Severe Acute Respiratory Syndrome and Particulate Matter Exposure: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Terms
2.2. Quality Assessment and Risk of Bias (RoB)
2.2.1. Assessment of Outcomes
2.2.2. Adjustment for Confounding
2.2.3. Control/Dose–Response Comparator Was Used for Comparative Analysis
2.3. Data Management/Extraction
2.4. Data Synthesis (GraphPad Prism 9; Ver 9.2.0)
3. Results/Synthesis
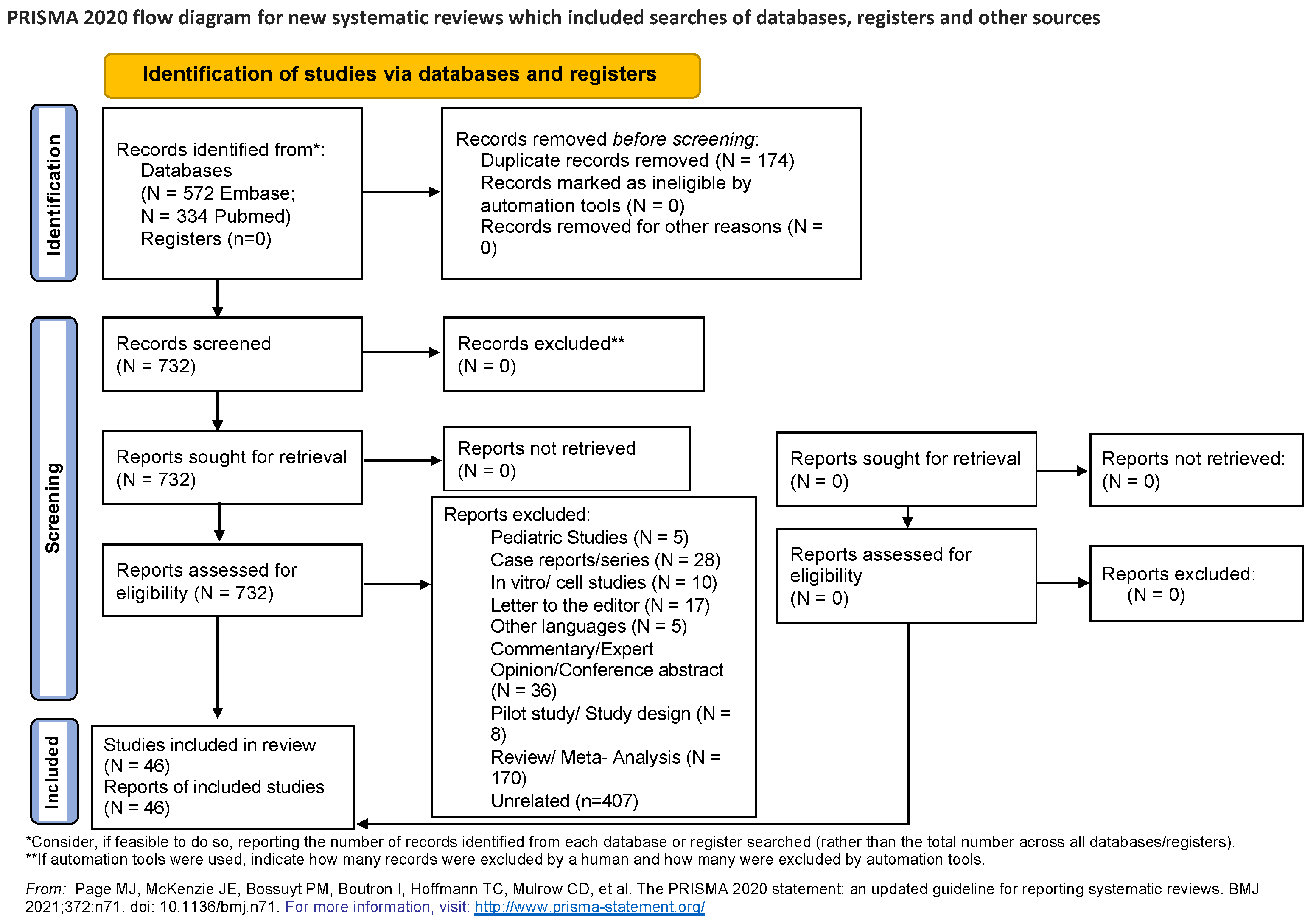
3.1. Literature Search


3.2. Study Characteristics
3.3. Coronaviruses Have Been the Cause of Several Outbreaks
3.4. Temporal Relationship of PM and SARS
3.5. Understanding Geographic Epidemiology Based on Region-Based Outcomes
3.6. Aerodynamic Diameter of PM and SARS (PM2.5 vs. PM10)
4. Discussion
4.1. Geographic Epidemiology
4.2. Temporal Association
5. Conclusions
6. Future Plans
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PM | Particulate matter |
| SARS | Severe acute respiratory syndrome |
| CoV | Coronaviruses |
| ARDS | Acute respiratory distress syndrome |
| C19 | COVID-19 |
| PEO | Population, Exposure, Outcome |
| RoB | Risk of bias |
| RT-PCR | Reverse transcription polymerase chain reaction |
| RAAS | Renin angiotensin aldosterone system |
| TMPRSS2 | Transmembrane serine protease 2 |
| ACE | Angiotensin converting enzyme |
| KKS | (Kallikrein-kinin) systems |
| COPD | Chronic Obstructive Pulmonary Disease |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| UK | United Kingdom |
| US | United States |
| CFR | Case Fatality Rate |
References
- Basics of COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/your-health/about-covid-19/basics-covid-19.html (accessed on 7 January 2023).
