SBRT for Localized Prostate Cancer: CyberKnife vs. VMAT-FFF, a Dosimetric Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. The CyberKnife System
2.2. SBRT-VMAT and FFF Delivery Mode
2.3. The Dosimetric Study: Patient Selection, Contouring and Planning
3. Statistical Analysis
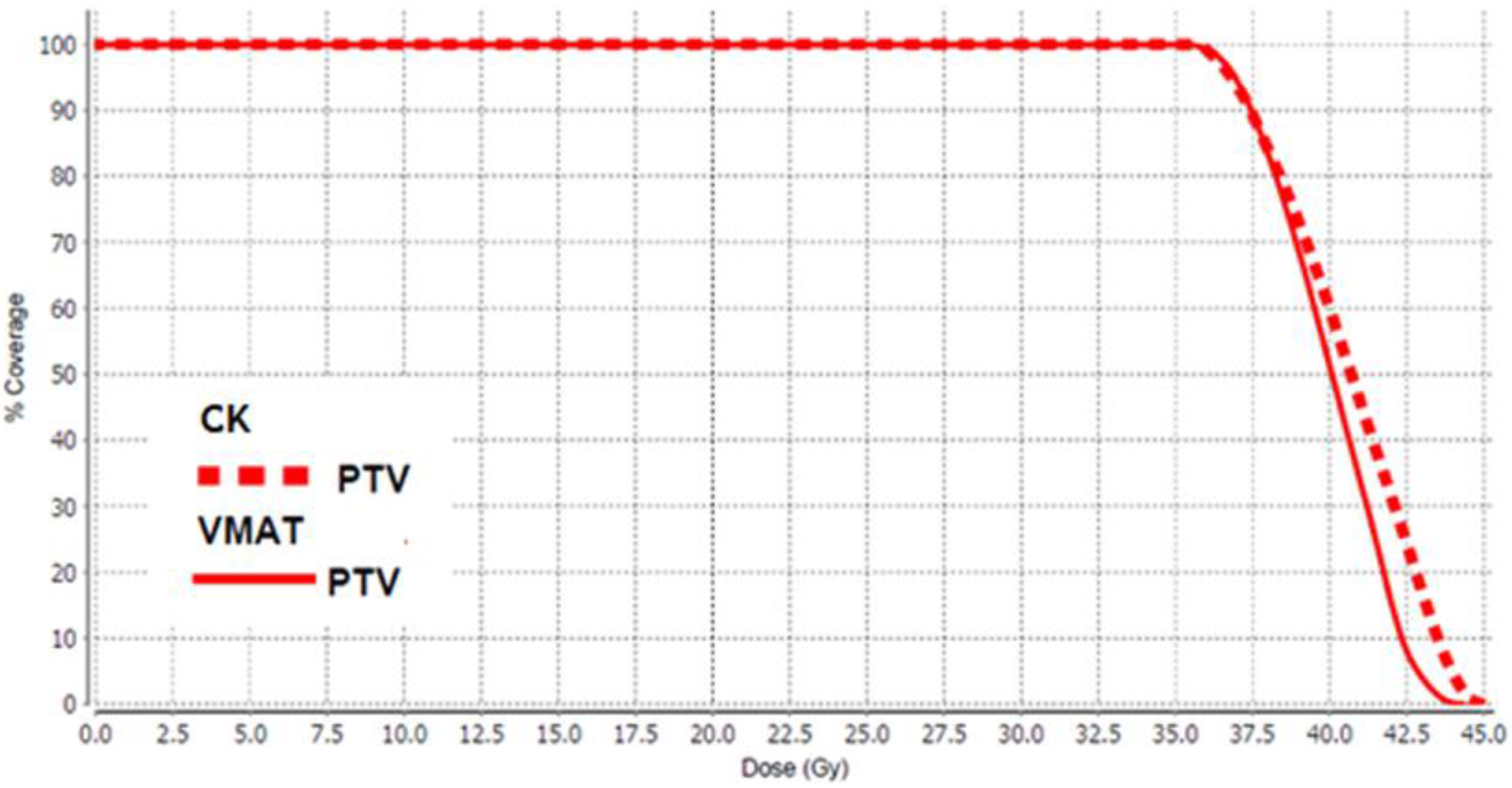
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- AIOM. I Numeri del Cancro in Italia, 2021; AIOM Associazione Italiana di Oncologia Medica: Milano, Italy, 2021. [Google Scholar]
- Leslie, S.W.; Soon-Sutton, T.L.; Sajjad, H.; Siref, L.E. Prostate Cancer; Stat Pearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Stangelberger, A.; Waldert, M.; Djavan, B. Prostate Cancer in Elderly Men. Rev. Urol. 2008, 10, 111–119. [Google Scholar] [PubMed]
- Rawla, P. Epidemiology of Prostate Cancer. World J. Oncol. 2019, 10, 63–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rebello, R.J.; Oing, C.; Knudsen, K.E.; Loeb, S.; Johnson, D.C.; Reiter, R.E.; Gillessen, S.; Van der Kwast, T.; Bristow, R.G. Prostate cancer. Nat. Rev. Dis. Prim. 2021, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Lam, T.B.; MacLennan, S.; Willemse, P.-P.M.; Mason, M.D.; Plass, K.; Shepherd, R.; Baanders, R.; Bangma, C.H.; Bjartell, A.; Bossi, A.; et al. Prostate Cancer Guideline Panel Consensus Statements for Deferred Treatment with Curative Intent for Localised Prostate Cancer from an International Collaborative Study (DETECTIVE Study). Eur. Urol. 2019, 76, 790–813. [Google Scholar] [CrossRef] [Green Version]
- Proust-Lima, C.; Taylor, J.M.; Sécher, S.; Sandler, H.; Kestin, L.; Pickles, T.; Williams, S. Confirmation of a low a/b ratio for prostate cancer treated by external beam radiation therapy alone using a post-treatment repeated measures model for PSA dynamics. Int. J. Radiat. Oncol. Biol. Phys. 2010, 79, 195e201. [Google Scholar] [CrossRef] [Green Version]
- Williams, S.G.; Taylor, J.M.; Liu, N.; Tra, Y.; Duchesne, G.M.; Kestin, L.L.; Sandler, H. Use of individual fraction size data from 3756 patients to directly determine the a/b ratio of prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 2007, 68, 24e33. [Google Scholar] [CrossRef]
- Cho, L.C.; Timmerman, R.; Kavanagh, B. Hypofractionated External-Beam Radiotherapy for Prostate Cancer. Prostate Cancer 2013, 2013, 103547. [Google Scholar] [CrossRef]
