Metastasis of Hepatocellular Carcinoma in the Pouch of Douglas Successfully Treated by Radiation Therapy: A Case Report
Abstract
:1. Introduction
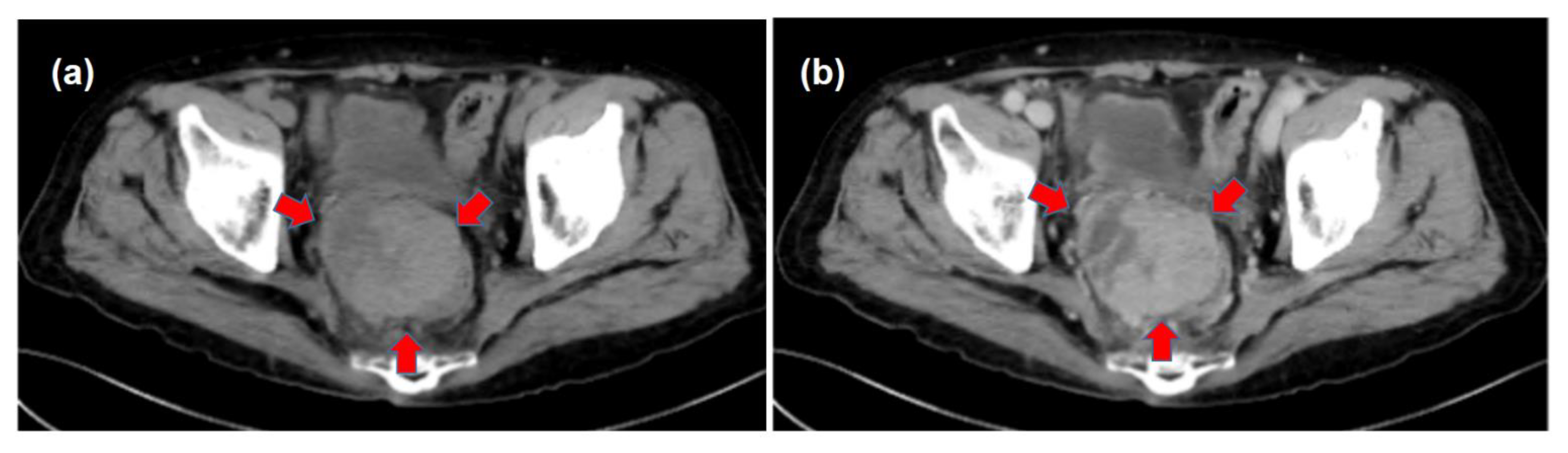
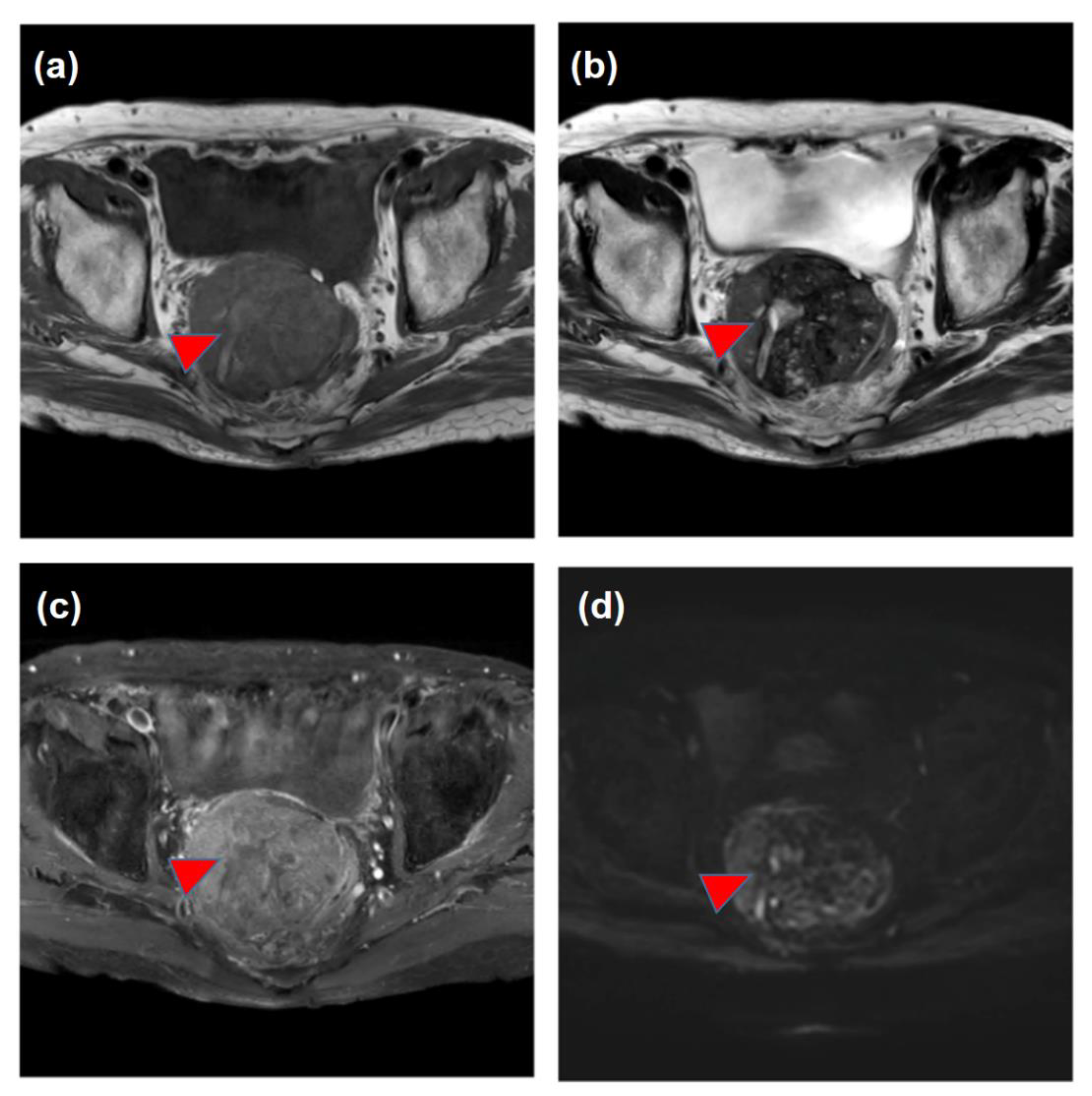
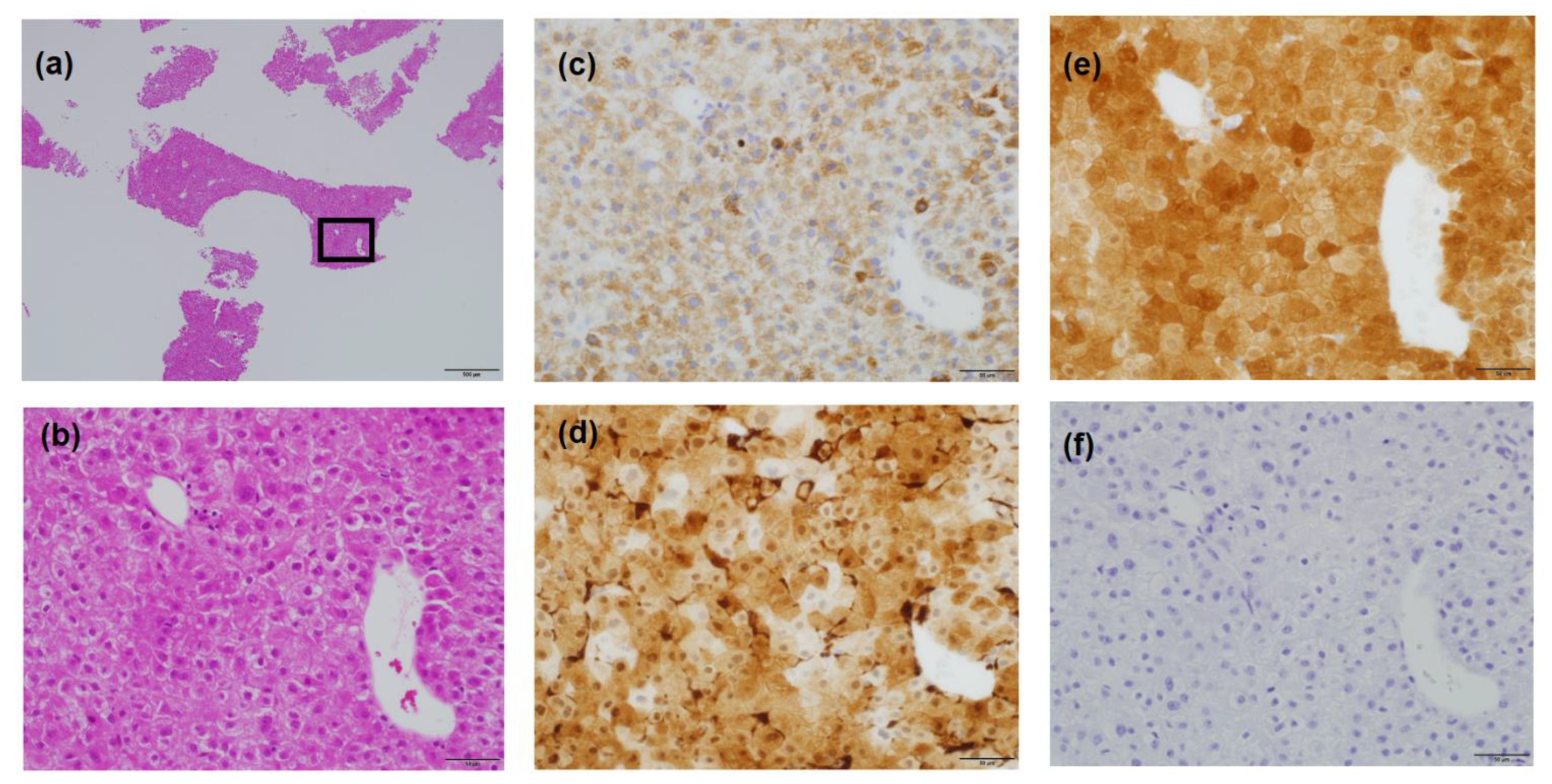
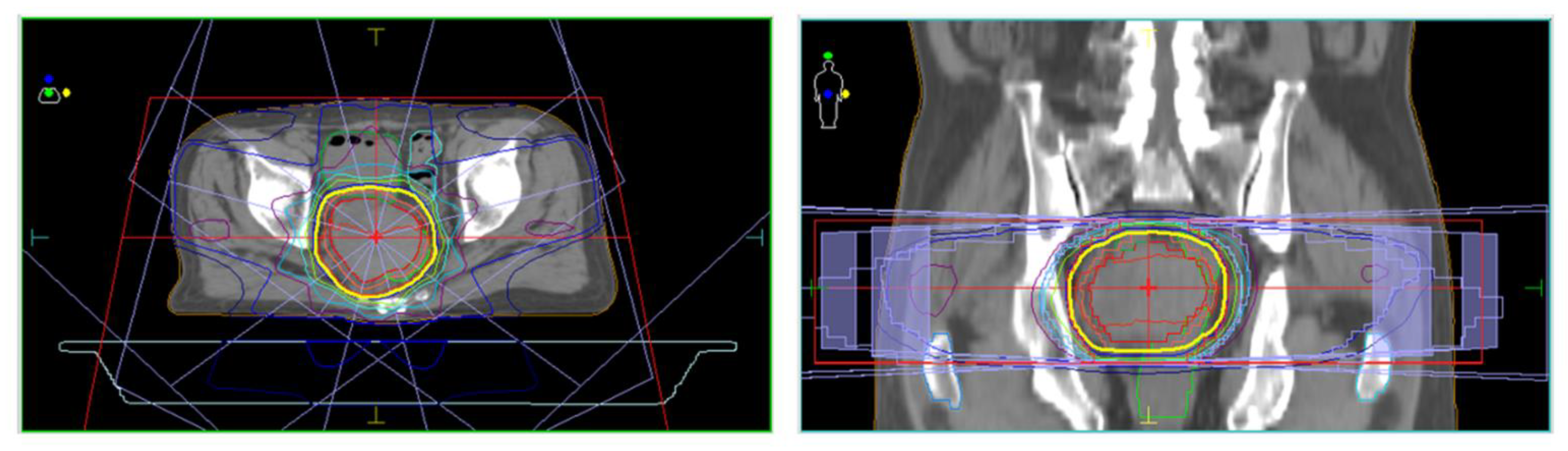
2. Case Report: Successful Radiation Therapy for the Treatment of Metastasis of Hepatocellular Carcinoma in the Pouch of Douglas (Table 1)
| Year | Month | Event |
|---|---|---|
| X-5 | The diagnosis of NASH-related liver cirrhosis | |
| January | Rupture of HCC and emergent hemostasis with TAE | |
| X-3 | May | Curative treatment of the HCC (re-TAE and additional RFA) |
| (Start of HCC follow-up in our hospital after curative therapy) | ||
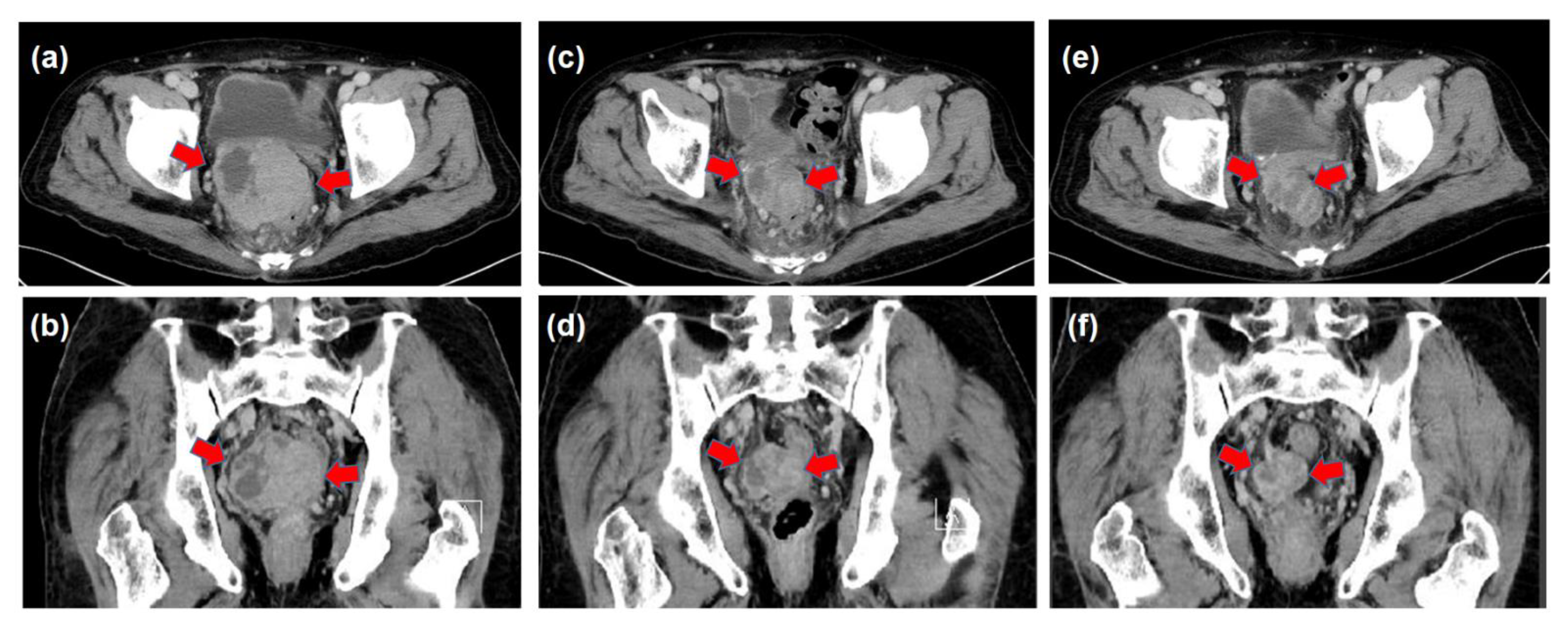
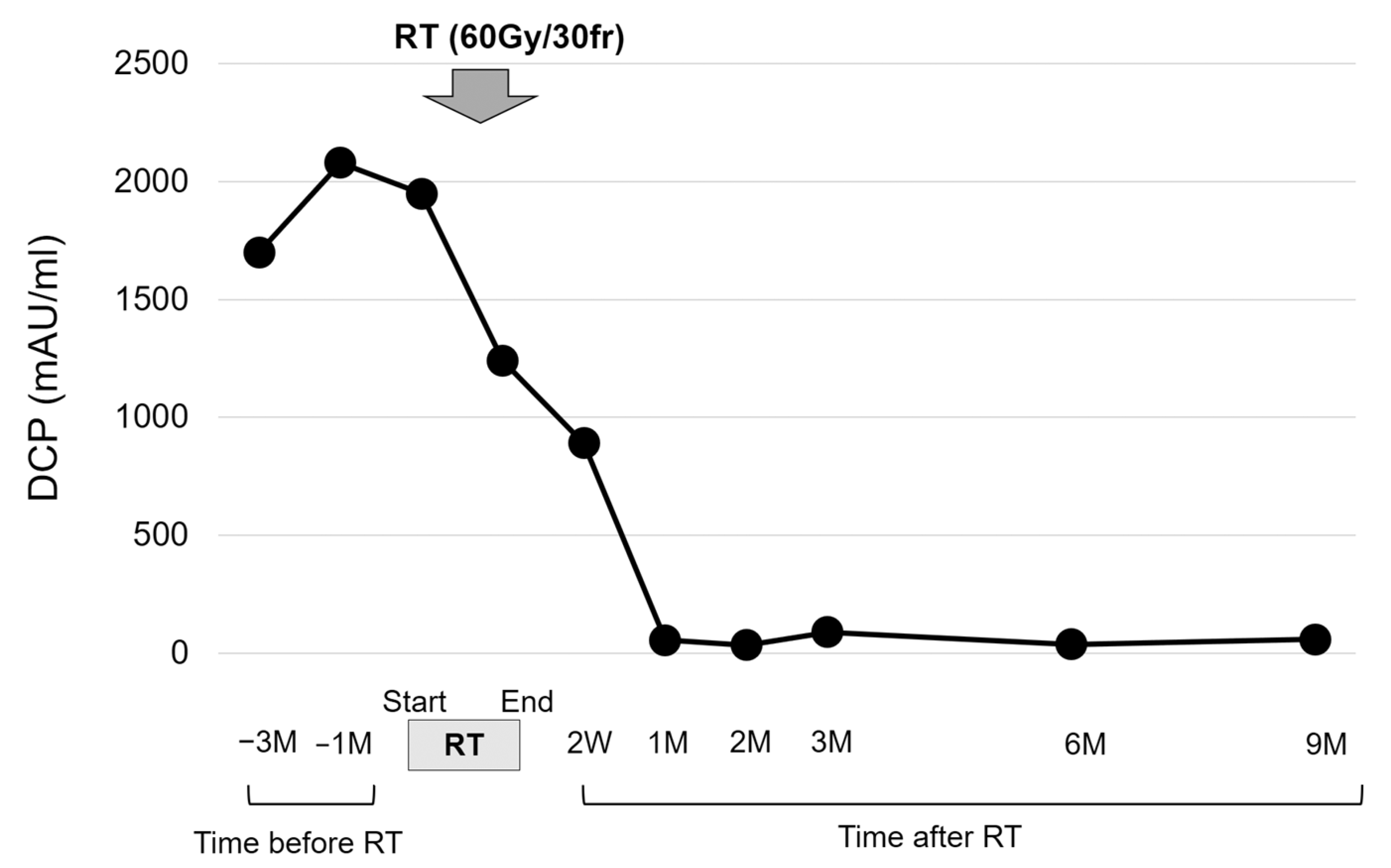
| March | Increase in the DCP and detection of the pelvic tumor Medical interview revealing mild constipation | |
| X | May | The histological diagnosis of pelvic metastasis of HCC |
| August–October | 3D-CRT (prescribed dose for the gross tumor: 60 Gy in 30 fractions) | |
| (Decrease in the tumor size and DCP values, constipation resolved) | ||
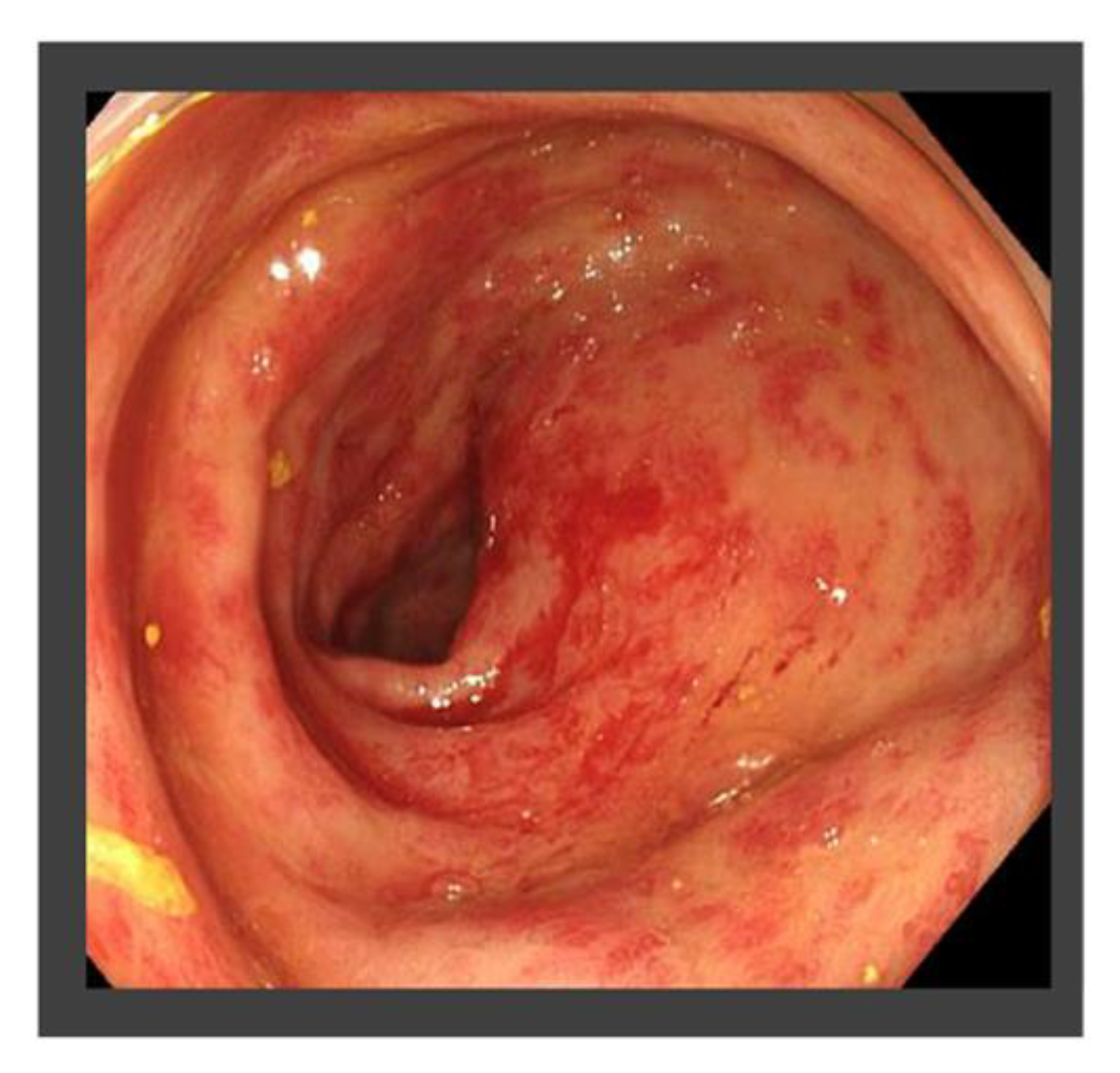
