Effectiveness of Deep Cervical Fascial Manipulation® and Sequential Yoga Poses on Pain and Function in Individuals with Mechanical Neck Pain: A Randomised Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
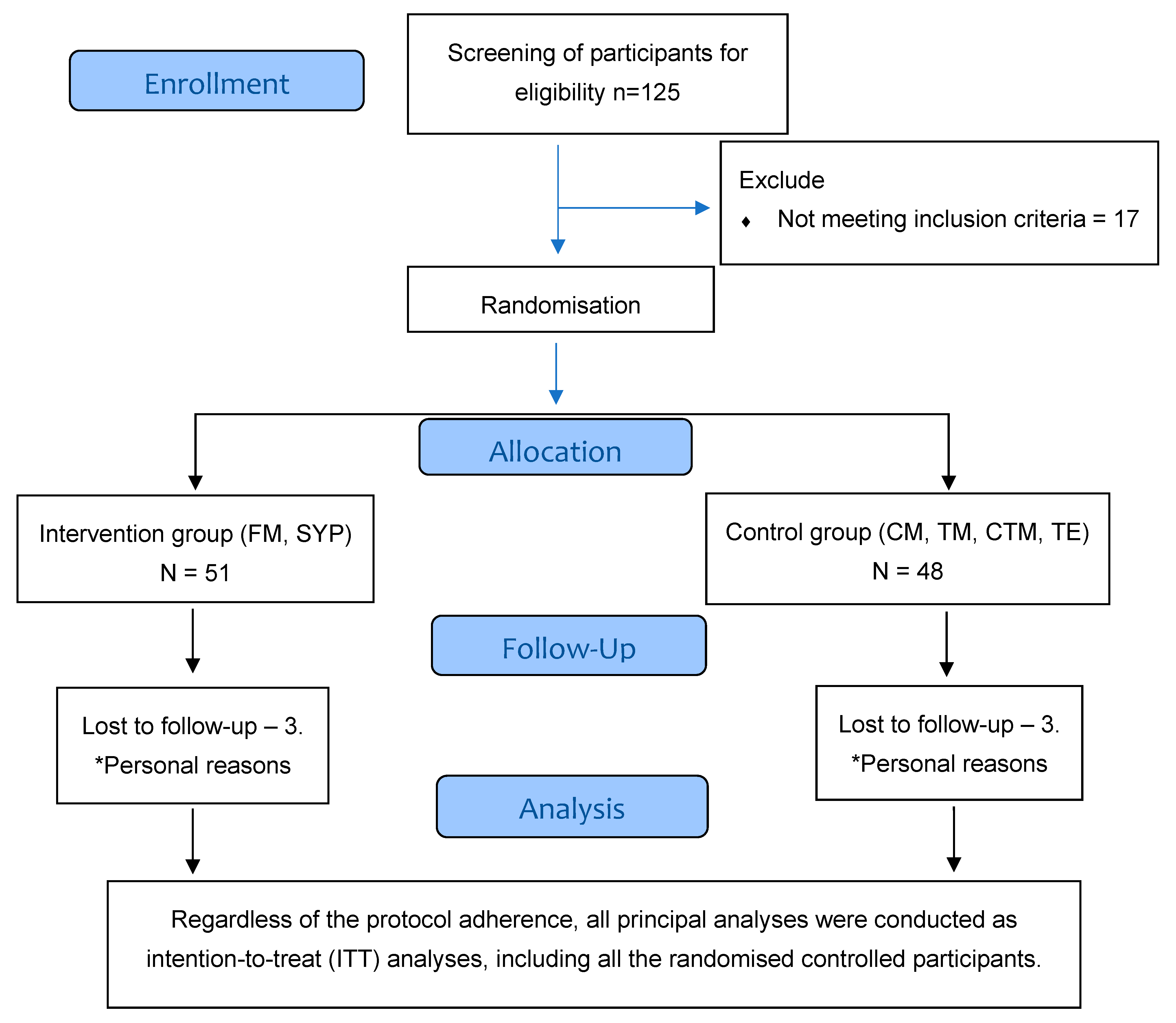
2.2. Study Design
