Phytochemicals: A Promising Alternative for the Prevention of Alzheimer’s Disease
Abstract
:1. Introduction
2. Factors Contributing to AD
2.1. Age Factors
2.2. Degeneration of Anatomical Pathways
2.2.1. Cholinergic Pathway
2.2.2. Cortico-Cortical Pathways
2.3. Environmental Factors
2.3.1. Aluminium Toxicity
2.3.2. Head Injury
2.3.3. Food and Malnutrition
2.4. Genetic Factors
2.4.1. Amyloid Precursor Protein (APP)
2.4.2. Presenilin (PSEN)
2.4.3. Apolipoprotein E (Apo E)
2.5. Mitochondrial Dysfunction
2.5.1. Reduction in Energy Metabolism
2.5.2. Changes in the Primary Oxidative Phosphorylation Enzymes
2.5.3. Dyshomeostasis of Calcium
2.5.4. Mitochondrial DNA (mtDNA)
2.6. Vascular Factor
2.7. Immune System Dysfunction
2.8. Infections
3. Treatment of AD
3.1. Chemical-Based Treatment
3.1.1. Cholinesterase Inhibitors
Donepezil
Rivastigmine
Galantamine (GAL)
3.1.2. N-methyl D-aspartate Receptor (NMDAR) Antagonists
Memantine
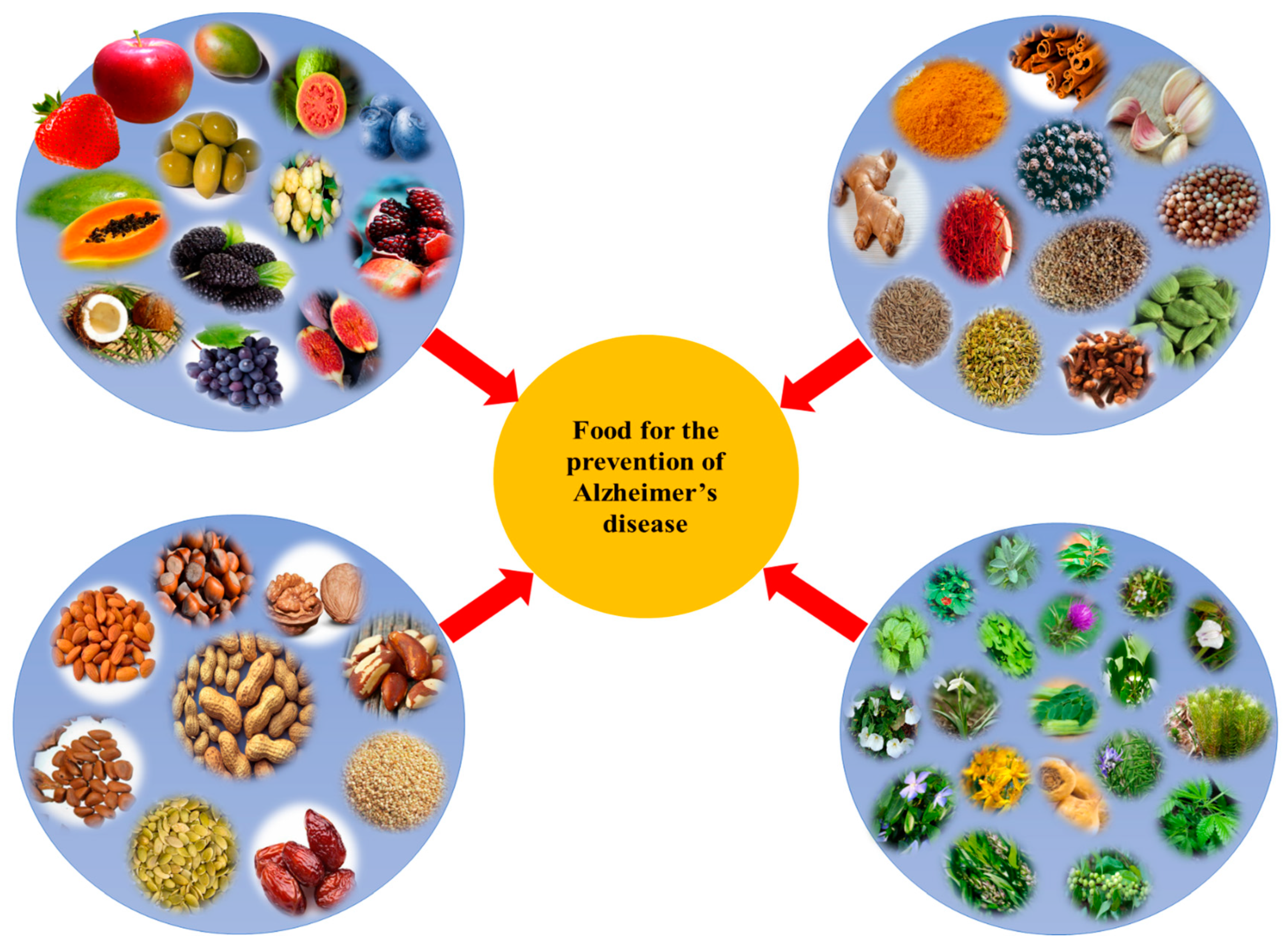
3.2. Plant-Based Treatment
4. Plants with Anti-Alzheimer Properties
4.1. Ginseng
4.2. Gotu Kola
4.3. Ginkgo
4.4. Turmeric
4.5. Brahmi
4.6. Ashwagandha
4.7. Saffron
4.8. Ginger
4.9. Rosemary
4.10. Date Palm
4.11. Pumpkin Seeds
4.12. Garlic
5. Phytochemicals
5.1. Huperzine A
5.2. Epigallocatechin-3-gallate
5.3. Resveratrol
5.4. Rosmarinic Acid
5.5. Galantamine
5.6. Curcumin
5.7. Caffeic Acid
5.8. Silymarin
6. Algal Phytochemicals for Prevention of AD
6.1. Fucoidan
6.2. Phlorotannins
6.3. Homotaurine
6.4. Spirolides
7. Future Prospective
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Haque, R.U.; Levey, A.I. Alzheimer’s disease: A clinical perspective and future nonhuman primate research opportunities. Proc. Natl. Acad. Sci. USA 2019, 116, 26224–26229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sosa-Ortiz, A.L.; Acosta-Castillo, I.; Prince, M.J. Epidemiology of dementias and Alzheimer’s disease. Arch. Med. Res. 2012, 43, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Kaj, B.; de Leon, M.J.; Zetterberg, H. Alzheimer’s disease. Lancet 2006, 368, 387–403. [Google Scholar]
- World Health Organization: Dementia. 2019. Available online: https://www.who.int/en/news–room/factsheets/detail/dementia (accessed on 20 December 2021).
- Prince, M.; Guerchet, M.; Prina, M. Policy Briefs for Heads of Governments. D. Ph.D. Thesis, Alzheimer’s Disease International, London, UK, 2013. [Google Scholar]
- Cumming, T.; Brodtmann, A. Dementia and stroke: The present and future epidemic. Int. J. Stroke 2010, 5, 453–454. [Google Scholar] [CrossRef] [PubMed]
- Marde, V.S.; Tiwari, P.L.; Wankhede, N.L.; Taksande, B.G.; Upaganlawar, A.B.; Umekar, M.J.; Kale, M.B. Neurodegenerative disorders associated with genes of mitochondria. Future J. Pharm. Sci. 2021, 7, 1–8. [Google Scholar] [CrossRef]
- Nunomura, A.; Perry, G.; Hirai, K.; Aliev, G.; Takeda, A.; Chiba, S.; Smith, M.A. Neuronal RNA oxidation in Alzheimer’s disease and Down’s syndrome. Ann. N.Y. Acad. Sci. 1999, 893, 362–364. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhao, B. Oxidative stress and the pathogenesis of Alzheimer’s disease. Oxid. Med. Cell. Longev. 2013, 2013, 316523. [Google Scholar] [CrossRef] [Green Version]
- Wattmo, C.; Minthon, L.; Wallin, Å.K. Mild versus moderate stages of Alzheimer’s disease: Three–year outcomes in a routine clinical setting of cholinesterase inhibitor therapy. Alzheimer’s Res. Ther. 2016, 8, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Chauhan, P.S.; Mishra, M.; Koul, B.; Sharma, M.; Yadav, D. Modifiable risk factors associated with Alzheimer’s disease with special reference to sleep disturbance. CNS Neurol. Disord. Drug Targets 2021, 20, 594–601. [Google Scholar] [CrossRef]
- Heneka, M.T.; Carson, M.J.; Khoury, J.E.; Landreth, G.E.; Brosseron, F.; Feinstein, D.L.; Jacobs, A.H.; Wyss-Coray, T.; Vitorica, J.; Ransohoff, R.M.; et al. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 2015, 14, 388–405. [Google Scholar] [CrossRef] [Green Version]
- Huang, W.J.; Zhang, X.; Chen, W.W. Role of oxidative stress in Alzheimer’s disease. Biomed. Rep. 2016, 4, 519–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karch, C.M.; Cruchaga, C.; Goate, A.M. Alzheimer’s Disease Genetics: From the Bench to the Clinic. Neuron 2014, 83, 11–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chin-Chan, M.; Navarro-Yepes, J.; Quintanilla-Vega, B. Environmental pollutants as risk factors for neurodegenerative disorders: Alzheimer and Parkinson diseases. Front. Cell. Neurosci. 2015, 9, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doroszkiewicz, J.; Mroczko, B. New possibilities in the therapeutic approach to Alzheimer’s Disease. Int. J. Mol. Sci. 2022, 23, 8902. [Google Scholar] [CrossRef]
- Wilson, B.; Geetha, K.M. Neurotherapeutic applications of nanomedicine for treating Alzheimer’s disease. J. Control Release 2020, 325, 25–37. [Google Scholar] [CrossRef]
- Barage, S.H.; Sonawane, K.D. Amyloid cascade hypothesis: Pathogenesis and therapeutic strategies in Alzheimer’s disease. Neuropeptides 2015, 52, 1–18. [Google Scholar] [CrossRef]
- Maresova, P.; Mohelska, H.; Dolejs, J.; Kuca, K. Socio–economic aspects of Alzheimer’s disease. Curr. Alzheimer Res. 2015, 12, 903–911. [Google Scholar] [CrossRef]
- Loureiro, J.A.; Gomes, B.; Coelho, M.A.; do Carmo Pereira, M.; Rocha, S. Targeting nanoparticles across the blood–brain barrier with monoclonal antibodies. Nanomedicine 2014, 9, 709–722. [Google Scholar] [CrossRef]
- Loureiro, J.A.; Gomes, B.; Fricker, G.; Coelho, M.A.N.; Rocha, S.; Pereira, M.C. Cellular uptake of PLGA nanoparticles targeted with anti–amyloid and anti–transferrin receptor antibodies for Alzheimer’s disease treatment. Colloids Surf. B Biointerfaces 2016, 145, 8–13. [Google Scholar] [CrossRef]
- Islam, M.A.; Khandker, S.S.; Alam, F.; Khalil, M.I.; Kamal, M.A.; Gan, S.H. Alzheimer’s Disease and Natural Products: Future Regiments Emerging from Nature. Curr. Top. Med. Chem. 2017, 17, 1408–1428. [Google Scholar]
- Chauhan, P.S.; Yadav, D.; Arukha, A.P. Dietary Nutrients and Prevention of Alzheimer’s disease. CNS Neurol. Disord.-Drug Targets (Former. Curr. Drug Targets-CNS Neurol. Disord.) 2022, 21, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Shafi, O. Inverse relationship between Alzheimer’s disease and cancer, and other factors contributing to Alzheimer’s disease: A systematic review. BMC Neurol. 2016, 16, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scheltens, P.; Strooper, B.D.; Kivipelto, M.; Holstege, H.; Chételat, G.; Teunissen, C.E.; Cummings, J.; van der Flier, W.M. Alzheimer’s disease. Lancet 2021, 397, 1577–1590. [Google Scholar] [CrossRef] [PubMed]
- Scarmeas, N.; Anastasiou, C.A.; Yannakoulia, M. Nutrition and prevention of cognitive impairment. Lancet Neurol. 2018, 17, 1006–1015. [Google Scholar] [CrossRef]
- Imhof, A.; Kövari, E.; Gunten, A.V.; Gold, G.; Rivara, C.B.; Herrmann, F.R.; Hof, P.R.; Bouras, C.; Giannakopoulos, P. Morphological substrates of cognitive decline in nonagenarians and centenarians: A new paradigm? J. Neurol. Sci. 2007, 257, 72–79. [Google Scholar] [CrossRef]
- Heneka, M.T.; Nadrigny, F.; Regen, T.; Martinez-Hernandez, A.; Dumitrescu-Ozimek, L.; Terwel, D.; Jardanhazi-Kurutz, D.; Walter, J.; Kirchhoff, F.; Hanisch, U.; et al. Locus ceruleus controls Alzheimer’s disease pathology by modulating microglial functions through norepinephrine. Proc. Natl. Acad. Sci. USA 2010, 107, 6058–6063. [Google Scholar] [CrossRef] [Green Version]
- Grudzien, A.; Shaw, P.; Weintraub, S.; Bigio, E.; Mash, D.C.; Mesulam, M.M. Locus coeruleus neurofibrillary degeneration in aging, mild cognitive impairment and early Alzheimer’s disease. Neurobiol. Aging 2007, 28, 327–335. [Google Scholar] [CrossRef]
- Sims, N.R.; Bowen, D.M. Changes in choline acetyltransferase and in acetylcholine synthesis. In Alzheimer’s Disease: The Standard Reference; MacMillan: New York, NY, USA, 1983; pp. 37–45. [Google Scholar]
- Whitehouse, P.J.; Price, D.L.; Clark, A.W.; Coyle, J.T.; DeLong, M.R. Alzheimer disease: Evidence for selective loss of cholinergic neurons in the nucleus basalis. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 1981, 10, 122–126. [Google Scholar] [CrossRef]
- Morrison, J.H.; Hof, P.R. Selective vulnerability of corticocortical and hippocampal circuits in aging and Alzheimer’s disease. Prog. Brain Res. 2002, 136, 467–486. [Google Scholar]
- Bowen, D.M.; Francis, P.T.; Palmer, A.M. The biochemistry of cortical and subcortical neurons in Alzheimer’s disease. In Advancing Frontiers in Alzheimer’s Disease Research; University of Texas Press: Austin, TX, USA, 1987; pp. 11–26. [Google Scholar]
- Stricker, N.H.; Schweinsburg, B.C.; Delano-Wood, L.; Wierenga, C.E.; Bangen, K.J.; Haaland, K.Y.; Frank, L.R.; Salmon, D.P.; Bondi, M.W. Decreased white matter integrity in late-myelinating fiber pathways in Alzheimer’s disease supports retrogenesis. Neuroimage 2009, 45, 10–16. [Google Scholar] [CrossRef] [Green Version]
- Delatour, B.; Blanchard, V.; Pradier, L.; Duyckaerts, C. Alzheimer pathology disorganizes cortico-cortical circuitry: Direct evidence from a transgenic animal model. Neurobiol. Dis. 2004, 16, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Scheff, S.W.; Price, D.A. Synapse loss in the temporal lobe in Alzheimer’s disease. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 1993, 33, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.B.; Anitha, S.; Hegde, M.L.; Zecca, L.; Garruto, R.M.; Ravid, R.; Shankar, S.K.; Stein, R.; Shanmugavelu, P.; Rao, K.S.J. Aluminium in Alzheimer’s disease: Are we still at a crossroad? Cell. Mol. Life Sci. 2005, 62, 143–158. [Google Scholar] [CrossRef]