| X + 1 | July | Occasional bloody stool and the diagnosis of radiation proctitis (grade 1) by colonoscopy |
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Da Fonseca, L.G.; Leonardi, P.C.; Hashizume, P.H.; Sansone, F.; Saud, L.R.; Carrilho, F.J.; Herman, P. A multidisciplinary approach to peritoneal metastasis from hepatocellular carcinoma: Clinical features, management and outcomes. Clin. Exp. Hepatol. 2022, 8, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Matsukuma, S.; Sato, K. Peritoneal seeding of hepatocellular carcinoma: Clinicopathological characteristics of 17 autopsy cases. Pathol. Int. 2011, 61, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Kwak, M.S.; Lee, J.H.; Yoon, J.H.; Yu, S.J.; Cho, E.J.; Jang, E.S.; Kim, Y.J.; Lee, H.S. Risk factors, clinical features, and prognosis of the hepatocellular carcinoma with peritoneal metastasis. Dig. Dis. Sci. 2012, 57, 813–819. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. Electronic address: Easloffice@easloffice.eu; European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordan, J.D.; Kennedy, E.B.; Abou-Alfa, G.K.; Beg, M.S.; Brower, S.T.; Gade, T.P.; Goff, L.; Gupta, S.; Guy, J.; Harris, W.P.; et al. Systemic Therapy for Advanced Hepatocellular Carcinoma: ASCO Guideline. J. Clin. Oncol. 2020, 38, 4317–4345. [Google Scholar] [CrossRef] [PubMed]
