Aerobic Fitness as an Important Moderator Risk Factor for Loneliness in Physically Trained Older People: An Explanatory Case Study Using Machine Learning
Abstract
1. Introduction
2. Materials and Methods
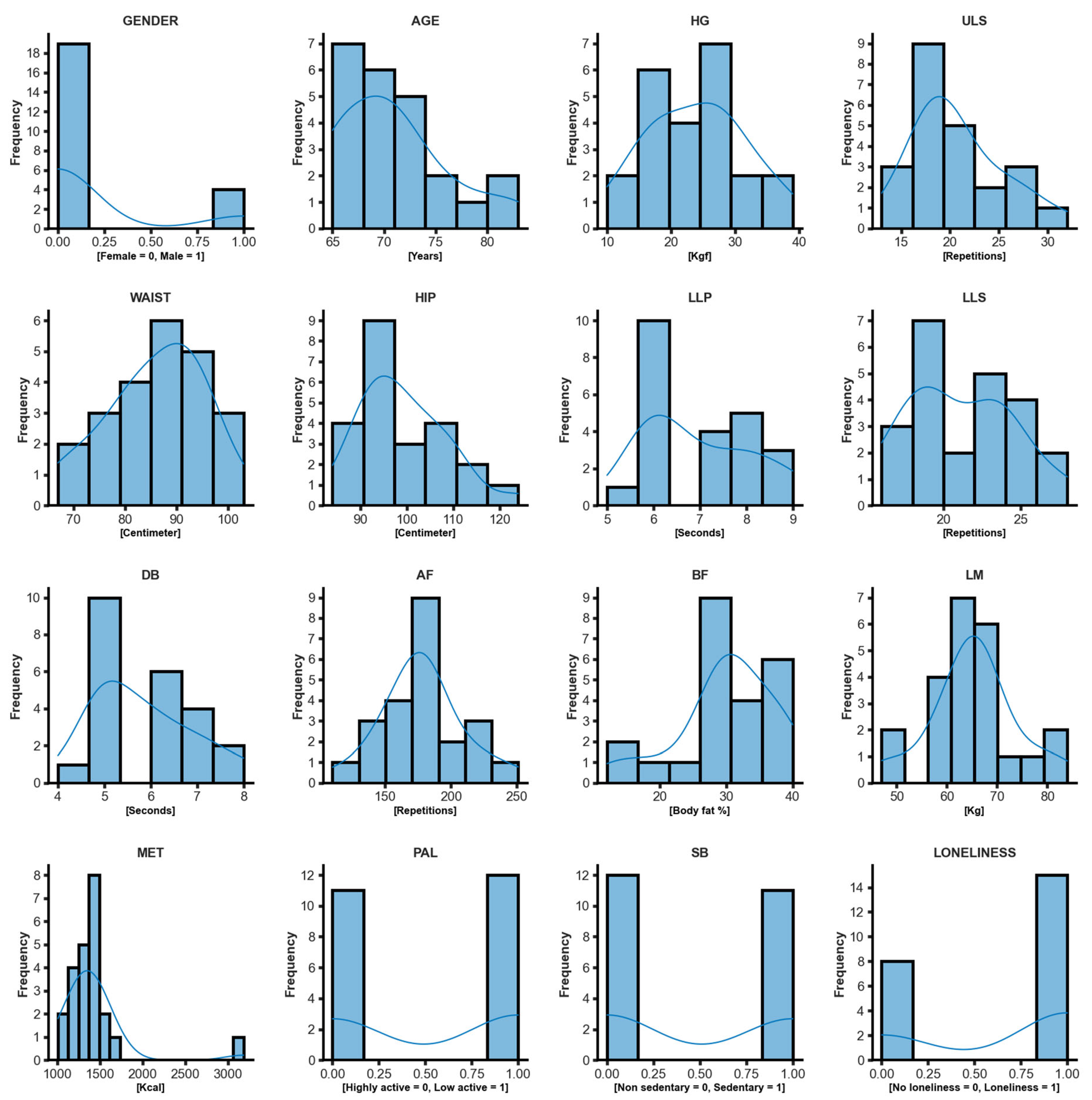
2.1. Dataset
2.2. Ethical Aspects
2.3. Sample Measurements
2.3.1. Body Composition
2.3.2. Sociodemographic Variables
2.3.3. Hand Grip Strength
2.3.4. Upper Limb Strength
2.3.5. Lower Limb Power
2.3.6. Lower Limb Muscle Strength
2.3.7. Dynamic Balance
2.3.8. Aerobic Fitness
2.3.9. Upper Limb Flexibility
2.4. Physical Activity Levels and Sedentary Behavior
Loneliness Feelings Scores
3. Naive-Byes Artificial Intelligence Algorithm Application
- P (Y), the “prior probability”, is the initial degree of belief in Y.
