Effects of Glucocorticoid Therapy on Sepsis Depend Both on the Dose of Steroids and on the Severity and Phase of the Animal Sepsis Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. In Vivo Sepsis Model Induction
2.2. Colony-Forming Unit (CFU) Assay
2.3. Plasma Chemistry Assay: ALT, Albumin, Blood Urea Nitrogen (BUN), Creatinine, and Lactate Dehydrogenase
2.4. Arterial Blood Gas Analysis
2.5. Cytokine Measurements
3. Statistical Analysis
4. Results
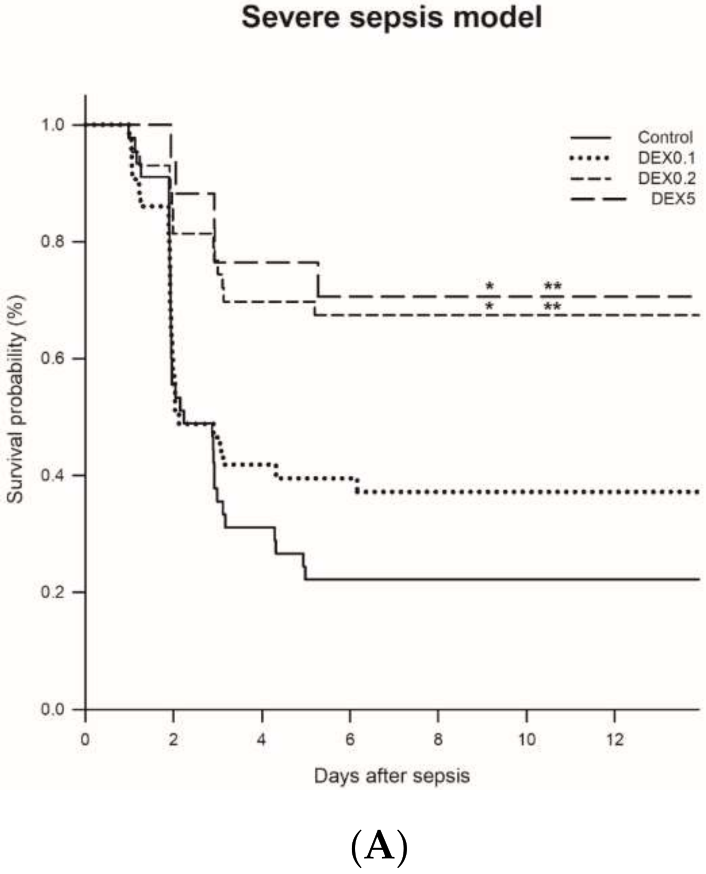
4.1. Survival Study According to the Dose of Steroid Depending on Severity of Sepsis
4.2. Survival Study According to The Phase of Sepsis
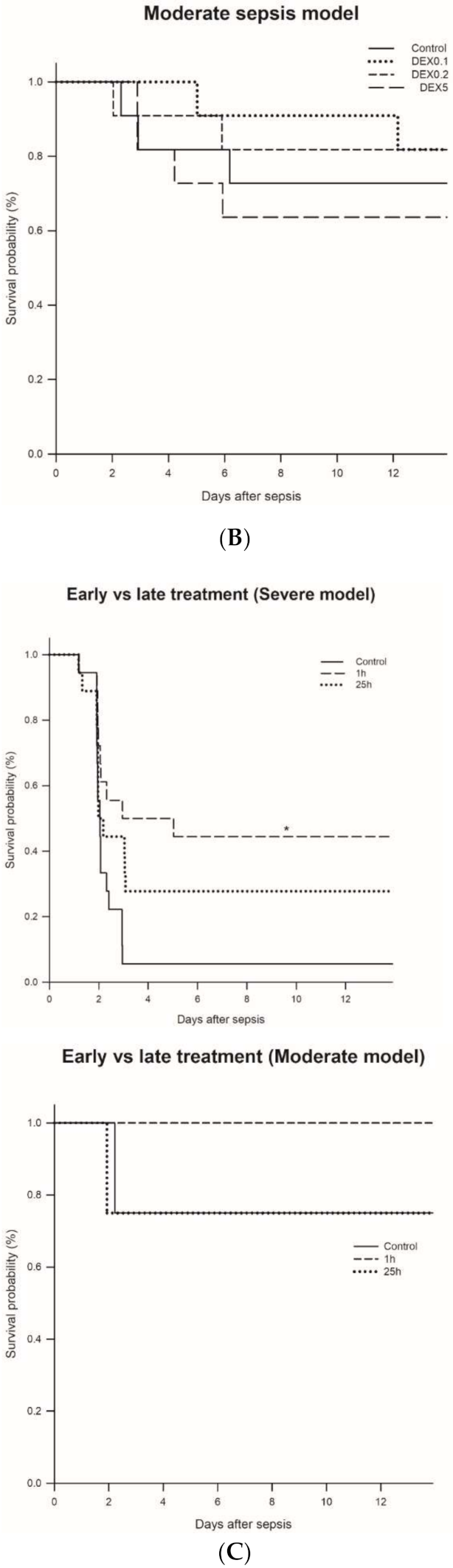
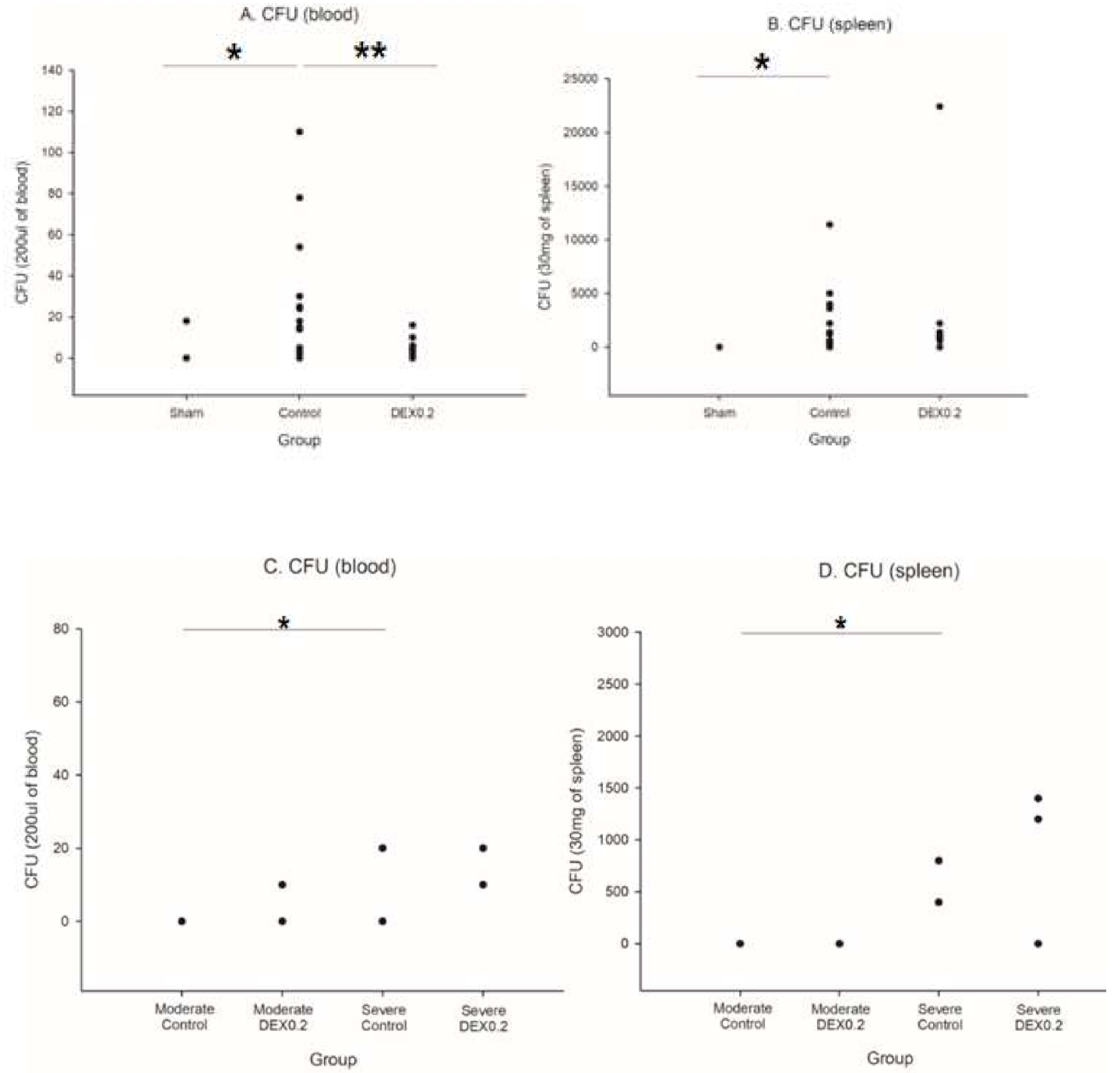
4.3. Serum Creatinine, BUN, and ALT
4.4. Cytokines
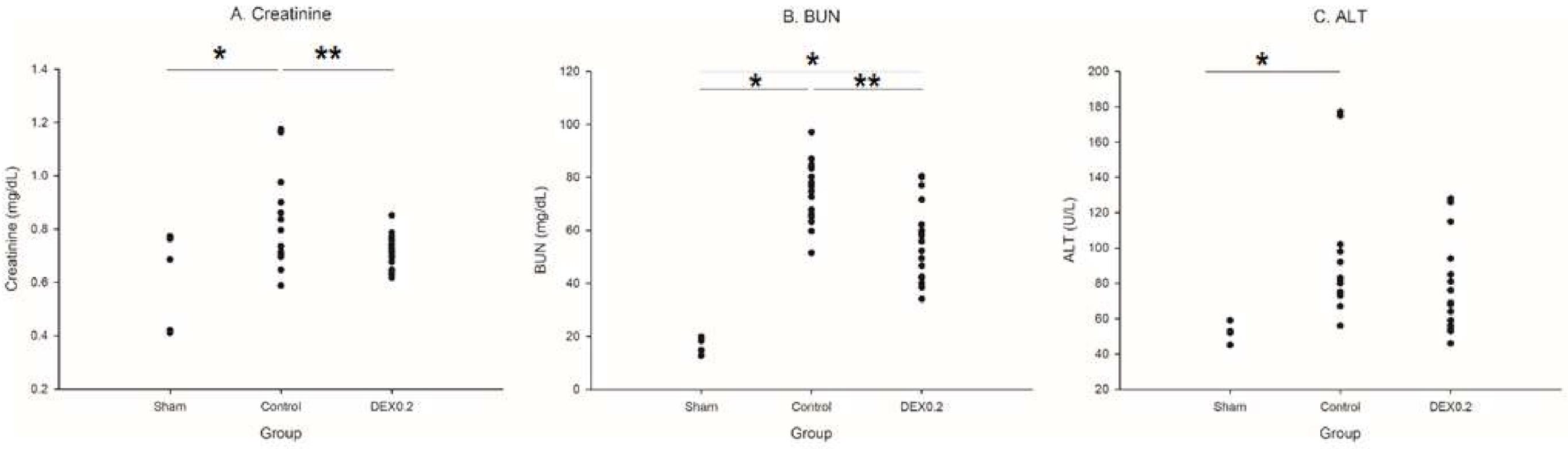
4.5. CFU Assay
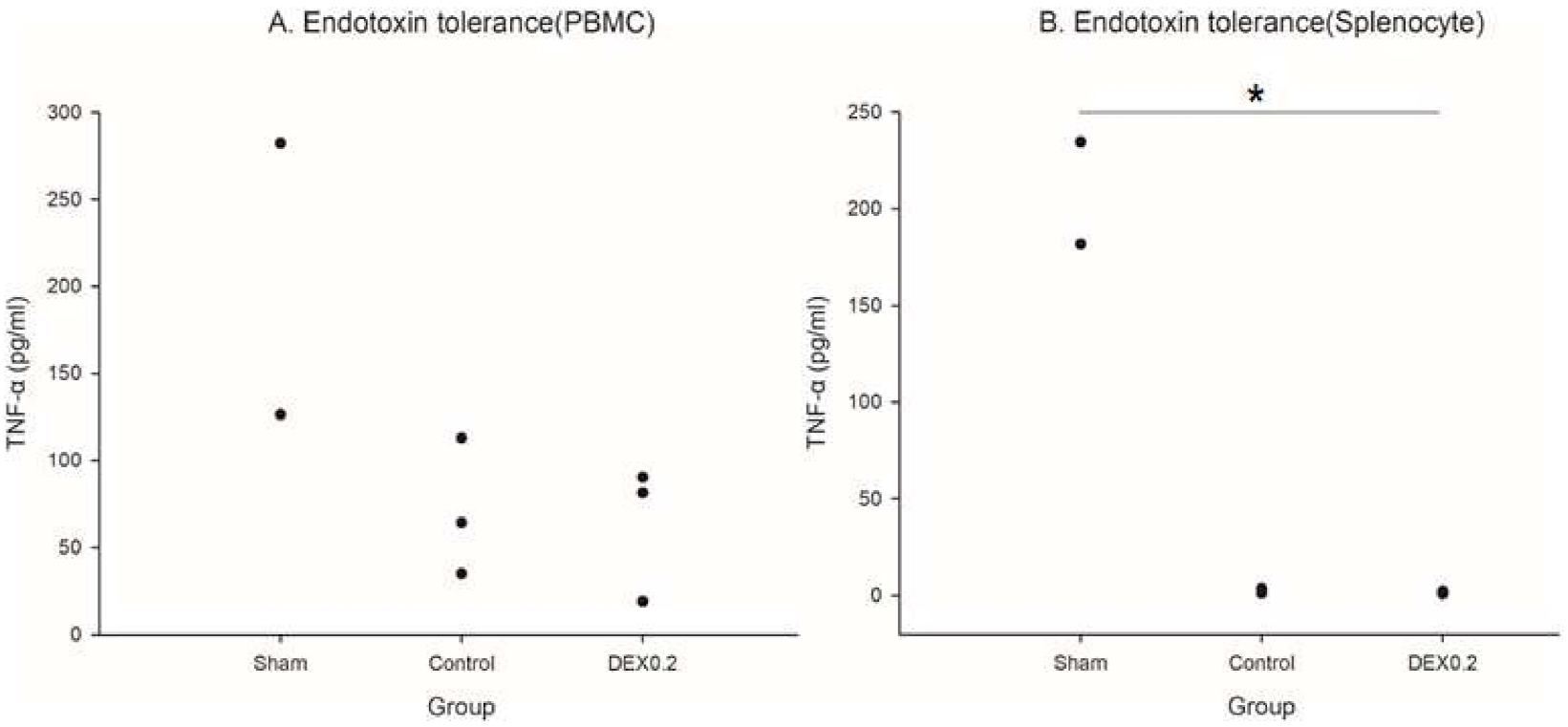
4.6. Endotoxin Tolerance (Ex Vivo PBMC and Splenocyte Stimulation with LPS)
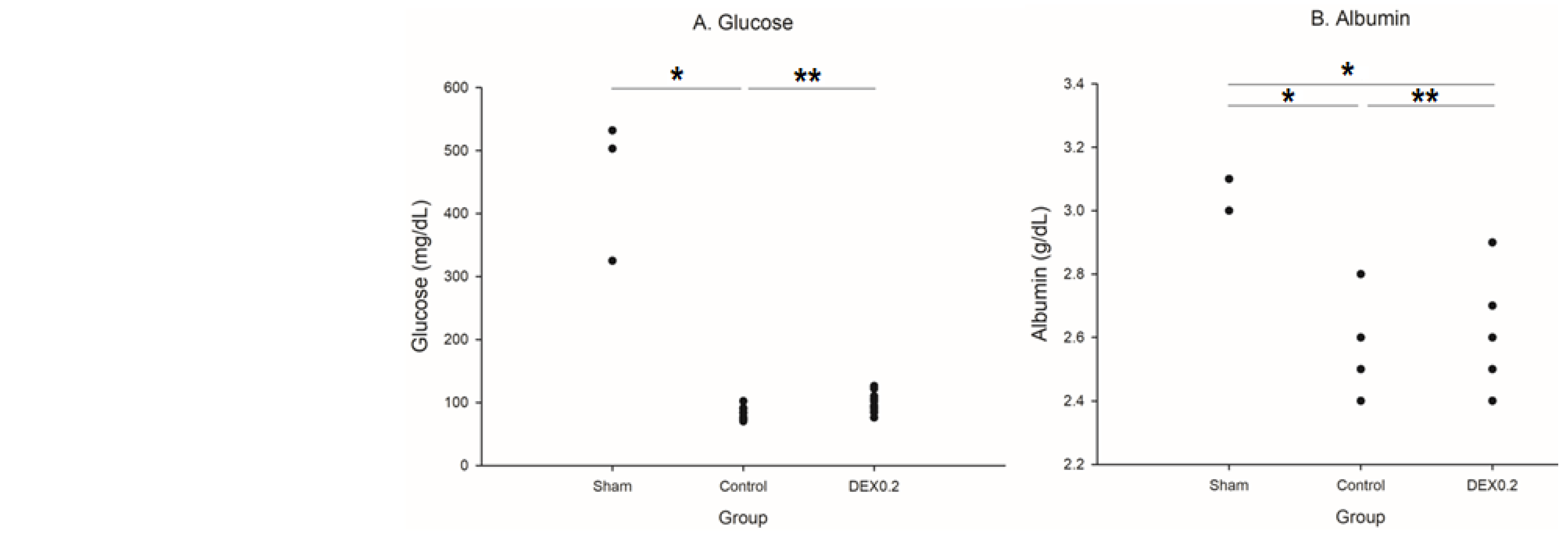
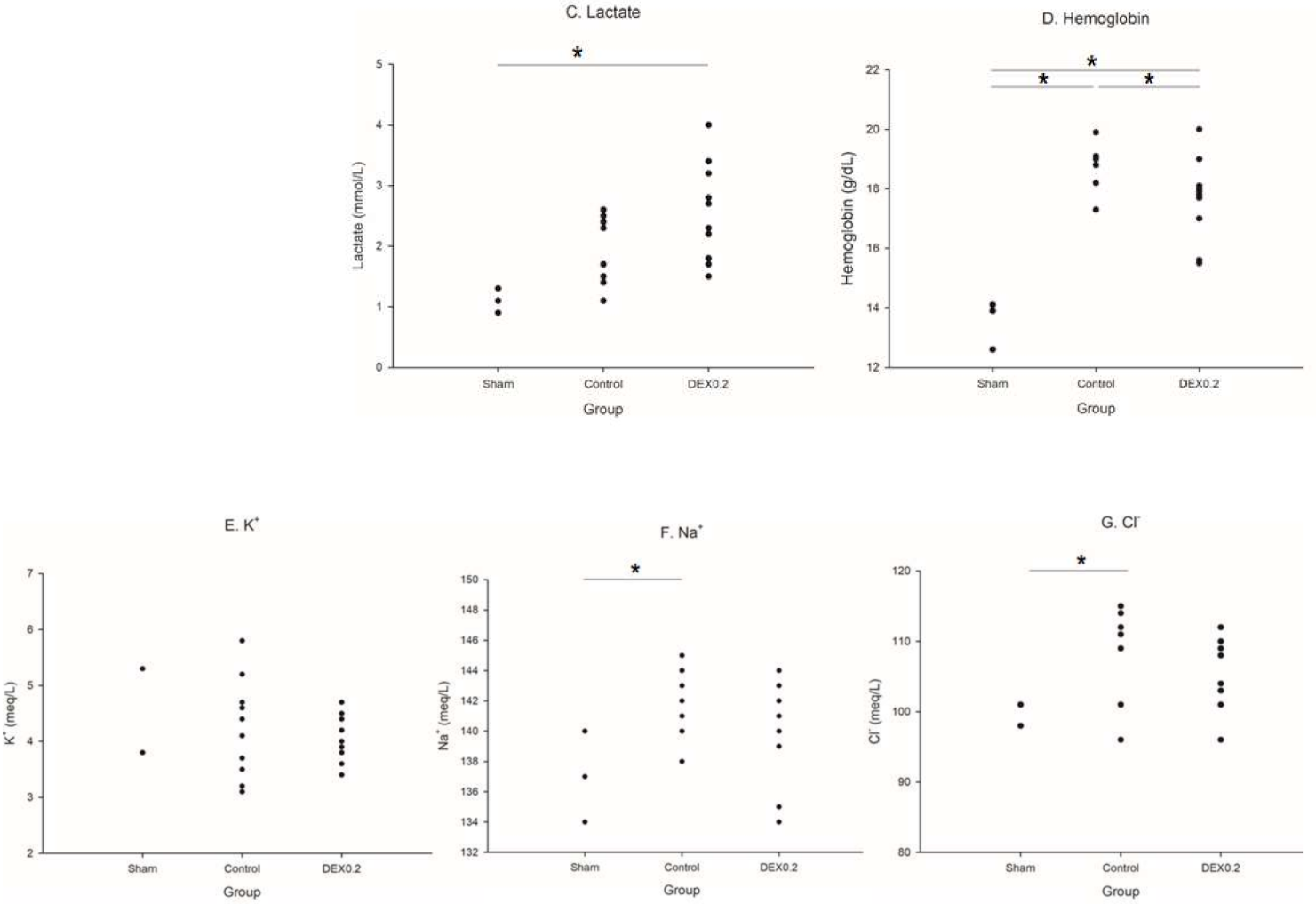
4.7. Other Laboratory Findings
4.8. Arterial Blood Gas Analysis and Lactate
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Kim, J.; Kim, K.; Lee, H.; Ahn, S. Epidemiology of sepsis in Korea: A population-based study of incidence, mortality, cost and risk factors for death in sepsis. Clin. Exp. Emerg. Med. 2019, 6, 49–63. [Google Scholar] [CrossRef] [PubMed]
