Restoration of Hip Geometry after Femoral Neck Fracture: A Comparison of the Femoral Neck System (FNS) and the Dynamic Hip Screw (DHS)
Abstract
:1. Introduction
2. Methods
3. Results
3.1. Demographics
3.2. Follow-Up
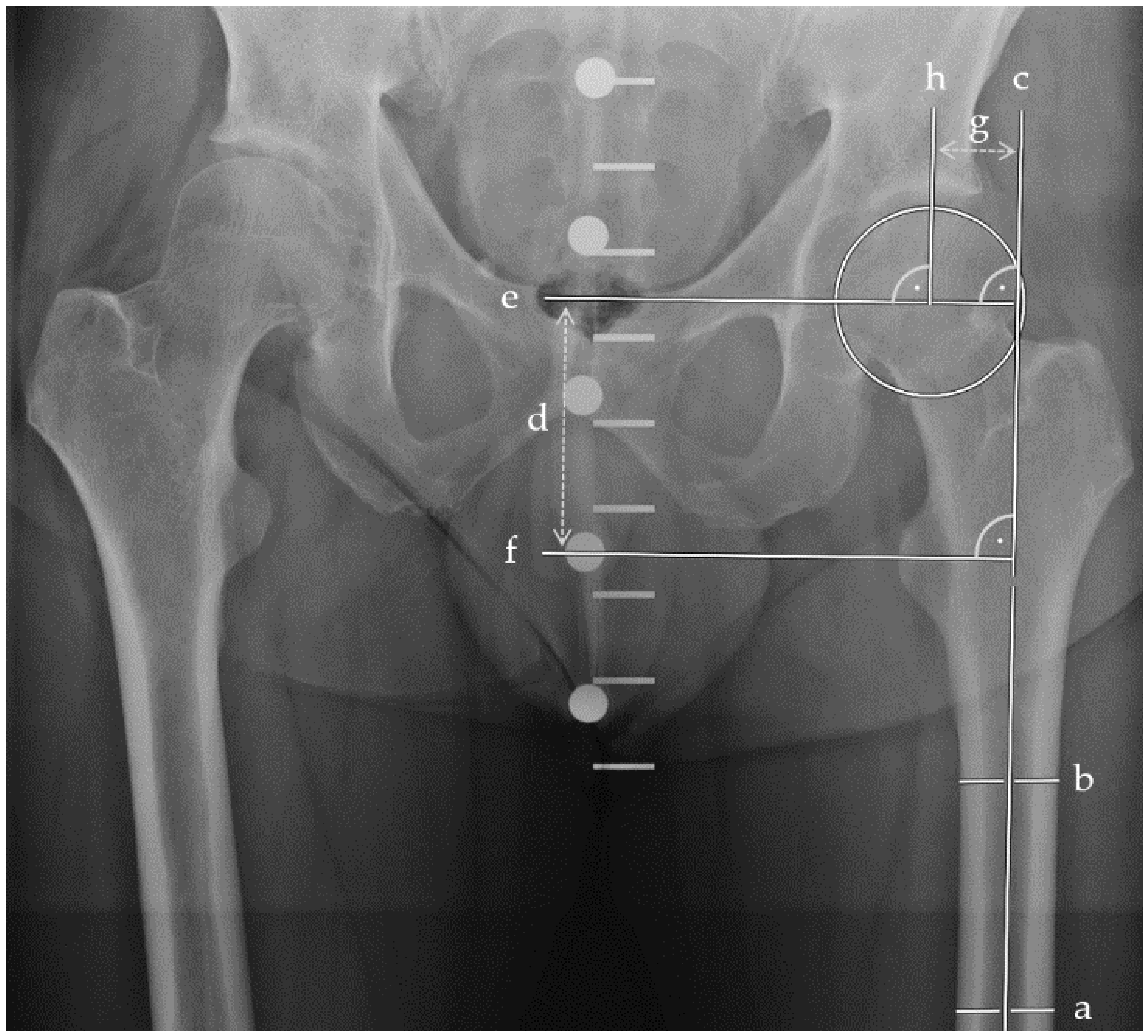
3.3. Radiographic Outcomes
3.4. Scar Lengths and PROM Assessment
3.5. Revision and Mortality Rate
3.6. Management of Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- DePuy Synthes. Femoral Neck System (FNS). 2019. Available online: https://www.jnjmedicaldevices.com/sites/default/files/user_uploaded_assets/pdf_assets/2019-09/FNS Value Brief.pdf (accessed on 4 January 2022).