2.3. Participant’s Recruitment
2.4. Interventions
2.4.1. Control Group (CM, CTM, TM, and TE)
2.4.2. Intervention Group (FM and SYP)
Fascial Manipulation®
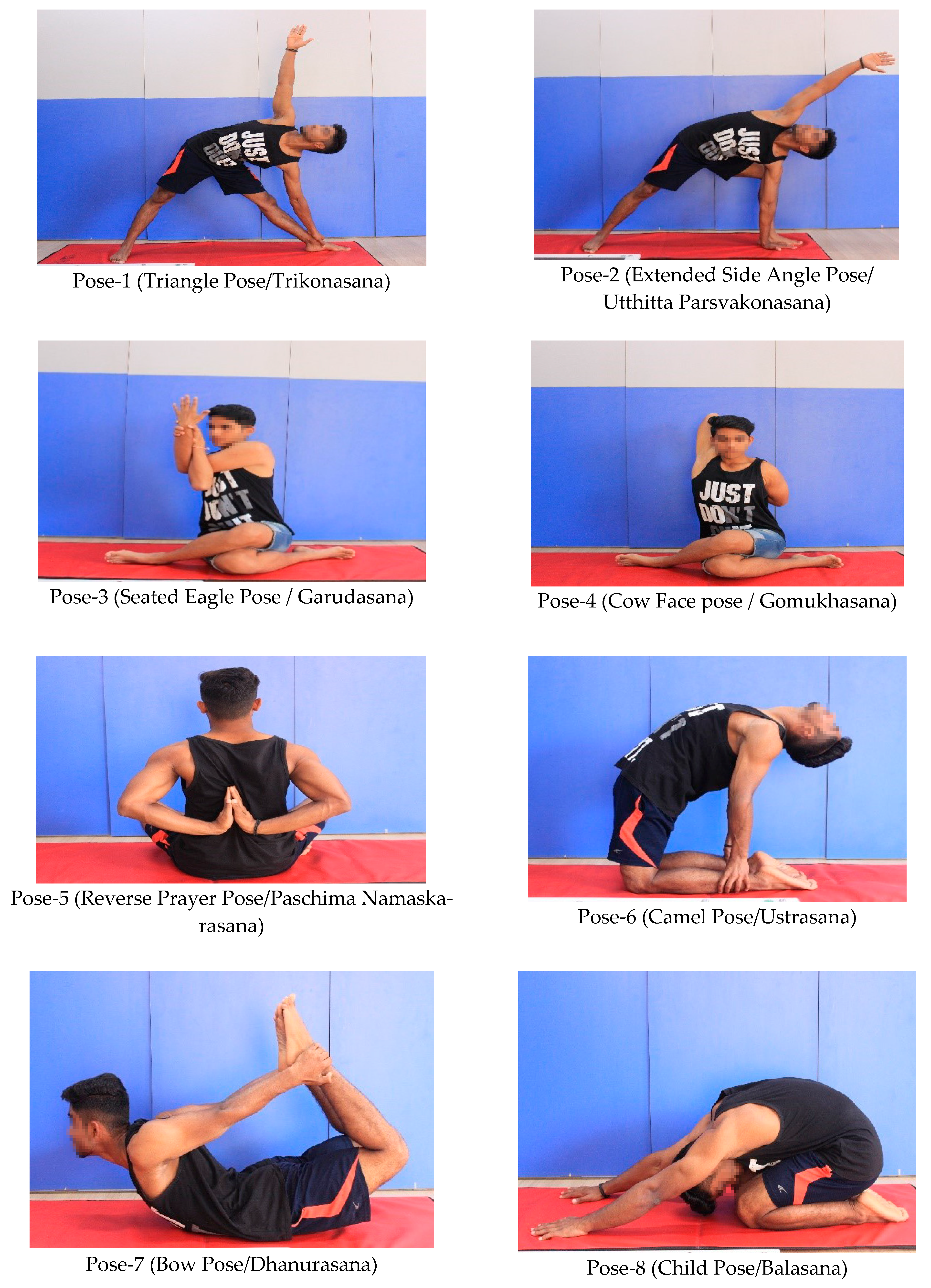
Sequential Yoga Poses
2.4.3. Intervention Adherence
2.5. Outcomes
- Numeric pain rating scale (NPRS).