- Armstrong, R.A. What causes Alzheimer’s disease? Folia Neuropathol. 2013, 51, 169–188. [Google Scholar] [CrossRef]
- Mirza, A.; King, A.; Troakes, C.; Exley, C. Aluminium in brain tissue in familial Alzheimer’s disease. J. Trace Elem. Med. Biol. 2017, 40, 30–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giunta, B.; Obregon, D.; Velisetty, R.; Sanberg, P.R.; Borlongan, C.V.; Tan, J. The immunology of traumatic brain injury: A prime target for Alzheimer’s disease prevention. J. Neuroinflamm. 2012, 9, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Rasmusson, D.X.; Brandt, J.; Brandt Martin, D.B.; Folstein, M.F. Head injury as a risk factor in Alzheimer’s disease. Brain Inj. 1995, 9, 213–219. [Google Scholar] [CrossRef]
- Plassman, B.L.; Havlik, R.J.; Steffens, D.C.; Helms, M.J.; Newman, T.N.; Drosdick, D.; Phillips, D.C.; Gau, B.A.; Welsh-Bohmer, K.A.; Burke, J.R.; et al. Documented head injury in early adulthood and risk of Alzheimer’s disease and other dementias. Neurology 2000, 55, 1158–1166. [Google Scholar] [CrossRef]
- Takizawa, C.; Gemmell, E.; Kenworthy, J.; Speyer, R. A systematic review of the prevalence of oropharyngeal dysphagia in stroke, Parkinson’s disease, Alzheimer’s disease, head injury, and pneumonia. Dysphagia 2016, 31, 434–441. [Google Scholar] [CrossRef]
- Amarya, S.; Singh, K.; Sabharwal, M. Changes during aging and their association with malnutrition. J. Clin. Gerontol. Geriatr. 2015, 6, 78–84. [Google Scholar] [CrossRef] [Green Version]
- Roque, M.; Salva, A.; Vellas, B. Malnutrition in community–dwelling adults with dementia (NutriAlz Trial). J. Nutr. Health Aging 2013, 17, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Fleminger, S.; Oliver, D.L.; Lovestone, S.; Rabe-Hesketh, S.; Giora, A. Head injury as a risk factor for Alzheimer’s disease: The evidence 10 years on; a partial replication. J. Neurol. Neurosurg. Psychiatry 2003, 74, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Hu, N.; Yu, J.T.; Tan, L.; Wang, Y.L.; Sun, L.; Tan, L. Nutrition and the risk of Alzheimer’s disease. Biomed. Res. Int. 2013, 2013, 524820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abate, G.; Marziano, M.; Rungratanawanich, W.; Memo, M.; Uberti, D. Nutrition and AGE–ing: Focusing on Alzheimer’s disease. Oxidative Med. Cell. Longev. 2017, 2017, 7039816. [Google Scholar] [CrossRef] [Green Version]
- Koyama, A.; Hashimoto, M.; Tanaka, H.; Fujise, N.; Matsushita, M.; Miyagawa, Y.; Hatada, Y.; Fukuhara, R.; Hasegawa, N.; Todani, S.; et al. Malnutrition in Alzheimer’s disease, dementia with lewy bodies, and frontotemporal lobar degeneration: Comparison using serum albumin, total protein, and hemoglobin level. PLoS ONE 2016, 11, e0157053. [Google Scholar] [CrossRef] [Green Version]
- Wiseman, F.K.; Al-Janabi, T.; Hardy, J.; Karmiloff-Smith, A.; Nizeticgoate, D.; Tybulewicz, V.L.J.; Fisher, E.M.C.; Strydom, A. A genetic cause of Alzheimer disease: Mechanistic insights from Down syndrome. Nat. Rev. Neurosci. 2015, 16, 564–574. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.W.; Thompson, R.; Zhang, H.; Xu, H. APP processing in Alzheimer’s disease. Mol. Brain 2011, 4, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Delacourte, A.; Sergeant, N.; Champain, D.; Wattez, A.; Maurage, C.A.; Maurage Lebert, F.; Pasquier, F.; David, J.P. Nonoverlapping but synergetic tau and APP pathologies in sporadic Alzheimer’s disease. Neurology 2002, 59, 398–407. [Google Scholar] [CrossRef]
- Kabir, M.T.; Uddin, M.S.; Setu, J.R.; Ashraf, G.M.; Bin-Jumah, M.N.; Abdel-Daim, M.M. Exploring the role of PSEN mutations in the pathogenesis of Alzheimer’s disease. Neurotox. Res. 2020, 38, 833–849. [Google Scholar] [CrossRef]
- Moro, M.L.; Giaccone, G.; Lombardi, R.; Indaco, A.; Uggetti, A.; Morbin, M.; Saccucci, S.; Fede, G.D.; Catania, M.; Walsh, D.M.; et al. APP mutations in the Aβ coding region are associated with abundant cerebral deposition of Aβ38. Acta Neuropathol. 2012, 124, 809–821. [Google Scholar] [CrossRef]
- De Strooper, B. Loss-of-function presenilin mutations in Alzheimer disease: Talking Point on the role of presenilin mutations in Alzheimer disease. EMBO Rep. 2007, 8, 141–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Godfrey, M.E.; Wojcik, D.P.; Krone, C.A. Apolipoprotein E genotyping as a potential biomarker for mercury neurotoxicity. J. Alzheimer’s Dis. 2003, 5, 189–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamazaki, Y.; Painter, M.M.; Bu, G.; Kanekiyo, T. Apolipoprotein E as a therapeutic target in Alzheimer’s disease: A review of basic research and clinical evidence. CNS Drugs 2016, 30, 773–789. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Calle, R.; Konings, S.C.; Frontiñán-Rubio, J.; García-Revilla, J.; Camprubí-Ferrer, L.; Svensson, M.; Martinson, I.; Boza-Serrano, A.; Venero, J.L.; Nielsen, H.M.; et al. APOE in the bullseye of neurodegenerative diseases: Impact of the APOE genotype in Alzheimer’s disease pathology and brain diseases. Mol. Neurodegener. 2022, 17, 62. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.C.; Kanekiyo, T.; Xu, H.; Bu, G. Apolipoprotein E and Alzheimer disease: Risk, mechanisms and therapy. Nat. Rev. Neurol. 2013, 9, 106–118. [Google Scholar] [CrossRef] [Green Version]
- Castellani, R.; Hirai, K.; Aliev, G.; Drew, K.L.; Nunomura, A.; Takeda, A.; Cash, A.D.; Obrenovich, M.E.; Perry, G.; Smith, M.A. Role of mitochondrial dysfunction in Alzheimer’s disease. J. Neurosci. Res. 2002, 70, 357–360. [Google Scholar] [CrossRef]
- Gibson, G.E.; Sheu, K.F.R.; Blass, J.P. Abnormalities of mitochondrial enzymes in Alzheimer disease. J. Neural Transm. 1998, 105, 855–870. [Google Scholar] [CrossRef]
- Wang, X.; Su, B.; Zheng, L.; Perry, G.; Smith, M.A.; Zhu, X. The role of abnormal mitochondrial dynamics in the pathogenesis of Alzheimer’s disease. J. Neurochem. 2009, 109, 153–159. [Google Scholar] [CrossRef] [Green Version]
- Yamane, T.; Ikari, Y.; Nishio, T.; Ishii, K.; Kato, T.; Ito, K.; Silverman, D.H.S.; Senda, M.; Asada, T.; Arai, H.; et al. Visual-statistical interpretation of 18F–FDG–PET images for characteristic Alzheimer patterns in a multicenter study: Inter–rater concordance and relationship to automated quantitative evaluation. AJNR Am. J. Neuroradiol. 2014, 35, 244–249. [Google Scholar] [CrossRef] [Green Version]
- Shokouhi, S.; Claassen, D.; Kang, H.; Ding, Z.; Rogers, B.; Mishra, A.; Riddle, W.R.; Alzheimer’s Disease Neuroimaging Initiative. Longitudinal progression of cognitive decline correlates with changes in the spatial pattern of brain 18F–FDG PET. J. Nucl. Med. 2013, 54, 1564–1569. [Google Scholar] [CrossRef] [Green Version]
- Landau, S.M.; Harvey, D.; Madison, C.M.; Koeppe, R.A.; Reiman, E.M.; Foster, N.L.; Weiner, M.W.; Jagust, W.J.; Alzheimer’s Disease Neuroimaging Initiative. Associations between cognitive, functional, and FDG–PET measures of decline in AD and MCI. Neurobiol. Aging 2011, 32, 1207–1218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cottrell, D.A.; Blakely, E.L.; Johnson, M.A.; Ince, P.G.; Turnbull, D.M. Mitochondrial enzyme-deficient hippocampal neurons and choroidal cells in AD. Neurology 2001, 57, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Gibson, G.E.; Chen, H.L.; Xu, H.; Qiu, L.; Xu, Z.; Denton, T.T.; Shi, Q. Deficits in the mitochondrial enzyme α–ketoglutarate dehydrogenase lead to Alzheimer’s disease–like calcium dysregulation. Neurobiol. Aging 2012, 33, 1121.e13–1121.e24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirai, K.; Aliev, G.; Nunomura, A.; Fujioka, H.; Russell, R.L.; Atwood, C.S.; Johnson, A.B.; Kress, y.; Vinters, H.V.; Tabaton, M.; et al. Mitochondrial abnormalities in Alzheimer’s disease. J. Neurosci. 2001, 21, 3017–3023. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mecocci, P.; MacGarvey, U.; Beal, F.M. Oxidative damage to mitochondrial DNA is increased in Alzheimer’s disease. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 1994, 36, 747–751. [Google Scholar] [CrossRef]
- Launer, L.J.; Ross, G.W.; Petrovitch, H.; Masaki, K.; Foley, D.; White, L.R.; Havlik, R.J. Havlik. Midlife blood pressure and dementia: The Honolulu-Asia aging study. Neurobiol. Aging 2000, 21, 49–55. [Google Scholar] [CrossRef]
- Snyder, H.M.; Corriveau, R.A.; Craft, S.; Faber, J.E.; Greenberg, S.M.; Knopman, D.; Lamb, B.T.; Montine, T.J.; Nedergaard, M.; Schaffer, C.B.; et al. Vascular contributions to cognitive impairment and dementia including Alzheimer’s disease. Alzheimer’s Dement. 2015, 11, 710–717. [Google Scholar] [CrossRef] [Green Version]
- Helzner, E.P.; Luchsinger, J.A.; Scarmeas, N.; Cosentino, S.; Brickman, A.M.; Glymour, M.M.; Stern, Y. Contribution of vascular risk factors to the progression in Alzheimer disease. Arch. Neurol. 2009, 66, 343–348. [Google Scholar] [CrossRef] [Green Version]
- Kivipelto, M.; Helkala, E.L.; Laakso, M.P.; Hänninen, T.; Hallikainen, M.; Alhainen, K.; Soininen, H.; Tuomilehto, J.; Nissinen, A. Midlife vascular risk factors and Alzheimer’s disease in later life: Longitudinal, population-based study. Bmj 2001, 322, 1447–1451. [Google Scholar] [CrossRef] [Green Version]
