Immunogenicity of Botulinum Toxin Type A in Different Clinical and Cosmetic Treatment, a Literature Review
Abstract
1. Introduction
2. Systematic Reviews and Meta-Analyses
3. Clinical Studies on Immunogenicity and Treatment Response
4. Correlation Studies and Methodological Evaluations
5. Efficacy and Safety Studies
6. Longitudinal Studies on Antibody Development and Impact
7. Case Reports and Observational Studies
8. Product-Sepcific Studies
9. Correlation Studies and Methodological Evaluation
10. Discussion
11. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Critchfield, J. Considering the immune response to botulinum toxin. Clin. J. Pain 2002, 18, S133–S141. [Google Scholar] [CrossRef] [PubMed]
- Dressler, D. Clinical presentation and management of antibody-induced failure of botulinum toxin therapy. Mov. Disord. 2004, 19 (Suppl. S8), S92–S100. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Stenmark, P. The structure and classification of botulinum toxins. In Botulinum Toxin Therapy; Handbook of Experimental Pharmacology; Springer: Cham, Switzerland, 2021; Volume 263, pp. 11–33. [Google Scholar]
- Simpson, L. The life history of a botulinum toxin molecule. Toxicon 2013, 68, 40–59. [Google Scholar] [CrossRef] [PubMed]
- Voller, B.; Moraru, E.; Auff, E.; Benesch, M.; Poewe, W.; Wissel, J.; Müller, J.; Entner, T.; Bigalke, H.; Schnider, P. Ninhydrin sweat test: A simple method for detecting antibodies neutralizing botulinum toxin type A. Mov. Disord. 2004, 19, 943–947. [Google Scholar] [CrossRef] [PubMed]
- Rahman, E.; Banerjee, P.S.; Asghar, A.; Gupta, N.K.; Mosahebi, A. Botulinum Toxin Type A Immunogenicity across Multiple Indications: An Overview Systematic Review. Plast. Reconstr. Surg. 2022, 149, 837–848. [Google Scholar] [CrossRef]
- Jankovic, J.; Carruthers, J.; Naumann, M.; Ogilvie, P.; Boodhoo, T.; Attar, M.; Gupta, S.; Singh, R.; Soliman, J.; Yushmanova, I.; et al. Neutralizing antibody formation with OnabotulinumtoxinA (BOTOX®) treatment from global registration studies across multiple indications: A meta-analysis. Toxins 2023, 15, 342. [Google Scholar] [CrossRef]
- Kranz, G.; Sycha, T.; Voller, B.; Kranz, G.S.; Schnider, P.; Auff, E. Neutralizing antibodies in dystonic patients who still respond well to botulinum toxin type A. Neurology 2008, 70, 133–136. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, G.; Li, C.; Mao, C.; Lei, X.; Lee, E. Safety and Efficacy of OnabotulinumtoxinA for Treatment of Crow’s Feet Lines in Chinese Subjects. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2079. [Google Scholar] [CrossRef]
- Harii, K.; Kawashima, M. A double-blind, randomized, placebo-controlled, two-dose comparative study of botulinum toxin type A for treating glabellar lines in Japanese subjects. Aesthetic Plast. Surg. 2008, 32, 724–730. [Google Scholar] [CrossRef]
- Coleman, C.; Hubble, J.; Schwab, J.; Beffy, J.L.; Picaut, P.; Morte, C. Immunoresistance in cervical dystonia patients after treatment with abobotulinumtoxinA. Int. J. Neurosci. 2012, 122, 358–362. [Google Scholar] [CrossRef]
- Oshima, M.; Deitiker, P.; Hastings-Ison, T.; Aoki, K.R.; Graham, H.K.; Atassi, M.Z. Antibody responses to botulinum neurotoxin type A of toxin-treated spastic equinus children with cerebral palsy: A randomized clinical trial comparing two injection schedules. J. Neuroimmunol. 2017, 306, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Tomic, M.T.; Farr-Jones, S.; Syar, E.S.; Niemuth, N.; Kobs, D.; Hackett, M.J.; Espinoza, Y.; Martinez, Z.; Pham, K.; Snow, D.M.; et al. Neutralizing concentrations of anti-botulinum toxin antibodies positively correlate with mouse neutralization assay results in a guinea pig model. Toxins 2021, 13, 671. [Google Scholar] [CrossRef] [PubMed]
- Birklein, F.; Walther, D.; Bigalke, H.; Winterholler, M.; Erbguth, F. Sudomotor testing predicts the presence of neutralizing botulinum A toxin antibodies. Ann. Neurol. 2002, 52, 68–73. [Google Scholar] [CrossRef]
- Cordivari, C.; Misra, V.P.; Vincent, A.; Catania, S.; Bhatia, K.P.; Lees, A.J. Secondary nonresponsiveness to botulinum toxin A in cervical dystonia: The role of electromyogram-guided injections, botulinum toxin A antibody assay, and the extensor digitorum brevis test. Mov. Disord. 2006, 21, 1737–1741. [Google Scholar] [CrossRef] [PubMed]
