Bilateral Angle Recession and Chronic Post-Traumatic Glaucoma: A Review of the Literature and a Case Report
Abstract
:1. Epidemiology of Ocular Trauma
1.1. General Risk Factors
1.2. Airbag-Related Eye Injuries
2. Angle Recession and Post-Traumatic Glaucoma
2.1. Pathophysiology
2.2. Diagnosis
2.3. Treatments
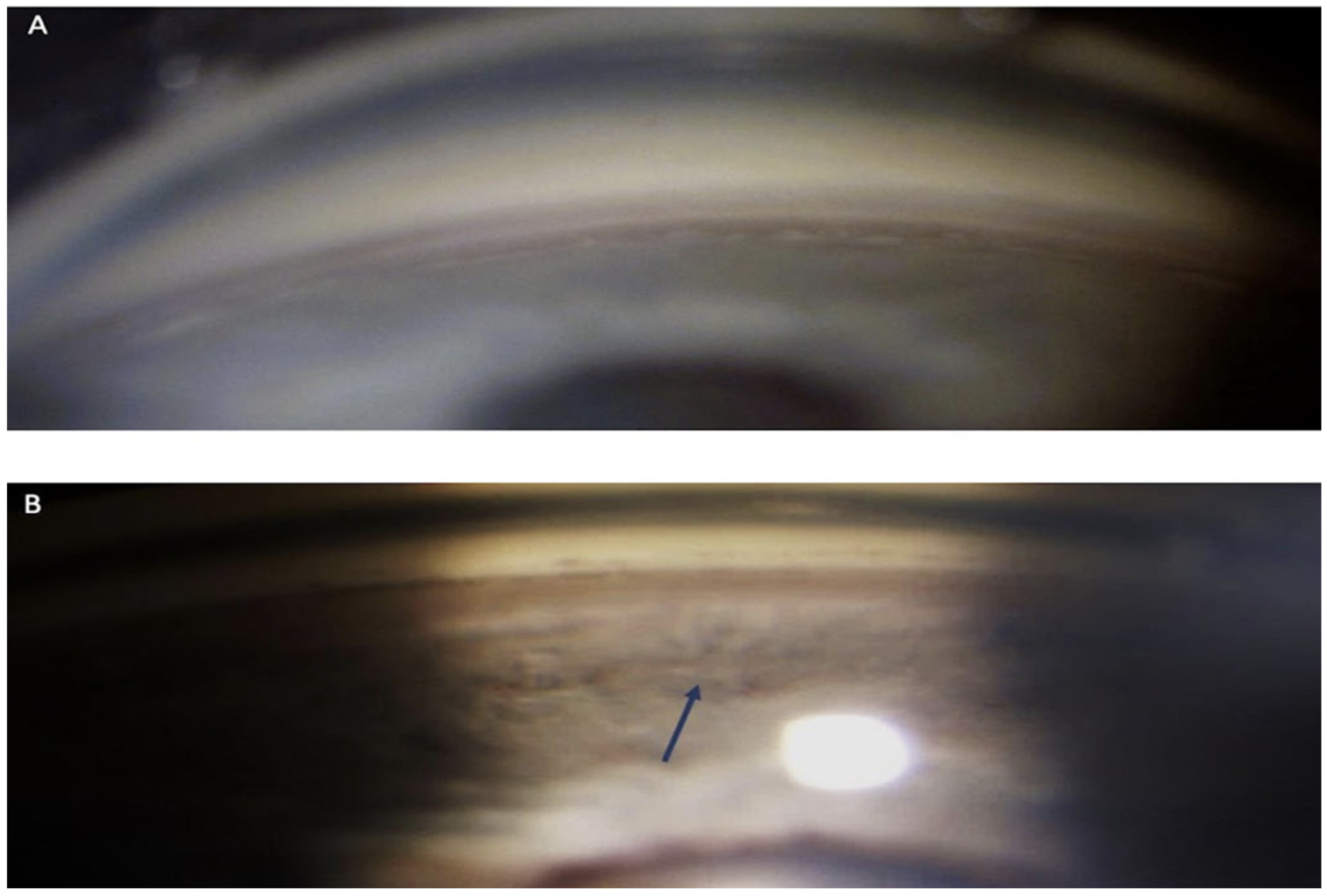
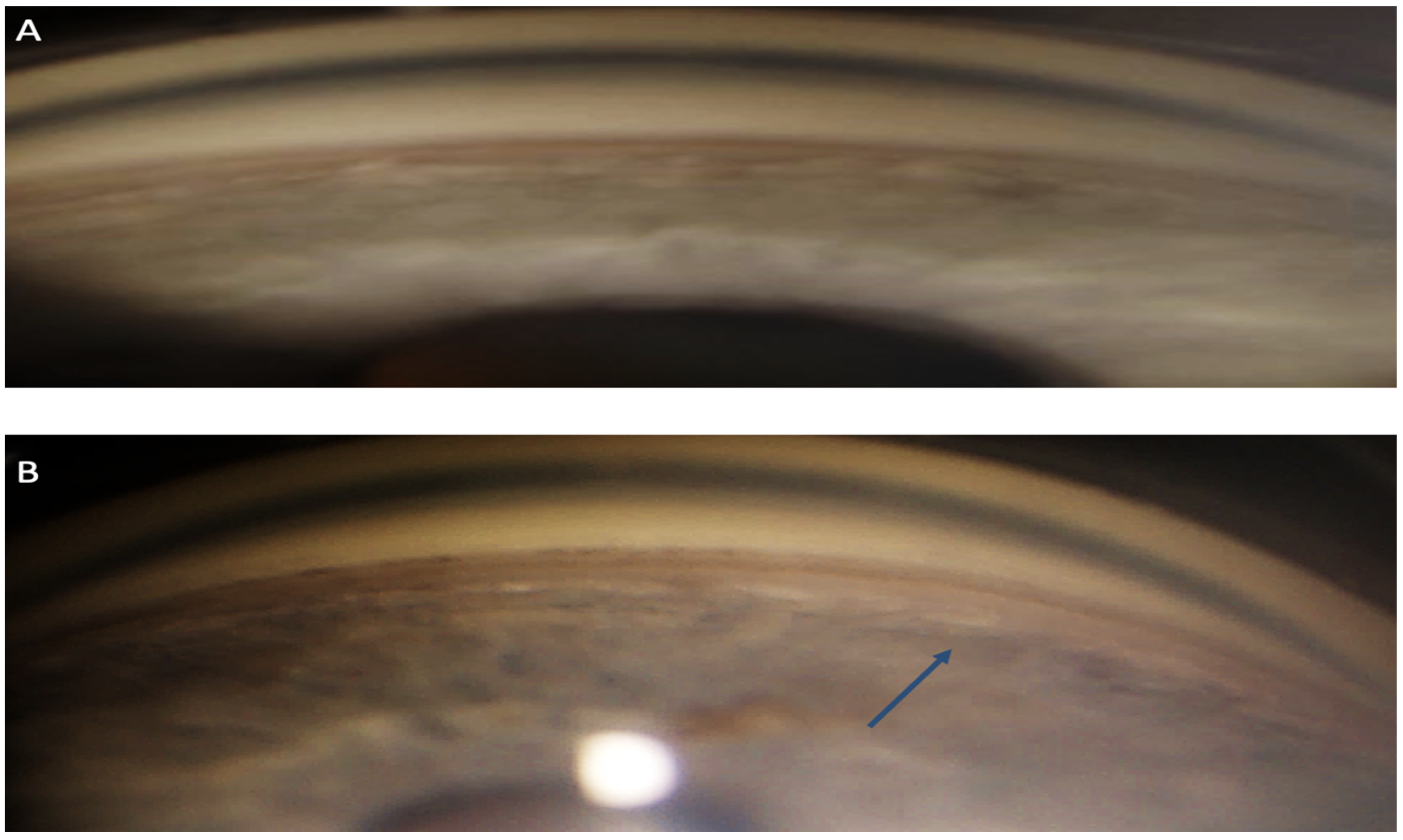
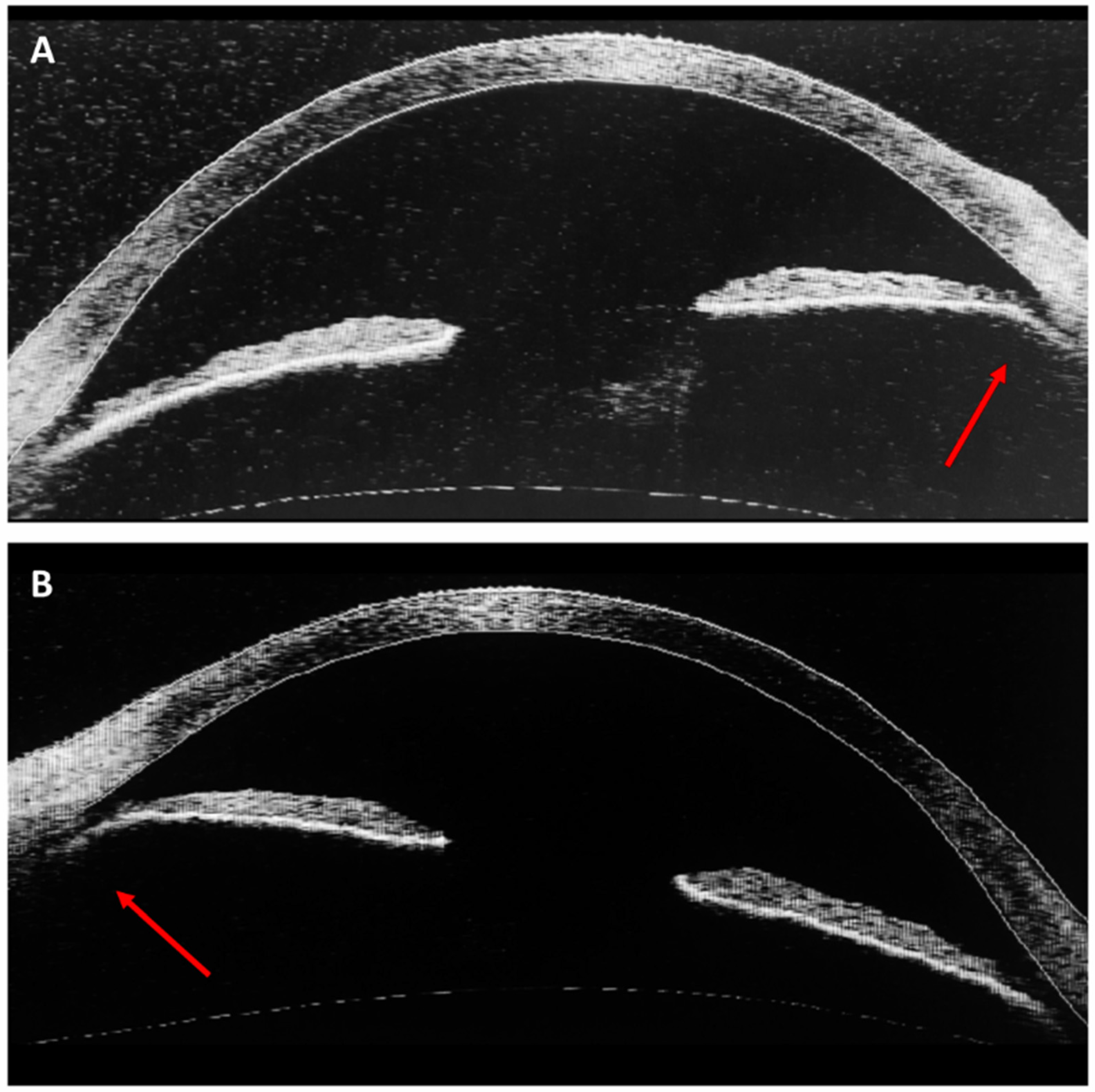
3. Case Report
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Négrel, A.D.; Thylefors, B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998, 5, 143–169. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.M.S.; Low, R.; Hoskin, A.K.; Rousselot, A.; Gunasekeran, D.V.; Natarajan, S.; Sundar, G.; Chee, C.K.L.; Mishra, C.; Sen, P. The application of clinical registries in ophthalmic trauma—The International Globe and Adnexal Trauma Epidemiology Study (IGATES). Graefes Arch. Clin. Exp. Ophthalmol. 2022, 260, 1055–1067. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, F.; Morris, R.; Witherspoon, C.D.; Heimann, K.; Jeffers, J.B.; Treister, G. A Standardized Classification of Ocular Trauma. Ophthalmology 1996, 103, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Pieramici, D.J.; Sternberg, P., Jr.; Aaberg, T.M., Sr.; Bridges, W.Z., Jr.; Capone, A., Jr.; Cardillo, J.A.; De Juan, E., Jr.; Kuhn, F.; Meredith, T.A.; Mieler, W.F.; et al. A System for classifying mechanical injuries of the eye (Globe). Am. J. Ophthalmol. 1997, 123, 820–831. [Google Scholar] [CrossRef] [PubMed]
- Bhalla, K.; Gleason, K. Effects of vehicle safety design on road traffic deaths, injuries, and public health burden in the Latin American region: A modelling study. Lancet Glob. Health 2020, 8, e819–e828. [Google Scholar] [CrossRef]
- International Transport Forum. Road Safety Annual Report 2016; OECD: Paris, France, 2016. [Google Scholar] [CrossRef]
- International Transport Forum. Road Safety Annual Report 2018; OECD: Paris, France, 2018. [Google Scholar] [CrossRef]
- Motley, W.W.; Kaufman, A.H.; West, C.E. Pediatric airbag-associated ocular trauma and endothelial cell loss. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2003, 7, 380–383. [Google Scholar] [CrossRef]
- Braver, E.R.; Ferguson, S.A.; Greene, M.A.; Lund, A.K. Reductions in deaths in frontal crashes among right front passengers in vehicles equipped with passenger air bags. JAMA 1997, 278, 1437–1439. [Google Scholar] [CrossRef]
- Wallis, L.A. Injuries associated with airbag deployment. Emerg. Med. J. 2002, 19, 490–493. [Google Scholar] [CrossRef]
