A Holistic View of Advanced Heart Failure
Abstract
:1. Introduction
2. Pathophysiology
3. Clinical Manifestations
4. Evaluation of Ventricular Systolic Function
4.1. Left Ventricular Ejection Fraction
4.2. Longitudinal Strain
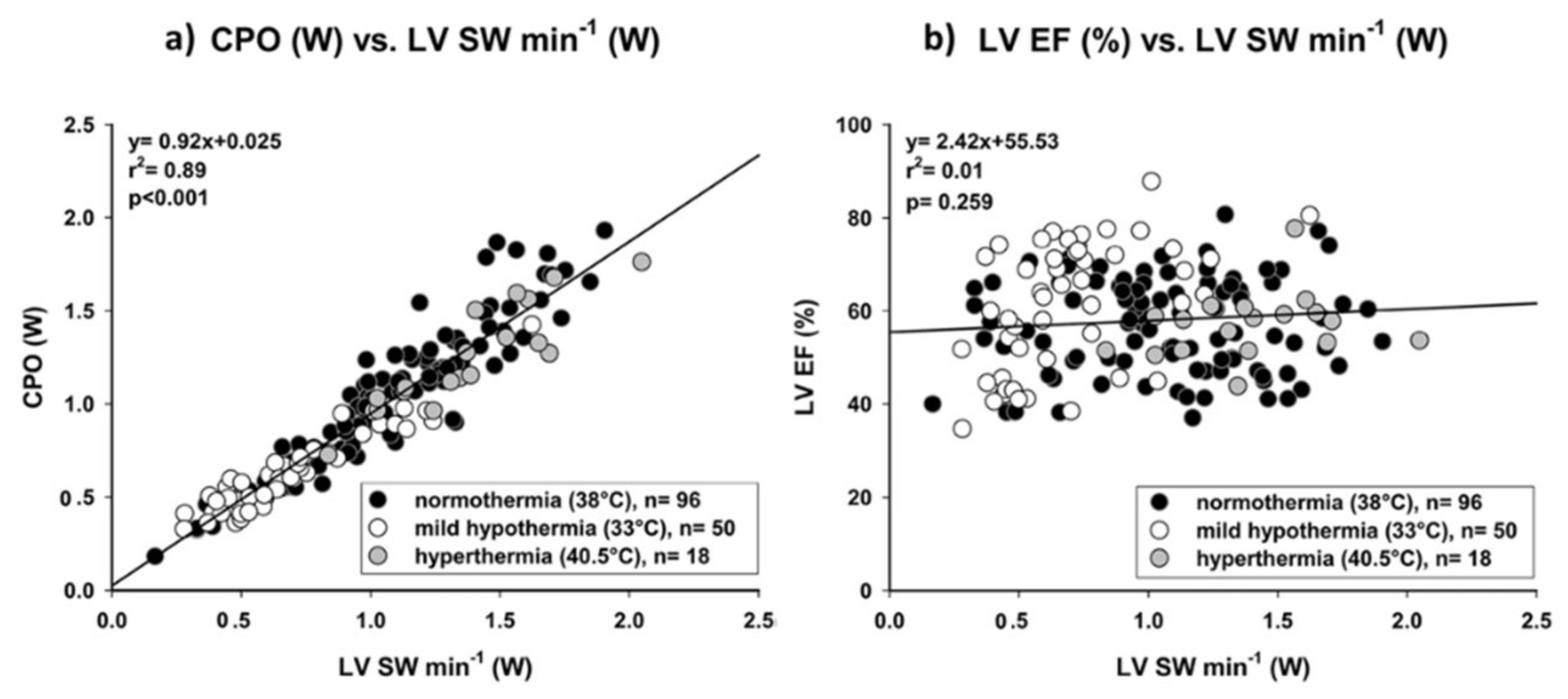
4.3. Cardiac Power Output
5. Treatment
5.1. Conventional Treatment
5.2. Advanced Treatment
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Solomon, S.D.; Dobson, J.; Pocock, S.; Skali, H.; Mcmurray, J.; Granger, C.B.; Yusuf, S.; Swedberg, K.; Young, J.B.; Michelson, E.L.; et al. Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation 2007, 116, 1482–1487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Setoguchi, S.; Stevenson, L.W.; Schneeweiss, S. Repeated hospitalizations predict mortality in the community population with heart failure. Am. Heart J. 2007, 154, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Ammar, K.A.; Jacobsen, S.J.; Mahoney, D.W.; Kors, J.A.; Redfield, M.M.; Burnett, J.C., Jr.; Rodeheffer, R.J. Prevalence and prognostic significance of heart failure stages: Application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation 2007, 115, 1563–1570. [Google Scholar] [CrossRef]
- Fang, J.C.; Ewald, G.A.; Allen, L.A.; Butler, J.; Canary, C.A.W.; Colvin-Adams, M.; Dickinson, M.G.; Levy, P.; Stough, W.G.; Sweitzer, N.K.; et al. Advanced (stage D) heart failure: A statement from the Heart Failure Society of America Guidelines Committee. J. Card. Fail. 2015, 21, 519–534. [Google Scholar] [CrossRef] [PubMed]
- Crespo-Leiro, M.G.; Metra, M.; Lund, L.H.; Milicic, D.; Costanzo, M.R.; Filippatos, G.; Gustafsson, F.; Tsui, S.; Barge-Caballero, E.; De Jonge, N.; et al. Advanced heart failure: A position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 1505–1535. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, L.W.; Pagani, F.D.; Young, J.B.; Jessup, M.; Miller, L.; Kormos, R.L.; Naftel, D.C.; Ulisney, K.; Desvigne-Nickens, P.; Kirklin, J.K. INTERMACS profiles of advanced heart failure: The current picture. J. Heart Lung Transplant. 2009, 28, 535–541. [Google Scholar] [CrossRef]
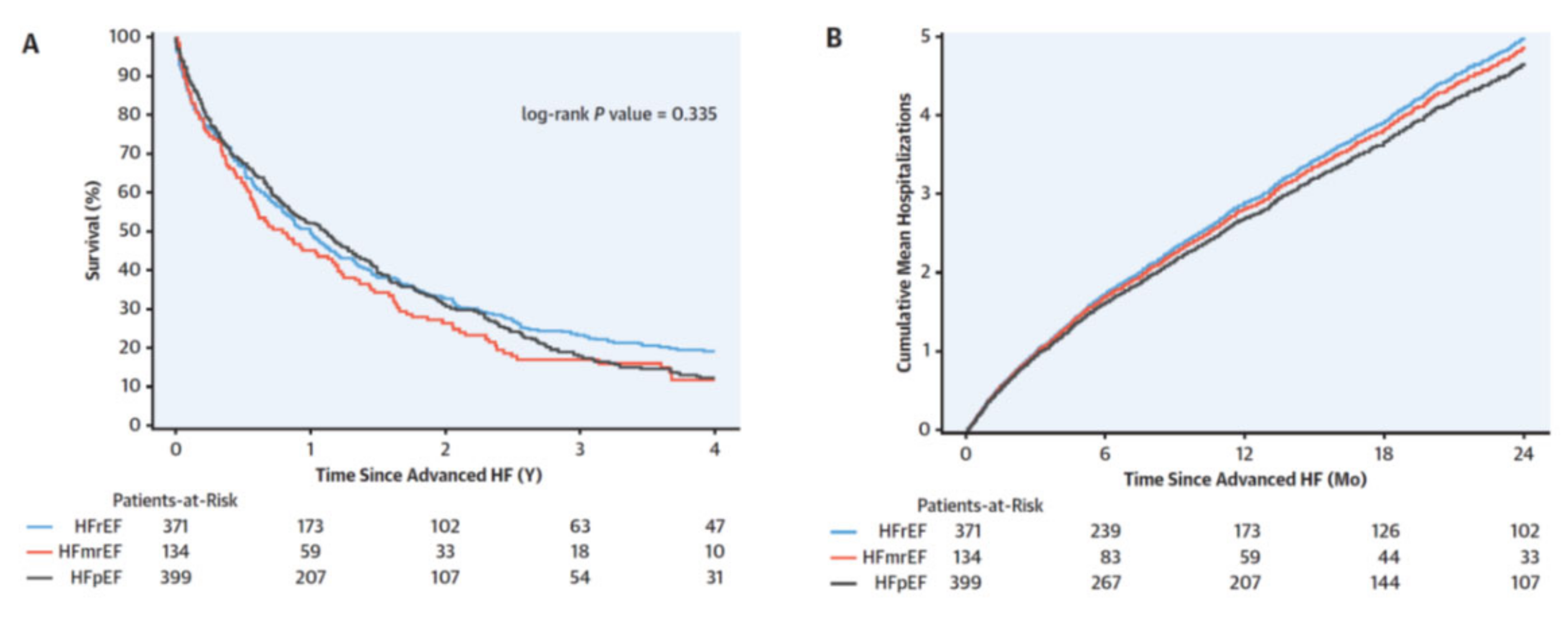
- Dunlay, S.; Roger, V.; Killian, J.; Weston, S.; Schulte, P.; Subramaniam, A.; Blecker, S.; Redfield, M. Advanced Heart Failure Epidemiology and Outcomes: A Population-Based Study. JACC Heart Fail. 2021, 9, 722–732. [Google Scholar] [CrossRef]
- Subramaniam, A.V.; Weston, S.A.; Killian, J.M.; Schulte, P.J.; Roger, V.L.; Redfield, M.M.; Blecker, S.B.; Dunlay, S.M. Development of Advanced Heart Failure: A Population-Based Study. Circ. Heart Fail. 2022, 15, e009218. [Google Scholar] [CrossRef]
- Biegus, J.; Niewinski, P.; Josiak, K.; Kulej, K.; Ponikowska, B.; Nowak, K.; Zymlinski, R.; Ponikowski, P. Pathophysiology of Advanced Heart Failure: What Knowledge Is Needed for Clinical Management? Heart Fail. Clin. 2021, 17, 519–531. [Google Scholar] [CrossRef]
- Triposkiadis, F.; Butler, J.; Abboud, F.M.; Armstrong, P.W.; Adamopoulos, S.; Atherton, J.J.; Backs, J.; Bauersachs, J.; Burkhoff, D.; Bonow, R.O.; et al. The continuous heart failure spectrum: Moving beyond an ejection fraction classification. Eur. Heart J. 2019, 40, 2155–2163. [Google Scholar] [CrossRef]
- Miller, W.L. Fluid Volume Overload and Congestion in Heart Failure: Time to Reconsider Pathophysiology and How Volume Is Assessed. Circ. Heart Fail. 2016, 9, e002922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fudim, M.; Hernandez, A.F.; Felker, G.M. Role of Volume Redistribution in the Congestion of Heart Failure. J. Am. Heart Assoc. 2017, 6, e006817. [Google Scholar] [CrossRef] [PubMed]
- Mullens, W.; Abrahams, Z.; Francis, G.S.; Sokos, G.; Taylor, D.O.; Starling, R.C.; Young, J.B.; Tang, W.H.W. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J. Am. Coll. Cardiol. 2009, 53, 589–596. [Google Scholar] [CrossRef] [Green Version]
- Husain-Syed, F.; Gröne, H.; Assmus, B.; Bauer, P.; Gall, H.; Seeger, W.; Ghofrani, A.; Ronco, C.; Birk, H. Congestive nephropathy: A neglected entity? Proposal for diagnostic criteria and future perspectives. ESC Heart Fail. 2021, 8, 183–203. [Google Scholar] [CrossRef] [PubMed]
