Ethnicity, Age, and Gender Differences in Glycated Hemoglobin (HbA1c) Levels among Adults in Northern and Eastern Sudan: A Community-Based Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Areas
2.2. Study Population and Design
2.3. Definitions
2.4. Inclusion Criteria
2.5. Exclusion Criteria
2.6. Data Collection
2.7. Anthropometric Measurements
2.8. Sample Collection and Processing
2.9. Sample Size Calculation
2.10. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Magliano, D.J.; Boyko, E.J. IDF Diabetes Atlas 2021, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Geller, A.; Shehab, N.; Lovegrove, M.; Kegler, S.; Weidenbach, K.; Ryan, G.; Budnitz, D.S. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. J. Am. Med. Assoc. 2014, 174, 678–686. [Google Scholar]
- Radin, M.S. Pitfalls in hemoglobin A1c measurement: When results may be misleading. J. Gen. Intern. Med. 2014, 29, 388–394. [Google Scholar] [CrossRef]
- Huang, S.H.; Huang, P.J.; Li, J.Y.; Su , Y.D.; Lu, C.C.; Shih, C.L. Hemoglobin A1c levels associated with age and gender in taiwanese adults without prior diagnosis with diabetes. Int. J. Environ. Res. Public Health 2021, 18, 3390. [Google Scholar] [CrossRef]
- Lee, H.S. Sex Difference in the Effect of Body Mass Index and Stress on High-Risk Diabetes Mellitus in Korean Adults. J. Korean Biol. Nurs. Sci. 2019, 21, 224–230. [Google Scholar] [CrossRef]
- Jørgensen, M.E.; Bjerregaard, P.; Borch-Johnsen, K.; Witte, D. New diagnostic criteria for diabetes: Is the change from glucose to HbA1c possible in all populations? J. Clin. Endocrinol. Metab. 2010, 95, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Ziemer, D.; Paul Kolm, P.; Weintraub, W.; Vaccarino, V.; Rhee, M.; Twombly, J.; Narayan, K.V.; Koch, D.D.; Phillips, L.S. Glucose-independent, black–white differences in hemoglobin A1c levels. Ann. Intern. Med. 2010, 152, 770–777. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q.; Liu, H.; Xiang, G.; Shan, W.; Xing, W. Association between glycated hemoglobin A1c levels with age and gender in Chinese adults with no prior diagnosis of diabetes mellitus. Biomed. Rep. 2016, 4, 737–740. [Google Scholar] [CrossRef]
- Seo, J.Y.; Hwang, S.S.; Kim, J.H.; Lee, Y.A.; Lee, S.Y.; Shin, C.H.; Yang, S.W. Distribution of glycated haemoglobin and its determinants in Korean youth and young adults: A nationwide population-based study. Sci. Rep. 2018, 8, 1962. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, D.; Liang, H.; He, J.; Luu, S.W.; Bray, C.L. Age—A significant independent factor of A1C levels. Evidence from the National Health and Nutrition Examination Survey 1999–2014. Prim. Care Diabetes 2020, 14, 420–424. [Google Scholar] [CrossRef] [PubMed]
- Hare, M.J.L.; Magliano, D.J.; Zimmet, P.Z.; Söderberg, S.; Joonas, N.; Pauvaday, V.; Larhubarbe, J.; Tuomilehto, J.; Kowlessur, S.; Alberti, K.G.M.; et al. Glucose-independent ethnic differences in HbA1c in people without known diabetes. Diabetes Care 2013, 36, 1534–1540. [Google Scholar] [CrossRef] [PubMed]
- Khosla, L.; Bhat, S.; Fullington, L.A.; Horlyck-Romanovsky, M.F. HbA1c performance in African descent populations in the United States with normal glucose tolerance, prediabetes, or diabetes: A scoping review. Prev. Chronic Dis. 2021, 18, E22. [Google Scholar] [CrossRef]
- Omer, S.; Musa, I.; ElSouli, A.; Adam, I. Prevalence, risk factors, and glycaemic control of type 2 diabetes mellitus in eastern Sudan: A community-based study. Ther. Adv. Vaccines 2019, 10, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Eltom, M.A.; Babiker Mohamed, A.H.; Elrayah-Eliadarous, H.; Yassin, K.; Noor, S.K.; Elmadhoun, W.M.; Ahmed, M.H. Increasing prevalence of type 2 diabetes mellitus and impact of ethnicity in north Sudan. Diabetes Res. Clin. Pract. 2018, 136, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Hassan, A.A.; Ahmed, B.E.; Osman, O.E.; Adam, I. Association between Helicobacter pylori seropositivity and hypertension among adults in Northern Sudan: A community-based case-control study. J. Int. Med. Res. 2023, 51, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sudan Goverment. 5th Sudan Population and Housing Census—2008. 2009. Available online: https://catalog.ihsn.org/index.php/catalog/4216/do (accessed on 20 June 2022).