- Hefter, H.; Hartmann, C.J.; Kahlen, U.; Samadzadeh, S.; Rosenthal, D.; Moll, M. Clinical Improvement After Treatment With IncobotulinumtoxinA (XEOMIN®) in Patients With Cervical Dystonia Resistant to Botulinum Toxin Preparations Containing Complexing Proteins. Front. Neurol. 2021, 12, 636590. [Google Scholar] [CrossRef] [PubMed]
- Charles, D.; Brashear, A.; Hauser, R.A.; Li, H.I.; Boo, L.M.; Brin, M.F. Efficacy, tolerability, and immunogenicity of onabotulinumtoxina in a randomized, double-blind, placebo-controlled trial for cervical dystonia. Clin. Neuropharmacol. 2012, 35, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Schulte-Baukloh, H.; Bigalke, H.; Miller, K.; Heine, G.; Pape, D.; Lehmann, J.; Knispel, H.H. Botulinum neurotoxin type A in urology: Antibodies as a cause of therapy failure. Int. J. Urol. 2008, 15, 407–415; discussion 415. [Google Scholar] [CrossRef]
- Kaňovský, P.; Slawek, J.; Denes, Z.; Platz, T.; Comes, G.; Grafe, S.; Pulte, I. Efficacy and safety of treatment with incobotulinum toxin A (botulinum neurotoxin type A free from complexing proteins; NT 201) in post-stroke upper limb spasticity. J. Rehabil. Med. 2011, 43, 486–492. [Google Scholar] [CrossRef]
- Truong, D.D.; Gollomp, S.M.; Jankovic, J.; LeWitt, P.A.; Marx, M.; Hanschmann, A.; Fernandez, H.H. Sustained efficacy and safety of repeated incobotulinumtoxinA (Xeomin®) injections in blepharospasm. J Neural Transm 2013, 120, 1345–1353. [Google Scholar] [CrossRef]
- Bakheit, A.M.; Fedorova, N.V.; Skoromets, A.A.; Timerbaeva, S.L.; Bhakta, B.B.; Coxon, L. The beneficial antispasticity effect of botulinum toxin type A is maintained after repeated treatment cycles. J. Neurol. Neurosurg. Psychiatry 2004, 75, 1558–1561. [Google Scholar] [CrossRef]
- Albrecht, P.; Jansen, A.; Lee, J.I.; Moll, M.; Ringelstein, M.; Rosenthal, D.; Bigalke, H.; Aktas, O.; Hartung, H.P.; Hefter, H. High prevalence of neutralizing antibodies after long-term botulinum neurotoxin therapy. Neurology 2019, 92, e48–e54. [Google Scholar] [CrossRef] [PubMed]
- Hegele, A.; Frohme, C.; Varga, Z.; Olbert, P.; Kranz, J.; Hofmann, R. Antibodies after botulinum toxin A injection into musculus detrusor vesicae: Incidence and clinical relevance. Urol. Int. 2011, 87, 439–444. [Google Scholar] [CrossRef]
- Mohammadi, B.; Buhr, N.; Bigalke, H.; Krampfl, K.; Dengler, R.; Kollewe, K. A long-term follow-up of botulinum toxin A in cervical dystonia. Neurol. Res. 2009, 31, 463–466. [Google Scholar] [CrossRef] [PubMed]
- Müller, K.; Mix, E.; Adib Saberi, F.; Dressler, D.; Benecke, R. Prevalence of neutralising antibodies in patients treated with botulinum toxin type A for spasticity. J. Neural Transm. 2009, 116, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Bakheit, A.M.; Liptrot, A.; Newton, R.; Pickett, A.M. The effect of total cumulative dose, number of treatment cycles, interval between injections, and length of treatment on the frequency of occurrence of antibodies to botulinum toxin type A in the treatment of muscle spasticity. Int. J. Rehabil. Res. 2012, 35, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Schulte-Baukloh, H.; Herholz, J.; Bigalke, H.; Miller, K.; Knispel, H.H. Results of a BoNT/A antibody study in children and adolescents after onabotulinumtoxin A (Botox®) detrusor injection. Urol. Int. 2011, 87, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Torres, S.; Hamilton, M.; Sanches, E.; Starovatova, P.; Gubanova, E.; Reshetnikova, T. Neutralizing antibodies to botulinum neurotoxin type A in aesthetic medicine: Five case reports. Clin. Cosmet. Investig. Dermatol. 2014, 7, 11–17. [Google Scholar] [CrossRef]
- Lawrence, I.; Moy, R. An evaluation of neutralizing antibody induction during treatment of glabellar lines with a new US formulation of botulinum neurotoxin type A. Aesthet. Surg. J. 2009, 29, S66–S71. [Google Scholar] [CrossRef]
- Brin, M.F.; Comella, C.L.; Jankovic, J.; Lai, F.; Naumann, M. Long-term treatment with botulinum toxin type A in cervical dystonia has low immunogenicity by mouse protection assay. Mov. Disord. 2008, 23, 1353–1360. [Google Scholar] [CrossRef]