- Boorsma, E.M.; Ter Maaten, J.M.; Voors, A.A.; van Veldhuisen, D.J. Renal Compression in Heart Failure: The Renal Tamponade Hypothesis. JACC Heart Fail. 2022, 10, 175–183. [Google Scholar] [CrossRef]
- Xanthopoulos, A.; Starling, R.C.; Kitai, T.; Triposkiadis, F. Heart Failure and Liver Disease: Cardiohepatic Interactions. JACC Heart Fail. 2019, 7, 87–97. [Google Scholar] [CrossRef]
- Ghio, S.; Gavazzi, A.; Campana, C.; Inserra, C.; Klersy, C.; Sebastiani, R.; Arbustini, E.; Recusani, F.; Tavazzi, L. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J. Am. Coll. Cardiol. 2001, 37, 183–188. [Google Scholar] [CrossRef] [Green Version]
- De Groote, P.; Millaire, A.; Foucher-Hossein, C.; Nugue, O.; Marchandise, X.; Ducloux, G.; Lablanche, J.M. Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J. Am. Coll. Cardiol. 1998, 32, 948–954. [Google Scholar] [CrossRef] [Green Version]
- Guerrero-Miranda, C.Y.; Hall, S.A. Cardiogenic Shock in Patients with Advanced Chronic Heart Failure. Methodist Debakey Cardiovasc. J. 2020, 16, 22–26. [Google Scholar] [CrossRef]
- Rihal, C.S.; Naidu, S.S.; Givertz, M.M.; Szeto, W.Y.; Burke, J.A.; Kapur, N.K.; Kern, M.; Garratt, K.N.; Goldstein, J.A.; Dimas, V.; et al. 2015 SCAI/ACC/HFSA/STS Clinical Expert Consensus Statement on the Use of Percutaneous Mechanical Circulatory Support Devices in Cardiovascular Care: Endorsed by the American Heart Association, the Cardiological Society of India, and Sociedad Latino Americana de Cardiologia Intervencionista; Affirmation of Value by the Canadian Association of Interventional Cardiology-Association Canadienne de Cardiologie d’intervention. J. Am. Coll. Cardiol. 2015, 65, 2140–2141. [Google Scholar]
- Abraham, J.; Blumer, V.; Burkhoff, D.A.N.; Pahuja, M.; Sinha, S.S.; Rosner, C.; Vorovich, E.; Grafton, G.; Bagnola, A.; Hernandez-Montfort, J.A.; et al. Heart Failure-Related Cardiogenic Shock: Pathophysiology, Evaluation and Management Considerations: Review of Heart Failure-Related Cardiogenic Shock. J. Card. Fail. 2021, 27, 1126–1140. [Google Scholar] [CrossRef] [PubMed]
- Jentzer, J.C.; Lawler, P.R.; Van Diepen, S.; Henry, T.D.; Menon, V.; Baran, D.A.; Džavík, V.; Barsness, G.W.; Holmes, D.R., Jr.; Kashani, K.B. Systemic Inflammatory Response Syndrome Is Associated with Increased Mortality Across the Spectrum of Shock Severity in Cardiac Intensive Care Patients. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e006956. [Google Scholar] [CrossRef] [PubMed]
- Severino, P.; D’Amato, A.; Prosperi, S.; Dei Cas, A.; Mattioli, A.V.; Cevese, A.; Novo, G.; Prat, M.; Pedrinelli, R.; Raddino, R.; et al. Do the Current Guidelines for Heart Failure Diagnosis and Treatment Fit with Clinical Complexity? J. Clin. Med. 2022, 11, 857. [Google Scholar] [CrossRef] [PubMed]
- Klindtworth, K.; Oster, P.; Hager, K.; Krause, O.; Bleidorn, J.; Schneider, N. Living with and dying from advanced heart failure: Understanding the needs of older patients at the end of life. BMC Geriatr. 2015, 15, 125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vijayakrishnan, R.; Steinhubl, S.R.; Ng, K.; Sun, J.; Byrd, R.J.; Daar, Z.; Williams, B.A.; de Filippi, C.; Ebadollahi, S.; Stewart, W.F. Prevalence of heart failure signs and symptoms in a large primary care population identified through the use of text and data mining of the electronic health record. J. Card. Fail. 2014, 20, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Fuentes-Abolafio, I.J.; Stubbs, B.; Pérez-Belmonte, L.M.; Bernal-López, M.R.; Gómez-Huelgas, R.; Cuesta-Vargas, A.I. Physical functional performance and prognosis in patients with heart failure: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2020, 20, 512. [Google Scholar] [CrossRef]
- Metra, M.; Dinatolo, E.; Dasseni, N. The New Heart Failure Association Definition of Advanced Heart Failure. Card. Fail. Rev. 2019, 5, 5–8. [Google Scholar] [CrossRef] [Green Version]