- P (Y|X), the “posterior probability”, is the degree of belief having accounted for X. It is interpreted as “the probability of Y, given that X is the case”.
- The quotient P(X|Y)/P(X) represents the support X provides for Y.
4. Results
5. Discussion
5.1. Strengths and Limitations
5.2. Practical Applications
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rodrigues, F.; Jacinto, M.; Figueiredo, N.; Monteiro, A.M.; Forte, P. Effects of a 24-Week Low-Cost Multicomponent Exercise Program on Health-Related Functional Fitness in the Community-Dwelling Aged and Older Adults. Medicina 2023, 59, 371. [Google Scholar] [CrossRef] [PubMed]
- Azeredo, Z.D.A.S.; Afonso, M.A.N. Loneliness from the Perspective of the Elderly. Rev. Bras. Geriatr. Gerontol. 2016, 19, 313–324. [Google Scholar] [CrossRef]
- Monteiro, S.F.D.S. Mudanças Relacionadas Com a Idade e Bem-Estar Subjetivo: A Influência da Saúde e da Solidão. Master’s Thesis, Universidade do Minho Escola de Psicologia, Braga, Portugal, 2019. [Google Scholar]
- Ribeiro-Gonçalves, J.A.; Costa, P.A.; Leal, I. Loneliness, Ageism, and Mental Health: The Buffering Role of Resilience in Seniors. Int. J. Clin. Health Psychol. 2023, 23, 100339. [Google Scholar] [CrossRef] [PubMed]
- Pocinho, M.; Farate, C.; Dias, C.A. Validação Psicométrica Da Escala UCLA-Loneliness Para Idosos Portugueses. Interações Soc. Novas Mod. 2010, 10, 65–77. [Google Scholar]
- Hawkley, L.C.; Capitanio, J.P. Perceived Social Isolation, Evolutionary Fitness and Health Outcomes: A Lifespan Approach. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2015, 370, 20140114. [Google Scholar] [CrossRef]
- Yang, K.; Victor, C. Age and Loneliness in 25 European Nations. Ageing Soc. 2011, 31, 1368–1388. [Google Scholar] [CrossRef]
- WHO. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- UN. World Population Prospects—Population Division—United Nations. Available online: https://population.un.org/wpp/ (accessed on 19 March 2022).
- Pels, F.; Kleinert, J. Loneliness and Physical Activity: A Systematic Review. Int. Rev. Sport Exerc. Psychol. 2016, 9, 231–260. [Google Scholar] [CrossRef]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour. Available online: https://www.who.int/publications-detail-redirect/9789240015128 (accessed on 19 March 2022).
- WHO. Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 25 March 2023).
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical Activity, Exercise, and Physical Fitness: Definitions and Distinctions for Health-Related Research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- CIH. What Is the Difference between Physical Activity and Exercise? Available online: https://www.cardio.com/blog/what-is-the-difference-between-physical-activity-and-exercise (accessed on 25 March 2023).
