrospective observational study from the optical coherence tomography registry. Circ. Cardiovasc. Imaging 2012, 5, 660–666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, D.; Attizzani, G.F.; Toma, C.; Sheth, T.; Wang, W.; Soud, M.; Aoun, R.; Tummala, R.; Leygerman, M.; Fares, A.; et al. Failure Mechanisms and Neoatherosclerosis Patterns in Very Late Drug-Eluting and Bare-Metal Stent Thrombosis. Circ. Cardiovasc. Interv. 2016, 9, e003785. [Google Scholar] [CrossRef] [Green Version]
- Jang, J.Y.; Kim, J.S.; Shin, D.H.; Kim, B.K.; Ko, Y.G.; Choi, D.; Jang, Y.; Hong, M.K. Favorable effect of optimal lipid-lowering therapy on neointimal tissue characteristics after drug-eluting stent implantation: Qualitative optical coherence tomographic analysis. Atherosclerosis 2015, 242, 553–559. [Google Scholar] [CrossRef]
- Sakai, R.; Sekimoto, T.; Arai, T.; Tanaka, H.; Ogura, K.; Oishi, Y.; Nomura, K.; Sakai, K.; Arai, K.; Tsujita, H.; et al. Contributions of small dense LDL and oxidized LDL on the formation of neoatherosclerosis in patients under statin treatment. Eur. Heart J. 2021, 42, ehab724-3370. [Google Scholar] [CrossRef]
- Paoletti, G.; Gomez-Lara, J.; Brugaletta, S.; Ñato, M.; Romaguera, R.; Roura, G.; Ferreiro, J.L.; Teruel, L.; Gracida, M.; Ortega-Paz, L. Association between coronary atherosclerosis progression and in-stent neoatherosclerosis in patients with ST-elevation myocardial infarction at five-year follow-up. EuroIntervention 2018, 14, 206–214. [Google Scholar] [CrossRef]
- Nishio, R.; Shinke, T.; Otake, H.; Nakagawa, M.; Nagoshi, R.; Inoue, T.; Kozuki, A.; Hariki, H.; Osue, T.; Taniguchi, Y.; et al. Stabilizing effect of combined eicosapentaenoic acid and statin therapy on coronary thin-cap fibroatheroma. Atherosclerosis 2014, 234, 114–119. [Google Scholar] [CrossRef]
- Kuroda, K.; Otake, H.; Shinohara, M.; Kuroda, M.; Tsuda, S.; Toba, T.; Nagano, Y.; Toh, R.; Ishida, T.; Shinke, T.; et al. Effect of rosuvastatin and eicosapentaenoic acid on neoatherosclerosis: The LINK-IT Trial. EuroIntervention 2019, 15, E1099–E1106. [Google Scholar] [CrossRef] [Green Version]
- Meng, L.; Liu, X.; Yu, H.; Wei, G.; Gu, X.; Chang, X.; Xie, M.; Qu, W.; Peng, X.; Sun, Y.; et al. Incidence and Predictors of Neoatherosclerosis in Patients with Early In-Stent Restenosis Determined Using Optical Coherence Tomography. Int. Heart J. 2020, 61, 872–878. [Google Scholar] [CrossRef]
- Nusca, A.; Patti, G. Platelet function and inhibition in ischemic heart disease. Curr. Cardiol. Rep. 2012, 14, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Valgimigli, M.; Bueno, H.; Byrne, R.A.; Collet, J.P.; Costa, F.; Jeppsson, A.; Jüni, P.; Kastrati, A.; Kolh, P.; Mauri, L.; et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur. J. Cardio-Thoracic Surg. 2018, 53, 34–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mauri, L.; Kereiakes, D.J.; Yeh, R.W.; Driscoll-Shempp, P.; Cutlip, D.E.; Steg, P.G.; Normand, S.L.T.; Braunwald, E.; Wiviott, S.D.; Cohen, D.J.; et al. Twelve or 30 Months of Dual Antiplatelet Therapy after Drug-Eluting Stents. N. Engl. J. Med. 2014, 371, 2155–2166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garratt, K.N.; Weaver, W.D.; Jenkins, R.G.; Pow, T.K.; Mauri, L.; Kereiakes, D.J.; Winters, K.J.; Christen, T.; Allocco, D.J.; Lee, D.P. Prasugrel plus aspirin beyond 12 months is associated with improved outcomes after taxus liberté paclitaxel-eluting coronary stent placement. Circulation 2015, 131, 62–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Habib, A.; Finn, A.V. Endothelialization of drug eluting stents and its impact on dual anti-platelet therapy duration. Pharmacol. Res. 2015, 93, 22–27. [Google Scholar] [CrossRef] [Green Version]