- Manisty, C.H.; Francis, D.P. Ejection fraction: A measure of desperation? Heart 2008, 94, 400–401. [Google Scholar] [CrossRef] [Green Version]
- Konstam, M.A.; Abboud, F.M. Ejection Fraction: Misunderstood and Overrated (Changing the Paradigm in Categorizing Heart Failure). Circulation 2017, 135, 717–719. [Google Scholar] [CrossRef] [Green Version]
- Triposkiadis, F.; Giamouzis, G.; Boudoulas, K.D.; Karagiannis, G.; Skoularigis, J.; Boudoulas, H.; Parissis, J. Left ventricular geometry as a major determinant of left ventricular ejection fraction: Physiological considerations and clinical implications. Eur. J. Heart Fail. 2018, 20, 436–444. [Google Scholar] [CrossRef] [Green Version]
- MacIver, D.H.; Townsend, M. A novel mechanism of heart failure with normal ejection fraction. Heart 2008, 94, 446–449. [Google Scholar] [CrossRef] [PubMed]
- Abou, R.; Van Der Bijl, P.; Bax, J.J.; Delgado, V. Global longitudinal strain: Clinical use and prognostic implications in contemporary practice. Heart 2020, 106, 1438–1444. [Google Scholar] [CrossRef] [PubMed]
- Stokke, T.M.; Hasselberg, N.E.; Smedsrud, M.K.; Sarvari, S.I.; Haugaa, K.H.; Smiseth, O.A.; Edvardsen, T.; Remme, E.W. Geometry as a Confounder When Assessing Ventricular Systolic Function: Comparison between Ejection Fraction and Strain. J. Am. Coll. Cardiol. 2017, 70, 942–954. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 16, 233–271. [Google Scholar]
- Park, J.J.; Park, J.B.; Park, J.H.; Cho, G.Y. Global Longitudinal Strain to Predict Mortality in Patients with Acute Heart Failure. J. Am. Coll. Cardiol. 2018, 71, 1947–1957. [Google Scholar] [CrossRef]
- Park, J.J.; Mebazaa, A.; Hwang, I.C.; Park, J.B.; Park, J.H.; Cho, G.Y. Phenotyping Heart Failure According to the Longitudinal Ejection Fraction Change: Myocardial Strain, Predictors, and Outcomes. J. Am. Heart Assoc. 2020, 9, e015009. [Google Scholar] [CrossRef]
- Tröbs, S.-O.; Prochaska, J.H.; Schwuchow-Thonke, S.; Schulz, A.; Müller, F.; Heidorn, M.W.; Göbel, S.; Diestelmeier, S.; Monteverde, J.L.; Lackner, K.J.; et al. Association of Global Longitudinal Strain with Clinical Status and Mortality in Patients with Chronic Heart Failure. JAMA Cardiol. 2021, 6, 448–456. [Google Scholar] [CrossRef]
- Negishi, T.; Negishi, K.; Thavendiranathan, P.; Cho, G.-Y.; Popescu, B.A.; Vinereanu, D.; Kurosawa, K.; Penicka, M.; Marwick, T.H.; Aakhus, S.; et al. Effect of Experience and Training on the Concordance and Precision of Strain Measurements. JACC Cardiovasc. Imaging 2017, 10, 518–522. [Google Scholar] [CrossRef]
- Tadic, M.; Nita, N.; Schneider, L.; Kersten, J.; Buckert, D.; Gonska, B.; Scharnbeck, D.; Reichart, C.; Belyavskiy, E.; Cuspidi, C.; et al. The Predictive Value of Right Ventricular Longitudinal Strain in Pulmonary Hypertension, Heart Failure, and Valvular Diseases. Front. Cardiovasc. Med. 2021, 8, 698158. [Google Scholar] [CrossRef]
- Badano, L.P.; Muraru, D.; Parati, G.; Haugaa, K.; Voigt, J.U. How to do right ventricular strain. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 825–827. [Google Scholar] [CrossRef]
- Badano, L.P.; Kolias, T.J.; Muraru, D.; Abraham, T.P.; Aurigemma, G.; Edvardsen, T.; D’Hooge, J.; Donal, E.; Fraser, A.G.; Marwick, T.; et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: A consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Muraru, D.; Onciul, S.; Peluso, D.; Soriani, N.; Cucchini, U.; Aruta, P.; Romeo, G.; Cavalli, G.; Iliceto, S.; Badano, L.P. Sex- and Method-Specific Reference Values for Right Ventricular Strain by 2-Dimensional Speckle-Tracking Echocardiography. Circ. Cardiovasc. Imaging 2016, 9, e003866. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cameli, M.; Lisi, M.; Righini, F.M.; Tsioulpas, C.; Bernazzali, S.; Maccherini, M.; Sani, G.; Ballo, P.; Galderisi, M.; Mondillo, S. Right ventricular longitudinal strain correlates well with right ventricular stroke work index in patients with advanced heart failure referred for heart transplantation. J. Card Fail. 2012, 18, 208–215. [Google Scholar] [CrossRef]