- Deane, R.; Yan, S.D.; Submamaryan, R.K.; LaRue, B.; Jovanovic, S.; Hogg, E.; Welch, D.; Manness, L.; Lin, C.; YU, J.; et al. RAGE mediates amyloid–β peptide transport across the blood-brain barrier and accumulation in brain. Nat. Med. 2003, 9, 907–913. [Google Scholar] [CrossRef]
- Eikelenboom, P.; Stam, F.C. Immunoglobulins and complement factors in senile plaques: An immunoperoxidase study. Acta Neuropathol. 1982, 57, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Heinonen, O.; Syrjänen, S.; Soininen, H.; Talasniemi, S.; Kaski, M.; Mäntyjärvi, R.; Syrjänen, K.; Riekkinen, P. Circulating immune complexes in sera from patients with Alzheimer’s disease, multi–infarct dementia and Down’s syndrome. Neurosci. Lett. 1993, 149, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Veerhuis, R. Histological and direct evidence for the role of complement in the neuroinflammation of AD. Curr. Alzheimer Res. 2011, 8, 34–58. [Google Scholar] [CrossRef]
- Acharya, N.K.; Nagele, E.P.; Han, M.; Coretti, N.J.; DeMarshall, C.; Kosciuk, M.C.; Boulos, P.A.; Nagele, R.G. Neuronal PAD4 expression and protein citrullination: Possible role in production of autoantibodies associated with neurodegenerative disease. J. Autoimmune. 2012, 38, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Miklossy, J. Emerging roles of pathogens in Alzheimer disease. Expert Rev. Mol. 2011, 13, e30. [Google Scholar] [CrossRef] [Green Version]
- Honjo, K.; Reekum, R.V.; Verhoeff, N.P.L.G. Alzheimer’s disease and infection: Do infectious agents contribute to progression of Alzheimer’s disease? Alzheimer. Dement. 2009, 5, 348–360. [Google Scholar] [CrossRef]
- Sochocka, M.; Zwolinska, K.; Leszek, J. The infectious etiology of Alzheimer’s disease. Curr. Neuropharmacol. 2017, 15, 996–1009. [Google Scholar] [CrossRef] [Green Version]
- Itzhaki, R.F.; Lathe, R.; Balin, B.J.; Ball, M.J.; Bearer, E.L.; Braak, H.; Bullido, M.J.; Carter, C.; Clerici, M.; Cosby, S.L.; et al. Microbes and Alzheimer’s disease. J. Alzheimer’s Dis. JAD 2016, 51, 979. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Davis, P.B.; Kaelber, D.C.; Xu, R. COVID-19 breakthrough infections and hospitalizations among vaccinated patients with dementia in the United States between December 2020 and August 2021. Alzheimers. Dement. 2023, 19, 421–432. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Wang, L.; Davis, P.B.; Volkow, N.D.; Berger, N.A.; Kaelber, D.C.; Xu, R. Association of COVID-19 with new-onset Alzheimer’s disease. J. Alzheimer’s Dis. 2022, 89, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Anand, P.; Singh, B. A review on cholinesterase inhibitors for Alzheimer’s disease. Arch. Pharm. Res. 2013, 36, 375–399. [Google Scholar] [CrossRef] [PubMed]
- Sharma, K. Cholinesterase inhibitors as Alzheimer’s therapeutics. Mol. Med. Rep. 2019, 20, 1479–1487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, A.; Sidhu, J.; Goyal, A.S.P. Alzheimer Disease; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Dooley, M.; Lamb, H.M. Donepezil: A review of its use in Alzheimer’s disease. Drugs Aging 2000, 16, 199–226. [Google Scholar] [CrossRef] [PubMed]
- Magnuson, T.M.; Keller, B.K.; Burke, W.J. Extrapyramidal side effects in a patient treated with risperidone plus donepezil. Am. J. Psychiatry 1998, 155, 1458–1459. [Google Scholar] [CrossRef]
- Wilcock, G.; Howe, I.; Coles, H.; Lilienfeld, S.; Truyen, L.; Zhu, Y.; Bullock, R.; Kershaw, P. A long–term comparison of galantamine and donepezil in the treatment of Alzheimer’s disease. Drugs Aging 2003, 20, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Hansen, R.A.; Gartlehner, G.; Webb, A.P.; Morgan, L.C.; Moore, C.G.; Jonas, D.E. Efficacy and safety of donepezil, galantamine, and rivastigmine for the treatment of Alzheimer’s disease: A systematic review and meta-analysis. Clin. Interv. Aging 2008, 3, 211–225. [Google Scholar]
- Annicchiarico, R.; Federici, A.; Pettenati, C.; Caltagirone, C. Rivastigmine in Alzheimer’s disease: Cognitive function and quality of life. Ther. Clin. Risk Manag. 2007, 3, 1113–1123. [Google Scholar]
- Khoury, R.; Rajamanickam, J.; Grossberg, G.T. An update on the safety of current therapies for Alzheimer’s disease: Focus on rivastigmine. Ther. Adv. Drug Saf. 2018, 9, 171–178. [Google Scholar] [CrossRef]
- Danysz, W.; Parsons, C.G. The NMDA receptor antagonist memantine as a symptomatological and neuroprotective treatment for Alzheimer’s disease: Preclinical evidence. Int. J. Geriatr. Psychiatry 2003, 18, S23–S32. [Google Scholar] [CrossRef]
- Malinow, R. New developments on the role of NMDA receptors in Alzheimer’s disease. Curr. Opin. Neurobiol. 2012, 22, 559–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, L.J.; Goa, K.L. Galantamine: A review of its use in Alzheimer’s disease. Drugs 2000, 60, 1095–1122. [Google Scholar] [CrossRef] [PubMed]
- Prvulovic, D.; Hampel, H.; Pantel, J. Galantamine for Alzheimer’s disease. Expert. Opin. Drug Metab. Toxicol. 2010, 6, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Folch, J.; Busquets, O.; Ettcheto, M.; Sánchez-López, E.; Castro-Torres, R.D.; Verdaguer, E.; Garcia, M.L.; Olloquequi, J.; Casadesús, G.; Beas-Zarate, C.; et al. Memantine for the treatment of dementia: A review on its current and future applications. J. Alzheimer’s D 2018, 62, 1223–1240. [Google Scholar] [CrossRef] [Green Version]
- Rogawski, M.A.; Wenk, G.L. The neuropharmacological basis for the use of memantine in the treatment of Alzheimer’s disease. CNS Drug Rev. 2003, 9, 275–308. [Google Scholar] [CrossRef] [PubMed]
- Filho, J.M.B.; Medeiros, K.C.P.; de Fátima, F.M.; Batista, L.M.; Athayde-Filho, P.F.; Silva, M.S.; da Cunha, E.V.L.; Almeida, J.R.G.S.; Quintans-Júnior, L.J. Natural products inhibitors of the enzyme acetylcholinesterase. Rev. Bras. Farmacogn. 2006, 16, 258–285. [Google Scholar] [CrossRef] [Green Version]
- Rahman, K. Studies on free radicals, antioxidants, and co–factors. Clin. Interv. Aging 2007, 2, 219–236. [Google Scholar]
- Gauthier, S.; Leuzy, A.; Racine, E.; Rosa-Neto, P. Diagnosis and management of Alzheimer’s disease: Past, present and future ethical issues. Prog. Neurobiol. 2013, 110, 102–113. [Google Scholar] [CrossRef]
- Dai, Q.; Borenstein, A.R.; Wu, Y.; Jackson, J.C.; Larson, E.B. Fruit and vegetable juices and Alzheimer’s disease: The Kame Project. Am. J. Med. 2006, 119, 751–759. [Google Scholar] [CrossRef] [Green Version]
- Upaganlawar, A.B.; Wankhede, N.L.; Kale, M.B.; Umare, M.D.; Sehgal, A.; Singh, S.; Bhatia, S.; Al-Harrasi, A.; Najda, A.; Nurzyńska-Wierdak, R.; et al. Interweaving epilepsy and neurodegeneration: Vitamin E as a treatment approach. Biomed. Pharmacother. 2021, 143, 112146. [Google Scholar] [CrossRef]
- Sehgal, N.; Gupta, A.; Valli, R.K.; Joshi, S.D.; Mills, J.T.; Hamel, E.; Khanna, P.; Jain, S.C.; Thakur, S.S.; Ravindranath, V. Withania somnifera reverses Alzheimer’s disease pathology by enhancing low–density lipoprotein receptor-related protein in liver. Proc. Natl. Acad. Sci. USA 2012, 109, 3510–3515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choudhary, M.I.; Nawaz, S.A.; Lodhi, M.A.; Ghayur, M.N.; Jalil, S.; Riaz, N.; Yousuf, S.; Malik, A.; Gilani, A.H. Withanolides, a new class of natural cholinesterase inhibitors with calcium antagonistic properties. Biochem. Biophys. Res. Commun. 2005, 334, 276–287. [Google Scholar] [CrossRef] [PubMed]
- Pase, M.P.; Kean, J.; Sarris, J.; Neale, C.; Scholey, A.B. Con Stough. The cognitive–enhancing effects of Bacopa monnieri: A systematic review of randomized, controlled human clinical trials. J. Altern. Complement. Med. 2012, 18, 647–652. [Google Scholar] [CrossRef]
- Mahalanobish, S.; Ghosh, N.; Sil, P.C. Panax quinquefolium (American Ginseng) and Physostigma venenosum (Calabar Bean). In Herbs, Shrubs, and Trees of Potential Medicinal Benefits; CRC Press: Boca Raton, FL, USA, 2022. [Google Scholar]
- Gulkari, V.D.; Maske, D.K. Role of herbal drugs in the prevention and treatment of alzheimer’s disease. World J. Pharm. Res. 2020, 9, 1042–1047. [Google Scholar]
- Pereira, P.; De Oliveira, P.A.; Ardenghi, P.; Rotta, L.; Henriques, J.A.P.; Picada, J.N. Neuropharmacological analysis of caffeic acid in rats. Basic Clin. Pharmacol. Toxicol. 2006, 99, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Baluchnejadmojarad, T.; Roghani, M.; Mafakheri, M. Neuroprotective effect of silymarin in 6–hydroxydopamine hemi–parkinsonian rat: Involvement of estrogen receptors and oxidative stress. Neurosci. Lett. 2010, 480, 206–210. [Google Scholar] [CrossRef]
- Rao, R.V.; Descamps, O.; John, V.; Bredesen, D.E. Ayurvedic medicinal plants for Alzheimer’s disease: A review. Alzheimer’s Res. Ther. 2012, 4, 1–9. [Google Scholar] [CrossRef]
- Fernandez-Panchon, M.S.; Villano, D.; Villano Troncoso, A.M.; Garcia-Parrilla, M.C. Antioxidant activity of phenolic compounds: From in vitro results to in vivo evidence. Crit. Rev. Food Sci. Nutr. 2008, 48, 649–671. [Google Scholar] [CrossRef]
- Zheng, Y.; Wang, C.Y.; Wang, S.Y.; Zheng, W. Effect of high-oxygen atmospheres on blueberry phenolics, anthocyanins, and antioxidant capacity. J. Agric. Food Chem. 2003, 51, 7162–7169. [Google Scholar] [CrossRef]
- Ferlemi, A.V.; Katsikoudi, A.; Kontogianni, V.G.; Kellici, T.F.; Iatrou, G.; Lamari, F.N.; Tzakos, A.G.; Margarity, M. Rosemary tea consumption results to anxiolytic–and anti–depressant–like behavior of adult male mice and inhibits all cerebral area and liver cholinesterase activity; phytochemical investigation and in silico studies. Chem. Biol. Interact. 2015, 237, 47–57. [Google Scholar] [CrossRef]
