The Incidence and Associated Risk Factors of Contrast-Induced Nephropathy after Contrast-Enhanced Computed Tomography in the Emergency Setting: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
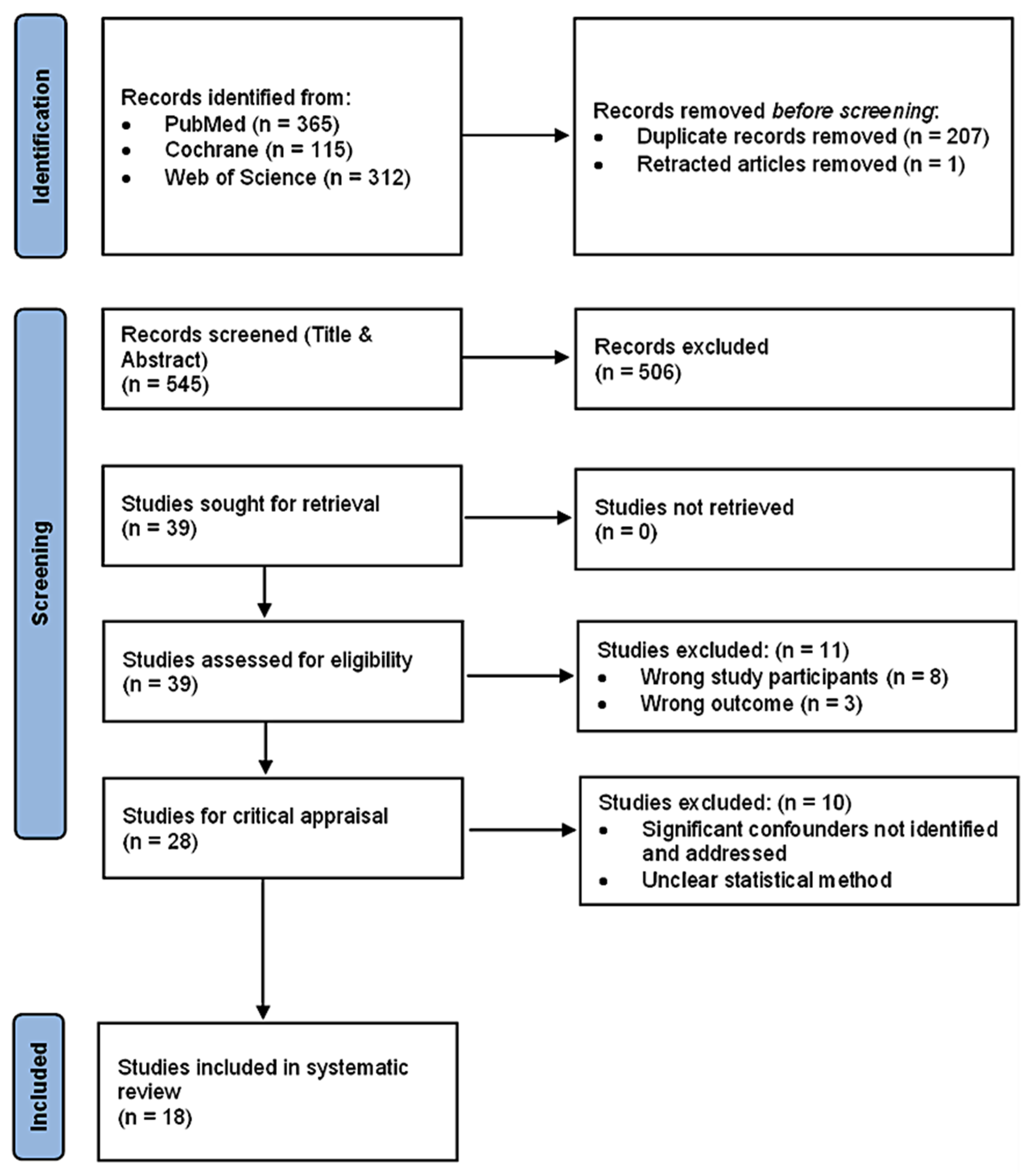
2.3. Study Selection
2.4. Data Collection
3. Results
3.1. Study Identification
3.2. Study Characteristics
| Author and Year | Study Design | Country | CECT Patients (n) | Patient Type | Definition of Nephropathy | Contrast Media | CT Scan Coverage | Incidence of CIN (High/Low Incidence *) | Dialysis | Mortality | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement of sCr | Post-CECT sCr Collection Time | Type | Volume (mL) | |||||||||
| Kene et al., 2021 [20] | Retrospective Cohort | USA | 5589 | Adult patients with CKD stage 3 to 5 | Absolute sCr increase of ≥0.3 mg/dL or ≥1.5-fold increase over baseline sCr | 24 to 72 h | LOCM | 75–150 | Head, neck, chest, abdomen or pelvis | 13.2% (High) | 0.7% (39 patients) | 7.1% (397 deaths) |
| Brito et al., 2020 [21] | Retrospective Cohort | Portugal | 161 | Adult patients with acute ischemic stroke | Absolute sCr increase of ≥0.3 mg/dL or ≥1.5-fold increase over baseline sCr | Within 72 h | LOCM | 90 | Brain | 6.2% (High) | 0.6% (1 patient) | NM |
| Akman and Bakirdogen, 2020 [22] | Retrospective Cohort | Turkey | 122 | Adult patients | Absolute increase of ≥0.5 mg/dL or ≥25% Increase over baseline sCr | Within 72 h | NM | NM | All regions | 36.9% (High) | NM | NM |
| Dağar et al., 2020 [12] | Retrospective Cohort | Turkey | 631 | Adult Patients | Absolute increase of ≥0.5 mg/dL or ≥25% increase over baseline sCr | 48 to 72 h | LOCM | 100 | Chest, abdomen or pelvis | 4.9% (Low) | 0.2% (1 patient) | 0% |
| Hinson et al., 2019 [23] | Retrospective Cohort | USA | 1464 | Adult patients with sepsis | Absolute sCr increase of ≥0.3 mg/dL or ≥1.5-fold increase over baseline sCr | 48 to 72 h | LOCM/IOCM | 80–120 | All regions | 7.2% (High) | NM | NM |
| Cho et al., 2019 [24] | Retrospective Cohort | South Korea | 632 | Adult Patients | Increase in sCr ≥ 0.3 mg/dL or ≥1.5 to 1.9-fold increase over baseline sCr | 48 to 72 h | LOCM | 60 | Chest | 6.49% (High) | 0.79% (5 patients) | NM |
| Hsu et al., 2019 [25] | Retrospective Cohort | Taiwan | 105 | Adult patients with sepsis | Absolute increase of 0.5 mg/dL or >50% increase over baseline sCr | 48 to 72 h | LOCM | Up to 120 | All regions | 12.4% (High) | 10.5% (11 patients) | 25.7% (27 deaths) |
| Puchol et al., 2019 [26] | Retrospective Cohort | Spain | 6642 | Adult patients |
| 24 to 72 h | LOCM | 50–200 | All regions |
| NM | NM |
| Hinson et al., 2017 [27] | Retrospective Cohort | USA | 7201 | Adult patients |
| 48 to 72 h | LOCM/IOCM | 80–120 | All regions |
| 0.4% (27 patients) | NM |
| Hong et al., 2016 [18] | Retrospective Cohort | South Korea | 820 | Adult patients with active cancer | Absolute increase of ≥0.5 mg/dL or ≥25% increase over baseline sCr | 48 to 72 h | LOCM | 80–150 | All regions | 7.5% **(High) | 0.1% (1 patient) | 0.8% (7 deaths: 1 renal failure related) |
| Huang et al., 2013 [28] | Retrospective Cohort | Northern Taiwan | 594 | Adult patients aged 65 and above | Increase in sCr ≥ 0.5 mg/dL | 48 to 72 h | NM | 92.2–105 | Chest or abdomen | 8.6% (High) | 0.5% (3 patients) | 13.1% (78 deaths) |
| Traub et al., 2013 [29] | Retrospective Case-control | USA | 5006 | Adult Patients | Absolute increase of ≥0.5 mg/dL or ≥25% increase over baseline sCr | 48 to 96 h | NM | NM | All regions | 7% (High) | NM | NM |
| Mitchell et al., 2012 [30] | Prospective Cohort | USA | 174 | Adult Patients | Absolute increase of ≥0.5 mg/dL or ≥25% increase over baseline sCr | 2 to 7 days | LOCM | NM | Chest | 14% (High) | 1.7% (3 Patients) | 3% (6 deaths: 2 renal failure related) |
| Sinert et al., 2012 [31] | Retrospective Cohort Study | USA | 773 | Adult Patients | Absolute increase of ≥0.5 mg/dL or ≥25% increase over baseline sCr | 48 to 72 h | LOCM/IOCM | 100–110 | Chest, abdomen or pelvis | 5.69% (High) | 0% | 0.5% (4 deaths) |