- Liang, L.W.; Jamil, A.; Mazurek, J.A.; Urgo, K.A.; Wald, J.; Birati, E.Y.; Han, Y. Right Ventricular Global Longitudinal Strain as a Predictor of Acute and Early Right Heart Failure Post Left Ventricular Assist Device Implantation. ASAIO J. 2021, 68, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Smiseth, O.A.; Aalen, J.M.; Skulstad, H. Heart failure and systolic function: Time to leave diagnostics based on ejection fraction? Eur. Heart J. 2021, 42, 786–788. [Google Scholar] [CrossRef] [PubMed]
- Anand, V.; Kane, G.C.; Scott, C.G.; Pislaru, S.V.; O Adigun, R.; McCully, R.B.; A Pellikka, P.; Pislaru, C. Prognostic value of peak stress cardiac power in patients with normal ejection fraction undergoing exercise stress echocardiography. Eur. Heart J. 2021, 42, 776–785. [Google Scholar] [CrossRef]
- Klasnja, A.V.; Jakovljevic, D.G.; Barak, O.F.; Gacesa, J.Z.P.; Lukac, D.D.; Grujic, N.G. Cardiac power output and its response to exercise in athletes and non-athletes. Clin. Physiol. Funct. Imaging 2013, 33, 201–205. [Google Scholar] [CrossRef]
- Abawi, D.; Faragli, A.; Schwarzl, M.; Manninger, M.; Zweiker, D.; Kresoja, K.-P.; Verderber, J.; Zirngast, B.; Maechler, H.; Steendijk, P.; et al. Cardiac power output accurately reflects external cardiac work over a wide range of inotropic states in pigs. BMC Cardiovasc. Disord. 2019, 19, 217. [Google Scholar] [CrossRef] [Green Version]
- Pugliese, N.R.; Fabiani, I.; Mandoli, G.E.; Guarini, G.; Galeotti, G.G.; Miccoli, M.; Lombardo, A.; Simioniuc, A.; Bigalli, G.; Pedrinelli, R.; et al. Echo-derived peak cardiac power output-to-left ventricular mass with cardiopulmonary exercise testing predicts outcome in patients with heart failure and depressed systolic function. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 700–708. [Google Scholar] [CrossRef]
- Dini, F.L. Assessment of cardiac dynamics during stress echocardiography by the peak power output-to-left ventricular mass ratio. Future Cardiol. 2011, 7, 347–356. [Google Scholar] [CrossRef]
- Lang, C.C.; Karlin, P.; Haythe, J.; Lim, T.K.; Mancini, D.M. Peak cardiac power output, measured noninvasively, is a powerful predictor of outcome in chronic heart failure. Circ. Heart Fail. 2009, 2, 33–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, S.; Cooke, G.; Wright, D.; Parsons, W.; Riley, R.; Marshall, P.; Tan, L.-B. Peak exercise cardiac power output; a direct indicator of cardiac function strongly predictive of prognosis in chronic heart failure. Eur. Heart J. 2001, 22, 1496–1503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tehrani, B.N.; Truesdell, A.G.; Sherwood, M.; Desai, S.; Tran, H.A.; Epps, K.C.; Singh, R.; Psotka, M.; Shah, P.; Cooper, L.B.; et al. Standardized Team-Based Care for Cardiogenic Shock. J. Am. Coll. Cardiol. 2019, 73, 1659–1669. [Google Scholar] [CrossRef]
- Fincke, R.; Hochman, J.S.; Lowe, A.M.; Menon, V.; Slater, J.N.; Webb, J.G.; LeJemtel, T.H.; Cotter, G. Cardiac power is the strongest hemodynamic correlate of mortality in cardiogenic shock: A report from the SHOCK trial registry. J. Am. Coll. Cardiol. 2004, 44, 340–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rab, T.; Ratanapo, S.; Kern, K.B.; Basir, M.B.; McDaniel, M.; Meraj, P.; King, S.B., 3rd; O’Neill, W. Cardiac Shock Care Centers: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2018, 72, 1972–1980. [Google Scholar] [CrossRef]
- Vahdatpour, C.; Collins, D.; Goldberg, S. Cardiogenic Shock. J. Am. Heart Assoc. 2019, 8, e011991. [Google Scholar] [CrossRef] [Green Version]
- Harada, T.; Yamaguchi, M.; Omote, K.; Iwano, H.; Mizuguchi, Y.; Amanai, S.; Yoshida, K.; Kato, T.; Kurosawa, K.; Nagai, T.; et al. Cardiac Power Output Is Independently and Incrementally Associated with Adverse Outcomes in Heart Failure with Preserved Ejection Fraction. Circ. Cardiovasc. Imaging 2022, 15, e013495. [Google Scholar] [CrossRef]
- Vonk Noordegraaf, A.; Westerhof, B.E.; Westerhof, N. The Relationship between the Right Ventricle and its Load in Pulmonary Hypertension. J. Am. Coll. Cardiol. 2017, 69, 236–243. [Google Scholar] [CrossRef]