- Xie, J.X.; Gunzburger, E.C.; Kaun, L.; Plomondon, M.E.; Barón, A.E.; Waldo, S.W.; Virani, S.S.; Maddox, T.M.; Mavromatis, K. Medical therapy utilization and long-term outcomes following percutaneous coronary intervention: Five-year results from the veterans affairs clinical assessment, reporting, and tracking system program. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005455. [Google Scholar] [CrossRef]
- Steg, P.G.; Bhatt, D.L.; Simon, T.; Fox, K.; Mehta, S.R.; Harrington, R.A.; Held, C.; Andersson, M.; Himmelmann, A.; Ridderstråle, W.; et al. Ticagrelor in Patients with Stable Coronary Disease and Diabetes. N. Engl. J. Med. 2019, 381, 1309–1320. [Google Scholar] [CrossRef] [Green Version]
- Bhatt, D.L.; Steg, P.G.; Mehta, S.R.; Leiter, L.A.; Simon, T.; Fox, K.; Held, C.; Andersson, M.; Himmelmann, A.; Ridderstråle, W.; et al. Ticagrelor in patients with diabetes and stable coronary artery disease with a history of previous percutaneous coronary intervention (THEMIS-PCI): A phase 3, placebo-controlled, randomised trial. Lancet 2019, 394, 1169–1180. [Google Scholar] [CrossRef]
- Bainey, K.R.; Welsh, R.C.; Connolly, S.J.; Marsden, T.; Bosch, J.; Fox, K.A.; Steg, P.G.; Vinereanu, D.; Connolly, D.L.; Berkowitz, S.D.; et al. Rivaroxaban Plus Aspirin Versus Aspirin Alone in Patients with Prior Percutaneous Coronary Intervention (COMPASS-PCI). Circulation 2020, 141, 1141–1151. [Google Scholar] [CrossRef]
- Niccoli, G.; Dato, I.; Imaeva, A.E.; Antonazzo Panico, R.; Roberto, M.; Burzotta, F.; Aurigemma, C.; Trani, C.; Gramegna, M.; Leone, A.M.; et al. Association between inflammatory biomarkers and in-stent restenosis tissue features: An Optical Coherence Tomography Study. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 917–925. [Google Scholar] [CrossRef] [Green Version]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef] [PubMed]
- Wessels, J.A.M.; Huizinga, T.W.J.; Guchelaar, H.J. Recent insights in the pharmacological actions of methotrexate in the treatment of rheumatoid arthritis. Rheumatology 2008, 47, 249–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, R.; Chen, S.; Zhang, H.; Liu, Q.; Xing, J.; Zhao, Q.; Wang, Y.; Yu, B.; Hou, J. Effects of Methotrexate in a Rabbit Model of In-Stent Neoatherosclerosis: An Optical Coherence Tomography Study. Sci. Rep. 2016, 6, 33657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cimmino, G.; Tarallo, R.; Conte, S.; Morello, A.; Pellegrino, G.; Loffredo, F.S.; Calì, G.; De Luca, N.; Golino, P.; Trimarco, B.; et al. Colchicine reduces platelet aggregation by modulating cytoskeleton rearrangement via inhibition of cofilin and LIM domain kinase 1. Vascul. Pharmacol. 2018, 111, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Kong, J.; Deng, Y.; Dong, Q.; Liu, W.; Lu, Y. Colchicine reduces restenosis after balloon angioplasty treatment for in-stent restenosis. Arch. Med. Res. 2015, 46, 101–106. [Google Scholar] [CrossRef]
- Deftereos, S.; Giannopoulos, G.; Raisakis, K.; Kossyvakis, C.; Kaoukis, A.; Panagopoulou, V.; Driva, M.; Hahalis, G.; Pyrgakis, V.; Alexopoulos, D.; et al. Colchicine treatment for the prevention of bare-metal stent restenosis in diabetic patients. J. Am. Coll. Cardiol. 2013, 61, 1679–1685. [Google Scholar] [CrossRef] [Green Version]
- Erdogdu, Ö.; Nathanson, D.; Sjöholm, Å.; Nyström, T.; Zhang, Q. Exendin-4 stimulates proliferation of human coronary artery endothelial cells through eNOS-, PKA- and PI3K/Akt-dependent pathways and requires GLP-1 receptor. Mol. Cell. Endocrinol. 2010, 325, 26–35. [Google Scholar] [CrossRef] [Green Version]
