Mitral Annular Calcification and Thromboembolic Risk
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Enrolment, Inclusion, and Exclusion Criteria
2.2. Clinical Investigation and Data Collection
2.3. Statistical Analysis
3. Results
3.1. Study Group Description
- Interventricular septum (IVS): 12.14 ± 1.754 mm;
- LV posterior wall: 12.16 ± 1.685 mm;
- LV end-diastolic diameter (LVEDD): 50.82 ± 9.045 mm.
3.2. Relationship between MAC and Clinical, Biological, and Echocardiographic Parameters
3.3. Relationship between MAC and Other Comorbidities
3.4. Multivariate Analysis of the Relationship between MAC and Clinical, Biological, and Echocardiographic Parameters
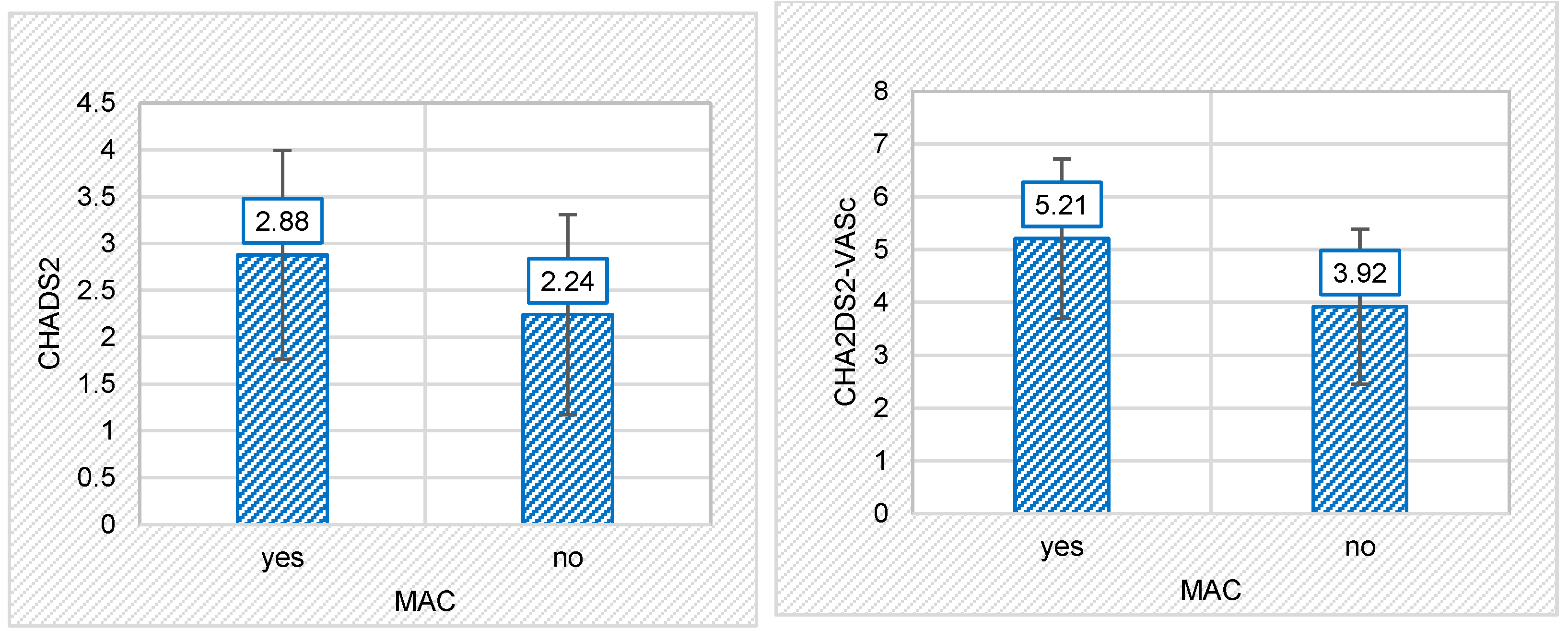
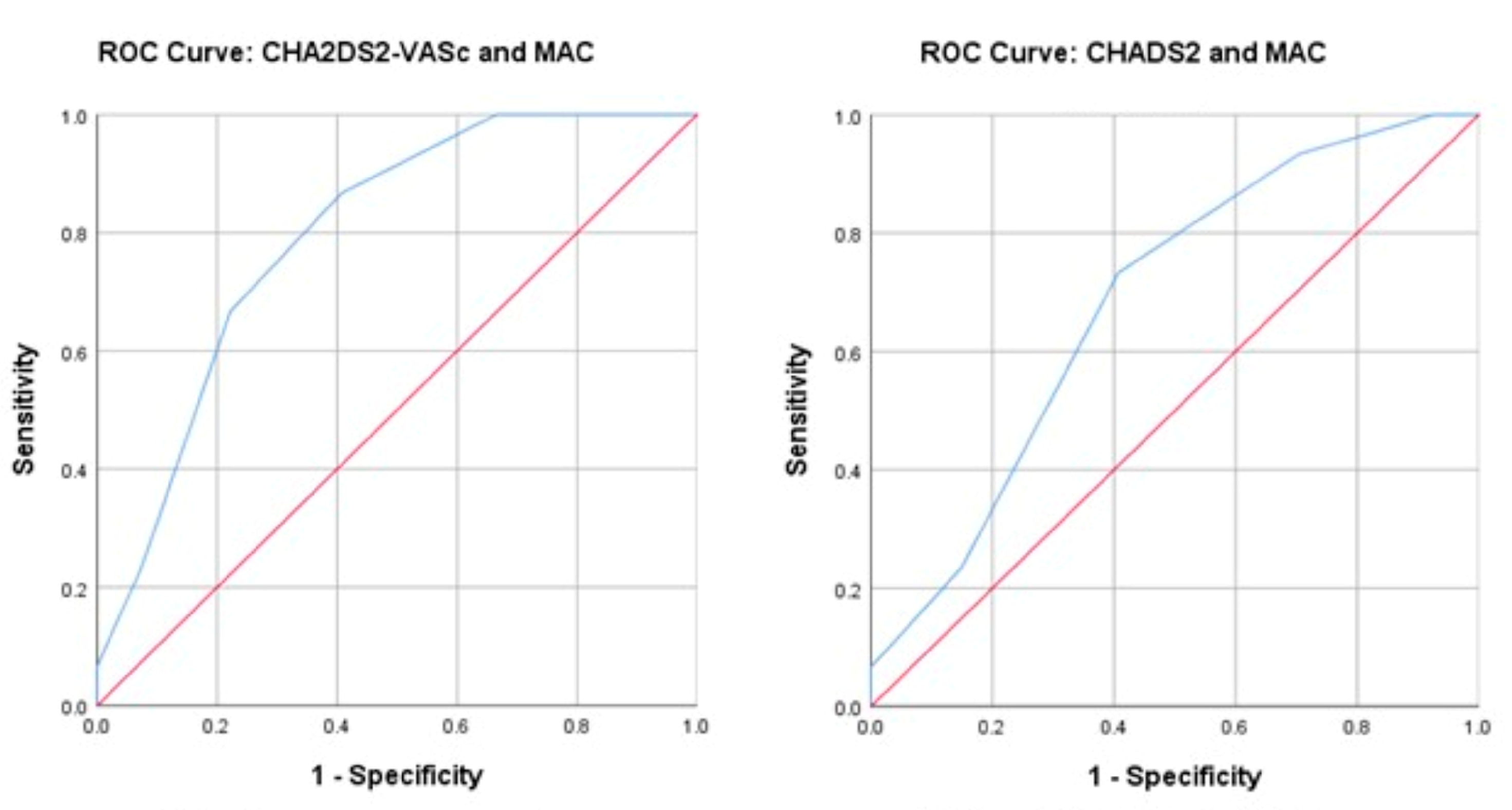
3.5. Relationship between MAC and Thromboembolic Risk Scores
3.6. Relationship between MAC and Thromboembolic Risk Depending on Gender
4. Discussion
4.1. Clinical Data
4.2. Echocardiographic Data
4.3. Thromboembolic Risk Scores
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abramowitz, Y.; Jilaihawi, H.; Chakravarty, T.; Mack, M.J.; Makkar, R.R. Mitral Annulus Calcification. J. Am. Coll. Cardiol. 2015, 66, 1934–1941. [Google Scholar] [CrossRef] [PubMed]
- Massera, D.; Kizer, J.R.; Dweck, M.R. Mechanisms of Mitral Annular Calcification. Trends Cardiovasc. Med. 2020, 30, 289–295. [Google Scholar] [CrossRef]
- Cavalcanti, L.R.P.; Sá, M.P.B.O.; Perazzo, Á.M.; Escorel Neto, A.C.; Gomes, R.A.F.; Weymann, A.; Zhigalov, K.; Ruhparwar, A.; Lima, R.C. Mitral Annular Calcification: Association with Atherosclerosis and Clinical Implications. Curr. Atheroscler. Rep. 2020, 22, 9. [Google Scholar] [CrossRef] [PubMed]
- Eberhard, M.; Schönenberger, A.L.N.; Hinzpeter, R.; Euler, A.; Sokolska, J.; Weber, L.; Kuzo, N.; Manka, R.; Kasel, A.M.; Tanner, F.C.; et al. Mitral Annular Calcification in the Elderly—Quantitative Assessment. J. Cardiovasc. Comput. Tomogr. 2021, 15, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Aksoy, F.; Guler, S.; Kahraman, F.; Kuyumcu, M.S.; Bagcı, A.; Bas, H.A.; Uysal, D.; Varol, E. The Relationship between Mitral Annular Calcification, Metabolic Syndrome and Thromboembolic Risk. Braz. J. Cardiovasc. Surg. 2019, 34, 535–541. [Google Scholar] [CrossRef]