- Pearlman, J.A.; Eong, K.G.A.; Kuhn, F.; Pieramici, D.J. Airbags and eye injuries. Surv. Ophthalmol. 2001, 46, 234–242. [Google Scholar] [CrossRef]
- Lee, W.B.; O’Halloran, H.S.; Pearson, P.A.; Sen, H.A.; Reddy, S.H.K. Airbags and bilateral eye injury: Five case reports and a review of the literature. J. Emerg. Med. 2001, 20, 129–134. [Google Scholar] [CrossRef]
- Malhotra, K.; Rose, J.; Homer, N. Devastating injury from blunt airbag trauma. J. Am. Coll. Emerg. Physicians Open 2022, 3, e12676. [Google Scholar] [CrossRef] [PubMed]
- Duma, S.M. The effect of frontal air bags on eye injury patterns in automobile crashes. Arch. Ophthalmol. 2002, 120, 1517. [Google Scholar] [CrossRef] [PubMed]
- Shirzadi, H.; Zohoor, H.; Naserkhaki, S. Biomechanical simulation of eye-airbag impacts during vehicle accidents. Proc. Inst. Mech. Eng. 2018, 232, 699–707. [Google Scholar] [CrossRef] [PubMed]
- Fukagawa, K.; Tsubota, K.; Kimura, C.; Hata, S.; Mashita, T.; Sugimoto, T.; Oguchi, Y. Corneal Endothelial Cell Loss Induced by Air Bags. Ophthalmology 1993, 100, 1819–1823. [Google Scholar] [CrossRef] [PubMed]
- Duma, S.M.; Kress, T.A.; Porta, D.J.; Simmons, R.J.; Alexander, C.L.; Woods, C.D. Airbag-induced eye injuries: Experiments with in situ cadaver eyes. Biomed. Sci. Instrum. 1997, 33, 106–111. [Google Scholar] [PubMed]
- Kobayashi, A.; Izaki, R.; Fujita, H.; Harada, K.; Ozaki, H.; Kadonosono, K.; Uchio, E. Finite element analysis of changes in tensile strain and deformation by airbag impact in eyes of various axial lengths. Int. Ophthalmol. 2023, 43, 2143–2151. [Google Scholar] [CrossRef]
- Huang, J.; Uchio, E.; Goto, S. Simulation of airbag impact on eyes with different axial lengths after transsclerally fixated posterior chamber intraocular lens by using finite element analysis. Clin. Ophthalmol. 2015, 9, 263–270. [Google Scholar] [CrossRef]
- Azukisawa, M.; Sato, T.; Ito, Y.; Kamezawa, H.; Nomura, E.; Nishide, T.; Kadonosono, K.; Uchio, E.; Goto, S. Simulation of airbag impact on eyes after trabeculectomy by finite element analysis method. Nippon Ganka Gakkai Zasshi 2005, 109, 406–416. [Google Scholar]
- Uchio, E.; Watanabe, Y.; Kadonosono, K.; Matsuoka, Y.; Goto, S. Simulation of airbag impact on eyes after photorefractive keratectomy by finite element analysis method. Graefes. Arch. Clin. Exp. Ophthalmol. 2003, 241, 497–504. [Google Scholar] [CrossRef]