- DePuy Synthes. Femoral Neck System Operationstechnik. 2018. Available online: http://synthes.vo.llnwd.net/o16/LLNWMB8/INT Mobile/Synthes International/Product Support Material/legacy_Synthes_PDF/DSEM-TRM-0614-0098-3a_LR.pdf (accessed on 4 January 2022).
- Märdian, S.; Tsitsilonis, S.; Ahmad, S.; Culemann, U.; Duda, G.; Heyland, M.; Stöckle, U. What constitutes a good osteosynthesis? Chirurg 2021, 92, 863–872. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.; Song, J.-U.; Yoo, J.-I.; Park, K.H.; Kim, J.-T.; Park, C.H.; Choy, W.-S. Improved control over implant anchorage under the use of the femoral neck system for fixation of femoral neck fractures: A technical note. BMC Musculoskelet. Disord. 2021, 22, 621. [Google Scholar] [CrossRef] [PubMed]
- Stoffel, K.; Zderic, I.; Gras, F.; Sommer, C.; Eberli, U.; Mueller, D.; Oswald, M.; Gueorguiev, B. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: A comparison with the dynamic hip screw and cannulated screws. J. Orthop. Trauma 2017, 31, 131–137. [Google Scholar] [CrossRef]
- He, C.; Lu, Y.; Wang, Q.; Ren, C.; Li, M.; Yang, M.; Xu, Y.; Li, Z.; Zhang, K.; Ma, T. Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet. Disord. 2021, 22, 994. [Google Scholar] [CrossRef]
- Hu, H.; Cheng, J.; Feng, M.; Gao, Z.; Wu, J.; Lu, S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J. Orthop. Surg. Res. 2021, 16, 370. [Google Scholar] [CrossRef]
- Tang, Y.; Zhang, Z.; Wang, L.; Xiong, W.; Fang, Q.; Wang, G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: A preliminary comparative study. J. Orthop. Surg. Res. 2021, 16, 504. [Google Scholar] [CrossRef]
- Vazquez, O.; Gamulin, A.; Hannouche, D.; Belaieff, W. Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): Short-term clinical and radiological outcomes. J. Orthop. Surg. Res. 2021, 16, 477. [Google Scholar] [CrossRef]
- Zhou, X.-Q.; Li, Z.-Q.; Xu, R.-J.; She, Y.-S.; Zhang, X.-X.; Chen, G.-X.; Yu, X. Comparison of early clinical results for femoral neck system and cannulated screws in the treatment of unstable femoral neck fractures. Orthop. Surg. 2021, 13, 1802–1809. [Google Scholar] [CrossRef]
- Mehraj, M.; Khurana, S.; Joshi, U.R.; Jain, A.; Kumar, B.; Prakash, B.B.; Shah, I. Early results of internal fixation with femoral neck system in young patients with femoral neck fracture. Ortop. Traumatol. Rehabil. 2022, 24, 305–309. [Google Scholar] [CrossRef]
- Schopper, C.; Zderic, I.; Menze, J.; Müller, D.; Rocci, M.; Knobe, M.; Shoda, E.; Richards, G.; Gueorguiev, B.; Stoffel, K. Higher stability and more predictive fixation with the Femoral Neck System versus Hansson Pins in femoral neck fractures Pauwels II. J. Orthop. Transl. 2020, 24, 88–95. [Google Scholar] [CrossRef]
- Nanty, L.; Canovas, F.; Rodriguez, T.; Faure, P.; Dagneaux, L. Femoral neck shortening after internal fixation of Garden I fractures increases the risk of femoral head collapse. Orthop. Traumatol. Surg. Res. 2019, 105, 999–1004. [Google Scholar] [CrossRef] [PubMed]