- Yildiz, O.; Yenigun, C.D. Prognostic Value of Right Ventricular Cardiac Power Output at Rest in Patients with Advanced Heart Failure. Acta Cardiol. Sin. 2021, 37, 404–411. [Google Scholar]
- Triposkiadis, F.; Xanthopoulos, A.; Starling, R.C. Medical Treatment of Heart Failure: Ignore the Ejection Fraction and Treat All? J. Card. Fail. 2021, 27, 907–909. [Google Scholar] [CrossRef]
- Wilcox, C.S.; Testani, J.M.; Pitt, B. Pathophysiology of Diuretic Resistance and Its Implications for the Management of Chronic Heart Failure. Hypertension 2020, 76, 1045–1054. [Google Scholar] [CrossRef] [PubMed]
- Ellison, D.H.; Felker, G.M. Diuretic Treatment in Heart Failure. N. Engl. J. Med. 2017, 377, 1964–1975. [Google Scholar] [CrossRef] [PubMed]
- Vargo, D.L.; Kramer, W.G.; Rn, P.K.B.; Smith, W.B.; Serpas, T.; Brater, D.C. Bioavailability, pharmacokinetics, and pharmacodynamics of torsemide and furosemide in patients with congestive heart failure. Clin. Pharmacol. Ther. 1995, 57, 601–609. [Google Scholar] [CrossRef]
- Charokopos, A.; Griffin, M.; Rao, V.S.; Inker, L.; Sury, K.; Asher, J.; Turner, J.; Mahoney, D.; Cox, Z.L.; Wilson, F.P.; et al. Serum and Urine Albumin and Response to Loop Diuretics in Heart Failure. Clin. J. Am. Soc. Nephrol. 2019, 14, 712–718. [Google Scholar] [CrossRef]
- Blázquez-Bermejo, Z.; Farré, N.; Llagostera, M.; Perez, P.C.; Morán-Fernández, L.; Fort, A.; De-Juan, J.; Ruiz, S.; Delgado, J.F. The development of chronic diuretic resistance can be predicted during a heart-failure hospitalization. Results from the REDIHF registry. PLoS ONE 2020, 15, e0240098. [Google Scholar] [CrossRef]
- Côté, J.-M.; Bouchard, J.; Murray, P.T.; Beaubien-Souligny, W. Diuretic strategies in patients with resistance to loop-diuretics in the intensive care unit: A retrospective study from the MIMIC-III database. J. Crit. Care 2021, 65, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Cox, Z.L.; Sarrell, B.A.; Cella, M.K.; Tucker, B.; Arroyo, J.P.; Umanath, K.; Tidwell, W.; Guide, A.; Testani, J.M.; Lewis, J.B.; et al. Multinephron Segment Diuretic Therapy to Overcome Diuretic Resistance in Acute Heart Failure: A Single-Center Experience. J. Card. Fail. 2022, 28, 21–31. [Google Scholar] [CrossRef]
- Nizamic, T.; Murad, M.H.; Allen, L.A.; McIlvennan, C.K.; Wordingham, S.E.; Matlock, D.D.; Dunlay, S.M. Ambulatory Inotrope Infusions in Advanced Heart Failure: A Systematic Review and Meta-Analysis. JACC Heart Fail. 2018, 6, 757–767. [Google Scholar] [CrossRef]
- Farmakis, D.; Agostoni, P.; Baholli, L.; Bautin, A.; Comin-Colet, J.; Crespo-Leiro, M.G.; Fedele, F.; García-Pinilla, J.M.; Giannakoulas, G.; Grigioni, F.; et al. A pragmatic approach to the use of inotropes for the management of acute and advanced heart failure: An expert panel consensus. Int. J. Cardiol. 2019, 297, 83–90. [Google Scholar] [CrossRef] [Green Version]
- Altenberger, J.; Gustafsson, F.; Harjola, V.-P.; Karason, K.; Kindgen-Milles, D.; Kivikko, M.; Malfatto, G.; Papp, Z.; Parissis, J.; Pollesello, P.; et al. Levosimendan in Acute and Advanced Heart Failure: An Appraisal of the Clinical Database and Evaluation of Its Therapeutic Applications. J. Cardiovasc. Pharmacol. 2018, 71, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Milwidsky, A.; Frydman, S.; Laufer-Perl, M.; Sadeh, B.; Sapir, O.; Granot, Y.; Hochstadt, A.; Korotetski, L.; Ketchker, L.; Topilsky, Y.; et al. Intermittent inotropic therapy with levosimendan vs. milrinone in advanced heart failure patients. ESC Heart Fail. 2022, 9, 1487–1491. [Google Scholar] [CrossRef] [PubMed]
- Burkhoff, D.; Borlaug, B.A.; Shah, S.J.; Zolty, R.; Tedford, R.J.; Thenappan, T.; Zamanian, R.T.; Mazurek, J.A.; Rich, J.D.; Simon, M.C.; et al. Levosimendan Improves Hemodynamics and Exercise Tolerance in PH-HFpEF: Results of the Randomized Placebo-Controlled HELP Trial. JACC Heart Fail. 2021, 9, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Nanayakkara, S.; Byrne, M.; Mak, V.; Carter, K.; Dean, E.; Kaye, D.M. Extended-Release Oral Milrinone for the Treatment of Heart Failure with Preserved Ejection Fraction. J. Am. Heart Assoc. 2020, 9, e015026. [Google Scholar] [CrossRef]