- De Marco, M.; Gerdts, E.; Casalnuovo, G.; Migliore, T.; Wachtell, K.; Boman, K.; Dahlöf, B.; Olsen, M.H.; Kizer, J.R.; Devereux, R.B.; et al. Mitral Annular Calcification and Incident Ischemic Stroke in Treated Hypertensive Patients: The LIFE Study. Am. J. Hypertens. 2013, 26, 567–573. [Google Scholar] [CrossRef]
- Kizer, J.R.; Wiebers, D.O.; Whisnant, J.P.; Galloway, J.M.; Welty, T.K.; Lee, E.T.; Best, L.G.; Resnick, H.E.; Roman, M.J.; Devereux, R.B. Mitral Annular Calcification, Aortic Valve Sclerosis, and Incident Stroke in Adults Free of Clinical Cardiovascular Disease: The Strong Heart Study. Stroke 2005, 36, 2533–2537. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Bax, J.J.; Boriani, G.; Dan, G.A.; Fauchier, L.; Kalman, J.M.; Lane, D.A.; Lettino, M.; et al. 2020 ESC Guidelines for the Diagnosis and Management of Atrial Fibrillation Developed in Collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef]
- Chen, J.Y.; Zhang, A.D.; Lu, H.Y.; Guo, J.; Wang, F.F.; Li, Z.C. CHADS2 versus CHA2DS2-VASc Score in Assessing the Stroke and Thromboembolism Risk Stratification in Patients with Atrial Fibrillation: A Systematic Review and Meta-Analysis. J. Geriatr. Cardiol. 2013, 10, 258–266. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Victor, M.A.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef]
- Kohsaka, S.; Jin, Z.; Rundek, T.; Boden-Albala, B.; Homma, S.; Sacco, R.L.; Di Tullio, M.R. Impact of Mitral Annular Calcification on Cardiovascular Events in a Multiethnic Community. The Northern Manhattan Study. JACC Cardiovasc. Imaging 2008, 1, 617–623. [Google Scholar] [CrossRef]
- Kanjanauthai, S.; Nasir, K.; Katz, R.; Rivera, J.J.; Takasu, J.; Blumenthal, R.S.; Eng, J.; Budoff, M.J. Relationships of Mitral Annular Calcification to Cardiovascular Risk Factors: The Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis 2010, 213, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Elmariah, S.; Budoff, M.J.; Delaney, J.A.C.; Hamirani, Y.; Eng, J.; Fuster, V.; Kronmal, R.A.; Halperin, J.L.; O’Brien, K.D. Risk Factors Associated with the Incidence and