- Enomoto, H.; Ueno, Y.; Hiasa, Y.; Nishikawa, H.; Hige, S.; Takikawa, Y.; Taniai, M.; Ishikawa, T.; Yasui, K.; Takaki, A.; et al. Transition in the etiology of liver cirrhosis in Japan: A nationwide survey. J. Gastroenterol. 2020, 55, 353–362. [Google Scholar] [PubMed] [Green Version]
- Sahu, S.K.; Chawla, Y.K.; Dhiman, R.K.; Singh, V.; Duseja, A.; Taneja, S.; Kalra, N.; Gorsi, U. Rupture of Hepatocellular Carcinoma: A Review of Literature. J. Clin. Exp. Hepatol. 2019, 9, 245–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xia, F.; Ndhlovu, E.; Zhang, M.; Chen, X.; Zhang, B.; Zhu, P. Ruptured Hepatocellular Carcinoma: Current Status of Research. Front. Oncol. 2022, 12, 848903. [Google Scholar] [CrossRef]
- Zhu, Q.; Li, J.; Yan, J.J.; Huang, L.; Wu, M.C.; Yan, Y.Q. Predictors and clinical outcomes for spontaneous rupture of hepatocellular carcinoma. World J. Gastroenterol. 2012, 18, 7302–7307. [Google Scholar] [CrossRef]
- Li, J.; Huang, L.; Liu, C.F.; Cao, J.; Yan, J.J.; Xu, F.; Wu, M.C.; Yan, Y.Q. Risk factors and surgical outcomes for spontaneous rupture of BCLC stages A and B hepatocellular carcinoma: A case-control study. World J. Gastroenterol. 2014, 20, 9121–9127. [Google Scholar]