| McGillicuddy et al., 2010 [13] | Retrospective Cohort | USA | 822 | Adult patients aged 55 or older | Absolute increase of ≥0.5 mg/dL or ≥25% increase over baseline sCr | Within 72 h | LOCM | 100 | All regions | 1.9% (Low) | 0.3% (2 patients) | NM |
| Mitchell et al., 2010 [32] | Prospective Cohort | USA | 633 | Adult Patients |
| 2 to 7 days | LOCM | NM | All regions |
| 0.8% (5 patients) | 0.9% (6 deaths: 4 renal failure related) |
| Hopyan et al., 2008 [33] | Retrospective Cohort | USA | 198 | Adult patients with acute ischemic stroke | ≥25% increase in baseline sCr | Within 72 h | LOCM/IOCM | Up to 90 | Brain | 2.9% (Low) | 0% | NM |
| Mitchell and Kline, 2007 [34] | Prospective Cohort | USA | 1224 | Adult patients | Absolute increase of ≥0.5 mg/dL or ≥25% increase over baseline sCr | 2 to 7 days | LOCM | 120 | Chest | 12% (High) | 0% | NM |
3.3. Outcomes
3.3.1. Overall CIN Incidence
3.3.2. CIN Definition in Various Studies
sCr Measurement
Post-CECT sCr Collection Time
3.3.3. CIN-Induced Complications
3.3.4. Validity of Classical Risk Factors for CIN in ED Settings
Positive Findings
Negative Findings
Inconclusive Findings
3.3.5. ICM Administration and AKI Development
4. Discussion
4.1. Findings
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Article | Codes | Summary | Subthemes/ Themes | Themes |
|---|---|---|---|---|
| (Kene et al., 2021) [20] | High incidence of CIN: 13.2% | With reference to the pooled CIN incidence of 4.96% reported in the meta-analysis by Moos et al. (2013), values above 4.96% were categorized as high incidence of CIN. | Overall CIN Incidence | |
| (Hinson et al., 2019) [23] | High incidence of CIN: 7.2% | |||
| (Mitchell & Kline, 2007) [34] | High incidence of CIN: 12% | |||
| (Brito et al., 2020) [21] | High incidence of CIN: 6.2% | |||
| (Hong et al., 2016) [18] | High incidence of CIN: 7.5% | |||
| (Sinert et al., 2012) [31] | High incidence of CIN: 5.69% | |||
| (Mitchell et al., 2010 [32] | High incidence of CIN: 11% and 6% | |||
| (Cho et al., 2019) [24] | High incidence of CIN: 6.49% | |||
| (Mitchell et al., 2012) [30] | High incidence of CIN: 14% | |||
| (Huang et al., 2013) [28] | High incidence of CIN: 8.6% | |||
| (Traub et al., 2013) [29] | High incidence of CIN: 7% | |||
| (Hinson et al., 2017) [27] | High incidence of CIN: 6.8% and 10.6% | |||
| (Hsu et al., 2019) [25] | High incidence of CIN: 12.4% | |||
| (Puchol et al., 2019) [26] | High incidence of CIN: 7.15% and 7.72% | |||
| (Akman & Bakirdogen, 2020) [22] | High incidence of CIN: 36.9% | |||
| (McGillicuddy et al., 2010) [13] | Low incidence of CIN: 1.9% | With reference to the pooled CIN incidence of 4.96% reported in the meta-analysis by Moos et al. (2013), values below 4.96% were categorized as low incidence of CIN. | ||
| (Hopyan et al., 2008) [33] | Low incidence of CIN: 2.9% | |||
| (Dağar et al., 2020) [12] | Low incidence of CIN: 4.9% | |||
| (Kene et al., 2021 [20]; Brito et al., 2020 [21]; Hinson et al., 2019 [23]) | Absolute sCr increase of ≥0.3 mg/dL or ≥1.5-fold increase over baseline sCr | The different serum creatinine (sCr) measurements used in the definition of nephropathy | sCr Measurement | CIN Definitions in various studies |
| (Akman & Bakirdogen, 2020 [22]; Dağar et al., 2020 [12]; Puchol et al., 2019 [26]; Hinson et al., 2017 [27]; Hong et al., 2016 [18]; Traub et al., 2013 [29]; Mitchell et al., 2012 [30]; Sinert et al., 2012 [31]; McGillicuddy et al., 2010 [13]; Mitchell et al., 2010 [32]; Mitchell & Kline, 2007 [34]) | Absolute increase of ≥0.5 mg/dL or ≥25% increase over baseline sCr | |||
| (Mitchell et al., 2010) [32] | An absolute rise in sCr of ≥0.3 mg/dL | |||
| (Cho et al., 2019 [24]; Hinson et al., 2017 [27]) | Increase in sCr ≥0.3 mg/dL or ≥1.5 to 1.9-fold increase from baseline sCr | |||
| (Hopyan et al., 2008) [33] | ≥25% increase in baseline sCr | |||
| (Huang et al., 2013) [28] | Increase in sCr ≥ 0.5 mg/dL | |||
| (Hsu et al., 2019) [25] | Absolute increase of 0.5 mg/dL or >50% increase in baseline sCr | |||
| (Puchol et al., 2019) [26] | Absolute increase of ≥0.3 mg/dL or 1.3 times greater than baseline sCr | |||