- Uchio, E.; Kadonosono, K.; Matsuoka, Y.; Goto, S. Simulation of air-bag impact on an eye with transsclerally fixated posterior chamber intraocular lens using finite element analysis. J. Cataract. Refract. Surg. 2004, 30, 483–490. [Google Scholar] [CrossRef]
- Uchio, E.; Ohno, S.; Kudoh, K.; Kadonosono, K.; Andoh, K.; Kisielewicz, L.T. Simulation of air-bag impact on post-radial keratotomy eye using finite element analysis. J. Cataract. Refract. Surg. 2001, 27, 1847–1853. [Google Scholar] [CrossRef] [PubMed]
- Stein, J.D.; Jaeger, E.A.; Jeffers, J.B. Air bags and ocular injuries. Trans. Am. Ophthalmol. Soc. 1999, 97, 59–82; discussion 82–86. [Google Scholar] [CrossRef]
- Lehto, K.S.; Sulander, P.O.; Tervo, T.M.T. Do motor vehicle airbags increase risk of ocular injuries in adults? Ophthalmology 2003, 110, 1082–1088. [Google Scholar] [CrossRef]
- Goldberg, M.A.; Valluri, S.; Pepose, J.S. Air Bag-related Corneal Rupture After Radial Keratotomy. Am. J. Ophthalmol. 1995, 120, 800–802. [Google Scholar] [CrossRef] [PubMed]
- Maharshak, I.; Bourla, D.; Grinbaum, A.; Weinberger, D.; Axer-Siegel, R. Airbag-induced bilateral corneal graft dehiscence. Cornea 2005, 24, 110–111. [Google Scholar] [CrossRef] [PubMed]
- Uchio, E.; Kadonosono, K. Are airbags a risk for patients after radial keratotomy? Br. J. Ophthalmol. 2001, 85, 640–642. [Google Scholar] [CrossRef] [PubMed]
- Zacovic, J.W.; McGuirk, T.D.; Knoop, K.J. Bilateral hyphemas as a result of air bag deployment. Am. J. Emerg. Med. 1997, 15, 323–324. [Google Scholar] [CrossRef]
- Salam, T.; Stavrakas, P.; Wickham, L.; Bainbridge, J. Airbag injury and bilateral globe rupture. Am. J. Emerg. Med. 2010, 28, 982.e5–982.e6. [Google Scholar] [CrossRef]
- Ogun, O.; Ikyaa, S.; Ogun, G. Rethinking airbag safety: Airbag injury causing bilateral blindness. Middle East Afr. J. Ophthalmol. 2014, 21, 196. [Google Scholar] [CrossRef]
- Subash, M.; Manzouri, B.; Wilkins, M. Airbag-induced chemical eye injury. Eur. J. Emerg. Med. 2010, 17, 22–23. [Google Scholar] [CrossRef]
- Welch, J.F. Bilateral chemical eye injury resulting from airbag deployment. J. R. Nav. Med. Serv. 2013, 99, 171–173. [Google Scholar] [CrossRef]
- Fante, R.J.; Trobe, J.D. Bilateral corneal abrasions from airbag deployment. N. Engl. J. Med. 2014, 370, e40. [Google Scholar] [CrossRef] [PubMed]
- Onwuzuruigbo, C.J.; Fulda, G.J.; Larned, D.; Hailstone, D. Traumatic blindness after airbag deployment: Bilateral lenticular dislocation. J. Trauma Inj. Infect. Crit. Care 1996, 40, 314–316. [Google Scholar] [CrossRef] [PubMed]