- UNICEF. Situation in Gedaref. 2022. Available online: https://www.unicef.org/sudan/media/8651/file/Gedarif.pdf (accessed on 15 July 2023).
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. 1), S31–S34. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. Available online: https://apps.who.int/iris/handle/10665/42330 (accessed on 12 March 2023).
- Riley, L.; Guthold, R.; Cowan, M.; Savin, S.; Bhatti, L.; Armstrong, T.; Bonita, R. The World Health Organization STEPwise approach to noncommunicable disease risk-factor surveillance: Methods, challenges, and opportunities. Am. J. Public Health 2016, 106, 74–78. [Google Scholar] [CrossRef]
- Dean, A.G.; Sullivan, K.M.; Soe, M.M. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version. updated 2013/04/06. Available online: www.OpenEpi.com (accessed on 13 September 2023).
- Cavagnolli, G.; Pimentel, A.L.; Freitas, P.A.C.; Gross, J.L.; Camargo, J.L. Effect of ethnicity on HbA1c levels in individuals without diabetes: Systematic review and meta-analysis. PLoS ONE 2017, 12, e0171315. [Google Scholar] [CrossRef]
- Basit, A.; Fawwad, A.; Abdul Basit, K.; Waris, N.; Tahir, B.; Siddiqui, I.A. Glycated hemoglobin (HbA1c) as diagnostic criteria for diabetes: The optimal cut-off points values for the Pakistani population; a study from second National Diabetes Survey of Pakistan (NDSP) 2016–2017. BMJ Open Diabetes Res. Care 2020, 8, e001058. [Google Scholar] [CrossRef]
- Klonoff, D.C. Hemoglobinopathies and Hemoglobin A1c in Diabetes Mellitus. J. Diabetes Sci. Technol. 2020, 14, 3–7. [Google Scholar] [CrossRef]
- Sadiya, A.; Jakapure, V.; Kumar, V. Ethnic variability in glucose and insulin response to rice among healthy overweight adults: A randomized cross-over study. Diabetes Metab. Syndr. Obes. 2023, 16, 993–1002. [Google Scholar] [CrossRef]
- Nowlin, S.; Cleland, C.M.; Parekh, N.; Hagan, H.; Melkus, G. Racial and ethnic disparities in predictors of glycemia: A moderated mediation analysis of inflammation-related predictors of diabetes in the NHANES 2007–2010. Nutr. Diabetes 2018, 8, 56. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, T.M.; Adam, I.; Abdelhadi, M.A.; Siddig, M.F.; Ali, A.A. Anaemia among adults in Kassala, Eastern Sudan. BMC Res. Notes 2012, 10, 202. [Google Scholar] [CrossRef] [PubMed]