- Patient-specific functional scale (PSFS)
- Fear-avoidance belief questionnaire—physical activity (FABQ-PA)
- Elbow extension range of motion during upper limb neurodynamics test 1 (ULNT1).
- Numeric Pain Rating Scale
- Patient-Specific Functional Scale
- Fear-Avoidance Beliefs Questionnaire-Physical Activity (FABQ-PA)
- Elbow Extension ROM during the Upper Limb Neurodynamic Test
2.6. Recruitment, Allocation, and Implementation
2.7. Statistical Methods
3. Results
3.1. Patient Characteristics
3.2. Mean Values of the Outcomes during Subsequent Measurements
3.2.1. NPRS
3.2.2. EEROM
3.2.3. FABQ-PA
3.2.4. PSFS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Muñoz-García, D.; Gil-Martínez, A.; López-López, A.; Lopez-de-Uralde-Villanueva, I.; La Touche, R.; Fernández-Carnero, J. Chronic Neck Pain and Cervico-Craniofacial Pain Patients Express Similar Levels of Neck Pain-Related Disability, Pain Catastrophizing, and Cervical Range of Motion. Pain. Res. Treat. 2016, 2016, 7296032. [Google Scholar] [CrossRef] [PubMed]
- Guzman, J.; Hurwitz, E.L.; Carroll, L.J.; Haldeman, S.; Côté, P.; Carragee, E.J.; Peloso, P.M.; van der Velde, G.; Holm, L.W.; Hogg-Johnson, S.; et al. A New Conceptual Model of Neck Pain: Linking Onset, Course, and Care: The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008, 33, S14–S23. [Google Scholar] [CrossRef] [PubMed]
- Dennison, B.; Leal, M. Neck and Arm Pain Syndromes. Evidence-Informed Screening, Diagnosis, and Management, 1st ed.; Elsevier Churchill Livingstone: Philadelphia, PA, USA, 2011. [Google Scholar]
- Yeun, Y.-R.; Han, S.-J. Factors Associated with Neck/Shoulder Pain in Young Adults. Biomed. Res. 2017, 28, 717–721. [Google Scholar]
- Binder, A.I. Neck Pain. BMJ Clin. Evid. 2008, 2008, 1103. [Google Scholar] [PubMed]
- Ayoub, L.J.; Seminowicz, D.A.; Moayedi, M. A Meta-Analytic Study of Experimental and Chronic Orofacial Pain Excluding Headache Disorders. Neuroimage Clin. 2018, 20, 901–912. [Google Scholar] [CrossRef]
- Gross, A.; Langevin, P.; Burnie, S.J.; Bédard-Brochu, M.-S.; Empey, B.; Dugas, E.; Faber-Dobrescu, M.; Andres, C.; Graham, N.; Goldsmith, C.H.; et al. Manipulation and Mobilisation for Neck Pain Contrasted against an Inactive Control or Another Active Treatment. Cochrane Database Syst. Rev. 2015, 9, CD004249. [Google Scholar] [CrossRef]
- Cleland, J.A.; Childs, J.D.; Fritz, J.M.; Whitman, J.M.; Eberhart, S.L. Development of a Clinical Prediction Rule for Guiding Treatment of a Subgroup of Patients with Neck Pain: Use of Thoracic Spine Manipulation, Exercise, and Patient Education. Phys. Ther. 2007, 87, 9–23. [Google Scholar] [CrossRef]
- Gross, A.; Kay, T.M.; Paquin, J.-P.; Blanchette, S.; Lalonde, P.; Christie, T.; Dupont, G.; Graham, N.; Burnie, S.J.; Gelley, G.; et al. Exercises for Mechanical Neck Disorders. Cochrane Database Syst. Rev. 2015, 1, CD004250. [Google Scholar] [CrossRef]
