Disparities in Female Oncofertility Care in the United States: More Questions Than Answers
Abstract
1. Introduction
2. Overview of Disparities Data
2.1. Racial and Ethnic Disparities
2.2. Socioeconomic Disparities
2.3. Age Disparities
2.4. Parity Disparities
3. Approaches to Bridge the Gap
3.1. Insurance Mandates
3.2. Decision Support
3.3. Access to Information
3.4. Impact of Bias
3.5. Provider Education
3.6. Low-Cost and Expedited Consultation Efforts
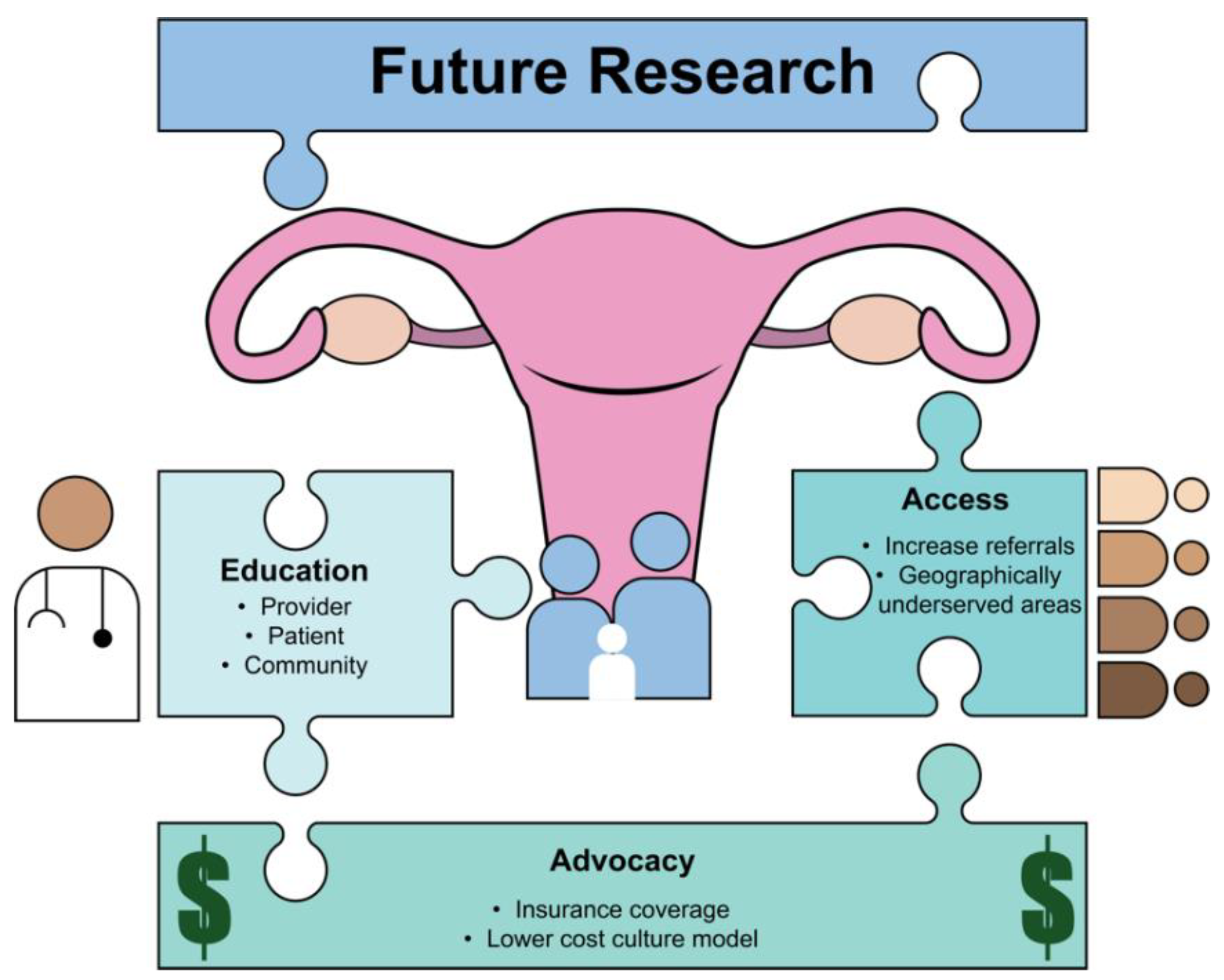
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oktay, K.; Harvey, B.E.; Partridge, A.H.; Quinn, G.P.; Reinecke, J.; Taylor, H.S.; Wallace, W.H.; Wang, E.T.; Loren, A.W. Fertility Preservation in Patients with Cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2018, 36, 1994–2001. [Google Scholar] [CrossRef] [PubMed]
- Bahroudi, Z.; Zarnaghi, M.R.; Izadpanah, M.; Abedelahi, A.; Niknafs, B.; Nasrabadi, H.T.; Seghinsara, A.M. Review of ovarian tissue cryopreservation techniques for fertility preservation. J. Gynecol. Obstet. Hum. Reprod. 2022, 51, 102290. [Google Scholar] [CrossRef]
- Cacciottola, L.; Donnez, J.; Dolmans, M.M. Ovarian tissue and oocyte cryopreservation prior to iatrogenic premature ovarian insufficiency. Best Pract. Res. Clin. Obstet. Gynaecol. 2022, 81, 119–133. [Google Scholar] [CrossRef] [PubMed]
- Keyser, E.A.; Berger-Chen, S.W. ACOG Committee Opinion No. 747: Gynecologic Issues in Children and Adolescent Cancer Patients and Survivors. Obstet. Gynecol. 2018, 132, e67–e77. [Google Scholar] [CrossRef]
- Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: A committee opinion. Fertil. Steril. 2019, 112, 1022–1033. [CrossRef]
- Letourneau, J.M.; Smith, J.F.; Ebbel, E.E.; Craig, A.; Katz, P.P.; Cedars, M.I.; Rosen, M.P. Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer. Cancer 2012, 118, 4579–4588. [Google Scholar] [CrossRef]
- Forman, E.J.; Anders, C.K.; Behera, M.A. A nationwide survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. Fertil. Steril. 2010, 94, 1652–1656. [Google Scholar] [CrossRef]
- Quinn, G.P.; Vadaparampil, S.T.; Lee, J.H.; Jacobsen, P.B.; Bepler, G.; Lancaster, J.; Keefe, D.L.; Albrecht, T.L. Physician referral for fertility preservation in oncology patients: A national study of practice behaviors. J. Clin. Oncol. 2009, 27, 5952–5957. [Google Scholar] [CrossRef]
- Banerjee, R.; Tsiapali, E. Occurrence and recall rates of fertility discussions with young breast cancer patients. Support. Care Cancer 2016, 24, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Missmer, S.A.; Seifer, D.B.; Jain, T. Cultural factors contributing to health care disparities among patients with infertility in Midwestern United States. Fertil. Steril. 2011, 95, 1943–1949. [Google Scholar] [CrossRef]
- Chandra, A.; Copen, C.E.; Stephen, E.H. Infertility and Impaired Fecundity in the United States, 1982–2010: Data from the National Survey of Family Growth; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Atlanta, GA, USA, 2013; pp. 1–18.