- Feng, M.Y.; Chan, L.L.; Chan, S.L. Drug Treatment for Advanced Hepatocellular Carcinoma: First-Line and Beyond. Curr. Oncol. 2022, 29, 434. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Pinyol, R.; Kelley, R.K.; El-Khoueiry, A.; Reeves, H.L.; Wang, X.W.; Gores, G.J.; Villanueva, A. Molecular pathogenesis and systemic therapies for hepatocellular carcinoma. Nat. Cancer 2022, 3, 386–401. [Google Scholar] [CrossRef] [PubMed]
- Sonbol, M.B.; Riaz, I.B.; Naqvi, S.A.A.; Almquist, D.R.; Mina, S.; Almasri, J.; Shah, S.; Almader-Douglas, D.; Uson Junior, P.L.S.; Mahipal, A.; et al. Systemic Therapy and Sequencing Options in Advanced Hepatocellular Carcinoma: A Systematic Review and Network Meta-analysis. JAMA. Oncol. 2020, 6, e204930. [Google Scholar] [CrossRef] [PubMed]
- Chow, K.C.; Tang, C.N.; Lai, E.C.; Li, M.K. Curative treatment for recurrent tumour implantation after ruptured hepatocellular carcinoma. Hong Kong Med. J. 2013, 19, 82–84. [Google Scholar] [PubMed]
- Fang, J.Z.; Yang, Y.; Zhu, H.D.; Sun, J.N.; Mi, H.C.; Lu, C.D. Surgical Treatment of Postoperative Abdominal Metastases of Hepatocellular Carcinoma: 10-Year Experience in a Single Center. Cancer Manag. Res. 2021, 13, 8673–8683. [Google Scholar] [CrossRef] [PubMed]
