Head-to-Head Comparison of FDG and Radiolabeled FAPI PET: A Systematic Review of the Literature
Abstract
:1. Introduction
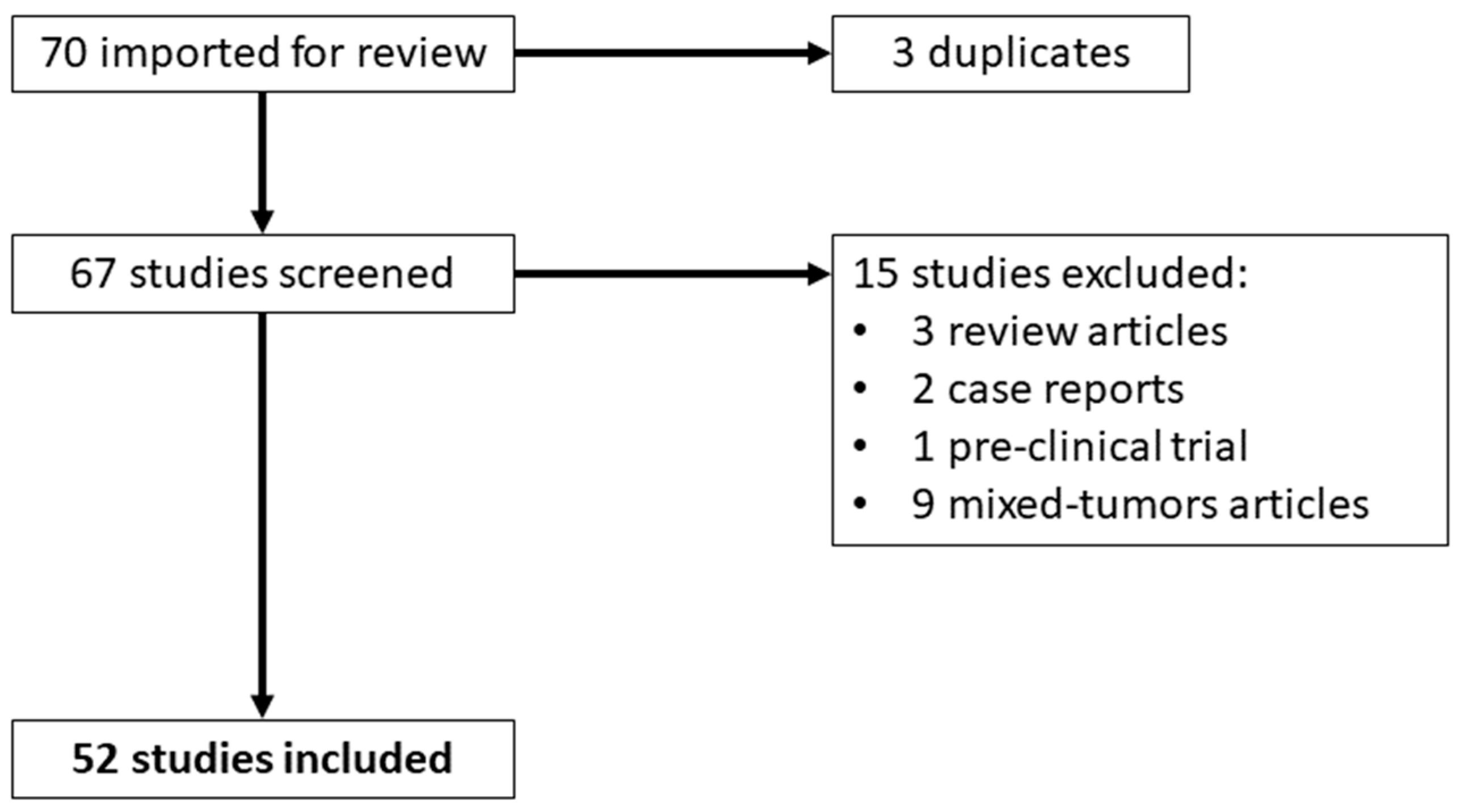
2. Materials and Methods
3. Results
3.1. Tumors with Low [18F]FDG Uptake
3.1.1. Thyroid Cancer
3.1.2. Liver and Biliary Tract Cancer
3.1.3. Peritoneal Carcinomatosis
3.1.4. Soft Tissue Sarcoma
3.2. Tumors with Variable [18F]FDG Uptake
3.2.1. Breast Cancer
3.2.2. Ovarian Cancer
3.2.3. Gastric Cancer
3.2.4. Multiple Myeloma
3.2.5. Gastrointestinal Stromal Tumor
3.2.6. Bladder Cancer
3.2.7. Pancreatic Cancer
3.3. Tumors with High [18F]FDG Uptake
3.3.1. Lung Cancer
3.3.2. Head and Neck Cancer
3.3.3. Esophageal Cancer
3.3.4. Colorectal Cancer
3.3.5. IgG4-Related Disease
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boellaard, R.; Delgado-Bolton, R.; Oyen, W.J.G.; Giammarile, F.; Tatsch, K.; Eschner, W.; Verzijlbergen, F.J.; Barrington, S.F.; Pike, L.C.; Weber, W.A.; et al. FDG PET/CT: EANM Procedure Guidelines for Tumour Imaging: Version 2.0. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 328–354. [Google Scholar] [CrossRef] [PubMed]
- Kawada, K.; Iwamoto, M.; Sakai, Y. Mechanisms Underlying 18F-Fluorodeoxyglucose Accumulation in Colorectal Cancer. World J. Radiol. 2016, 8, 880–886. [Google Scholar] [CrossRef] [PubMed]
- Pliszka, M.; Szablewski, L. Glucose Transporters as a Target for Anticancer Therapy. Cancers 2021, 13, 4184. [Google Scholar] [CrossRef] [PubMed]
- Treglia, G.; Sadeghi, R.; Del Sole, A.; Giovanella, L. Diagnostic Performance of PET/CT with Tracers Other than F-18-FDG in Oncology: An Evidence-Based Review. Clin. Transl. Oncol. 2014, 16, 770–775. [Google Scholar] [CrossRef]
- Becker, J.; Schwarzenböck, S.M.; Krause, B.J. FDG PET Hybrid Imaging. Recent Results Cancer Res. 2020, 216, 625–667. [Google Scholar] [CrossRef] [PubMed]
- Gomes Marin, J.F.; Nunes, R.F.; Coutinho, A.M.; Zaniboni, E.C.; Costa, L.B.; Barbosa, F.G.; Queiroz, M.A.; Cerri, G.G.; Buchpiguel, C.A. Theranostics in Nuclear Medicine: Emerging and Re-Emerging Integrated Imaging and Therapies in the Era of Precision Oncology. Radiographics 2020, 40, 1715–1740. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Hanahan, D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022, 12, 31–46. [Google Scholar] [CrossRef]
- Dvorak, H.F. Tumors: Wounds That Do Not Heal. Similarities between Tumor Stroma Generation and Wound Healing. N. Engl. J. Med. 1986, 315, 1650–1659. [Google Scholar] [CrossRef]
- Lasek, W. Cancer Immunoediting Hypothesis: History, Clinical Implications and Controversies. Cent. Eur. J. Immunol. 2022, 47, 168–174. [Google Scholar] [CrossRef]
- Dunn, G.P.; Bruce, A.T.; Ikeda, H.; Old, L.J.; Schreiber, R.D. Cancer Immunoediting: From Immunosurveillance to Tumor Escape. Nat. Immunol. 2002, 3, 991–998. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, R.D.; Old, L.J.; Smyth, M.J. Cancer Immunoediting: Integrating Immunity’s Roles in Cancer Suppression and Promotion. Science 2011, 331, 1565–1570. [Google Scholar] [CrossRef] [PubMed]
- Gilardi, L.; Airò Farulla, L.S.; Demirci, E.; Clerici, I.; Omodeo Salè, E.; Ceci, F. Imaging Cancer-Associated Fibroblasts (CAFs) with FAPi PET. Biomedicines 2022, 10, 523. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Han, C.; Wang, S.; Fang, P.; Ma, Z.; Xu, L.; Yin, R. Cancer-Associated Fibroblasts: An Emerging Target of Anti-Cancer Immunotherapy. J. Hematol. Oncol. 2019, 12, 86. [Google Scholar] [CrossRef]
- Kessler, L.; Ferdinandus, J.; Hirmas, N.; Zarrad, F.; Nader, M.; Kersting, D.; Weber, M.; Kazek, S.; Sraieb, M.; Hamacher, R.; et al. Pitfalls and Common Findings in 68Ga-FAPI PET: A Pictorial Analysis. J. Nucl. Med. 2022, 63, 890–896. [Google Scholar] [CrossRef]
- Kratochwil, C.; Flechsig, P.; Lindner, T.; Abderrahim, L.; Altmann, A.; Mier, W.; Adeberg, S.; Rathke, H.; Röhrich, M.; Winter, H.; et al. 68Ga-FAPI PET/CT: Tracer Uptake in 28 Different Kinds of Cancer. J. Nucl. Med. 2019, 60, 801–805. [Google Scholar] [CrossRef]
- Hamson, E.J.; Keane, F.M.; Tholen, S.; Schilling, O.; Gorrell, M.D. Understanding Fibroblast Activation Protein (FAP): Substrates, Activities, Expression and Targeting for Cancer Therapy. Proteom. Clin. Appl. 2014, 8, 454–463. [Google Scholar] [CrossRef]
- Yazbeck, R.; Jaenisch, S.E.; Abbott, C.A. Potential Disease Biomarkers: Dipeptidyl Peptidase 4 and Fibroblast Activation Protein. Protoplasma 2018, 255, 375–386. [Google Scholar] [CrossRef]
- Tillmanns, J.; Hoffmann, D.; Habbaba, Y.; Schmitto, J.D.; Sedding, D.; Fraccarollo, D.; Galuppo, P.; Bauersachs, J. Fibroblast Activation Protein Alpha Expression Identifies Activated Fibroblasts after Myocardial Infarction. J. Mol. Cell. Cardiol. 2015, 87, 194–203. [Google Scholar] [CrossRef]
- Backhaus, P.; Gierse, F.; Burg, M.C.; Büther, F.; Asmus, I.; Dorten, P.; Cufe, J.; Roll, W.; Neri, D.; Cazzamalli, S.; et al. Translational Imaging of the Fibroblast Activation Protein (FAP) Using the New Ligand [68Ga]Ga-OncoFAP-DOTAGA. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 1822–1832. [Google Scholar] [CrossRef]
- Fitzgerald, A.A.; Weiner, L.M. The Role of Fibroblast Activation Protein in Health and Malignancy. Cancer Metastasis Rev. 2020, 39, 783–803. [Google Scholar] [CrossRef] [PubMed]
- Xin, L.; Gao, J.; Zheng, Z.; Chen, Y.; Lv, S.; Zhao, Z.; Yu, C.; Yang, X.; Zhang, R. Fibroblast Activation Protein-α as a Target in the Bench-to-Bedside Diagnosis and Treatment of Tumors: A Narrative Review. Front. Oncol. 2021, 11, 648187. [Google Scholar] [CrossRef] [PubMed]
- Loktev, A.; Lindner, T.; Mier, W.; Debus, J.; Altmann, A.; Jäger, D.; Giesel, F.; Kratochwil, C.; Barthe, P.; Roumestand, C.; et al. A Tumor-Imaging Method Targeting Cancer-Associated Fibroblasts. J. Nucl. Med. 2018, 59, 1423–1429. [Google Scholar] [CrossRef] [PubMed]