| (Kene et al., 2021 [20]; Puchol et al., 2019 [26]) | 24 to 72 h | The different timings of sCr follow-ups after CECT used in the definition of nephropathy | Post-CECT sCr Collection Time | |
| (Dağar et al., 2020 [12]; Cho et al., 2019 [24]; Hinson et al., 2019 [23]; Hsu et al., 2019 [25]; Hinson et al., 2017 [27]; Hong et al., 2016 [18]; Huang et al., 2013 [28]; Sinert et al., 2012 [31]) | 48 to 72 qh | |||
| (Akman & Bakirdogen, 2020 [22]; Brito et al., 2020 [21]; McGillicuddy et al., 2010 [13]; Hopyan et al., 2008 [33]) | Within 72 h | |||
| (Mitchell et al., 2012, [30], 2010 [32]; Mitchell & Kline, 2007 [34]) | 2 to 7 days | |||
| (Traub et al., 2013) [29] | 48 to 96 h | |||
| (Sinert et al., 2012 [31]; Hopyan et al., 2008 [33]; Mitchell and Kline, 2007 [34]) | No dialysis was required | Complications of CIN include adverse renal events such as dialysis, chronic kidney disease, end-stage renal disease, and renal transplantation. | CIN-induced Complications | |
| (Kene et al., 2021 [31]; Brito et al., 2020 [21]; Dağar et al., 2020 [12]; Huang et al., 2013 [28]; McGillicuddy et al., 2010 [13]; Hinson et al., 2017 [27]) | Low incidence of dialysis | |||
| (Hsu et al., 2019) [25] | High incidence of dialysis | |||
| (Brito et al., 2020 [21]; Dağar et al., 2020 [12]; Hsu et al., 2019 [25]; Huang et al., 2013 [28]) | Temporary haemodialysis only, none required permanent dialysis | |||
| (McGillicuddy et al., 2010) [13] | Require permanent dialysis | |||
| (Cho et al., 2019) [24] | Renal replacement therapy required for 5 patients | |||
| (Hsu et al., 2019 [25]; Hinson et al., 2017 [27]) | IV administration of contrast does not increase the risk of emergent dialysis | |||
| (Hinson et al., 2019) [23] | IV administration of contrast does not increase the risk of diagnosis of CKD and renal transplantation at 6 months | |||
| (Mitchell et al., 2010 [32], 2012 [30]) | Association between CIN development and higher risk of severe renal failure within 45 days | |||
| (Kene et al., 2021 [20]; Hsu et al., 2019 [25]; Huang et al., 2013 [28]; Mitchel et al., 2012 [30]; McGillicuddy et al., 2010 [13]) | CIN is associated with an increased risk of death | Mortality is another complication of CIN | ||
| (Hsu et al., 2019 [25]; Hong et al., 2016 [18]; Sinert et al., 2012 [31]) | No significant differences in mortality rates between the CECT and non-CECT groups | |||
| (Hong et al., 2016) [18] | No association between CIN and LOS | Increased length of stay (LOS) is also a complication of CIN | ||
| (McGillicuddy et al., 2010) [13] | CIN was associated with an increased LOS | |||
| (Hinson et al., 2019 [23]; Hinson et al., 2017 [27]; Traub et al., 2013 [29]) | Congestive heart failure was associated with development of CIN | Congestive heart failure, acute hypotension, liver diseases, and illness severity of patients are associated with development of CIN in the ED. | Positive Findings | Validity of Classical Risk factors for CIN in ED settings |
| (Brito et al., 2020) [21] | Congestive heart failure was not a predictor of CIN | |||
| (Dağar et al., 2020 [12]; Hong et al., 2016 [18]; Huang et al., 2013 [28]) | Patients with acute hypotension are at a higher risk for CIN | |||
| (Hong et al., 2016 [18]; Traub et al., 2013 [29]) | Patients with liver diseases such as liver cirrhosis are at a higher risk of CIN | |||
| (Hinson et al., 2019 [23]; Puchol et al., 2019 [26]) | CIN was associated with patients that were more severely ill | |||
| (Dağar et al., 2020 [12]; Puchol et al., 2019 [26]; Hinson et al., 2017 [27]) | Age is associated with an increased likelihood of CIN development | Age, gender, eGFR, diabetes, vascular disease, anaemia, and smoking habits were not associated with CIN development in the ED. | Negative Findings | |
| (Brito et al., 2020 [21]; Hong et al., 2016 [18]; Traub et al., 2013 [29]; Sinert et al., 2012 [31]) | Age is not associated with risk of developing CIN | |||
| (Puchol et al., 2019 [26]; Hong et al., 2016 [18]) | Gender is not associated with CIN development | |||