- Raja, G.P.; Bhat, N.S.; Fernández-de-Las-Peñas, C.; Gangavelli, R.; Davis, F.; Shankar, R.; Prabhu, A. Effectiveness of Deep Cervical Fascial Manipulation and Yoga Postures on Pain, Function, and Oculomotor Control in Patients with Mechanical Neck Pain: Study Protocol of a Pragmatic, Parallel-Group, Randomized, Controlled Trial. Trials 2021, 22, 574. [Google Scholar] [CrossRef]
- Butler, D. Mobilisation of the Nervous System, 1st ed.; Churchill Livingstone: Melbourne, Australia, 1991. [Google Scholar]
- Purslow, P.P. Muscle Fascia and Force Transmission. J. Bodyw. Mov. Ther. 2010, 14, 411–417. [Google Scholar] [CrossRef]
- Schleip, R.; Findley, T.; Chaitow, L.; Huijing, P. (Eds.) The Tensional Network of the Human Body; Elsevier: Amsterdam, The Netherlands; Churchill Livingstone: Melbourne, Australia, 2012. [Google Scholar]
- Raja, G.P.; Fernandes, S.; Cruz, A.M.; Prabhu, A. The Plausible Role of Deep Cervical Fascia and Its Continuum in Chronic Craniofacial and Cervicobrachial Pain: A Case Report. Heliyon 2020, 6, e04560. [Google Scholar] [CrossRef]
- Bordoni, B.; Zanier, E. Clinical and Symptomatological Reflections: The Fascial System. J. Multidiscip. Healthc. 2014, 7, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Mathew, N.P.; Raja, G.P.; Davis, F. Effect of Fascial Manipulation on Glenohumeral Internal Rotation Deficit in Overhead Athletes a Randomized Controlled Trial. Muscles Ligaments Tendons J. (MLTJ) 2020, 10, 17–23. [Google Scholar] [CrossRef]
- Stecco, A.; Cowman, M.; Pirri, N.; Raghavan, P.; Pirri, C. Densification: Hyaluronan Aggregation in Different Human Organs. Bioengineering 2022, 9, 159. [Google Scholar] [CrossRef]
- Stecco, L. Fascial Manipulation for Musculoskeletal Pain, 1st ed.; Piccin: Padua, Italy, 2004. [Google Scholar]
- Kamani, N.C.; Poojari, S.; Prabu, R.G. The Influence of Fascial Manipulation on Function, Ankle Dorsiflexion Range of Motion and Postural Sway in Individuals with Chronic Ankle Instability. J. Bodyw. Mov. Ther. 2021, 27, 216–221. [Google Scholar] [CrossRef]
- Myers, T.W. Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists, 3rd ed.; Churchill Livingstone: Melbourne, Australia, 2014. [Google Scholar]
- Joanne, A. Yoga: Fascia, Form, and Functional Movement, 3rd ed.; Handspring Publishing: London, UK, 2015. [Google Scholar]
- Scaravelli, V. Awakening the Spine: Yoga for Health, Vitality, and Energy, 2nd ed.; HarperOne: San Francisco, CA, USA, 2015. [Google Scholar]
- Cleland, J.A.; Childs, J.D.; Whitman, J.M. Psychometric Properties of the Neck Disability Index and Numeric Pain Rating Scale in Patients with Mechanical Neck Pain. Arch. Phys. Med. Rehabil. 2008, 89, 69–74. [Google Scholar] [CrossRef]
- Gibbons, P.; Tehan, P. Manipulation of the Spine, Thorax and Pelvis, 4th ed.; Elsevier: Amsterdam, The Netherlands; Churchill Livingstone: Melbourne, Australia, 2016. [Google Scholar]