- Coleman, W.P., 3rd; Sattler, G.; Weissenberger, P.; Hast, M.A.; Hanschmann, A. Safety of IncobotulinumtoxinA in the Treatment of Facial Lines: Results From a Pooled Analysis of Randomized, Prospective, Controlled Clinical Studies. Dermatol. Surg. 2017, 43 (Suppl. S3), S293–S303. [Google Scholar] [CrossRef]
- Solish, N.; Carruthers, J.; Kaufman, J.; Rubio, R.G.; Gross, T.M.; Gallagher, C.J. Overview of DaxibotulinumtoxinA for Injection: A Novel Formulation of Botulinum Toxin Type A. Drugs 2021, 81, 2091–2101. [Google Scholar] [CrossRef] [PubMed]
- Lange, O.; Bigalke, H.; Dengler, R.; Wegner, F.; deGroot, M.; Wohlfarth, K. Neutralizing antibodies and secondary therapy failure after treatment with botulinum toxin type A: Much ado about nothing? Clin. Neuropharmacol. 2009, 32, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Münchau, A.; Bhatia, K.P. Uses of botulinum toxin injection in medicine today. BMJ 2000, 320, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Frueh, B.R.; Felt, D.P.; Wojno, T.H.; Musch, D.C. Treatment of blepharospasm with botulinum toxin. A preliminary report. Arch. Ophthalmol. 1984, 102, 1464–1468. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.B. Botulinum toxin injection of eye muscles to correct strabismus. Trans. Am. Ophthalmol. Soc. 1981, 79, 734–770. [Google Scholar]
- Ferrante, F.M.; Bearn, L.; Rothrock, R.; King, L. Evidence against trigger point injection technique for the treatment of cervicothoracic myofascial pain with botulinum toxin type A. Anesthesiology 2005, 103, 377–383. [Google Scholar] [CrossRef]
- Bhidayasiri, R.; Truong, D.D. Evidence for effectiveness of botulinum toxin for hyperhidrosis. J. Neural Transm. 2008, 115, 641–645. [Google Scholar] [CrossRef]
- Camargo, C.H.; Cattai, L.; Teive, H.A. Pain Relief in Cervical Dystonia with Botulinum Toxin Treatment. Toxins 2015, 7, 2321–2335. [Google Scholar] [CrossRef]
- Brisinda, G.; Cadeddu, F.; Mazzeo, P.; Maria, G. Botulinum toxin A for the treatment of chronic anal fissure. Expert. Rev. Gastroenterol. Hepatol. 2007, 1, 219–228. [Google Scholar] [CrossRef]
- Gui, D.; Cassetta, E.; Anastasio, G.; Bentivoglio, A.R.; Maria, G.; Albanese, A. Botulinum toxin for chronic anal fissure. Lancet 1994, 344, 1127–1128. [Google Scholar] [CrossRef]
- Duthie, J.B.; Vincent, M.; Herbison, G.P.; Wilson, D.I.; Wilson, D. Botulinum toxin injections for adults with overactive bladder syndrome. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef]
- Hsieh, P.F.; Chiu, H.C.; Chen, K.C.; Chang, C.H.; Chou, E.C. Botulinum toxin A for the treatment of overactive bladder. Toxins 2016, 8, 59. [Google Scholar] [CrossRef] [PubMed]
- Benecke, R. Clinical relevance of botulinum toxin immunogenicity. BioDrugs 2012, 26, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Rzany, B.; Ascher, B.; Monheit, G. Treatment of glabellar lines with botulinum toxin type A (Speywood Unit): A clinical overview. J. Eur. Acad. Dermatol. Venereol. 2010, 24 (Suppl. S1), 1–14. [Google Scholar] [CrossRef] [PubMed]
- Naumann, M.; Carruthers, A.; Carruthers, J.; Aurora, S.K.; Zafonte, R.; Abu-Shakra, S.; Boodhoo, T.; Miller-Messana, M.A.; Demos, G.; James, L.; et al. Meta-analysis of neutralizing antibody conversion with onabotulinumtoxinA (BOTOX®) across multiple indications. Mov. Disord. 2010, 25, 2211–2218. [Google Scholar] [CrossRef] [PubMed]
- Ho, W.W.; Albrecht, P.; Calderon, P.E.; Corduff, N.; Loh, D.; Martin, M.U.; Park, J.Y.; Suseno, L.S.; Tseng, F.W.; Vachiramon, V.; et al. Emerging trends in botulinum neurotoxin A resistance: An international multidisciplinary review and consensus. Plast. Reconstr. Surg.–Glob. Open 2022, 10, e4407. [Google Scholar] [CrossRef]
- Herrmann, J.; Geth, K.; Mall, V.; Bigalke, H.; Schulte Mönting, J.; Linder, M.; Kirschner, J.; Berweck, S.; Korinthenberg, R.; Heinen, F.; et al. Clinical impact of antibody formation to botulinum toxin A in children. Ann. Neurol. 2004, 55, 732–735. [Google Scholar] [CrossRef]
- Srinoulprasert, Y.; Wanitphakdeedecha, R. Antibody-induced botulinum toxin treatment failure: A review and novel management approach. J. Cosmet. Dermatol. 2020, 19, 2491–2496. [Google Scholar] [CrossRef]
- Corduff, N.; Park, J.Y.; Calderon, P.E.; Choi, H.; Dingley, M.; Ho, W.W.S.; Martin, M.U.; Suseno, L.S.; Tseng, F.W.; Vachiramon, V.; et al. Real-world Implications of Botulinum Neurotoxin A Immunoresistance for Consumers and Aesthetic Practitioners: Insights from ASCEND Multidisciplinary Panel. Plast. Reconstr. Surg. Glob. Open 2024, 12, e5892. [Google Scholar] [CrossRef]