- Iida, H.; Tani, M.; Aihara, T.; Hasegawa, K.; Eguchi, H.; Tanabe, M.; Yamamoto, M.; Yamaue, H. New metastasectomy criteria for peritoneal metastasis of hepatocellular carcinoma: A study of the Japanese Society of Hepato-Biliary-Pancreatic Surgery. Hepatobiliary Pancreat. Sci. 2020, 27, 673–681. [Google Scholar] [CrossRef]
- Hung, K.C.; Yang, K.L.; Huang, G.C.; Chen, Y.F.; Chang, W.T.; Chuang, C.C. Cytoreduction surgery and hyperthermic intraperitoneal chemotherapy for treating advanced peritoneal metastases of hepatocellular carcinoma. Pleura Peritoneum 2020, 5, 20190030. [Google Scholar]
- Chua, T.C.; Morris, D.L. Exploring the role of resection of extrahepatic metastases from hepatocellular carcinoma. Surg. Oncol. 2012, 21, 95–101. [Google Scholar] [CrossRef]
- Weichselbaum, R.R.; Hellman, S. Oligometastases revisited. Nat. Rev. Clin. Oncol. 2011, 8, 378–382. [Google Scholar] [CrossRef]
- Kim, K.; Kim, T.H.; Kim, T.H.; Seong, J. Efficacy of Local Therapy for Oligometastatic Hepatocellular Carcinoma: A Propensity Score Matched Analysis. J. Hepatocell. Carcinoma 2021, 8, 35–44. [Google Scholar] [CrossRef]