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef] [Green Version]
- Vincent, J.L.; Sakr, Y.; Singer, M.; Martin-Loeches, I.; Machado, F.R.; Marshall, J.C.; Finfer, S.; Pelosi, P.; Brazzi, L.; Aditianingsih, D.; et al. Prevalence and Outcomes of Infection Among Patients in Intensive Care Units in 2017. JAMA 2020, 323, 1478–1487. [Google Scholar] [CrossRef] [PubMed]
- Reinhart, K.; Daniels, R.; Kissoon, N.; Machado, F.R.; Schachter, R.D.; Finfer, S. Recognizing Sepsis as a Global Health Priority—A WHO Resolution. N. Engl. J. Med. 2017, 377, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef] [PubMed]
- Annane, D.; Sebille, V.; Charpentier, C.; Bollaert, P.E.; Francois, B.; Korach, J.M.; Capellier, G.; Cohen, Y.; Azoulay, E.; Troche, G.; et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 2002, 288, 862–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Annane, D.; Renault, A.; Brun-Buisson, C.; Megarbane, B.; Quenot, J.P.; Siami, S.; Cariou, A.; Forceville, X.; Schwebel, C.; Martin, C.; et al. Hydrocortisone plus Fludrocortisone for Adults with Septic Shock. N. Engl. J. Med. 2018, 378, 809–818. [Google Scholar] [CrossRef]
- Schumer, W. Steroids in the treatment of clinical septic shock. Ann. Surg. 1976, 184, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Sprung, C.L.; Caralis, P.V.; Marcial, E.H.; Pierce, M.; Gelbard, M.A.; Long, W.M.; Duncan, R.C.; Tendler, M.D.; Karpf, M. The