- Chandra, A.; Copen, C.E.; Stephen, E.H. Infertility service use in the United States: Data from the National Survey of Family Growth, 1982–2010. Natl. Health Stat. Rep. 2014, 1–21. [Google Scholar]
- Chin, H.B.; Howards, P.P.; Kramer, M.R.; Mertens, A.C.; Spencer, J.B. Racial Disparities in Seeking Care for Help Getting Pregnant. Paediatr. Perinat. Epidemiol. 2015, 29, 416–425. [Google Scholar] [CrossRef]
- Bitler, M.; Schmidt, L. Health disparities and infertility: Impacts of state-level insurance mandates. Fertil. Steril. 2006, 85, 858–865. [Google Scholar] [CrossRef]
- Quinn, G.P.; Vadaparampil, S.T.; Gwede, C.K.; Miree, C.; King, L.M.; Clayton, H.B.; Wilson, C.; Munster, P. Discussion of fertility preservation with newly diagnosed patients: Oncologists’ views. J. Cancer Surviv. 2007, 1, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Flink, D.M.; Sheeder, J.; Kondapalli, L.A. Do Patient Characteristics Decide if Young Adult Cancer Patients Undergo Fertility Preservation? J. Adolesc. Young Adult Oncol. 2017, 6, 223–228. [Google Scholar] [CrossRef]
- Goodman, L.R.; Balthazar, U.; Kim, J.; Mersereau, J.E. Trends of socioeconomic disparities in referral patterns for fertility preservation consultation. Hum. Reprod. 2012, 27, 2076–2081. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Heytens, E.; Moy, F.; Ozkavukcu, S.; Oktay, K. Determinants of access to fertility preservation in women with breast cancer. Fertil. Steril. 2011, 95, 1932–1936. [Google Scholar] [CrossRef] [PubMed]
- Zebrack, B. Information and service needs for young adult cancer survivors. Support. Care Cancer 2009, 17, 349–357. [Google Scholar] [CrossRef]
- Vadaparampil, S.T.; Christie, J.; Quinn, G.P.; Fleming, P.; Stowe, C.; Bower, B.; Pal, T. A pilot study to examine patient awareness and provider discussion of the impact of cancer treatment on fertility in a registry-based sample of African American women with breast cancer. Support. Care Cancer 2012, 20, 2559–2564. [Google Scholar] [CrossRef]
- Salsman, J.M.; Yanez, B.; Smith, K.N.; Beaumont, J.L.; Snyder, M.A.; Barnes, K.; Clayman, M.L. Documentation of Fertility Preservation Discussions for Young Adults with Cancer: Examining Compliance with Treatment Guidelines. J. Natl. Compr. Cancer Netw. 2016, 14, 301–309. [Google Scholar] [CrossRef]
- Quinn, G.P.; Block, R.G.; Clayman, M.L.; Kelvin, J.; Arvey, S.R.; Lee, J.H.; Reinecke, J.; Sehovic, I.; Jacobsen, P.B.; Reed, D.; et al. If you did not document it, it did not happen: Rates of documentation of discussion of infertility risk in adolescent and young adult oncology patients’ medical records. J. Oncol. Pract. 2015, 11, 137–144. [Google Scholar] [CrossRef]
- Meernik, C.; Engel, S.M.; Wardell, A.; Baggett, C.D.; Gupta, P.; Rodriguez-Ormaza, N.; Luke, B.; Baker, V.L.; Wantman, E.; Rauh-Hain, J.A.; et al. Disparities in fertility preservation use among adolescent and young adult women with cancer. J. Cancer Surviv. 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Meernik, C.; Jorgensen, K.; Wu, C.F.; Murphy, C.C.; Baker, V.L.; Brady, P.C.; Nitecki, R.; Nichols, H.B.; Rauh-Hain, J.A. Disparities in the use of assisted reproductive technologies after breast cancer: A population-based study. Breast Cancer Res. Treat. 2023, 198, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Voigt, P.; Persily, J.; Blakemore, J.K.; Licciardi, F.; Thakker, S.; Najari, B. Sociodemographic differences in utilization of fertility services among reproductive age women diagnosed with cancer in the USA. J. Assist. Reprod. Genet. 2022, 39, 963–972. [Google Scholar] [CrossRef]
- Voigt, P.E.; Blakemore, J.K.; McCulloh, D.; Fino, M.E. Equal opportunity for all? An analysis of race and ethnicity in fertility preservation in New York City. J. Assist. Reprod. Genet. 2020, 37, 3095–3102. [Google Scholar] [CrossRef]