- Loktev, A.; Lindner, T.; Burger, E.-M.; Altmann, A.; Giesel, F.; Kratochwil, C.; Debus, J.; Marmé, F.; Jäger, D.; Mier, W.; et al. Development of Fibroblast Activation Protein-Targeted Radiotracers with Improved Tumor Retention. J. Nucl. Med. 2019, 60, 1421–1429. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Dendl, K.; Cardinale, J.; Kratochwil, C.; Giesel, F.L.; Haberkorn, U. FAPI PET: Fibroblast Activation Protein Inhibitor Use in Oncologic and Nononcologic Disease. Radiology 2023, 306, e220749. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Crespo, A. Comparison of Gallium-68 and Fluorine-18 Imaging Characteristics in Positron Emission Tomography. Appl. Radiat. Isot. 2013, 76, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Laudicella, R.; Spataro, A.; Crocè, L.; Giacoppo, G.; Romano, D.; Davì, V.; Lopes, M.; Librando, M.; Nicocia, A.; Rappazzo, A.; et al. Preliminary Findings of the Role of FAPi in Prostate Cancer Theranostics. Diagnostics 2023, 13, 1175. [Google Scholar] [CrossRef] [PubMed]
- Mu, X.; Huang, X.; Jiang, Z.; Li, M.; Jia, L.; Lv, Z.; Fu, W.; Mao, J. [18F]FAPI-42 PET/CT in Differentiated Thyroid Cancer: Diagnostic Performance, Uptake Values, and Comparison with 2-[18F]FDG PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2023, 50, 1205–1215. [Google Scholar] [CrossRef]
- Fu, H.; Wu, J.; Huang, J.; Sun, L.; Wu, H.; Guo, W.; Qiu, S.; Chen, H. 68Ga Fibroblast Activation Protein Inhibitor PET/CT in the Detection of Metastatic Thyroid Cancer: Comparison with 18F-FDG PET/CT. Radiology 2022, 304, 397–405. [Google Scholar] [CrossRef]
- Rajaraman, V.; Meenakshi, L.A.; Selvaraj, A.J.; Pottakkat, B.; Halanaik, D. Role of 68Ga-FAPI PET/CT in Assessing Hepatobiliary Malignancies: A Prospective Pilot Study. Clin. Nucl. Med. 2023, 48, e281–e288. [Google Scholar] [CrossRef]
- Pabst, K.M.; Trajkovic-Arsic, M.; Cheung, P.F.Y.; Ballke, S.; Steiger, K.; Bartel, T.; Schaarschmidt, B.M.; Milosevic, A.; Seifert, R.; Nader, M.; et al. Superior Tumor Detection for 68Ga-FAPI-46 Versus 18F-FDG PET/CT and Conventional CT in Patients with Cholangiocarcinoma. J. Nucl. Med. 2023, 64, 1049–1055. [Google Scholar] [CrossRef]
- Zhang, J.; He, Q.; Jiang, S.; Li, M.; Xue, H.; Zhang, D.; Li, S.; Peng, H.; Liang, J.; Liu, Z.; et al. [18F]FAPI PET/CT in the Evaluation of Focal Liver Lesions with [18F]FDG Non-Avidity. Eur. J. Nucl. Med. Mol. Imaging 2023, 50, 937–950. [Google Scholar] [CrossRef]
- Wang, H.; Zhu, W.; Ren, S.; Kong, Y.; Huang, Q.; Zhao, J.; Guan, Y.; Jia, H.; Chen, J.; Lu, L.; et al. 68Ga-FAPI-04 Versus 18F-FDG PET/CT in the Detection of Hepatocellular Carcinoma. Front. Oncol. 2021, 11, 693640. [Google Scholar] [CrossRef] [PubMed]
- Siripongsatian, D.; Promteangtrong, C.; Kunawudhi, A.; Kiatkittikul, P.; Boonkawin, N.; Chinnanthachai, C.; Jantarato, A.; Chotipanich, C. Comparisons of Quantitative Parameters of Ga-68-Labelled Fibroblast Activating Protein Inhibitor (FAPI) PET/CT and [18F]F-FDG PET/CT in Patients with Liver Malignancies. Mol. Imaging Biol. 2022, 24, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Pang, Y.; Yao, L.; Zhao, L.; Fan, C.; Ke, J.; Guo, P.; Hao, B.; Fu, H.; Xie, C.; et al. Imaging Fibroblast Activation Protein in Liver Cancer: A Single-Center Post Hoc Retrospective Analysis to Compare [68Ga]Ga-FAPI-04 PET/CT versus MRI and [18F]-FDG PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1604–1617. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Xing, H.; Yang, X.; Li, F.; Yao, S.; Congwei, J.; Zhao, H.; Hacker, M.; Huo, L.; Li, X. Comparison of PET Imaging of Activated Fibroblasts and 18F-FDG for Diagnosis of Primary Hepatic Tumours: A Prospective Pilot Study. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1593–1603. [Google Scholar] [CrossRef]
- Lan, L.; Zhang, S.; Xu, T.; Liu, H.; Wang, W.; Feng, Y.; Wang, L.; Chen, Y.; Qiu, L. Prospective Comparison of 68Ga-FAPI versus 18F-FDG PET/CT for Tumor Staging in Biliary Tract Cancers. Radiology 2022, 304, 648–657. [Google Scholar] [CrossRef]
- Zhao, L.; Pang, Y.; Luo, Z.; Fu, K.; Yang, T.; Zhao, L.; Sun, L.; Wu, H.; Lin, Q.; Chen, H. Role of [68Ga]Ga-DOTA-FAPI-04 PET/CT in the Evaluation of Peritoneal Carcinomatosis and Comparison with [18F]-FDG PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1944–1955. [Google Scholar] [CrossRef]
- Güzel, Y.; Kaplan, İ. Comparison of 68GA-FAPI-04 PET/CT and 18F-FDG PET/CT Findings in Peritonitis Carcinomatosa Cases. Hell. J. Nucl. Med. 2023, 26, 26–34. [Google Scholar] [CrossRef]
- Elboga, U.; Sahin, E.; Kus, T.; Cayirli, Y.B.; Aktas, G.; Okuyan, M.; Cinkir, H.Y.; Teker, F.; Sever, O.N.; Aytekin, A.; et al. Comparison of 68Ga-FAPI PET/CT and 18FDG PET/CT Modalities in Gastrointestinal System Malignancies with Peritoneal Involvement. Mol. Imaging Biol. 2022, 24, 789–797. [Google Scholar] [CrossRef]
- Gu, B.; Liu, X.; Wang, S.; Xu, X.; Liu, X.; Hu, S.; Yan, W.; Luo, Z.; Song, S. Head-to-Head Evaluation of [18F]FDG and [68 Ga]Ga-DOTA-FAPI-04 PET/CT in Recurrent Soft Tissue Sarcoma. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2889–2901. [Google Scholar] [CrossRef] [PubMed]
- Ballal, S.; Yadav, M.P.; Roesch, F.; Wakade, N.; Raju, S.; Sheokand, P.; Mishra, P.; Moon, E.S.; Tripathi, M.; Martin, M.; et al. Head-to-Head Comparison between [68Ga]Ga-DOTA.SA.FAPi and [18F]F-FDG PET/CT Imaging in Patients with Breast Cancer. Pharmaceuticals 2023, 16, 521. [Google Scholar] [CrossRef] [PubMed]
- Kömek, H.; Can, C.; Güzel, Y.; Oruç, Z.; Gündoğan, C.; Yildirim, Ö.A.; Kaplan, İ.; Erdur, E.; Yıldırım, M.S.; Çakabay, B. 68Ga-FAPI-04 PET/CT, a New Step in Breast Cancer Imaging: A Comparative Pilot Study with the 18F-FDG PET/CT. Ann. Nucl. Med. 2021, 35, 744–752. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Lin, J.; Zhu, Y.; Chen, Y.; Zhang, J.; Chen, X.; Miao, W. 68Ga-FAPI Versus 18F-FDG PET/CT in Evaluating Newly Diagnosed Breast Cancer Patients: A Head-to-Head Comparative Study. Clin. Nucl. Med. 2023, 48, e104–e109. [Google Scholar] [CrossRef] [PubMed]
- Elboga, U.; Sahin, E.; Kus, T.; Cayirli, Y.B.; Aktas, G.; Uzun, E.; Cinkir, H.Y.; Teker, F.; Sever, O.N.; Aytekin, A.; et al. Superiority of 68Ga-FAPI PET/CT Scan in Detecting Additional Lesions Compared to 18FDG PET/CT Scan in Breast Cancer. Ann. Nucl. Med. 2021, 35, 1321–1331. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; Liu, L.; Feng, Y.; Wang, L.; Chen, Y. Comparison of 68 Ga-FAPI-04 and Fluorine-18-Fluorodeoxyglucose PET/Computed Tomography in the Detection of Ovarian Malignancies. Nucl. Med. Commun. 2023, 44, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Feng, Z.; Xu, X.; Ge, H.; Ju, X.; Wu, X.; Song, S. Head-to-Head Comparison of [18F]-FDG and [68 Ga]-DOTA-FAPI-04 PET/CT for Radiological Evaluation of Platinum-Sensitive Recurrent Ovarian Cancer. Eur. J. Nucl. Med. Mol. Imaging 2023, 50, 1521–1531. [Google Scholar] [CrossRef]