- Basmajian, J.V.; Nyberg, R. Rational Manual Therapies: Manipulation, Spinal Motion and Soft Tissue Mobilization; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 1993. [Google Scholar]
- Hengeveld, E.; Banks, K. Maitland’s Vertebral Manipulation Management of Neuromusculoskeletal Disorders, 8th ed.; Elsevier: Amsterdam, The Netherlands, 2013; Volume 1. [Google Scholar]
- Evans, D.W.; Breen, A.C. A Biomechanical Model for Mechanically Efficient Cavitation Production during Spinal Manipulation: Prethrust Position and the Neutral Zone. J. Manip. Physiol. Ther. 2006, 29, 72–82. [Google Scholar] [CrossRef]
- Boyling, J.D.; Jull, G.A. Grieve’s Modern Manual Therapy: The Vertebral Column, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2004. [Google Scholar]
- Bollen, J.C.; Dean, S.G.; Siegert, R.J.; Howe, T.E.; Goodwin, V.A. A Systematic Review of Measures of Self-Reported Adherence to Unsupervised Home-Based Rehabilitation Exercise Programmes, and Their Psychometric Properties. BMJ Open 2014, 4, e005044. [Google Scholar] [CrossRef]
- Argent, R.; Daly, A.; Caulfield, B. Patient Involvement with Home-Based Exercise Programs: Can Connected Health Interventions Influence Adherence? JMIR Mhealth Uhealth 2018, 6, e47. [Google Scholar] [CrossRef]
- Salaffi, F.; Stancati, A.; Silvestri, C.A.; Ciapetti, A.; Grassi, W. Minimal Clinically Important Changes in Chronic Musculoskeletal Pain Intensity Measured on a Numerical Rating Scale. Eur. J. Pain. 2004, 8, 283–291. [Google Scholar] [CrossRef]
- Stratford, P.; Gill, C.; Westaway, M.; Binkley, J. Assessing Disability and Change on Individual Patients: A Report of a Patient Specific Measure. Physiother. Can. 1995, 47, 258–263. [Google Scholar] [CrossRef]
- Fritz, J.M.; George, S.Z. Identifying Psychosocial Variables in Patients with Acute Work-Related Low Back Pain: The Importance of Fear-Avoidance Beliefs. Phys. Ther. 2002, 82, 973–983. [Google Scholar] [CrossRef] [PubMed]
- George, S.Z.; Stryker, S.E. Fear-Avoidance Beliefs and Clinical Outcomes for Patients Seeking Outpatient Physical Therapy for Musculoskeletal Pain Conditions. J. Orthop. Sports Phys. Ther. 2011, 41, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-C.; Chiu, T.T.W.; Lam, T.-H. Psychometric Properties of the Fear-Avoidance Beliefs Questionnaire in Patients with Neck Pain. Clin. Rehabil. 2006, 20, 909–920. [Google Scholar] [CrossRef]
- Costello, M.; Puentedura, E.; Cleland, J.; Ciccone, C.D. The Immediate Effects of Soft Tissue Mobilisation versus Therapeutic Ultrasound for Patients with Neck and Arm Pain with Evidence of Neural Mechanosensitivity: A Randomised Clinical Trial. J. Man. Manip. Ther. 2016, 24, 128–140. [Google Scholar] [CrossRef]
- Smoot, B.; Boyd, B.S.; Byl, N.; Dodd, M. Mechanosensitivity in the Upper Extremity Following Breast Cancer Treatment. J. Hand Ther. 2014, 27, 4–11. [Google Scholar] [CrossRef]