- Chafekar, A.; Fielding, B.C. MERS-CoV: Understanding the Latest Human Coronavirus Threat. Viruses 2018, 10, 93. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Timeline. Available online: https://www.cdc.gov/museum/timeline/covid19.html#:~:text=February%2011%2C%202020,of%20%E2%80%9CCoronavirus%20Disease%202019.%E2%80%9D (accessed on 7 January 2023).
- COVID-19 Was Third Leading Cause of Death in U.S. Available online: https://www.cdc.gov/media/releases/2022/s0422-third-leading-cause.html (accessed on 21 November 2022).
- U.S. Environmental Protection Agency. Health and Environmental Effects of Particulate Matter (PM). Available online: https://www.epa.gov/pm-pollution/health-and-environmental-effects-particulate-matter-pm (accessed on 24 June 2022).
- Cai, B.; Xia, T.; Qian, Y.; Lu, H.; Cai, R.; Wang, C. Association Between Fine Particulate Matter and Fatal Hemorrhagic Stroke Incidence: A Time Stratified Case-Crossover Study in Shanghai, China. J. Occup. Environ. Med. 2020, 62, 916–921. [Google Scholar] [CrossRef] [PubMed]
- 9 out of 10 People Worldwide Breathe Polluted Air, but More Countries Are Taking Action. Available online: https://www.who.int/news/item/02-05-2018-9-out-of-10-people-worldwide-breathe-polluted-air-but-more-countries-are-taking-action (accessed on 7 July 2022).
- Seaton, A.; MacNee, W.; Donaldson, K.; Godden, D. Particulate air pollution and acute health effects. Lancet 1995, 345, 176–178. [Google Scholar] [CrossRef]
- Becker, S.; Soukup, J.M. Exposure to urban air particulates alters the macrophage-mediated inflammatory response to respiratory viral infection. J. Toxicol. Environ. Health A 1999, 57, 445–457. [Google Scholar] [CrossRef]
- Mishra, R.; Krishnamoorthy, P.; Gangamma, S.; Raut, A.A.; Kumar, H. Particulate matter (PM10) enhances RNA virus infection through modulation of innate immune responses. Environ. Pollut. 2020, 266, 115148. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.S.; Tsai, F.T.; Lin, C.K.; Yang, C.Y.; Chan, C.C.; Young, C.Y.; Lee, C.H. Ambient influenza and avian influenza virus during dust storm days and background days. Environ. Health Perspect. 2010, 118, 1211–1216. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Zhang, W.; Li, S.; Williams, G.; Liu, C.; Morgan, G.G.; Jaakkola, J.J.K.; Guo, Y. Is short-term exposure to ambient fine particles associated with measles incidence in China? A multi-city study. Environ. Res. 2017, 156, 306–311. [Google Scholar] [CrossRef]
- Croft, D.P.; Zhang, W.; Lin, S.; Thurston, S.W.; Hopke, P.K.; Masiol, M.; Squizzato, S.; van Wijngaarden, E.; Utell, M.J.; Rich, D.Q. The Association between Respiratory Infection and Air Pollution in the Setting of Air Quality Policy and Economic Change. Ann. Am. Thorac. Soc. 2019, 16, 321–330. [Google Scholar] [CrossRef]
- Croft, D.P.; Zhang, W.; Lin, S.; Thurston, S.W.; Hopke, P.K.; van Wijngaarden, E.; Squizzato, S.; Masiol, M.; Utell, M.J.; Rich, D.Q. Associations between Source-Specific Particulate Matter and Respiratory Infections in New York State Adults. Environ. Sci. Technol. 2020, 54, 975–984. [Google Scholar] [CrossRef]
- Ye, Q.; Fu, J.F.; Mao, J.H.; Shang, S.Q. Haze is a risk factor contributing to the rapid spread of respiratory syncytial virus in children. Environ. Sci. Pollut. Res. Int. 2016, 23, 20178–20185. [Google Scholar] [CrossRef]
- Aguilera, R.; Corringham, T.; Gershunov, A.; Benmarhnia, T. Wildfire smoke impacts respiratory health more than fine particles from other sources: Observational evidence from Southern California. Nat. Commun. 2021, 12, 1493. [Google Scholar] [CrossRef] [PubMed]
- Khaniabadi, Y.O.; Daryanoosh, S.M.; Amrane, A.; Polosa, R.; Hopke, P.K.; Goudarzi, G.; Mohammadi, M.J.; Sicard, P.; Armin, H. Impact of Middle Eastern Dust storms on human health. Atmos. Pollut. Res. 2017, 8, 606–613. [Google Scholar] [CrossRef]
- Kim Oanh, N.T.; Nghiem, L.H.; Phyu, Y.L. Emission of Polycyclic Aromatic Hydrocarbons, Toxicity, and Mutagenicity from Domestic Cooking Using Sawdust Briquettes, Wood, and Kerosene. Environ. Sci. Technol. 2002, 36, 833–839. [Google Scholar] [CrossRef]
- Copat, C.; Cristaldi, A.; Fiore, M.; Grasso, A.; Zuccarello, P.; Signorelli, S.S.; Conti, G.O.; Ferrante, M. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: A systematic review. Environ. Res. 2020, 191, 110129. [Google Scholar] [CrossRef]
- Maleki, M.; Anvari, E.; Hopke, P.K.; Noorimotlagh, Z.; Mirzaee, S.A. An updated systematic review on the association between atmospheric particulate matter pollution and prevalence of SARS-CoV-2. Environ. Res. 2021, 195, 110898. [Google Scholar] [CrossRef]