- Heinrich, M.; Teoh, H.L. Galanthamine from snowdrop-the development of a modern drug against Alzheimer’s disease from local Caucasian knowledge. J. Ethnopharmacol. 2004, 92, 147–162. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.; Palanivelu, K. The effect of curcumin (turmeric) on Alzheimer’s disease: An overview. Ann. Indian Acad. Neurol. 2008, 11, 13. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.; Gilani, A.H. Therapeutic potential of turmeric in Alzheimer’s disease: Curcumin or curcuminoids? Phytother Res. 2014, 28, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Brenn, A.; Grube, M.; Jedlitschky, G.; Fischer, A.; Strohmeier, B.; Eiden, M.; Keller, M.; Groschup, M.H.; Vogelgesang, S. St. John’s Wort Reduces Beta-Amyloid Accumulation in a Double Transgenic Alzheimer’s Disease Mouse Model-Role of P-Glycoprotein. Brain Pathol. 2014, 24, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Dinamarca, M.C.; Cerpa, W.; Garrido, J.; Hancke, J.L.; Inestrosa, N.C. Hyperforin prevents β–amyloid neurotoxicity and spatial memory impairments by disaggregation of Alzheimer’s amyloid–β–deposits. Mol. Psychiatry 2006, 11, 1032–1048. [Google Scholar] [CrossRef]
- Yusuf, M.; Khan, M.; Khan, R.A.; Ahmed, B. Preparation, characterization, in vivo and biochemical evaluation of brain targeted piperine solid lipid nanoparticles in an experimentally induced Alzheimer’s disease model. J. Drug Target. 2013, 21, 300–311. [Google Scholar] [CrossRef]
- Gupta, V.B.; Indi, S.S.; Rao, K.S.J. Garlic extract exhibits antiamyloidogenic activity on amyloid-beta fibrillogenesis: Relevance to Alzheimer’s disease. Phytother. Res. 2009, 23, 111–115. [Google Scholar] [CrossRef]
- Chauhan, N.B.; Sandoval, J. Amelioration of early cognitive deficits by aged garlic extract in Alzheimer’s transgenic mice. Phytother Res. 2007, 21, 629–640. [Google Scholar] [CrossRef]
- Fehske, C.J.; Leuner, K.; Müller, W.E. Ginkgo biloba extract (EGb761®) influences monoaminergic neurotransmission via inhibition of NE uptake, but not MAO activity after chronic treatment. Pharmacol. Res. 2009, 60, 68–73. [Google Scholar] [CrossRef]
- DeFeudis, F.V.; Drieu, K. Stress-alleviating” and “vigilance-enhancing” actions of Ginkgo biloba extract (EGb 761). Drug Dev. Res. 2004, 62, 1–25. [Google Scholar] [CrossRef]
- Cioanca, O.; Hritcu, L.; Mihasan, M.; Hancianu, M. Cognitive-enhancing and antioxidant activities of inhaled coriander volatile oil in amyloid β (1–42) rat model of Alzheimer’s disease. Physiol. Behav. 2013, 120, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Mani, V.; Parle, M. Memory–enhancing activity of Coriandrum sativum in rats. Pharmacologyonline 2009, 2, 827–839. [Google Scholar]
- Choudhary, S.; Kumar, P.; Malik, J. Plants and phytochemicals for Huntington’s disease. Pharmacogn. Rev. 2013, 7, 81. [Google Scholar]
- Remington, R.; Chan, A.; Lepore, A.; Kotlya, E.; Shea, T.B. Apple juice improved behavioral but not cognitive symptoms in moderate–to–late–stage Alzheimer’s disease in an open–label pilot study. Am. J. Alzheimers Dis. Other Demen. 2010, 25, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Jung, S.W.; Kim, S.Y.; Cho, I.H.; Kim, H.C.; Rhim, H.; Kim, M.; Nah, S. Panax ginseng as an adjuvant treatment for Alzheimer’s disease. J. Ginseng Res. 2018, 42, 401–411. [Google Scholar] [CrossRef]
- Chen, F.; Eckman, E.A.; Eckman, C.B. Reductions in levels of the Alzheimer’s amyloid beta peptide after oral administration of ginsenosides. FASEB J. 2006, 20, 1269–1271. [Google Scholar] [CrossRef]
- Xia, C.L.; Tang, G.H.; Guo, Y.Q.; Xu, Y.K.; Huang, Z.S.; Yin, S. Mulberry Diels–Alder–type adducts from Morus alba as multi–targeted agents for Alzheimer’s disease. Phytochemistry 2019, 157, 82–91. [Google Scholar] [CrossRef]
- Dhanasekaran, M.; Holcomb, L.A.; Hitt, A.R.; Tharakan, B.; Porter, J.W.; Young, K.A.; Manyam, B.V. Centella asiatica extract selectively decreases amyloid β levels in hippocampus of alzheimer’s disease animal model. Phytother. Res. 2009, 23, 14–19. [Google Scholar] [CrossRef]
- Jia, H.; Jiang, Y.; Ruan, Y.; Zhang, Y.; Ma, X.; Zhang, J.; Beyreuther, K.; Tu, P.; Zhang, D. Tenuigenin treatment decreases secretion of the Alzheimer’s disease amyloid β–protein in cultured cells. Neurosci. Lett. 2004, 367, 123–128. [Google Scholar] [CrossRef]
- Park, C.H.; Choi, S.H.; Koo, J.W.; Seo, J.H.; Kim, H.S.; Jeong, S.J.; Suh, Y.H. Novel cognitive improving and neuroprotective activities of Polygala tenuifolia Willdenow extract, BT-11. J. Neurosci. Res. 2002, 70, 484–492. [Google Scholar] [CrossRef]
- Elameen, A.; Dragland, S.; Klemsdal, S.S. Bioactive compounds produced by clones of Rhodiola rosea maintained in the Norwegian germplasm collection. Pharmazie 2010, 65, 618–623. [Google Scholar] [PubMed]
- Qu, Z.Q.; Zhou, Y.; Zeng, Y.S.; Li, Y.; Chung, P. Pretreatment with Rhodiola rosea extract reduces cognitive impairment induced by intracerebroventricular streptozotocin in rats: Implication of anti–oxidative and neuroprotective effects. Biomed. Environ. Sci. 2009, 22, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, D.O.; Scholey, A.B.; Tildesley, N.T.J.; Perry, E.K.; Wesnes, K.A. Modulation of mood and cognitive performance following acute administration of Melissa officinalis (lemon balm). Pharmacol. Biochem. Behav. 2002, 72, 953–964. [Google Scholar] [CrossRef] [PubMed]
- Nyakas, C.; Klara, F.; Robert, S.; Keijser, J.N.; Luiten, P.G.M.; Szombathelyi, Z.; Tihanyi, K. Neuroprotective effects of vinpocetine and its major metabolite cis-apovincaminic acid on NMDA-induced neurotoxicity in a rat entorhinal cortex lesion model. CNS Neuros. Ther. 2009, 15, 89–99. [Google Scholar] [CrossRef]
- Rezai-Zadeh, K.; Arendash, G.W.; Hou, H.; Fernandez, F.; Jensen, M.; Runfeldt, M.; Shytle, R.D.; Tan, J. Green tea epigallocatechin–3–gallate (EGCG) reduces β–amyloid mediated cognitive impairment and modulates tau pathology in Alzheimer transgenic mice. Brain Res. 2008, 1214, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Biasibetti, R.; Tramontina, A.C.; Costa, A.P.; Dutra, M.F.; Quincozes-Santos, A.; Patrícia, N.; Bernardi, C.L.; Wartchow, K.M.; Lunardi, P.S.; Gonçalves, C.A. Green tea (−) epigallocatechin–3–gallate reverses oxidative stress and reduces acetylcholinesterase activity in a streptozotocin–induced model of dementia. Behav. Brain Res. 2013, 236, 186–193. [Google Scholar] [CrossRef]
- Sun, A.Y.; Wang, Q.; Simonyi, A.; Sun, G.Y. Botanical phenolics and brain health. Neuromol. Med. 2008, 10, 259–274. [Google Scholar] [CrossRef] [Green Version]
- Eubanks, L.M.; Rogers, C.J.; Beuscher IV, A.E.; Koob, G.F.; Olson, A.J.; Dickerson, T.J.; Janda, K.D. A molecular link between the active component of marijuana and Alzheimer’s disease pathology. Mol. Pharm. 2006, 3, 773–777. [Google Scholar] [CrossRef] [Green Version]
- Bazoti, F.N.; Bergquist, J.; Markides, K.E.; Tsarbopoulos, A. Noncovalent interaction between amyloid–β–peptide (1–40) and oleuropein studied by electrospray ionization mass spectrometry. J. Am. Soc. Mass Spectrom. 2006, 17, 568–575. [Google Scholar] [CrossRef] [Green Version]
- Singhal, A.K.; Naithani Vijay, N.; Bangar, O.P. Medicinal plants with a potential to treat Alzheimer and associated symptoms. Int. J. Nutr. Pharmacol. Neurol. Dis. 2012, 2, 84. [Google Scholar] [CrossRef]
- Ma, X.; Gang, D.R. In vitro production of huperzine A, a promising drug candidate for Alzheimer’s disease. Phytochemistry 2008, 69, 2022–2028. [Google Scholar] [CrossRef] [PubMed]
- Hartman, R.E.; Shah, A.; Fagan, A.M.; Schwetye, K.E.; Parsadanian, M.; Schulman, R.N.; Finn, M.B.; Holtzman, D.M. Pomegranate juice decreases amyloid load and improves behavior in a mouse model of Alzheimer’s disease. Neurobiol. Dis. 2006, 24, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Kwak, H.M.; Jeon, S.Y.; Sohng, B.H.; Kim, J.G.; Lee, J.M.; Lee, K.B.; Jeong, H.H.; Hur, J.M.; Kang, Y.H.; Song, K.S. β–Secretase (BACE1) inhibitors from pomegranate (Punica granatum) husk. Arch. Pharm. Res. 2005, 28, 1328–1332. [Google Scholar] [CrossRef] [PubMed]
- da Silva, A.L.; Piato, Â.L.; Ferreira, J.G.; Martins, B.S.; Nunes, D.S.; Elisabetsky, E. Promnesic effects of Ptychopetalum olacoides in aversive and non–aversive learning paradigms. J. Ethnopharmacol. 2007, 109, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Figueiró, M.; Ilha, J.; Linck, V.M.; Herrmann, A.P.; Nardin, P.; Menezes, C.B.; Achaval, M.; Gonçalves, C.A.; Porciúncula, L.O.; Nunes, D.S.; et al. The Amazonian herbal Marapuama attenuates cognitive impairment and neuroglial degeneration in a mouse Alzheimer model. Phytomedicine 2011, 18, 327–333. [Google Scholar] [CrossRef]
- Arantes, S.; Piçarra, A.; Candeias, F.; Teixeira, D.; Caldeira, A.T.; Martins, M.R. Antioxidant activity and cholinesterase inhibition studies of four flavouring herbs from Alentejo. Nat. Prod. Res. 2017, 31, 2183–2187. [Google Scholar] [CrossRef] [Green Version]
- Essa, M.M.; Vijayan, R.K.; Castellano-Gonzalez, G.; Memon, M.A.; Braidy, N.; Guillemin, G.J. Neuroprotective effect of natural products against Alzheimer’s disease. Neurochem. Res. 2012, 37, 1829–1842. [Google Scholar] [CrossRef]
- Akhondzadeh, S.; Sabet, M.S.; Harirchian, M.H.; Togha, M.; Cheraghmakani, H.; Razeghi, S.; Hejazi, S.S.; Yousefi, M.H.; Alimardani, R.; Jamshidi, A.; et al. A 22–week, multicenter, randomized, double–blind controlled trial of Crocus sativus in the treatment of mild–to–moderate Alzheimer’s disease. Psychopharmacology 2010, 207, 637–643. [Google Scholar] [CrossRef]