- Lewis, S.; Dawson, L.; Barry, A.; Stanescu, T.; Mohamad, I.; Hosni, A. Stereotactic body radiation therapy for hepatocellular carcinoma: From infancy to ongoing maturity. JHEP. Rep. 2022, 4, 100498. [Google Scholar] [CrossRef] [PubMed]
- Rim, C.H.; Seong, J. Application of radiotherapy for hepatocellular carcinoma in current clinical practice guidelines. Radiat. Oncol. J. 2016, 34, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Leone, P.; Solimando, A.G.; Fasano, R.; Argentiero, A.; Malerba, E.; Buonavoglia, A.; Lupo, L.G.; De Re, V.; Silvestris, N.; Racanelli, V. The Evolving Role of Immune Checkpoint Inhibitors in Hepatocellular Carcinoma Treatment. Vaccines 2021, 9, 532. [Google Scholar] [CrossRef] [PubMed]
- Solimando, A.G.; Susca, N.; Argentiero, A.; Brunetti, O.; Leone, P.; De Re, V.; Fasano, R.; Krebs, M.; Petracci, E.; Azzali, I.; et al. Second-line treatments for Advanced Hepatocellular Carcinoma: A Systematic Review and Bayesian Network Meta-analysis. Clin. Exp. Med. 2022, 22, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Yoshii, Y.; Okazaki, S.; Takeda, M. Current Status of Next-Generation Sequencing-Based Cancer Genome Profiling Tests in Japan and Prospects for Liquid Biopsy. Life 2021, 11, 796. [Google Scholar] [CrossRef]