- Frontera, A.; Martin, C.; Vlachos, K.; Sgubin, G. Regional air pollution persistence links to COVID-19 infection zoning. J. Infect. 2020, 81, 318–356. [Google Scholar] [CrossRef]
- Wu, X.; Nethery, R.C.; Sabath, B.M.; Braun, D.; Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study. medRxiv 2020. [Google Scholar] [CrossRef]
- Wang, B.; Chen, H.; Chan, Y.L.; Oliver, B.G. Is there an association between the level of ambient air pollution and COVID-19? Am. J. Physiol. Lung Cell. Mol. Physiol. 2020, 319, L416–L421. [Google Scholar] [CrossRef] [PubMed]
- Coker, E.S.; Cavalli, L.; Fabrizi, E.; Guastella, G.; Lippo, E.; Parisi, M.L.; Pontarollo, N.; Rizzati, M.; Varacca, A.; Vergalli, S. The Effects of Air Pollution on COVID-19 Related Mortality in Northern Italy. Environ. Resour. Econ. 2020, 76, 611–634. [Google Scholar] [CrossRef]
- Frontera, A.; Cianfanelli, L.; Vlachos, K.; Landoni, G.; Cremona, G. Severe air pollution links to higher mortality in COVID-19 patients: The “double-hit” hypothesis. J. Infect. 2020, 81, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Rev. Esp. Cardiol. 2021, 74, 790–799. [Google Scholar] [CrossRef]
- Particulate Matter (PM) Basics. Available online: https://www.epa.gov/pm-pollution/particulate-matter-pm-basics (accessed on 26 November 2022).
- Lee, K.K.; Bing, R.; Kiang, J.; Bashir, S.; Spath, N.; Stelzle, D.; Mortimer, K.; Bularga, A.; Doudesis, D.; Joshi, S.S.; et al. Adverse health effects associated with household air pollution: A systematic review, meta-analysis, and burden estimation study. Lancet Glob. Health 2020, 8, e1427–e1434. [Google Scholar] [CrossRef]
- Systematic Reviews. Available online: https://rmit.libguides.com/systematicreviews/synthesise (accessed on 6 January 2022).
- Kan, H.D.; Chen, B.H.; Fu, C.W.; Yu, S.Z.; Mu, L.N. Relationship between ambient air pollution and daily mortality of SARS in Beijing. Biomed. Environ. Sci. 2005, 18, 1–4. [Google Scholar]
- Li, H.; Xu, X.L.; Dai, D.W.; Huang, Z.Y.; Ma, Z.; Guan, Y.J. Air pollution and temperature are associated with increased COVID-19 incidence: A time series study. Int. J. Infect. Dis. 2020, 97, 278–282. [Google Scholar] [CrossRef]
- Lu, B.; Wu, N.; Jiang, J.; Li, X. Associations of acute exposure to airborne pollutants with COVID-19 infection: Evidence from China. Environ. Sci. Pollut. Res. Int. 2021, 28, 50554–50564. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, M.M. Significance between air pollutants, meteorological factors, and COVID-19 infections: Probable evidences in India. Environ. Sci. Pollut. Res. Int. 2021, 28, 40474–40495. [Google Scholar] [CrossRef]
- Sangkham, S.; Thongtip, S.; Vongruang, P. Influence of air pollution and meteorological factors on the spread of COVID-19 in the Bangkok Metropolitan Region and air quality during the outbreak. Environ. Res. 2021, 197, 111104. [Google Scholar] [CrossRef]
- Shao, L.; Cao, Y.; Jones, T.; Santosh, M.; Silva, L.F.O.; Ge, S.; da Boit, K.; Feng, X.; Zhang, M.; BéruBé, K. COVID-19 mortality and exposure to airborne PM(2.5): A lag time correlation. Sci. Total Environ. 2022, 806, 151286. [Google Scholar] [CrossRef]
- Yao, Y.; Pan, J.; Wang, W.; Liu, Z.; Kan, H.; Qiu, Y.; Meng, X.; Wang, W. Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Sci. Total Environ. 2020, 741, 140396. [Google Scholar] [CrossRef]
- Beig, G.; Bano, S.; Sahu, S.K.; Anand, V.; Korhale, N.; Rathod, A.; Yadav, R.; Mangaraj, P.; Murthy, B.S.; Singh, S.; et al. COVID-19 and environmental -weather markers: Unfolding baseline levels and veracity of linkages in tropical India. Environ. Res. 2020, 191, 110121. [Google Scholar] [CrossRef]
- Laxmipriya, S.; Narayanan, R.M. COVID-19 and its relationship to particulate matter pollution—Case study from part of greater Chennai, India. Mater. Today Proc. 2021, 43, 1634–1639. [Google Scholar] [CrossRef]
- Bianconi, V.; Bronzo, P.; Banach, M.; Sahebkar, A.; Mannarino, M.R.; Pirro, M. Particulate matter pollution and the COVID-19 outbreak: Results from Italian regions and provinces. Arch. Med. Sci. 2020, 16, 985–992. [Google Scholar] [CrossRef]
- Dragone, R.; Licciardi, G.; Grasso, G.; Del Gaudio, C.; Chanussot, J. Analysis of the Chemical and Physical Environmental Aspects that Promoted the Spread of SARS-CoV-2 in the Lombard Area. Int. J. Environ. Res. Public Health 2021, 18, 1226. [Google Scholar] [CrossRef]
- Fattorini, D.; Regoli, F. Role of the chronic air pollution levels in the COVID-19 outbreak risk in Italy. Environ. Pollut. 2020, 264, 114732. [Google Scholar] [CrossRef] [PubMed]