- Bano, R.; Durrani, A. Age and Gender Specific Prevalence among Non-Insulin Dependent Diabetes Mellitus (Type II) and its Correlation with HbA1c % level, A Hospital-Based Cross-Sectional Study. Int. J. Health Sci. Res. 2022, 8, 102–108. [Google Scholar]
- Hovestadt, I.; Kiess, W.; Lewien, C.; Willenberg, A.; Poulain, T.; Meigen, C.; Körner, A.; Vogel, M. HbA1c percentiles and the association between BMI, age, gender, puberty, and HbA1c levels in healthy German children and adolescents. Pediatr. Diabetes 2022, 23, 194–202. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, X.P.; Yuan, J.; Cai, B.; Wang, X.L.; Wu, X.L.; Zhang, Y.H.; Zhang, X.Y.; Yin, T.; Zhu, X.H.; et al. Association of body mass index and age with incident diabetes in Chinese adults: A population-based cohort study. BMJ Open 2018, 8, e021768. [Google Scholar] [CrossRef]
- Song, X.; Qiu, M.; Zhang, X.; Wang, H.; Tong, W.; Ju, L.; Gu, L.; Sun, S.; Zhang, H.; Wang, W.; et al. Gender-related affecting factors of prediabetes on its 10-year outcome. BMJ Open Diabetes Res. Care 2016, 4, 1–6. [Google Scholar] [CrossRef]
- Mustafa, I.O.; Tanko, Y.; Yusuf, R.; Musa, S.A. Case reports gender disparity in the management of diabetes among residents of Sabon Gari local government area of Kaduna State, Nigeria. J. Diagn. Case Rep. 2023, 4, 1–3. [Google Scholar] [CrossRef]
- Harreiter, J.; Kautzky-Willer, A. Sex and gender differences in prevention of type 2 diabetes. Front. Endocrinol. 2018, 9, 220. [Google Scholar] [CrossRef]
- Duarte, F.G.; Da Silva Moreira, S.; Almeida, M.D.C.C.; De Souza Teles, C.A.; Andrade, C.S.; Reingold, A.L.; Moreira, E.D., Jr. Sex differences and correlates of poor glycaemic control in type 2 diabetes: A cross-sectional study in Brazil and Venezuela. BMJ Open 2019, 9, e023401. [Google Scholar] [CrossRef]
- Kautzky-Willer, A.; Harreiter, J.; Pacini, G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr. Rev. 2016, 37, 278–316. [Google Scholar] [CrossRef]
| Variable | Total (898) | Northern Sudan (363) | Eastern Sudan (535) | p Value | |