- Dasso, N.A. How Is Exercise Different from Physical Activity? A Concept Analysis. Nurs. Forum 2019, 54, 45–52. [Google Scholar] [CrossRef]
- PSU. Exercise vs. Physical Activity; Penn State College of Medicine Research: Hershey, PA, USA, 2023. [Google Scholar]
- Park, W.; Park, H.-Y.; Lim, K.; Park, J. The Role of Habitual Physical Activity on Arterial Stiffness in Elderly Individuals: A Systematic Review and Meta-Analysis. J. Exerc. Nutr. Biochem. 2017, 21, 16–21. [Google Scholar] [CrossRef]
- Morgan, G.S.; Willmott, M.; Ben-Shlomo, Y.; Haase, A.M.; Campbell, R.M. A Life Fulfilled: Positively Influencing Physical Activity in Older Adults—A Systematic Review and Meta-Ethnography. BMC Public Health 2019, 19, 362. [Google Scholar] [CrossRef]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Silva, E.S.; Hallgren, M.; Ponce De Leon, A.; Dunn, A.L.; Deslandes, A.C.; et al. Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef]
- Forte, P.; Monteiro, A.M. The Physical Activity and Exercise as Key Role Topic in Sports Medicine for Old People Quality of Life. Medicina 2022, 58, 797. [Google Scholar] [CrossRef]
- Landi, F.; Calvani, R.; Picca, A.; Tosato, M.; Martone, A.M.; D’Angelo, E.; Serafini, E.; Bernabei, R.; Marzetti, E. Impact of Habitual Physical Activity and Type of Exercise on Physical Performance across Ages in Community-Living People. PLoS ONE 2018, 13, e0191820. [Google Scholar] [CrossRef]
- Yao, L.; Fang, H.; Leng, W.; Li, J.; Chang, J. Effect of Aerobic Exercise on Mental Health in Older Adults: A Meta-Analysis of Randomized Controlled Trials. Front. Psychiatry 2021, 12, 74825. [Google Scholar] [CrossRef]
- Zhidong, C.; Wang, X.; Yin, J.; Song, D.; Chen, Z. Effects of Physical Exercise on Working Memory in Older Adults: A Systematic and Meta-Analytic Review. Eur. Rev. Aging Phys. Act. 2021, 18, 18. [Google Scholar] [CrossRef]
- Basu, K.; Sinha, R.; Ong, A.; Basu, T. Artificial Intelligence: How Is It Changing Medical Sciences and Its Future? Indian J. Dermatol. 2020, 65, 365–370. [Google Scholar] [CrossRef]
- Bianchini, S.; Müller, M.; Pelletier, P. Artificial Intelligence in Science: An Emerging General Method of Invention. Res. Policy 2022, 51, 104604. [Google Scholar] [CrossRef]
- Unpingco, J. Python for Probability, Statistics, and Machine Learning; Springer: Berlin/Heidelberg, Germany, 2016; Volume 1. [Google Scholar]
- Wang, Y.; Carter, B.Z.; Li, Z.; Huang, X. Application of Machine Learning Methods in Clinical Trials for Precision Medicine. JAMIA Open 2022, 5, ooab107. [Google Scholar] [CrossRef]
- Ćosić, K.; Popović, S.; Šarlija, M.; Kesedžić, I.; Jovanovic, T. Artificial Intelligence in Prediction of Mental Health Disorders Induced by the COVID-19 Pandemic among Health Care Workers. Croat. Med. J. 2020, 61, 279–288. [Google Scholar] [CrossRef]
- Tutun, S.; Johnson, M.E.; Ahmed, A.; Albizri, A.; Irgil, S.; Yesilkaya, I.; Ucar, E.N.; Sengun, T.; Harfouche, A. An AI-Based Decision Support System for Predicting Mental Health Disorders. Inf. Syst. Front. 2022, 25, 1261–1276. [Google Scholar] [CrossRef] [PubMed]