- Coppieters, M.; Stappaerts, K.; Janssens, K.; Jull, G. Reliability of Detecting “onset of Pain” and “Submaximal Pain” during Neural Provocation Testing of the Upper Quadrant. Physiother. Res. Int. 2002, 7, 146–156. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Bellotti, S.; Busato, M.; Cattaneo, C.; Branchini, M. Effectiveness of the Fascial Manipulation Approach Associated with a Physiotherapy Program in Recurrent Shoulder Disease. Life 2023, 13, 1396. [Google Scholar] [CrossRef]
- Suzuki, H.; Aono, S.; Inoue, S.; Imajo, Y.; Nishida, N.; Funaba, M.; Harada, H.; Mori, A.; Matsumoto, M.; Higuchi, F.; et al. Clinically Significant Changes in Pain along the Pain Intensity Numerical Rating Scale in Patients with Chronic Low Back Pain. PLoS ONE 2020, 15, e0229228. [Google Scholar] [CrossRef]
- Pawlukiewicz, M.; Kochan, M.; Niewiadomy, P.; Szuścik-Niewiadomy, K.; Taradaj, J.; Król, P.; Kuszewski, M.T. Fascial Manipulation Method Is Effective in the Treatment of Myofascial Pain, but the Treatment Protocol Matters: A Randomised Control Trial—Preliminary Report. J. Clin. Med. 2022, 11, 4546. [Google Scholar] [CrossRef] [PubMed]
- Edgar, D.; Jull, G.; Sutton, S. The Relationship between Upper Trapezius Muscle Length and Upper Quadrant Neural Tissue Extensibility. Aust. J. Physiother. 1994, 40, 99–103. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fascial Entrapment Neuropathy—Stecco—2019—Clinical Anatomy—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/10.1002/ca.23388 (accessed on 11 September 2023).
- Cleland, J.A.; Childs, J.D.; Fritz, J.M.; Whitman, J.M. Interrater Reliability of the History and Physical Examination in Patients with Mechanical Neck Pain. Arch. Phys. Med. Rehabil. 2006, 87, 1388–1395. [Google Scholar] [CrossRef] [PubMed]
- Stecco, C.; Pirri, C.; Fede, C.; Fan, C.; Giordani, F.; Stecco, L.; Foti, C.; De Caro, R. Dermatome and Fasciatome. Clin. Anat. 2019, 32, 896–902. [Google Scholar] [CrossRef]
- Monticone, M.; Frigau, L.; Vernon, H.; Rocca, B.; Giordano, A.; Simone Vullo, S.; Mola, F.; Franchignoni, F. Reliability, Responsiveness and Minimal Clinically Important Difference of the Two Fear Avoidance and Beliefs Questionnaire Scales in Italian Subjects with Chronic Low Back Pain Undergoing Multidisciplinary Rehabilitation. Eur. J. Phys. Rehabil. Med. 2020, 56, 600–606. [Google Scholar] [CrossRef]

| Characteristics | Group | Mean ± SD | |
|---|---|---|---|
| Age | CG | N = 48 | 26.1 ± 5.83 |
| IG | N = 51 | 27.8 ± 8.00 | |
| Gender: n (%) | CG | Male | 27 (27.3) |
| Female | 21 (21.2) | ||
| IG | Male | 23 (23.2) | |
| Female | 28 (28.3) | ||
| Timeline | Group | NPRS (Mean ± SD) | EEROM (Mean ± SD) | FABQ (Mean ± SD) | PSFS (Mean ± SD) |
|---|---|---|---|---|---|
| Baseline | CG | 5.93 ± 1.572 | 131.60 ± 35.70 | 14.02 ± 5.187 | 4.52 ± 1.592 |
| IG | 6.29 ± 1.969 | 112.92 ± 57.960 | 11.27 ± 7.274 | 3.71 ± 1.958 | |
| 2nd session | CG | 4.64 ± 1.417 | 139.02 ± 31.484 | ||