- Litwin, S.E.; Zile, M.R. The Vexing Problem of HFpEF Therapeutics: Inching Toward Success. JACC Heart Fail. 2021, 9, 371–373. [Google Scholar] [CrossRef] [PubMed]
- Glikson, M.; Nielsen, J.C.; Kronborg, M.B.; Michowitz, Y.; Auricchio, A.; Barbash, I.M.; Barrabés, J.A.; Boriani, G.; Braunschweig, F.; Brignole, M.; et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur. Heart J. 2021, 42, 3427–3520. [Google Scholar] [CrossRef]
- Vogler, J.; Keelani, A.; Traub, A.; Tilz, R.R. ESC guidelines 2021 on cardiac pacing and cardiac resynchronization therapy: What’s new? Herz 2022, 47, 31–40. [Google Scholar] [CrossRef]
- Fudim, M.; Ali-Ahmed, F.; Parzynski, C.S.; Ambrosy, A.P.; Friedman, D.J.; Pokorney, S.D.; Curtis, J.P.; Fonarow, G.C.; Masoudi, F.A.; Hernandez, A.F.; et al. Periprocedural Risk and Survival Associated with Implantable Cardioverter-Defibrillator Placement in Older Patients with Advanced Heart Failure. JAMA Cardiol. 2020, 5, 643–651. [Google Scholar] [CrossRef]
- Kapur, N.K.; Esposito, M.L.; Bader, Y.; Morine, K.J.; Kiernan, M.S.; Pham, D.T.; Burkhoff, D. Mechanical Circulatory Support Devices for Acute Right Ventricular Failure. Circulation 2017, 136, 314–326. [Google Scholar] [CrossRef] [Green Version]
- Combes, A.; Price, S.; Slutsky, A.S.; Brodie, D. Temporary circulatory support for cardiogenic shock. Lancet 2020, 396, 199–212. [Google Scholar] [CrossRef]
- Thiele, H.; Ohman, E.M.; De Waha-Thiele, S.; Zeymer, U.; Desch, S. Management of cardiogenic shock complicating myocardial infarction: An update 2019. Eur. Heart J. 2019, 40, 2671–2683. [Google Scholar] [CrossRef] [Green Version]
- Esposito, M.; Bader, Y.; Pedicini, R.; Breton, C.; Mullin, A.; Kapur, N.K. The role of acute circulatory support in ST-segment elevation myocardial infarction complicated by cardiogenic shock. Indian Heart J. 2017, 69, 668–674. [Google Scholar] [CrossRef] [PubMed]
- Jiritano, F.; Coco, V.L.; Matteucci, M.; Fina, D.; Willers, A.; Lorusso, R. Temporary Mechanical Circulatory Support in Acute Heart Failure. Card. Fail. Rev. 2020, 6, e01. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frigerio, M. Left Ventricular Assist Device: Indication, Timing, and Management. Heart Fail. Clin. 2021, 17, 619–634. [Google Scholar] [CrossRef] [PubMed]
- Rajapreyar, I.; Kumar, S.; Rao, R.A. Ambulatory advanced heart failure patients: Timing of mechanical circulatory support—Delaying the inevitable? Curr. Opin. Cardiol. 2021, 36, 186–197. [Google Scholar] [CrossRef]
- Kawabori, M.; Kurihara, C.; Conyer, R.; Sugiura, T.; Critsinelis, A.C.; Lee, V.-V.; Civitello, A.B.; Morgan, J.A. A left ventricular end-diastolic dimension less than 6.0 cm is associated with mortality after implantation of an axial-flow pump. J. Thorac. Cardiovasc. Surg. 2019, 157, 2302–2310. [Google Scholar] [CrossRef] [PubMed]
- Truong, V.T.; Shreenivas, S.; Mazur, W.; Egnaczyk, G.F.; Palmer, C.; Rao, S.D.; Rame, J.E.; Chung, E.S. Left Ventricular End-Diastolic Dimension and Clinical Outcomes After Centrifugal Flow Left Ventricular Assist Device Implantation. ASAIO J. 2022, 68, 220–225. [Google Scholar] [CrossRef]
- Molina, E.; Jain, A.; Ahmed, S.; Lam, P.; Rao, S.; Hockstein, M.; Kadakkal, A.; Hofmeyer, M.; Rodrigo, M.; Chou, J.; et al. The impact of left ventricular size on outcomes after centrifugal-flow left ventricular assist device implantation. Eur. J. Cardiothorac. Surg. 2021, 62, ezab480. [Google Scholar] [CrossRef]
- Pagani, F.D. Commentary: Left ventricular size and left ventricular assist device support outcomes: Bigger is better? J. Thorac. Cardiovasc. Surg. 2019, 157, 2313–2314. [Google Scholar] [CrossRef] [Green Version]
- Chivukula, V.K.; Beckman, J.A.; Prisco, A.R.; Lin, S.; Dardas, T.F.; Cheng, R.; Farris, S.D.; Smith, J.W.; Mokadam, N.A.; Mahr, C.; et al. Small Left Ventricular Size Is an Independent Risk Factor for Ventricular Assist Device Thrombosis. ASAIO J. 2019, 65, 152–159. [Google Scholar] [CrossRef]