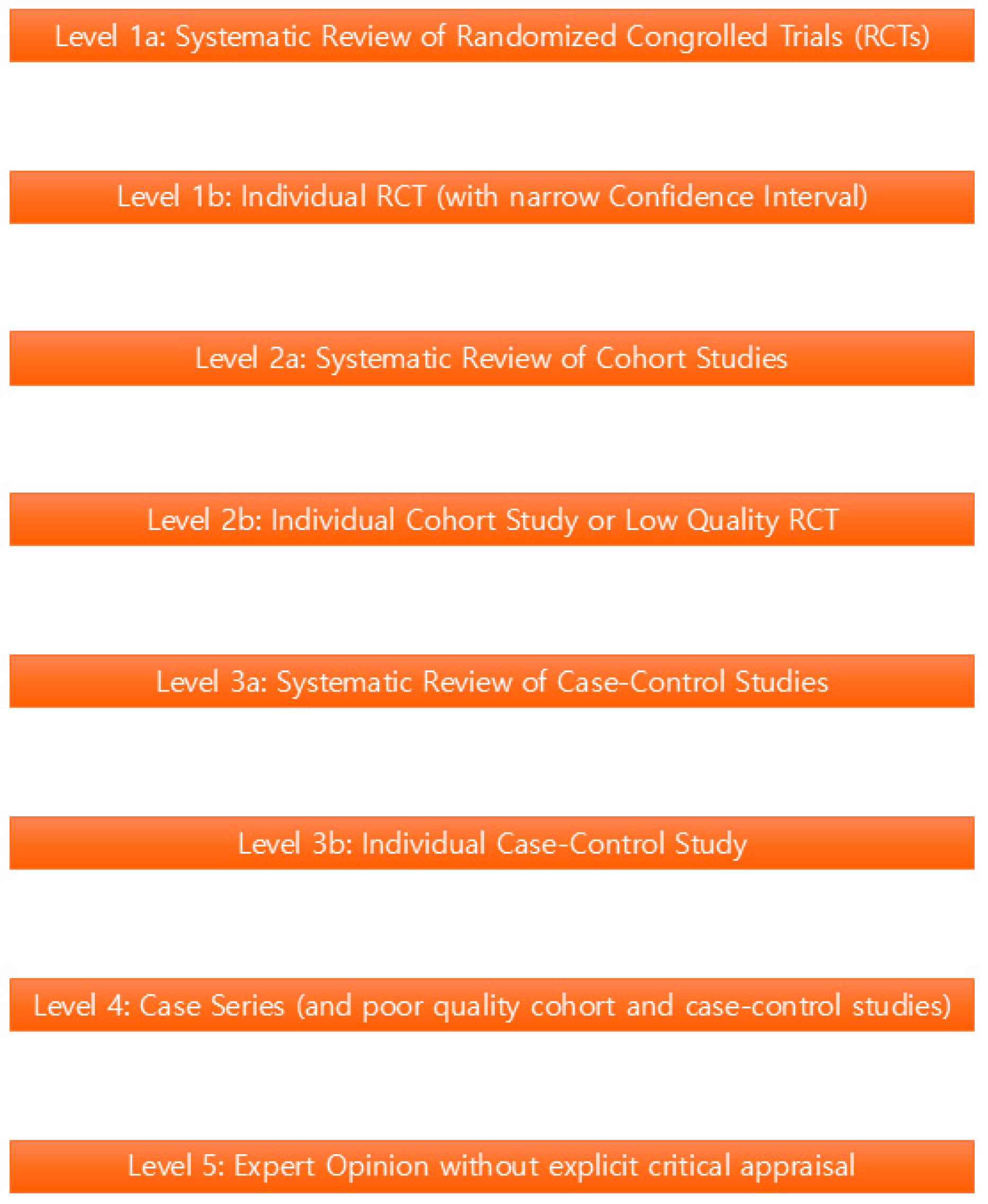
| Study | Objective | Methodology | Key Findings | Conclusion | Level of Evidence |
|---|---|---|---|---|---|
| Kranz et al. [8] | Investigate the presence of neutralizing antibodies against botulinum toxin type A in dystonia patients who continue to respond well to treatment. | 50 dystonia patients treated with botulinum toxin type A for ≥6 months. Blood samples tested for neutralizing antibodies using a functional assay. Clinical evaluation of treatment response. | 44% of patients had detectable neutralizing antibodies. All 22 patients with antibodies continued to respond well to treatment. No association with dose requirement or duration of effect. | Presence of neutralizing antibodies does not necessarily predict loss of treatment response. Immune response may be overwhelmed by high toxin dose or altered toxin binding sites. | IIc |
| Wu et al. [9] | Evaluate the safety, efficacy, and immunogenicity of onabotulinumtoxinA for crow’s feet lines in Chinese subjects. | 120 Chinese patients with moderate to severe crow’s feet lines. Randomized, double-blind, placebo-controlled study. Severity of crow’s feet lines assessed at 30 days post-treatment. | OnabotulinumtoxinA significantly reduced severity of crow’s feet lines (p < 0.001). No serious adverse events. Antibody titers remained stable in treatment group, indicating no significant immunogenicity. | OnabotulinumtoxinA is effective and well-tolerated for crow’s feet lines in Chinese patients, with no significant immunogenicity observed during the study period. | IIb |
| Wu et al. [9] | Evaluate the efficacy, safety, and immunogenicity of botulinum toxin type A for glabellar lines in Chinese patients. | 120 patients with moderate to severe glabellar lines. Double-blind, randomized, placebo-controlled trial. Severity of glabellar lines assessed at 30 days post-treatment. | Botulinum toxin type A significantly improved glabellar lines (p < 0.001). Antibody titers stable in treatment group, indicating no significant immunogenicity. Improvement maintained for 180 days. | Botulinum toxin type A is effective and well-tolerated for glabellar lines, with no significant immunogenicity and prolonged effect observed in Chinese patients. | IIa |
| Harii et al. [10] | Compare efficacy and safety of two doses of botulinum toxin type A for glabellar lines in Japanese subjects. | 120 Japanese patients with moderate to severe glabellar lines. Double-blind, randomized, placebo-controlled trial. Low dose (25 units), high dose (50 units), or placebo. | Both doses significantly improved glabellar lines (p < 0.001). Antibody titers stable in treatment groups, indicating no significant immunogenicity. Improvement maintained for 180 days. | Both low and high doses of botulinum toxin type A are effective and safe for glabellar lines, with no significant immunogenicity observed and long-lasting improvement. | IIa |
| Coleman et al. [11] | Investigate the development of immunoresistance in cervical dystonia patients receiving abobotulinumtoxinA therapy. | 44 patients with cervical dystonia. AbobotulinumtoxinA injections every 12 weeks for ≥24 weeks. Serum samples tested for antibodies using radioimmunoprecipitation assay. | 25% of patients developed immunoresistance after median 16 weeks. Immunoresistance associated with reduced clinical response and higher baseline antibody levels. | Immunoresistance is a significant issue in cervical dystonia patients on abobotulinumtoxinA, requiring monitoring for antibodies and potentially alternative treatments. | IIb |
| Oshima et al. [12] | Compare antibody response to botulinum toxin type A in children with spastic equinus foot treated with different injection schedules. | 44 children with spastic equinus foot due to cerebral palsy. Randomized to standard (every 3–4 months) or extended (every 6–8 months) treatment schedules. 12 injections over 24 months. | Extended treatment group had higher antibody response (60.9% vs. 25.9%). Similar clinical response between groups, but higher risk of antibody development with extended schedule. | Extended treatment schedule increases risk of antibody development, potentially reducing effectiveness of subsequent treatments in children with spastic equinus foot. | IIa |