effects of high-dose corticosteroids in patients with septic shock. A prospective, controlled study. N. Engl. J. Med. 1984, 311, 1137–1143. [Google Scholar] [CrossRef]
- Bone, R.C.; Fisher, C.J., Jr.; Clemmer, T.P.; Slotman, G.J.; Metz, C.A.; Balk, R.A. A controlled clinical trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 1987, 317, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, B.; Finfer, S.; Cohen, J.; Rajbhandari, D.; Arabi, Y.; Bellomo, R.; Billot, L.; Correa, M.; Glass, P.; Harward, M.; et al. Adjunctive Glucocorticoid Therapy in Patients with Septic Shock. N. Engl. J. Med. 2018, 378, 797–808. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Chang, W.; Xie, J.; Wu, Z.; Yang, Y.; Qiu, H. The Efficacy, Safety, and Optimal Regimen of Corticosteroids in Sepsis: A Bayesian Network Meta-Analysis. Crit. Care Explor. 2020, 2, e0094. [Google Scholar] [CrossRef] [PubMed]
- Cicarelli, D.D.; Vieira, J.E.; Bensenor, F.E. Early dexamethasone treatment for septic shock patients: A prospective randomized clinical trial. Sao Paulo Med. J. 2007, 125, 237–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, M.J.; Kim, K.; Jo, Y.H.; Lee, J.H.; Hwang, J.E. Dose-dependent mortality and organ injury in a cecal slurry peritonitis model. J. Surg. Res. 2016, 206, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.W.; Lee, M.J.; Chung, T.N.; Lee, H.A.R.; Lee, J.H.; Choi, S.Y.; Park, Y.J.; Kim, C.H.; Jin, I.; Kim, S.H.; et al. The immune modulatory effects of mitochondrial transplantation on cecal slurry model in rat. Crit. Care 2021, 25, 20. [Google Scholar] [CrossRef]
- Posel, C.; Moller, K.; Frohlich, W.; Schulz, I.; Boltze, J.; Wagner, D.C. Density gradient centrifugation compromises bone marrow mononuclear cell yield. PLoS ONE 2012, 7, e50293. [Google Scholar] [CrossRef] [Green Version]
- Nemzek, J.A.; Hugunin, K.M.; Opp, M.R. Modeling sepsis in the laboratory: Merging sound science with animal well-being. Comp. Med. 2008, 58, 120–128. [Google Scholar]
- Sprung, C.L.; Annane, D.; Keh, D.; Moreno, R.; Singer, M.; Freivogel, K.; Weiss, Y.G.; Benbenishty, J.; Kalenka, A.; Forst, H.; et al. Hydrocortisone therapy for patients with septic shock. N. Engl. J. Med. 2008, 358, 111–124. [Google Scholar] [CrossRef] [Green Version]
- Keh, D.; Trips, E.; Marx, G.; Wirtz, S.P.; Abduljawwad, E.; Bercker, S.; Bogatsch, H.; Briegel, J.; Engel, C.; Gerlach, H.; et al. Effect of Hydrocortisone on Development of Shock Among Patients with Severe Sepsis: The HYPRESS Randomized Clinical Trial. JAMA 2016, 316, 1775–1785. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; McIntyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Cui, X.; Li, X.; Solomon, S.B.; Danner, R.L.; Banks, S.M.; Fitz, Y.; Annane, D.; Natanson, C.; Eichacker, P.Q. Risk of death does not alter the efficacy of hydrocortisone therapy in a mouse E. coli pneumonia model: Risk and corticosteroids in sepsis. Intensive Care Med. 2008, 34, 568–577. [Google Scholar] [CrossRef]
- Hicks, C.W.; Sweeney, D.A.; Danner, R.L.; Eichacker, P.Q.; Suffredini, A.F.; Feng, J.; Sun, J.; Moriyama, B.; Wesley, R.; Behrend, E.N.; et al. Beneficial effects of stress-dose corticosteroid therapy in canines depend on the severity of staphylococcal pneumonia. Intensive Care Med. 2012, 38, 2063–2071. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Munch, M.W.; Myatra, S.N.; Vijayaraghavan, B.K.T.; Saseedharan, S.; Benfield, T.; Wahlin, R.R.; Rasmussen, B.S.; Andreasen, A.S.; Poulsen, L.M.; Cioccari, L.; et al. Effect of 12 mg vs 6 mg of Dexamethasone on the Number of Days Alive Without Life Support in Adults With COVID-19 and Severe Hypoxemia: The COVID STEROID 2 Randomized Trial. JAMA 2021, 326, 1807–1817. [Google Scholar] [PubMed]
- Bone, R.C. Toward a theory regarding the pathogenesis of the systemic inflammatory response syndrome: What we do and do not know about cytokine regulation. Crit Care Med. 1996, 24, 163–172. [Google Scholar] [CrossRef]
- Rubio, I.; Osuchowski, M.F.; Shankar-Hari, M.; Skirecki, T.; Winkler, M.S.; Lachmann, G.; La Rosée, P.; Monneret, G.; Venet, F.; Bauer, M.; et al. Current gaps in sepsis immunology: New opportunities for translational research. Lancet Infect. Dis. 2019, 19, e422–e436. [Google Scholar] [CrossRef]