- Morgan, S.C.; Hoffman, K.; Loblaw, D.A.; Buyyounouski, M.K.; Patton, C.; Barocas, D.; Sandler, H. Hypofractionated Radiation Therapy for Localized Prostate Cancer: Executive Summary of an ASTRO, ASCO, and AUA Evidence-Based Guideline. Pract. Radiat. Oncol. 2018, 8, 354–360. [Google Scholar] [CrossRef]
- Fransson, P.; Nilsson, P.; Gunnlaugsson, A.; Beckman, L.; Tavelin, B.; Norman, D.; Thellenberg-Karlsson, C.; Hoyer, M.; Lagerlund, M.; Kindblom, J.; et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer (HYPO-RT-PC): Patient-reported quality-of-life outcomes of a randomised, controlled, non-inferiority, phase 3 trial. Lancet Oncol. 2021, 22, 235–245. [Google Scholar] [CrossRef]
- Brand, D.H.; Tree, A.C.; Ostler, P.; Van Der Voet, H.; Loblaw, A.; Chu, W.; Ford, D.; Tolan, S.; Jain, S.; Martin, A.; et al. Intensity-modulated fractionated radiotherapy versus stereotactic body radiotherapy for prostate cancer (PACE-B): Acute toxicity findings from an international, randomised, open-label, phase 3, non-inferiority trial. Lancet Oncol. 2019, 20, 1531–1543. [Google Scholar] [CrossRef]
- Wolf, F.; Sedlmayer, F.; Aebersold, D.; Albrecht, C.; Böhmer, D.; Flentje, M.; Ganswindt, U.; Ghadjar, P.; Höcht, S.; Hölscher, T.; et al. Ultrahypofractionation of localized prostate cancer: Statement from the DEGRO working group prostate cancer. Strahlentherapie Onkologie 2020, 197, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Lehrer, E.J.; Kishan, A.U.; Yu, J.B.; Trifiletti, D.M.; Showalter, T.N.; Ellis, R.; Zaorsky, N.G. Ultrahypofractionated versus hypofractionated and conventionally fractionated radiation therapy for localized prostate cancer: A systematic review and meta-analysis of phase III randomized trials. Radiother. Oncol. 2020, 148, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Bijina, T.K.; Ganesh, K.M.; Pichandi, A.; Muthuselvi, C.A. Cyberknife, Helical Tomotherapy and Rapid Arc SIB-SBRT Treatment Plan Comparison for Carcinoma Prostate. Asian Pac. J. Cancer Prev. 2020, 21, 1149–1154. [Google Scholar] [CrossRef]
- Brochure Equipment Specifications—CyberKnife. Available online: http://www.cyberknifelatin.com/pdf/brochure-tecnico.pdf (accessed on 30 March 2022).