- Koutsouleris, N.; Hauser, T.U.; Skvortsova, V.; Choudhury, M.D. From Promise to Practice: Towards the Realisation of AI-Informed Mental Health Care. Lancet Digit. Health 2022, 4, e829–e840. [Google Scholar] [CrossRef] [PubMed]
- Basso, J.C.; Suzuki, W.A. The Effects of Acute Exercise on Mood, Cognition, Neurophysiology, and Neurochemical Pathways: A Review. Brain Plast. 2017, 2, 127–152. [Google Scholar] [CrossRef]
- Borrega-Mouquinho, Y.; Sánchez-Gómez, J.; Fuentes-García, J.P.; Collado-Mateo, D.; Villafaina, S. Effects of High-Intensity Interval Training and Moderate-Intensity Training on Stress, Depression, Anxiety, and Resilience in Healthy Adults During Coronavirus Disease 2019 Confinement: A Randomized Controlled Trial. Front. Psychol. 2021, 12, 64306. [Google Scholar] [CrossRef] [PubMed]
- Lampinen, P.; Heikkinen, R.-L.; Ruoppila, I. Changes in Intensity of Physical Exercise as Predictors of Depressive Symptoms among Older Adults: An Eight-Year Follow-Up. Prev. Med. 2000, 30, 371–380. [Google Scholar] [CrossRef]
- Lee, Y.; Park, K. Does Physical Activity Moderate the Association between Depressive Symptoms and Disability in Older Adults? Int. J. Geriatr. Psychiatry 2008, 23, 249–256. [Google Scholar] [CrossRef]
- Korman, N.; Armour, M.; Chapman, J.; Rosenbaum, S.; Kisely, S.; Suetani, S.; Firth, J.; Siskind, D. High Intensity Interval Training (HIIT) for People with Severe Mental Illness: A Systematic Review & Meta-Analysis of Intervention Studies- Considering Diverse Approaches for Mental and Physical Recovery. Psychiatry Res. 2020, 284, 112601. [Google Scholar] [CrossRef]
- Moyers, S.A.; Hagger, M.S. Physical Activity and Cortisol Regulation: A Meta-Analysis. Biol. Psychol. 2023, 179, 108548. [Google Scholar] [CrossRef]
- Bermejo, J.-L.; Valldecabres, R.; Villarrasa-Sapiña, I.; Monfort-Torres, G.; Marco-Ahulló, A.; Ribeiro Do Couto, B. Increased Cortisol Levels Caused by Acute Resistance Physical Exercise Impair Memory and Learning Ability. PeerJ 2022, 10, e13000. [Google Scholar] [CrossRef]
- Lucertini, F.; Ponzio, E.; Di Palma, M.; Galati, C.; Federici, A.; Barbadoro, P.; D’Errico, M.M.; Prospero, E.; Ambrogini, P.; Cuppini, R.; et al. High Cardiorespiratory Fitness Is Negatively Associated with Daily Cortisol Output in Healthy Aging Men. PLoS ONE 2015, 10, e0141970. [Google Scholar] [CrossRef]
- Kim, J.; Park, G.-R. Chronic Loneliness, Gender, and Trajectories of Change in Hand Grip Strength in Older Adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2023, 78, 649–658. [Google Scholar] [CrossRef]
- Tajika, T.; Kuboi, T.; Oya, N.; Endo, F.; Shitara, H.; Ichinose, T.; Sasaki, T.; Hamano, N.; Chikuda, H. Association between Upper-Extremity Health Condition and Depressive Status in an Elderly General Population. Inquiry 2021, 58, 00469580211059952. [Google Scholar] [CrossRef]
- Borg, G. Escala CR10 de Borg. Escalas de Borg Para a Dor e Esforço Percebido; Manole: São Paulo, Brazil, 2000; pp. 43–47. [Google Scholar]