Progression of Mitral Annulus Calcification: The Multi-Ethnic Study of Atherosclerosis. Am. Heart J. 2013, 166, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Sugihara, N.; Matsuzaki, M. The Influence of Severe Bone Loss on Mitral Annular Calcification in Postmenopausal Osteoporosis of Elderly Japanese Women. Jpn. Circ. J. 1993, 57, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.C.; Leopold, J.A.; Loscalzo, J. Vascular Calcification: Pathobiological Mechanisms and Clinical Implications. Circ. Res. 2006, 99, 1044–1059. [Google Scholar] [CrossRef]
- Adler, Y.; Fink, N.; Spector, D.; Wiser, I.; Sagie, A. Mitral Annulus Calcification—A Window to Diffuse Atherosclerosis of the Vascular System. Atherosclerosis 2001, 155, 1–8. [Google Scholar] [CrossRef]
- Garg, P.K.; Buzkova, P.; Meyghani, Z.; Budoff, M.J.; Lima, J.; Criqui, M.; Cushman, M.; Allison, M. Valvular Calcification and Risk of Peripheral Artery Disease: TheMulti-Ethnic Study of Atherosclerosis (MESA). Eur. Heart J. Cardiovasc. Imaging 2020, 21, 1152–1159. [Google Scholar] [CrossRef]
- Barasch, E.; Gottdiener, J.S.; Marino Larsen, E.K.; Chaves, P.H.M.; Newman, A.B.; Manolio, T.A. Clinical Significance of Calcification of the Fibrous Skeleton of the Heart and Aortosclerosis in Community Dwelling Elderly. The Cardiovascular Health Study (CHS). Am. Heart J. 2006, 151, 39–47. [Google Scholar] [CrossRef]
- Adler, Y.; Levinger, U.; Koren, A.; Gabbay, R.; Shapira, Y.; Vaturi, M.; Fink, N.; Herz, I.; Zelikovski, A.; Sagie, A. Association between Mitral Annulus Calcification and Peripheral Arterial Atherosclerotic Disease. Angiology 2000, 51, 639–646. [Google Scholar]
- Atar, S.; Jeon, D.S.; Luo, H.; Siegel, R.J. Mitral Annular Calcification: A Marker of Severe Coronary Artery Disease in Patients under 65 Years Old. Heart 2003, 89, 161–164. [Google Scholar] [CrossRef]
- Grigorescu, E.-D.; Lăcătușu, C.-M.; Floria, M.; Cazac, G.-D.; Onofriescu, A.; Ceasovschih, A.; Crețu, I.; Mihai, B.-M.; Șorodoc, L. Association of Inflammatory and Metabolic Biomarkers with Mitral Annular Calcification in Type 2 Diabetes Patients. J. Pers. Med. 2022, 12, 1484. [Google Scholar] [CrossRef]