- Linde, F.; Andersen, E.; Hvass, I.; Madsen, F.; Pallesen, R. Avascular femoral head necrosis following fracture fixation. Injury 1986, 17, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Moya-Angeler, J.; Gianakos, A.L.; Villa, J.C.; Ni, A.; Lane, J.M. Current concepts on osteonecrosis of the femoral head. World J. Orthop. 2015, 6, 590–601. [Google Scholar] [CrossRef]
- Konarski, W.; Poboży, T.; Śliwczyński, A.; Kotela, I.; Krakowiak, J.; Hordowicz, M.; Kotela, A. Avascular necrosis of femoral head-overview and current state of the art. Int. J. Environ. Res. Public Health 2022, 19, 7348. [Google Scholar] [CrossRef] [PubMed]
- Cintean, R.; Pankratz, C.; Hofmann, M.; Gebhard, F.; Schütze, K. Early results in non-displaced femoral neck fractures using the Femoral Neck System. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 21514593211050153. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-Z.; Lin, Y.; Li, C.; Yue, X.-J.; Li, G.-Y.; Wang, B.; Zhu, Z.-Q. A comparative analysis of Femoral Neck System and three cannulated screws fixation in the treatment of femoral neck fractures: A six-month follow-up. Orthop. Surg. 2022, 14, 686–693. [Google Scholar] [CrossRef]
- Lin, H.; Lai, C.; Zhou, Z.; Wang, C.; Yu, X. Femoral Neck System vs. four cannulated screws in the treatment of Pauwels III femoral neck fracture. J. Orthop. Sci. 2022, in press. [CrossRef] [PubMed]
- Niemann, M.; Braun, K.F.; Ahmad, S.S.; Stöckle, U.; Märdian, S.; Graef, F. Comparing perioperative outcome measures of the Dynamic Hip Screw and the Femoral Neck System. Medicina 2022, 58, 352. [Google Scholar] [CrossRef]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Pauwels, F. Der Schenkelhalsbruch. In Gesammelte Abhandlungen zur Funktionellen Anat des Bewegungsapparates; Springer: Berlin/Heidelberg, Germany, 1965; pp. 1–138. Available online: https://link.springer.com/chapter/10.1007/978-3-642-86841-2_1 (accessed on 2 February 2022).
- Garden, R.S. Low-angle fixation in fractures of the femoral neck. Bone Jt. J. 1961, 43-B, 647–663. [Google Scholar] [CrossRef]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Jt. Surg. 1969, 51, 737–755. [Google Scholar] [CrossRef]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Motulsky, H.J.; Brown, R.E. Detecting outliers when fitting data with nonlinear regression—A new method based on robust nonlinear regression and the false discovery rate. BMC Bioinform. 2006, 7, 123. [Google Scholar] [CrossRef] [PubMed]
- Riley, J.C. Rising Life Expectancy: A Global History; Cambridge University Press: Cambridge, UK, 2015; pp. 1–243. Available online: https://www.cambridge.org/core/books/rising-life-expectancy/5CACDE4BC65980FBFC28337C8F4E2C84 (accessed on 5 January 2023).