- Tsumura, T.; Doi, K.; Marusawa, H. Precision Medicine of Hepatobiliary and Pancreatic Cancers: Focusing on Clinical Trial Outcomes. Cancers 2022, 14, 3674. [Google Scholar] [CrossRef]

| WBC | 2780 | /μL | (4000–9000) | T-bil | 1.6 | mg/dL | (0.2–1.2) | PT-INR | 1.28 | (0.91–1.14) | |
| RBC | 320 | ×104/μL | (410–550) | AST | 61 | U/L | (13–30) | PT% | 62.9 | % | (70–120) |
| Hb | 11.2 | g/dL | (13.0–17.0) | ALT | 57 | U/L | (10–42) | (46–260) | |||
| Hct | 33.3 | % | (35.0–51.0) | ALP | 197 | U/L | (38–113) | HBsAg | (-) | (-) | |
| Plt | 88 | ×103/μL | (150–350) | γ-GTP | 23 | U/L | (13–64) | HBsAb | (-) | (-) | |
| Alb | 2.3 | g/dL | (4.1–5.1) | HCVAb | (-) | (-) | |||||
| Na | 137 | mmol/L | (138–145) | NH3 | 146 | μg/dL | (12–66) | ||||
| K | 4.0 | mmol/L | (3.6–4.8) | CEA | 5.6 | ng/mL | (≤5.0) | ||||
| Cl | 108 | mmol/L | (101–108) | BS | 180 | mg/dL | (70–109) | CA19–9 | 16.3 | U/mL | (≤37.0) |
| BUN | 14 | mg/dL | (8–20) | HbA1c | 4.8 | % | (4.6–6.2) | AFP | 2.9 | ng/mL | (≤10.0) |
| CRE | 0.73 | mg/dL | (0.65–1.07) | CRP | 0.29 | mg/dL | (≤0.3) | DCP | 1950 | mAU/mL | (<40) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Enomoto, H.; Fujiwara, M.; Kono, H.; Kako, Y.; Takahagi, M.; Taniguchi, J.; Ishikawa, E.; Ikeda, N.; Takashima, T.; Yuri, Y.; et al. Metastasis of Hepatocellular Carcinoma in the Pouch of Douglas Successfully Treated by Radiation Therapy: A Case Report. Life 2023, 13, 225. https://doi.org/10.3390/life13010225