| (Akman & Bakirdogen, 2020) [22] | Older females associated with higher risk of CIN, compared to males who are younger | |||
| (Brito et al., 2020 [21]; Cho et al., 2019 [24]; Hinson et al., 2019 [23]; Hinson et al., 2017 [27]; Hong et al., 2016 [18]; Sinert et al., 2012 [31]) | No association between eGFR and CIN | |||
| (Mitchell et al., 2012) [30] | eGFR < 60 mL/min/1.73 m2 may be an insensitive predictor of CIN after CTPA | |||
| (Brito et al., 2020) [21] | eGFR < 60 mL/min/1.73 m2 is a predictor of CIN | |||
| (Kene et al., 2021) [20] | Patients with CKD stage 3 at higher risk of AKI, but not for CKD 4–5 patients | |||
| (Hinson et al., 2017) [27] | Pre-existing diagnosis of CKD was associated with increased likelihood of CIN by multivariable logistic regression modelling | |||
| (Brito et al., 2020 [21]; Sinert et al., 2012 [31] Hopyan et al., 2008 [33]) | No association between CIN and diabetes | |||
| (Huang et al., 2013 [28]; Traub et al., 2013 [29]) | Diabetes mellitus was a risk factor for CIN | |||
| (Mitchell & Kline, 2007) [34] | A relatively high AKI frequency among those with coronary artery disease | |||
| (Brito et al., 2020 [21]; Traub et al., 2013 [29]) | History of vascular disease failed to predict CIN | |||
| (Traub et al., 2013) [29] | Anaemia was not a risk factor of CIN | |||
| (Brito et al., 2020) [21] | Smoking habits was not a predictor of CIN. | |||
| (Brito et al., 2020 [21]; Akman & Bakirdogen, 2020 [22]; Puchol et al., 2019 [26]) | Baseline sCr was associated with a higher risk of developing CIN | There was inconclusive evidence to conclude if sCr levels and hypertension were risk factors for CIN development after receiving iodinated contrast in the ED. | Inconclusive Findings | |
| (Huang et al., 2013) [28] | Pre-contrast sCr of more than 1.5 mg/dL was a risk factor for CIN | |||
| (Traub et al., 2013) [29] | Pre-contrast creatinine level > 2.0 mg/dL is an independent predictor of CIN, but not for creatinine > 1.5 mg/dL | |||
| (Hinson et al., 2017 [27]; Hong et al., 2016 [18]; Sinert et al., 2012 [31]) | sCr level is not associated with risk of CIN | |||
| (Mitchell et al., 2012) [30] | Elevated sCr measurement was not associated with an increased risk of CIN following CTPA | |||
| (Mitchell & Kline, 2007) [34] | Laboratory-defined CIN occurred at a lower than expected frequency among those with an elevated baseline sCr concentration (6% vs. 15% among those with normal baseline sCr). | |||
| (Traub et al., 2013) [29] | Hypertension was a predictor of CIN | |||
| (Brito et al., 2020) [21] | Hypertension is not a predictor of AKI | |||
| (Kene et al., 2021) [20] | Administration of iodinated contrast is associated with increased risk of CIN development | The relationship between iodinated contrast media (ICM) and development of acute kidney injury (AKI). | ICM Administration and AKI Development | |
| (Brito et al., 2020 [21]; Hinson et al., 2019 [23]; Puchol et al., 2019 [26]; Hsu et al., 2019 [25]; Hinson et al., 2017 [27]; McGillicuddy et al., 2010 [13]; Hopyan et al., 2008 [33]) | No association between administration of iodinated contrast and development of CIN | |||
References
- Maxwell, S.; Ha, N.T.; Bulsara, M.K.; Doust, J.; Mcrobbie, D.; O’Leary, P.; Slavotinek, J.; Moorin, R. Increasing Use of CT Requested by Emergency Department Physicians in Tertiary Hospitals in Western Australia 2003–2015: An Analysis of Linked Administrative Data. BMJ Open 2021, 11, e043315. [Google Scholar] [CrossRef] [PubMed]
- Bellolio, M.F.; Heien, H.C.; Sangaralingham, L.R.; Jeffery, M.M.; Campbell, R.L.; Cabrera, D.; Shah, N.D.; Hess, E.P. Increased Computed Tomography Utilization in the Emergency Department and Its Association with Hospital Admission. West. J. Emerg. Med. 2017, 18, 835–845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American College of Radiology. ACR Appropriateness Criteria®|American College of Radiology. Available online: https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria (accessed on 11 February 2022).