- Rikli, R.E.; Jones, C.J. Development and Validation of Criterion-Referenced Clinically Relevant Fitness Standards for Maintaining Physical Independence in Later Years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Patterson, R.; McNamara, E.; Tainio, M.; de Sá, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary Behaviour and Risk of All-Cause, Cardiovascular and Cancer Mortality, and Incident Type 2 Diabetes: A Systematic Review and Dose Response Meta-Analysis. Eur. J. Epidemiol. 2018, 33, 811–829. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Alcazar, J.; Losa-Reyna, J.; Rodriguez-Lopez, C.; Acha, A.; Rodríguez-Mañas, L.; Ara, I.; García García, F.; Alegre, L. The Sit-to-Stand Muscle Power Test: An Easy, Inexpensive and Portable Procedure to Assess Muscle Power in Older People. Exp. Gerontol. 2018, 112, 38–43. [Google Scholar] [CrossRef]
- Silva, G.S.; Yang, H.; Collins, J.E.; Losina, E. Validating Fitbit for Evaluation of Physical Activity in Patients with Knee Osteoarthritis: Do Thresholds Matter? ACR Open Rheumatol. 2019, 1, 585–592. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; De Bourdeaudhuij, I.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Lutes, L.D.; et al. How Many Steps/Day Are Enough? For Older Adults and Special Populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef]
- Russell, D.; Peplau, L.A.; Ferguson, M.L. Developing a Measure of Loneliness. J. Personal. Assess. 1978, 42, 290–294. [Google Scholar] [CrossRef]
- Russell, D.; Peplau, L.A.; Cutrona, C.E. The Revised UCLA Loneliness Scale: Concurrent and Discriminant Validity Evidence. J. Personal. Soc. Psychol. 1980, 39, 472. [Google Scholar] [CrossRef]
- Russell, D.W. UCLA Loneliness Scale (Version 3): Reliability, Validity, and Factor Structure. J. Personal. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef] [PubMed]
- Python Welcome to Python.Org. Available online: https://www.python.org/ (accessed on 13 March 2023).
- Wong, T.-T. Performance Evaluation of Classification Algorithms by K-Fold and Leave-One-out Cross Validation. Pattern Recognit. 2015, 48, 2839–2846. [Google Scholar] [CrossRef]
- Haslwanter, T. An Introduction to Statistics with Python, with Applications in the Life Sciences; Springer International Publishing: Cham, Switzerland, 2016. [Google Scholar]
- Chen, H.; Hu, S.; Hua, R.; Zhao, X. Improved Naive Bayes Classification Algorithm for Traffic Risk Management. EURASIP J. Adv. Signal Process. 2021, 2021, 30. [Google Scholar] [CrossRef]
- Langarizadeh, M.; Moghbeli, F. Applying Naive Bayesian Networks to Disease Prediction: A Systematic Review. Acta Inform. Med. 2016, 24, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, H. Can Naive Bayes Classifier Predict Infection in a Close Contact of COVID-19? A Comparative Test for Predictability of the Predictive Model and Healthcare Workers in Japan. J. Infect. Chemother. 2022, 28, 774–779. [Google Scholar] [CrossRef]
- NIA. Social Isolation, Loneliness in Older People Pose Health Risks. Available online: https://www.nia.nih.gov/news/social-isolation-loneliness-older-people-pose-health-risks (accessed on 28 May 2023).