- Ruddy, K.J.; Gelber, S.I.; Tamimi, R.M.; Ginsburg, E.S.; Schapira, L.; Come, S.E.; Borges, V.F.; Meyer, M.E.; Partridge, A.H. Prospective study of fertility concerns and preservation strategies in young women with breast cancer. J. Clin. Oncol. 2014, 32, 1151–1156. [Google Scholar] [CrossRef]
- Jorgensen, K.; Meernik, C.; Wu, C.F.; Murphy, C.C.; Baker, V.L.; Jarmon, P.; Brady, P.C.; Nitecki, R.; Nichols, H.B.; Rauh-Hain, J.A. Disparities in Fertility-Sparing Treatment and Use of Assisted Reproductive Technology after a Diagnosis of Cervical, Ovarian, or Endometrial Cancer. Obstet. Gynecol. 2023, 141, 341–353. [Google Scholar] [CrossRef]
- Duffy, C.M.; Allen, S.M.; Clark, M.A. Discussions regarding reproductive health for young women with breast cancer undergoing chemotherapy. J. Clin. Oncol. 2005, 23, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Mobley, E.M.; Ryan, G.L.; Sparks, A.E.; Monga, V.; Terry, W.W. Factors Impacting Fertility Preservation in Adolescents and Young Adults with Cancer: A Retrospective Study. J. Adolesc. Young Adult Oncol. 2020, 9, 208–221. [Google Scholar] [CrossRef]
- Cobo, A.; García-Velasco, J.A.; Coello, A.; Domingo, J.; Pellicer, A.; Remohí, J. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil. Steril. 2016, 105, 755–764.E8. [Google Scholar] [CrossRef]
- Franasiak, J.M.; Forman, E.J.; Hong, K.H.; Werner, M.D.; Upham, K.M.; Treff, N.R.; Scott, R.T., Jr. The nature of aneuploidy with increasing age of the female partner: A review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil. Steril. 2014, 101, 656–663.E1. [Google Scholar] [CrossRef]
- Goldman, R.H.; Racowsky, C.; Farland, L.V.; Munné, S.; Ribustello, L.; Fox, J.H. Predicting the likelihood of live birth for elective oocyte cryopreservation: A counseling tool for physicians and patients. Hum. Reprod. 2017, 32, 853–859. [Google Scholar] [CrossRef] [PubMed]
- Branch, B.; Conway, D. Health Insurance Coverage by Race and Hispanic Origin: 2021; US Department of Commerce, US Census Bureau: Suitland, MD, USA, 2022.
- Peavey, M.; Arian, S.; Gibbons, W.; Lu, K.; Gershenson, D.; Woodard, T. On-Site Fertility Preservation Services for Adolescents and Young Adults in a Comprehensive Cancer Center. J. Adolesc. Young Adult Oncol. 2017, 6, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.; Hughes, J.; Mahmoodi, N.; Smith, E.; Skull, J.; Ledger, W. What factors hinder the decision-making process for women with cancer and contemplating fertility preservation treatment? Hum. Reprod. Update 2017, 23, 433–457. [Google Scholar] [CrossRef] [PubMed]
- Moravek, M.B.; Confino, R.; Lawson, A.K.; Smith, K.N.; Kazer, R.R.; Klock, S.C.; Gradishar, W.J.; Jeruss, J.S.; Pavone, M.E. Predictors and outcomes in breast cancer patients who did or did not pursue fertility preservation. Breast Cancer Res. Treat. 2021, 186, 429–437. [Google Scholar] [CrossRef]
- Peate, M.; Meiser, B.; Cheah, B.C.; Saunders, C.; Butow, P.; Thewes, B.; Hart, R.; Phillips, K.A.; Hickey, M.; Friedlander, M. Making hard choices easier: A prospective, multicentre study to assess the efficacy of a fertility-related decision aid in young women with early-stage breast cancer. Br. J. Cancer 2012, 106, 1053–1061. [Google Scholar] [CrossRef]
- Jones, G.L.; Moss, R.H.; Darby, F.; Mahmoodi, N.; Phillips, B.; Hughes, J.; Vogt, K.S.; Greenfield, D.M.; Brauten-Smith, G.; Gath, J.; et al. Cancer, Fertility and Me: Developing and Testing a Novel Fertility Preservation Patient Decision Aid to Support Women at Risk of Losing Their Fertility Because of Cancer Treatment. Front. Oncol. 2022, 12, 896939. [Google Scholar] [CrossRef]
- Vest, A.N.; Kuete, N.T.; Mehta, A. Is fertility preservation a part of comprehensive cancer care in the USA? A study of NCI-designated cancer center websites. J. Cancer Surviv. 2021, 15, 906–911. [Google Scholar] [CrossRef]
- Clear & Simple. 7 July 2021. 2021. Available online: https://www.nih.gov/institutes-nih/nih-office-director/office-communications-public-liaison/clear-communication/clear-simple (accessed on 5 May 2023).