- Kuten, J.; Levine, C.; Shamni, O.; Pelles, S.; Wolf, I.; Lahat, G.; Mishani, E.; Even-Sapir, E. Head-to-Head Comparison of [68Ga]Ga-FAPI-04 and [18F]-FDG PET/CT in Evaluating the Extent of Disease in Gastric Adenocarcinoma. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 743–750. [Google Scholar] [CrossRef]
- Gündoğan, C.; Kömek, H.; Can, C.; Yildirim, Ö.A.; Kaplan, İ.; Erdur, E.; Poyraz, K.; Güzel, Y.; Oruç, Z.; Çakabay, B. Comparison of 18F-FDG PET/CT and 68Ga-FAPI-04 PET/CT in the Staging and Restaging of Gastric Adenocarcinoma. Nucl. Med. Commun. 2022, 43, 64–72. [Google Scholar] [CrossRef]
- Lin, R.; Lin, Z.; Chen, Z.; Zheng, S.; Zhang, J.; Zang, J.; Miao, W. [68Ga]Ga-DOTA-FAPI-04 PET/CT in the Evaluation of Gastric Cancer: Comparison with [18F]FDG PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2960–2971. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, W.; Xu, T.; Ding, H.; Li, Y.; Liu, H.; Huang, Y.; Liu, L.; Du, T.; Zhao, Y.; et al. Comparison of Diagnostic Efficacy of [68Ga]Ga-FAPI-04 and [18F]FDG PET/CT for Staging and Restaging of Gastric Cancer. Front. Oncol. 2022, 12, 925100. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Pang, Y.; Li, J.; Kang, F.; Xu, W.; Meng, T.; Shang, Q.; Zhao, J.; Guan, Y.; Wu, H.; et al. Comparison of [68Ga]Ga-FAPI and [18F]FDG Uptake in Patients with Gastric Signet-Ring-Cell Carcinoma: A Multicenter Retrospective Study. Eur. Radiol. 2023, 33, 1329–1341. [Google Scholar] [CrossRef] [PubMed]
- Jiang, D.; Chen, X.; You, Z.; Wang, H.; Zhang, X.; Li, X.; Ren, S.; Huang, Q.; Hua, F.; Guan, Y.; et al. Comparison of [68 Ga]Ga-FAPI-04 and [18F]-FDG for the Detection of Primary and Metastatic Lesions in Patients with Gastric Cancer: A Bicentric Retrospective Study. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.; Shao, F.; Gai, Y.; Liu, Q.; Ruan, W.; Liu, F.; Hu, F.; Lan, X. 68Ga-DOTA-FAPI-04 PET/MR in the Evaluation of Gastric Carcinomas: Comparison with 18F-FDG PET/CT. J. Nucl. Med. 2022, 63, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Miao, Y.; Feng, R.; Guo, R.; Huang, X.; Hai, W.; Li, J.; Yu, T.; Qu, Q.; Zhang, M.; Shangguan, C.; et al. Utility of [68Ga]FAPI-04 and [18F]FDG Dual-Tracer PET/CT in the Initial Evaluation of Gastric Cancer. Eur. Radiol. 2023, 33, 4355–4366. [Google Scholar] [CrossRef]
- Elboga, U.; Sahin, E.; Cayirli, Y.B.; Okuyan, M.; Aktas, G.; Haydaroglu Sahin, H.; Dogan, I.; Kus, T.; Akkurd, D.M.; Cimen, U.; et al. Comparison of [68Ga]-FAPI PET/CT and [18F]-FDG PET/CT in Multiple Myeloma: Clinical Experience. Tomography 2022, 8, 293–302. [Google Scholar] [CrossRef]
- Wu, C.; Zhang, X.; Zeng, Y.; Wu, R.; Ding, L.; Xia, Y.; Chen, Z.; Zhang, X.; Wang, X. [18F]FAPI-42 PET/CT versus [18F]FDG PET/CT for Imaging of Recurrent or Metastatic Gastrointestinal Stromal Tumors. Eur. J. Nucl. Med. Mol. Imaging 2022, 50, 194–204. [Google Scholar] [CrossRef]
- Novruzov, E.; Dendl, K.; Ndlovu, H.; Choyke, P.L.; Dabir, M.; Beu, M.; Novruzov, F.; Mehdi, E.; Guliyev, F.; Koerber, S.A.; et al. Head-to-Head Intra-Individual Comparison of [68Ga]-FAPI and [18F]-FDG PET/CT in Patients with Bladder Cancer. Mol. Imaging Biol. 2022, 24, 651–658. [Google Scholar] [CrossRef]
- Liu, Q.; Shi, S.; Liu, S.; Xu, X.; Hu, S.; Zhang, J.; Wang, C.; Yu, X.; Song, S. The Added Value of [68Ga]Ga-DOTA-FAPI-04 PET/CT in Pancreatic Cancer: A Comparison to [18F]F-FDG. Eur. Radiol. 2023, 33, 5007–5016. [Google Scholar] [CrossRef]
- Zhang, Z.; Jia, G.; Pan, G.; Cao, K.; Yang, Q.; Meng, H.; Yang, J.; Zhang, L.; Wang, T.; Cheng, C.; et al. Comparison of the Diagnostic Efficacy of 68 Ga-FAPI-04 PET/MR and 18F-FDG PET/CT in Patients with Pancreatic Cancer. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2877–2888. [Google Scholar] [CrossRef]
- Wang, L.; Tang, G.; Hu, K.; Liu, X.; Zhou, W.; Li, H.; Huang, S.; Han, Y.; Chen, L.; Zhong, J.; et al. Comparison of 68Ga-FAPI and 18F-FDG PET/CT in the Evaluation of Advanced Lung Cancer. Radiology 2022, 303, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Can, C.; Kepenek, F.; Kömek, H.; Gündoğan, C.; Kaplan, İ.; Taşdemir, B.; Güzel, Y.; Agüloğlu, N.; Karaoğlan, H. Comparison of 18 F-FDG PET/CT and 68 Ga-FAPI-04 PET/CT in Patients with Non-Small Cell Lung Cancer. Nucl. Med. Commun. 2022, 43, 1084–1091. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Wang, S.; Xu, X.; Meng, X.; Zhang, H.; Zhang, A.; Song, Y.; Zhu, H.; Yang, Z.; Li, N. Higher Accuracy of [68 Ga]Ga-DOTA-FAPI-04 PET/CT Comparing with 2-[18F]FDG PET/CT in Clinical Staging of NSCLC. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2983–2993. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Deng, H.; Zhong, H.; Wang, T.; Rao, Z.; Wang, Y.; Chen, Y.; Zhang, C. Comparison of 68Ga-FAPI and 18F-FDG PET/CT in the Evaluation of Patients With Newly Diagnosed Non-Small Cell Lung Cancer. Front. Oncol. 2022, 12, 924223. [Google Scholar] [CrossRef]
- Linz, C.; Brands, R.C.; Kertels, O.; Dierks, A.; Brumberg, J.; Gerhard-Hartmann, E.; Hartmann, S.; Schirbel, A.; Serfling, S.; Zhi, Y.; et al. Targeting Fibroblast Activation Protein in Newly Diagnosed Squamous Cell Carcinoma of the Oral Cavity—Initial Experience and Comparison to [18F]FDG PET/CT and MRI. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 3951–3960. [Google Scholar] [CrossRef]
- Promteangtrong, C.; Siripongsatian, D.; Jantarato, A.; Kunawudhi, A.; Kiatkittikul, P.; Yaset, S.; Boonkawin, N.; Chotipanich, C. Head-to-Head Comparison of 68Ga-FAPI-46 and 18F-FDG PET/CT for Evaluation of Head and Neck Squamous Cell Carcinoma: A Single-Center Exploratory Study. J. Nucl. Med. 2022, 63, 1155–1161. [Google Scholar] [CrossRef]
- Chen, S.; Chen, Z.; Zou, G.; Zheng, S.; Zheng, K.; Zhang, J.; Huang, C.; Yao, S.; Miao, W. Accurate Preoperative Staging with [68Ga]Ga-FAPI PET/CT for Patients with Oral Squamous Cell Carcinoma: A Comparison to 2-[18F]FDG PET/CT. Eur. Radiol. 2022, 32, 6070–6079. [Google Scholar] [CrossRef]