- Rovetta, A.; Bhagavathula, A.S.; Castaldo, L. Modeling the Epidemiological Trend and Behavior of COVID-19 in Italy. Cureus 2020, 12, e9884. [Google Scholar] [CrossRef] [PubMed]
- Moshammer, H.; Poteser, M.; Hutter, H.P. COVID-19 and air pollution in Vienna-a time series approach. Wien. Klin. Wochenschr. 2021, 133, 951–957. [Google Scholar] [CrossRef]
- Dettori, M.; Deiana, G.; Balletto, G.; Borruso, G.; Murgante, B.; Arghittu, A.; Azara, A.; Castiglia, P. Air pollutants and risk of death due to COVID-19 in Italy. Environ. Res. 2021, 192, 110459. [Google Scholar] [CrossRef]
- Meo, S.A.; Adnan Abukhalaf, A.; Sami, W.; Hoang, T.D. Effect of environmental pollution PM2.5, carbon monoxide, and ozone on the incidence and mortality due to SARS-CoV-2 infection in London, United Kingdom. J. King Saud Univ. Sci. 2021, 33, 101373. [Google Scholar] [CrossRef]
- Scalsky, R.J.; Chen, Y.J.; Ying, Z.; Perry, J.A.; Hong, C.C. The Social and Natural Environment′s Impact on SARS-CoV-2 Infections in the UK Biobank. Int. J. Environ. Res. Public Health 2022, 19, 533. [Google Scholar] [CrossRef]
- Kogevinas, M.; Castaño-Vinyals, G.; Karachaliou, M.; Espinosa, A.; de Cid, R.; Garcia-Aymerich, J.; Carreras, A.; Cortés, B.; Pleguezuelos, V.; Jiménez, A.; et al. Ambient Air Pollution in Relation to SARS-CoV-2 Infection, Antibody Response, and COVID-19 Disease: A Cohort Study in Catalonia, Spain (COVICAT Study). Environ. Health Perspect. 2021, 129, 117003. [Google Scholar] [CrossRef]
- Marquès, M.; Correig, E.; Ibarretxe, D.; Anoro, E.; Antonio Arroyo, J.; Jericó, C.; Borrallo, R.M.; Miret, M.; Näf, S.; Pardo, A.; et al. Long-term exposure to PM10 above WHO guidelines exacerbates COVID-19 severity and mortality. Environ. Int. 2022, 158, 106930. [Google Scholar] [CrossRef]
- Veronesi, G.; De Matteis, S.; Calori, G.; Pepe, N.; Ferrario, M.M. Long-term exposure to air pollution and COVID-19 incidence: A prospective study of residents in the city of Varese, Northern Italy. Occup. Environ. Med. 2022, 79, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Zoran, M.A.; Savastru, R.S.; Savastru, D.M.; Tautan, M.N.; Baschir, L.A.; Tenciu, D.V. Assessing the impact of air pollution and climate seasonality on COVID-19 multiwaves in Madrid, Spain. Environ. Res. 2022, 203, 111849. [Google Scholar] [CrossRef] [PubMed]
- Semczuk-Kaczmarek, K.; Rys-Czaporowska, A.; Sierdzinski, J.; Kaczmarek, L.D.; Szymanski, F.M.; Platek, A.E. Association between air pollution and COVID-19 mortality and morbidity. Intern. Emerg. Med. 2021, 17, 467–473. [Google Scholar] [CrossRef]
- Di Ciaula, A.; Bonfrate, L.; Portincasa, P.; Appice, C.; Belfiore, A.; Binetti, M.; Cafagna, G.; Campanale, G.; Carrieri, A.; Cascella, G.; et al. Nitrogen dioxide pollution increases vulnerability to COVID-19 through altered immune function. Environ. Sci. Pollut. Res. Int. 2022, 29, 44404–44412. [Google Scholar] [CrossRef]
- Czwojdzińska, M.; Terpińska, M.; Kuźniarski, A.; Płaczkowska, S.; Piwowar, A. Exposure to PM2.5 and PM10 and COVID-19 infection rates and mortality: A one-year observational study in Poland. Biomed. J. 2021, 44, S25–S36. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.; Romer Present, P.; Richardson, K. Long-term air pollution and other risk factors associated with COVID-19 at the census tract level in Colorado. Environ. Pollut. 2021, 287, 117584. [Google Scholar] [CrossRef]
- Bozack, A.; Pierre, S.; DeFelice, N.; Colicino, E.; Jack, D.; Chillrud, S.N.; Rundle, A.; Astua, A.; Quinn, J.W.; McGuinn, L.; et al. Long-Term Air Pollution Exposure and COVID-19 Mortality: A Patient-Level Analysis from New York City. Am. J. Respir. Crit. Care Med. 2021, 205, 651–662. [Google Scholar] [CrossRef]
- Fang, F.; Mu, L.; Zhu, Y.; Rao, J.; Heymann, J.; Zhang, Z.F. Long-Term Exposure to PM2.5, Facemask Mandates, Stay Home Orders and COVID-19 Incidence in the United States. Int. J. Environ. Res. Public Health 2021, 18, 6274. [Google Scholar] [CrossRef]
- Kiser, D.; Elhanan, G.; Metcalf, W.J.; Schnieder, B.; Grzymski, J.J. SARS-CoV-2 test positivity rate in Reno, Nevada: Association with PM2.5 during the 2020 wildfire smoke events in the western United States. J. Expo. Sci. Environ. Epidemiol. 2021, 31, 797–803. [Google Scholar] [CrossRef]
- Mendy, A.; Wu, X.; Keller, J.L.; Fassler, C.S.; Apewokin, S.; Mersha, T.B.; Xie, C.; Pinney, S.M. Air pollution and the pandemic: Long-term PM2.5 exposure and disease severity in COVID-19 patients. Respirology 2021, 26, 1181–1187. [Google Scholar] [CrossRef]