- Weiss, B.D. Health Literacy: A Manual for Clinicians; American Medical Association: Chicago, IL, USA, 2006; Available online: http://lib.ncfh.org/pdfs/6617.pdf (accessed on 5 May 2023).
- Hoyos-Martinez, A.; Hoyos, L.R.; Putra, M.; Armstrong, A.A.; Rambhatla, A.; Allen-Rhoades, W.; Brennan, K. Availability of Fertility Preservation Information on the Websites of U.S. News and World Report Top-Ranked Pediatric Cancer Programs. J. Adolesc. Young Adult Oncol. 2021, 10, 66–70. [Google Scholar] [CrossRef]
- Chapman, E.N.; Kaatz, A.; Carnes, M. Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. J. Gen. Intern. Med. 2013, 28, 1504–1510. [Google Scholar] [CrossRef]
- FitzGerald, C.; Hurst, S. Implicit bias in healthcare professionals: A systematic review. BMC Med. Ethics 2017, 18, 19. [Google Scholar] [CrossRef] [PubMed]
- Saraf, A.J.; Stanek, J.; Audino, A.; DaJusta, D.; Hansen-Moore, J.; McCracken, K.; Whiteside, S.; Yeager, N.; Nahata, L. Examining predictors and outcomes of fertility consults among children, adolescents, and young adults with cancer. Pediatr. Blood Cancer 2018, 65, e27409. [Google Scholar] [CrossRef] [PubMed]
- Quinn, G.P.; Vadaparampil, S.T.; King, L.; Miree, C.A.; Wilson, C.; Raj, O.; Watson, J.; Lopez, A.; Albrecht, T.L. Impact of physicians’ personal discomfort and patient prognosis on discussion of fertility preservation with young cancer patients. Patient Educ. Couns. 2009, 77, 338–343. [Google Scholar] [CrossRef] [PubMed]
- 2020 National ART Summary. Secondary 2020 National ART Summary 21 February 2023; 2020. Available online: https://www.cdc.gov/art/reports/2020/summary.html (accessed on 5 May 2023).
- Anderson, K.; Spurlin, E.E.; Ratts, V.S.; Jimenez, P.T.; Keller, S.L.; Omurtag, K. Use of Telehealth Services to Improve Access to Fertility Preservation Consultations in Patients Diagnosed with Cancer. N. Am. Proc. Gynecol. Obstet. 2022, 64, 49–96. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turner, K.A.; Spurlin, E.E.; Jimenez, P.T. Disparities in Female Oncofertility Care in the United States: More Questions Than Answers. Life 2023, 13, 1547. https://doi.org/10.3390/life13071547
Turner KA, Spurlin EE, Jimenez PT. Disparities in Female Oncofertility Care in the United States: More Questions Than Answers. Life. 2023; 13(7):1547. https://doi.org/10.3390/life13071547
Chicago/Turabian StyleTurner, Kati A., Emily E. Spurlin, and Patricia T. Jimenez. 2023. "Disparities in Female Oncofertility Care in the United States: More Questions Than Answers" Life 13, no. 7: 1547. https://doi.org/10.3390/life13071547
APA StyleTurner, K. A., Spurlin, E. E., & Jimenez, P. T. (2023). Disparities in Female Oncofertility Care in the United States: More Questions Than Answers. Life, 13(7), 1547. https://doi.org/10.3390/life13071547