- Jiang, Y.; Wen, B.; Li, C.; Tian, Y.; Xiao, Z.; Xu, K.; Xing, D.; Yu, Z.; Huang, J.; Jia, J.; et al. The Performance of 68Ga-FAPI-04 PET/CT in Head and Neck Squamous Cell Carcinoma: A Prospective Comparison with 18F-FDG PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2023, 50, 2114–2126. [Google Scholar] [CrossRef]
- Ding, H.; Liang, J.; Qiu, L.; Xu, T.; Cai, L.; Wan, Q.; Wang, L.; Liu, Y.; Chen, Y. Prospective Comparison of 68Ga-FAPI-04 and 18F-FDG PET/CT for Tumor Staging in Nasopharyngeal Carcinoma. Front. Oncol. 2022, 12, 1047010. [Google Scholar] [CrossRef]
- Zheng, J.; Liu, F.; Lin, K.; Zhang, L.; Huang, N.; Zheng, W.; Zhang, J.; Yao, S.; Miao, W. [68Ga]Ga-FAPI PET/CT Improves the T Staging of Patients with Newly Diagnosed Nasopharyngeal Carcinoma: A Comparison with [18F]F-FDG. Mol. Imaging Biol. 2022, 24, 973–985. [Google Scholar] [CrossRef]
- Qin, C.; Liu, F.; Huang, J.; Ruan, W.; Liu, Q.; Gai, Y.; Hu, F.; Jiang, D.; Hu, Y.; Yang, K.; et al. A Head-to-Head Comparison of 68Ga-DOTA-FAPI-04 and 18F-FDG PET/MR in Patients with Nasopharyngeal Carcinoma: A Prospective Study. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 3228–3237. [Google Scholar] [CrossRef] [PubMed]
- Wegen, S.; van Heek, L.; Linde, P.; Claus, K.; Akuamoa-Boateng, D.; Baues, C.; Sharma, S.J.; Schomäcker, K.; Fischer, T.; Roth, K.S.; et al. Head-to-Head Comparison of [68 Ga]Ga-FAPI-46-PET/CT and [18F]F-FDG-PET/CT for Radiotherapy Planning in Head and Neck Cancer. Mol. Imaging Biol. 2022, 24, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Serfling, S.; Zhi, Y.; Schirbel, A.; Lindner, T.; Meyer, T.; Gerhard-Hartmann, E.; Lapa, C.; Hagen, R.; Hackenberg, S.; Buck, A.K.; et al. Improved Cancer Detection in Waldeyer’s Tonsillar Ring by 68Ga-FAPI PET/CT Imaging. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1178–1187. [Google Scholar] [CrossRef]
- Gu, B.; Xu, X.; Zhang, J.; Ou, X.; Xia, Z.; Guan, Q.; Hu, S.; Yang, Z.; Song, S. The Added Value of 68Ga-FAPI PET/CT in Patients with Head and Neck Cancer of Unknown Primary with 18F-FDG-Negative Findings. J. Nucl. Med. 2022, 63, 875–881. [Google Scholar] [CrossRef]
- Liu, Q.; Shi, S.; Xu, X.; Yu, X.; Song, S. The Superiority of [68Ga]-FAPI-04 over [18F]-FDG PET/CT in Imaging Metastatic Esophageal Squamous Cell Carcinoma. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1248–1249. [Google Scholar] [CrossRef]
- Liu, H.; Hu, Z.; Yang, X.; Dai, T.; Chen, Y. Comparison of [68Ga]Ga-DOTA-FAPI-04 and [18F]FDG Uptake in Esophageal Cancer. Front. Oncol. 2022, 12, 875081. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Li, Y.; Wang, S.; Zhang, Y.; Chen, X.; Wei, M.; Zhu, H.; Wu, A.; Yang, Z.; Wang, X. Diagnostic Value of [68Ga]Ga-FAPI-04 in Patients with Colorectal Cancer in Comparison with [18F]F-FDG PET/CT. Front. Oncol. 2022, 12, 1087792. [Google Scholar] [CrossRef] [PubMed]
- Kömek, H.; Can, C.; Kaplan, İ.; Gündoğan, C.; Kepenek, F.; Karaoglan, H.; Demirkıran, A.; Ebinç, S.; Güzel, Y.; Gündeş, E. Comparison of [68 Ga]Ga-DOTA-FAPI-04 PET/CT and [18F]FDG PET/CT in Colorectal Cancer. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 3898–3909. [Google Scholar] [CrossRef]
- Luo, Y.; Pan, Q.; Zhang, W. IgG4-Related Disease Revealed by 68Ga-FAPI and 18F-FDG PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 2625–2626. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Cabanillas, M.E.; McFadden, D.G.; Durante, C. Thyroid Cancer. Lancet 2016, 388, 2783–2795. [Google Scholar] [CrossRef]
- Aashiq, M.; Silverman, D.A.; Na’ara, S.; Takahashi, H.; Amit, M. Radioiodine-Refractory Thyroid Cancer: Molecular Basis of Redifferentiation Therapies, Management, and Novel Therapies. Cancers 2019, 11, 1382. [Google Scholar] [CrossRef] [PubMed]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed]
- Manohar, P.M.; Beesley, L.J.; Bellile, E.L.; Worden, F.P.; Avram, A.M. Prognostic Value of FDG-PET/CT Metabolic Parameters in Metastatic Radioiodine-Refractory Differentiated Thyroid Cancer. Clin. Nucl. Med. 2018, 43, 641–647. [Google Scholar] [CrossRef]
- Ballal, S.; Yadav, M.P.; Moon, E.S.; Roesch, F.; Kumari, S.; Agarwal, S.; Tripathi, M.; Sahoo, R.K.; Mangu, B.S.; Tupalli, A.; et al. Novel Fibroblast Activation Protein Inhibitor-Based Targeted Theranostics for Radioiodine-Refractory Differentiated Thyroid Cancer Patients: A Pilot Study. Thyroid 2022, 32, 65–77. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zheng, S.; Zhang, J.; Yao, S.; Miao, W. Pleural Metastasis of Papillary Thyroid Cancer Depicted by 68Ga-FAPI PET/CT. Clin. Nucl. Med. 2022, 47, 467–468. [Google Scholar] [CrossRef] [PubMed]
- Fu, H.; Fu, J.; Huang, J.; Su, X.; Chen, H. 68Ga-FAPI PET/CT in Thyroid Cancer With Thyroglobulin Elevation and Negative Iodine Scintigraphy. Clin. Nucl. Med. 2021, 46, 427–430. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zheng, S.; Zhang, J.; Yao, S.; Miao, W. 68Ga-DOTA-FAPI-04 PET/CT Imaging in Radioiodine-Refractory Differentiated Thyroid Cancer (RR-DTC) Patients. Ann. Nucl. Med. 2022, 36, 610–622. [Google Scholar] [CrossRef]
- Forner, A.; Reig, M.; Bruix, J. Hepatocellular Carcinoma. Lancet 2018, 391, 1301–1314. [Google Scholar] [CrossRef]
- Banales, J.M.; Marin, J.J.G.; Lamarca, A.; Rodrigues, P.M.; Khan, S.A.; Roberts, L.R.; Cardinale, V.; Carpino, G.; Andersen, J.B.; Braconi, C.; et al. Cholangiocarcinoma 2020: The next Horizon in Mechanisms and Management. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 557–588. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. Electronic address: Easloffice@easloffice.eu; European Association for the Study of the Liver EASL Clinical Practice Guidelines: Management of Hepatocellular Carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed]
- Boulter, L.; Bullock, E.; Mabruk, Z.; Brunton, V.G. The Fibrotic and Immune Microenvironments as Targetable Drivers of Metastasis. Br. J. Cancer 2021, 124, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Şahin, E.; Elboğa, U.; Çelen, Y.Z.; Sever, Ö.N.; Çayırlı, Y.B.; Çimen, U. Comparison of 68Ga-DOTA-FAPI and 18FDG PET/CT Imaging Modalities in the Detection of Liver Metastases in Patients with Gastrointestinal System Cancer. Eur. J. Radiol. 2021, 142, 109867. [Google Scholar] [CrossRef]