- Odouard, C.; Kuo, C.; Tariq, Y.M.; Ha, J.H.; Swamy, B. Central visual loss following a motor vehicle accident: Traumatic airbag maculopathy. Med. J. Aust. 2016, 205, 443–444. [Google Scholar] [CrossRef]
- Ball, D.C.; Bouchard, C.S. Ocular morbidity associated with airbag deployment: A report of seven cases and a Review of the Literature. Cornea 2001, 20, 159–163. [Google Scholar] [CrossRef]
- Savastano, A.; Donati, M.C.; Rizzo, S. Retinal tear related to air bag deployment. JAMA Ophthalmol. 2016, 134, e155021. [Google Scholar] [CrossRef] [PubMed]
- Lueder, G. Air bag-associated ocular trauma in children. Ophthalmology 2000, 107, 1472–1475. [Google Scholar] [CrossRef]
- Ingraham, H.J. Air-Bag Keratitis. N. Engl. J. Med. 1991, 324, 1599–1600. [Google Scholar] [CrossRef]
- Criado, A.L.; López, P.B.; Alonso, A.G. Permanent visual loss secondary to airbag deployment. Acta Ophthalmol. 2010, 88, e341. [Google Scholar] [CrossRef]
- Driver, P.J.; Cashwell, L.F.; Yeatts, R.P. Airbag-associated bilateral hyphemas and angle recession. Am. J. Ophthalmol. 1994, 118, 250–251. [Google Scholar] [CrossRef]
- Michaeli-Cohen, A.; Neufeld, M.; Lazar, M.; Geyer, O.; Haddad, R.; Kashtan, H. Bilateral corneal contusion and angle recession caused by an airbag. Br. J. Ophthalmol. 1996, 80, 487. [Google Scholar] [CrossRef] [PubMed]
- Alquraini, T.A.; Aggour, M.A.; Zamzam, A.M. Airbag induced facial and bilateral ocular injuries in a 14-year-old child. Saudi J. Ophthalmol. 2011, 25, 421–425. [Google Scholar] [CrossRef]
- Ghafouri, A.; Burgess, S.K.; Hrdlicka, Z.K.; Zagelbaum, B.M. Air bag-related ocular trauma. Am. J. Emerg. Med. 1997, 15, 389–392. [Google Scholar] [CrossRef] [PubMed]
- Girkin, C.A.; McGwin, G.; Morris, R.; Kuhn, F. Glaucoma following penetrating ocular trauma: A cohort study of the United States Eye Injury Registry. Am. J. Ophthalmol. 2005, 139, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Girkin, C.A.; McGwin, G.; Long, C.; Morris, R.; Kuhn, F. Glaucoma after ocular contusion: A cohort study of the United States eye injury registry. J. Glaucoma 2005, 14, 470–473. [Google Scholar] [CrossRef]
- Yanoff, M.; Duker, J.S. (Eds.) Ophthalmology, 4th ed.; Elsevier Saunders: Amsterdam, The Netherlands, 2014; pp. 1084–1089. [Google Scholar]
- Tumbocon, J.A.J.; Latina, M.A. Angle recession glaucoma. Int. Ophthalmol. Clin. 2002, 42, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Collins, E.T. On the Pathological Examination of Three Eyes Lost from Concussion; Ophthalmological Society of the United Kingdom: London, UK, 1890; Volume XII. [Google Scholar]