|---|---|---|---|---|---|
| Mean (Standard Deviation) | |||||
| Age, years | 44.0 (16.0) | 44.7 (15.7) | 43.54 (16.2) | 0.292 | |
| Body mass index, kg/m2 | 27.00 (6.63) | 26.61 (6.30) | 27.27 (6.83) | 0.140 | |
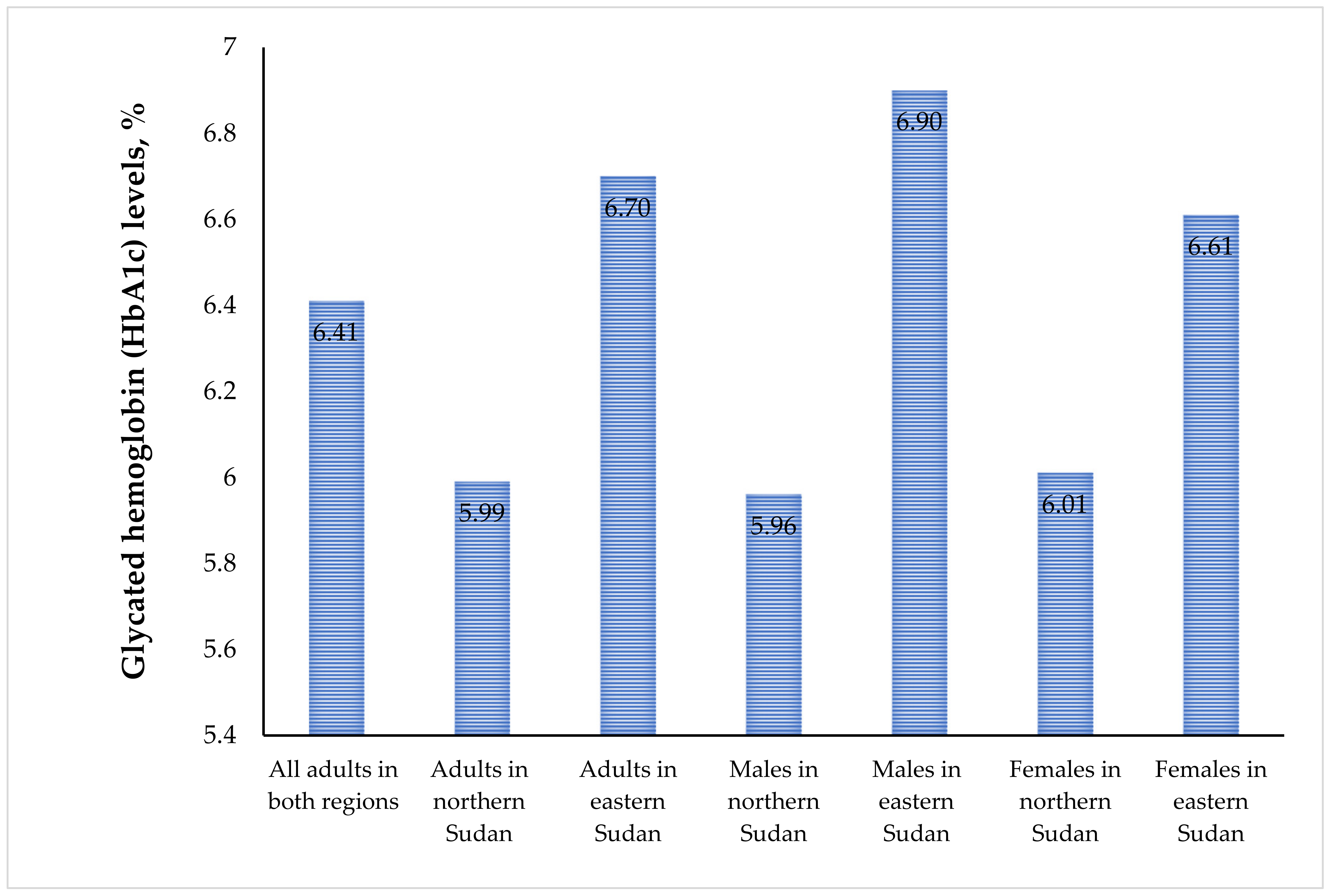
| Glycated hemoglobin (HbA1c) for both sexes | 6.41 (1.51) | 5.99 (1.01) | 6.70 (1.71) | <0.001 | |
| HbA1c for all females | 6.42 (1.51) | 6.01 (0.99) | 6.61 (1.66) | <0.001 | |
| HbA1c for all males | 6.39 (1.51) | 5.96 (1.02) | 6.90 (1.80) | <0.001 | |
| Frequency (Proportion) | |||||
| Gender | Male | 349 (38.9) | 189 (52.1) | 160 (29.9) | <0.001 |
| Female | 549 (61.1) | 174 (47.9) | 375 (70.1) | ||
| Education level | ≥ secondary | 559 (62.2) | 243 (66.9) | 316 (59.1) | 0.017 |
| < secondary | 339 (37.8) | 120 (33.1) | 219 (40.9) | ||
| Obesity | No | 625 (69.6) | 259 (71.3) | 366 (68.4) | 0.347 |
| Yes | 273 (30.4) | 104 (28.7) | 169 (31.6) | ||
| HbA1c | <6.5% | 615 (68.5) | 295 (81.3) | 320 (59.8) | <0.001 |
| ≥6.5% | 283 (31.5) | 68 (18.7) | 215 (40.2) | ||
| Variable | All Studied Participants (n = 898) HbA1c | HbA1c <6.5% Participants | HbA1c ≥6.5% Participants | ||||
|---|---|---|---|---|---|---|---|
| Coefficient (Standard Error) | p Value | Coefficient (Standard Error) | p Value | Coefficient (Standard Error) | p Value | ||
| Age, years | 0.006 (0.001) | <0.001 | 0.001 (0.001) | 0.246 | 0.012 (0.007) | 0.102 | |
| Body mass index, kg/m2 | 0.007 (0.002) | 0.002 | 0.007 (0.003) | 0.037 | −0.014 (0.015) | 0.354 | |
| Gender | Male | Reference | |||||
| Female | −0.05 (0.03) | 0.162 | −0.03 (0.05) | 0.583 | 0.03 (0.22) | 0.883 | |
| Education level | ≥secondary | Reference | |||||
| <secondary | −0.03 (0.03) | 0.652 | 0.01 (0.05) | 0.946 | 0.12 (0.22) | 0.608 | |
| Location | Northern Sudan | Reference | |||||
| Eastern Sudan | 0.22 (0.03) | <0.001 | 0.9 (0.04) | 0.034 | 0.79 (0.25) | 0.001 | |
| Variable | Northern Sudan | Eastern Sudan | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HbA1c | Hba1c <6.5% | HbA1c ≥6.5% | HbA1c | HbA1c <6.5% | HbA1c ≥6.5% | ||||||||