- Gude, E.; Fiane, A.E. Can mechanical circulatory support be an effective treatment for HFpEF patients? Heart Fail. Rev. 2021. online ahead of print. [Google Scholar] [CrossRef]
- Kirklin, J.K.; Pagani, F.D.; Kormos, R.L.; Stevenson, L.W.; Blume, E.D.; Myers, S.L.; Miller, M.A.; Baldwin, J.T.; Young, J.B.; Naftel, D.C. Eighth annual INTERMACS report: Special focus on framing the impact of adverse events. J. Heart Lung Transpl. 2017, 36, 1080–1086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LaRue, S.J.; Raymer, D.S.; Pierce, B.R.; Nassif, M.E.; Sparrow, C.T.; Vader, J.M. Clinical outcomes associated with INTERMACS-defined right heart failure after left ventricular assist device implantation. J. Heart Lung Transpl. 2017, 36, 475–477. [Google Scholar] [CrossRef] [PubMed]
- Kirklin, J.K.; Xie, R.; Cowger, J.; de By, T.M.; Nakatani, T.; Schueler, S.; Taylor, R.; Lannon, J.; Mohacsi, P.; Gummert, J.; et al. Second annual report from the ISHLT Mechanically Assisted Circulatory Support Registry. J. Heart Lung Transpl. 2018, 37, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Frankfurter, C.; Molinero, M.; Vishram-Nielsen, J.K.; Foroutan, F.; Mak, S.; Rao, V.; Billia, F.; Orchanian-Cheff, A.; Alba, A.C. Predicting the Risk of Right Ventricular Failure in Patients Undergoing Left Ventricular Assist Device Implantation: A Systematic Review. Circ. Heart Fail. 2020, 13, e006994. [Google Scholar] [CrossRef]
- Topkara, V.K.; Garan, A.R.; Fine, B.; Godier-Furnémont, A.F.; Breskin, A.; Cagliostro, B.; Yuzefpolskaya, M.; Takeda, K.; Takayama, H.; Mancini, D.M.; et al. Myocardial Recovery in Patients Receiving Contemporary Left Ventricular Assist Devices: Results From the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS). Circ. Heart Fail. 2016, 9, e003157. [Google Scholar] [CrossRef] [Green Version]
- Belkin, M.N.; Kagan, V.; Labuhn, C.; Pinney, S.P.; Grinstein, J. Physiology and Clinical Utility of HeartMate Pump Parameters. J. Card. Fail. 2021, 28, 845–862. [Google Scholar] [CrossRef]
- Birks, E.J.; Drakos, S.G.; Patel, S.R.; Lowes, B.D.; Selzman, C.H.; Starling, R.C.; Trivedi, J.; Slaughter, M.S.; Alturi, P.; Goldstein, D.; et al. Prospective Multicenter Study of Myocardial Recovery Using Left Ventricular Assist Devices (RESTAGE-HF [Remission from Stage D Heart Failure]): Medium-Term and Primary End Point Results. Circulation 2020, 142, 2016–2028. [Google Scholar] [CrossRef]
- Vela, M.M.; Baston, V.R.; Panoulas, V.; Gil, F.R.; Simon, A. A detailed explantation assessment protocol for patients with left ventricular assist devices with myocardial recovery. Interact. Cardiovasc. Thorac. Surg. 2021, 32, 298–305. [Google Scholar] [CrossRef]
- Shah, P.; Psotka, M.; Taleb, I.; Alharethi, R.; Shams, M.A.; Wever-Pinzon, O.; Yin, M.; Latta, F.; Stehlik, J.; Fang, J.C.; et al. Framework to Classify Reverse Cardiac Remodeling with Mechanical Circulatory Support: The Utah-Inova Stages. Circ. Heart Fail. 2021, 14, e007991. [Google Scholar] [CrossRef]
- Rodrigues, J.C.L.; Rooms, B.; Hyde, K.; Rohan, S.; Nightingale, A.K.; Paton, J.; Manghat, N.; Bucciarelli-Ducci, C.; Hamilton, M.; Zhang, H.; et al. The corrected left ventricular ejection fraction: A potential new measure of ventricular function. Int. J. Cardiovasc. Imaging 2021, 37, 1987–1997. [Google Scholar] [CrossRef]
- Rosenbaum, A.N.; Geske, J.B.; Stulak, J.M.; Kushwaha, S.S.; Clavell, A.L.; Behfar, A. Left Ventricular Hemodynamics and Relationship with Myocardial Recovery and Optimization in Patients Supported on CF-LVAD Therapy. J. Card. Fail. 2021, 28, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Burkhoff, D.; Topkara, V.K.; Sayer, G.; Uriel, N. Reverse Remodeling with Left Ventricular Assist Devices. Circ. Res. 2021, 128, 1594–1612. [Google Scholar] [CrossRef] [PubMed]