- Wolff, S.M.; Zimmerman, L.E. Chronic secondary glaucoma. Associated with retrodisplacement of iris root and deepening of the anterior chamber angle secondary to contusion. Am. J. Ophthalmol. 1962, 54, 547–563. [Google Scholar] [CrossRef]
- Reese, A.B. Deep-chamber glaucoma due to the formation of a cuticular product in the filtration Angle. Trans. Am. Ophthalmol. Soc. 1944, 42, 155–169. [Google Scholar] [CrossRef]
- D’Ombrain, A. Traumatic or “concussion” chronic glaucoma. Br. J. Ophthalmol. 1949, 33, 495–500. [Google Scholar] [CrossRef]
- Walton, W.; Von Hagen, S.; Grigorian, R.; Zarbin, M. Management of traumatic hyphema. Surv. Ophthalmol. 2002, 47, 297–334. [Google Scholar] [CrossRef]
- Loo, Y.; Tun, T.A.; Vithana, E.N.; Loo, Y.; Tun, T.A.; Vithana, E.N.; Perera, S.A.; Husain, R.; Wong, T.T.; Aung, T.; et al. Association of peripheral anterior synechiae with anterior segment parameters in eyes with primary angle closure glaucoma. Sci. Rep. 2021, 11, 13906. [Google Scholar] [CrossRef]
- Jensen, O.A. Contusive angle recession. A histopathological study of a danish material. Acta Ophthalmol. 2009, 46, 1207–1212. [Google Scholar] [CrossRef]
- Pujari, A.; Selvan, H.; Behera, A.K.; Gagrani, M.; Kapoor, S.; Dada, T. The probable mechanism of traumatic angle recession and cyclodialysis. J. Glaucoma 2020, 29, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Duke-Elder, S. (Ed.) Mechanical Injuries; Kimpton: San Francisco, CA, USA, 1972; (Reprinted). [Google Scholar]
- Eagling, E.M. Ocular damage after blunt trauma to the eye. Its relationship to the nature of the injury. Br. J. Ophthalmol. 1974, 58, 126–140. [Google Scholar] [CrossRef] [PubMed]
- Tönjum, A.M. Gonioscopy in traumatic hyphema. Acta Ophthalmol. 1966, 44, 650–664. [Google Scholar] [CrossRef] [PubMed]
- Mooney, D. Anterior chamber angle tears after non-perforating injury. Br. J. Ophthalmol. 1972, 56, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Blanton, F.M. Anterior chamber angle recession and secondary glaucoma: A study of the aftereffects of traumatic hyphemas. Arch. Ophthalmol. 1964, 72, 39. [Google Scholar] [CrossRef]
- Kaufman, J.H.; Tolpin, D.W. Glaucoma after traumatic angle recession a ten-year prospective study. Am. J. Ophthalmol. 1974, 78, 648–654. [Google Scholar] [CrossRef]
- Mooney, D. Angle recession and secondary glaucoma. Br. J. Ophthalmol. 1973, 57, 608–612. [Google Scholar] [CrossRef]