- Meo, S.A.; Abukhalaf, A.A.; Alessa, O.M.; Alarifi, A.S.; Sami, W.; Klonoff, D.C. Effect of environmental pollutants PM2.5, CO, NO2, and O3 on the incidence and mortality of SARS-CoV-2 infection in five regions of the USA. Int. J. Environ. Res. Public Health 2021, 18, 7810. [Google Scholar] [CrossRef]
- Meo, S.A.; Abukhalaf, A.A.; Alomar, A.A.; Alessa, O.M. Wildfire and COVID-19 pandemic: Effect of environmental pollution PM2.5 and carbon monoxide on the dynamics of daily cases and deaths due to SARS-CoV-2 infection in San-Francisco USA. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 10286–10292. [Google Scholar] [CrossRef]
- Meo, S.A.; Abukhalaf, A.A.; Alomar, A.A.; Alessa, O.M.; Sami, W.; Klonoff, D.C. Effect of environmental pollutants PM2.5, carbon monoxide, and ozone on the incidence and mortality of SARS-CoV-2 infection in ten wildfire affected counties in California. Sci. Total Environ. 2021, 757, 143948. [Google Scholar] [CrossRef]
- Meo, S.A.; Almutairi, F.J.; Abukhalaf, A.A.; Usmani, A.M. Effect of green space environment on air pollutants PM2.5, PM10, CO, O3 and incidence and mortality of SARS-CoV-2 in highly green and less-green countries. Int. J. Environ. Res. Public Health 2021, 18, 13151. [Google Scholar] [CrossRef]
- Adhikari, A.; Yin, J. Short-term effects of Ambient Ozone, PM2.5, and meteorological factors on COVID-19 confirmed cases and deaths in Queens, New York. Int. J. Environ. Res. Public Health 2020, 17, 4047. [Google Scholar] [CrossRef]
- Gujral, H.; Sinha, A. Association between exposure to airborne pollutants and COVID-19 in Los Angeles, United States with ensemble-based dynamic emission model. Environ. Res. 2021, 194, 110704. [Google Scholar] [CrossRef]
- Cortes-Ramirez, J.; Michael, R.N.; Knibbs, L.D.; Bambrick, H.; Haswell, M.R.; Wraith, D. The association of wildfire air pollution with COVID-19 incidence in New South Wales, Australia. Sci. Total Environ. 2022, 809, 151158. [Google Scholar] [CrossRef]
- Ben Maatoug, A.; Triki, M.B.; Fazel, H. How do air pollution and meteorological parameters contribute to the spread of COVID-19 in Saudi Arabia? Environ. Sci. Pollut. Res. Int. 2021, 28, 44132–44139. [Google Scholar] [CrossRef]
- Hadei, M.; Hopke, P.K.; Shahsavani, A.; Raeisi, A.; Jafari, A.J.; Yarahmadi, M.; Farhadi, M.; Rahmatinia, M.; Bazazpour, S.; Bandpey, A.M.; et al. Effect of short-term exposure to air pollution on COVID-19 mortality and morbidity in Iranian cities. J. Environ. Health Sci. Eng. 2021, 19, 1807–1816. [Google Scholar] [CrossRef]
- Meo, S.A.; Almutairi, F.J.; Abukhalaf, A.A.; Alessa, O.M.; Al-Khlaiwi, T.; Meo, A.S. Sandstorm and its effect on particulate matter PM2.5, carbon monoxide, nitrogen dioxide, ozone pollutants and SARS-CoV-2 cases and deaths. Sci. Total Environ. 2021, 795, 148764. [Google Scholar] [CrossRef] [PubMed]
- Ghanim, A.A.J. Analyzing the severity of coronavirus infections in relation to air pollution: Evidence-based study from Saudi Arabia. Environ. Sci. Pollut. Res. Int. 2022, 29, 6267–6277. [Google Scholar] [CrossRef] [PubMed]
- Akan, A.P. Transmission of COVID-19 pandemic (Turkey) associated with short-term exposure of air quality and climatological parameters. Environ. Sci. Pollut. Res. Int. 2022, 31, 41695–41712. [Google Scholar] [CrossRef]
- Norouzi, N.; Asadi, Z. Air pollution impact on the COVID-19 mortality in Iran considering the comorbidity (obesity, diabetes, and hypertension) correlations. Environ. Res. 2022, 204 Pt A, 112020. [Google Scholar] [CrossRef]
- Bolano-Ortiz, T.R.; Camargo-Caicedo, Y.; Puliafito, S.E.; Ruggeri, M.F.; Bolano-Diaz, S.; Pascual-Flores, R.; Saturno, J.; Ibarra-Espinosa, S.; Mayol-Bracero, O.L.; Torres-Delgado, E.; et al. Spread of SARS-CoV-2 through Latin America and the Caribbean region: A look from its economic conditions, climate and air pollution indicators. Environ. Res. 2020, 191, 109938. [Google Scholar] [CrossRef]
- Lopez-Feldman, A.; Heres, D.; Marquez-Padilla, F. Air pollution exposure and COVID-19: A look at mortality in Mexico City using individual-level data. Sci. Total Environ. 2021, 756, 143929. [Google Scholar] [CrossRef]
- Salgado, M.V.; Smith, P.; Opazo, M.A.; Huneeus, N. Long-term exposure to fine and coarse particulate matter and COVID-19 incidence and mortality rate in chile during 2020. Int. J. Environ. Res. Public Health 2021, 18, 7409. [Google Scholar] [CrossRef]
- SARS Basics Fact Sheet. Available online: https://www.cdc.gov/sars/about/fs-sars.html (accessed on 22 November 2022).