- Perry, N.S.L.; Bollen, C.; Perry, E.K.; Ballard, C. Salvia for dementia therapy: Review of pharmacological activity and pilot tolerability clinical trial. Pharmacol. Biochem. Behav. 2003, 75, 651–659. [Google Scholar] [CrossRef]
- de Oliveira, T.S.; Thomaz, D.V.; Neri, H.F.S.; Cerqueira, L.B.; Garcia, L.F.; Gil, H.P.V.; Pontarolo, R.; Campos, F.R.; Costa, E.A.; Santos, F.C.A.D.; et al. Neuroprotective effect of Caryocar brasiliense Camb. leaves are associated with anticholinesterase and antioxidant properties. Oxid. Med. Cell. Longev. 2018, 2018, 9842908. [Google Scholar] [CrossRef] [Green Version]
- Fernando, W.M.A.D.B.; Martins, I.J.; Goozee, K.G.; Brennan, C.S.; Jayasena, V.; Martins, R.N. The role of dietary coconut for the prevention and treatment of Alzheimer’s disease: Potential mechanisms of action. Br. J. Nutr. 2015, 114, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.L.; Chen, M.F.; Li, T.C.; Li, S.C.; Tang, N.Y.; Hsieh, C.T.; Pon, C.Z.; Lin, J.G. Anticonvulsant effect of Uncaria rhynchophylla (Miq) Jack. in rats with kainic acid–induced epileptic seizure. Am. J. Chin. Med. 1999, 27, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Parihar, M.S.; Chaudhary, M.; Shetty, R.; Hemnani, T. Susceptibility of hippocampus and cerebral cortex to oxidative damage in streptozotocin treated mice: Prevention by extracts of Withania somnifera and Aloe vera. J. Clin. Neurosci. 2004, 11, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; He, X.; Han, W.; Chen, X.; Liu, P.; Zhao, X.; Wang, X.; Zhang, L.; Wu, S.; Zheng, X. Genus Tetradium L.: A comprehensive review on traditional uses, phytochemistry, and pharmacological activities. J Ethnopharmacol 2019, 231, 337–354. [Google Scholar] [CrossRef] [PubMed]
- Ekong, M.B.; Ekpo, M.M.; Akpanyung, E.O.; Nwaokonko, D.U. Neuroprotective effect of Moringa oleifera leaf extract on aluminium–induced temporal cortical degeneration. Metab. Brain Dis. 2017, 32, 1437–1447. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, N.; Wang, K.C.; Wegiel, J.; Malik, M.N. Walnut extract inhibits the fibrillization of amyloid beta–protein, and also defibrillizes its preformed fibrils. Curr. Alzheimer Res. 2004, 1, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Muthaiyah, B.; Essa, M.M.; Chauhan, V.; Chauhan, A. Protective effects of walnut extract against amyloid beta peptide–induced cell death and oxidative stress in PC12 cells. Neurochem. Res. 2011, 36, 2096–2103. [Google Scholar] [CrossRef] [Green Version]
- George, R.C.; Lew, J.; Graves, D.J. Interaction of cinnamaldehyde and epicatechin with tau: Implications of beneficial effects in modulating Alzheimer’s disease pathogenesis. J. Alzheimer’s Dis. 2013, 36, 21–40. [Google Scholar] [CrossRef]
- Uddin, M.S.; Mamun, A.A.; Hossain, M.S.; Ashaduzzaman, M.; Noor, M.A.A.N.; Hossain, M.S.; Uddin, M.J.; Sarker, J.; Asaduzzaman, M. Neuroprotective effect of Phyllanthus acidus L. on learning and memory impairment in scopolamine–induced animal model of dementia and oxidative stress: Natural wonder for regulating the development and progression of Alzheimer’s disease. Adv. Alzheimer’s Dis. 2016, 5, 53–72. [Google Scholar] [CrossRef] [Green Version]
- Akram, M.; Nawaz, A. Effects of medicinal plants on Alzheimer’s disease and memory deficits. Neural Regen Res. 2017, 12, 660. [Google Scholar] [CrossRef]
- Rasool, I.F.; Aziz, A.; Khalid, W.; Koraqi, H.; Siddiqui, S.A.; Al-Farga, A.; Lai, W.F.; Ali, A. Industrial Application and Health Prospective of Fig (Ficus carica) By–Products. Molecules 2023, 28, 960. [Google Scholar] [CrossRef] [PubMed]
- Saxena, D.; Sharma, U.; Gupta, S.; Mahajan, S. Pumpkin seeds as a power house of nutrition: A Review. Indian J. Nutr. Diet. 2022, 59, 379–387. [Google Scholar] [CrossRef]
- Parihar, M.S.; Hemnani, T. Phenolic antioxidants attenuate hippocampal neuronal cell damage against kainic acid induced excitotoxicity. J. Biosci. 2003, 28, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Sethiya, N.K.; Nahata, A.; Mishra, S.H.M.; Dixit, V.K. An update on Shankhpushpi, a cognition–boosting Ayurvedic medicine. Chin. J. Integr. Med. 2009, 7, 1001–1022. [Google Scholar] [CrossRef]
- Agarwal, P.; Holland, T.M.; Wang, Y.; Bennett, D.A.; Morris, M.C. Association of strawberries and anthocyanidin intake with Alzheimer’s dementia risk. Nutrients 2019, 11, 3060. [Google Scholar] [CrossRef] [Green Version]
- Kaur, N.; Sarkar, B.; Gill, I.; Kaur, S.; Mittal, S.; Dhiman, M.; Padala, P.R.; Polo, R.P.; Mantha, A.K. Indian herbs and their therapeutic potential against Alzheimer’s disease and other neurological disorders. In Neuroprotective Effects of Phytochemicals in Neurological Disorders; Wiley Online Library: Hoboken, NJ, USA, 2017; pp. 79–112. [Google Scholar] [CrossRef]
- Ravikumar, C. Therapeutic potential of Brassica oleracea (broccoli)–a review. Int. J. Drug Dev. Res. 2015, 7, 9–10. [Google Scholar]
- Jiraungkoorskul, W. Review of neuro–nutrition used as anti–alzheimer plant, spinach, Spinacia oleracea. Pharmacogn. Rev. 2016, 10, 105–108. [Google Scholar] [CrossRef] [Green Version]
- Subash, S.; Essa, M.M.; Braidy, N.; Awlad-Thani, K.; Vaishnav, R.; Al-Adawi, S.; Al-Asmi, A.; Guillemin, G.J. Diet rich in date palm fruits improves memory, learning and reduces beta amyloid in transgenic mouse model of Alzheimer’s disease. J. Ayurveda Integr. Med. 2015, 6, 111–120. [Google Scholar]
- Yang, Y.; Liang, X.; Jin, P.; Li, N.; Zhang, Q.; Yan, W.; Zhang, H.; Sun, J. Screening and determination for potential acetylcholinesterase inhibitory constituents from ginseng stem–leaf saponins using ultrafiltration (UF)-LC-ESI-MS2. Phytochem. Anal. 2019, 30, 26–33. [Google Scholar] [CrossRef] [Green Version]
- Choi, D.Y.; Lee, Y.J.; Hong, J.T.; Lee, H.J. Antioxidant properties of natural polyphenols and their therapeutic potentials for Alzheimer’s disease. Brain Res. Bull. 2012, 87, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Prachayasittikul, V.; Prachayasittikul, S.; Ruchirawat, S.; Prachayasittikul, V. 8–Hydroxyquinolines: A review of their metal chelating properties and medicinal applications. Drug Des. Devel. Ther. 2013, 7, 1157–1178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moon, J.; Choi, S.H.; Shim, J.Y.; Park, H.J.; Oh, M.J.; Kim, M.; Nah, S.Y. Gintonin administration is safe and potentially beneficial in cognitively impaired elderly. Alzheimer Dis. Assoc. Disord. 2018, 32, 85–87. [Google Scholar] [CrossRef] [PubMed]
- Soumyanath, A.; Zhong, Y.P.; Henson, E.; Wadsworth, T.; Bishop, J.; Gold, B.G.; Quinn, J.F. Centella asiatica extract improves behavioral deficits in a mouse model of Alzheimer’s disease: Investigation of a possible mechanism of action. Int. J. Alzheimers Dis. 2012, 2012, 381974. [Google Scholar]
- Gupta, Y.K.; Kumar, M.H.V.; Srivastava, A.K. Effect of Centella asiatica on pentylenetetrazole–induced kindling, cognition and oxidative stress in rats. Pharmacol. Biochem. Behav. 2003, 74, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Matthews, D.G.; Caruso, M.; Murchison, C.F.; Zhu, J.Y.; Wright, K.M.; Harris, C.J.; Gray, N.E.; Quinn, J.F.; Soumyanath, A. Centella Asiatica Improves Memory and Promotes Antioxidative Signaling in 5XFAD Mice. Antioxidants 2019, 8, 630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barbosa, N.R.; Pittella, F.; Gattaz, F. Centella asiatica water extract inhibits iPLA2 and cPLA2 activities in rat cerebellum. Phytomedicine 2008, 15, 896–900. [Google Scholar] [CrossRef]
- Malík, M.; Tlustoš, P. Nootropic Herbs, Shrubs, and Trees as Potential Cognitive Enhancers. Plants 2023, 12, 1364. [Google Scholar] [CrossRef] [PubMed]
- Kudolo, G.B.; Dorsey, S.; Blodgett, J. Effect of the ingestion of Ginkgo biloba extract on platelet aggregation and urinary prostanoid excretion in healthy and Type 2 diabetic subjects. Thromb. Res. 2002, 108, 151–160. [Google Scholar] [CrossRef]
- Barbalho, S.M.; Direito, R.; Laurindo, L.F.; Marton, L.T.; Guiguer, E.L.; Goulart, R.A.; Tofano, R.J.; Carvalho, A.C.A.; Flato, U.A.P.; Tofano, V.A.C.; et al. Ginkgo biloba in the aging process: A narrative review. Antioxidants 2022, 11, 525. [Google Scholar] [CrossRef]
- Li, D.; Ma, J.; Wei, B.; Gao, S.; Lang, Y.; Wan, X. Effectiveness and safety of ginkgo biloba preparations in the treatment of Alzheimer’s disease: A systematic review and meta-analysis. Front. Aging Neurosci. 2023, 15, 1124710. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Kim, D.S.H.L. Discovery of natural products from Curcuma l onga that protect cells from beta–amyloid insult: A drug discovery effort against Alzheimer’s disease. J. Nat. Prod. 2002, 65, 1227–1231. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Alloza, M.; Borrelli, L.A.; Rozkalne, A.; Hyman, B.T.; Bacskai, B.J. Curcumin labels amyloid pathology in vivo, disrupts existing plaques, and partially restores distorted neurites in an Alzheimer mouse model. J. Neurochem. 2007, 102, 1095–1104. [Google Scholar] [CrossRef]
- Kim, G.Y.; Kim, K.H.; Lee, S.H.; Yoon, M.S.; Lee, H.J.; Moon, D.O.; Lee, C.M.; Ahn, S.C.; Park, Y.C.; Park, Y.M. Curcumin inhibits immunostimulatory function of dendritic cells: MAPKs and translocation of NF–κB as potential targets. J. Immunol. 2005, 174, 8116–8124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadhu, A.; Upadhyay, P.; Agrawal, A.; Ilango, K.; Karmakar, D.; Singh, G.P.I.; Dubey, G.P. Management of cognitive determinants in senile dementia of Alzheimer’s type: Therapeutic potential of a novel polyherbal drug product. Clin. Drug Investig. 2014, 34, 857–869. [Google Scholar] [CrossRef] [PubMed]