| Study | Objective | Methodology | Key Findings | Conclusion | Level of Evidence |
|---|---|---|---|---|---|
| Tomic et al. [13] | Evaluate correlation between neutralizing concentrations of anti-botulinum toxin antibodies and MNA results in guinea pigs. | Guinea pigs immunized with botulinum toxin. Sera tested via neutralization assay using a mouse bioassay. Correlation analysis between neutralizing concentrations and MNA results. | Strong positive correlation between neutralizing antibody concentrations and MNA results (r = 0.92, p < 0.01). MNA accurately reflects neutralizing capacity. | MNA is a reliable method for detecting and quantifying anti-botulinum toxin antibodies. MNA results can estimate neutralizing concentrations of antibodies. | IIb |
| Voller et al. [5] | Describe a simple, non-invasive method (ninhydrin sweat test) for detecting neutralizing antibodies against botulinum toxin type A. | Study included 21 dystonia patients and 10 healthy controls. Ninhydrin solution applied to forearms; sweat production measured. | 71% of patients had positive ninhydrin sweat tests. Sensitivity of 95%, specificity of 100%. | Ninhydrin sweat test is a simple, non-invasive, and inexpensive method for detecting neutralizing antibodies, useful for monitoring patients receiving botulinum toxin therapy. | IIb |
| Birklein et al. [14] | Investigate if sudomotor testing can predict presence of neutralizing botulinum A toxin antibodies in patients treated with BTX-A. | 21 patients with cervical dystonia were tested. Sudomotor tests: TST, SSR, VIP stimulation. Compared to serum neutralization assays. | TST detected NTAs in 86% of patients; SSR in 43%, VIP in 29%. Sudomotor testing more accurate than serum assays. | Sudomotor testing, especially TST, is a useful adjunctive tool for predicting presence of NTAs, aiding in treatment decisions and dose adjustments for BTX-A therapy. | IIa |
| Cordivari et al. [15] | Investigate causes of secondary nonresponsiveness to botulinum toxin type A in cervical dystonia patients. | 24 patients were evaluated with EMG-guided injections, BoNT-A antibody assay, and EDB test. | 83% of patients had BoNT-A antibodies; 58% had abnormal EMG; 71% had positive EDB tests. Antibodies and abnormal EMG linked to poor treatment response. | Secondary nonresponsiveness is associated with BoNT-A antibodies, abnormal EMG, and positive EDB tests. These factors may identify patients at risk for nonresponsiveness. | IIb |
| Study | Objective | Methodology | Key Findings | Conclusion | Level of Evidence |
|---|---|---|---|---|---|
| Hefter et al. [16]. | Investigate the efficacy and safety of incobotulinumtoxinA (Xeomin) in cervical dystonia patients resistant to other botulinum toxin products. | 24 patients with cervical dystonia resistant to other botulinum toxin products. IncobotulinumtoxinA injections every 12 weeks for 6 months. Primary endpoint: Change in TWSTRS scores at week 24. | Xeomin led to significant improvement in TWSTRS scores at week 24, with a mean reduction of 14.6 points. 75% of patients had ≥30% reduction in TWSTRS scores. Mild and transient adverse events. | XEOMIN is an effective and safe treatment for cervical dystonia patients resistant to other botulinum toxin products containing complexing proteins. | IIb |
| Charles et al. [17]. | Evaluate the efficacy, tolerability, and immunogenicity of onabotulinumtoxinA (Botox) in cervical dystonia patients. | 131 patients with cervical dystonia. Randomized, double-blind, placebo-controlled trial. Botox injections every 12 weeks for 24 weeks. Primary endpoint: Change in TWSTRS scores at week 24. | Botox significantly improved cervical dystonia symptoms compared to placebo. 64.7% of Botox patients had ≥30% reduction in TWSTRS scores. 10.1% developed neutralizing antibodies. | Botox is an effective and well-tolerated treatment for cervical dystonia, with a high response rate. Neutralizing antibodies did not affect treatment efficacy in the short term. | Ia |