- Patel, C.M.; Sahdev, A.; Reznek, R.H. CT, MRI and PET Imaging in Peritoneal Malignancy. Cancer Imaging 2011, 11, 123–139. [Google Scholar] [CrossRef] [PubMed]
- Benz, M.R.; Crompton, J.G.; Harder, D. PET/CT Variants and Pitfalls in Bone and Soft Tissue Sarcoma. Semin. Nucl. Med. 2021, 51, 584–592. [Google Scholar] [CrossRef]
- Noebauer-Huhmann, I.M.; Weber, M.-A.; Lalam, R.K.; Trattnig, S.; Bohndorf, K.; Vanhoenacker, F.; Tagliafico, A.; van Rijswijk, C.; Vilanova, J.C.; Afonso, P.D.; et al. Soft Tissue Tumors in Adults: ESSR-Approved Guidelines for Diagnostic Imaging. Semin. Musculoskelet. Radiol. 2015, 19, 475–482. [Google Scholar] [CrossRef]
- Salaün, P.-Y.; Abgral, R.; Malard, O.; Querellou-Lefranc, S.; Quere, G.; Wartski, M.; Coriat, R.; Hindie, E.; Taieb, D.; Tabarin, A.; et al. Good Clinical Practice Recommendations for the Use of PET/CT in Oncology. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 28–50. [Google Scholar] [CrossRef]
- Dohi, O.; Ohtani, H.; Hatori, M.; Sato, E.; Hosaka, M.; Nagura, H.; Itoi, E.; Kokubun, S. Histogenesis-Specific Expression of Fibroblast Activation Protein and Dipeptidylpeptidase-IV in Human Bone and Soft Tissue Tumours. Histopathology 2009, 55, 432–440. [Google Scholar] [CrossRef]
- Evangelista, L.; Filippi, L.; Schillaci, O. What Radiolabeled FAPI Pet Can Add in Breast Cancer? A Systematic Review from Literature. Ann. Nucl. Med. 2023, 37, 442–450. [Google Scholar] [CrossRef]
- Huang, Y.; Simms, A.E.; Mazur, A.; Wang, S.; León, N.R.; Jones, B.; Aziz, N.; Kelly, T. Fibroblast Activation Protein-α Promotes Tumor Growth and Invasion of Breast Cancer Cells through Non-Enzymatic Functions. Clin. Exp. Metastasis 2011, 28, 567–579. [Google Scholar] [CrossRef]
- Bosch, K.D.; Chicklore, S.; Cook, G.J.; Davies, A.R.; Kelly, M.; Gossage, J.A.; Baker, C.R. Staging FDG PET-CT Changes Management in Patients with Gastric Adenocarcinoma Who Are Eligible for Radical Treatment. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Capobianco, A.; Cottone, L.; Monno, A.; Manfredi, A.A.; Rovere-Querini, P. The Peritoneum: Healing, Immunity, and Diseases. J. Pathol. 2017, 243, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Zamagni, E.; Tacchetti, P.; Cavo, M. Imaging in Multiple Myeloma: How? When? Blood 2019, 133, 644–651. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.-H.; Kwon, S.Y.; Min, J.-J.; Bom, H.-S.; Ahn, S.-Y.; Jung, S.-Y.; Lee, S.-S.; Park, M.-R.; Yang, D.-H.; Ahn, J.-S.; et al. 18F-FDG PET/CT Is Useful for Determining Survival Outcomes of Patients with Multiple Myeloma Classified as Stage II and III with the Revised International Staging System. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Zhong, X.; Diao, W.; Zhao, C.; Jia, Z. Fluorodeoxyglucose-Avid Focal Lesions and Extramedullary Disease on 18F-FDG PET/Computed Tomography Predict the Outcomes of Newly Diagnosed Symptomatic Multiple Myeloma Patients. Nucl. Med. Commun. 2020, 41, 950–958. [Google Scholar] [CrossRef]
- Rasche, L.; Angtuaco, E.; McDonald, J.E.; Buros, A.; Stein, C.; Pawlyn, C.; Thanendrarajan, S.; Schinke, C.; Samant, R.; Yaccoby, S.; et al. Low Expression of Hexokinase-2 Is Associated with False-Negative FDG-Positron Emission Tomography in Multiple Myeloma. Blood 2017, 130, 30–34. [Google Scholar] [CrossRef]
- Blay, J.-Y.; Kang, Y.-K.; Nishida, T.; von Mehren, M. Gastrointestinal Stromal Tumours. Nat. Rev. Dis. Primers 2021, 7, 22. [Google Scholar] [CrossRef]
- Alessandrino, F.; Tirumani, S.H.; Jagannathan, J.P.; Ramaiya, N.H. Imaging Surveillance of Gastrointestinal Stromal Tumour: Current Recommendation by National Comprehensive Cancer Network and European Society of Medical Oncology-European Reference Network for Rare Adult Solid Cancers. Clin. Radiol. 2019, 74, 746–755. [Google Scholar] [CrossRef]
- Revheim, M.-E.; Hole, K.H.; Mo, T.; Bruland, Ø.S.; Reitan, E.; Julsrud, L.; Seierstad, T. Multimodal Functional Imaging for Early Response Assessment in Patients with Gastrointestinal Stromal Tumor Treated with Tyrosine Kinase Inhibitors. Acta Radiol. 2022, 63, 995–1004. [Google Scholar] [CrossRef]
- Hahn, S.; Bauer, S.; Heusner, T.A.; Ebeling, P.; Hamami, M.E.; Stahl, A.; Forsting, M.; Bockisch, A.; Antoch, G. Postoperative FDG-PET/CT Staging in GIST: Is There a Benefit Following R0 Resection? Eur. J. Radiol. 2011, 80, 670–674. [Google Scholar] [CrossRef]
- Choi, H.; Charnsangavej, C.; de Castro Faria, S.; Tamm, E.P.; Benjamin, R.S.; Johnson, M.M.; Macapinlac, H.A.; Podoloff, D.A. CT Evaluation of the Response of Gastrointestinal Stromal Tumors after Imatinib Mesylate Treatment: A Quantitative Analysis Correlated with FDG PET Findings. AJR Am. J. Roentgenol. 2004, 183, 1619–1628. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.; Tang, C.-M.; Banerjee, S.; Yebra, M.; Noh, S.; Burgoyne, A.M.; la Torre, J.D.; De Siena, M.; Liu, M.; Klug, L.R.; et al. Cancer-Associated Fibroblast Secretion of PDGFC Promotes Gastrointestinal Stromal Tumor Growth and Metastasis. Oncogene 2021, 40, 1957–1973. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.; Tang, C.-M.; Banerjee, S.; Delgado, A.L.; Yebra, M.; Davis, J.; Sicklick, J.K. TGF-Β1-Mediated Transition of Resident Fibroblasts to Cancer-Associated Fibroblasts Promotes Cancer Metastasis in Gastrointestinal Stromal Tumor. Oncogenesis 2021, 10, 13. [Google Scholar] [CrossRef]
- Girard, A.; Vila Reyes, H.; Shaish, H.; Grellier, J.-F.; Dercle, L.; Salaün, P.-Y.; Delcroix, O.; Rouanne, M. The Role of 18F-FDG PET/CT in Guiding Precision Medicine for Invasive Bladder Carcinoma. Front. Oncol. 2020, 10, 565086. [Google Scholar] [CrossRef] [PubMed]
- Galgano, S.J.; Porter, K.K.; Burgan, C.; Rais-Bahrami, S. The Role of Imaging in Bladder Cancer Diagnosis and Staging. Diagnostics 2020, 10, 703. [Google Scholar] [CrossRef] [PubMed]
- Mezheyeuski, A.; Segersten, U.; Leiss, L.W.; Malmström, P.-U.; Hatina, J.; Östman, A.; Strell, C. Fibroblasts in Urothelial Bladder Cancer Define Stroma Phenotypes That Are Associated with Clinical Outcome. Sci. Rep. 2020, 10, 281. [Google Scholar] [CrossRef]