- Di Franco, R.; Borzillo, V.; Alberti, D.; Ametrano, G.; Petito, A.; Coppolaro, A.; Tarantino, I.; Rossetti, S.; Pignata, S.; Iovane, G.; et al. Acute Toxicity in Hypofractionated/Stereotactic Prostate Radiotherapy of Elderly Patients: Use of the Image-guided Radio Therapy (IGRT) Clarity System. In Vivo 2021, 35, 1849–1856. [Google Scholar] [CrossRef]
- Dang, A.; Kupelian, P.A.; Cao, M.; Agazaryan, N.; Kishan, A.U. Image-guided radiotherapy for prostate cancer. Transl. Androl. Urol. 2018, 7, 308–320. [Google Scholar] [CrossRef]
- O’Neill, A.G.M.; Jain, S.; Hounsell, A.R.; O’Sullivan, J.M. Fiducial marker guided prostate radiotherapy: A review. Br. J. Radiol. 2016, 89, 20160296. [Google Scholar] [CrossRef] [Green Version]
- Lachaine, M.; Falco, T. Intrafractional prostate motion management with the clarity autoscan system. Med. Phys. Int. J. 2013, 1, 72. [Google Scholar]
- Grimwood, A.; Rivaz, H.; Zhou, H.; McNair, H.A.; Jakubowski, K.; Bamber, J.C.; Tree, A.C.; Harris, E.J. Improving 3D ultrasound prostate localisation in radiotherapy through increased automation of interfraction matching. Radiother. Oncol. 2020, 149, 134–141. [Google Scholar] [CrossRef]
- Buono, M.; Capussela, T.; Loffredo, F.; Di Pasquale, M.A.; Serra, M.; Quarto, M. Dose-Tracking Software: A Retrospective Analysis of Dosimetric Data in CT Procedures. Health Phys. 2022, 122, 548–555. [Google Scholar] [CrossRef]
- Benedek, H.; Lerner, M.; Nilsson, P.; Knöös, T.; Gunnlaugsson, A.; Ceberg, C. The effect of prostate motion during hypofractionated radiotherapy can be reduced by using flattening filter free beams. Phys. Imaging Radiat. Oncol. 2018, 6, 66–70. [Google Scholar] [CrossRef] [Green Version]
- Scorsetti, M.; Alongi, F.; Clerici, E.; Comito, T.; Fogliata, A.; Iftode, C.; Mancosu, P.; Navarria, P.; Reggiori, G.; Tomatis, S.; et al. Stereotactic body radiotherapy with flattening filter-free beams for prostate cancer: Assessment of patient-reported quality of life. J. Cancer Res. Clin. Oncol. 2014, 140, 1795–1800. [Google Scholar] [CrossRef] [PubMed]
- Buyyounouski, M.K.; Price, R.A.; Harris, E.E.; Miller, R.; Tomé, W.; Schefter, T.; Wallner, P.E. Stereotactic body radiotherapy for primary management of early-stage, low- to intermediate-risk prostate cancer: Report of the American Society for Therapeutic Radiology and Oncology emerging technology committee. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 1297–1304. [Google Scholar] [CrossRef] [PubMed]
- Miralbell, R.; Roberts, S.; Zubizarreta, E.; Hendry, J.H. Dose-Fractionation Sensitivity of Prostate Cancer Deduced From Radiotherapy Outcomes of 5,969 Patients in Seven International Institutional Datasets: α/β = 1.4 (0.9–2.2) Gy. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, e17–e24. [Google Scholar] [CrossRef] [PubMed]
- Nahum, A.E. The radiobiology of hypofractionation. Clin. Oncol. R. Coll. Radiol. 2015, 27, 260–269. [Google Scholar] [CrossRef] [PubMed]