- Asmat, U.; Abad, K.; Ismail, K. Diabetes Mellitus and Oxidative Stress—A Concise Review. Saudi Pharm. J. 2016, 24, 547–553. [Google Scholar] [CrossRef]
- Fuentes, E.; Palomo, I. Role of Oxidative Stress on Platelet Hyperreactivity during Aging. Life Sci. 2016, 148, 17–23. [Google Scholar] [CrossRef]
- Rao, A.K.; Djamali, A.; Korcarz, C.E.; Aeschlimann, S.E.; Wolff, M.R.; Stein, J.H. Mitral Annular Calcification Is Associated with Reduced Left Ventricular Function and Inflammation in Patients with Chronic Kidney Disease. J. Am. Soc. Echocardiogr. 2008, 21, 747–750. [Google Scholar] [CrossRef] [PubMed]
- Cioffi, G.; Faganello, G.; De Feo, S.; Berlinghieri, N.; Tarantini, L.; Di Lenarda, A.; Pinamonti, B.; Candido, R.; Faggiano, P. Combined Circumferential and Longitudinal Left Ventricular Systolic Dysfunction in Patients with Type 2 Diabetes Mellitus without Myocardial Ischemia. Exp. Clin. Cardiol. 2013, 18, e26–e31. [Google Scholar] [PubMed]
- Gökdeniz, T.; Boyaci, F.; Hatem, E.; Bektaş, H.; Kalaycioʇlu, E.; Gürsoy, M.O.; Aykan, A.Ç.; Yildiz, B.Ş.; Altintaş, B. Association of Mitral Annular Calcification with Left Ventricular Mechanics: A Speckle Tracking Study. Echocardiography 2015, 32, 1374–1383. [Google Scholar] [CrossRef]
- Faganello, G.; Faggiano, P.; Candido, R.; Tarantini, L.; Di Lenarda, A.; De Feo, S.; Cioffi, G. The Worrisome Liaison between Left Ventricular Systolic Dysfunction and Mitral Annulus Calcification in Type 2 Diabetes without Coronary Artery Disease: Data from the SHORTWAVE Study. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 1188–1194. [Google Scholar] [CrossRef]
- Kurtoǧlu, E.; Korkmaz, H.; Aktürk, E.; Ylmaz, M.; Altaş, Y.; Uçkan, A. Association of Mitral Annulus Calcification with High-Sensitivity C-Reactive Protein, Which Is a Marker of Inflammation. Mediat. Inflamm. 2012, 2012, 606207. [Google Scholar] [CrossRef]
- Rytand, D.A. Clinical aspects of calcification of the mitral annulus fibrosus. Arch. Intern. Med. 1946, 78, 544–564. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Plehn, J.F.; D’Agostino, R.B.; Belanger, A.J.; Comai, K.; Fuller, D.L.; Wolf, P.A.; Levy, D. Mitral Annular Calcification and the Risk of Stroke in an Elderly Cohort. N. Engl. J. Med. 1992, 327, 374–379. [Google Scholar] [CrossRef]