- Limpeanchob, N.; Jaipan, S.; Rattanakaruna, S.; Phrompittayarat, W.; Ingkaninan, K. Neuroprotective effect of Bacopa monnieri on beta–amyloid–induced cell death in primary cortical culture. J. Ethnopharmacol. 2008, 120, 112–117. [Google Scholar] [CrossRef]
- Chaudhari, K.S.; Tiwari, N.R.; Tiwari, R.R.; Sharma, R.S. Neurocognitive effect of nootropic drug Brahmi (Bacopa monnieri) in Alzheimer’s disease. Ann. Neurosci. 2017, 24, 111–122. [Google Scholar] [CrossRef] [Green Version]
- Bhattacharya, S.K.; Bhattacharya, A.; Kumar, A.; Ghosal, S. Antioxidant activity of Bacopa monniera in rat frontal cortex, striatum and hippocampus. Phytother. Res. 2000, 14, 174–179. [Google Scholar] [CrossRef]
- Peng, J.; Zheng, T.T.; Li, X.; Liang, Y.; Wang, L.J.; Huang, Y.C.; Xiao, H.T. Plant–derived alkaloids: The promising disease–modifying agents for inflammatory bowel disease. Front. Pharmacol. 2019, 10, 351. [Google Scholar] [CrossRef] [Green Version]
- Morgan, A.; Stevens, J. Does Bacopa monnieri improve memory performance in older persons? Results of a randomized, placebo-controlled, double-blind trial. J. Altern. Complement. Med. 2010, 16, 753–759. [Google Scholar] [CrossRef] [Green Version]
- Mirjalili, M.H.; Moyano, E.; Bonfill, M.; Cusido, R.M.; Palazón, J. Steroidal lactones from Withania somnifera, an ancient plant for novel medicine. Molecules 2009, 14, 2373–2393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, Q.; Zhang, L.; Yu, J.; Wageh, S.; Al-Ghamdi, A.A.; Jaroniec, M. Direct Z–scheme photocatalysts: Principles, synthesis, and applications. Mater. Today 2018, 21, 1042–1063. [Google Scholar] [CrossRef]
- Singh, N.; Bhalla, M.; de Jager, P.; Gilca, M. An overview on ashwagandha: A Rasayana (rejuvenator) of Ayurveda. Afr. J. Tradit. Complement. Altern. Med. 2011, 8, 208–213. [Google Scholar] [CrossRef]
- Saini, D.; Srivastava, M.; Vaid, S.; Kesharwani, V. Therapeutic effects of Withania somnifera: An Overview with Special Focus on Alzheimer’s Disease and Infertility among Youth. Nutraceuticals Funct. Foods Immunomodulators 2023, 331–348. [Google Scholar] [CrossRef]
- Choudhary, D.; Bhattacharyya, S.; Bose, S. Efficacy and Safety of Ashwagandha (Withania somnifera (L.) Dunal) Root Extract in Improving Memory and Cognitive Functions. J. Diet. Suppl. 2017, 14, 599–612. [Google Scholar] [CrossRef] [PubMed]
- Ghadrdoost, B.; Vafaei, A.A.; Rashidy-Pour, A.; Hajisoltani, R.; Bandegi, A.R.; Motamedi, F.; Haghighi, S.; Sameni, H.R.; Pahlvan, S. Protective effects of saffron extract and its active constituent crocin against oxidative stress and spatial learning and memory deficits induced by chronic stress in rats. Eur. J. Pharmacol. 2011, 667, 222–229. [Google Scholar] [CrossRef]
- Ghaffari, S.; Hatami, H.; Dehghan, G. Saffron ethanolic extract attenuates oxidative stress, spatial learning, and memory impairments induced by local injection of ethidium bromide. Res. Pharm. Sci. 2015, 10, 222. [Google Scholar]
- Papandreou, M.A.; Kanakis, C.D.; Polissiou, M.G.; Efthimiopoulos, S.; Cordopatis, P.; Margarity, M.; Lamari, F.N. Inhibitory activity on amyloid–β aggregation and antioxidant properties of Crocus sativus stigmas extract and its crocin constituents. J. Agric. Food Chem. 2006, 54, 8762–8768. [Google Scholar] [CrossRef]
- Oboh, G.; Ademiluyi, A.O.; Akinyemi, A.J. Inhibition of acetylcholinesterase activities and some pro–oxidant induced lipid peroxidation in rat brain by two varieties of ginger (Zingiber officinale). Exp. Toxicol. Pathol. 2012, 64, 315–319. [Google Scholar] [CrossRef]
- Zeng, G.F.; Zhang, Z.Y.; Lu, L.; Xiao, D.Q.; Zong, S.H.; He, J.M. Protective effects of ginger root extract on Alzheimer disease-induced behavioral dysfunction in rats. Rejuvenation Res. 2013, 16, 124–133. [Google Scholar] [CrossRef]
- Na, J.Y.; Song, K.; Lee, J.W.; Kim, S.; Kwon, J. 6-Shogaol has anti-amyloidogenic activity and ameliorates Alzheimer’s disease via CysLT1R-mediated inhibition of cathepsin B. Biochem. Biophys. Res. Commun. 2016, 477, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Machado, D.G.; Cunha, M.P.; Neis, V.B.; Balen, G.O.; Colla, A.R.; Grando, J.; Brocardo, P.S.; Bettio, L.E.B.; Dalmarco, J.B.; Rial, D.; et al. Rosmarinus officinalis L. hydroalcoholic extract, similar to fluoxetine, reverses depressive–like behavior without altering learning deficit in olfactory bulbectomized mice. J. Ethnopharmacol. 2012, 143, 158–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, D.; Lee, B.; Nutter, A.; Song, P.; Dolatabadi, N.; Parker, J.; Sanz-Blasco, S.; Newmeyer, T.; Ambasudhan, R.; McKercher, S.R.; et al. Protection from cyanide-induced brain injury by the Nrf2 transcriptional activator carnosic acid. J. Neurochem. 2015, 133, 898–908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lian, K.C.; Chuang, J.J.; Hsieh, C.W.; Wung, B.S.; Huang, G.D.; Jian, T.Y.; Sun, Y.W. Dual mechanisms of NF–κB inhibition in carnosol–treated endothelial cells. Toxicol. Appl. Pharmacol. 2010, 245, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Foresti, R.; Bains, S.K.; Pitchumony, T.S.; Brás, L.E.C.; Drago, F.; Dubois-Randé, J.L.; Bucolo, C.; Motterlini, R. Small molecule activators of the Nrf2–HO–1 antioxidant axis modulate heme metabolism and inflammation in BV2 microglia cells. Pharmacol. Res. 2013, 76, 132–148. [Google Scholar] [CrossRef] [Green Version]
- Nematolahi, P.; Mehrabani, M.; Karami-Mohajeri, S.; Dabaghzadeh, F. Effects of Rosmarinus officinalis L. on memory performance, anxiety, depression, and sleep quality in university students: A randomized clinical trial. Complement. Ther. Clin. Pract. 2018, 30, 24–28. [Google Scholar] [CrossRef]
- Manickavasagan, A.; Essa, M.M.; Ethirajan, S. (Eds.) Dates: Production, Processing, Food, and Medicinal Values; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Daoud, R.T.E. Studies on Folkloric Medicinal Plants Used by Palestinians in the Qalqilia district. Ph.D. Thesis, An-Najah National University, Nablus, Palestine, 2008. [Google Scholar]
- Pujari, R.R.; Vyawahare, N.S.; Thakurdesai, P.A. Neuroprotective and antioxidant role of Phoenix dactylifera in permanent bilateral common carotid occlusion in rats. J. Acute Dis. 2014, 3, 104–114. [Google Scholar] [CrossRef] [Green Version]
- Subash, S.; Essa, M.M.; Al-Asmi, A.; Al-Adawi, S.; Vaishnav, R.; Guillemin, G.J. Effect of dietary supplementation of dates in Alzheimer’s disease APPsw/2576 transgenic mice on oxidative stress and antioxidant status. Nutr. Neurosci. 2015, 18, 281–288. [Google Scholar] [CrossRef]
- Richard, D.M.; Dawes, M.A.; Mathias, C.W.; Acheson, A.; Hill-Kapturczak, N.; Dougherty, D.M. L–tryptophan: Basic metabolic functions, behavioral research and therapeutic indications. Int. J. Tryptophan Res. 2009, 2, 45–60. [Google Scholar] [CrossRef] [Green Version]
- Zeisel, S.H. Nutritional importance of choline for brain development. J. Am. Coll. Nutr. 2004, 23, 621S–626S. [Google Scholar] [CrossRef]
- Jawaid, T.; Shakya, A.K.; Siddiqui, H.H.; Kamal, M. Evaluation of Cucurbita maxima extract against scopolamine–induced amnesia in rats: Implication of tumour necrosis factor alpha. Z. Naturforsch. C J. Biosci. 2014, 69, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.C.; Su, M.S. Evaluating the anti–neuroinflammatory capacity of raw and steamed garlic as well as five organosulfur compounds. Molecules 2014, 19, 17697–17714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, G.H.; Lee, Y.J.; Choi, D.Y.; Han, S.B.; Jung, J.K.; Hwang, B.Y.; Moon, D.C.; Kim, Y.; Lee, M.K.; Oh, K.-W.; et al. Anti–amyloidogenic effect of thiacremonone through anti–inflamation in vitro and in vivo models. J. Alzheimer’s Dis. 2012, 29, 659–676. [Google Scholar] [CrossRef] [PubMed]
- Ha, G.T.; Wong, R.K.; Zhang, Y. Huperzine a as potential treatment of Alzheimer’s disease: An assessment on chemistry, pharmacology, and clinical studies. Chem. Biodivers. 2011, 8, 1189–1204. [Google Scholar] [CrossRef] [PubMed]
- Gordon, R.K.; Nigam, S.V.; Weitz, J.A.; Dave, J.R.; Doctor, B.P.; Ved, H.S. The NMDA receptor ion channel: A site for binding of Huperzine A. J. Appl. Toxicol. 2001, 21, S47–S51. [Google Scholar] [CrossRef]
- Wang, C.Y.; Zheng, W.; Wang, T.; Xie, J.W.; Wang, S.L.; Zhao, B.L.; Teng, W.P.; Wang, Z.Y. Huperzine A activates Wnt/β–catenin signaling and enhances the nonamyloidogenic pathway in an Alzheimer transgenic mouse model. Neuropsychopharmacology 2011, 36, 1073–1089. [Google Scholar] [CrossRef]
- Smith, A.; Giunta, B.; Bickford, P.C.; Fountain, M.; Tan, J.; Shytle, R.D. Nanolipidic particles improve the bioavailability and α–secretase inducing ability of epigallocatechin–3–gallate (EGCG) for the treatment of Alzheimer’s disease. Int. J. Pharm. 2010, 389, 207–212. [Google Scholar] [CrossRef] [Green Version]
- Cano, A.; Ettcheto, M.; Chang, J.H.; Barroso, E.; Espina, M.; Kühne, B.A.; Barenys, M.; Auladell, C.; Folch, J.; Souto, E.B.; et al. Dual–drug loaded nanoparticles of Epigallocatechin–3–gallate (EGCG)/Ascorbic acid enhance therapeutic efficacy of EGCG in a APPswe/PS1dE9 Alzheimer’s disease mice model. J. Control Release 2019, 301, 62–75. [Google Scholar] [CrossRef]