- Alper, M.G. Contusion angle deformity and glaucoma: Gonioscopic observations and clinical course. Arch. Ophthalmol. 1963, 69, 455. [Google Scholar] [CrossRef]
- Salmon, J.F.; Mermoud, A.; Ivey, A.; Swanevelder, S.A.; Hoffman, M. The detection of post-traumatic angle recession by gonioscopy in a population-based glaucoma survey. Ophthalmology 1994, 101, 1844–1850. [Google Scholar] [CrossRef] [PubMed]
- Sihota, R. Early predictors of traumatic glaucoma after closed globe injury: Trabecular pigmentation, widened angle recess, and higher baseline intraocular pressure. Arch. Ophthalmol. 2008, 126, 921. [Google Scholar] [CrossRef] [PubMed]
- European Glaucoma Society. Terminology and Guidelines for Glaucoma, 5th Edition. Br. J. Ophthalmol. 2021, 105 (Suppl. S1), 1–169. [Google Scholar] [CrossRef] [PubMed]
- Jindal, A.; Ctori, I.; Virgili, G.; Lucenteforte, E.; Lawrenson, J.G. Non-contact tests for identifying people at risk of primary angle closure glaucoma. Cochrane Database Syst. Rev. 2020, 2020. [Google Scholar] [CrossRef]
- Mowatt, L.; Chambers, C. Ocular Morbidity of traumatic hyphema in a Jamaican Hospital. Eur. J. Ophthalmol. 2010, 20, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Capão Filipe, J.A.; Barros, H.; Castro-Correia, J. Sports-related Ocular Injuries. Ophthalmology 1997, 104, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Shah, C.; Sen, P.; Tabani, S.; Prasad, K.; Peeush, P.; Jain, E. Clinical features of early-onset pediatric traumatic glaucoma and predictive factors for the need of early glaucoma surgery. Indian J. Ophthalmol. 2023, 71, 967. [Google Scholar] [CrossRef] [PubMed]
- Bai, H.Q.; Yao, L.; Wang, D.B.; Jin, R.; Wang, Y.X. Causes and Treatments of Traumatic Secondary Glaucoma. Eur. J. Ophthalmol. 2009, 19, 201–206. [Google Scholar] [CrossRef]
- Cheng, H.; Ye, W.; Zhang, S.; Xie, Y.; Gu, J.; Le, R.; Deng, Y.; Hu, C.; Zhao, Z.; Ke, Z.; et al. Clinical outcomes of penetrating canaloplasty in patients with traumatic angle recession glaucoma: A prospective interventional case series. Br. J. Ophthalmol. 2023, 107, 1092–1097. [Google Scholar] [CrossRef]
- Kaushik, J.; Parihar, J.K.S.; Singh, A.; Shetty, R.; Singhal, A.; Chaitanya, Y.V.K.; Jain, V.K.; Mathur, V. Evaluation of primary Ahmed Glaucoma valve implantation in post-traumatic angle recession glaucoma in Indian eyes. Int. Ophthalmol. 2022, 42, 817–827. [Google Scholar] [CrossRef]
- Senthil, S.; Dangeti, D.; Battula, M.; Rao, H.L.; Garudadri, C. Trabeculectomy with mitomycin-C in post-traumatic angle recession glaucoma in phakic eyes with no prior intraocular intervention. Semin. Ophthalmol. 2022, 37, 171–176. [Google Scholar] [CrossRef]