- Musich, S.; Wang, S.S.; Schaeffer, J.A.; Kraemer, S.; Wicker, E.; Yeh, C.S. The Association of Physical Activity with Loneliness, Social Isolation, and Selected Psychological Protective Factors among Older Adults. Geriatr. Nurs. 2022, 47, 87–94. [Google Scholar] [CrossRef]
- Wu, Z.-J.; Wang, Z.-Y.; Gao, H.-E.; Zhou, X.-F.; Li, F.-H. Impact of High-Intensity Interval Training on Cardiorespiratory Fitness, Body Composition, Physical Fitness, and Metabolic Parameters in Older Adults: A Meta-Analysis of Randomized Controlled Trials. Exp. Gerontol. 2021, 150, 111345. [Google Scholar] [CrossRef]
- Dziurkowska, E.; Wesolowski, M. Cortisol as a Biomarker of Mental Disorder Severity. J. Clin. Med. 2021, 10, 5204. [Google Scholar] [CrossRef]
- Montoliu, T.; Hidalgo, V.; Salvador, A. The Relationship between Loneliness and Cognition in Healthy Older Men and Women: The Role of Cortisol. Psychoneuroendocrinology 2019, 107, 270–279. [Google Scholar] [CrossRef]
- Soysal, P.; Hurst, C.; Demurtas, J.; Firth, J.; Howden, R.; Yang, L.; Tully, M.A.; Koyanagi, A.; Ilie, P.C.; López-Sánchez, G.F.; et al. Handgrip Strength and Health Outcomes: Umbrella Review of Systematic Reviews with Meta-Analyses of Observational Studies. J. Sport Health Sci. 2021, 10, 290–295. [Google Scholar] [CrossRef]
- Kwak, Y.; Kim, Y. Mental Health and Handgrip Strength Among Older Adults: A Nationwide Study. Inquiry 2022, 59, 00469580211067481. [Google Scholar] [CrossRef]
- Vingeliene, S.; Hiyoshi, A.; Lentjes, M.; Fall, K.; Montgomery, S. Ageing Accounts for Much of the Association between Decreasing Grip Strength and Subsequent Loneliness: The English Longitudinal Study of Ageing. J. Epidemiol. Community Health 2023, 77, 175–181. [Google Scholar] [CrossRef]
- Torres, J.L.; Vaz, C.T.; Pinheiro, L.C.; Braga, L.S.; Moreira, B.S.; Oliveira, C.; Lima-Costa, M.F. The Relationship between Loneliness and Healthy Aging Indicators in Brazil (ELSI-Brazil) and England (ELSA): Sex Differences. Public Health 2023, 216, 33–38. [Google Scholar] [CrossRef]
- Tavares, J.P.D.A.; de Sá-Couto, P.M.F.; Pedreira, L.C. Predictors of Frailty in Older People Users of Primary Health Care. Rev. Bras. Enferm. 2022, 75 (Suppl. S4), e20201292. [Google Scholar] [CrossRef]
- Vasconcelos Rocha, S.; Souza dos Santos, S.; Carneiro Vasconcelos, L.R.; Alves dos Santos, C. Strength and Ability to Implement the Activities of Daily Living in Elderly Resident in Rural Areas. Colomb. Med. 2016, 47, 167–171. [Google Scholar] [CrossRef]
- Gyasi, R.M.; Peprah, P.; Abass, K.; Pokua Siaw, L.; Dodzi Ami Adjakloe, Y.; Kofi Garsonu, E.; Phillips, D.R. Loneliness and Physical Function Impairment: Perceived Health Status as an Effect Modifier in Community-Dwelling Older Adults in Ghana. Prev. Med. Rep. 2022, 26, 101721. [Google Scholar] [CrossRef]
- Furtado, G.E.; Vaz, C.; Bovolini, A.; Marques, E.; Serra, N.; Costa-Brito, A.R.; Vila-Chã, C. The Impact of Physical Activity Levels and Functional Fitness Status on the Quality of Life Perceived by Older Adults Living in Rural and Urban Areas: The Portuguese Inland Case. Healthcare 2022, 10, 1266. [Google Scholar] [CrossRef]
- Schrempft, S.; Jackowska, M.; Hamer, M.; Steptoe, A. Associations between Social Isolation, Loneliness, and Objective Physical Activity in Older Men and Women. BMC Public Health 2019, 19, 74. [Google Scholar] [CrossRef]