| IG | 4.31 ± 1.557 | 130.04 ± 43.561 | |||
| 3rd session | CG | 4.11 ± 1.799 | 141.02 ± 30.881 | ||
| IG | 3.10 ± 1.896 | 146.61 ± 32.495 | |||
| 4th session | CG | 3.33 ± 1.871 | 143.78 ± 31.947 | 11.75 ± 4.352 | 6.23 ± 1.696 |
| IG | 1.63 ± 1.482 | 163.90 ± 21.045 | 6.71 ± 6.334 | 6.49 ± 2.559 | |
| Outcomes | F Value | p-Value | Partial η2 | |
|---|---|---|---|---|
| Huynh–Feldt | NPRS | 270.58 | <0.001 | 0.746 |
| NPRS * Group | 22.482 | <0.001 | 0.196 | |
| Greenhouse–Geisser | EEROM | 53.89 | <0.001 | 0.369 |
| EEROM * Group | 21.46 | <0.001 | 0.189 | |
| Huynh–Feldt | FABQ | 70.02 | <0.001 | 0.435 |
| FABQ * GROUP | 7.806 | 0.006 | 0.079 | |
| Huynh–Feldt | PSFS | 79.04 | <0.001 | 0.465 |
| PSFS * GROUP | 4.517 | 0.036 | 0.047 |
| Timeline | NPRS | EEROM | FABQ | PSFS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MD | SE | p-Value | η2p | MD | SE | p-Value | η2p | MD | SE | p-Value | η2p | MD | SE | p-Value | η2p | |
| Baseline | 0.352 | 0.370 | 0.343 | 0.010 | −18.6 | 10.03 | 0.066 | 0.036 | −2.75 | 1.32 | 0.04 | 0.046 | −0.80 | 0.37 | 0.033 | 0.049 |
| 2nd session | −0.338 | 0.308 | 0.275 | 0.013 | −8.98 | 7.90 | 0.259 | 0.014 | ||||||||
| 3rd session | −10.00 | 0.382 | 0.010 | 0.070 | 5.59 | 6.55 | 0.396 | 0.008 | ||||||||
| 4th session | −10.70 | 0.347 | <0.001 | 0.207 | 20.12 | 5.53 | <0.001 | 0.126 | −5.03 | 1.14 | <0.001 | 0.17 | 0.26 | 0.45 | 0.566 | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raja G, P.; Bhat, S.; Gangavelli, R.; Prabhu, A.; Stecco, A.; Pirri, C.; Jaganathan, V.; Fernández-de-Las-Peñas, C. Effectiveness of Deep Cervical Fascial Manipulation® and Sequential Yoga Poses on Pain and Function in Individuals with Mechanical Neck Pain: A Randomised Controlled Trial. Life 2023, 13, 2173. https://doi.org/10.3390/life13112173
Raja G P, Bhat S, Gangavelli R, Prabhu A, Stecco A, Pirri C, Jaganathan V, Fernández-de-Las-Peñas C. Effectiveness of Deep Cervical Fascial Manipulation® and Sequential Yoga Poses on Pain and Function in Individuals with Mechanical Neck Pain: A Randomised Controlled Trial. Life. 2023; 13(11):2173. https://doi.org/10.3390/life13112173
Chicago/Turabian StyleRaja G, Prabu, Shyamasunder Bhat, Ranganath Gangavelli, Anupama Prabhu, Antonio Stecco, Carmelo Pirri, Vennila Jaganathan, and César Fernández-de-Las-Peñas. 2023. "Effectiveness of Deep Cervical Fascial Manipulation® and Sequential Yoga Poses on Pain and Function in Individuals with Mechanical Neck Pain: A Randomised Controlled Trial" Life 13, no. 11: 2173. https://doi.org/10.3390/life13112173
APA StyleRaja G, P., Bhat, S., Gangavelli, R., Prabhu, A., Stecco, A., Pirri, C., Jaganathan, V., & Fernández-de-Las-Peñas, C. (2023). Effectiveness of Deep Cervical Fascial Manipulation® and Sequential Yoga Poses on Pain and Function in Individuals with Mechanical Neck Pain: A Randomised Controlled Trial. Life, 13(11), 2173. https://doi.org/10.3390/life13112173