- Fowler, J.F. The radiobiology of prostate cancer including new aspects of fractionated radiotherapy. Acta Oncol. 2005, 44, 265–276. [Google Scholar] [CrossRef]
- Liao, Y.; Joiner, M.; Huang, Y.; Burmeister, J. Hypofractionation: What Does It Mean for Prostate Cancer Treatment? Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 260–268. [Google Scholar] [CrossRef]
- Hickey, B.E.; James, M.L.; Daly, T.; Soh, F.-Y.; Jeffery, M. Hypofractionation for clinically localized prostate cancer. Cochrane Database Syst. Rev. 2019, 2019, CD011462. [Google Scholar] [CrossRef]
- Kishan, A.U.; Dang, A.; Katz, A.J.; Mantz, C.A.; Collins, S.P.; Aghdam, N.; Chu, F.-I.; Kaplan, I.D.; Appelbaum, L.; Fuller, D.B.; et al. Long-term outcomes of stereotactic body radiotherapy for low-risk and intermediate-risk prostate cancer. JAMA Netw. Open 2019, 2, e188006. [Google Scholar] [CrossRef] [Green Version]
- Tsang, Y.M.; Tharmalingam, H.; Belessiotis-Richards, K.; Armstrong, S.; Ostler, P.; Hughes, R.; Alonzi, R.; Hoskin, P.J. Ultra-hypofractionated radiotherapy for low- and intermediate risk prostate cancer: High-dose-rate brachytherapy vs stereotactic ablative radiotherapy. Radiother. Oncol. 2021, 158, 184–190. [Google Scholar] [CrossRef]
- Kishan, A.U.; King, C.R. Stereotactic Body Radiotherapy for Low- and Intermediate-Risk Prostate Cancer. Semin. Radiat. Oncol. 2017, 27, 268–278. [Google Scholar] [CrossRef]
- Katz, A. Stereotactic Body Radiotherapy for Low-Risk Prostate Cancer: A Ten-Year Analysis. Cureus 2019, 9, e1668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Royce, T.J.; Mavroidis, P.; Wang, K.; Falchook, A.D.; Sheets, N.C.; Fuller, D.B.; Collins, S.P.; El Naqa, I.; Song, D.Y.; Ding, G.X.; et al. Tumor control probability modeling and systematic review of the literature of stereotactic body radiation therapy for prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 2020, 110, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Musunuru, H.B.; Quon, H.; Davidson, M.; Cheung, P.; Zhang, L.; D’Alimonte, L.; DeAbreu, A.; Mamedov, A.; Loblaw, A. Dose-escalation of five-fraction SABR in prostate cancer: Toxicity comparison of two prospective trials. Radiother. Oncol. 2016, 118, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Scobioala, S.; Kittel, C.; Elsayad, K.; Kroeger, K.; Oertel, M.; Samhouri, L.; Haverkamp, U.; Eich, H.T. A treatment planning study comparing IMRT techniques and cyber knife for stereotactic body radiotherapy of low-risk prostate carcinoma. Radiat. Oncol. 2019, 14, 143. [Google Scholar] [CrossRef]
- Serra, M.; Ametrano, G.; Borzillo, V.; Quarto, M.; Muto, M.; Di Franco, R.; Federica, S.; Loffredo, F.; Paolo, M. Dosimetric comparison among cyberknife, helical tomotherapy and VMAT for hypofractionated treatment in localized prostate cancer. Medicine 2020, 99, e23574. [Google Scholar] [CrossRef]