- Lim, S.; Lee, G.Y.; Park, H.S.; Lee, D.H.; Jung, O.T.; Min, K.K.; Kim, Y.B.; Jun, H.S.; Chul, J.H.; Park, K.S. Attenuation of carotid neointimal formation after direct delivery of a recombinant adenovirus expressing glucagon-like peptide-1 in diabetic rats. Cardiovasc. Res. 2017, 113, 183–194. [Google Scholar] [CrossRef] [Green Version]
- Eriksson, L.; Saxelin, R.; Röhl, S.; Roy, J.; Caidahl, K.; Nyström, T.; Hedin, U.; Razuvaev, A. Glucagon-Like Peptide-1 Receptor Activation Does not Affect Re-Endothelialization but Reduces Intimal Hyperplasia via Direct Effects on Smooth Muscle Cells in a Nondiabetic Model of Arterial Injury. J. Vasc. Res. 2015, 52, 41–52. [Google Scholar] [CrossRef]
- Xia, J.; Li, Q.; Liu, Y.; Ren, Q.; Gao, J.; Tian, Y.; Li, J.; Zhang, B.; Sun, H.; Liu, S. A GLP-1 Analog Liraglutide Reduces Intimal Hyperplasia After Coronary Stent Implantation via Regulation of Glycemic Variability and NLRP3 Inflammasome/IL-10 Signaling in Diabetic Swine. Front. Pharmacol. 2020, 11, 372. [Google Scholar] [CrossRef]
- Lee, C.H.; Hsieh, M.J.; Chang, S.H.; Hung, K.C.; Wang, C.J.; Hsu, M.Y.; Juang, J.H.; Hsieh, I.C.; Wen, M.S.; Liu, S.J. Nanofibrous vildagliptin-eluting stents enhance re-endothelialization and reduce neointimal formation in diabetes: In vitro and in vivo. Int. J. Nanomed. 2019, 14, 7503–7513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nusca, A.; Tuccinardi, D.; Pieralice, S.; Giannone, S.; Carpenito, M.; Monte, L.; Watanabe, M.; Cavallari, I.; Maddaloni, E.; Ussia, G.P.; et al. Platelet Effects of Anti-diabetic Therapies: New Perspectives in the Management of Patients with Diabetes and Cardiovascular Disease. Front. Pharmacol. 2021, 12, 1003. [Google Scholar] [CrossRef] [PubMed]
- Santos-Pardo, I.; Lagerqvist, B.; Ritsinger, V.; Witt, N.; Norhammar, A.; Nyström, T. Risk of stent failure in patients with diabetes treated with glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors: A nationwide observational study. Int. J. Cardiol. 2021, 330, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Alfonso, F.; Pérez-Vizcayno, M.J.; Cuesta, J.; García del Blanco, B.; García-Touchard, A.; López-Mínguez, J.R.; Masotti, M.; Zueco, J.; Cequier, A.; Velázquez, M.; et al. 3-Year Clinical Follow-Up of the RIBS IV Clinical Trial: A Prospective Randomized Study of Drug-Eluting Balloons Versus Everolimus-Eluting Stents in Patients With In-Stent Restenosis in Coronary Arteries Previously Treated With Drug-Eluting Stents. JACC. Cardiovasc. Interv. 2018, 11, 981–991. [Google Scholar] [CrossRef]
- Alfonso, F.; Pérez-Vizcayno, M.J.; García del Blanco, B.; Otaegui, I.; Masotti, M.; Zueco, J.; Veláquez, M.; Sanchís, J.; García-Touchard, A.; Lázaro-García, R.; et al. Long-Term Results of Everolimus-Eluting Stents Versus Drug-Eluting Balloons in Patients With Bare-Metal In-Stent Restenosis: 3-Year Follow-Up of the RIBS V Clinical Trial. JACC. Cardiovasc. Interv. 2016, 9, 1246–1255. [Google Scholar] [CrossRef]
- Gonzalo, N.; Salazar, C.H.; Pérez-Vizcayno, M.J.; Gómez-Polo, J.C.; Jiménez-Quevedo, P.; Jiménez-Valero, S.; Masotti, M.; Romaguera, R.; Fernández-Ortiz, A.; Escaned, J.; et al. Influence of neoatherosclerosis on prognosis and treatment response in patients with in-stent restenosis. Rev. Española Cardiol. 2021, 74, 427–435. [Google Scholar] [CrossRef]
- Tada, T.; Kadota, K.; Hosogi, S.; Miyake, K.; Ohya, M.; Amano, H.; Izawa, Y.; Kanazawa, T.; Kubo, S.; Ichinohe, T.; et al. Association between tissue characteristics assessed with optical coherence tomography and mid-term results after percutaneous coronary intervention for in-stent restenosis lesions: A comparison between balloon angioplasty, paclitaxel-coated balloon dilata. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 1101–1111. [Google Scholar] [CrossRef] [Green Version]