- Chiu, R.W.; Chim, S.S.; Tong, Y.K.; Fung, K.S.; Chan, P.K.; Zhao, G.P.; Lo, Y.M. Tracing SARS-coronavirus variant with large genomic deletion. Emerg. Infect. Dis. 2005, 11, 168–170. [Google Scholar] [CrossRef]
- SARS-CoV-2 Variant Classification and Definitions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html (accessed on 21 November 2022).
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 22 November 2022).
- Kanu, F.A.; Smith, E.E.; Offutt-Powell, T.; Hong, R.; Delaware Case, I.; Contact Tracing, T.; Dinh, T.H.; Pevzner, E. Declines in SARS-CoV-2 Transmission, Hospitalizations, and Mortality After Implementation of Mitigation Measures- Delaware, March-June 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1691–1694. [Google Scholar] [CrossRef]
- Mortality Analyses. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 22 November 2022).
- Signorini, C.; Pignatti, P.; Coccini, T. How Do Inflammatory Mediators, Immune Response and Air Pollution Contribute to COVID-19 Disease Severity? A Lesson to Learn. Life 2021, 11, 182. [Google Scholar] [CrossRef]
- Mazzoli-Rocha, F.; Fernandes, S.; Einicker-Lamas, M.; Zin, W.A. Roles of oxidative stress in signaling and inflammation induced by particulate matter. Cell Biol. Toxicol. 2010, 26, 481–498. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Zhang, Z.F.; Froines, J.; Zhao, J.; Wang, H.; Yu, S.Z.; Detels, R. Air pollution and case fatality of SARS in the People′s Republic of China: An ecologic study. Environ. Health 2003, 2, 15. [Google Scholar] [CrossRef] [PubMed]
- Nor, N.S.M.; Yip, C.W.; Ibrahim, N.; Jaafar, M.H.; Rashid, Z.Z.; Mustafa, N.; Hamid, H.H.A.; Chandru, K.; Latif, M.T.; Saw, P.E.; et al. Particulate matter (PM2.5) as a potential SARS-CoV-2 carrier. Sci. Rep. 2021, 11, 2508. [Google Scholar] [CrossRef]
- Sagawa, T.; Tsujikawa, T.; Honda, A.; Miyasaka, N.; Tanaka, M.; Kida, T.; Hasegawa, K.; Okuda, T.; Kawahito, Y.; Takano, H. Exposure to particulate matter upregulates ACE2 and TMPRSS2 expression in the murine lung. Environ. Res. 2021, 195, 110722. [Google Scholar] [CrossRef] [PubMed]
- Tung, N.T.; Cheng, P.-C.; Chi, K.-H.; Hsiao, T.-C.; Jones, T.; BéruBé, K.; Ho, K.-F.; Chuang, H.-C. Particulate matter and SARS-CoV-2: A possible model of COVID-19 transmission. Sci. Total Environ. 2021, 750, 141532. [Google Scholar] [CrossRef]
- Comunian, S.; Dongo, D.; Milani, C.; Palestini, P. Air Pollution and COVID-19: The Role of Particulate Matter in the Spread and Increase of COVID-19’s Morbidity and Mortality. Int. J. Environ. Res. Public Health 2020, 17, 4487. [Google Scholar] [CrossRef]
- Aztatzi-Aguilar, O.G.; Uribe-Ramírez, M.; Arias-Montaño, J.A.; Barbier, O.; De Vizcaya-Ruiz, A. Acute and subchronic exposure to air particulate matter induces expression of angiotensin and bradykinin-related genes in the lungs and heart: Angiotensin-II type-I receptor as a molecular target of particulate matter exposure. Part. Fibre Toxicol. 2015, 12, 17. [Google Scholar] [CrossRef]
- Chen, J.; Guo, X.; Pan, H.; Zhong, S. What determines city’s resilience against epidemic outbreak: Evidence from China’s COVID-19 experience. Sustain. Cities Soc. 2021, 70, 102892. [Google Scholar] [CrossRef]
- Bossak, B.H.; Turk, C.A. Spatial Variability in COVID-19 Mortality. Int. J. Environ. Res. Public Health 2021, 18, 5892. [Google Scholar] [CrossRef] [PubMed]
- Bo, M.; Mercalli, L.; Pognant, F.; Cat Berro, D.; Clerico, M. Urban air pollution, climate change and wildfires: The case study of an extended forest fire episode in northern Italy favoured by drought and warm weather conditions. Energy Rep. 2020, 6, 781–786. [Google Scholar] [CrossRef]
- Han, C.H.; Pak, H.; Lee, J.M.; Chung, J.H. Short-term effects of exposure to particulate matter on hospital admissions for asthma and chronic obstructive pulmonary disease. Medicine 2022, 101, e30165. [Google Scholar] [CrossRef]