- Chen, C.-Y.; Lee, L.-M.; Yu, H.-W.; Lee, S.P.; Lee, H.-L.; Lin, Y.-W.; Wen, Y.-C.; Chen, Y.-J.; Chen, C.-P.; Tsai, J.-T. Dosimetric and radiobiological comparison of Cyberknife and Tomotherapy in stereotactic body radiotherapy for localized prostate cancer. J. X-ray Sci. Technol. 2017, 25, 465–477. [Google Scholar] [CrossRef]
- Seppälä, J.; Suilamo, S.; Tenhunen, M.; Sailas, L.; Virsunen, H.; Kaleva, E.; Keyriläinen, J. Dosimetric Comparison and Evaluation of 4 Stereotactic Body Radiotherapy Techniques for the Treatment of Prostate Cancer. Technol. Cancer Res. Treat. 2017, 16, 238–245. [Google Scholar] [CrossRef] [Green Version]
- Ślosarek, K.; Osewski, W.; Grządziel, A.; Radwan, M.; Dolla, Ł.; Szlag, M.; Stąpór-Fudzińska, M. Integral dose: Comparison between four techniques for prostate radiotherapy. Rep. Pr. Oncol. Radiother. 2014, 20, 99–103. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.-W.; Lin, K.-H.; Ho, H.-W.; Lin, H.-M.; Lin, L.-C.; Lee, S.P.; Chui, C.-S. Treatment plan comparison between stereotactic body radiation therapy techniques for prostate cancer: Non-isocentric CyberKnife versus isocentric RapidArc. Phys. Med. 2014, 30, 654–661. [Google Scholar] [CrossRef]
- Alongi, F.; Rigo, M.; Figlia, V.; Cuccia, F.; Giaj-Levra, N.; Nicosia, L.; Ricchetti, F.; Sicignano, G.; De Simone, A.; Naccarato, S.; et al. 1.5 T MR-guided and daily adapted SBRT for prostate cancer: Feasibility, preliminary clinical tolerability, quality of life and patient-reported outcomes during treatment. Radiat. Oncol. 2020, 15, 69. [Google Scholar] [CrossRef]
- Mazzola, R.; Figlia, V.; Rigo, M.; Cuccia, F.; Ricchetti, F.; Giaj-Levra, N.; Nicosia, L.; Vitale, C.; Sicignano, G.; De Simone, A.; et al. Feasibility and safety of 1.5 T MR-guided and daily adapted abdominal-pelvic SBRT for elderly cancer patients: Geriatric assessment tools and preliminary patient-reported outcomes. J. Cancer Res. Clin. Oncol. 2020, 146, 2379–2397. [Google Scholar] [CrossRef] [PubMed]
| Patient | Age | Total PSA | Target Volume (cc) | Gleason Score (GS) | Clinical Stage |
|---|---|---|---|---|---|
| 1 (CK) | 72 | 5.63 | 51.06 | 1 | 1c |
| 2 (CK) | 72 | 10.84 | 85.82 | 1 | 1c |
| 3 (CK) | 65 | 16.6 | 62.26 | 1 | 2b |
| 4 (CK) | 70 | 6.3 | 44.08 | 2 | 2a |
| 5 (CK) | 65 | 7.32 | 36.48 | 1 | 1b |
| 6 (CK) | 76 | 8.63 | 86.90 | 1 | 2a |
| 7 (CK) | 63 | 4 | 47.08 | 2 | 2a |
| 8 (CK) | 62 | 4.5 | 80.12 | 2 | 2b |
| 9 (CK) | 72 | 5.5 | 66.36 | 1 | 2a |
| 10 (CK) | 73 | 7.6 | 72.35 | 2 | 2a |
| 1 (VMAT-FFF) | 78 | 7.29 | 37.75 | 2 | 1c |
| 2 (VMAT-FFF) | 78 | 4.37 | 31.10 | 2 | 2b |
| 3 (VMAT-FFF) | 77 | 10.69 | 30.78 | 2 | 2b |
| 4 (VMAT-FFF) | 81 | 8.71 | 33 | 2 | |
| 5 (VMAT-FFF) | 76 | 9.6 | 68.17 | 1 | 2b |
| 6 (VMAT-FFF) | 78 | 7.22 | 36.28 | 1 | 2b |
| 7 (VMAT-FFF) | 72 | 12 | 53.91 | 1 | 1c |
| 8 (VMAT-FFF) | 72 | 6.21 | 44.55 | 1 | 2b |
| 9 (VMAT-FFF) | 78 | 11 | 23.74 | 2 | 2b |
| 10 (VMAT-FFF) | 70 | 6.76 | 79.75 | 1 | 2a |
| Parameter | CK | VMAT | p-Value | |
|---|---|---|---|---|
| Bladder | DMAX (Gy) | 39 ± 2 | 41 ± 2 | 0.1 |
| D1 CC (Gy) | 37 ± 2 | 38 ± 1 | 0.05 | |