- Lesher, M.P. Corneal Edema, Hyphema, and angle recession after air bag inflation. Arch. Ophthalmol. 1993, 111, 1320. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.K.; Desai, U.R.; Raman, S.V. Incidence of ocular injuries in motor vehicle crash victims with concomitant air bag deployment. Ophthalmology 2002, 109, 2356–2358. [Google Scholar] [CrossRef]
- Qing, G.; Wang, N.; Wang, H. Pigment dispersion secondary to anterior chamber angle recession. Graefes Arch. Clin. Exp. Ophthalmol. 2012, 250, 779–780. [Google Scholar] [CrossRef] [PubMed]
- Bhavsar, A.R.; Chen, T.C.; Goldstein, D.A. Corneoscleral laceration associated with passenger-side airbag inflation. Br. J. Ophthalmol. 1997, 81, 513b. [Google Scholar] [CrossRef]
- Tseng, S.S.; Keys, M.P. Battered child syndrome simulating congenital glaucoma. Arch. Ophthalmol. 1976, 94, 839–840. [Google Scholar] [CrossRef]
- Palmer, E.; Lieberman, T.W.; Burns, S. Contusion angle deformity in prizefighters. Arch. Ophthalmol. 1976, 94, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Giovinazzo, V.J.; Yannuzzi, L.A.; Sorenson, J.A.; Delrowe, D.J.; Cambell, E.A. The ocular complications of boxing. Ophthalmology 1987, 94, 587–596. [Google Scholar] [CrossRef]


| Closed globe | Contusion: blunt trauma without laceration of sclera and/or cornea. |
| Lamellar laceration: partial thickness laceration of sclera and/or cornea. | |
| SOB *: foreign body embedded in the conjunctiva, cornea, or sclera without full thickness defect. | |
| Open globe | Rupture: blunt trauma with full-thickness laceration of sclera and/or cornea. |
| Penetration: full-thickness laceration of sclera and/or cornea due to a sharp object, without exit wound. | |
| IOFB **: foreign body retained after full-thickness laceration of sclera and/or cornea. | |
| Perforation: full-thickness laceration of sclera and/or cornea due to a sharp object, with an exit wound. | |
| Mixed injuries: a combination of the mechanisms above. |
| Post-traumatic glaucoma | |
| Early onset | Late onset |
| Trabeculitis/iritis | Angle recession |
| Trabecular disruption | Peripheral anterior synechiae |
| Hyphema | Ghost cell glaucoma |
| Massive choroidal hemorrhage | Lens-related * |
| Chemical injury | Delayed closure of cyclodialysis cleft |
| Epithelial downgrowth | |
| Retained intraocular foreign body | |
| Rhegmatogenous retinal detachment (Schwartze syndrome) | |
| Grade | Gonioscopy Description |