- Rice, M.B.; Ljungman, P.L.; Wilker, E.H.; Dorans, K.S.; Gold, D.R.; Schwartz, J.; Koutrakis, P.; Washko, G.R.; O’Connor, G.T.; Mittleman, M.A. Long-term exposure to traffic emissions and fine particulate matter and lung function decline in the Framingham heart study. Am. J. Respir. Crit. Care Med. 2015, 191, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, L.I.; Jones, S.A.; Cerfolio, R.J.; Francois, F.; Greco, J.; Rudy, B.; Petrilli, C.M. Trends in COVID-19 Risk-Adjusted Mortality Rates. J. Hosp. Med. 2021, 16, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E. Remdesivir for the Treatment of COVID-19—Preliminary Report. Reply. N. Engl. J. Med. 2020, 383, 994. [Google Scholar] [CrossRef]
- Group, R.C.; Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; et al. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef]
- Gandhi, M.; Rutherford, G.W. Facial Masking for COVID-19. Reply. N. Engl. J. Med. 2020, 383, 2093–2094. [Google Scholar] [CrossRef] [PubMed]
| Study Author [Ref.] | Country | Exposure/ Design | Study Size/Time Period | Specimen/ Assay | End Points | Additional Findings | ||
|---|---|---|---|---|---|---|---|---|
| 1 | ASIA | Kan [30] | China | PM10 Cohort Study | Beijing/N = 37/ 25 April–31 May 2003 | RT-PCR | Mortality |
|
| 2 | Li [31] | China | PM2.5 and 10 Time series Study | Wuhan and Xiaogan 26 January–29 February 2020 | RT-PCR | Incidence |
| |
| 3 | Lu [32] | China | PM2.5 Cohort study | 41 cities/N = 22,970/ 20 January–29 February 2020 | RT-PCR | Incidence |
| |
| 4 | Sahoo [33] | India | PM2.5 and 10 Time series study | 32 states and union territories/N = 21,700/30 January–24 April 2020 | RT-PCR | Incidence |
| |
| 5 | Sangkham [34] | Thailand | PM2.5, and 10 Cohort Study | Bangkok City 30 March 2020 | RT-PCR | Incidence |
| |
| 6 | Shao [35] | China | PM2.5 and 10 Cohort Study | Wuhan City 23 January–7 April 2020 | RT-PCR | Mortality |
| |
| 7 | Yao [36] | China | PM2.5 and 10 Cohort Study | 49 cities February 2020 | RT-PCR | Case fatality rate (CFR) |
| |
| 8 | Beig [37] | India | PM2.5 Cohort Study | 6 Cities May 2022 | RT-PCR | Mortality |
| |
| 9 | Laxmipriya [38] | India | PM2.5 and 10 Cohort study | 11 stations in Chennai city/July 2020 | RT-PCR | Incidence |
| |
| 10 | EUROPE | Frontera [25] | Italy | PM2.5 Cohort study | 21 territories/ March 2020 | RT-PCR | Prevalence, ICU admissions, Mortality |
|
| 11 | Bianconii [39] | Italy | PM2.5 and 10 Cohort Study | 20 provinces/N = 105,792 31 March 2020 | RT-PCR | Incidence proportion and mortality |
| |
| 12 | Dragone [40] | Italy | PM2.5 and 10 Cohort study | Lombard region/ N = 42,283/ 1 February–31 March 2020 | RT-PCR | Prevalence |
| |
| 13 | Fattorini [41] | Italy | PM2.5 and 10 Cohort study | N = 18,000 February–April 2020 | RT-PCR | Incidence |
| |
| 14 | Rovetta [42] | Italy | PM2.5 and 10 Cohort study | Lombardy; N = 82,992/ February–March 2020 | Unclear | Mortality rate |
| |
| 15 | Moshammer [43] | Austria | PM10 Time Series study | Vienna/N = 1665/ March–April 2020 | RT-PCR | Incidence |
| |
| 16 | Dettori [44] | Italy | PM10 Cohort Study | N = 60,359,546/ June 2020 | RT-PCR | Standardized Mortality Ratio |
| |
| 17 | Meo [45] | United Kingdom | PM2.5 Cohort Study | Cases 24 February–2 November 2020 | RT-PCR | Incidence and Mortality |
| |
| 18 | Scalsky [46] | United Kingdom | PM2.5 Cohort | UK biobank; N = 15,156/16 March 2020–16 March 2021 | RT-PCR | Incidence |
| |
| 19 | Kogevinas [47] | Spain | PM2.5 Cohort Study | Catalonia/N = 9605/June–November 2020 | RT-PCR | Incidence |
| |
| 20 | Marques [48] | Spain | PM10 Cohort Study | Catalan hospitals N = 2112 April–June 2020 | RT-PCR | C19 severity and mortality |
| |
| 21 | Veronesi [49] | Italy | PM2.5 and 10 Cohort Study | Varese; N = 62,848 25 February 2020–13 March 2021 | RT-PCR | Incidence |
| |
| 22 | Zoran [50] | Spain | PM2.5 and 10 Cohort Study | 6.61 million Inhabitants January 2020–July 2021 | RT-PCR | Incidence, Prevalence and Mortality |
| |
| 23 | Semczuk–Kaczmarek [51] | Poland | PM2.5 and 10 Cohort Study | N = 18,016 4 March–15 May 2020 | RT-PCR | Mortality and Morbidity |
| |
| 24 | Di Ciaula [52] | Italy | PM10 Cohort Study | 10 cities; N = 147 March–April 2020 | RT-PCR | Mortality |
| |
| 25 | Czwojdzinska [53] | Poland | PM2.5 and 10 Cohort study | N = 38,411,148 4 March–18 November 2020 | RT-PCR | Incidence and mortality |
| |