- Gullberg, B.; Johnell, O.; Kanis, J.A. World-wide projections for hip fracture. Osteoporos. Int. 1997, 7, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Dyer, S.M.; Crotty, M.; Fairhall, N.; Magaziner, J.; Beaupre, L.A.; Cameron, I.D.; Sherrington, C. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016, 16, 158. [Google Scholar] [CrossRef] [PubMed]
- Slobogean, G.P.; Sprague, S.; Bzovsky, S.; Scott, T.; Thabane, L.; Heels-Ansdell, D.; O’Toole, R.V.; Howe, A.; Gaski, G.E.; Hill, L.C.; et al. Fixation using Alternative Implants for the Treatment of Hip fractures (FAITH-2): The exploratory health-related quality of life and patient-reported functional outcomes of a multi-centre 2 × 2 factorial randomized controlled pilot trial in young femoral neck fracture patients. Injury 2021, 52, 3051–3059. [Google Scholar]
- Fischer, H.; Maleitzke, T.; Eder, C.; Ahmad, S.; Stöckle, U.; Braun, K.F. Management of proximal femur fractures in the elderly: Current concepts and treatment options. Eur. J. Med. Res. 2021, 26, 86. [Google Scholar] [CrossRef]
- Bhandari, M.; Swiontkowski, M. Management of acute hip fracture. N. Engl. J. Med. 2017, 377, 2053–2062. [Google Scholar] [CrossRef] [PubMed]
- Klestil, T.; Röder, C.; Stotter, C.; Winkler, B.; Nehrer, S.; Lutz, M.; Klerings, I.; Wagner, G.; Gartlehner, G.; Nussbaumer-Streit, B. Impact of timing of surgery in elderly hip fracture patients: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 13933. [Google Scholar] [CrossRef]
- Zelle, B.A.; Salazar, L.M.; Howard, S.L.; Parikh, K.; Pape, H.C. Surgical treatment options for femoral neck fractures in the elderly. Int. Orthop. 2022, 46, 1111–1122. [Google Scholar] [CrossRef]
- Tian, P.; Kuang, L.; Li, Z.J.; Xu, G.J.; Fu, X. Comparison between femoral neck systems and cannulated cancellous screws in treating femoral neck fractures: A meta-analysis. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221113533. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.F.; Luo, Z.H.; Hu, L.C.; Luo, Y.W. Efficacy of the femoral neck system in femoral neck fracture treatment in adults: A systematic review and meta-analysis. World J. Clin. Cases 2022, 10, 11454–11465. [Google Scholar] [CrossRef] [PubMed]
- Gupta, G.K.; Rai, A.; Mandal, S.; Rani, S.; Shekhar, S.; Halder, S.; Prasad, P.; Kumar, A.; Haque, Z.U. Comparison of Femoral Neck System versus cannulated cancellous screws for the fixation of femoral neck fracture in young adults: A systematic review and meta-analysis. Cureus 2022, 14, e32011. [Google Scholar] [CrossRef]
- Lu, Y.; Huang, Z.; Xu, Y.; Huang, Q.; Ren, C.; Li, M.; Li, Z.; Sun, L.; Xue, H.; Zhang, K.; et al. Femoral neck system versus cannulated screws for fixation of femoral neck fracture in young adults: A systematic review and meta-analysis. Am. J. Transl. Res. 2022, 14, 5480–5490. Available online: https://pubmed.ncbi.nlm.nih.gov/36105033/ (accessed on 2 January 2023). [PubMed]
- Patel, S.; Kumar, V.; Baburaj, V.; Dhillon, M.S. The use of the femoral neck system (FNS) leads to better outcomes in the surgical management of femoral neck fractures in adults compared to fixation with cannulated screws: A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2022, 33, 2101–2109. [Google Scholar] [CrossRef]
- Stassen, R.C.; Jeuken, R.M.; Boonen, B.; Meesters, B.; de Loos, E.R.; van Vugt, R. First clinical results of 1-year follow-up of the femoral neck system for internal fixation of femoral neck fractures. Arch. Orthop. Trauma Surg. 2021, 142, 3755–3763. [Google Scholar] [CrossRef] [PubMed]
- Davidson, A.; Blum, S.; Harats, E.; Kachko, E.; Essa, A.; Efraty, R.; Peyser, A.; Giannoudis, P.V. Neck of femur fractures treated with the femoral neck system: Outcomes of one hundred and two patients and literature review. Int. Orthop. 2022, 46, 2105–2115. [Google Scholar] [CrossRef]