| Coefficient (Standard Error) | p Value | Coefficient (Standard Error) | p Value | Coefficient (Standard Error) | p Value | Coefficient (Standard Error) | p Value | Coefficient (Standard Error) | p Value | Coefficient (Standard Error) | p Value | ||
| Age, years | 0.014 (0.003) | <0.001 | 0.004 (0.002) | 0.016 | −0.014 (0.012) | 0.249 | 0.023 (0.005) | <0.001 | −0.001 (0.002) | 0.524 | 0.021 (0.009) | 0.025 | |
| Body mass index, kg/m2 | −0.004 (0.009) | 0.669 | 0.001 (0.04) | 0.873 | −0.039 (0.028) | 0.177 | 0.03 (0.01) | 0.010 | 0.011 (0.004) | 0.012 | −0.011 (0.018) | 0.530 | |
| Gender | Male | Reference | |||||||||||
| Female | 0.16 (0.12) | 0.199 | 0.08 (0.06) | 0.204 | 0.31 (0.38) | 0.421 | −0.26 (0.16) | 0.104 | −0.12 (0.07) | 0.073 | −0.02 (0.26) | 0.932 | |
| Education level | ≥secondary | Reference | |||||||||||
| <secondary | 0.15 (0.11) | 0.184 | 0.01 (0.06) | 0.850 | 0.22 (0.37) | 0.553 | −0.14 (0.16) | 0.378 | 0.05 (0.06) | 0.397 | −0.03 (0.29) | 0.919 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, S.F.; Hassan, A.A.; Eltayeb, M.M.; Omar, S.M.; Adam, I. Ethnicity, Age, and Gender Differences in Glycated Hemoglobin (HbA1c) Levels among Adults in Northern and Eastern Sudan: A Community-Based Cross-Sectional Study. Life 2023, 13, 2017. https://doi.org/10.3390/life13102017
Ahmed SF, Hassan AA, Eltayeb MM, Omar SM, Adam I. Ethnicity, Age, and Gender Differences in Glycated Hemoglobin (HbA1c) Levels among Adults in Northern and Eastern Sudan: A Community-Based Cross-Sectional Study. Life. 2023; 13(10):2017. https://doi.org/10.3390/life13102017
Chicago/Turabian StyleAhmed, Sumia F., Ahmed A. Hassan, Majdolin M. Eltayeb, Saeed M. Omar, and Ishag Adam. 2023. "Ethnicity, Age, and Gender Differences in Glycated Hemoglobin (HbA1c) Levels among Adults in Northern and Eastern Sudan: A Community-Based Cross-Sectional Study" Life 13, no. 10: 2017. https://doi.org/10.3390/life13102017
APA StyleAhmed, S. F., Hassan, A. A., Eltayeb, M. M., Omar, S. M., & Adam, I. (2023). Ethnicity, Age, and Gender Differences in Glycated Hemoglobin (HbA1c) Levels among Adults in Northern and Eastern Sudan: A Community-Based Cross-Sectional Study. Life, 13(10), 2017. https://doi.org/10.3390/life13102017