- Pal, N.; Din, J.; O’Kane, P. Contemporary management of stent failure: Part One. Interv. Cardiol. Rev. 2019, 14, 10–16. [Google Scholar] [CrossRef]
- Nicolais, C.; Lakhter, V.; Ul, H.; Virk, H.; Sardar, P.; Bavishi, C.; Murchu, B.O. Therapeutic Options for In-Stent Restenosis. Curr. Cardiol. Rep. 2018, 20, 7. [Google Scholar] [CrossRef]
- Vom Dahl, J.; Dietz, U.; Haager, P.K.; Silber, S.; Niccoli, L.; Buettner, H.J.; Schiele, F.; Thomas, M.; Commeau, P.; Ramsdale, D.R.; et al. Rotational atherectomy does not reduce recurrent in-stent restenosis: Results of the angioplasty versus rotational atherectomy for treatment of diffuse in-stent restenosis trial (ARTIST). Circulation 2002, 105, 583–588. [Google Scholar] [CrossRef] [Green Version]
- Ichimoto, E.; Kadohira, T.; Nakayama, T.; De Gregorio, J. Long-term clinical outcomes after treatment with excimer laser coronary atherectomy for in-stent restenosis of drug-eluting stent. Int. Heart J. 2018, 59, 14–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sato, T.; Tsuchida, K.; Yuasa, S.; Taya, Y.; Koshikawa, T.; Tanaka, K.; Fujita, S.; Ikeda, Y.; Takahashi, M.; Okabe, M.; et al. The effect of the debulking by excimer laser coronary angioplasty on long-term outcome compared with drug-coating balloon: Insights from optical frequency domain imaging analysis. Lasers Med. Sci. 2020, 35, 403–412. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Okura, H.; Kume, T.; Yamada, R.; Kobayashi, Y.; Fukuhara, K.; Koyama, T.; Neishi, Y.; Hayashida, A.; Kawamoto, T.; et al. Impact of target lesion coronary calcification on stent expansion. Circ. J. 2014, 78, 2209–2214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, Z.A.; Nef, H.; Escaned, J.; Werner, N.; Banning, A.P.; Hill, J.M.; De Bruyne, B.; Montorfano, M.; Lefevre, T.; Stone, G.W.; et al. Safety and Effectiveness of Coronary Intravascular Lithotripsy for Treatment of Severely Calcified Coronary Stenoses: The Disrupt CAD II Study. Circ. Cardiovasc. Interv. 2019, 12, e008434. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.M.; Kereiakes, D.J.; Shlofmitz, R.A.; Klein, A.J.; Riley, R.F.; Price, M.J.; Herrmann, H.C.; Bachinsky, W.; Waksman, R.; Stone, G.W. Intravascular Lithotripsy for Treatment of Severely Calcified Coronary Artery Disease. J. Am. Coll. Cardiol. 2020, 76, 2635–2646. [Google Scholar] [CrossRef]
- Perfetti, M.; Cocco, N.; Radico, F.; Pescetelli, I.; Maddestra, N.; Zimarino, M. Shockwave intravascular lithotripsy for multiple undilatable in-stent restenosis. Cardiol. J. 2020, 27, 431–432. [Google Scholar] [CrossRef]
- Moscarella, E.; Varricchio, A.; Stabile, E.; Latib, A.; Ielasi, A.; Tespili, M.; Cortese, B.; Calabrò, P.; Granata, F.; Panoulas, V.F.; et al. Bioresorbable vascular scaffold implantation for the treatment of coronary in-stent restenosis: Results from a multicenter Italian experience. Int. J. Cardiol. 2015, 199, 366–372. [Google Scholar] [CrossRef]
- Moscarella, E.; Ielasi, A.; Granata, F.; Coscarelli, S.; Stabile, E.; Latib, A.; Cortese, B.; Tespili, M.; Tanaka, A.; Capozzolo, C.; et al. Long-Term Clinical Outcomes After Bioresorbable Vascular Scaffold Implantation for the Treatment of Coronary In-Stent Restenosis: A Multicenter Italian Experience. Circ. Cardiovasc. Interv. 2016, 9, 366–372. [Google Scholar] [CrossRef] [Green Version]