- MacLean, L.D.; Meakins, J.L.; Taguchi, K.; Duignan, J.P.; Dhillon, K.S.; Gordon, J. Host resistance in sepsis and trauma. Ann. Surg. 1975, 182, 207–217. [Google Scholar] [CrossRef]
- Xiao, W.; Mindrinos, M.N.; Seok, J.; Cuschieri, J.; Cuenca, A.G.; Gao, H.; Hayden, D.L.; Hennessy, L.; Moore, E.E.; Minei, J.P.; et al. A genomic storm in critically injured humans. J. Exp. Med. 2011, 208, 2581–2590. [Google Scholar] [CrossRef]
- Gentile, L.F.; Cuenca, A.G.; Efron, P.A.; Ang, D.; Bihorac, A.; McKinley, B.A.; Moldawer, L.L.; Moore, F.A. Persistent inflammation and immunosuppression: A common syndrome and new horizon for surgical intensive care. J. Trauma Acute Care Surg. 2012, 72, 1491–1501. [Google Scholar] [CrossRef] [Green Version]
- Hotchkiss, R.S.; Monneret, G.; Payen, D. Immunosuppression in sepsis: A novel understanding of the disorder and a new therapeutic approach. Lancet Infect. Dis. 2013, 13, 260–268. [Google Scholar] [CrossRef] [Green Version]
- Bellomo, R.; Kellum, J.A.; Ronco, C.; Wald, R.; Martensson, J.; Maiden, M.; Bagshaw, S.M.; Glassford, N.J.; Lankadeva, Y.; Vaara, S.T.; et al. Acute kidney injury in sepsis. Intensive Care Med. 2017, 43, 