- Rogers, L.Q.; Courneya, K.S.; Oster, R.A.; Anton, P.M.; Robbs, R.S.; Forero, A.; McAuley, E. Physical Activity and Sleep Quality in Breast Cancer Survivors: A Randomized Trial. Med. Sci. Sports Exerc. 2017, 49, 2009–2015. [Google Scholar] [CrossRef]
- Yang, Q.; Tang, Y.; Jennings, G.; Zhao, B.; Zhu, F.; Ma, X. Physical Activity and Subjective Well-Being of Older Adults during COVID-19 Prevention and Control Normalization: Mediating Role of Outdoor Exercise Environment and Regulating Role of Exercise Form. Front. Psychol. 2022, 13, 1014967. [Google Scholar] [CrossRef]


| Variables | M | SD |
|---|---|---|
| Age (years) | 71 | 5 |
| Height (cm) | 158 | 6 |
| Body weight (kg) | 65 | 10 |
| Lean muscle mass (kg) | 5 | 9 |
| Basal metabolism (kcal) | 1427 | 473 |
| HG (kgf) | 24 | 8 |
| AF (step repetitions) | 178 | 31 |
| Demographics | N | % | p-Value |
|---|---|---|---|
| Female sex | 19 | 82% | 0.001 |
| Scholarly level (<9 Years of School) | 8 | 34% | 0.01 |
| Marital status (single or divorced or widow) | 7 | 30% | 0.001 |
| Live alone | 4 | 17% | 0.001 |
| Income (<2 monthly Wages) | 15 | 65% | NS |
| Religion status (religious) | 22 | 96% | 0.001 |
| Smoker | 3 | 13% | 0.001 |
| Drink alcohol | 4 | 17% | 0.001 |
| Sedentary behavior | 11 | 48% | NS |
| Low physical activity levels | 12 | 52% | NS |
| Medical conditions | |||
| Loneliness | 16 | 70% | 0.04 |
| BMI overweight (>25 Kg/M2 for men—26.6 Kg/M2 for women) | 12 | 52% | NS |
| Waist circumference (≥97 cm for men—≥88 cm for women) | 11 | 48% | NS |
| Hypertension | 6 | 26% | 0.001 |
| Diabetes | 5 | 22% | 0.001 |
| Deregulated cholesterol | 11 | 48% | NS |
| Cardiovascular disease | 1 | 4% | 0.001 |
| Stroke | 0 | 0% | 0.001 |
| Column pain | 7 | 30% | 0.001 |
| Respiratory disease | 1 | 4% | 0.001 |
| Arthrosis | 10 | 43% | NS |
| Osteoporosis | 5 | 22% | 0.001 |
| Labyrinthitis | 1 | 4% | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Encarnação, S.; Vaz, P.; Fortunato, Á.; Forte, P.; Vaz, C.; Monteiro, A.M. Aerobic Fitness as an Important Moderator Risk Factor for Loneliness in Physically Trained Older People: An Explanatory Case Study Using Machine Learning. Life 2023, 13, 1374. https://doi.org/10.3390/life13061374
Encarnação S, Vaz P, Fortunato Á, Forte P, Vaz C, Monteiro AM. Aerobic Fitness as an Important Moderator Risk Factor for Loneliness in Physically Trained Older People: An Explanatory Case Study Using Machine Learning. Life. 2023; 13(6):1374. https://doi.org/10.3390/life13061374
Chicago/Turabian StyleEncarnação, Samuel, Paula Vaz, Álvaro Fortunato, Pedro Forte, Cátia Vaz, and António Miguel Monteiro. 2023. "Aerobic Fitness as an Important Moderator Risk Factor for Loneliness in Physically Trained Older People: An Explanatory Case Study Using Machine Learning" Life 13, no. 6: 1374. https://doi.org/10.3390/life13061374
APA StyleEncarnação, S., Vaz, P., Fortunato, Á., Forte, P., Vaz, C., & Monteiro, A. M. (2023). Aerobic Fitness as an Important Moderator Risk Factor for Loneliness in Physically Trained Older People: An Explanatory Case Study Using Machine Learning. Life, 13(6), 1374. https://doi.org/10.3390/life13061374