- Stoffel, K.; Michelitsch, C.; Arora, R.; Babst, R.; Candrian, C.; Eickhoff, A.; Gebhard, F.; Platz, A.; Schmid, F.A.; Weschenfelder, W.; et al. Clinical performance of the Femoral Neck System within 1 year in 125 patients with acute femoral neck fractures, a prospective observational case series. Arch. Orthop. Trauma Surg. 2022, 143, 4155–4164. [Google Scholar] [CrossRef]
- Xu, X.; Fan, J.; Zhou, F.; Lv, Y.; Tian, Y.; Ji, H.; Zhang, Z.; Guo, Y.; Yang, Z.; Hou, G. Comparison of femoral neck system to multiple cancellous screws and dynamic hip screws in the treatment of femoral neck fractures. Injury 2022, 54 (Suppl. S2), S28–S35. [Google Scholar] [CrossRef]
- Schuetze, K.; Burkhardt, J.; Pankratz, C.; Eickhoff, A.; Boehringer, A.; Degenhart, C.; Gebhard, F.; Cintean, R. Is new always better: Comparison of the femoral neck system and the dynamic hip screw in the treatment of femoral neck fractures. Arch. Orthop. Trauma Surg. 2022, 143, 3155–3161. [Google Scholar] [CrossRef]
- Moon, J.-K.; Lee, J.-I.; Hwang, K.-T.; Yang, J.-H.; Park, Y.-S.; Park, K.-C. Biomechanical comparison of the femoral neck system and the dynamic hip screw in basicervical femoral neck fractures. Sci. Rep. 2022, 12, 7915. [Google Scholar] [CrossRef] [PubMed]





| DHS (N = 14) | FNS (N = 11) | Statistics | ||
|---|---|---|---|---|
| Harris Hip Score | 95.90 (IQR 72.20, 99.85) | 94.70 (IQR 90.55, 99.85) | p = 0.53 | |
| SF-36 | Physical functioning [%] | 57.50 (IQR 21.25, 95.00) | 75.00 (IQR 50.00, 90.00) | p = 0.41 |
| Role limitations due to physical health [%] | 50.00 (IQR 0.00, 100.00) | 100.00 (IQR 25.00, 100.00) | p = 0.19 | |
| Role limitations due to emotional problems [%] | 83.35 (IQR 0.00, 100.00) | 100.00 (IQR 100.00, 100.00) | p = 0.02 | |
| Energy/fatigue [%] | 47.50 (IQR 38.75, 71.25) | 55.00 (IQR 50.00, 80.00) | p = 0.04 | |
| Emotional well-being [%] | 58.00 (IQR 38.00, 89.00) | 76.00 (IQR 60.00, 96.00) | p = 0.12 | |
| Social functioning [%] | 81.25 (IQR 31.25, 100.00) | 87.50 (IQR 75.00, 100.00) | p = 0.42 | |
| Pain [%] | 62.50 (IQR 39.38, 92.50) | 67.50 (IQR 55.00, 90.00) | p = 0.39 | |
| General health [%] | 62.50 (IQR 42.50, 78.75) | 75.00 (IQR 50.00, 90.00) | p = 0.25 | |
| Health change [%] | 50.00 (IQR 43.75, 81.25) | 50.00 (IQR 25.00, 100.00) | p = 0.70 | |
| NRS | 2 (IQR 1, 5) | 2 (IQR 1, 3) | p = 0.67 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niemann, M.; Maleitzke, T.; Jahn, M.; Salmoukas, K.; Braun, K.F.; Graef, F.; Stöckle, U.; Meller, S. Restoration of Hip Geometry after Femoral Neck Fracture: A Comparison of the Femoral Neck System (FNS) and the Dynamic Hip Screw (DHS). Life 2023, 13, 2073. https://doi.org/10.3390/life13102073
Niemann M, Maleitzke T, Jahn M, Salmoukas K, Braun KF, Graef F, Stöckle U, Meller S. Restoration of Hip Geometry after Femoral Neck Fracture: A Comparison of the Femoral Neck System (FNS) and the Dynamic Hip Screw (DHS). Life. 2023; 13(10):2073. https://doi.org/10.3390/life13102073
Chicago/Turabian StyleNiemann, Marcel, Tazio Maleitzke, Markus Jahn, Katharina Salmoukas, Karl F. Braun, Frank Graef, Ulrich Stöckle, and Sebastian Meller. 2023. "Restoration of Hip Geometry after Femoral Neck Fracture: A Comparison of the Femoral Neck System (FNS) and the Dynamic Hip Screw (DHS)" Life 13, no. 10: 2073. https://doi.org/10.3390/life13102073
APA StyleNiemann, M., Maleitzke, T., Jahn, M., Salmoukas, K., Braun, K. F., Graef, F., Stöckle, U., & Meller, S. (2023). Restoration of Hip Geometry after Femoral Neck Fracture: A Comparison of the Femoral Neck System (FNS) and the Dynamic Hip Screw (DHS). Life, 13(10), 2073. https://doi.org/10.3390/life13102073