- Qasim, A.N.; Rafeek, H.; Rasania, S.P.; Churchill, T.W.; Yang, W.; Ferrari, V.A.; Jha, S.; Master, S.M.; Mulvey, C.K.; Terembula, K.; et al. Cardiovascular Risk Factors and Mitral Annular Calcification in Type 2 Diabetes. Atherosclerosis 2013, 226, 419–424. [Google Scholar] [CrossRef] [PubMed]
- O’Neal, W.T.; Efird, J.T.; Nazarian, S.; Alonso, A.; Michos, E.D.; Szklo, M.; Heckbert, S.R.; Soliman, E.Z. Mitral Annular Calcification Progression and the Risk of Atrial Fibrillation: Results from MESA. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.K.M.; Griffin, B.P.; Xu, B.; Rodriguez, L.L.; Popovic, Z.B.; Gillinov, M.A.; Pettersson, G.B.; Desai, M.Y. Relationships between Mitral Annular Calcification and Cardiovascular Events: A Meta-Analysis. Echocardiography 2020, 37, 1723–1731. [Google Scholar] [CrossRef] [PubMed]
- Calicchio, F.; Onuegbu, A.; Kinninger, A.; Nakanishi, R.; Carr, J.J.; Nasir, K.; Gottesman, R.; Budoff, M.J. Mitral annular calcification as a predictor of stroke in the multi ethnic study of atherosclerosis. J. Am. Coll. Cardiol. 2022, 79, 1199. [Google Scholar] [CrossRef]
- Fashanu, O.E.; Bizanti, A.; Al-Abdouh, A.; Zhao, D.; Budoff, M.J.; Thomas, I.C.; Longstreth, W.T.; Michos, E.D. Progression of Valvular Calcification and Risk of Incident Stroke: The Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis 2020, 307, 32–38. [Google Scholar] [CrossRef] [PubMed]


| Parameter | Overall (n = 103) | with MAC (n = 52) | without MAC (n = 51) | p-Value |
|---|---|---|---|---|
| Clinical parameters | ||||
| Age (years) | 72.59 ± 9.914 | 74.46 ± 10.019 | 70.69 ± 9.528 | 0.042 * |
| BMI (kg/m2) | 28.65 ± 5.939 | 29.20 ± 6.463 | 28.10 ± 5.378 | 0.669 |
| Female gender (%) | 57 (55.3%) | 30 (57.7%) | 27 (52.9%) | 0.628 |
| Smoking (%) | 45 (43.7%) | 24 (46.2%) | 21 (41.2%) | 0.611 |
| Comorbidities | ||||
| Arterial hypertension (%) | 86 (83.5%) | 46 (88.5%) | 40 (78,4%) | 0.170 |
| Diabetes mellitus (%) | 31 (30.1%) | 22 (42.3%) | 9 (17.6%) | 0.006 * |
| Obesity (%) | 35 (34.0%) | 20 (38.5%) | 15 (29.4%) | 0.332 |