|---|---|
| Grade I Shallow angle tear | No definite ciliary cleft: ciliary band is darker and wider than in the other eye |
| Grade II Moderate angle tear | Definite ciliary cleft: the angle is deeper than that of the other eye due to a tear of the ciliary body |
| Grade III Deep angle tear | Deep fissure into the ciliary body: the apex of the fissure cannot be identified gonioscopically |
| Author | Angle Recession n (%) | Bilateral Angle Recession n (%) | Comment |
|---|---|---|---|
| Lesher, M.P. (1993) [77] | - | - | Case report; unilateral angle recession, associated to corneal edema and hyphema |
| Driver, P.J. (1994) [42] | - | - | Letter to editor; bilateral angle recession and hyphema |
| Michaeli Cohen, A. (1995) [43] | - | - | Letter to editor; bilateral angle recession, corneal contusion and hyphema |
| Ghafouri, A. (1997) [45] | 6 (15.4%) | 0 (0%) | Case series and review of the literature; 32 patients with airbag-related ocular injury |
| Stein, J.D. (1999) [24] | 11 (11.3%) | 2 (2.1%) | Review of the literature; 97 patients with airbag-related ocular injury |
| Pearlman, J.A. (2001) [11] | 11 (11%) | 2 (2%) | Review of the literature; 101 patients with airbag-related ocular injury |
| Alquraini, T.A. (2010) [44] | - | - | Case report, 14-year-old patient; bilateral angle recession, hyphema and corneal abrasion, left vitreous hemorrhage and macular edema |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iannucci, V.; Manni, P.; Alisi, L.; Mecarelli, G.; Lambiase, A.; Bruscolini, A. Bilateral Angle Recession and Chronic Post-Traumatic Glaucoma: A Review of the Literature and a Case Report. Life 2023, 13, 1814. https://doi.org/10.3390/life13091814
Iannucci V, Manni P, Alisi L, Mecarelli G, Lambiase A, Bruscolini A. Bilateral Angle Recession and Chronic Post-Traumatic Glaucoma: A Review of the Literature and a Case Report. Life. 2023; 13(9):1814. https://doi.org/10.3390/life13091814
Chicago/Turabian StyleIannucci, Valeria, Priscilla Manni, Ludovico Alisi, Giulia Mecarelli, Alessandro Lambiase, and Alice Bruscolini. 2023. "Bilateral Angle Recession and Chronic Post-Traumatic Glaucoma: A Review of the Literature and a Case Report" Life 13, no. 9: 1814. https://doi.org/10.3390/life13091814
APA StyleIannucci, V., Manni, P., Alisi, L., Mecarelli, G., Lambiase, A., & Bruscolini, A. (2023). Bilateral Angle Recession and Chronic Post-Traumatic Glaucoma: A Review of the Literature and a Case Report. Life, 13(9), 1814. https://doi.org/10.3390/life13091814