- Tempero, M.A. NCCN Guidelines Updates: Pancreatic Cancer. J. Natl. Compr. Cancer Netw. 2019, 17, 603–605. [Google Scholar] [CrossRef]
- Daamen, L.A.; Groot, V.P.; Goense, L.; Wessels, F.J.; Borel Rinkes, I.H.; Intven, M.P.W.; van Santvoort, H.C.; Molenaar, I.Q. The Diagnostic Performance of CT versus FDG PET-CT for the Detection of Recurrent Pancreatic Cancer: A Systematic Review and Meta-Analysis. Eur. J. Radiol. 2018, 106, 128–136. [Google Scholar] [CrossRef]
- Wartski, M.; Sauvanet, A. 18F-FDG PET/CT in Pancreatic Adenocarcinoma: A Role at Initial Imaging Staging? Diagn. Interv. Imaging 2019, 100, 735–741. [Google Scholar] [CrossRef]
- Chien, C.-R.; Liang, J.-A.; Chen, J.-H.; Wang, H.-N.; Lin, C.-C.; Chen, C.-Y.; Wang, P.-H.; Kao, C.-H.; Yeh, J.-J. [(18)F]Fluorodeoxyglucose-Positron Emission Tomography Screening for Lung Cancer: A Systematic Review and Meta-Analysis. Cancer Imaging 2013, 13, 458–465. [Google Scholar] [CrossRef]
- Iwano, S.; Ito, S.; Tsuchiya, K.; Kato, K.; Naganawa, S. What Causes False-Negative PET Findings for Solid-Type Lung Cancer? Lung Cancer 2013, 79, 132–136. [Google Scholar] [CrossRef]
- Feng, M.; Yang, X.; Ma, Q.; He, Y. Retrospective Analysis for the False Positive Diagnosis of PET-CT Scan in Lung Cancer Patients. Medicine 2017, 96, e7415. [Google Scholar] [CrossRef]
- Ballal, S.; Yadav, M.P.; Moon, E.S.; Kramer, V.S.; Roesch, F.; Kumari, S.; Tripathi, M.; ArunRaj, S.T.; Sarswat, S.; Bal, C. Biodistribution, Pharmacokinetics, Dosimetry of [68Ga]Ga-DOTA.SA.FAPi, and the Head-to-Head Comparison with [18F]F-FDG PET/CT in Patients with Various Cancers. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1915–1931. [Google Scholar] [CrossRef]
- Lan, L.; Liu, H.; Wang, Y.; Deng, J.; Peng, D.; Feng, Y.; Wang, L.; Chen, Y.; Qiu, L. The Potential Utility of [68 Ga]Ga-DOTA-FAPI-04 as a Novel Broad-Spectrum Oncological and Non-Oncological Imaging Agent-Comparison with [18F]FDG. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 963–979. [Google Scholar] [CrossRef] [PubMed]
- Giesel, F.L.; Kratochwil, C.; Lindner, T.; Marschalek, M.M.; Loktev, A.; Lehnert, W.; Debus, J.; Jäger, D.; Flechsig, P.; Altmann, A.; et al. 68Ga-FAPI PET/CT: Biodistribution and Preliminary Dosimetry Estimate of 2 DOTA-Containing FAP-Targeting Agents in Patients with Various Cancers. J. Nucl. Med. 2019, 60, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Röhrich, M.; Leitz, D.; Glatting, F.M.; Wefers, A.K.; Weinheimer, O.; Flechsig, P.; Kahn, N.; Mall, M.A.; Giesel, F.L.; Kratochwil, C.; et al. Fibroblast Activation Protein-Specific PET/CT Imaging in Fibrotic Interstitial Lung Diseases and Lung Cancer: A Translational Exploratory Study. J. Nucl. Med. 2022, 63, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Bai, L.; Shang, J.; Tang, Y.; Ling, X.; Guo, B.; Gong, J.; Wang, L.; Xu, H. Preliminary Clinical Results for PET/MR Compared with PET/CT in Patients with Nasopharyngeal Carcinoma. Oncol. Rep. 2020, 43, 177–187. [Google Scholar] [CrossRef]
- Chan, S.-C.; Yeh, C.-H.; Yen, T.-C.; Ng, S.-H.; Chang, J.T.-C.; Lin, C.-Y.; Yen-Ming, T.; Fan, K.-H.; Huang, B.-S.; Hsu, C.-L.; et al. Clinical Utility of Simultaneous Whole-Body 18F-FDG PET/MRI as a Single-Step Imaging Modality in the Staging of Primary Nasopharyngeal Carcinoma. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 1297–1308. [Google Scholar] [CrossRef]
- Cao, C.; Yang, P.; Xu, Y.; Niu, T.; Hu, Q.; Chen, X. Feasibility of Multiparametric Imaging with PET/MR in Nasopharyngeal Carcinoma: A Pilot Study. Oral Oncol. 2019, 93, 91–95. [Google Scholar] [CrossRef]
- Jiang, C.; Chen, Y.; Zhu, Y.; Xu, Y. Systematic Review and Meta-Analysis of the Accuracy of 18F-FDG PET/CT for Detection of Regional Lymph Node Metastasis in Esophageal Squamous Cell Carcinoma. J. Thorac. Dis. 2018, 10, 6066–6076. [Google Scholar] [CrossRef]
- Zhao, L.; Chen, S.; Lin, L.; Sun, L.; Wu, H.; Lin, Q.; Chen, H. [68Ga]Ga-DOTA-FAPI-04 Improves Tumor Staging and Monitors Early Response to Chemoradiotherapy in a Patient with Esophageal Cancer. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 3188–3189. [Google Scholar] [CrossRef]
- Zhao, L.; Chen, S.; Chen, S.; Pang, Y.; Dai, Y.; Hu, S.; Lin, L.; Fu, L.; Sun, L.; Wu, H.; et al. 68Ga-Fibroblast Activation Protein Inhibitor PET/CT on Gross Tumour Volume Delineation for Radiotherapy Planning of Oesophageal Cancer. Radiother. Oncol. 2021, 158, 55–61. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Dekker, E.; Tanis, P.J.; Vleugels, J.L.A.; Kasi, P.M.; Wallace, M.B. Colorectal Cancer. Lancet 2019, 394, 1467–1480. [Google Scholar] [CrossRef] [PubMed]
- Biller, L.H.; Schrag, D. Diagnosis and Treatment of Metastatic Colorectal Cancer: A Review. JAMA 2021, 325, 669–685. [Google Scholar] [CrossRef] [PubMed]
- Borello, A.; Russolillo, N.; Lo Tesoriere, R.; Langella, S.; Guerra, M.; Ferrero, A. Diagnostic Performance of the FDG-PET/CT in Patients with Resected Mucinous Colorectal Liver Metastases. Surgeon 2021, 19, e140–e145. [Google Scholar] [CrossRef]
- Deshpande, V.; Zen, Y.; Chan, J.K.; Yi, E.E.; Sato, Y.; Yoshino, T.; Klöppel, G.; Heathcote, J.G.; Khosroshahi, A.; Ferry, J.A.; et al. Consensus Statement on the Pathology of IgG4-Related Disease. Mod. Pathol. 2012, 25, 1181–1192. [Google Scholar] [CrossRef]
- Pan, Q.; Luo, Y.; Zhang, W. Recurrent Immunoglobulin G4-Related Disease Shown on 18F-FDG and 68Ga-FAPI PET/CT. Clin. Nucl. Med. 2020, 45, 312–313. [Google Scholar] [CrossRef]
- Luo, Y.; Pan, Q.; Yang, H.; Peng, L.; Zhang, W.; Li, F. Fibroblast Activation Protein-Targeted PET/CT with 68Ga-FAPI for Imaging IgG4-Related Disease: Comparison to 18F-FDG PET/CT. J. Nucl. Med. 2021, 62, 266–271. [Google Scholar] [CrossRef]
- Guglielmo, P.; Guerra, L. Radiolabeled Fibroblast Activation Protein Inhibitor (FAPI) PET in Oncology: Has the Time Come for 18F-Fluorodeoxyglucose to Think to a Well-Deserved Retirement? Clin. Transl. Imaging 2021, 9, 1–2. [Google Scholar] [CrossRef]