- Cascella, M.; Bimonte, S.; Muzio, M.R.; Schiavone, V.; Cuomo, A. The efficacy of Epigallocatechin–3–gallate (green tea) in the treatment of Alzheimer’s disease: An overview of pre–clinical studies and translational perspectives in clinical practice. Infect. Agents Cancer 2017, 12, 1–7. [Google Scholar] [CrossRef]
- Li, F.; Gong, Q.; Dong, H.; Shi, J. Resveratrol, a neuroprotective supplement for Alzheimer’s disease. Curr. Pharm. Des. 2012, 18, 27–33. [Google Scholar] [CrossRef]
- Kola, A.; Hecel, A.; Lamponi, S.; Valensin, D. Novel perspective on Alzheimer’s disease treatment: Rosmarinic acid molecular interplay with copper (II) and amyloid β. Life 2020, 10, 118. [Google Scholar] [CrossRef] [PubMed]
- Noguchi-Shinohara, M.; Ono, K.; Hamaguchi, T.; Nagai, T.; Kobayashi, S.; Komatsu, J.; Samuraki-Yokohama, M.; Iwasa, K.; Yokoyama, K.; Nakamura, H.; et al. Safety and efficacy of Melissa officinalis extract containing rosmarinic acid in the prevention of Alzheimer’s disease progression. Sci. Rep. 2020, 10, 18627. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.P.S.N.; Seghal, N.; Padi, S.S.V. Neuroprotective effects of resveratrol against intracerebroventricular colchicine–induced cognitive impairment and oxidative stress in rats. Pharmacol. Res. 2007, 79, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Shekarchi, M.; Hajimehdipoor, H.; Saeidnia, S.; Gohari, A.R.; Hamedani, M.P. Comparative study of rosmarinic acid content in some plants of Labiatae family. Pharmacogn. Mag. 2012, 8, 37–41. [Google Scholar] [PubMed] [Green Version]
- Petersen, M.; Simmonds, M.S.J. Rosmarinic acid. Phytochemistry 2003, 62, 121–125. [Google Scholar] [CrossRef]
- Brodaty, H.; Corey-Bloom, J.; Potocnik, F.C.V.; Truyen, L.; Gold, M.; Damaraju, C.R.V. Galantamine prolonged–release formulation in the treatment of mild to moderate Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 2005, 20, 120–132. [Google Scholar] [CrossRef]
- Hathout, R.M.; El-Ahmady, S.H.; Metwally, A.A. Curcumin or bisdemethoxycurcumin for nose–to–brain treatment of Alzheimer disease? A bio/chemo–informatics case study. Nat. Prod. Res. 2018, 32, 2873–2881. [Google Scholar] [CrossRef]
- Yang, F.; Lim, G.P.; Begum, A.N.; Ubeda, O.J.; Simmons, M.R.; Ambegaokar, S.S.; Chen, P.P.; Kayed, R.; Glabe, C.G.; Frautschy, S.A.; et al. Curcumin inhibits formation of amyloid β oligomers and fibrils, binds plaques, and reduces amyloid in vivo. J. Biol. Chem. 2005, 280, 5892–5901. [Google Scholar] [CrossRef] [Green Version]
- Shytle, R.D.; Bickford, P.C.; Rezai-zadeh, K.; Zeng, H.L.; Tan, J.; Sanberg, P.R.; Sanberg, C.D.; Roschek, B.; Fink, R.C.; Alberte, R.S. Optimized turmeric extracts have potent anti-amyloidogenic effects. Curr. Alzheimer Res. 2009, 6, 564–571. [Google Scholar] [CrossRef]
- Jomova, K.; Valko, M. Importance of iron chelation in free radical-induced oxidative stress and human disease. Curr. Pharm. Des. 2011, 17, 3460–3473. [Google Scholar] [CrossRef]
- Bajda, M.; Guzior, N.; Ignasik, M.; Malawska, B. Multi-target-directed ligands in Alzheimer’s disease treatment. Curr Med Chem. 2011, 18, 4949–4975. [Google Scholar] [CrossRef] [PubMed]
- Cox, K.H.; Pipingas, A.; Scholey, A.B. Investigation of the effects of solid lipid curcumin on cognition and mood in a healthy older population. J. Psychopharmacol. 2015, 29, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.C.; Huang, D.W.; Lo, Y.M.; Tee, Q.Q.; Kuo, P.; Wu, J.S.; Huang, W.C.; Shen, Z.C. Protective Effect of Caffeic Acid against Alzheimer’s Disease Pathogenesis via Modulating Cerebral Insulin Signaling, beta–Amyloid Accumulation, and Synaptic Plasticity in Hyperinsulinemic Rats. J. Agric. Food Chem. 2019, 67, 7684–7693. [Google Scholar] [CrossRef] [PubMed]
- Murata, N.; Murakami, K.; Ozawa, Y.; Kinoshita, N.; Irie, K.; Shirasawa, T.; Shimizu, T. Silymarin attenuated the amyloid β plaque burden and improved behavioral abnormalities in an Alzheimer’s disease mouse model. Biosci. Biotechnol. Biochem. 2010, 74, 2299–2306. [Google Scholar] [CrossRef] [Green Version]
- Yaghmaei, P.; Azarfar, K.; Dezfulian, M.; Ebrahim-Habibi, A. Silymarin effect on amyloid–β plaque accumulation and gene expression of APP in an Alzheimer’s disease rat model. Daru 2014, 22, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Ganguli, M.; Chandra, V.; Kamboh, M.I.; Johnston, J.M.; Dodge, H.H.; Thelma, B.K.; Juyal, R.C.; Pandav, R.; Belle, S.H.; DeKosky, S.T. Apolipoprotein E polymorphism and Alzheimer disease: The Indo–US cross–national dementia study. Arch. Neurol. 2000, 57, 824–830. [Google Scholar] [CrossRef] [Green Version]
- Debbab, A.; Aly, A.H.; Lin, W.H.; Proksch, P. Bioactive compounds from marine bacteria and fungi. Microb. Biotechnol. 2010, 3, 544–563. [Google Scholar] [CrossRef] [Green Version]
- Abida, H.; Ruchaud, S.; Rios, L.; Humeau, A.; Probert, I.; Vargas, C.D.; Bach, S.; Bowler, C. Bioprospecting marine plankton. Mar. Drugs 2013, 11, 4594–4611. [Google Scholar] [CrossRef] [Green Version]
- Silva, M.; Seijas, P.; Otero, P. Exploitation of Marine Molecules to Manage Alzheimer’s Disease. Mar. Drugs 2021, 19, 373. [Google Scholar] [CrossRef]
- Jin, J.O.; Yadav, D.; Madhwani, K.; Puranik, N.; Chavda, V.; Song, M. Seaweeds in the Oncology Arena: Anti-Cancer Potential of Fucoidan as a Drug—A Review. Molecules 2022, 27, 6032. [Google Scholar] [CrossRef]
- Cowan, C.M.; Thai, J.; Krajewski, S.; Reed, J.C.; Nicholson, D.W.; Kaufmann, S.H.; Roskams, J.A. Caspases 3 and 9 send a pro–apoptotic signal from synapse to cell body in olfactory receptor neurons. J. Neurosci. 2001, 21, 7099–7109. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Zhang, Q.; Wang, H.; Cui, Y.; Sun, Z.; Yang, J.; Zheng, Y.; Jia, J.; Yu, F.; Wang, X.; et al. Fucoidan protects against dopaminergic neuron death in vivo and in vitro. Eur. J. Pharmacol. 2009, 617, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.Q.; Jia, Y.J.; Zhang, T.; Zhang, Q.B.; Wang, X.M. Fucoidan protects against lipopolysaccharide-induced rat neuronal damage and inhibits the production of proinflammatory mediators in primary microglia. CNS Neurosci. Ther. 2012, 18, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.H.; Lee, N.; Youn, K.; Jo, M.R.; Kim, H.R.; Lee, D.S.; Ho, C.T.; Jun, M. Dieckol ameliorates Aβ production via PI3K/Akt/GSK–3β regulated APP processing in SweAPP N2a Cell. Mar. Drugs 2021, 19, 152. [Google Scholar] [CrossRef]
- Tsolaki, M. Future strategies of management of Alzheimer’s Disease. The role of homotaurine. Hell. J. Nucl. Med. 2019, 22, 82–94. [Google Scholar] [PubMed]
- Caltagirone, C.; Ferrannini, L.; Marchionni, N.; Nappi, G.; Scapagnini, G.; Trabucchi, M. The potential protective effect of tramiprosate (homotaurine) against Alzheimer’s disease: A review. Aging Clin. Exp. Res. 2012, 24, 580–587. [Google Scholar]
- Jakaria, M.; Azam, S.; Haque, M.E.; Jo, S.H.; Uddin, M.S.; Kim, I.S.; Choi, D.K. Taurine and its analogs in neurological disorders: Focus on therapeutic potential and molecular mechanisms. Redox. Biol. 2019, 24, 101223. [Google Scholar] [CrossRef]
- Otero, P.A.Z.; Alfonso, A.; Vieytes, M.R.; Cabado, A.G.; Vieites, J.M.; Botana, L.M. Effects of environmental regimens on the toxin profile of Alexandrium ostenfeldii. Toxicol. Environ. Chem. 2010, 29, 301–310. [Google Scholar] [CrossRef]
- Alonso, E.; Otero, P.; Vale, C.; Alfonso, A.; Antelo, A.; Giménez-Llort, L.; Chabaud, L.; Guillou, C.; Botana, L.M. Benefit of 13–desmethyl spirolide C treatment in triple transgenic mouse model of Alzheimer disease: Beta–amyloid and neuronal markers improvement. Curr. Alzheimer Res. 2013, 10, 279–289. [Google Scholar] [CrossRef]
- Suganthy, N.; Ramkumar, V.S.; Pugazhendhi, A.; Benelli, G.; Archunan, G. Biogenic synthesis of gold nanoparticles from Terminalia arjuna bark extract: Assessment of safety aspects and neuroprotective potential via antioxidant, anticholinesterase, and antiamyloidogenic effects. Environ. Sci. Pollut. Res. 2018, 25, 10418–10433. [Google Scholar] [CrossRef]


| Plant | Botanical Name | Family | Part Used | Active Compounds | Properties | References |
|---|---|---|---|---|---|---|
| Ashwangdha | Withania somnifera | Solanaceae | Roots | Glycowithanolides (Withaferin A, Withasomniferin A) | It has neuroprotective functions. | [106,107] |
| Brahmi | Bacopa monnieri | Plantaginaceae | Arial parts | Brahmine, bacosides A and B, apigenin, and quercetin | It works as a memory enhancer. | [108] |
| Calabar bean | Physostigma venenosum | Fabaceae | Seeds | physostigmine | It has acetylcholinesterase inhibitor activities. | [109] |
| Coffee | Coffea arabica | Rubiaceae | Seeds | Caffeic acid, chlorogenic acid | It is effective against Alzheimer’s disease. | [110] |
| Milk thistle | Silybum marianum | Asteraceae | Seeds | Silymarin | It acts as a scavenger of free radicals and protects the central nervous system against any injury and memory impairment. | [111] |
| Guggulu | Commiphora wightii | Burseraceae | Bark | Ferulic acid, commiphoric acid, eugenol, and commophorinic acid | It acts as a scavenger of superoxide radicals. | [112] |
| German chamomile | Matricaria recutita | Asteraceae | leaves | apigenin | It helps in stimulating the brain and calms the nerves. | [113] |
| Blueberry | Vaccinium corymbosum | Ericaceae | Fruit | Antioxidants, vitamins C, B, β-carotene, lutein, and zeaxanthin | It has anti-inflammatory and antidiabetic, properties, and also helps in preventing Alzheimer’s disease. | [114,115] |