- Huynh, K.; Baghdanian, A.H.; Baghdanian, A.A.; Sun, D.S.; Kolli, K.P.; Zagoria, R.J. Updated Guidelines for Intravenous Contrast Use for CT and MRI. Emerg. Radiol. 2020, 27, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Davenport, M.S.; Perazella, M.A.; Yee, J.; Dillman, J.R.; Fine, D.; McDonald, R.J.; Rodby, R.A.; Wang, C.L.; Weinreb, J.C. Use of Intravenous Iodinated Contrast Media in Patients with Kidney Disease: Consensus Statements from the American College of Radiology and the National Kidney Foundation. Radiology 2020, 294, 660–668. [Google Scholar] [CrossRef] [Green Version]
- Beckett, K.R.; Moriarity, A.K.; Langer, J.M. Safe Use of Contrast Media: What the Radiologist Needs to Know. RadioGraphics 2015, 35, 1738–1750. [Google Scholar] [CrossRef]
- American College of Radiology. ACR Manual on Contrast Media; 2015. Available online: https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf (accessed on 11 February 2022).
- Kidney Disease Improving Global Outcomes. Section 2: AKI Definition. Kidney Int. Suppl. 2012, 2, 19–36. [Google Scholar] [CrossRef] [Green Version]
- Stacul, F.; van der Molen, A.J.; Reimer, P.; Webb, J.A.W.; Thomsen, H.S.; Morcos, S.K.; Almén, T.; Aspelin, P.; Bellin, M.-F.; Clement, O.; et al. Contrast Induced Nephropathy: Updated ESUR Contrast Media Safety Committee Guidelines. Eur. Radiol. 2011, 21, 2527–2541. [Google Scholar] [CrossRef]
- Turedi, S.; Erdem, E.; Karaca, Y.; Tatli, O.; Sahin, A.; Turkmen, S.; Gunduz, A. The High Risk of Contrast-Induced Nephropathy in Patients with Suspected Pulmonary Embolism Despite Three Different Prophylaxis: A Randomized Controlled Trial. Acad. Emerg. Med. 2016, 23, 1136–1145. [Google Scholar] [CrossRef] [Green Version]
- Bashir, A.A.; Kong, V.; Skinner, D.; Bruce, J.; Laing, G.; Brysiewicz, P.; Clarke, D. Contrast-Induced Nephropathy Following CT Scan for Trauma Is Not Rare and Is Associated with Increased Mortality in South African Trauma Patients. Eur. J. Trauma Emerg. Surg. 2019, 45, 1129–1135. [Google Scholar] [CrossRef]
- Dagar, S.; Emektar, E.; Uzunosmanoglu, H.; Corbacioglu, S.; Oztekin, O.; Cevik, Y. Risk of Acute Kidney Injury after Contrast-Enhanced Computed Tomography in Emergency Department. Hong Kong J. Emerg. Med. 2020. [Google Scholar] [CrossRef]
- McGillicuddy, E.A.; Schuster, K.M.; Kaplan, L.J.; Maung, A.A.; Lui, F.Y.; Maerz, L.L.; Johnson, D.C.; Davis, K.A. Contrast-Induced Nephropathy in Elderly Trauma Patients. J. Trauma 2010, 68, 294–297. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.M.; Kline, J.A.; Jones, A.E.; Tumlin, J.A. Major Adverse Events One Year After Acute Kidney Injury After Contrast-Enhanced Computed Tomography. Ann. Emerg. Med. 2015, 66, 267–274.e4. [Google Scholar] [CrossRef] [PubMed]
- Coca, S.G.; Peixoto, A.J.; Garg, A.X.; Krumholz, H.M.; Parikh, C.R. The Prognostic Importance of a Small Acute Decrement in Kidney Function in Hospitalized Patients: A Systematic Review and Meta-Analysis. Am. J. Kidney Dis. 2007, 50, 712–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joanna Briggs Institute. Critical Appraisal Tools. Available online: https://jbi.global/critical-appraisal-tools (accessed on 22 February 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.-I.; Ahn, S.; Lee, Y.-S.; Kim, W.Y.; Lim, K.S.; Lee, J.H.; Lee, J.-L. Contrast-Induced Nephropathy in Patients with Active Cancer Undergoing Contrast-Enhanced Computed Tomography. Support Care Cancer 2016, 24, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Moos, S.I.; van Vemde, D.N.H.; Stoker, J.; Bipat, S. Contrast Induced Nephropathy in Patients Undergoing Intravenous (IV) Contrast Enhanced Computed Tomography (CECT) and the Relationship with Risk Factors: A Meta-Analysis. Eur. J. Radiol. 2013, 82, e387–e399. [Google Scholar] [CrossRef]
- Kene, M.; Arasu, V.A.; Mahapatra, A.K.; Huang, J.; Reed, M.E. Acute Kidney Injury After CT in Emergency Patients with Chronic Kidney Disease: A Propensity Score-Matched Analysis. West. J. Emerg. Med. 2021, 22, 614–622. [Google Scholar] [CrossRef]
- Brito, C.; Falcão, L.; Raimundo, M.; Fernandes, S.; Fernandes, A.; Silva, S.; Vilela, P.; de Almeida, E. Contrast-Induced Acute Kidney Injury in Acute Ischaemic Stroke Patients. Neuroradiol. J. 2020. [Google Scholar] [CrossRef]
- Akman, C.; Bakirdogen, S. The Impact of Serum Creatinine, Albumin, Age, and Gender on the Development of Contrast-Induced Nephropathy in Patients Exposed to Contrast Agent Upon Admission to the Emergency Department. Cureus 2020, 12, e11051. [Google Scholar] [CrossRef]
- Hinson, J.S.; Al Jalbout, N.; Ehmann, M.R.; Klein, E.Y. Acute Kidney Injury Following Contrast Media Administration in the Septic Patient: A Retrospective Propensity-Matched Analysis. J. Crit. Care 2019, 51, 111–116. [Google Scholar] [CrossRef]