| Heart failure (%) | 82 (79.6%) | 41 (78.8%) | 41 (80.4%) | 0.846 |
| Myocardial infarction (%) | 7 (6.8%) | 5 (9.6%) | 2 (3.9%) | 0.437 |
| Prior stroke (%) | 8 (7.8%) | 6 (11.5%) | 2 (3.9%) | 0.269 |
| Atrial fibrillation (%) | 42 (40.8%) | 24 (46.2%) | 18 (35.3%) | 0.262 |
| Aortic atherosclerosis plaques (%) | 68 (66.0%) | 47 (90.4%) | 21 (41.2%) | <0.001 * |
| Vascular disease (%) | 67 (65.0%) | 48 (92.3%) | 19 (37.3%) | <0.001 * |
| Peripheral artery disease (%) | 22 (21.4%) | 12 (23.1%) | 10 (19.6%) | 0.668 |
| Biological parameters | ||||
| Total cholesterol (mg/dL) | 191.86 ± 54.270 | 189.00 ± 51.406 | 194.78 ± 57.407 | 0.591 |
| Triglycerides (mg/dL) | 117.75 ± 53.757 | 114.94 ± 59.352 | 120.61 ± 47.808 | 0.288 |
| Fasting Glycemia (mg/dL) | 120.44 ± 47.576 | 126.85 ± 61.046 | 113.78 ± 26.418 | 0.870 |
| AST (U/L) | 29.31 ± 39.397 | 32.33 ± 48.947 | 26.24 ± 26.522 | 0.484 |
| ALT (U/L) | 30.54 ± 35.991 | 33.13 ± 41.888 | 27.90 ± 28.959 | 0.702 |
| GGT (U/L) | 66.85 ± 122.845 | 94.72 ± 173.207 | 42.39 ± 32.441 | 0.633 |
| Echocardiographic parameters | ||||
| LVEF (%) | 49.50 ± 13.085 | 46.48 ± 13.126 | 52.59 ± 12.423 | 0.010 * |
| IVS (mm) | 12.14 ± 1.754 | 12.27 ± 1.868 | 12.00 ± 1.637 | 0.263 |
| LVPW (mm) | 12.16 ± 1.685 | 12.25 ± 1.823 | 12.08 ± 1.545 | 0.583 |
| LVEDD (mm) | 50.82 ± 9.045 | 50.52 ± 8.012 | 51.14 ± 10.062 | 0.653 |
| TE risk scores | ||||
| CHADS2 | 2.56 ± 1.135 | 2.88 ± 1.114 | 2.24 ± 1.069 | 0.005 * |
| CHA2-DS2-VASc | 4.57 ± 1.619 | 5.21 ± 1.513 | 3.92 ± 1.468 | <0.001 * |
| Treatment | ||||
| Statins (%) | 70 | 71 | 69 | 0.623 |
| Antiplatelets (%) | 57 | 58 | 57 | 0.779 |
| Oral anticoagulants (%) | 39 | 50 | 27 | 0.018 * |
| Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|
| p | OR (95% CI) | p | OR (95% CI) | B Coef. | |
| Age (years) | 0.042 * | - | 0.200 | 1.037 (0.981 ÷ 1.097) | 0.036 |
| Diabetes mellitus (%) | 0.006 * | 3.422 (1.383 ÷ 8.469) | 0.017 * | 4.226 (1.293 ÷ 13.814) | 1.441 |
| Aortic atherosclerosis plaques (%) | <0.001 * | 13.429 (4.572 ÷ 39.444) | 0.955 | 1.071 (0.100 ÷ 11.430) | 0.068 |
| Vascular disease (%) | <0.001 * | 20.211 (6.290 ÷ 64.944) | 0.019 * | 18.027 (1.618 ÷ 200.800) | 2892 |