- Alfonso, F.; Cuesta, J.; Pérez-Vizcayno, M.J.; García del Blanco, B.; Rumoroso, J.R.; Bosa, F.; Pérez de Prado, A.; Masotti, M.; Moreno, R.; Cequier, A.; et al. Bioresorbable Vascular Scaffolds for Patients with In-Stent Restenosis: The RIBS VI Study. JACC Cardiovasc. Interv. 2017, 10, 1841–1851. [Google Scholar] [CrossRef]

| Native Atherosclerosis | Neo-Atherosclerosis | |
|---|---|---|
| Earliest lesion | Intimal thickening, which could regress | Intimal thickening with VSMCs proliferation |
| Intimal xanthoma (“fatty streaks”) | Individual foam cells interspersed throughout the intima | Foam cells clusters in surface or in peristrut regions |
| Pathological intimal thickening | Present | Absent. Rarely present in BMS |
| Necrotic cores | Deep | Superficial |
| Intraplaque hemorrhage | Arising from the lumen and/or leaky neoangiogenic vessels | Arising from the lumen and/or leaky neoangiogenic vessels |
| Plaque erosion | Occasional | Rare |
| Calcification | Microcalcification, calcified sheets, or calcified fragments | Microcalcification, calcified sheets, or calcified fragments. Calcified fibrin in DES |
| Eruptive calcified nodules | Rare | Absent |
| Fibrocalcific plaque | Very common | Common, especially in DES |
| Thrombosis | 60–70% due to plaque rupture; less frequently by plaque erosion. Rarely eruptive calcified nodules. | Primarily due to plaque rupture. In-stent erosion is a rare event |
| Chronic total occlusion | Very common | Organized thrombus; not always derived from plaque rupture or restenosis |
| Study | BMS | G1-DES | G2-DES |
|---|---|---|---|
| Tada et al. [27] | 1.5% | 2.2% | 1.0% |
| EXAMINATION Trial [28] | 2.1% | - | 0.8% |
| TYPHOON Trial [29] | 4.0% | 3.6% | - |
| SESAMI Trial [30] | 1.3% | 1.9% | - |
| COMFORTABLE-AMI Trial [31] | 2.2% | - | 3.9% |
| RACES-MI Trial [32] | - | 1.2% | 0% |
| Raber et al. [33] | - | 1.6% (PES) 1.0% (SES) | 0.3% |
| Study (Year) | Type of Study | Methodology | Main Findings |
|---|---|---|---|
| Kang et al. (2010) [42] | Observational | VH-IVUS-guided tissue characterization of 117 restenotic lesions after BMS and DES implantation | BMS- and DES-treated lesions develop in-stent necrotic core and dense calcium, suggesting the development of in-stent neoatherosclerosis |
| Ando et al. (2013) [14] | Observational | IB-IVUS-guided tissue characterization of 54 restenotic lesions after BMS and SES implantation | The neo-intimal tissue after SES implantation had a significantly larger percentage of lipid tissue and a significantly smaller percentage of fibrous tissue compared with that after BMS |
| Yoshizane et al. (2019) [61] | Observational | IB-IVUS-guided tissue characterization of 125 restenotic lesions after BMS and DES implantation | On long-term FUP, a significant difference was observed in the change of TD of the BMS group (low value in the early period with later increase), whereas TD of the DES group tended to be high from the early period |
| Gonzalo et al. (2009) [47] | Observational | Quantitative and qualitative OCT-guided restenotic tissue structure characterization of 25 lesions | Layered, homogeneous and heterogeneous pattern of restenotic tissue have been identified. |
| Habara et al. (2011) [62] | Observational | Quantitative and qualitative OCT-guided restenotic tissue structure characterization of 43 patients with very-late ISR compared with 39 patients with early ISR | Heterogeneous pattern of restenotic tissue was significantly higher in patients with very-late ISR compared to patients with early ISR |
| Kang et al. (2011) [55] | Observational | OCT-guided analysis of 50 DES in-stent restenosis lesions | OCT findings of NA was frequently identified especially in patients with late ISR, including TFCA-containing neointima, intimal rupture and thrombi. |