- Cho, A.; Kim, M.J.; You, J.S.; Shin, H.J.; Lee, E.J.; Park, I.; Chung, S.P.; Kim, J.H. Postcontrast Acute Kidney Injury After Computed Tomography Pulmonary Angiography for Acute Pulmonary Embolism. J. Emerg. Med. 2019, 57, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.C.; Su, H.Y.; Sun, C.K.; Liang, C.Y.; Chen, T.B.; Hsu, C.W. Risk of Post-Contrast Acute Kidney Injury in Emergency Department Patients with Sepsis. Hong Kong Med. J. 2019, 25, 429–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puchol, M.D.F.; García, P.M.; Navarro, M.F.; Rodrigo, E.S.; Pérez, E.B.; López, E.T. The administration of contrast media: Is there a risk of acute kidney injury? Radiologia 2019, 61, 306–314. [Google Scholar] [CrossRef]
- Hinson, J.S.; Ehmann, M.R.; Fine, D.M.; Fishman, E.K.; Toerper, M.F.; Rothman, R.E.; Klein, E.Y. Risk of Acute Kidney Injury After Intravenous Contrast Media Administration. Ann. Emerg. Med. 2017, 69, 577–586.e4. [Google Scholar] [CrossRef]
- Huang, M.-K.; Hsu, T.-F.; Chiu, Y.-H.; Chiang, S.-C.; Kao, W.-F.; Yen, D.H.-T.; Huang, M.-S. Risk Factors for Acute Kidney Injury in the Elderly Undergoing Contrast-Enhanced Computed Tomography in the Emergency Department. J. Chin. Med. Assoc. 2013, 76, 271–276. [Google Scholar] [CrossRef] [Green Version]
- Traub, S.J.; Kellum, J.A.; Tang, A.; Cataldo, L.; Kancharla, A.; Shapiro, N.I. Risk Factors for Radiocontrast Nephropathy after Emergency Department Contrast-Enhanced Computerized Tomography. Acad. Emerg. Med. 2013, 20, 40–45. [Google Scholar] [CrossRef]
- Mitchell, A.M.; Jones, A.E.; Tumlin, J.A.; Kline, J.A. Prospective Study of the Incidence of Contrast-Induced Nephropathy among Patients Evaluated for Pulmonary Embolism by Contrast-Enhanced Computed Tomography. Acad. Emerg. Med. 2012, 19, 618–625. [Google Scholar] [CrossRef] [Green Version]
- Sinert, R.; Brandler, E.; Subramanian, R.A.; Miller, A.C. Does the Current Definition of Contrast-Induced Acute Kidney Injury Reflect a True Clinical Entity? Acad. Emerg. Med. 2012, 19, 1261–1267. [Google Scholar] [CrossRef]
- Mitchell, A.M.; Jones, A.E.; Tumlin, J.A.; Kline, J.A. Incidence of Contrast-Induced Nephropathy after Contrast-Enhanced Computed Tomography in the Outpatient Setting. Clin. J. Am. Soc. Nephrol. 2010, 5, 4–9. [Google Scholar] [CrossRef]
- Hopyan, J.J.; Gladstone, D.J.; Mallia, G.; Schiff, J.; Fox, A.J.; Symons, S.P.; Buck, B.H.; Black, S.E.; Aviv, R.I. Renal Safety of CT Angiography and Perfusion Imaging in the Emergency Evaluation of Acute Stroke. AJNR Am. J. Neuroradiol. 2008, 29, 1826–1830. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, A.M.; Kline, J.A. Contrast Nephropathy Following Computed Tomography Angiography of the Chest for Pulmonary Embolism in the Emergency Department. J. Thromb. Haemost. 2007, 5, 50–54. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.S.; McDonald, R.J.; Comin, J.; Williamson, E.E.; Katzberg, R.W.; Murad, M.H.; Kallmes, D.F. Frequency of Acute Kidney Injury Following Intravenous Contrast Medium Administration: A Systematic Review and Meta-Analysis. Radiology 2013, 267, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Morcos, R.; Kucharik, M.; Bansal, P.; Al Taii, H.; Manam, R.; Casale, J.; Khalili, H.; Maini, B. Contrast-Induced Acute Kidney Injury: Review and Practical Update. Clin. Med. Insights Cardiol. 2019, 13, 1179546819878680. [Google Scholar] [CrossRef] [PubMed]
- Kooiman, J.; Pasha, S.M.; Zondag, W.; Sijpkens, Y.W.J.; van der Molen, A.J.; Huisman, M.V.; Dekkers, O.M. Meta-Analysis: Serum Creatinine Changes Following Contrast Enhanced CT Imaging. Eur. J. Radiol. 2012, 81, 2554–2561. [Google Scholar] [CrossRef]
- Hossain, M.A.; Costanzo, E.; Cosentino, J.; Patel, C.; Qaisar, H.; Singh, V.; Khan, T.; Cheng, J.S.; Asif, A.; Vachharajani, T.J. Contrast-Induced Nephropathy: Pathophysiology, Risk Factors, and Prevention. Saudi J. Kidney Dis. Transplant. 2018, 29, 1–9. [Google Scholar] [CrossRef]
- Aycock, R.D.; Westafer, L.M.; Boxen, J.L.; Majlesi, N.; Schoenfeld, E.M.; Bannuru, R.R. Acute Kidney Injury After Computed Tomography: A Meta-Analysis. Ann. Emerg. Med. 2018, 71, 44–53.e4. [Google Scholar] [CrossRef]
- Guillon, B.; Ecarnot, F.; Marcucci, C.; Ducloux, D.; Chatot, M.; Badoz, M.; Bonnet, B.; Chopard, R.; Frey, P.; Meneveau, N.; et al. Incidence, Predictors, and Impact on Six-Month Mortality of Three Different Definitions of Contrast-Induced Acute Kidney Injury After Coronary Angiography. Am. J. Cardiol. 2018, 121, 818–824. [Google Scholar] [CrossRef]
- Thomsen, H.S.; Morcos, S.K.; Erley, C.M.; Grazioli, L.; Bonomo, L.; Ni, Z.; Romano, L. The ACTIVE Trial: Comparison of the Effects on Renal Function of Iomeprol-400 and Iodixanol-320 in Patients with Chronic Kidney Disease Undergoing Abdominal Computed Tomography. Investig. Radiol. 2008, 43, 170–178. [Google Scholar] [CrossRef]
- Cao, D.; Mehran, R.; Chandiramani, R.; Goel, R.; Roumeliotis, A.; Blum, M.; Singleton, R.; Dangas, G.; Baber, U.; Stefanini, G.G.; et al. Influence of Ethnicity on the Incidence of Contrast-Induced Acute Kidney Injury After Percutaneous Coronary Intervention. Available online: https://www.ahajournals.org/doi/10.1161/circ.140.suppl_1.14762 (accessed on 22 February 2022).