| LVEF (%) | 0.010 * | - | 0.461 | 0.986 (0.949 ÷ 1.024) | −0.014 |
| Constant | −4.420 | ||||
| CHADS2 | CHA2DS2-VASC | |||||
|---|---|---|---|---|---|---|
| r | p | Regression Line | r | p | Regression Line | |
| Age (years) | 0.456 | 0.000 * | y = 0.052 ∗ x − 1.229 | 0.612 | 0.000 * | y = 0.100 ∗ x − 2.683 |
| BMI (kg/m2) | 0.138 | 0.230 | 0.032 | 0.782 | ||
| Total cholesterol (mg/dL) | −0.142 | 0.151 | −0.006 | 0.952 | ||
| Triglycerides (mg/dL) | 0.000 | 0.997 | 0.023 | 0.821 | ||
| Fasting Glycemia (mg/dL) | 0.294 | 0.003 * | y = 0.007 ∗ x + 1.762 | 0.257 | 0.009 * | y = 0.009 ∗ x + 3.533 |
| AST (U/L) | 0.122 | 0.221 | 0.076 | 0.443 | ||
| ALT (U/L) | 0.126 | 0.204 | 0.035 | 0.727 | ||
| GGT (U/L) | 0.057 | 0.591 | −0.051 | 0.626 | ||
| LVEF (%) | −0.161 | 0.104 | −0.139 | 0.161 | ||
| IVS (mm) | 0.146 | 0.141 | 0.090 | 0.367 | ||
| LVPW (mm) | 0.106 | 0.285 | 0.042 | 0.676 | ||
| LVEDD (mm) | 0.031 | 0.755 | −0.050 | 0.619 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morariu, P.C.; Tanase, D.M.; Iov, D.E.; Sîrbu, O.; Oancea, A.F.; Mircea, C.G.; Chiriac, C.P.; Baroi, G.L.; Morariu, I.-D.; Dascălu, C.G.; et al. Mitral Annular Calcification and Thromboembolic Risk. Life 2023, 13, 1568. https://doi.org/10.3390/life13071568
Morariu PC, Tanase DM, Iov DE, Sîrbu O, Oancea AF, Mircea CG, Chiriac CP, Baroi GL, Morariu I-D, Dascălu CG, et al. Mitral Annular Calcification and Thromboembolic Risk. Life. 2023; 13(7):1568. https://doi.org/10.3390/life13071568
Chicago/Turabian StyleMorariu, Paula Cristina, Daniela Maria Tanase, Diana Elena Iov, Oana Sîrbu, Alexandru Florinel Oancea, Cornel Gabriel Mircea, Cristina Petronela Chiriac, Genoveva Livia Baroi, Ionela-Daniela Morariu, Cristina Gena Dascălu, and et al. 2023. "Mitral Annular Calcification and Thromboembolic Risk" Life 13, no. 7: 1568. https://doi.org/10.3390/life13071568
APA StyleMorariu, P. C., Tanase, D. M., Iov, D. E., Sîrbu, O., Oancea, A. F., Mircea, C. G., Chiriac, C. P., Baroi, G. L., Morariu, I.-D., Dascălu, C. G., Şorodoc, L., & Floria, M. (2023). Mitral Annular Calcification and Thromboembolic Risk. Life, 13(7), 1568. https://doi.org/10.3390/life13071568