| Rosemary | Rosmarinus officinalis | Lamiaceae | Leaves | Carnosic acid, carnosol, rosemanol, rosmarinic acid, and α-pinene | It has antioxidant properties and reduces the risk of AD. | [116] |
| Snowdrop | Galanthus nivalis | Amaryllidaceae | Bulbs | Galanthamine, nivalidine, narwedine, and lycorine | It has antioxidant and antiamyloid activities. | [117] |
| Turmeric | Curcuma longa | Zingiberaceae | Rhizome | Curcumin, bisdemethoxycurcumin, eugenol demethoxycurcumin, zingiberene dihydrocurcumin, azulene, D-camphene, caprylic acid, cineol, and turmerone | It has antioxidant properties so it helps in preventing Alzheimer’s disease. | [118,119] |
| St. John Wort | Hypericum perforatum | Hypericaceae | Entire plant | quercetin, Hypericin, rutin quercetin, and isorhamnetin, | It possesses antioxidant and antiamyloid activities. | [120,121] |
| Black pepper | Piper nigrum | Piperaceae | Seeds | piperine | It reduces acetylcholinesterase levels and shows better results in the treatment of Alzheimer’s disease. | [122] |
| Garlic | Allium sativum | Lilliaceae | Cloves | S-allyl-cysteine, S-allyl-mercaptocysteine Biophenols: caffeic acid, and ferulic acid | It shows antiamyloid and antitangle properties. | [123,124] |
| Ginkgo | Ginkgo biloba | Ginkgoaceae | Leaves | Ginkgolides A, B, C, J and M, bilobalide, quercetin, sesquiterpene kaempferol, and isorhamnetin | It has antioxidant properties. It increases the blood flow in the brain and acts as a scavenger of free radicals and shows neuroprotective properties. | [125,126] |
| Coriander | Coriandrum sativum | Apiaceae | Leaves | Camphor, limonene, alpha-pinene, geraniol, petroselinic acid, and linalool | It helps in improving memory and also helps in managing Alzheimer’s disease. | [127,128] |
| Sesame | Sesamum indicum | Pedaliaceae | seeds | Sesaminol, sesamine | It shows neuroprotective properties. | [129] |
| Apple | Malus pumila | Rosaceae | Fruit | Quercetin, catechin, and epicatechin | It improves cognitive functions. | [130] |
| Ginseng | Panax ginseng | Araliaceae | Roots | Ginsenosides, gintonin | It improves the functioning of the central nervous system, and it also shows anti-amyloid activity. | [131,132] |
| Mulberry | Morus alba | Moraceae | Fruit | resveratrol, oxyresveratrol, chlorogenic acid, mulberroside, moracin, and maclurin | It has antioxidant properties and helps in lowering the risk of AD. | [133] |
| Gotu kola | Centella asiatica | Apiaceae | Leaves | Quercetin, myricetin, kaempferol, rutin, and apigenin | It possesses anti-amyloid properties. | [134] |
| Seneca snakeroot | Polygala tenuifolia | Polygalaceae | Roots | Tenuigenin, tenuifolin, and xanthone glycosides | It acts as an acetylcholinesterase and beta-secretase 1 inhibitor. | [135,136] |
| Golden root | Rhodiola rosea | Crassulaceae | Roots | Rosavin, salidroside, rosin, cinnamoyl alcohol, and tyrosol | It has very good antioxidant activity and also acts as a cognitive enhancer. | [137,138] |
| Lemon balm | Melissa officinalis | Lamiaceae | Leaves | Citral, protocatechuic acid, caffeic acid, and rosmarinic acid | It acts as a memory enhancer. | [139] |
| Dwarf periwinkle | Vinca minor | Apocynaceae | Upper parts | Vinpocetine, apovincaminic acid, kaempferol glycosides, hydroxybenzoic acids, and chlorogenic acid | It acts as a memory enhancer and also shows antioxidant properties. | [140] |
| Green tea | Camellia sinensis | Theaceae | Leaves | Gallocatechin, Gallic acid, epigallocatechin, epicatechin, epigallocatechin gallate, and caffeine | It possesses antioxidant and antiamyloid activities. | [141,142] |
| Grapes | Vitis vinifera | Vitaceae | Fruit | Resveratrol, quercetin, and catechins | It has antioxidant and antiamyloid properties and is used in preventing neurodegeneration. | [143] |
| Marijuana | Cannabis sativa | Cannabaceae | Bud and leaves | Tetrahydrocannabinol, cannabidiol | It shows antiamyloid activity. | [144] |
| Olive | Olea europaea | Oleaceae | Fruit, oil, leaves | Oleuropein, tyrosol, hydroxytyrosol, caffeic acid, verbascoside, and rutin | It possesses antioxidant, anti-inflammatory, and antiamyloid properties. | [145] |
| Brazil nut | Bertholettia excelsa | Lecythidaceae | Nut | Lecithin | It increases the level of acetylcholine n AD patients. | [146] |
| firmoss | Huperzia serrata | Lycopodiaceae | Aerial parts | Huperzines | It possesses antiamyloid activity. | [147] |
| Pomegranate | Punica granatum | Punicaceae | Fruit | Ellagic acid, gallagic acid punicalagin, and punicic acid | It possesses antioxidant and antiamyloid activities. | [148,149] |
| Marapuama | Ptychopetalum olacoides | Olacaceae | Roots | Ptychonal, muirapuamine, and theobromine | It possesses antiamnesic, anticholinesterase, and neuroprotective properties. | [150,151] |
| Fennel | Foeniculum vulgare | Apiaceae | Seed | Estragole, limonene, fenchone, and β-myrcene | It shows an inhibitory effect against acetylcholinesterase and butyrlcholinesterase. | [152] |
| Papaya | Carica papaya | Caricaceae | Fruit | Quercetin, β-sitosterol | It possesses radical scavenging activity. | [153] |
| Saffron | Crocus sativus | Iridaceae | Stigma | Crocin, crocetin, picrocrocin, safranin, and safranal, | It possesses antioxidant and antiamyloid activities. | [154] |
| Ginger | Zingiber officinale | Zingiberaceae | Rhizome | Shagol, gingerol, zingerone | It shows antioxidant properties. | [155] |
| Sage | Salvia officinalis | Lamiaceae | Leaves | Rosmarinic acid, thujone, cineol, and camphor | It shows antioxidant properties. It has cognitive-enhancing properties and helps in preventing age-related problems. | [156] |
| Camb | Caryocar brasiliense | Caryocaracea | Leaf | Gallic acid, quinic acid, quercetin, and quercetin 3-o arabinose | It has neuroprotective effects. | [157] |
| Coconut | Cocos nucifera | Arecaceae | Seed | Caproic acid, Caprylic acid, Capric acid, Lauric acid, and Myristic acid | It helps in preventing Alzheimer’s disease. | [158] |
| Gouteng | Uncaria rhynchophylla | Rubiaceae | Stem | Rhynchophylline, isorhynchophylline, and hirsuteine | It shows free radical scavenging activity and also exhibits protection against kainic acid-induced neuronal damage. | [159] |
| Aloe vera | Aloe barbadensis miller | Aloaceae | Juice | Aloin, β-secretase, aloe-emodin | It improves brain functioning. | [160] |
| Wuzhuyu | Tetradium ruticarpum | Rutaceae | Fruit | Evodiamine, rutaecarpine, evocarpine, and quinoline | It increases the blood flow in the brain and also inhibits the effect of acetylcholinesterase. | [161] |
| Moringa | Moring oleifera | Moringaceae | Leaves | Glycoside niazirin, niaziminim A and B, | It maintains the monoamine level in the brain and helps in treating Alzheimer’s disease. | [162] |
| Walnut | Juglans regia | Juglandaceae | Kernel | α-tocopherol, ellagic acid, and juglone | It reduces the risk of Alzheimer’s disease by reducing oxidative stress and it also shows amyloidogenic activity. | [163,164] |
| Cinnamon | Cinnamomum verum | Lauraceae | Extract of bark | Cinnamaldehyde, eugenol, and trans cinnamaldehyde | It promotes the disassembly of tau filaments and also shows anti-inflammatory activity. | [165] |
| Tahitian gooseberry | Phyllanthus acidus | Phyllanthaceae | Fruit | Terpine | It lowers oxidative stress, decreases lipid peroxidation, and helps in increasing the level of antioxidant enzymes in the brain. | [166] |
| Fig | Ficus carica | Moraceae | Fruit | Quercetin, C-Sitosterol | It has antioxidant activity, exhibits memory-enhancing effects and better learning abilities. | [167] |
| Pumpkin | Cucurbita maxima | Cucurbitaceae | seeds | Ferulic acid, caffeic acid, and coumaric acid | It has antioxidant properties and helps in relieving stress. | [168] |
| Shankhpushpi | Convolvulus pluricaulis | Convolvulaceae | Whole plant | Flavonol glycosides, anthocyanins, and triterpenoids | It is consumed as a tonic for enhancing memory and it calms the nerves. | [169,170] |
| Strawberry | Fragaria ananassa | Rosaceae | Fruit | Pelargonidin | It has antioxidant properties. | [171] |
| Butterfly pea | Clitoria ternatea | Fabaceae | Root and leaf extract | Myricetin, quercetin | It shows antioxidant properties and AChE inhibitor activities. | [172] |
| Broccoli | Brassica oleracea var. italica | Brassicaceae | Floret | Kaempferol, sulforaphane | It possesses antioxidant activities and reduces cerebral oedema. | [173] |
| Spinach | Spinacia oleracea | Amaranthaceae | Leaves | Ferulic acid, coumaric acid, quercetin, spinacetin, and myricetin, | It reduces the neuronal death and production of ROS. | [174] |
| Date palm | Phoenix dactylifera L. | Arecaceae | Fruit | Cinnamic acid, caffeic acid, protocatechuic, gallic acid, dactylifiric acid, and epicatechin | It has antioxidant properties and helps in enhancing memory | [175] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koul, B.; Farooq, U.; Yadav, D.; Song, M. Phytochemicals: A Promising Alternative for the Prevention of Alzheimer’s Disease. Life 2023, 13, 999. https://doi.org/10.3390/life13040999
Koul B, Farooq U, Yadav D, Song M. Phytochemicals: A Promising Alternative for the Prevention of Alzheimer’s Disease. Life. 2023; 13(4):999. https://doi.org/10.3390/life13040999
Chicago/Turabian StyleKoul, Bhupendra, Usma Farooq, Dhananjay Yadav, and Minseok Song. 2023. "Phytochemicals: A Promising Alternative for the Prevention of Alzheimer’s Disease" Life 13, no. 4: 999. https://doi.org/10.3390/life13040999