- Khush, K.K. Donor selection in the modern era. Ann. Cardiothorac. Surg. 2018, 7, 126–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsich, E.M. Matching the Market for Heart Transplantation. Circ. Heart Fail. 2016, 9, e002679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coniglio, A.C.; Patel, C.B.; Kittleson, M.; Schlendorf, K.; Schroder, J.N.; DeVore, A.D. Innovations in Heart Transplantation: A Review. J. Card. Fail. 2021, 28, 467–476. [Google Scholar] [CrossRef] [PubMed]
- Cogswell, R.; John, R.; Estep, J.D.; Duval, S.; Tedford, R.J.; Pagani, F.D.; Martin, C.M.; Mehra, M.R. An early investigation of outcomes with the new 2018 donor heart allocation system in the United States. J. Heart Lung Transpl. 2020, 39, 1–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Estep, J.D.; Soltesz, E.; Cogswell, R. The new heart transplant allocation system: Early observations and mechanical circulatory support considerations. J. Thorac. Cardiovasc. Surg. 2020, 161, 1839–1846. [Google Scholar] [CrossRef] [PubMed]
- Ayesta, A. Influence of Sex-Mismatch on Prognosis After Heart Transplantation. Front. Cardiovasc. Med. 2021, 8, 617062. [Google Scholar] [CrossRef]
- Bergenfeldt, H.; Stehlik, J.; Hoglund, P.; Andersson, B.; Nilsson, J. Donor-recipient size matching and mortality in heart transplantation: Influence of body mass index and gender. J. Heart Lung Transpl. 2017, 36, 940–947. [Google Scholar] [CrossRef] [Green Version]
- Habal, M.V. Current Desensitization Strategies in Heart Transplantation. Front. Immunol 2021, 12, 702186. [Google Scholar] [CrossRef]
- Pinnelas, R.; Kobashigawa, J.A. Ex vivo normothermic perfusion in heart transplantation: A review of the TransMedics((R)) Organ Care System. Future Cardiol. 2022, 18, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Shu, S.; Ren, J.; Song, J. Correction to: Cardiac xenotransplantation: A promising way to treat advanced heart failure. Heart Fail. Rev. 2021, 26, 1527. [Google Scholar] [CrossRef] [PubMed]
- Pierson, R.N., III; Fishman, J.A.; Lewis, G.D.; D’Alessandro, D.A.; Connolly, M.R.; Burdorf, L.; Madsen, J.C.; Azimzadeh, A.M. Progress Toward Cardiac Xenotransplantation. Circulation 2020, 142, 1389–1398. [Google Scholar] [CrossRef] [PubMed]




| Characteristic | Comment | Clarifications |
|---|---|---|
| Admissions in hospital | Planned or unplanned |
|
| Biomarkers | High risk profile |
|
| Cardiac dysfunction | Severe structural and functional abnormalities | Ventricular dysfunction
-Severe mitral regurgitation refractory to decongestion Rhythm disturbances
|
| Diuretic resistance | Common cause of recurrent rehospitalizations and death predictor |
|
| Extracardiac organ dysfunction | When present may affect treatment options and survival |
|
| Functional capacity | Severe limitation |
|
| GMT intolerance or non-response | Inability to implement appropriate treatment (dose or drug) or treatment failure |
|
| Hemodynamic instability | Hypotension (SBP < 90 mmHg) with minimal or in the absence of medical treatment |
|
| Profile | Characteristics | Risk |
|---|---|---|
| Profile 1 | Cardiogenic hock |  |
| Profile 2 | Progressive decline | |
| Profile 3 | Stable, but Inotrope dependent | |
| Profile 4 | Resting symptoms | |
| Profile 5 | Exertion intolerant | |
| Profile 6 | Exertion limited | |
| Profile 7 | Advanced NYHA Class III |
| Old Adult Allocation System | New Adult Allocation System | Criteria |
|---|---|---|
| Status 1A | Status 1 |
|
| Status 2 |
| |
| Status 3 |
| |
| Status 1B | Status 4 |
|
| Status 2 | Diagnosis
| |
| Stage 5 |
| |
| Stage 6 |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Triposkiadis, F.; Giamouzis, G.; Kitai, T.; Skoularigis, J.; Starling, R.C.; Xanthopoulos, A. A Holistic View of Advanced Heart Failure. Life 2022, 12, 1298. https://doi.org/10.3390/life12091298
Triposkiadis F, Giamouzis G, Kitai T, Skoularigis J, Starling RC, Xanthopoulos A. A Holistic View of Advanced Heart Failure. Life. 2022; 12(9):1298. https://doi.org/10.3390/life12091298
Chicago/Turabian StyleTriposkiadis, Filippos, Grigorios Giamouzis, Takeshi Kitai, John Skoularigis, Randall C. Starling, and Andrew Xanthopoulos. 2022. "A Holistic View of Advanced Heart Failure" Life 12, no. 9: 1298. https://doi.org/10.3390/life12091298