- Modi, K.; Padala, S.A.; Gupta, M. Contrast-Induced Nephropathy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Shams, E.; Mayrovitz, H.N. Contrast-Induced Nephropathy: A Review of Mechanisms and Risks. Cureus 2021, 13, e14842. [Google Scholar] [CrossRef]
- Lee, Y.-C.; Hsieh, C.-C.; Chang, T.-T.; Li, C.-Y. Contrast-Induced Acute Kidney Injury Among Patients with Chronic Kidney Disease Undergoing Imaging Studies: A Meta-Analysis. Am. J. Roentgenol. 2019, 213, 728–735. [Google Scholar] [CrossRef]
- De Simone, B.; Ansaloni, L.; Sartelli, M.; Gaiani, F.; Leandro, G.; de’Angelis, G.L.; Di Mario, F.; Coccolini, F.; Catena, F. Is the risk of contrast-induced nephropathy a real contraindication to perform intravenous contrast enhanced Computed Tomography for non-traumatic acute abdomen in Emergency Surgery Department? Acta Bio Med. Atenei Parm. 2018, 89 (Suppl. 9), 158–172. [Google Scholar] [CrossRef]
- Davenport, M.S.; Perazella, M.A.; Yee, J.; Dillman, J.R.; Fine, D.; McDonald, R.J.; Rodby, R.A.; Wang, C.L.; Weinreb, J.C. Use of Intravenous Iodinated Contrast Media in Patients with Kidney Disease: Consensus Statements from the American College of Radiology and the National Kidney Foundation. Kidney Med. 2020, 2, 85–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.; Kim, M.H.; Kang, E.; Park, S.; Jo, H.A.; Lee, H.; Kim, S.M.; Lee, J.P.; Oh, K.H.; Joo, K.W.; et al. Contrast-Induced Nephropathy After Computed Tomography in Stable CKD Patients with Proper Prophylaxis: 8-Year Experience of Outpatient Prophylaxis Program. Medicine 2016, 95, e3560. [Google Scholar] [CrossRef]
- Neilipovitz, J.; Rosenberg, H.; Hiremath, S.; Savage, D.W.; Ohle, R.; Alaref, A.; Yadav, K.; Atkinson, P. CJEM Debate Series: Contrast-enhanced imaging should not be withheld for emergency department patients as contrast-induced acute kidney injury is very uncommon. CJEM 2021, 23, 432–436. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.; Gardiner, J.C.; Bradley, C.J. Applying Propensity Score Methods in Medical Research: Pitfalls and Prospects. Med. Care Res. Rev. 2010, 67, 528–554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Hajjar, M.; Bashir, I.; Khan, M.; Min, J.; Torosoff, M.; DeLago, A. Incidence of Contrast-Induced Nephropathy in Patients with Chronic Renal Insufficiency Undergoing Multidetector Computed Tomographic Angiography Treated with Preventive Measures. Am. J. Cardiol. 2008, 102, 353–356. [Google Scholar] [CrossRef]
- Khalili, H.; Dashti-Khavidaki, S.; Tabifar, H.; Ahmadinejad, N.; Ahmadi, F. Evaluating the Efficacy of Single Daily Dose of 1200mg of N-Acetyl-Cysteine in Preventing Contrast Agent-Associated Nephrotoxicity. Internet J. Intern. Med. 2005, 6, 1. [Google Scholar]
- O’Neil, M.; Berkman, N.; Hartling, L.; Chang, S.; Anderson, J.; Motu’apuaka, M.; Guise, J.-M.; McDonagh, M.S. Observational Evidence and Strength of Evidence Domains: Case Examples. Syst. Rev. 2014, 3, 35. [Google Scholar] [CrossRef] [Green Version]
- Mueller, C.; Buerkle, G.; Buettner, H.J.; Petersen, J.; Perruchoud, A.P.; Eriksson, U.; Marsch, S.; Roskamm, H. Prevention of Contrast Media-Associated Nephropathy: Randomized Comparison of 2 Hydration Regimens in 1620 Patients Undergoing Coronary Angioplasty. Arch. Intern. Med. 2002, 162, 329–336. [Google Scholar] [CrossRef]
- Weisbord, S.D.; Palevsky, P.M. Prevention of Contrast-Induced Nephropathy with Volume Expansion. CJASN 2008, 3, 273–280. [Google Scholar] [CrossRef] [Green Version]
- Nijssen, E.C.; Nelemans, P.J.; Rennenberg, R.J.; van Ommen, V.; Wildberger, J.E. Prophylactic Intravenous Hydration to Protect Renal Function from Intravascular Iodinated Contrast Material (AMACING): Long-Term Results of a Prospective, Randomised, Controlled Trial. EClinicalMedicine 2018, 4, 109–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weisbord, S.D.; Gallagher, M.; Jneid, H.; Garcia, S.; Cass, A.; Thwin, S.-S.; Conner, T.A.; Chertow, G.M.; Bhatt, D.L.; Shunk, K.; et al. Outcomes after Angiography with Sodium Bicarbonate and Acetylcysteine. N. Engl. J. Med. 2018, 378, 603–614. [Google Scholar] [CrossRef] [PubMed]