- Hicks, R.J.; Roselt, P.J.; Kallur, K.G.; Tothill, R.W.; Mileshkin, L. FAPI PET/CT: Will It End the Hegemony of 18F-FDG in Oncology? J. Nucl. Med. 2021, 62, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Fendler, W.P.; Pabst, K.M.; Kessler, L.; Fragoso Costa, P.; Ferdinandus, J.; Weber, M.; Lippert, M.; Lueckerath, K.; Umutlu, L.; Kostbade, K.; et al. Safety and Efficacy of 90Y-FAPI-46 Radioligand Therapy in Patients with Advanced Sarcoma and Other Cancer Entities. Clin. Cancer Res. 2022, 28, 4346–4353. [Google Scholar] [CrossRef] [PubMed]
- Zboralski, D.; Osterkamp, F.; Simmons, A.D.; Bredenbeck, A.; Schumann, A.; Paschke, M.; Beindorff, N.; Mohan, A.-M.; Nguyen, M.; Xiao, J.; et al. 571P Preclinical Evaluation of FAP-2286, a Peptide-Targeted Radionuclide Therapy (PTRT) to Fibroblast Activation Protein Alpha (FAP). Ann. Oncol. 2020, 31, S488. [Google Scholar] [CrossRef]
- Zboralski, D.; Hoehne, A.; Bredenbeck, A.; Schumann, A.; Nguyen, M.; Schneider, E.; Ungewiss, J.; Paschke, M.; Haase, C.; von Hacht, J.L.; et al. Preclinical Evaluation of FAP-2286 for Fibroblast Activation Protein Targeted Radionuclide Imaging and Therapy. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 3651–3667. [Google Scholar] [CrossRef]
- Baum, R.P.; Schuchardt, C.; Singh, A.; Chantadisai, M.; Robiller, F.C.; Zhang, J.; Mueller, D.; Eismant, A.; Almaguel, F.; Zboralski, D.; et al. Feasibility, Biodistribution, and Preliminary Dosimetry in Peptide-Targeted Radionuclide Therapy of Diverse Adenocarcinomas Using 177Lu-FAP-2286: First-in-Humans Results. J. Nucl. Med. 2022, 63, 415–423. [Google Scholar] [CrossRef]


| First Author | Journal | Year | Country | FAPI-Based Tracer Used | Study Design | Primary Tumor Site | Clinical Indication | Reference Standard | Number of Patients (M:F) | Median (Range) or Mean (±SD) Age | Metastases (Y/N) | Advantage over [18F]FDG |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fu, H. | Radiology | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Thyroid | Suspect of distant metastasis | Histopathology OR clinical/imaging follow-up | 35 (18:17) | 44 (28–58) | Y | Y |
| Mu, X. | EJNMMI | 2023 | China | [18F]FAPI-42 | P | Thyroid | Detection of recurrence | Imaging | 42 (16:26) | 46 (12–75) | Y | D |
| Zhang, J. | EJNMMI | 2023 | China | [18F]FAPI | P | Liver | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 37 (34:3) | 57 (48–67) | Y | Y |
| Wang, H. | Frontiers in Oncology | 2021 | China | [68Ga]Ga-DOTA-FAPI-04 | R | Liver | Diagnostic accuracy | n.a. | 25 (24:1) | 59.40 ± 6.90 | Y | Y |
| Siripongsatian, D. | Molecular Imaging and Biology | 2022 | Thailand | [68Ga]Ga-FAPI-46 | R | Liver | Diagnostic accuracy | MRI images | 27 (21:6) | 68 (60–74) | Y | Y |
| Guo, W. | EJNMMI | 2021 | China | [68Ga]Ga-DOTA-FAPI-04 | R | Liver | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 34 (25:9) | 60.6 (33–75) | Y | Y |
| Rajaraman, V. | Clinical Nuclear Medicine | 2023 | India | [68Ga]Ga-DOTA-FAPI-04 | P | Liver and biliary tract | Diagnostic accuracy | n.a. | 41 (28:13) | n.a. | Y | Y |
| Shi, X. | EJNMMI | 2021 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Liver | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 20 (18:2) | 58.0 ± 9.4 | Y | Y |
| Pabst, K.M. | JNM | 2023 | Germany | [68Ga]Ga-FAPI-46 | P | Biliary tract | Staging | Histopathology OR clinical/imaging follow-up | 10 (6:4) | 55.5 (40–79) | Y | Y |
| Lan, L. | Radiology | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Biliary tract | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 18 (6:12) | 61 ± 10 | Y | Y |
| Elboga, U. | Molecular Imaging and Biology | 2022 | Turkey | [68Ga]Ga-DOTA-FAPI-04 | R | Peritoneal carcinomatosis | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 37 (23:14) | 62.8 ± 12.7 | Y | Y |
| Güzel, Y. | Hellenic Journal of Nuclear Medicine | 2023 | Turkey | [68Ga]Ga-DOTA-FAPI-04 | R | Peritoneal carcinomatosis | Diagnostic accuracy | CT images | 57 (25:32) | 54 (22–86) | Y | Y |
| Zhao, L. | EJNMMI | 2021 | China | [68Ga]Ga-DOTA-FAPI-04 | R | Peritoneal carcinomatosis | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 46 (14:32) | 57 (32–80) | Y | Y |
| Zheng, S. | Clinical Nuclear Medicine | 2023 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Breast | Initial staging | Histopathology | 34 F | 51.5 (36–72) | Y | Y |
| Kömek, H. | Annals of Nuclear Medicine | 2021 | Turkey | [68Ga]Ga-DOTA-FAPI-04 | P | Breast | Staging OR detection of recurrence | n.a. | 20 F | 44 (32–65) | Y | Y |
| Ballal, S. | Pharmaceuticals | 2023 | India | [68Ga]Ga-DOTA.SA.FAPI | R | Breast | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 47 F | 44.8 ± 9.9 | Y | Y |
| Elboga, U. | Annals of Nuclear Medicine | 2021 | Turkey | [68Ga]Ga-DOTA-FAPI-04 | R | Breast | Diagnostic accuracy | n.a. | 48 F | 53.3 ± 11.7 | Y | Y |
| Zheng, W. | Nuclear Medicine Communications | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | R | Ovary | Staging OR detection of recurrence | Histopathology OR clinical/imaging follow-up | 27 F | 56 ± 12 | Y | Y |
| Liu, S. | EJNMMI | 2023 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Ovary | Detection of recurrence | n.a. | 29 F | 56.90 ± 8.38 | Y | Y |
| Wegen, S. | Clinical Nuclear Medicine | 2023 | Germany | [68Ga]Ga-FAPI-46 | R | Cervical | Initial staging | Histopathology | 7 F | 57 (34–67) | Y | Y |
| Wu, C. | EJNMMI | 2022 | China | [18F]FAPI-42 | R | GIST | Detection of recurrence or distant metastases | Histopathology OR clinical/imaging follow-up | 35 (21:14) | 54 (32–76) | Y | Y |
| Lin, R. | EJNMMI | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Stomach | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 56 (40:16) | 63.8 ± 14.9 | Y | Y |
| Qin, C. | JNM | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Stomach | Diagnostic accuracy | n.a. | 20 (9:11) | 56 (29–70) | Y | Y |
| Jiang, D. | EJNMMI | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | R | Stomach | Diagnostic accuracy | Histopathology | 29 (20:9) | 67 (25–86) | Y | Y |
| Chen, H. | European Radiology | 2023 | China | [68Ga]Ga-DOTA-FAPI-04 | R | Stomach | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 34 (16–18) | 51 (25–85) | Y | Y |