| Schulte-Baukloh et al. [18] | Investigate the incidence and impact of antibody formation on treatment efficacy in patients with detrusor overactivity treated with botulinum toxin type A. | 30 patients with detrusor overactivity. Repeated BoNT-A injections into the detrusor muscle. Serum samples tested for antibodies at baseline, 3 months, and 6 months after the first injection. | 76.7% developed antibodies against BoNT-A. Antibody-positive patients had a significantly lower response to treatment. Mean IPSS improved by 2.5 points in antibody-negative patients vs. 1.2 points in antibody-positive patients. | Development of antibodies against BoNT-A is common in detrusor overactivity patients, potentially contributing to treatment failure. | IIb |
| Kaňovský et al. [19] | Evaluate the efficacy and safety of incobotulinum toxin A (NT 201) in post-stroke upper limb spasticity patients. | 40 patients with post-stroke upper limb spasticity. Single NT 201 injection (20–40 units) into affected muscles. Primary outcomes: MAS scores, DAS scores, PGIC. | NT 201 significantly reduced muscle tone (MAS score from 2.4 to 1.3). Significant improvement in DAS scores (mean reduction of 2.5 points). 75% reported symptom improvement (PGIC). | NT 201 is an effective and safe treatment for post-stroke upper limb spasticity, with a prolonged duration of effect and no development of neutralizing antibodies. | IIa |
| Troung et al. [20] | Evaluate the long-term efficacy and safety of repeated incobotulinumtoxinA (Xeomin) injections for blepharospasm. | 64 patients with blepharospasm. Xeomin injections every 3–4 months for up to 2 years. Efficacy assessed using BDS and PGIC. | Mean BDS score improved significantly from baseline to week 24 and remained stable until week 96. 74% reported “much” or “very much” improvement (PGIC). Mild and temporary adverse events. | Repeated Xeomin injections are effective for maintaining blepharospasm symptom improvement over 2 years, with a favorable safety profile and no development of neutralizing antibodies. | IIa |
| Bakheit et al. [21] | Investigate the long-term efficacy and safety of botulinum toxin type A treatment for spasticity. | 30 patients with upper limb spasticity. 12–16 injections of botulinum toxin type A over 24 months. Patients randomized to receive 10–20 units or 20–40 units per injection every 3–4 months. | Muscle tone reduction remained stable over 24 months (~50% decrease from baseline). 80% reported significant symptom improvement. No significant difference in efficacy between dosage groups. | Botulinum toxin type A is an effective long-term treatment for spasticity, with sustained benefits after repeated cycles and no development of neutralizing antibodies. | IIb |
| Albrecht et al. [22] | Investigate the prevalence of neutralizing antibodies against botulinum neurotoxin type A after long-term treatment. | 134 patients treated with BoNT-A for at least 2 years. Patients divided into short-term (<2 years), medium-term (2–5 years), and long-term (>5 years) groups based on treatment duration. | Prevalence of neutralizing antibodies increased with longer treatment duration (12.5% in short-term vs. 34.6% in long-term). Patients with antibodies had significantly lower treatment response. | Development of neutralizing antibodies is common after long-term BoNT-A treatment and can significantly reduce subsequent treatment efficacy. | IIa |
| Study | Objective | Methodology | Key Findings | Conclusion | Level of Evidence |
|---|---|---|---|---|---|
| Hefter et al. [16] | Evaluate the development of neutralizing antibody titers and their impact on treatment efficacy over 4 years in patients with secondary non-responders. | 35 patients with secondary non-responders. Continuous treatment with Myobloc for a mean duration of 48 months. Antibody titers tested at baseline, 6 months, and every 6 months. | 20% of patients had detectable antibodies at baseline, increasing to 60% at 4 years. No significant decrease in treatment efficacy despite antibody development. | Antibody development is common in continuous botulinum toxin type A treatment but does not necessarily reduce treatment efficacy. Preparations without complexing proteins may have a lower risk. | IIa |