816–828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pena, O.M.; Hancock, D.G.; Lyle, N.H.; Linder, A.; Russell, J.A.; Xia, J.; Fjell, C.D.; Boyd, J.H.; Hancock, R.E. An Endotoxin Tolerance Signature Predicts Sepsis and Organ Dysfunction at Initial Clinical Presentation. EBioMedicine 2014, 1, 64–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ottens, T.H.; Nijsten, M.W.; Hofland, J.; Dieleman, J.M.; Hoekstra, M.; van Dijk, D.; van der Maaten, J.M. Effect of high-dose dexamethasone on perioperative lactate levels and glucose control: A randomized controlled trial. Crit. Care 2015, 19, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mizen, K.; Woodman, J.; Boysen, S.R.; Wagg, C.; Greco-Otto, P.; Leguillette, R.; Roy, M.F. Effect of Dexamethasone on Resting Blood Lactate Concentrations in Horses. J. Vet. Intern. Med. 2017, 31, 164–169. [Google Scholar] [CrossRef]
- Nguyen, H.B.; Rivers, E.P.; Abrahamian, F.M.; Moran, G.J.; Abraham, E.; Trzeciak, S.; Huang, D.T.; Osborn, T.; Stevens, D.; Talan, D.A.; et al. Strategies to Improve Survival Working, G., Severe sepsis and septic shock: Review of the literature and emergency department management guidelines. Ann. Emerg. Med. 2006, 48, 28–54. [Google Scholar] [CrossRef] [PubMed]