| 26 | USA | Berg [54] | USA | PM2.5 Cohort study | Colorado N = 34,439 1 March–31 August 2020 | RT-PCR | Incidence, hospitalization and mortality |
|
| 27 | Bozack [55] | USA | PM2.5 Cohort Study | Seven NYC hospitals N = 6542 8 March–30 August 2020 | RT-PCR | Mortality, ICU admission, Intubation |
| |
| 28 | Fang [56] | USA | 3096 counties; PM2.5 Cohort Study | Cumulative Cases: 1st [May: 20,764] and 2nd [September: 34,596] surge in 2020 | RT-PCR | Incidence |
| |
| 29 | Kiser [57] | USA | Nevada/PM2.5/Cohort Study | Regional hospital, Reno/15 May–20 October 2020 | RT-PCR | Incidence |
| |
| 30 | Mendy [58] | USA | PM2.5/Cohort study | Cincinnati/N = 14,783/ 13 March–30 September 2020 | RT-PCR | Disease Severity |
| |
| 31 | Meo [59] | USA | PM2.5/Cohort study | 5 regions; N = 1192 13 March–31 December 2020 | RT-PCR | Incidence and Mortality |
| |
| 32 | Meo [60] | USA | PM2.5/Cohort Study | California 20 March–16 September 2020 | RT-PCR | Incidence, Prevalence and mortality |
| |
| 33 | Meo [61] | USA | California /PM2.5/ Cohort study | California/19 March–15 August 2020 | RT-PCR | Incidence and mortality |
| |
| 34 | Meo [62] | USA | PM2.5 Cohort study | 17 countries 25 January 2020–11 July 2021 | RT-PCR | Incidence and Mortality |
| |
| 35 | Adhikari [63] | USA | PM2.5 Cohort study | New York/N = 42,023 cases/April 2020 | RT-PCR | Incidence Rate Ratio, Mortality |
| |
| 36 | Gujral [64] | USA | PM2.5 Cohort study | California January–July 2020 | RT-PCR | Incidence |
| |
| 37 | AUSTRALIA | Cortes-Ramirez [65] | Australia | PM10 Cohort study | New South Wales/ 2 March–2 August 2020 | RT-PCR | Incidence |
|
| 38 | MIDDLE EAST | Maatoug [66] | Saudi Arabia | PM10 Cohort study | Riyadh, Jeddah, Makkah/N = 354,813 9 March–9 November 2020 | RT-PCR | Incidence |
|
| 39 | Hadei [67] | Iran | PM2.5 and 10 Cohort study | N = 114,964 February–January 2021 | RT-PCR | Mortality and morbidity |
| |
| 40 | Meo [68] | Saudi Arabia | PM2.5 Cohort Study | Riyadh 20 February–2 April 2021 | RT-PCR | Incidence and mortality |
| |
| 41 | Ghanim [69] | Saudi Arabia | PM10 Cohort study | 13 regions; N = 194,255 June 2020 | RT-PCR | Incidence and Mortality |
| |
| 42 | Akan [70] | Turkey | PM2.5 and 10 Cohort study | 15 Provinces N = 42,618,331 8 February–8 May 2021 | RT-PCR | Incidence |
| |
| 43 | Norouzi [71] | Iran | PM2.5 Cohort study | 12 cities/N = 73,080/ 1 March 2019–31 August 2020 | RT-PCR | Incidence |
| |
| 44 | LATIN AMERICA | Bolano-Ortiz [72] | Latin America and Caribbean | PM2.5 and 10 Cohort study | Ten cities/N = 56.95 million/1 April–31 May 2020 | Unknown | Incidence rate and mortality |
|
| 45 | Lopez-Feldman [73] | Mexico | PM2.5 Cohort study | Residents of (Hidalgo, and Mexico City) 7 October 2020 | RT-PCR | Mortality |
| |
| 46 | Salgado [74] | Chile | PM2.5 and 10 Cohort Study | 188 communes/N = 4574 May 2021 | RT-PCR | Incidence and mortality |
| |
 Positive association
Positive association  Negative association
Negative association  Unclear/Equivocal association
Unclear/Equivocal association  Late Pandemic
Late Pandemic  SARS-1.
SARS-1.Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Podury, S.; Kwon, S.; Javed, U.; Farooqi, M.S.; Li, Y.; Liu, M.; Grunig, G.; Nolan, A. Severe Acute Respiratory Syndrome and Particulate Matter Exposure: A Systematic Review. Life 2023, 13, 538. https://doi.org/10.3390/life13020538
Podury S, Kwon S, Javed U, Farooqi MS, Li Y, Liu M, Grunig G, Nolan A. Severe Acute Respiratory Syndrome and Particulate Matter Exposure: A Systematic Review. Life. 2023; 13(2):538. https://doi.org/10.3390/life13020538
Chicago/Turabian StylePodury, Sanjiti, Sophia Kwon, Urooj Javed, Muhammad S. Farooqi, Yiwei Li, Mengling Liu, Gabriele Grunig, and Anna Nolan. 2023. "Severe Acute Respiratory Syndrome and Particulate Matter Exposure: A Systematic Review" Life 13, no. 2: 538. https://doi.org/10.3390/life13020538
APA StylePodury, S., Kwon, S., Javed, U., Farooqi, M. S., Li, Y., Liu, M., Grunig, G., & Nolan, A. (2023). Severe Acute Respiratory Syndrome and Particulate Matter Exposure: A Systematic Review. Life, 13(2), 538. https://doi.org/10.3390/life13020538