| Databases | Search Terms | Results | |
|---|---|---|---|
| PubMed | #1 | “contrast-induced nephropathy”[tw] OR “contrast induced nephropathy”[tw] OR “CIN”[tw] OR “renal disorder”[tw] OR “nephrosis”[tw] OR “nephropathy”[tw] OR “nephrotoxicity”[tw] OR “acute kidney injury”[tw] OR “AKI”[tw] OR “kidney disease”[tw] OR “Acute Kidney Injury”[Mesh] OR “Kidney Diseases/chemically induced”[Mesh] | 236,637 |
| #2 | “Contrast enhanced Computed tomography”[tw] OR “CECT”[tw] OR “CT”[tw] OR “computed tomography”[tw] OR “CT angio*”[tw] OR “CTA”[tw] OR “Tomography, X-ray Computed” [Mesh] | 745,818 | |
| #3 | “ED”[tw] OR “ER”[tw] OR “trauma”[tw] OR “emergency”[tw] OR “Emergency Service, Hospital”[Mesh] | 725,803 | |
| #4 | #1 AND #2 AND #3 | 365 | |
| Cochrane | #1 | MeSH descriptor: [Acute Kidney Injury] explode all trees | 1540 |
| #2 | MeSH descriptor: [Kidney Diseases] explode all trees and with qualifier(s): [chemically induced—CI] | 840 | |
| #3 | (“contrast-induced nephropathy”):ti,ab,kw OR (“contrast induced nephropathy”):ti,ab,kw OR (“CIN”):ti,ab,kw OR (“renal disorder”):ti,ab,kw OR (“nephrosis”):ti,ab,kw | 2130 | |
| #4 | (“nephropathy”):ti,ab,kw OR (“nephrotoxicity”):ti,ab,kw OR (“acute kidney injury”):ti,ab,kw OR (“AKI”):ti,ab,kw OR (“kidney disease”):ti,ab,kw | 26,657 | |
| #5 | #1 OR #2 OR #3 OR #4 | 27,810 | |
| #6 | MeSH descriptor: [Tomography, X-Ray Computed] explode all trees | 5206 | |
| #7 | (“Contrast enhanced Computed tomography”):ti,ab,kw OR (“CECT”):ti,ab,kw OR (“CT”):ti,ab,kw OR (“computed tomography”):ti,ab,kw OR (“CTA “):ti,ab,kw | 86,780 | |
| #8 | (“CT angiogram”):ti,ab,kw OR (“CT angiography”):ti,ab,kw | 1003 | |
| #9 | #6 OR #7 OR #8 | 87,767 | |
| #10 | MeSH descriptor: [Emergency Service, Hospital] explode all trees | 2550 | |
| #11 | (“ED”):ti,ab,kw OR (“ER”):ti,ab,kw OR (“trauma”):ti,ab,kw OR (“emergency”):ti,ab,kw | 84,580 | |
| #12 | #10 OR #11 | 84,580 | |
| #13 | #5 AND #9 AND #12 | 115 | |
| Web of Science | #1 | TS = (“contrast-induced nephropathy” OR “contrast induced nephropathy” OR “CIN” OR “renal disorder” OR “nephrosis” OR “nephropathy” OR “nephrotoxicity” OR “acute kidney injury” OR “AKI” OR “kidney disease”) | 237,874 |
| #2 | TS = (“Contrast enhanced Computed tomography” OR “CECT” OR “CT” OR “computed tomography” OR “CT angiogra*” OR “CTA”) | 640,682 | |
| #3 | TS = (“ED” OR “ER” OR “trauma” OR “emergency”) | 777,572 | |
| #4 | #1 AND #2 AND #3 | 312 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ong, M.-Y.; Koh, J.J.-H.; Kothan, S.; Lai, C. The Incidence and Associated Risk Factors of Contrast-Induced Nephropathy after Contrast-Enhanced Computed Tomography in the Emergency Setting: A Systematic Review. Life 2022, 12, 826. https://doi.org/10.3390/life12060826
Ong M-Y, Koh JJ-H, Kothan S, Lai C. The Incidence and Associated Risk Factors of Contrast-Induced Nephropathy after Contrast-Enhanced Computed Tomography in the Emergency Setting: A Systematic Review. Life. 2022; 12(6):826. https://doi.org/10.3390/life12060826
Chicago/Turabian StyleOng, Mei-Yi, Justin Jie-Hui Koh, Suchart Kothan, and Christopher Lai. 2022. "The Incidence and Associated Risk Factors of Contrast-Induced Nephropathy after Contrast-Enhanced Computed Tomography in the Emergency Setting: A Systematic Review" Life 12, no. 6: 826. https://doi.org/10.3390/life12060826
APA StyleOng, M.-Y., Koh, J. J.-H., Kothan, S., & Lai, C. (2022). The Incidence and Associated Risk Factors of Contrast-Induced Nephropathy after Contrast-Enhanced Computed Tomography in the Emergency Setting: A Systematic Review. Life, 12(6), 826. https://doi.org/10.3390/life12060826