- Tilouche, N.; Jaoued, O.; Ali, H.B.S.; Gharbi, R.; Fekih Hassen, M.; Elatrous, S. Comparison Between Continuous and Intermittent Administration of Hydrocortisone During Septic Shock: A Randomized Controlled Clinical Trial. Shock 2019, 52, 481–486. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, Y.J.; Lee, M.J.; Bae, J.; Lee, J.H.; Lee, H.A.R.; Mun, S.; Kim, Y.-s.; Yune, C.J.; Chung, T.N.; Kim, K. Effects of Glucocorticoid Therapy on Sepsis Depend Both on the Dose of Steroids and on the Severity and Phase of the Animal Sepsis Model. Life 2022, 12, 421. https://doi.org/10.3390/life12030421
Park YJ, Lee MJ, Bae J, Lee JH, Lee HAR, Mun S, Kim Y-s, Yune CJ, Chung TN, Kim K. Effects of Glucocorticoid Therapy on Sepsis Depend Both on the Dose of Steroids and on the Severity and Phase of the Animal Sepsis Model. Life. 2022; 12(3):421. https://doi.org/10.3390/life12030421
Chicago/Turabian StylePark, Ye Jin, Min Ji Lee, Jinkun Bae, Jung Ho Lee, Han A Reum Lee, Sehwan Mun, Yun-seok Kim, Chang June Yune, Tae Nyoung Chung, and Kyuseok Kim. 2022. "Effects of Glucocorticoid Therapy on Sepsis Depend Both on the Dose of Steroids and on the Severity and Phase of the Animal Sepsis Model" Life 12, no. 3: 421. https://doi.org/10.3390/life12030421
APA StylePark, Y. J., Lee, M. J., Bae, J., Lee, J. H., Lee, H. A. R., Mun, S., Kim, Y.-s., Yune, C. J., Chung, T. N., & Kim, K. (2022). Effects of Glucocorticoid Therapy on Sepsis Depend Both on the Dose of Steroids and on the Severity and Phase of the Animal Sepsis Model. Life, 12(3), 421. https://doi.org/10.3390/life12030421