Enomoto H, Fujiwara M, Kono H, Kako Y, Takahagi M, Taniguchi J, Ishikawa E, Ikeda N, Takashima T, Yuri Y, et al. Metastasis of Hepatocellular Carcinoma in the Pouch of Douglas Successfully Treated by Radiation Therapy: A Case Report. Life. 2023; 13(1):225. https://doi.org/10.3390/life13010225
Chicago/Turabian StyleEnomoto, Hirayuki, Masayuki Fujiwara, Hiroshi Kono, Yasukazu Kako, Motonori Takahagi, Junichi Taniguchi, Eri Ishikawa, Naoto Ikeda, Tomoyuki Takashima, Yukihisa Yuri, and et al. 2023. "Metastasis of Hepatocellular Carcinoma in the Pouch of Douglas Successfully Treated by Radiation Therapy: A Case Report" Life 13, no. 1: 225. https://doi.org/10.3390/life13010225
APA StyleEnomoto, H., Fujiwara, M., Kono, H., Kako, Y., Takahagi, M., Taniguchi, J., Ishikawa, E., Ikeda, N., Takashima, T., Yuri, Y., Aizawa, N., Okamoto, M., Yoshihara, K., Yoshioka, R., Kawata, S., Ota, S., Nakano, R., Shiomi, H., Nishimura, T., ... Iijima, H. (2023). Metastasis of Hepatocellular Carcinoma in the Pouch of Douglas Successfully Treated by Radiation Therapy: A Case Report. Life, 13(1), 225. https://doi.org/10.3390/life13010225