| Kim et al. (2012) [56] | Observational | OCT-guided evaluation of serial changes in stent strut coverage and neointima characteristics of 76 DES-treated lesions at 9-months and 2-years FUP | Neointimal coverage improved during FUP without significant changes in the incidence of malapposed struts and intracoronary thrombus; NA including transformation to lipid-laden neointima increases during extended FUP |
| Yonetsu et al. (2012) [63] | Observational | Determining the predictors of NA using OCT-analysis of 179 stent-treated lesions | Stent type (DES), stent age (>48 months), age (>65 years), current smoking, chronic kidney disease and ACEi/ARBs use are significant predictors of NA. |
| Nakamura et al. (2016) [64] | Observational | OCT-guided evaluation of failure mechanisms and NA patterns in 61 patients with very-late DES or BMS stent thrombosis | Uncovered struts, malapposed struts and stent underexpansion were more frequently observed in DES; NA, lipid neo-intima, TCFA neo-intima were more frequently observed and had a more diffuse pattern of distribution in BMS. |
| Joner et al. (2018) [54] | Observational | OCT-guided assessment of NA in 134 patients with VLST | NA was frequently observed in VLST (43.3%); in-stent plaque rupture resulted the dominant mechanism causing VLST. |
| Nakamura et al. (2019) [59] | Observational | OCT-guided analysis of NA patterns among 98 patients with ISR and previously BMS/DES treated lesions | NA with ISR was more frequent with DES than BMS and its pattern exhibited a more focal and thicker fibrous cap as compared with BMS. |
| Yamamoto et al. (2020) [60] | Observational | OCT-guided evaluation of 133 lesions with ISR after DES implantation | Neo-intimal tissue was classified in six different patterns: homogeneous high-intensity tissue (type I), heterogeneous tissue with signal attenuation (type II), speckled heterogeneous tissue (type III), heterogeneous tissue containing poorly delineated region with invisible strut (type IV), heterogeneous tissue containing sharply delineated low-intensity region (type V), or bright protruding tissue with an irregular surface (type VI) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nusca, A.; Viscusi, M.M.; Piccirillo, F.; De Filippis, A.; Nenna, A.; Spadaccio, C.; Nappi, F.; Chello, C.; Mangiacapra, F.; Grigioni, F.; et al. In Stent Neo-Atherosclerosis: Pathophysiology, Clinical Implications, Prevention, and Therapeutic Approaches. Life 2022, 12, 393. https://doi.org/10.3390/life12030393
Nusca A, Viscusi MM, Piccirillo F, De Filippis A, Nenna A, Spadaccio C, Nappi F, Chello C, Mangiacapra F, Grigioni F, et al. In Stent Neo-Atherosclerosis: Pathophysiology, Clinical Implications, Prevention, and Therapeutic Approaches. Life. 2022; 12(3):393. https://doi.org/10.3390/life12030393
Chicago/Turabian StyleNusca, Annunziata, Michele Mattia Viscusi, Francesco Piccirillo, Aurelio De Filippis, Antonio Nenna, Cristiano Spadaccio, Francesco Nappi, Camilla Chello, Fabio Mangiacapra, Francesco Grigioni, and et al. 2022. "In Stent Neo-Atherosclerosis: Pathophysiology, Clinical Implications, Prevention, and Therapeutic Approaches" Life 12, no. 3: 393. https://doi.org/10.3390/life12030393
APA StyleNusca, A., Viscusi, M. M., Piccirillo, F., De Filippis, A., Nenna, A., Spadaccio, C., Nappi, F., Chello, C., Mangiacapra, F., Grigioni, F., Chello, M., & Ussia, G. P. (2022). In Stent Neo-Atherosclerosis: Pathophysiology, Clinical Implications, Prevention, and Therapeutic Approaches. Life, 12(3), 393. https://doi.org/10.3390/life12030393