| Hegele et al. [23] | Investigate the development of antibodies against botulinum toxin A and their impact on treatment efficacy in overactive bladder patients. | 44 patients with overactive bladder. Botulinum toxin A injections into detrusor muscle every 6–8 weeks for up to 2 years. Antibodies tested at baseline, 6 weeks, and every 6 weeks. | 25% developed antibodies after the first injection, 50% after the second. 15% developed neutralizing antibodies. Lower treatment response in antibody-positive patients. | Antibodies against botulinum toxin A are common in overactive bladder treatment and can reduce efficacy, potentially requiring more frequent injections to maintain response. | IIa |
| Herrmann et al. [23] | Assess the clinical impact of antibody formation in children receiving repeated botulinum toxin A injections. | 134 children with dystonia, blepharospasm, or strabismus. Repeated botulinum toxin A injections. Antibodies tested using radioimmunoassay. | 27% developed antibodies, leading to a 44.1% reduction in clinical response. Higher risk of neutralizing antibodies in antibody-positive children. | Antibody development is common in children treated with botulinum toxin A and may significantly reduce clinical response to subsequent treatments. | IIa |
| Mohammadi et al. [24] | Evaluate the long-term efficacy and safety of botulinum toxin A in cervical dystonia patients over 3.5 years. | 34 patients with cervical dystonia. Botulinum toxin A injections every 12 weeks for 3.5 years. TWSE and PROM scores as primary outcomes. | Significant improvement in TWSE and PROM scores maintained over 3.5 years. Low rate (5.9%) of neutralizing antibodies, not affecting efficacy. | Botulinum toxin A is effective and safe for long-term treatment of cervical dystonia, with sustained efficacy and low risk of neutralizing antibody development. | IIa |
| Müller et al. [25] | Investigate the prevalence of neutralizing antibodies in spasticity patients treated with botulinum toxin A over 2.5 years. | 245 spasticity patients. Botulinum toxin A injections every 4–16 weeks. Patients divided into groups based on injection frequency. | Prevalence of antibodies increased from 0% at baseline to 15.9% at the end of the study. Highest antibody prevalence in patients with more frequent injections. | Repeated botulinum toxin A injections can lead to antibody development, especially with more frequent dosing, which may reduce subsequent treatment efficacy. | IIb |
| Bakheit et al. [26] | Examine factors influencing antibody development in spasticity patients receiving botulinum toxin A. | 143 spasticity patients. Botulinum toxin A treatment for an average of 24 months. Relationship between dose, treatment cycles, and antibody development analyzed. | Cumulative dose and number of treatment cycles were strong predictors of antibody development. Plateauing effect after 10 treatment cycles. | Total cumulative dose and number of treatment cycles are key factors in determining the risk of antibody development. Clinicians should consider these when planning treatments. | IIa |
| Schulte-Baukloh et al. [27] | Investigate antibody development in children and adolescents with detrusor overactivity receiving onabotulinumtoxinA injections. | 23 children/adolescents with detrusor overactivity. OnabotulinumtoxinA injections every 6–12 months. Antibodies tested using ELISA. | 30.4% developed antibodies with a mean duration of 6.8 months. No significant reduction in treatment response or increase in adverse effects in antibody-positive patients. | Antibody development can occur in children/adolescents after onabotulinumtoxinA injections, but its clinical relevance remains unclear. Further research is needed. | IIb |
| Study | Molecule | Indication | Sample Size | Antibody Formation | Impact on Efficacy | Conclusion |
|---|---|---|---|---|---|---|
| Rahman et al. (2022) [6] | Botulinum Toxin Type A | Multiple Indications | 24 studies | 10.1% | Varies across indications; repeated injections increase risk | Low incidence overall; further research needed on antibody formation mechanisms |
| Jankovic et al. (2023) [7] | OnabotulinumtoxinA (Botox) | Various | 34 studies | 10.3% | Higher with repeated injections; dose-related | Immunogenicity low but varies; significant influence from dosage and repetition |