| V37.5 Gy < 5 cm3 | 1 ± 2 | 3 ± 2 | 0.1 | |
| V37 Gy < 10 cm3 | 2 ± 2 | 4 ± 2 | 0.2 | |
| V36.25 Gy < 10% | 2 ± 2 | 3 ± 1 | 0.2 | |
| V18.125 Gy < 40% | 37 ± 12 | 35 ± 10 | 0.7 | |
| V5 Gy (%) | 92 ± 11 | 68 ± 22 | 0.02 | |
| V10 Gy (%) | 76 ± 18 | 57 ± 21 | 0.06 | |
| V20 Gy (%) | 32 ± 11 | 30 ± 9 | 0.7 | |
| Bladder wall | DMAX (Gy) | 40 ± 2 | 41 ± 1 | 0.3 |
| D10 cm3 (Gy) | 32 ± 3 | 33 ± 2 | 0.5 | |
| Rectum | DMAX Gy | 37 ± 2 | 37 ± 1 | 0.3 |
| V36.25 Gy < 5 cm3 | 0.2 ± 0.3 | 0.5 ± 0.7 | 0.1 | |
| V36 Gy < 1 cm3 | 0.1 ± 0.2 | 0.5 ± 0.6 | 0.07 | |
| V32.625 Gy < 10% | 4 ± 2 | 4 ± 3 | 0.5 | |
| V29 Gy < 20% | 10 ± 4 | 9 ± 4 | 0.7 | |
| V18.125 Gy < 50% | 35 ± 8 | 37 ± 9 | 0.7 | |
| V5 Gy (%) | 88 ± 12 | 87 ± 10 | 0.9 | |
| V10 Gy (%) | 67 ± 15 | 79 ± 10 | 0.09 | |
| V20 Gy (%) | 29 ± 7 | 28 ± 8 | 0.8 | |
| Rectal wall | DMAX (Gy) | 37 ± 2 | 37 ± 2 | 0.9 |
| Bowel | V30 Gy < 1 cm3 | 1 ± 2 | 0.02 ± 0.05 | 0.1 |
| DMAX (Gy) | 24 ± 10 | 13 ± 11 | 0.09 | |
| V10 Gy (%) | 4 ± 4 | 0.2 ± 0.2 | 0.03 | |
| V20 Gy (%) | 0.3 ± 0.5 | 0.02 ± 0.05 | 0.1 | |
| LFH | V14.5 Gy < 5% | 1 ± 2 | 1 ± 2 | 0.8 |
| DMAX (Gy) | 15 ± 3 | 14 ± 2 | 0.5 | |
| RFH | V14.5 Gy < 5% | 1 ± 3 | 0.2 ± 0.5 | 0.3 |
| DMAX (Gy) | 15 ± 3 | 13 ± 2 | 0.3 | |
| Penis bulb | V29.5 Gy < 50% | 1 ± 3 | 13 ± 18 | 0.08 |
| V10 Gy (%) | 28 ± 30 | 62 ± 30 | 0.04 | |
| V20 Gy < 90% | 8 ± 10 | 34 ± 30 | 0.03 |
| Parameter | CK | VMAT | p-Value |
|---|---|---|---|
| CI | 1.09 ± 0.04 | 1.01 ± 0.02 | 0.0006 |
| HI | 1.24 ± 0.03 | 1.2 ± 0.02 | 0.01 |
| GI25 | 24 ± 8 | 22 ± 3 | 0.01 |
| GI50 | 5 ± 1 | 5 ± 1 | 0.6 |
| GI75 | 2.7 ± 0.5 | 2.5 ± 0.2 | 0.2 |
| Treatment Time (min) | 47 ± 9 | 3 ± 1 | ≪0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serra, M.; De Martino, F.; Savino, F.; D’Alesio, V.; Arrichiello, C.; Quarto, M.; Loffredo, F.; Di Franco, R.; Borzillo, V.; Muto, M.; et al. SBRT for Localized Prostate Cancer: CyberKnife vs. VMAT-FFF, a Dosimetric Study. Life 2022, 12, 711. https://doi.org/10.3390/life12050711
Serra M, De Martino F, Savino F, D’Alesio V, Arrichiello C, Quarto M, Loffredo F, Di Franco R, Borzillo V, Muto M, et al. SBRT for Localized Prostate Cancer: CyberKnife vs. VMAT-FFF, a Dosimetric Study. Life. 2022; 12(5):711. https://doi.org/10.3390/life12050711
Chicago/Turabian StyleSerra, Marcello, Fortuna De Martino, Federica Savino, Valentina D’Alesio, Cecilia Arrichiello, Maria Quarto, Filomena Loffredo, Rossella Di Franco, Valentina Borzillo, Matteo Muto, and et al. 2022. "SBRT for Localized Prostate Cancer: CyberKnife vs. VMAT-FFF, a Dosimetric Study" Life 12, no. 5: 711. https://doi.org/10.3390/life12050711
APA StyleSerra, M., De Martino, F., Savino, F., D’Alesio, V., Arrichiello, C., Quarto, M., Loffredo, F., Di Franco, R., Borzillo, V., Muto, M., Ametrano, G., & Muto, P. (2022). SBRT for Localized Prostate Cancer: CyberKnife vs. VMAT-FFF, a Dosimetric Study. Life, 12(5), 711. https://doi.org/10.3390/life12050711