| Zhang, S. | Frontiers in Oncology | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | R | Stomach | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 25 (12:13) | 56 ± 12 | Y | Y |
| Gündoğan, C. | Nuclear Medicine Communications | 2021 | Turkey | [68Ga]Ga-DOTA-FAPI-04 | P | Stomach | Diagnostic accuracy | n.a. | 21 (12:9) | 61 (40–81) | Y | Y |
| Kuten, J. | EJNMMI | 2022 | Israel | [68Ga]Ga-DOTA-FAPI-04 | P | Stomach | Detection rate | Histopathology OR clinical/imaging follow-up | 10 (n.a.) | 71 (42–87) | Y | Y |
| Miao, Y. | European Radiology | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Stomach | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 62 (44:18) | 64 (24–75) | Y | Y |
| Wang, L. | Radiology | 2022 | China | [68Ga]Ga-FAPI | P | Lung | Diagnostic accuracy | MRI images (brain) | 34 (20:14) | 64 (46–80) | Y | Y |
| Wu, J. | Frontiers in Oncology | 2022 | China | [68Ga]Ga-FAPI | P | Lung | Staging | Histopathology OR clinical/imaging follow-up | 28 (13:15) | 60.5 (34–78) | Y | Y |
| Can, C. | Nuclear Medicine Communications | 2022 | Turkey | [68Ga]Ga-DOTA-FAPI-04 | R | Lung | Diagnostic accuracy | n.a. | 29 (27:2) | 71 (46–84) | Y | D |
| Zhou, X. | EJNMMI | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Lung | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 74 (39:35) | 63 ± 8 | Y | Y |
| Zheng, J. | Molecular Imaging and Biology | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Nasopharyngeal | Diagnostic accuracy | CT and MRI images | 47 (32:15) | 52.3 ± 13.8 | Y | Y |
| Qin, C. | EJNMMI | 2021 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Nasopharyngeal | Diagnostic accuracy | MRI images | 15 (8:7) | 51.2 ± 9.4 | Y | Y |
| Chen, S. | European Radiology | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Oral cavity | Preoperative staging | Histopathology | 36 (29:7) | 62.5 (34–87) | Y | Y |
| Promteangtrong, C. | JNM | 2022 | Thailand | [68Ga]Ga-FAPI-46 | P | Head and neck | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 40 (27:13) | 57.5 (32–86) | Y | D |
| Wegen, S. | Molecular Imaging and Biology | 2022 | Germany | [68Ga]Ga-FAPI-46 | R | Head and neck | Radiotherapy planning | n.a. | 15 (12:3) | 66 (37–82) | Y | D |
| Ding, H. | Frontiers in Oncology | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Nasopharyngeal | Initial staging | Histopathology OR imaging follow-up | 28 (23:5) | 53 ± 11 | Y | Y |
| Serfling, S. | EJNMMI | 2021 | Germany | [68Ga]Ga-DOTA-FAPI-04 | R | Waldeyer’s tonsillar ring | Suspect of disease | n.a. | 8 (n.a.) | 62 (58–72) | Y | D |
| Linz, C. | EJNMMI | 2021 | Germany | [68Ga]Ga-DOTA-FAPI-04 | P | Oral cavity | Initial staging | Histopathology | 10 (8:2) | 62 ± 9 | Y | D |
| Jiang, Y. | EJNMMI | 2023 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Head and neck | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 77 (61:16) | 58 (20, 89) | Y | Y |
| Gu, B. | JNM | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Head and neck | Detection FDG- findings | Histopathology | 18 (16:2) | 55 (24–72) | Y | Y |
| Liu, H. | Frontiers in Oncology | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | R | Esophagus | Diagnostic accuracy | Histopathology OR clinical/imaging follow-up | 35 (32:3) | 63.5 (44–83) | Y | Y |
| Kömek, H. | EJNMMI | 2021 | Turkey | [68Ga]Ga-DOTA-FAPI-04 | P | Colon or rectum | Diagnostic accuracy | Histopathology | 39 (22:17) | 61 (29–83) | Y | Y |
| Lin, X. | Frontiers in Oncology | 2023 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Colon or rectum | Diagnostic accuracy | Histopathology OR imaging follow-up | 61 (42:19) | 62 (32–81) | Y | Y |
| Liu, Q. | European Radiology | 2023 | China | [68Ga]Ga-DOTA-FAPI-04 | R | Pancreas | Diagnostic accuracy and prognostic stratification | Histopathology OR clinical/imaging follow-up | 26 (19:7) | 62.4 ± 11.9 | Y | Y |
| Zhang, Z. | EJNMMI | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Pancreas | Suspect of disease | Histopathology | 33 (19:14) | 63 (46–81) | Y | D |
| Novruzov, E. | Molecular Imaging and Biology | 2022 | Germany | [68Ga]Ga-DOTA-FAPI-04 | R | Bladder | Diagnostic accuracy | Histopathology (only bladder) | 8 M | 66 (57–78) | Y | Y |
| Gu, B. | EJNMMI | 2022 | China | [68Ga]Ga-DOTA-FAPI-04 | P | Soft tissue | Detection of recurrence | Histopathology OR clinical/imaging follow-up | 45 (24:21) | 46 (18–71) | Y | Y |
| Luo, Y. | JNM | 2021 | China | [68Ga]Ga-DOTA-FAPI-04 | P | IgG4-related disease | Diagnostic accuracy | FDG PET/CT | 26 (20:6) | 51.5 ± 12.9 | Y | D |
| Elboga, U. | Tomography | 2022 | Turkey | [68Ga]Ga-DOTA-FAPI-04 | R | MM | Detection rate | Histopathology OR clinical/imaging follow-up | 14 (7:7) | 58 (39–81) | Y | D |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guglielmo, P.; Alongi, P.; Baratto, L.; Abenavoli, E.; Buschiazzo, A.; Celesti, G.; Conte, M.; Filice, R.; Gorica, J.; Jonghi-Lavarini, L.; et al. Head-to-Head Comparison of FDG and Radiolabeled FAPI PET: A Systematic Review of the Literature. Life 2023, 13, 1821. https://doi.org/10.3390/life13091821
Guglielmo P, Alongi P, Baratto L, Abenavoli E, Buschiazzo A, Celesti G, Conte M, Filice R, Gorica J, Jonghi-Lavarini L, et al. Head-to-Head Comparison of FDG and Radiolabeled FAPI PET: A Systematic Review of the Literature. Life. 2023; 13(9):1821. https://doi.org/10.3390/life13091821
Chicago/Turabian StyleGuglielmo, Priscilla, Pierpaolo Alongi, Lucia Baratto, Elisabetta Abenavoli, Ambra Buschiazzo, Greta Celesti, Miriam Conte, Rossella Filice, Joana Gorica, Lorenzo Jonghi-Lavarini, and et al. 2023. "Head-to-Head Comparison of FDG and Radiolabeled FAPI PET: A Systematic Review of the Literature" Life 13, no. 9: 1821. https://doi.org/10.3390/life13091821
APA StyleGuglielmo, P., Alongi, P., Baratto, L., Abenavoli, E., Buschiazzo, A., Celesti, G., Conte, M., Filice, R., Gorica, J., Jonghi-Lavarini, L., Lanzafame, H., Laudicella, R., Librando, M., Linguanti, F., Mattana, F., Miceli, A., Olivari, L., Piscopo, L., Romagnolo, C., ... Evangelista, L. (2023). Head-to-Head Comparison of FDG and Radiolabeled FAPI PET: A Systematic Review of the Literature. Life, 13(9), 1821. https://doi.org/10.3390/life13091821