| Kranz et al. (2008) [8] | Botulinum Toxin Type A | Dystonia | 50 patients | 44% | No significant decrease in treatment efficacy | Presence of antibodies does not predict loss of response |
| Wu et al. (2019) [9] | OnabotulinumtoxinA | Crow’s Feet Lines | 120 patients | Stable titers | Significant reduction in crow’s feet lines severity | Well-tolerated, no significant immunogenicity observed |
| Harii et al. (2008) [10] | Botulinum Toxin Type A | Glabellar Lines | 120 patients | Stable titers | Significant improvement in glabellar lines; no significant antibody development | Treatment effective with low immunogenicity |
| Coleman et al. (2012) [11] | AbobotulinumtoxinA | Cervical Dystonia | 44 patients | 25% immunoresistance | Significant decrease in clinical response | Monitoring for antibodies recommended; may need alternative treatments |
| Oshima et al. (2017) [12] | Botulinum Toxin Type A | Spastic Equinus Foot | 44 children | 60.9% | Higher risk with extended treatment schedule | Increased exposure to toxin over time may reduce treatment effectiveness |
| Tomic et al. (2021) [13] | Botulinum Toxin Type A | Various | Guinea pig model | High correlation | Mouse neutralization assay results positively correlated with antibody concentrations | MNA reliable for detecting neutralizing antibodies |
| Voller et al. (2004) [5] | Botulinum Toxin Type A | Dystonia | 21 patients | 71% positive sweat test | Reduced sweat production used as a marker for neutralizing antibodies | Simple, non-invasive test for detecting antibodies |
| Hefter et al. (2021) [16] | IncobotulinumtoxinA (Xeomin) | Cervical Dystonia | 35 patients | 60% at 4 years | No significant decrease in treatment efficacy despite antibody titers | Preparations without complexing proteins may lower antibody development risk |
| Schulte-Baukloh et al. (2008) [18] | Botulinum Toxin Type A | Detrusor Overactivity | 30 patients | 76.7% | Lower response in antibody-positive patients | Antibody formation common and may contribute to treatment failure |
| Bakheit et al. (2004) [21] | Botulinum Toxin Type A | Spasticity | 30 patients | Low incidence | Beneficial effects maintained after repeated cycles | Botulinum toxin A effective with sustained efficacy in long-term use |
| Albrecht et al. (2019) [22] | Botulinum Toxin Type A | Long-term Treatment | 134 patients | 34.6% | Significant reduction in treatment response | High prevalence of neutralizing antibodies after long-term treatment |
| Herrmann et al. (2004) [23] | Botulinum Toxin Type A | Children with Dystonia | 134 children | 27% | Significant reduction in response; higher risk of neutralizing antibodies | Clinicians should consider alternative treatments for children developing antibodies |
| Mohammadi et al. (2009) [24] | Botulinum Toxin Type A | Cervical Dystonia | 34 patients | 5.9% | No significant reduction in efficacy | Long-term treatment effective and safe with low neutralizing antibody formation |
| Müller et al. (2009) [25] | Botulinum Toxin Type A | Spasticity | 245 patients | 15.9% | Decreased treatment efficacy associated with antibody development | Clinicians should monitor antibody development, consider treatment frequency |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.W.A.; Chan, L.K.W.; Lee, A.W.K.; Lee, C.H.; Wan, J.; Yi, K.-H. Immunogenicity of Botulinum Toxin Type A in Different Clinical and Cosmetic Treatment, a Literature Review. Life 2024, 14, 1217. https://doi.org/10.3390/life14101217
Lee KWA, Chan LKW, Lee AWK, Lee CH, Wan J, Yi K-H. Immunogenicity of Botulinum Toxin Type A in Different Clinical and Cosmetic Treatment, a Literature Review. Life. 2024; 14(10):1217. https://doi.org/10.3390/life14101217
Chicago/Turabian StyleLee, Kar Wai Alvin, Lisa Kwin Wah Chan, Angela Wai Kay Lee, Cheuk Hung Lee, Jovian Wan, and Kyu-Ho Yi. 2024. "Immunogenicity of Botulinum Toxin Type A in Different Clinical and Cosmetic Treatment, a Literature Review" Life 14, no. 10: 1217. https://doi.org/10.3390/life14101217
APA StyleLee, K. W. A., Chan, L. K. W., Lee, A. W. K., Lee, C. H., Wan, J., & Yi, K.-H. (2024). Immunogenicity of Botulinum Toxin Type A in Different Clinical and Cosmetic Treatment, a Literature Review. Life, 14(10), 1217. https://doi.org/10.3390/life14101217






